Abstract
COVID-19, reduced funding and a shortage of healthcare workers has led to growing international concern about patient violence towards medical staff in medical settings. As the number of reported physical and verbal assaults increases, many medical staff are considering leaving their positions due to the resulting impact on their mental and physical wellbeing, creating a critical need to understand the causes for violence towards medical staff working on the front line. This study aims to examine the causes for patient violence towards medical staff in China during the COVID-19 pandemic. A case library was created containing twenty reported incidents of patient violence towards medical staff during the pandemic in China. Based on the Triadic Reciprocal Determinism (TRD) theory, we identify the personal, environmental, and behavioral factors, that cause incidents of violence towards medical staff. The outcome was set as ‘Medical Staff Casualties’, referring to whether, due to the violence experienced, the medical staff member was injured or died, or only experienced threatening or insulting behavior. Data was analyzed using Qualitative Comparative Analysis (QCA) to clarify the relationship between the different conditions and their relationship with the outcome. The study’s results reveal that Relationship Closeness is a necessary condition for patient violence in the presence of outcome. Secondly, four distinct types of causes for patient violence towards medical staff were identified: Strong Relationship Oriented Violence, Healthcare Resources and Services Mismatched Violence, Violence caused by Ineffective Patient-Physician Communication, and Ineffective Communication Superimposed Low Patient Compliance Violence. Scientific guidance is provided for the creation of measures to prevent future violence towards medical staff from occurring. Strict precautions should be taken for preventing violence to protect a healthy society and harmonious medical environment, emphasizing the need for joint governance of multiple participants.
Keywords: Workplace violence, Medical staff, Qualitative comparative analysis, Triadic reciprocal determinism
Introduction
Incidents of patient violence towards medical staff has increased significantly in recent years. This is often attributed to reduced healthcare funding, a shortage of healthcare workers and, more recently, an increase in the volume of patients due to COVID-19. Workplace hazards, such as falls and exposure to infectious diseases, is common in the medical sector, however violence towards medical staff, including physical and verbal abuse from patients and their relatives, is becoming more commonplace, creating long-term effects on staff psychological and physical well-being. Levels of exposure to violence is increasing in medical settings, resulting in more frequent patient-physician conflicts and a deterioration of the patient-physician relationship. The International Labor Organization (ILO) and the World Health Organization (WHO) have defined violence towards medical staff as those workers that experience verbal and physical attacks and threats towards them in the workplace. Despite duty of care provisions provided by healthcare providers, these experiences pose a clear or implicit challenge to staff safety, health and physical wellbeing (Wang et al., 2020). The common types of violence towards medical staff include physical violence, psychological violence, and sexual violence (Spector et al., 2014), which mainly include verbal attacks, threats and insults; sexual harassment and rape; and physical abuse of medical workers. In China, physical and psychological violence imparted by patients or their relatives is most common (Pich & Roche, 2020; Wang et al., 2020; Yesilbas & Baykal, 2021). Violence towards medical staff has serious adverse consequences for patients, physicians, hospitals and the general society. Firstly, violence can often result in increased hazards to medical staff, such as a reduction in their safety, feeling of disrespect and being unsafe. These experiences can have a long-term negative impact on their psychology and working state (Elamin et al., 2021; Yang et al., 2021a). Secondly, patient violence can negatively impact their subsequent treatment and overall healthcare (Roche et al., 2010). Thirdly, for the medical industry, it not only drives local medical talent away, but also destroys the order of public places (Du et al., 2020; Yang et al., 2021b). In this study, violence towards medical staff in China is defined as any violence behaviors medical staff experienced in their workplace, including but not limited to insults, threats or physical attacks by patients or their companions, resulting in physical or mental health harm, as well as disturbing normal medical work. The prevalence of violence towards medical staff and corresponding huge negative social impacts make explorations on the cause of patient violence worthwhile. It contributes to patient violence reduction, workplace environment improvement and good patient-physician relationship maintenance.
Violence towards medical staff is a complex and dynamic process, and the cause of patient violence is multi-folded. Scholars have identified various factors of violence towards medical staff. For example, Levin et al. used Ecological Occupational Health Framework to explain violence towards emergency department nurses, and found nurse factors, hospital factors, and social environment factors (Levin et al., 1998). Ramacciati et al. categorized the causes of violence towards emergency nurses into nurse factors, patient factors, and hospital organizational environment factors based on the Global Approach to Violence towards Emergency Nurses (GAVEN) (Ramacciati et al., 2018). Chapman et al. developed the STAMPEDAR (note: acronyms for the nine behavioral manifestations) violence assessment framework, which includes the patient’s behavioral presentation such as mumbling and pacing, as well as the patient’s mood and disease process, to help medical staff quickly identify patients with violent tendency and reduce violence in the workplace (Chapman et al., 2009). Generally, causes of patient violence towards medical staff can be divided into the following three aspects. First, at the patient aspect, individual’s characteristics are crucial. For example, patient’s disease severity (Cai et al., 2019; Liu et al., 2019), mental stability (Crilly et al., 2004; Vezyridis et al., 2015), and emotions (Ma et al., 2021). Patient’s poor education and low ethical standards (Li et al., 2017), and increased patients’ rights awareness (Yu et al., 2015) are identified as important factors contributing to patient violence. In addition, patient behavioral factors, including uncooperative treatment behavior (Zhang et al., 2021), refusal to communicate (Khan et al., 2021), and refusal to accept treatment results (Ma et al., 2021) are frequently mentioned. Second, at the physician perspective, physician’s characteristics, including inadequate knowledge of professional skills and unfriendly service attitudes (Cai et al., 2019), as well as physician’s inappropriate behavior, such as disrespect for patients (Shafran-Tikva et al., 2017) during healthcare service delivery are common factors. Third, the environmental factors include internal environment of patient-physician interaction, hospital environment, and social environment. The internal environment of interaction refers to information asymmetry (Kesavan et al., 2020). The hospital environment includes crowded conditions (He, 2014; Thomas et al., 2019), excessively long queues (Abdellah & Salama, 2017; Alhamad et al., 2021), and inadequate healthcare resources (Shafran-Tikva et al., 2017; Shaikh et al., 2020), which are highly likely to bring multiple adverse stimuli to patients in such noisy and dangerous situations. The social environment related factors, including expensive costs (Kesavan et al., 2020), negative media coverage (Jiao et al., 2015; Yu et al., 2015), and distorted social norms (Du et al., 2020), which lead to patients’ prejudice towards medical staff, eroded patient-physician trust (Qi, 2020; Tucker et al., 2015), and induces patient violence.
The COVID-19 pandemic has added significant strain to healthcare resources, including costs associated with healthcare provision. As a result, however, a new sphere of research has emerged for scholars to explore the determinants of violence towards medical staff during a major public health emergency. A study conducted in Egypt revealed that violence towards medical staff mainly occurred due to patients’ panic about the epidemic, shortage of healthcare resources, long waiting times, and poor communication (Arafa et al., 2021). Another study from Peru attributed frequent patient violence to the lack of healthcare service options during the pandemic (Del Carpio-Toia et al., 2021). In Pakistan, a systematic analysis of reports written during the first six months after the COVID-19 outbreak found that the reasons for violence towards medical staff is mainly due to patients’ distrust in physicians, inability to accept patient deaths, and resistance to epidemic prevention measures (Bhatti et al., 2021). Some scholars have also compared the underlying reasons that cause violence towards medical staff during the normal period (i.e., prior to COVID-19) and the COVID-19 pandemic. For instance, Garg et al. (2020) compared the causes of violence towards medical staff in Western India before and during the COVID-19 pandemic. Their results showed similar reasons in both instances, such as shortages in security personnel, poor construction of hospital facilities, and the poor ability of medical staff. The main differences, however, were attributed to overcrowding of hospital environments, long wait times, deterioration of patients’ condition, and poor quality of food received during hospital stay. In China, some studies have shown that patient-physician relationships have improved since the outbreak of COVID-19 (Hu et al., 2021) while the level of trust between patients and physicians has also enhanced (Chi et al., 2021; Gao et al., 2020; Zhou et al., 2021a). Zhou et al. (2021a) attributed these changes to Chinese citizens’ united fight against COVID-19 and the critical role played by medical staff on the front line. Similarly, positive reports from news outlets, as well as new medical policies, benefited citizens (Zhou et al., 2021b). However, as China’s government has attempted to control the spread of COVID-19, incidents of violence towards medical staff has continued (Devi, 2020; Xie et al., 2021). In this sense, further research is expected to identify the influencing mechanism of patient violence towards medical staff during a major public health crisis.
To sum up, firstly, most extant research has featured on patients (Du et al., 2020; Ma et al., 2019) or healthcare workers (Naveen Kumar et al., 2020; Seema et al., 2019) to determine the factors that cause patient violence towards healthcare workers by cross-sectional survey design (Garg et al., 2020; Shafran-Tikva et al., 2017; Spelten et al., 2020). However, the data collected is subjective and may not be universally accepted in reality. Secondly, many extant studies relied structural modeling approach to determine the factors and their influencing path on patient violence, as well as risk factors of healthcare workers’ exposure to patient violence (Cheung et al., 2017; Tian et al., 2020; Zhu et al., 2022). Although the complexity of violence towards medical staff requires significant further research into the interactions between influencing factors, extant research has focused predominantly on the roles of the independent factors rather than the combination of different conditions. Traditional approaches have failed to satisfy the need of coupling possible influencing factors to explain the causes of patient violence. This leads to the existing coping strategies for patient violence are much the same but slightly different, and poor guidance for practice. Additionally, the particular context of global COVID-19 pandemic provides new research potential. Therefore, this study aims to identify the determinants of patient violence towards medical staff from multiple cases collected during the COVID-19 pandemic in China. Specifically, building upon Triadic Reciprocal Determinism theory, this study explores the role of possible combinations of determinants in predicting violence using the QCA approach, and the proposed targeted strategies for patient violence reduction. The research questions are as follows. What are the coupling determinants leading to the increase in patient violence during the COVID-19 pandemic? and, how do they differ compared to the normal state, prior to the outbreak of COVID-19 periods?
Theoretical framework: triadic reciprocal determinism
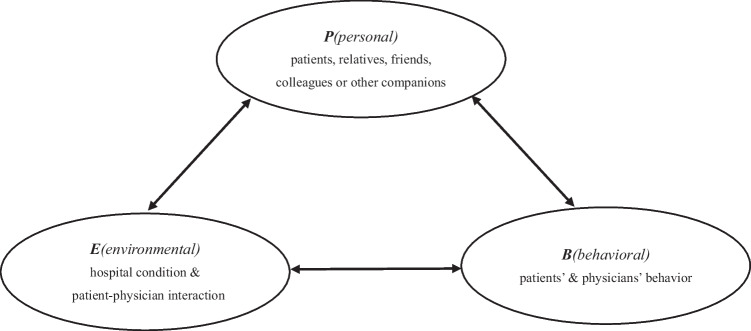
This study uses the Triadic Reciprocal Determinism theory, proposed by Albert Bandura in 1986, to explain the causes of patient violence towards medical staff in China during the COVID-19 pandemic. The TRD theory emphasizes the impact of personal factors, environmental factors, and behavioral factors, on human behavior, and posits that the three elements have relatively independent but interactive change relationships (Bandura, 1986). Personal factors include individuals’ perception of the environment and cognition of behavior, as well as other internal characteristics, such as thinking, self-evaluation, physiological response-ability, and cognitive ability (Guo & Jiang, 2008). Environmental factors mainly refer to external environmental factors and the internal objective environment between patients and physicians which affects the personal cognition and behavior of patients. The behaviors of individuals are an observable social activity and are expressed through action and language during communication. The TRD theory highlights the interaction mechanism among personal internal characteristic factors, external environmental factors, and personal behavioral factors which is the important theoretical basis for exploring the causes of violence towards medical staff and the relationship between the various factors (Fig. 1).
Fig. 1.
