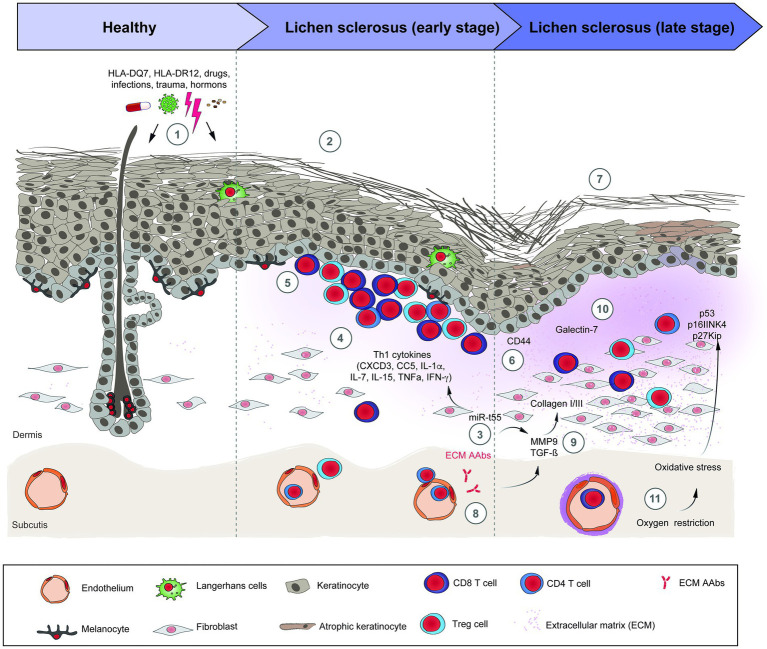
Figure 1.
Schematic overview of lichen sclerosus pathogenesis. (1) Risk factors for LS; (2) The inflammatory early stage of LS is unspecific and shows a dermoepidermal interface band of mostly T-cells. (3) miR-155 is overexpressed in LS, stimulates the Th1 profile and the dermal sclerosis. (4) Th1 cytokines implicated in the pathogenesis of LS. (5) Lichenoid infiltrate of TCD4+, TCD8+, and Tregs cells in the upper dermis. (6) Abnormal expression of CD44 in the epidermis and lichenoid infiltrate. (7) The sclerotic late stage of LS presents an atrophic epidermis, with comedo-like plugs and a cleft in the stratum corneum, dermal sclerosis, reduction and dilation of dermal vessels and the appendages disappear. (8) The autoantibodies against EMC1 may activate MMP9, which subsequently activates TGF-β. (9) TGF-β and BMP2 induce the synthesis of collagen I and III in fibroblasts. (10) Galectin-7 induces the synthesis of collagen I and III. (11) Along with inflammation, the vessel sclerosis contributes to the oxidative stress in LS, leading to downregulation of tumor suppressors genes and overexpression of p53 in the skin, factors related with the development of skin carcinomas. The precise sequence of events and their interactions are only incompletely understood. References: BMP2: bone morphogenetic protein 2; EMC1: extracellular matrix protein 1; LS: lichen sclerosus; MMP9: metalloproteinase 9; TGF-β: tumor growth factor beta. TNF-α: Tumor necrosis factor alpha.