Abstract
Background and Purpose
Epilepsy increases the risk of death in affected individuals of any age. We aimed to determine the mortality caused by epilepsy and its time trends in Korea.
Methods
We obtained population and cause of death data between 1993 and 2019 from Statistics Korea. We identified death caused by epilepsy or status epilepticus. We calculated the crude mortality rate (CMR), age-specific mortality rate, age-standardized mortality rate (ASMR, corresponding to epilepsy-related deaths per 100,000 persons in the general population), and the proportional mortality (PM, corresponding to the proportion of epilepsy-related deaths among all-cause deaths).
Results
In 2019, 471 deaths were caused by epilepsy (CMR=0.92), accounting for 0.16% of all deaths in that year. The age-specific mortality rate increased with age, up to 7.01% among individuals aged 80 years and older, while the PM was the highest (3.80%) among individuals aged 5–14 years, which decreased with age. Between 1993 and 2019, the CMR, ASMR, and PM peaked in 2002, and the CMR then rebounded after the trough in this trend in 2011 while the ASMR continued to decrease, and the PM became relatively stable from 2011. Starting in 2005, the age-specific mortality rate for epilepsy had an increasing tendency over time among those aged 75 years or older, and a decreasing tendency in the younger age groups.
Conclusions
A declining tendency of mortality from epilepsy was found in the overall population of Korea over recent decades. However, epilepsy is a notable cause of death in children, and epilepsy-related mortality is increasing in the elderly population.
Keywords: epilepsy, mortality, epidemiology, mortality rate, proportional mortality, temporal trends
INTRODUCTION
Epilepsy is a common neurological disease that affects individuals of any age and is associated with significant morbidity and mortality.1 Its burden is estimated to be approximately 13 million disability-adjusted life years (which equates to one lost year of healthy life), accounting for more than 0.5% of the global burden of disease (GBD).2,3
The prevalence and incidence of epilepsy were reported to be 3.84 per 1,000 persons4 and 28.70 per 100,000 persons, respectively, in Korea in 2009; these rates were showing increasing trends, particularly among elderly individuals.5 In addition to the prevalence and incidence data, mortality data have also been used to quantify the burden of specific conditions within the population.6 People with epilepsy (PWE) have a threefold higher risk of premature death than the general population because of status epilepticus (SE), sudden unexpected death in epilepsy (SUDEP), and unexpected injuries including drowning, motor vehicle collisions, falls, and suicide.7 Mortality data in the GBD indicate that epilepsy is responsible for 0.2% of all deaths worldwide.3 Recent systematic reviews found that the standardized mortality ratio (SMR) among PWE ranged from 1.6 to 3.0 in high-income countries (HICs).8
However, there has been no epidemiological study of epilepsy-related mortality in Korea. We therefore aimed to estimate the annual mortality caused by epilepsy and its time trend to help assess the priority of epilepsy in public health.
METHODS
Data source
The annual numbers of deaths and their underlying causes were obtained from Korean Statistical Information Service.9 Statistics Korea is the national office of statistics and collects data from death notifications filed at local administration offices and death certificates issued by physicians. Causes of death were classified into 236 categories, which includes epilepsy, according to the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10), as recommended by the World Health Organization (WHO). Mortality data were based on the underlying cause of death described in the death certificate and were complemented by 22 types of administrative data, including health insurance data from the National Health Insurance Service, the cancer registry from the National Cancer Center, criminal investigation records and traffic collision investigation data from the National Police Agency, autopsy records from the National Forensic Service, and emergency records from the National Emergency Medical Center.10
The total population in each year divided into age and sex categories was acquired from statistics based on resident registration provided by the Ministry of the Interior and Safety.11
Assessment of death caused by epilepsy
Death caused by epilepsy was identified as the underlying cause of death using ICD-10 codes G40 (epilepsy) and G41 (SE). Death directly related to epilepsy included SE, SUDEP, and accidents following a seizure, including trauma, drowning, and iatrogenic injury (e.g., drug toxicity and suicide).12 In these cases, code G40 or G41 may be assigned as the cause of death.
We assessed the number of deaths caused by epilepsy in Korea for each year from 1993 to 2019. The crude mortality rate (CMR), age-specific mortality rates by sex, and age-standardized mortality rate (ASMR) by sex were estimated for each year by the number of epilepsy deaths per 100,000 persons in the general population. The ASMR for epilepsy was calculated using the WHO standard population distribution (last edited in 2001).13 We estimated the age- and sex-specific proportional mortality (PM) for epilepsy or SE among all-cause deaths.
Death statistics were grouped into 16 five-year age groups for those aged 0–4 years to those aged 75–79 years, and 1 age group for people older than 79 years. The trends according to age during the study period were compared by dividing age into the following groups: 0–14, 15–35, 35–54, 55–74, and 75 years or older.
Statistical analysis
The annual trends in mortality over time were assessed using a Poisson regression model and expressed as mortality rate ratios. All reported p-values were two-tailed, and p<0.05 was considered significant. All statistical analyses were performed using SPSS (version 26.0, IBM Corporation, Armonk, NY, USA).
Ethics statement
This study was approved by the Institutional Review Board of Kangwon National University Hospital (approval number: KNUH-2021-10-002). The need to obtain informed consent was waived because anonymized public data were used.