Triadic reciprocal determinism theory model
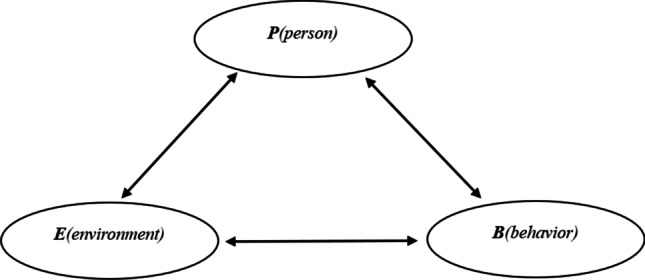
According to the TRD theory model, violence towards medical staff is essentially the result of the interaction between the patients’ personal factors, the environment, and the behavior during the patient-physician interaction. Throughout the medical treatment, any activities may contribute to the occurrence of violence behavior. In this study, we refer to personal factors as those pertaining to patients, including their relatives, friends, colleagues, or other companions. Personal factors include both attributes of individual characteristics such as severity of disease and stability of mental state, attributes of intimate relationships established between patients and other individuals in the current healthcare settings, and individual moral standards expressed through their certain behaviors. Environmental factors refer to the organizational factors within the healthcare settings, as well as factors within the patient-physician interaction, such as the information asymmetry within patient and physician during the healthcare service process. Behavioral factors represent both the patients’ and physicians’ behavior throughout the process of healthcare service delivery, i.e., the behavioral feedback that individuals provide in response to perceived environmental stimuli in a complex and dynamic healthcare delivery environment. As shown in Fig. 2, P represents personal factors, E represents environmental factors, and B represents behavioral factors. The two-way arrow between every two factors indicates their mutual connections. By analyzing the combined effects between different variables to investigate and explain the causes of patient violence behavior.
Fig. 2.
TRD-based analytical framework for patients’ violence
Patients’ experiences, perceptions, expectations, and evaluation of the healthcare services they receive are closely linked to their violence towards medical staff. Their behavior is always triggered by external stimuli (Bulle & Rode, 2018; Piraianu et al., 2021) which are workplace hazards, similar to risk of infection or slips and falls. In addition, external stimuli can be triggered by human interaction, such as verbal communication, physical contact, and conflicts. Due to differences in perceptions of the environment and patients’ cognitive behavior, their resulting behavior can be different. Under the various conditions experienced in medial settings, a minor issue can evolve into a violent action towards medical staff. For example, in a noisy overcrowded hospital environment, patients can experience extreme anxiety and tension, and fear for their health. If they see busy medical staff or experience long wait times, they are more likely to develop dissatisfaction. Once a small external stimulus is triggered, their emotions are likely enhanced. Consequently, the medical staff (i.e., the direct contact with patients) will bear most of the anger and violence that ensues. In return, the unfriendly behavior will exacerbate already intense patient-physician conflicts and erode the established trust between patients and physicians.
Method
Qualitative comparative analysis
This study employs a qualitative comparative analysis (QCA) approach, proposed by Charles Ragin in 1987, to examine the determinants of patient violence towards medical staff during the COVID-19 pandemic in China. The QCA approach, widely used in social sciences research, contributes to exploring multiple concurrent causalities through a small or medium-sized case comparison, usually with 10–40 samples to meet research needs (Rihoux & Ragin, 2008). QCA expands the analytical framework of causality (Furnari et al., 2021; Rihoux & Ragin, 2008). First, the assumption of concurrent causality replaces the ideology of a single factor acting independently. Second, multiple combinations of antecedents have equivalent effects on the emergence of a particular outcome. Again, causal effects are no longer consistent, the antecedent variable exerts positive or negative utility depending on its combination with other conditions. Finally, QCA emphasizes the asymmetry of causes, i.e., the emergence or non-emergence of an outcome may require different combinations of causes to explain it separately. In sum, QCA can better explain the heterogeneity across cases, as well as the complex configuration effect between conditions (Huo & Li, 2022), which is the highlight of this study in exploring the causes of violence towards medical staff. By using QCA, it allows us to assess the influence of possible factor combinations for the exploration of the mechanism of multiple factors regarding a specific research question (Ragin, 1987).
The more widely used QCA analysis techniques include crisp-set QCA (csQCA), multi-value set QCA (mvQCA), and fuzzy-set QCA (fsQCA). The csQCA calibrates variables as dichotomous variables, assigned 0 or 1. While, mvQCA is an extension of csQCA, allowing multi-valued variables, and fsQCA introduces the concept of set affiliation, representing the degree to which different cases belong to a certain set through fuzzy set scores. This study adopted csQCA method for analysis to elucidate the mechanisms of patient violence towards medical staff. It can reduce the complexity of the phenomenon by measuring the presence or absence of variables and has a greater advantage in studies dealing with small to medium-sized sample sizes (Kogut & Ragin, 2006; Roig-Tierno et al., 2017).
Data collection
As part of this study, we created a case library containing incidences of patient violence towards medical staff during the COVID-19 pandemic in China. The time period in which cases were collected was from 1 December, 2019, to 1 July, 2020. This period was chosen as it captures the entire first wave of the epidemic in China. Meanwhile, incidents of patient violence towards medical staff received significant attention from media outlets and the public during COVID-19 which can help in providing sufficient information and case novelty. Since the causes of patient violence may vary between private and public hospitals, we limit our search to public hospitals in China. To ensure the completeness and accuracy of each case, we collected the case information across different channels, including Sina Weibo, WeChat, Toutiao.com, and other websites. The search strategy employed used the following key phrases: patient’s violence, medical disputes, violence against medical staff, and violence in hospitals. In the process of searching for the cases, we also cross-checked the case reports, comments, and all other relevant information from different sources. In addition, efforts were made to ensure the heterogeneity of cases by searching for as many potential cases as possible.
A case library containing twenty-six cases was initially created after retrieving information pertaining to violent incidents that were widely reported in the media. After this, further selection criteria were applied, including: (1) the patient violence towards medical staff occurred in China; (2) the patients and physicians exposed to the violent incidents have an established connection i.e., they are engaged in the delivery or receiving of healthcare services; (3) the case information collected is sufficient for analysis purposes, including a storyline, causes, development process, and consequences. As a result, six cases were removed following this screening process (see Table 9 in the Appendix for details). In one case, the patient and physician did not commence the delivery of the healthcare service and, therefore, we determined that they did not establish a real patient-physician relationship. In addition, the other five cases did not report sufficient information, such as the causes and process of violence.
Table 9.
Details of the eliminated cases
| Number | Date | Case | Elimination reason |
|---|---|---|---|
| 1 | 2020.1.26 |
The First Affiliate Hospital of Guangzhou Medical University Patient held a nurse with a syringe and needles for the purpose of seeing experts. |
Unprovoked provocation and the cause described vaguely in the report. |
| 2 | 2020.2.27 |
Funing People’s Hospital Drunken patient pushed and insulted medical staff without reason and scratched physician who came to persuade them. |
Unprovoked provocation and the cause described vaguely in the report. |
| 3 | 2020.3.19 |
Ordos Central Hospital Patient with a long history of renal failure stabbed the physician premeditated with a knife. |
Unprovoked provocation and the cause described vaguely in the report. |
| 4 | 2020.3.28 |
Ganzhou Fifth People’s Hospital Patient asked the physician to issue a disease certificate. The physician refused because of insufficient information and unwilling examination. |
No medical service relationship exists between the patient and physician. |
| 5 | 2020.4.7 |
Hospital in Liwan District, Guangzhou Patient insulted a nurse because of negative emotion. |
Unprovoked provocation and the cause described vaguely in the report. |
| 6 | 2020.6.8 |
Baofeng Maternal and Child Health Hospital Two drunken patients with knives went into the hospital for treatment, and threatened and insulted nurses without reason. |
Unprovoked provocation and the cause described vaguely in the report. |
In total, twenty cases were included in the case library (see Table 10 in the Appendix for details). The time period for these was from 24 December, 2019, to 22 June, 2020. The cases occurred across 15 cities and 12 provinces in China, of which Beijing had the most cases (30%), followed by Hubei Province (15%) and Sichuan Province (10%). The result of all incidents can be divided into two types: medical staff casualties and no casualties. With regards the identity of those committing violence towards medical staff, 19 cases involved patients or their relatives, of which the patient or their immediate relatives accounted for 63%. In terms of the rank of hospital where violence occurred, cases included not only first-level hospitals in small villages, but also tertiary level hospitals in first-tier Chinese cities. Specifically, the case library included one first-level hospital, two secondary hospitals, and seventeen tertiary level hospitals, including twelve tertiary first-class hospitals.
Table 10.
Case library details
| Number | Date | Case | Outcome | Place | Hospital rank |
|---|---|---|---|---|---|
| C1 | 2019.12.24 |
Civil Aviation General Hospital Patient’s family suspected physician of repeatedly refusing examination and treatment results. The patient’s son was dissatisfied and killed the physician using a knife. |
Physician died | Beijing | Tertiary hospital |
| C2 | 2019.12.29 |
Chang’an Hospital The nurse prevented a man who took their child to the emergency department to see a doctor from queue jumping. During skin testing, the child cried and the parents beat the nurse as they believe the nurse was acting in retaliation. |
Nurse sustained injuries |
Xian City, Shanxi Province |
Tertiary hospital |
| C3 | 2020.1.1 |
Peking University People’s Hospital Patient’s family was dissatisfied that they were prevented from jumping in line and claimed to cut the physician. |
No casualties | Beijing | Tertiary hospital |
| C4 | 2020.1.1 |
Second Hospital of Shanxi Medical University The emergency attendant was stabbed by a drunken patient’s companion. |
Nurse sustained injuries | Taiyuan City, Shanxi Province | Tertiary hospital |
| C5 | 2020.1.10 |
Sichuan Provincial People’s Hospital Patient was anxious to leave the hospital while her medical insurance was not reviewed and did not meet the discharge conditions. The patient believed that the physician deliberately created difficulties and neglected them. As a result, her husband attacked the physician. |
Physician sustained injuries | Chengdu City, Sichuan Province | Tertiary hospital |
| C6 | 2020.1.16 |
Zhangqiu District Maternal and Child Health Hospital Patient’s parents were dissatisfied with the routine withdrawal of infusion pillows and decided to insult and beat the nurse. |
Nurse sustained injuries | Jinan City, Shandong Province | Tertiary hospital |
| C7 | 2020.1.17 |
Hejiang People’s Hospital Patient’s family threatened to kill the physician if they failed to resuscitate the patient. The patient, who had massive myocardial infarction, died and the patient’s husband, sister and son, beat the physicians. |
Three physicians sustained injuries | Luzhou City, Sichuan Province | Tertiary hospital |
| C8 | 2020.1.19 |
Jingmen No.1 People’s Hospital Patient’s family questioned the physician’s treatment process after the patient died in a car accident. Subsequently, they beat the physician and forced them to kneel. |
Physician sustained injuries | Jingmen City, Hubei Province | Tertiary hospital |
| C9 | 2020.1.20 |
Beijing Chao Yang Hospital Patient resented their physician and took revenge using a knife as their eye examination results did not meet their expectations. |
Two physicians sustained injuries | Beijing | Tertiary hospital |
| C10 | 2020.1.29 |
Wuhan Fourth Hospital Patient’s family clashed with the hospital due to transfer. The patient died during the night and, as a result, the patient’s son-in-law was sad and beat the medical staff. |
Nurse and physician sustained injuries | Wuhan City, Hubei Province | Tertiary hospital |
| C11 | 2020.2.1 |
Xinyu People’s Hospital Patient’s son believed that the physician did not diagnose and treat the patient in time and repeatedly accused the physician for no reason. This caused disturbance to normal order in the hospital. |
No casualties | Xinyu City, Jiangxi Province | Tertiary hospital |
| C12 | 2020.2.6 |
Caoyankou Health Center The physician reminded the patient’s son who came to visit the patient after drinking to wear a mask and stopped them from smoking in the oxygen treatment ward. The patient’s son became dissatisfied and beat the physicians. |
Two physicians sustained injuries | Yancheng City, Jiangsu Province | First-level hospital |
| C13 | 2020.3.2 |
Shangdu County People’s Hospital Drunken patients repeatedly molested and beat the female healthcare workers when receiving medical treatment. |
Medical worker sustained injuries | Wulanchabu City, Neimenggu Province | Secondary hospital |
| C14 | 2020.3.7 |
Shengjing Hospital of China Medical University During the patient’s rescue from a traffic accident, the patient’s husband argued with the physician and beat them due to nursing problems. |
Physician sustained injuries | Shenyang City, Liaoning Province | Tertiary hospital |
| C15 | 2020.3.27 |
Hanchuan People’s Hospital Two COVID-19 rehabilitation patients disputed with a physician and injured them due to the long wait time. |
Physician sustained injuries | Hanchuan City, Hubei Province | Tertiary hospital |
| C16 | 2020.4.1 |
Guangzhou Eighth People’s Hospital A foreign patient diagnosed with COVID-19 ignored the nurse’s notification about the blood test and tried to follow the nurse to forcibly leave the isolation ward. The patient was stopped by the nurse and, as a result, pushed the nurse down and bit them. |
Nurse sustained injuries | Guangzhou City, Guangdong Province | Tertiary hospital |
| C17 | 2020.4.29 |
Peking University Third Hospital Yanqing Hospital Patient asked to be discharged after completing hospital procedures. Considering the physical condition of the pregnant woman, the physician refused stating that the patient required further observation. The patient’s husband became dissatisfied and yelled and beat the physician. |
Physician sustained injuries | Beijing | Secondary hospital |
| C18 | 2020.5.25 |
Beijing Yanhua Hospital Patient had a dispute with the physician on duty due to the order of treatment and hurt the physician. |
Physician sustained injuries | Beijing | Tertiary hospital |
| C19 | 2020.5.28 |
Peking University First Hospital Patient’s family was dissatisfied with the operation arrangements and injured the physician that communicated with them. |
Physician sustained injuries | Beijing | Tertiary hospital |
| C20 | 2020.6.22 |
The First Affiliated Hospital of Zhengzhou University Patient believed that their disease was caused by the improper diagnosis and treatment by the physician and complained that the disease was not cured. The contradiction remained unsolved and the patient took revenge on the physician using a knife. |
Two physicians sustained injuries | Zhengzhou City, Henan Province | Tertiary hospital |
Coding scheme
The study’s outcome was set to Medical Staff Casualties. Violence reported in the cases included injuries or deaths of medical staff, as well as verbal threats or insults. Eighteen cases reported casualties while two cases reported no casualties. In considering the outcome of the violence with casualties, we set those cases that resulted in the injury or death of medical staff as 1 and those that reported no casualties as 0. Building on the theoretical framework proposed in this study, we identified the conditions associated with personal factors (i.e., Disease Severity, Mental Stability, Relationship Closeness, and Moral Standard), environmental factors (i.e., Insufficient Resources, Hospital Rank, Information Asymmetry, and Treatment Experience), and behavioral factors (i.e., Inappropriate Service Behavior, Psychological Deviant Behavior, Patient Cooperativeness, and Patient-Physician Communication).
Personal factors refer to individuals’ characteristics and the internal driving force for their responsive behavior. These include the Disease Severity, Mental Stability, Relationship Closeness, and Moral Standard of the person committing the violence towards medical staff.
Disease severity
The health condition of the patient has long been regarded as a crucial determinant for violence towards medical staff (Ma et al., 2019). It is believed that hospital emergency departments have a much higher risk of experiencing patient violence towards their medical staff as patients are more likely to experience critical healthcare issues (Cai et al., 2019; Liu et al., 2019). In general, patients with acute and severe conditions attach more significance to their diagnosis and therapeutic effect. In addition, violence is more likely to occur during uncertain events, such as when physicians relay upsetting news. In this study, if the patient’s disease is critical (i.e., the case reported that the patient has a severe disease, the patient requires emergency rescue or surgical treatment), it was coded as 1, otherwise 0.
Mental stability
Mental stability refers to the mental condition of the person committing the violence towards medical staff and highlights the individual’s capacity to remain rational when solving conflicts (Shafran-Tikva et al., 2017). In general, if patients or their companions maintain a calm state of mind, they are less likely to assault medical staff. On the contrary, if they are in a poor mental state (e.g., mental disorder, drunk, drug abuse, or suffer from long-term illness), they are likely to have less tolerance and can be easily irritated and become violence (Crilly et al., 2004; Vezyridis et al., 2015). In this study, if the mental stability of the perpetrator is unreliable, as demonstrated by drunkenness, drug abuse, or mental disorder, it was coded as 1, otherwise 0.
Relationship closeness
Relationship closeness describes the relationship between the patient and their companions during healthcare delivery. Evidence shows that the perpetrators of violence against medical staff are mainly the patients and their relatives, for instance, parent-child relationships and brother-sister relationships (Aljohani et al., 2021; Byon et al., 2021). Compared to other forms of relationship, a close relationship with the patient is more likely to develop much stronger empathy and attack medical staff with unpleasant treatment experiences. In this study, if the perpetrators are the patients and / or their relatives, it was coded as 1, otherwise 0.
Moral standard
An individual’s moral standards refer to their ability to follow social values, including respecting others and being compliant with hospital rules. For those being violent towards medical staff, they may demonstrate early signs of unfriendly behavior due to low moral standards. This behavior is frequently reported in previous literature on patient violence, including e.g., patients ignoring hospital rules regarding smoking or queuing (Li et al., 2017). Once their requests are refused, they are more likely to develop violent behavior. In this study, if patients or their companions cut in line, accuse medical staff for no reason, smoke in public places, or make unreasonable demands, it was coded as 1, otherwise 0.
Environmental factors include both the hospital environment, in terms of the medical facilities and resources, and the internal environment patients experience during the healthcare service process. They are demonstrated in Insufficient Resources, Hospital Rank, Information Asymmetry, and Treatment Experience.
Insufficient resources
Insufficient resources refer to the division between the healthcare demands of patients and their corresponding service providers e.g., shortages in healthcare professionals (Singh et al., 2019). Due to the imbalanced economic development level across eastern and western cities in China, the total amount of high-quality healthcare resources is relatively insufficient in less-developed western China which leads to maladjustment and mismatch between healthcare service provision and public demand (Chai et al., 2020). In addition, the siphon effect of large hospitals in large cities has further widened the imbalance of healthcare resources. Qualified medical staff, advanced medical equipment and facilities, high-quality healthcare resources, and drugs are relatively concentrated (Yu et al., 2021). However, this misallocation of resources means that hospitals with insufficient resources are less likely to satisfy the demands of patients and are more likely, therefore, to experience patient violence towards medical staff. In this study, if the hospital is described as facing a shortage of medical staff, holding patients exceeding capacity, or low efficiency in the case, it was coded as 1, otherwise 0.
Hospital rank
In China, hospitals are classified into different ranks considering their amount of healthcare resources, capacity, and service population size. In general, the higher the rank of hospital, the better the healthcare service received by patients. However, excessive medical treatment from physicians in high-rank hospitals happens frequently (He, 2014). If patients suffer unfair treatment, they may demonstrate bad emotions, leading to conflicts or violent attacks. In this study, we assign violence occurred in tertiary hospitals as 1, otherwise 0.
Information asymmetry
The healthcare knowledge gap between patients and physicians is widely acknowledged (Kesavan et al., 2020). During diagnosis and treatment of patients, it is difficult for physicians to answer all patient’s concerns. In addition, as most patients use the Internet frequently, they may find it difficult to distinguish between misleading health information and information provided by their physician. The inability to appropriately understand the physician’s explanation and their blind trust in alternative health information found online make patients less confident in physicians. In this study, if the cases have emphasized the sharp differences in the healthcare knowledge gap, it was coded as 1, otherwise 0.
Treatment experience
Treatment experience is directly connected to the hospital environment, including the hospital’s facilities and the attitude of medical staff encountered (Li et al., 2017). It is demonstrated as a hospital’s noisy environment and crowded space (Darawad et al., 2015; Thomas et al., 2019), long wait times (Abdellah & Salama, 2017; Raveel & Schoenmakers, 2019), and poor guidance provided at reception. All these factors may cause patients to experience negative emotions towards physicians with possible violence ensuing. In this study, if the cases state the reason as long waiting time or dissatisfaction with the physician’s treatment, experiencing conflicts and quarrels with medical staff, it was coded as 1, otherwise 0.
Behavioral factors concern the interactive behavior and consequences experienced by the patient. They are demonstrated in Inappropriate Service Behavior, Psychological Deviant Behavior, Patient Cooperativeness, and Patient-Physician Communication.
Inappropriate service behavior
In the process of receiving healthcare services, some inappropriate behavior of physicians may be experienced by patients e.g., an unfriendly behavior may lead patients to become violent (Shafran-Tikva et al., 2017). Specifically, it can be the physician’s avoidance of patients, refusal of patient registration, ironic language usage and others. In this study, if the report emphasized an existence of physician’s inappropriate service behavior, it was coded as 1, otherwise 0.
Psychological deviant behavior
Psychological deviant behavior is deeply rooted in the culture that physicians portray when solving patient problems (Ma et al., 2021). It is caused by the unrealistic expectation of patients towards healthcare services, such as expecting a higher quality of physician or hospital. If the treatment effect fails to satisfy the patient’s expectations, a psychological deviation tendency is likely to be present. In a typical case, patients develop moderate or high resistance to the treatment effect and demand a detailed explanation which can easily induce violent behavior. In this study, if the report indicates that the patient refused the treatment result, it was coded as 1, otherwise 0.
Patient cooperativeness
Patient cooperativeness refers to a patient’s compliance with physicians and their cooperation with the physicians’ treatment plan. If the patient demonstrates a low willingness to cooperate with the physician, patient-physician conflict is likely to occur and lead to violence (Zhang et al., 2021). In this study, if the report demonstrates that the patient did not obey the treatment plan, it was coded as 1, otherwise 0.
Patient-physician communication
Patient-physician communication refers to the two-way interaction between patients and physicians, which requires time and energy to support. Insufficient or unsuccessful communication between the two parties is often observed in healthcare settings (Khan et al., 2021; Zhang et al., 2021). Failure to effectively establish patient-physician communication may result in patients becoming violent. In this study, if the case highlighted failed or insufficient patient-physician communication, it was coded as 1, otherwise 0.
By following the instructions of the csQCA approach, each condition was created into a dichotomized variable. Table 1 provides the details.
Table 1.
Coding and judgment description
| Type | Element | Variable | Explanation | Coding |
|---|---|---|---|---|
| Conditional variables | Personal factors |
Disease Severity DS |
Patient has a severe disease; patient requires emergency rescue or surgical treatment. | 1 |
| Patient does not have a severe disease. | 0 | |||
|
Mental Stability MTS |
Perpetrator’s mental stability is unreliable, demonstrated by drunkenness, drug abuse or mental disorder. | 1 | ||
| Perpetrator’s mental stability is reliable. | 0 | |||
|
Relationship Closeness RC |
Perpetrator is the patient himself or his relative. | 1 | ||
| Perpetrator is a friend or colleague or other, not kinship, with the patient. | 0 | |||
|
Moral Standard MRS |
Perpetrator has low moral standards and demonstrates unfriendly behavior. | 1 | ||
| Perpetrator demonstrates friendly behavior in line with moral standards. | 0 | |||
| Environmental factors |
Insufficient Resources IR |
The hospital has a shortage in medical staff, inability to accommodate excess patients or low efficiency. | 1 | |
| The hospital has no shortage of resources. | 0 | |||
|
Hospital Rank HR |
Tertiary hospital. | 1 | ||
| Non-tertiary hospital. | 0 | |||
|
Information Asymmetry IA |
Sharp differences in the healthcare knowledge gap between patients and physicians. | 1 | ||
| No healthcare knowledge gap. | 0 | |||
|
Treatment Experience TE |
Long waiting time or unsatisfactory treatment received. | 1 | ||
| Good treatment experience. | 0 | |||
| Behavioral factors |
Inappropriate Service Behavior ISB |
Physicians show inappropriate service behavior. | 1 | |
| Physicians show appropriate service behavior. | 0 | |||
|
Psychological Deviant Behavior PDB |
Patient refuses to accept the treatment results. | 1 | ||
| Patient receives the results willingly. | 0 | |||
|
Patient Cooperativeness PC |
Patient does not obey the physician’s medical plan. | 1 | ||
| Patient obeys the physician’s medical plan. | 0 | |||
|
Patient-Physician Communication PPC |
Failed or insufficient patient-physician communication. | 1 | ||
| Effective patient-physician communication. | 0 | |||
| Outcome variable |
Medical Staff Casualties MSC |
Medical staff is injured or died because of the violence. | 1 | |
| Medical staff is only threatened or insulted by words. | 0 |
Results
Analysis of normal necessity and sufficiency
Firstly, the normal analysis of necessity and sufficiency was performed for each condition in the presence of Medical Staff Casualties. The sufficient condition refers to the presence of a condition that can predict the expected outcome, but is not the only cause of the outcome. The necessary condition predicts the outcome in combination with other conditions, and the necessary condition appears in all such combinations (Heidrich & Bandelow, 2019; Schneider & Wagemann, 2012). Consistency and coverage are two indicators for the judgment of necessity or sufficiency between conditions and outcome (Ragin, 2006). Superscript (*) indicates that the condition meets or exceeds the consistency requirement of 0.90, which can be considered a necessary condition for the outcome in QCA analyses (Ragin, 2000). Table 2 shows that Relationship Closeness is a necessary condition for patients’ violence to cause physicians to be injured or die, which can be explained by the existence of the Relationship Closeness in all conditional configurations leading to the violence. However, this does not mean that the stronger relationship, the more likely violence is to occur. Since patients’ violence towards medical staff is the result of the interaction of numerous factors, it is necessary to further examine the configurations of all conditions at the same time. This study, therefore, explores the configurations of conditions to reveal the causes and mechanisms of patients’ violence towards medical staff during the COVID-19 pandemic in China.
Table 2.
Analysis of necessary conditions
| Condition | Medical Staff Casualties (MSC) | ||
|---|---|---|---|
| Consistency | Coverage | ||
| Disease severity | DS | 0.50 | 0.90 |
| ~DS | 0.50 | 0.90 | |
| Mental stability | MTS | 0.22 | 1.00 |
| ~MTS | 0.78 | 0.88 | |
| Relationship closeness | RC | 0.94* | 0.89 |
| ~RC | 0.06 | 1.00 | |
| Moral standard | MRS | 0.72 | 0.87 |
| ~MRS | 0.28 | 1.00 | |
| Insufficient resources | IR | 0.11 | 0.67 |
| ~IR | 0.89 | 0.94 | |
| Hospital rank | HR | 0.83 | 0.88 |
| ~HR | 0.17 | 1.00 | |
| Information asymmetry | IA | 0.56 | 1.00 |
| ~IA | 0.44 | 0.80 | |
| Treatment experience | TE | 0.67 | 0.92 |
| ~TE | 0.33 | 0.86 | |
| Inappropriate service behavior | ISB | 0.17 | 0.75 |
| ~ISB | 0.83 | 0.94 | |
| Psychological deviant behavior | PDB | 0.28 | 1.00 |
| ~PDB | 0.72 | 0.87 | |
| Patient cooperativeness | PC | 0.61 | 1.00 |
| ~PC | 0.39 | 0.78 | |
| Patient-physician communication | PPC | 0.78 | 0.93 |
| ~PPC | 0.22 | 0.80 | |
~ represents the absence of a condition or the logical operation “NOT”
* Meets 0.90 consistency requirement for necessary condition
Source: Processed with the fsQCA 3.1b software
Standard analysis
For QCA, the number of condition combinations increases exponentially with the addition of condition variables (Rihoux & Ragin, 2008). This study identified three condition variables, and the number of possible logical condition combinations exceeds the number of existing cases. Direct QCA analysis of 12 conditions may yield complex combinations, and fail in effective theoretical refinement. Followed the practice on addressing the problems (Zhu & Wang, 2020), this study investigates critical factors causing patient violence in terms of personal factors, environmental factors, and behavioral factors, as well as their possible combinations, building upon TRD theory.
Standard analysis was completed in the presence of Medical Staff Casualties. Intermediate solutions were created and selected that were superior to both parsimonious solutions and complex solutions (Rihoux & Ragin, 2008) to complete subsequent configurations. Ragin (1987) proposed that the results are good when the consistency value of the intermediate solution is above 0.8 and the coverage value is above 0.5. We also built truth tables that are critical to QCA to explain the presence of patients’ violent behavior. Truth tables are an analysis tool based on the principle of formal logic (Smela & Sejkora, 2022), which can demonstrate all possible condition combinations and states in the result set, as well as the number of cases in each configuration (Kahwati & Kane, 2018). QCA requires that the minimum case frequency threshold should be set to 1 or 2 when the sample size is relatively small (Ragin, 1995). Considering the number of cases in this study and avoiding extreme case configurations, we set the minimum case frequency threshold to 2, meaning that we only included configurations with 2 or more cases. The consistency threshold value was set to the default value of 0.8 (Rihoux & Ragin, 2008), which means that configurations with PRI (Proportional Reduction in Inconsistency) consistency less than 0.8 in the outcome column were coded as 0.
With regards personal factors, two configurations can lead to medical staff being injured or dying (coverage: 0.89, consistency: 0.89). Configuration A1 indicates that strong relationship closeness and reliable mental stability leads to the injury of medical staff. In configuration A2, the combination of low disease severity, strong relationship closeness, and low moral standard, stimulates violence from patients.
Configurations A1 and A2 can be combined as MSC=A1+A2=~MTS*RC+~DS*RC*MRS=RC*(~ MTS + ~ DS*MRS). The Relationship Closeness can be regarded as the necessary condition for personal factors to affect the outcome. The Disease Severity, Mental Stability, and Moral Standard can influence the outcome combined with Relationship Closeness. From the twenty cases reviewed, nineteen incidents of violence were committed by the patients themselves and / or their relatives. Therefore, timely detection and soothing of patients’ and their companions’ emotions plays a pivotal role in avoiding contradictions and violence towards medical staff (Tables 3 and 4).
Table 3.
Truth Table A
| DS | MTS | RC | MRS | Number | MSC |
|---|---|---|---|---|---|
| 0 | 0 | 1 | 0 | 2 | 1 |
| 1 | 0 | 1 | 0 | 2 | 1 |
| 0 | 1 | 1 | 1 | 2 | 1 |
| 0 | 0 | 1 | 1 | 6 | 1 |
| 1 | 0 | 1 | 1 | 6 | 1 |
Source: Processed using the fsQCA 3.1b software
Table 4.
Configurations of personal factors
| Conditional configuration | Raw coverage | Unique coverage | Solution consistency | Solution coverage | |
|---|---|---|---|---|---|
| A1 | ~MTS*RC | 0.78 | 0.5 | 0.89 | 0.89 |
| A2 | ~DS*RC*MRS | 0.39 | 0.11 |
~ represents the absence of a condition or the logical operation “NOT”
* represents the intersections of a condition or the logical operation “AND”
+ represents the logical operation “OR”
Source: Processed using the fsQCA 3.1b software
With regards environmental factors, two configurations were identified as being able to describe the conditions that cause medical staff injury or death (coverage: 0.56, consistency: 1). Configuration B1 indicates that the combination of sufficient resources, high-rank hospital, and unsatisfactory treatment experience leads to patient violence towards medical staff. Configuration B2 indicates that the combination of sufficient resources, high-rank hospital, and high information asymmetry stimulates violent behavior.
Configurations B1 and B2 can be combined as MSC = B1 + B2 = ~ IR*HR*TE + ~ IR*HR*IA = HR*~IR*(TE + IA). The combination of HR and ~ IR appears as the necessary condition for environmental factors to affect the outcome, just as we know that the higher the rank of a hospital usually has sufficient medical supplies in our real life. From the twenty cases reviewed, fourteen had the necessary combination (Tables 5 and 6).
Table 5.
Truth Table B
| IR | HR | IA | TE | Number | MSC |
|---|---|---|---|---|---|
| 0 | 1 | 1 | 1 | 6 | 1 |
| 0 | 1 | 0 | 0 | 4 | 0 |
| 0 | 1 | 1 | 0 | 2 | 1 |
| 0 | 1 | 0 | 1 | 2 | 1 |
| 1 | 1 | 0 | 1 | 2 | 0 |
Source: Processed using the fsQCA 3.1b software
Table 6.
Configurations of environmental factors
| Conditional configuration | Raw coverage | Unique coverage | Solution consistency | Solution coverage | |
|---|---|---|---|---|---|
| B1 | ~IR*HR*TE | 0.44 | 0.11 | 1 | 0.56 |
| B2 | ~IR*HR*IA | 0.44 | 0.11 |
~ represents the absence of a condition or the logical operation “NOT”
* represents the intersections of a condition or the logical operation “AND”
+ represents the logical operation “OR”
Source: Processed using the fsQCA 3.1b software
Regarding behavioral factors, three configurations can explain the conditions that lead to medical staff being injured or dying (coverage: 0.72, consistency: 0.93). Configuration C1 indicates that the combination of appropriate service behavior, no psychological deviant behavior, and ineffective patient-physician communication results in medical staff casualties. Configurations C2 and C3 demonstrate that the combinations of low patient cooperativeness and ineffective patient-physician communication, with appropriate service behavior or no rejection of the treatment results, brings about the patient’s violent behavior. Based on configuration C1, configurations C2 and C3 superimpose the situation that patients do not cooperate with physicians during the treatment process, which means that the situation and likelihood of violent behavior towards medical staff is more detailed.
Configurations C1, C2 and C3 can be combined as MSC = C1 + C2 + C3 = ~ ISB*~PDB*PPC + ~ PDB*PC*PPC + ~ ISB*PC*PPC = PPC*(~ ISB*~PDB + ~ PDB*PC + ~ ISB*PC). Obviously, Patient-Physician Communication can be regarded as an important condition for behavioral factors affecting the outcome. It forms three paths that ultimately led to medical staff casualties by combining any two conditions. In this study, 75% of cases showed ineffective communication between patients and physicians. When receiving healthcare services, patients have the right to choose their diagnosis and treatment plan on the premise that they receive clear guidance about the associated risks. However, this cannot be used as an excuse for patients not to cooperate with physicians. If the patients question the physician’s advice or refuses to cooperate, and the communication and mediation with the physician are ineffective, the unpredictable conditions can cause unnecessary trouble (Tables 7 and 8).
Table 7.
Truth Table C
| ISB | PDB | PC | PPC | Number | MSC |
|---|---|---|---|---|---|
| 0 | 0 | 1 | 1 | 4 | 1 |
| 0 | 1 | 1 | 1 | 3 | 1 |
| 1 | 0 | 1 | 1 | 2 | 1 |
| 0 | 0 | 0 | 1 | 5 | 1 |
Source: Processed using the fsQCA 3.1b software
Table 8.
Configurations of behavioral factors
| Conditional configuration | Raw coverage | Unique coverage | Solution consistency | Solution coverage | |
|---|---|---|---|---|---|
| C1 | ~ISB*~PDB*PPC | 0.44 | 0.22 | 0.93 | 0.72 |
| C2 | ~PDB*PC*PPC | 0.33 | 0.11 | ||
| C3 | ~ISB*PC*PPC | 0.39 | 0.17 |
~ represents the absence of a condition or the logical operation “NOT”
* represents the intersections of a condition or the logical operation “AND”
+ represents the logical operation “OR”
Source: Processed using the fsQCA 3.1b software
Robustness check
Robustness check is crucial in QCA analysis (De Marchi et al., 2022; Wu et al., 2021). The most common testing method is to adjust relevant parameters, such as consistency threshold value and minimum case frequency threshold (Waldkirch et al., 2021; White et al., 2021). In this study, the robustness check is performed by comparing the combination of variables and the differences in parameters of the configurations in the before and after results (Schneider & Wagemann, 2012). Following previous studies, this study conducted the robustness check by adjusting the consistency threshold value from 0.8 to 0.82 (Huo & Li, 2022). Results showed that there was no difference in the before-after comparison between the configurations of personal and environmental factors, and the configuration of environmental factors changed, but the important roles of two variables, Patient Cooperativeness and Patient-Physician Communication, remained prominent. Therefore, our results are robust.
Discussion
Patient violence towards medical staff has become an increasingly common occurrence in healthcare settings worldwide (Ozdamar Unal et al., 2022). The COVID-19 global pandemic exposed this situation which poses serious challenges to the safety, and mental and physical wellbeing of medical staff (Bellman et al., 2022; Catton, 2020; Romate & Rajkumar, 2022). Throughout the pandemic, medical staff have experienced threats and challenges related to e.g., extreme mental pressure, shortages in personal protective equipment, pressures to diagnose and treat patients suffering from COVID-19, communication problems between patients, their companions and physicians, and the unknown fear of death surrounding the disease (Huang & Zhao, 2020; Kang et al., 2020).
As previous studies have demonstrated, violence is not caused by a single factor but is a result of a combination of many factors (Al-Shaban et al., 2021). We outlined four types of patient violence built upon TRD-based analytical framework for patients’ violence, and further explained the interaction and determinism relationship across factors. First, the interactive determination between personal factors and environmental factors. When exposed to stressful and crowded hospital environment, patients are prone to have more anxiety and intense about their health condition. In turn, the negativity spread by individuals continues to fuel unrest in the hospital environment. Meanwhile, if the patient companions had close intimate relationships, they are more sensitive to the negative stimulus of the environment. Second, the interactive determination between environmental factors and behavioral factors. Hospital visits increase greatly because of the pandemic. As a result, the healthcare environment is fully occupied, and fail to satisfy the patient healthcare need in terms of waiting time and treatment time. The psychological imbalance may trigger violence towards medical staff, and cause medical resources lost. Third, the interactive determination between personal factors and behavioral factors. Although patient participation increases during healthcare consultations, healthcare knowledge gap persists. Some patients may reluctant to follow physician advices and refuse to communicate when disagreement arises. This, in return, leads to poor treatment outcomes for patients.
Strong relationship oriented violence
We summarized configurations A1 and A2 as Strong Relationship Oriented Violence. In medical settings, compared to the friends or colleagues of patients, relatives are more likely to have stronger empathy for patients’ diseases and have greater opportunity for contact with the physicians (Lafta & Falah, 2019). They are more sensitive to negative “stimuli” in the limited healthcare service environment, and to give behavioral feedback (e.g., violence behavior that harms healthcare professionals).
Relationship Closeness is a necessary condition for inciting patient violence towards medical staff resulting in casualties. The majority of perpetrators are patients themselves and / or their relatives which is a prominent feature of violence towards medical staff both before (AbuAlRub & Al-Asmar, 2011; Albashtawy et al., 2015; Shea et al., 2017) and during the COVID-19 pandemic (Ghareeb et al., 2021; Naseem et al., 2022). A study conducted in Iraq during the pandemic found that 93.9% of medical staff experienced violence towards them from patients or their families (Lafta et al., 2021). Another study in Peru reached a similar conclusion (Del Carpio-Toia et al., 2021). The reasons may be as follows: First, patients and their families face numerous mental pressures when receiving healthcare services, such as possibility of fatal disease (Muzembo et al., 2015). Their emotions can become unstable and fluctuate. Physicians, as the object of patients’ emotional expression, bear most of the brunt of patients’ negative emotions. Ultimately, patients may choose extreme ways to vent their frustrations if their problem is not solved in a perceived satisfactory manner, such as being violent towards medical staff. Second, some relatives may protest or become violent towards medical staff to demonstrate their affection towards the patient (Liu & Tan, 2021). To some extent, relatives may show their concern for their loved ones to self-satisfy their performance needs for family affection or simply to obtain economic benefits, such as higher compensation. Third, strict prevention policies enforced during COVID-19 increased the complexity and risks associated with receiving medical treatment, leading to difficulties in patients’ families being able to accompany them or visit them during their hospital stay. The restricted visits to patients (Dopelt et al., 2022; Xie et al., 2021) and dissatisfaction with hospitals’ prevention policies (Freytag et al., 2021) have been confirmed as two of the causes for patient violence towards medical staff. In an analysis by Arafa et al. (Arafa et al., 2021), they found that patients’ extreme panic and anxiety about COVID-19 fueled conflict with physicians and escalated patient violence towards medical staff during the pandemic. During the prevention and control stages of the COVID-19 pandemic, patients and their companions were situated in hospitals with a high risk of infection and poorly protected equipment. Hospitals in heavily affected areas took measures to limit the number of caregivers on duty at any onetime and implemented more strict administration at the hospital entrance.
To prevent Strong Relationship Oriented Violence, firstly, physicians should realize the importance of recognizing and caring for the emotional changes of patients and their companions. Physicians should detect and alleviate patients’ medical anxiety in a timely manner rather than simply collecting disease-related information for diagnosis purposes. Secondly, patients are expected to improve their moral cultivation and standards, reasonably control their negative emotions, and strictly abide by hospital regulations, including disease prevention policies. Thirdly, hospitals must strengthen education surrounding moral standards for both physicians and patients by combining traditional and new media approaches. Prior research has suggested that social media and other communication channels are critical to combating violence towards medical staff (Bellizzi et al., 2022). Furthermore, hospitals should effectively promote that any violence towards medical staff will result in legal action.
Healthcare resources and service mismatch violence
Configurations B1 and B2 were summarized as the Healthcare Resources and Services Mismatched Violence. During the pandemic, highly ranked hospitals were often overcrowded due to the significant flow of people demanding medical attention. This meant that medical settings became more complex and contained risk factors that may result in violent incidents towards medical staff (Yang et al., 2021a). With the implementation of the Healthy China Strategy, people’s health awareness has been raised and the demand for health and disease management has expanded, surge in proactive patients causing overcrowding in hospitals. In noisy hospital environments, patients may quickly become discomforted which breeds conflict because seeing a doctor is a highly private behavior. In tertiary hospitals, patients have higher expectations about the healthcare services and treatment they will receive. The imbalance between patients’ expectations and actual feelings (Wu et al., 2015) may eventually lead to violence towards medical staff. In addition, the professional quality of physicians in higher-rank hospitals is stronger, and the difference in healthcare knowledge with patients is more obvious, which plays a leading role in patient-physician cultural conflict and further stimulates conflict.
The problem of insufficient healthcare resources is not too prominent in China. Previous studies have emphasized that a lack of resources is a significant factor which leads to patient violence towards medical staff. Specifically, insufficient resources can include long wait times, but short consultation times (Arafa et al., 2021), declining medical environment (Basis et al., 2021), and the shortage of healthcare resources, such as ICU wards and ventilators (Chamsi-Pasha et al., 2020; McKay et al., 2020). During the severe stage of the COVID-19 pandemic, the Chinese government tried its hardest to ensure the supply of medical materials to all levels of hospitals. Similarly, hospitals in China also received medical supplies and assistance from other countries. We emphasize that based on the relative adequacy of hardware environmental conditions, the soft skills of medical services are extraordinarily important to the patient’s experience and satisfaction. In this study, one of the most common causes for violence towards medical staff was patients becoming dissatisfied about the long wait times. During the pandemic, hospitals made flexible adjustments according to the current pandemic situation. For example, some hospitals stopped receiving patients and created designated hospitals for fever clinics. The serious imbalance in the number of patients and physicians due to a great number of patients flocking to a few hospitals directly led to the extension of waiting times of patients.
To prevent Healthcare Resources and Services Mismatched Violence, first, the physicians should strengthen their professional capabilities. When delivering healthcare to patients, physicians should timely synchronize the relay of disease information to patients in an easy-to-understand language to fully respect patients’ right to know. For patients, the most important action is to establish correct medical cognition and have reasonable psychological expectations for treatment. For hospitals, as providers of healthcare services, they should realize the need for improving healthcare resources and services. On the one hand, it is necessary to focus on improving the overall quality of healthcare delivered, which is the core task of a hospitals, but they should also actively cultivate physicians’ professional ability and good service awareness, and organize health education and charity activities to promote healthcare knowledge which shortens the distance between patients and physicians. On the other hand, the COVID-19 pandemic reminds us that hospitals should ensure the reserve of medical materials and respond to public health emergencies with sufficient strength. For governments, they should allocate high-quality healthcare resources in a fair manner and speed-up the cultivation and retention of medical talent to alleviate the problem of the great disparity in the number of patients and physicians.
Violence caused by ineffective patient-physician communication
We named configuration C1 as the Violence caused by Ineffective Patient-Physician Communication. When delivering healthcare services, the decision-making involved in diagnosis and treatment, and the follow-up care requires effective patient-physician communication. In this situation, the patients are in a weak position with regards communication with physicians. In most incidents of violence, patients’ verbal expressions show an irrational state, which can lead to a failure in patient-physician communication.
Patient-Physician Communication is a critical element of delivering healthcare services successfully (Tai-Seale et al., 2021). Ineffective or failed communication between patients and physicians is considered a common cause of violence towards medical staff (Boafo, 2016; Ramacciati et al., 2018; Wu et al., 2012). Recent research indicates that a friendly physician attitude and behavior improved the patient-physician relationship during the COVID-19 pandemic, which provides a new research perspective to clarify the importance of patient-physician communication (Basis et al., 2021; Hu et al., 2021; Zhou et al., 2021a). At the same time, it also provides a direction for future research in terms of improving the relationship between patients and physicians (Gao et al., 2020). The friendly communication style of physicians causes a series of positive chain reactions which not only improves the patient-physician relationship but also reduces the chances of violence towards medical staff. In this study, we did not find the significant effect of physicians’ inappropriate behavior on violence towards medical staff. A study conducted in Turkey found that 58.2% of physicians developed excessive medical accident anxiety during the pandemic (Buran & Altin, 2021), which shows that physicians are becoming more aware of if they are portraying inappropriate behavior when delivering services. This suggests that when physicians pay attention to their behavior, it can prevent violence to a certain extent.
To prevent Violence due to Ineffective Patient-Physician Communication, both patients and physicians must trust and respect each other. The patients and physicians should strive to learn and develop communication skills and improve communication efficiency to create an effective dialogue with a friendly attitude. For physicians, they should develop their empathy ability to be healthcare workers with sound temperament and they should try to think from the standpoint of patients, which is the entry point of a good patient-physician relationship. For patients, it is necessary for them to actively communicate with physicians and be able to rationally express their views without becoming frustrated. Even if a dispute inevitably occurs, patients should remain objective and calm and use legal means to solve the dispute to safeguard their rights and interests. Hospitals should intervene in times of dispute and deal with patients’ complaints fairly, which is an effective way to curb future disputes turning into violent incidents.
Ineffective communication superimposed low patient compliance violence
We summarized configurations C2 and C3 as the Ineffective Communication Superimposed Low Patient Compliance Violence, which emphasizes the combination of ineffective patient-physician communication and low patient cooperativeness. The results of the communication and cooperation between patients and physicians are directly related to patients’ health and wellbeing. The low patient compliance and ineffective communication will aggravate the patient’s condition which may become a potential reason for contradiction and future acts of violence.
Many studies have shown that communication skills, as well as attitudes and modes between patients and physicians, play an important role in the continuous and normal promotion of healthcare services (Kwon & Noh, 2013). The tension between patients and physicians has been eased, which not only benefits from the positive improvement of patient-physician communication but is also inseparable from the active cooperation of patients with physicians’ medical plans. The positive feedback demonstrates that communication and cooperation are extremely important during patient-physician interactions. However, the impact of patient compliance with physicians on violence towards medical staff has not garnered significant attention in current research. In this study, patient compliance mainly refers to patients’ cooperation with physicians’ advice, arrangements, and decisions. Patients act as participatory decision-makers in the collaborative model of healthcare services (Taube, 2016). The diagnosis and treatment of diseases are based on a great deal of interaction and communication between patients and physicians. Patient compliance and acceptance of treatment results have been confirmed to affect the patient-physician relationship (de Waard et al., 2018), and a poor patient-physician relationship may lead to violence towards medical staff (Zhou et al., 2021a).
To prevent the Ineffective Communication Superimposed Low Patient Compliance Violence, first, patients should respect and cooperate with the physicians’ treatment plan based on friendly communication. The patients should fully understand the advantages and disadvantages of different treatment plans and choose carefully in combination with the professional advice received from physicians. Second, physicians should improve their professionalism when delivering healthcare services and guidance, and should give more personalized treatment plans to obtain the full trust of patients. Third, governments should actively publicize positive stories and gradually cultivate the trust of patient groups in physicians. It is believed that the incidents of violence can be reduced at the source through the joint efforts of patients and physicians and the improvement of a social environment.
Limitations
Theoretically, this study not only extends the application of TRD theory in explaining causes of violence towards medical staff, but also provides a novel perspective to group the influencing factors of patient violence. Compared with previous studies with extensive efforts in identifying different factors among stakeholders, this study regards the causes of patient violence as mutually affected based on TRD theory. Benefited from the advantages of QCA analysis for explaining multiple concurrent causal relationships, this study adopted flexible configurational combinations to reveal the neglected interactions and substitutions among factors of patient violence towards medical staff. Practically, since the combined effect among factors specifies types and characteristics of violence towards medical staff, it provides important guidance for formulating targeted violence prevention and control measures. Meanwhile, this study also emphasizes the importance of relationships, healthcare service quality, and patient-physician communication and collaboration in patient violence prevention during public health emergencies. In addition, patient compliance is much more important in precipitating patient violence during COVID-19 pandemic than that of normal times. This may help in understanding of the patient-physician relationship in the Asian cultural context.
Specifically, this study has implications for healthcare service delivery, hospital management, and the policy-making. For healthcare service delivery, medical professionals need to strengthen the emotional care of both patients and their companions, especially those who have low patient compliance. They are expected to master more patient and empathetic communication skills to relieve the negative emotions in time, and keep patient well informed of possible disease consequences and the necessity to cooperate with treatment. For hospital management, in addition to sufficient supply of staff resources and medical materials, the hospital should protect personal safety of medical staff throughout the offline consultation environment including the pre-consultation, consultation and post-consultation stages. For example, strict security checks for patients in the pre-consultation stage, warm-hearted hospital guide and emotional care during the consultation stage, efficient medical insurance reimbursement and medical record review in the post-consultation stage. For major public health emergencies like COVID-19 pandemic, as patients surge in the hospital, many threatening factors emerge. The hospital should increase security checks to maintain stable medical order, and respond quickly to adverse events and requests for help in time. Meanwhile, medical administrators are required to be fully prepared to spot potential conflicts and resolve the disputes in a timely manner. For policymakers, violence towards medical staff during COVID-19 is not only about the personal safety of healthcare workers, but also about epidemic prevention and control. Although the conduct is minor during normal times, the same conduct may jeopardize the public during emergencies. It is necessary to emphasize the harsh of penalties during public health emergencies, and promote zero tolerance of patient violence atmosphere in the society.
Although this study has contributed significantly to current understanding about the impact of COVID-19 on the causes of patient violence towards medical staff, it does have numerous limitations. First, the actual impact may be different across geographical regions. Future studies can develop the existing case library to further compare the differentiated impacts of the pandemic. Secondly, we identified the mechanism solely on selected cases and this might neglect potential determinants from unreported information. Future research can explore more critically the causes of patient violence using a qualitative approach with patients, physicians, hospital managers, and healthcare administrators. In addition, the forms of violence against medical staff can be more than verbal and physical violence in the emerging digitalized world. Future study can look up to the Internet-based violence towards medical staff, for example the characters, causes and counter measurements for cyberbullying towards medical staff (Zhu et al., 2021).
Conclusion
Building on the TRD theory, this study identified twelve conditions from three elements (i.e., personal, environmental and behavioral factors) to systematically analyze and characterize the causes of patient violence towards medical staff during the COVID-19 pandemic in China. We adopted csQCA to analyze the formation mechanism of patients’ violence from the combined effect of conditions perspective. First, this study classified four types of causes of violence, including Strong Relationship Oriented Violence, Healthcare Resources and Services Mismatched Violence, Violence caused by Ineffective Patient-Physician Communication, and Ineffective Communication Superimposed Low Patient Compliance Violence, to characterize the differentiated mechanism of patients’ violence during a major public health crisis. Second, similar to pre-COVID-19 outbreak studies, we reconfirmed the important role of kinship, resources and services inequality, and patient-physician communication in precipitating patient violence. While, the difference highlighted is that patient compliance with treatment is also a strong predictor of patient violence towards medical staff, which has not been emphasized in relevant studies prior to the outbreak of COVID-19. This study also contributes to the creation of anti-violence strategies that target various types of patient violence for physicians, hospitals, and health administrators.
Appendix
Authors’ contribution
MY, WZ, RE, CZ, LW and JS conceptualized the paper, MY, WZ, CZ and LW contributed in the data collection and analysis, MY and WZ wrote the draft, RE, CZ, LW and JS contributed to the Discussion and revision of the paper. All authors have agreed the submission.
Funding
This paper is supported by National Natural Science Foundation of China (Project No. 72104087), National Social Science Foundation of China (Project No. 18CZZ001), and China Association for Science and Technology High-end Science and Technology Innovation New Think Tank Youth Fund(Project No. 2021ZZZLFZB1207041).
Declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abdellah, R. F., & Salama, K. M. (2017). Prevalence and risk factors of workplace violence against health care workers in emergency department in Ismailia, Egypt [Article]. Pan African Medical Journal, 26, 8, Article 21. 10.11604/pamj.2017.26.21.10837 [DOI] [PMC free article] [PubMed]
- AbuAlRub RF, Al-Asmar AH. Physical violence in the workplace among Jordanian Hospital Nurses. Journal of Transcultural Nursing. 2011;22(2):157–165. doi: 10.1177/1043659610395769. [DOI] [PubMed] [Google Scholar]
- Al-Shaban ZR, Al-Otaibi ST, Alqahtani HA. Occupational violence and staff safety in health-care: a cross-sectional study in a large public hospital [Article] Risk Management and Healthcare Policy. 2021;14:1649–1657. doi: 10.2147/rmhp.S305217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albashtawy M, Al-Azzam M, Rawashda A, Batiha AM, Bashaireh I, Sulaiman M. Workplace violence toward emergency department staff in Jordanian Hospitals: a cross-sectional study [Article] Journal of Nursing Research. 2015;23(1):75–81. doi: 10.1097/jnr.0000000000000075. [DOI] [PubMed] [Google Scholar]
- Alhamad, R., Suleiman, A., Bsisu, I., Santarisi, A., Al Owaidat, A., Sabri, A., … Mahseeri, M. (2021). Violence against physicians in Jordan: an analytical cross-sectional study [Article]. Plos One, 16(1), 14. Article e0245192. 10.1371/journal.pone.0245192 [DOI] [PMC free article] [PubMed]
- Aljohani B, Burkholder J, Tran QK, Chen C, Beisenova K, Pourmand A. Workplace violence in the emergency department: a systematic review and meta-analysis [Review] Public Health. 2021;196:186–197. doi: 10.1016/j.puhe.2021.02.009. [DOI] [PubMed] [Google Scholar]
- Arafa, A., Shehata, A., Youssef, M., & Senosy, S. (2021). Violence against healthcare workers during the COVID-19 pandemic: a cross-sectional study from Egypt [Article; early Access]. Archives of Environmental & Occupational Health, 7. 10.1080/19338244.2021.1982854 [DOI] [PubMed]
- Bandura A. Social foundations of thought and action: a social cognitive theory. Journal of Applied Psychology. 1986;12(1):169. [Google Scholar]
- Basis, F., Moskovitz, K., & Tzafrir, S. (2021). Did the events following the COVID-19 outbreak influence the incidents of violence against hospital staff? [Article]. Israel Journal of Health Policy Research, 10(1), 7, Article 36. 10.1186/s13584-021-00471-z [DOI] [PMC free article] [PubMed]
- Bellizzi S, Pichierri G, Farina G, Cegolon L, Abdelbaki W. Perspective piece violence against healthcare: a public health issue beyond conflict settings [Article] American Journal of Tropical Medicine and Hygiene. 2022;106(1):15–16. doi: 10.4269/ajtmh.21-0979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellman V, Thai D, Chinthalapally A, Russell N, Saleem S. Inpatient violence in a psychiatric hospital in the middle of the pandemic: clinical and community health aspects [Article] Aims Public Health. 2022;9(2):342–356. doi: 10.3934/publichealth.2022024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatti OA, Rauf H, Aziz N, Martins RS, Khan JA. Violence against healthcare workers during the COVID-19 pandemic: a review of incidents from a lower-middle-income country [Review] Annals of Global Health. 2021;87(1):11. doi: 10.5334/aogh.3203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boafo, I. M. (2016)“…they think we are conversing, so we don’t care about them…” Examining the causes of workplace violence against nurses in Ghana. BMC Nursing15, 68. 10.1186/s12912-016-0189-8 [DOI] [PMC free article] [PubMed]
- Bulle DR, Rode MM. Risk factors in committing domestic violence in light of gender psychology [Article] Current Issues in Personality Psychology. 2018;6(2):143–153. doi: 10.5114/cipp.2018.72262. [DOI] [Google Scholar]
- Buran, F., & Altin, Z. (2021). Burnout among physicians working in a pandemic hospital during the COVID-19 pandemic [Article]. Legal Medicine, 51, 6, Article 101881. 10.1016/j.legalmed.2021.101881 [DOI] [PMC free article] [PubMed]
- Byon, H. D., Sagherian, K., Kim, Y., Lipscomb, J., Crandall, M., & Steege, L. (2021). Nurses’ experience with type II workplace violence and underreporting during the COVID-19 pandemic [Article; early Access]. Workplace Health & Safety, 9, Article 21650799211031233. 10.1177/21650799211031233 [DOI] [PubMed]
- Cai RL, Tang J, Deng CH, Lv GF, Xu XH, Sylvia S, Pan J. Violence against health care workers in China, 2013–2016: evidence from the national judgment documents [Article] Human Resources for Health. 2019;17(1):14. doi: 10.1186/s12960-019-0440-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catton H. Nursing and health policy perspectives 2020-a year to remember or one to forget? [Article] International Nursing Review. 2020;67(4):450–452. doi: 10.1111/inr.12647. [DOI] [PubMed] [Google Scholar]
- Chai KC, Zhang YB, Chang KC. Regional disparity of medical resources and its effect on mortality rates in China [Article] Frontiers in Public Health. 2020;8:8. doi: 10.3389/fpubh.2020.00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamsi-Pasha H, Chamsi-Pasha M, Albar MA. Ethical dilemmas in the era of COVID-19 [; review] Avicenna Journal of Medicine. 2020;10(3):102–105. doi: 10.4103/ajm.ajm_119_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman, R., Perry, L., Styles, I., & Combs, S. (2009). Predicting patient aggression against nurses in all hospital areas. British Journal of Nursing (Mark Allen Publishing),18(8), 478–483. 10.12968/bjon.2009.18.8.41810. [DOI] [PubMed]
- Cheung, T., Lee, P. H., & Yip, P. S. F. (2017). Workplace violence toward Physicians and Nurses: Prevalence and correlates in Macau [Article]. International Journal of Environmental Research and Public Health, 14(8), 15. Article 879. 10.3390/ijerph14080879 [DOI] [PMC free article] [PubMed]
- Chi SX, Chen JH, Lv SJ, Chen L. Public trust in medical staff during COVID-19 epidemic in China: a cross-srctional survey. Chinese Journal of Public Health. 2021;37(12):1783–1787. [Google Scholar]
- Crilly J, Chaboyer W, Creedy D. Violence towards emergency department nurses by patients [Comparative study;] Accident and Emergency Nursing. 2004;12(2):67–73. doi: 10.1016/j.aaen.2003.11.003. [DOI] [PubMed] [Google Scholar]
- Darawad MW, Al-Hussami M, Saleh AM, Mustafa WM, Odeh H. Violence against nurses in emergency departments in Jordan nurses’ perspective [Article] Workplace Health & Safety. 2015;63(1):9–17. doi: 10.1177/2165079914565348. [DOI] [PubMed] [Google Scholar]
- De Marchi, V., Molina-Morales, F. X., & Martinez-Chafer, L. (2022). Environmental innovation and cooperation: a configurational approach [Article]. Technological Forecasting and Social Change, 182, 13, Article 121835. 10.1016/j.techfore.2022.121835
- de Waard CS, Poot AJ, den Elzen WPJ, Wind AW, Caljouw MAA, Gussekloo J. Perceived doctor-patient relationship and satisfaction with general practitioner care in older persons in residential homes [Article] Scandinavian Journal of Primary Health Care. 2018;36(2):189–197. doi: 10.1080/02813432.2018.1459229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Carpio-Toia AM, del Carpio LBM, Mayta-Tristan P, Alarcon-Yaquetto DE, Malaga G. Workplace violence against physicians treating COVID-19 patients in Peru: a cross-sectional study [Article] Joint Commission Journal on Quality and Patient Safety. 2021;47(10):637–645. doi: 10.1016/j.jcjq.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devi, S. (2020). COVID-19 exacerbates violence against health workers. Lancet, 396(10252), 658–658. 10.1016/S0140-6736(20)31858-4 [DOI] [PMC free article] [PubMed]
- Dopelt, K., Davidovitch, N., Stupak, A., Ben Ayun, R., Eltsufin, A. L., & Levy, C. (2022). Workplace violence against Hospital Workers during the COVID-19 pandemic in Israel: implications for Public Health [Article]. International Journal of Environmental Research and Public Health, 19(8), 12, Article 4659. 10.3390/ijerph19084659 [DOI] [PMC free article] [PubMed]
- Du, Y. X., Wang, W. X., Washburn, D. J., Lee, S., Towne, S. D., Zhang, H., & Maddock, J. E. (2020). Violence against healthcare workers and other serious responses to medical disputes in China: surveys of patients at 12 public hospitals [Article]. BMC Health Services Research,20(1), 10, Article 253. 10.1186/s12913-020-05104-w [DOI] [PMC free article] [PubMed]
- Elamin, M. M., Hamza, S. B., Abbasher, K., Idris, K. E., Abdallah, Y. A., Muhmmed, K. A. A., … Mustafa, A. A. M. (2021). Workplace violence against doctors in Khartoum State, Sudan, 2020. Sudan Journal of Medical Sciences,16(2), 301–319. 10.18502/sjms.v16i2.9296
- Freytag, S., Dammermann, A., Schultes, K., Bieber, A., Fleischer, S., Sander, M., … Namen, H. K. (2021). Gewalt und Gewaltpravention in der stationaren Altenpflege wahrend der COVID-19-Pandemie teilanalyse von interviews mit leitungspersonen [Article]. Pflege,34(5), 241–249. 10.1024/1012-5302/a000823 [DOI] [PubMed]
- Furnari S, Crilly D, Misangyi VF, Greckhamer T, Fiss PC, Aguilera RV. Capturing causal complexity: heuristics for configurational theorizing [Article] Academy of Management Review. 2021;46(4):778–799. doi: 10.5465/amr.2019.0298. [DOI] [Google Scholar]
- Gao, Y., Wang, Z., Gui, Y., Wang, Y., Shou, S., Chai, Y., & Lu, W. (2020). A questionnaire survey on doctor - patient relationship in China under the COVID – 19 epidemic [新型冠状病毒肺炎疫情下我国医患关系的问卷调查研究] [Article]. Chinese Journal of Critical Care Medicine,40(8), 753–758.
- Garg N, Garg R, Sharma DK, Gupta SK, Dudeja P. Violence against health care workforce in COVID and non COVID times: analysis of predisposing factors [Article] Indian Journal of Community Health. 2020;32(4):659–664. doi: 10.47203/IJCH.2020.v32i04.009. [DOI] [Google Scholar]
- Ghareeb NS, El-Shafei DA, Eladl AM. Workplace violence among healthcare workers during COVID-19 pandemic in a jordanian governmental hospital: the tip of the iceberg [Article] Environmental Science and Pollution Research. 2021;28(43):61441–61449. doi: 10.1007/s11356-021-15112-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo, B., & Jiang, F. (2008). Self-efficacy theory and it’s application. Shanghai Educational Publishing House.
- He JW. Defensive medicine and its contributing factors of public hospitals in China: research findings from a physician survey in a city of Guangdong province. Chinese Journal of Health Policy. 2014;7(10):33–39. [Google Scholar]
- Heidrich S, Bandelow NC. When the bulldozers trundle: why infrastructure policy conflicts escalate into violence [Article] Politische Vierteljahresschrift. 2019;60(3):539–560. doi: 10.1007/s11615-019-00175-9. [DOI] [Google Scholar]
- Hu, L. M., Bai, L. J., Zhao, S. Y., & Lu, R. J. (2021). Analysis of doctor-patient relationship in post-COVID-19 period: perspective differences between citizen and medical staff [Article]. Inquiry-the Journal of Health Care Organization Provision and Financing, 58, 10, Article 00469580211060300. 10.1177/00469580211060300 [DOI] [PMC free article] [PubMed]
- Huang, Y. E., & Zhao, N. (2020). Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey [Article]. Psychiatry Research, 288, 6, Article 112954. 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed]
- Huo, H., & Li, Q. X. (2022). Influencing factors of the continuous use of a knowledge payment platform-fuzzy-set qualitative comparative analysis based on triadic reciprocal determinism [Article]. Sustainability, 14(6), 15, Article 3696. 10.3390/su14063696
- Jiao, M. L., Ning, N., Li, Y., Gao, L. J., Cui, Y., Sun, H., … Hao, Y. H. (2015). Workplace violence against nurses in chinese hospitals: a cross-sectional survey [Article]. BMJ Open, 5(3), 9, Article e006719. 10.1136/bmjopen-2014-006719 [DOI] [PMC free article] [PubMed]
- Kahwati, L. C., & Kane, H. L. (2018). Qualitative comparative analysis in mixed methods research and evaluation (6 vol.). SAGE Publications.
- Kang, L. J., Li, Y., Hu, S. H., Chen, M., Yang, C., Yang, B. X., … Liu, Z. C. (2020). The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus [Letter]. Lancet Psychiatry,7(3), E14–E14. 10.1016/s2215-0366(20)30047-x [DOI] [PMC free article] [PubMed]
- Kesavan R, Abraham VM, Reddy V, Khan T, Sankar V, Swathi R. Workplace violence against healthcare professionals - a cross-sectional study to assess the current scenario in Chennai City, India [Article] Journal of Evolution of Medical and Dental Sciences-Jemds. 2020;9(35):2515–2520. doi: 10.14260/jemds/2020/547. [DOI] [Google Scholar]
- Khan, M. N., Haq, U., Khan, Z., Wali, M., Baddia, S., Rasul, F., … Ramirez-Mendoza, S. (2021). Prevalence and determinants of violence against health care in the metropolitan city of Peshawar: a cross sectional study [Article]. BMC Public Health,21(1), 11. 10.1186/s12889-021-10243-8 [DOI] [PMC free article] [PubMed]
- Kogut B, Ragin C. Exploring complexity when diversity is limited: institutional complementarity in theories of rule of law and national systems revisited [Article] European Management Review. 2006;3(1):44–59. doi: 10.1057/palgrave.emr.1500048. [DOI] [Google Scholar]
- Kwon YD, Noh JW. Development of physician coaching model for improvement of patient-doctor communication [환자-의사 커뮤니케이션 개선을 위한 의사코칭 모델 개발] [research-article] The Journal of the Korea Contents Association. 2013;13(2):331–340. doi: 10.5392/jkca.2013.13.02.331. [DOI] [Google Scholar]
- Lafta, R., Qusay, N., Mary, M., & Burnham, G. (2021). Violence against doctors in Iraq during the time of COVID-19 [Article]. PLoS One, 16(8), 12, Article e0254401. 10.1371/journal.pone.0254401 [DOI] [PMC free article] [PubMed]
- Lafta RK, Falah N. Violence against health-care workers in a conflict affected city. Medicine Conflict and Survival. 2019;35(1):65–79. doi: 10.1080/13623699.2018.1540095. [DOI] [PubMed] [Google Scholar]
- Levin PF, Hewitt JB, Misner ST. Insights of nurses about assault in hospital-based emergency departments. Image–the Journal of Nursing Scholarship. 1998;30(3):249–254. doi: 10.1111/j.1547-5069.1998.tb01300.x. [DOI] [PubMed] [Google Scholar]
- Li, Z., Yan, C. M., Shi, L., Mu, H. T., Li, X., Li, A. Q., … Mu, Y. (2017). Workplace violence against medical staff of Chinese children’s hospitals: a cross-sectional study [Article]. PLoS One, 12(6), 19, Article e0179373. 10.1371/journal.pone.0179373 [DOI] [PMC free article] [PubMed]
- Liu, J. X., Gan, Y., Jiang, H., Li, L. Q., Dwyer, R., Lu, K., … Lu, Z. X. (2019). Prevalence of workplace violence against healthcare workers: a systematic review and meta-analysis [Review]. Occupational and Environmental Medicine,76(12), 927–937. 10.1136/oemed-2019-105849 [DOI] [PubMed]
- Liu, T. Y., & Tan, X. (2021). A sociopolitical analysis of Yi Nao: public disruption, performativity and the power of doctors in Chinese Medical Disputes. China-an International Journal,19(2), 133–153.
- Ma BL, Hu ZC, Li YR, Wang H. Study on causes of medical violence behavior of patients based on QCA. Journal of Beijing Institute of Technology(Social Sciences Edition) 2019;21(05):101–114. doi: 10.15918/j.jbitss1009-3370.2019.1059. [DOI] [Google Scholar]
- Ma, J., Chen, X., Zheng, Q. J., Zhang, Y., Ming, Z., Wang, D. X., … Li, X. S. (2021). Serious workplace violence against healthcare providers in China between 2004 and 2018 [Article]. Frontiers in Public Health, 8, 8, Article 574765. 10.3389/fpubh.2020.574765 [DOI] [PMC free article] [PubMed]
- McKay D, Heisler M, Mishori R, Catton H, Kloiber O. Attacks against health-care personnel must stop, especially as the world fights COVID-19 [Editorial Material] Lancet. 2020;395(10239):1743–1745. doi: 10.1016/s0140-6736(20)31191-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muzembo BA, Mbutshu LH, Ngatu NR, Malonga KF, Eitoku M, Hirota R, Suganuma N. Workplace violence towards congolese health care workers: a survey of 436 healthcare facilities in Katanga province, Democratic Republic of Congo [Article] Journal of Occupational Health. 2015;57(1):69–80. doi: 10.1539/joh.14-0111-OA. [DOI] [PubMed] [Google Scholar]
- Naseem, M., Feroz, A. S., Arshad, H., Ashraf, S., Asim, M., Jamali, S., & Mian, A. (2022). Perceptions, challenges and experiences of frontline healthcare providers in Emergency Departments regarding Workplace Violence during the COVID-19 pandemic: a protocol for an exploratory qualitative study from an LMIC [Article]. British Medical Journal Open,12(2), 6, Article e055788. 10.1136/bmjopen-2021-055788 [DOI] [PMC free article] [PubMed]
- Naveen Kumar P, Betadur D, Chandermani Study on mitigation of workplace violence in hospitals. Medical journal Armed Forces India. 2020;76(3):298–302. doi: 10.1016/j.mjafi.2019.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozdamar Unal G, Iscan G, Unal O. The occurrence and consequences of violence against healthcare workers in Turkey: before and during the COVID-19 pandemic. Family Practice. 2022 doi: 10.1093/fampra/cmac024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pich, J., & Roche, M. (2020). Violence on the job: the experiences of nurses and midwives with violence from patients and their friends and relatives [Article]. Healthcare, 8(4), 12, Article 522. 10.3390/healthcare8040522 [DOI] [PMC free article] [PubMed]
- Piraianu A, Neagu M, Neagu AI, Fulga A, Ciubara A, Ciubara BA, Fulga I. Triogenesis of extreme hetero-aggressive behaviour in psychiatric forensic expert practice [Article] Archiv Euromedica. 2021;11(5):72–75. doi: 10.35630/2199-885x/2021/11/5.20. [DOI] [Google Scholar]
- Qi XX. Cause analysis and legal response to the “intensification” of doctor-patient disputes -- concerned about three violent attacks on doctors. Seeking Truth. 2020;47(01):12–18. doi: 10.19667/j.cnki.cn23-1070/c.2020.01.003. [DOI] [Google Scholar]
- Ragin, C. (1987). The comparative method: moving Beyond qualitative and quantitative methods. University of California.
- Ragin, C. (1995). Using qualitative comparative analysis to study configurations. Computer-aided Qualitative Data Analysis (pp.177–189). London
- Ragin, C. C. (2000). Fuzzy-set Social Science. University of Chicago Press Economics Books.
- Ragin CC. Set relations in social research: evaluating their consistency and coverage [Article] Political Analysis. 2006;14(3):291–310. doi: 10.1093/pan/mpj019. [DOI] [Google Scholar]
- Ramacciati N, Ceccagnoli A, Addey B, Rasero L. Violence towards emergency nurses. The Italian National Survey 2016: a qualitative study. International Journal of Nursing Studies. 2018;81:21–29. doi: 10.1016/j.ijnurstu.2018.01.017. [DOI] [PubMed] [Google Scholar]
- Raveel, A., & Schoenmakers, B. (2019). Interventions to prevent aggression against doctors: a systematic review [Review]. BMJ Open, 9(9), 20, Article e028465. 10.1136/bmjopen-2018-028465 [DOI] [PMC free article] [PubMed]
- Rihoux, B., & Ragin, C. C. (2008). Configurational comparative methods: qualitative comparative analysis (QCA) and related techniques. Sage Publications.
- Roche M, Diers D, Duffield C, Catling-Paull C. Violence toward nurses, the work environment, and patient outcomes. Journal of Nursing Scholarship. 2010;42(1):13–22. doi: 10.1111/j.1547-5069.2009.01321.x. [DOI] [PubMed] [Google Scholar]
- Roig-Tierno N, Gonzalez-Cruz TF, Llopis-Martinez J. An overview of qualitative comparative analysis: a bibliometric analysis [Article] Journal of Innovation & Knowledge. 2017;2(1):15–23. doi: 10.1016/j.jik.2016.12.002. [DOI] [Google Scholar]
- Romate, J., & Rajkumar, E. (2022). Exploring the experiences, psychological well-being and needs of frontline healthcare workers of government hospitals in India: a qualitative study [Article]. Humanities & Social Sciences Communications, 9(1), 21, Article 89. 10.1057/s41599-022-01093-9
- Schneider, C. Q., & Wagemann, C. (2012). Set-theoretic methods for the social sciences: A guide to qualitative comparative analysis. Cambridge University Press.
- Seema S, Nayer J, Praveen A, R KS. Perception of workplace violence in the emergency department. Journal of Emergencies Trauma and Shock. 2019;12(3):179–184. doi: 10.4103/JETS.JETS_81_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafran-Tikva S, Chinitz D, Stern Z, Feder-Bubis P. Violence against physicians and nurses in a hospital: how does it happen? A mixed-methods study. Israel Journal of Health Policy Research. 2017;6:59. doi: 10.1186/s13584-017-0183-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaikh, S., Baig, L. A., Hashmi, I., Khan, M., Jamali, S., Khan, M. N., … Zaib, S. (2020). The magnitude and determinants of violence against healthcare workers in Pakistan [Article]. BMJ Global Health, 5(4), 13, Article e002112. 10.1136/bmjgh-2019-002112 [DOI] [PMC free article] [PubMed]
- Shea T, Sheehan C, Donohue R, Cooper B, De Cieri H. Occupational violence and aggression experienced by nursing and caring professionals [Article] Journal of Nursing Scholarship. 2017;49(2):236–243. doi: 10.1111/jnu.12272. [DOI] [PubMed] [Google Scholar]
- Singh G, Singh A, Chaturvedi S, Khan S. Workplace violence against resident doctors: a multicentric study from Government Medical Colleges of Uttar Pradesh [Article] Indian Journal of Public Health. 2019;63(2):143–146. doi: 10.4103/ijph.IJPH_70_18. [DOI] [PubMed] [Google Scholar]
- Smela M, Sejkora J. Natural resource revenue management: which institutional factors matter? [Article] Review of Economic Perspectives. 2022;22(1):3–23. doi: 10.2478/revecp-2022-0001. [DOI] [Google Scholar]
- Spector PE, Zhou ZQE, Che XX. Nurse exposure to physical and nonphysical violence, bullying, and sexual harassment: a quantitative review [Review] International Journal of Nursing Studies. 2014;51(1):72–84. doi: 10.1016/j.ijnurstu.2013.01.010. [DOI] [PubMed] [Google Scholar]
- Spelten, E., Thomas, B., O’Meara, P., van Vuuren, J., & McGillion, A. (2020). Violence against emergency department nurses; can we identify the perpetrators? [Article]. PLoS One, 15(4), 12, Article e0230793. 10.1371/journal.pone.0230793 [DOI] [PMC free article] [PubMed]
- Tai-Seale, M., Rosen, R., Ruo, B., Hogarth, M., Longhurst, C. A., Lander, L., … Millen, M. (2021). Implementation of Patient Engagement Tools in Electronic Health Records to enhance patient-centered communication: protocol for feasibility evaluation and preliminary results [Article]. Jmir Research Protocols, 10(8), 8, Article e30431. 10.2196/30431 [DOI] [PMC free article] [PubMed]
- Taube KM. Patient-doctor relationship in dermatology: from compliance to concordance [Review] Acta Dermato-Venereologica. 2016;96:25–29. doi: 10.2340/00015555-2452. [DOI] [PubMed] [Google Scholar]
- Thomas JA, Thomas JJ, Paul AB, Acharya S, Shukla S, Rasheed A, Pratapa SK. Medical vandalism: awareness and opinions; beyond the clinician’s window [Article] Journal of Family Medicine and Primary Care. 2019;8(12):4015–4020. doi: 10.4103/jfmpc.jfmpc_830_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian YS, Yue YC, Wang JJ, Luo T, Li YM, Zhou JS. Workplace violence against hospital healthcare workers in China: a national WeChat-based survey [Article] BMC Public Health. 2020;20(1):8. doi: 10.1186/s12889-020-08708-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker, J. D., Cheng, Y., Wong, B., Gong, N., Nie, J. B., & Zhu, W., … Patient Phys Trust Project, T. (2015). Patient-physician mistrust and violence against physicians in Guangdong Province, China: a qualitative study [Article]. BMJ Open, 5(10), 10, Article e008221. 10.1136/bmjopen-2015-008221 [DOI] [PMC free article] [PubMed]
- Vezyridis P, Samoutis A, Mavrikiou PM. Workplace violence against clinicians in cypriot emergency departments: a national questionnaire survey [Article] Journal of Clinical Nursing. 2015;24(9–10):1210–1222. doi: 10.1111/jocn.12660. [DOI] [PubMed] [Google Scholar]
- Waldkirch, M., Kammerlander, N., & Wiedeler, C. (2021). Configurations for corporate venture innovation: investigating the role of the dominant coalition [Article]. Journal of Business Venturing, 36(5), 20, Article 106137. 10.1016/j.jbusvent.2021.106137
- Wang, L. C., Zhang, J., Shi, Y., Yin, H. Y., Fu, H., & Zhan, T. (2020). Research progress and literature review of workplace violence towards staffs in medical field in China. Chinese Hospital Management, v.40;No.471(10), 78–81.
- White L, Lockett A, Currie G, Hayton J. Hybrid context, management practices and organizational performance: a configurational approach [Article] Journal of Management Studies. 2021;58(3):718–748. doi: 10.1111/joms.12609. [DOI] [Google Scholar]
- Wu, J., An, W. W., Zheng, X., & Zhang, J. Q. (2021). How business model designs influence firm growth in a transforming economy: a configurational perspective [Article]. Management and Organization Review,17(2), 226–253, Article Pii s1740877620000546. 10.1017/mor.2020.54
- Wu, J., Liu, F., Hu, H., Shang, S., Liu, H., & Wang, Z. (2015). Medical staffs’ attitude towards the causes and precautions of docter-patient dispute [医护人员对医患纠纷发生原因及预防措施态度的研究] [Article]. Chinese Nursing Management,15(10), 1237–1241.
- Wu SY, Zhu W, Li HY, Lin SW, Chai WL, Wang XR. Workplace violence and influencing factors among medical professionals in China [Article] American Journal of Industrial Medicine. 2012;55(11):1000–1008. doi: 10.1002/ajim.22097. [DOI] [PubMed] [Google Scholar]
- Xie, X. M., Zhao, Y. J., An, F. R., Zhang, Q. E., Yu, H. Y., Yuan, Z., … Xiang, Y. T. (2021). Workplace violence and its association with quality of life among mental health professionals in China during the COVID-19 pandemic [Article]. Journal of Psychiatric Research,135, 289–293. 10.1016/j.jpsychires.2021.01.023 [DOI] [PMC free article] [PubMed]
- Yang, Y., Li, Y., An, Y., Zhao, Y. J., Zhang, L., Cheung, T., … Xiang, Y. T. (2021a). Workplace violence against Chinese Frontline Clinicians during the COVID-19 pandemic and its Associations with demographic and clinical characteristics and quality of life: a structural equation modeling investigation [Article]. Frontiers in Psychiatry, 12, 8, Article 649989. 10.3389/fpsyt.2021.649989 [DOI] [PMC free article] [PubMed]
- Yang, Y. M., Wang, P. G., Kelifa, M. O., Wang, B., Liu, M. X., Lu, L. L., & Wang, W. (2021b). How workplace violence correlates turnover intention among Chinese health care workers in COVID-19 context: The mediating role of perceived social support and mental health [Article; Early Access]. Journal of Nursing Management, 8. 10.1111/jonm.13325 [DOI] [PMC free article] [PubMed]
- Yesilbas, H., & Baykal, U. (2021). Causes of workplace violence against nurses from patients and their relatives: a qualitative study [Article]. Applied Nursing Research, 62, 8, Article 151490. 10.1016/j.apnr.2021.151490 [DOI] [PubMed]
- Yu, H. M., Yu, S. Y., He, D., & Lu, Y. A. (2021). Equity analysis of Chinese physician allocation based on Gini coefficient and theil index [Article]. BMC Health Services Research, 21(1), 8, Article 455. 10.1186/s12913-021-06348-w [DOI] [PMC free article] [PubMed]
- Yu HX, Hu ZL, Zhang XF, Li B, Zhou SC. How to overcome violence against healthcare professionals, reduce medical disputes and ensure patient safety [Article] Pakistan Journal of Medical Sciences. 2015;31(1):4–8. doi: 10.12669/pjms.311.6446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, X., Li, Y. Z., Yang, C. S., & Jiang, G. (2021). Trends in Workplace Violence Involving Health Care Professionals in China from 2000 to 2020: a review [Review]. Medical Science Monitor, 27, 9, Article e928393. 10.12659/msm.928393 [DOI] [PMC free article] [PubMed]
- Zhou, Y. A., Chen, S. B., Liao, Y. H., Wu, Q. X., Ma, Y. J., Wang, D. F., … Yang, W. F. Z. (2021a). General perception of doctor-patient relationship from patients during the COVID-19 pandemic in China: a cross-sectional study [Article]. Frontiers in Public Health, 9(11), Article 646486. 10.3389/fpubh.2021.646486 [DOI] [PMC free article] [PubMed]
- Zhou, Y. A., Ma, Y. J., Yang, W. F. Z., Wu, Q. X., Wang, Q. J., Wang, D. F., … Wu, X. M. (2021b). Doctor-patient relationship improved during COVID-19 pandemic, but weakness remains [Article]. Bmc Family Practice,22(1), 9. 10.1186/s12875-021-01600-y [DOI] [PMC free article] [PubMed]
- Zhu, C. Y., Huang, S. Q., Evans, R., & Zhang, W. (2021). Cyberbullying among adolescents and children: a comprehensive review of the global situation, risk factors, and preventive measures [Review]. Frontiers in Public Health, 9, 12, Article 634909. 10.3389/fpubh.2021.634909 [DOI] [PMC free article] [PubMed]
- Zhu DQ, Wang GH. Influencing factors and mechanism of netizens’ social emotions in emergencies - qualitative comparative analysis of multiple cases based on ternary interactive determinism (QCA) Journal of Intelligence. 2020;39(3):95–104. [Google Scholar]
- Zhu, H. F., Liu, X. N., Yao, L. Y., Zhou, L. P., Qin, J. F., Zhu, C. P., … Pan, H. Y. (2022). Workplace violence in primary hospitals and associated risk factors: a cross-sectional study [Article]. Nursing Open,9(1), 513–518. 10.1002/nop2.1090 [DOI] [PMC free article] [PubMed]