RESULTS
Death caused by epilepsy in 2019
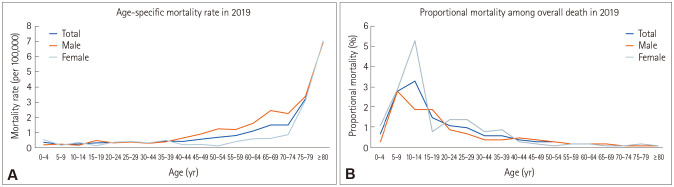
In 2019, 471 deaths were caused by epilepsy (268 males and 203 females) across all age groups. Statistics of death caused by epilepsy in 2019 are presented in Supplementary Table 1 in the online-only Data Supplement and Fig. 1. The CMR for epilepsy in 2019 was 0.92 per 100,000 persons; the highest CMR was 7.01 per 100,000 persons in those aged 80 and older, while the lowest was 0.22 per 100,000 persons in those aged 5–9 years, presenting an increasing trend with age. The CMRs for epilepsy in males and females were 1.05 and 0.79 per 100,000 persons, respectively.
Fig. 1. Age-specific mortality caused by epilepsy in 2019. The mortality rate (A) showed an increasing trend with age, while proportional mortality (B) showed a decreasing trend with age.
The PM for epilepsy was 0.16%: 0.17% in males and 0.15% in females. The highest PM was 3.80% in those aged 5–14 years, with a decreasing trend as age increased. Epilepsy was the 23rd most common cause of death in those aged 1–9 years among the 236 analyzed causes of death.
Annual trend of death caused by epilepsy between 1993 and 2019
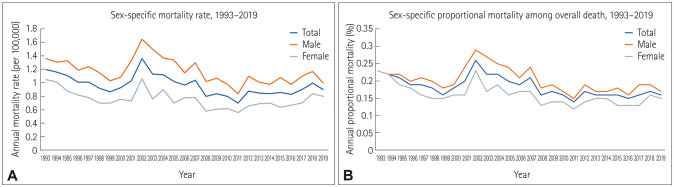
Between 1993 and 2019, the annual number of deaths attributable to epilepsy ranged from 352 to 653, with a CMR ranging from 0.70 to 1.36 per 100,000 persons (Supplementary Table 2 in the online-only Data Supplement). The annual CMR peaked in 2002, decreased from 1993 to 1999, increased from 1999 to 2002, decreased from 2002 to 2011, and then increased slightly after 2011. Both male and female CMRs followed the trend of the overall CMR. Both males and females had troughs in 2011. The CMR for epilepsy was higher in males than in females throughout the observation period (Fig. 2A).
Fig. 2. Annual trend of mortality caused by epilepsy between 1993 and 2019. The CMR (A) and PM (B) peaked in 2002, and CMR then rebounded after the trough in 2011, while PM became relatively stable from 2011. Both CMR and PM were higher in males than in females throughout the study period. CMR, crude mortality rate; PM, proportional mortality.
The PM ranged from 0.14% to 0.26%. The PM for epilepsy was higher in males than in females, excluding in 1993 and 1994. The annual PM trend was similar to that of the CMR until 2011, when the former began to fluctuate. Both males and females had troughs in 2011 (Fig. 2B).
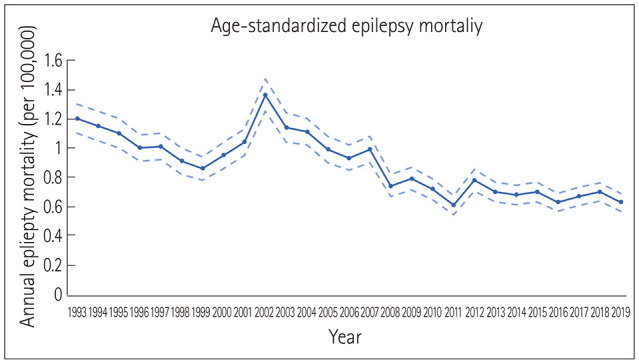
The ASMR ranged from 0.62 to 1.37 per 100,000 persons. It showed a similar trend to the CMR from 1993 to 2011 with a smaller range of annual changes and then kept decreasing over time without rebounding (Fig. 3).
Fig. 3. Annual trend of ASMR caused by epilepsy between 1993 and 2019. The ASMR for epilepsy (solid line) peaked in 2002, and then continuously decreased. Dashed lines indicate 95% confidence intervals. ASMR, age-standardized mortality rate.
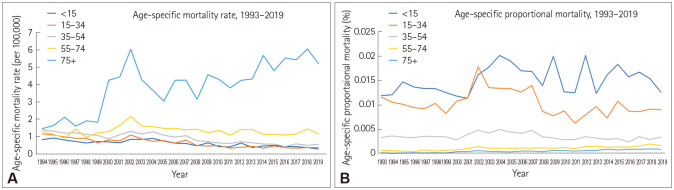
Compared with the reference year (2005), the age-specific mortality rate for epilepsy had an increasing tendency over time among those aged 75 years or older (mortality rate ratio=1.036 per 100,000 persons, 95% CI=1.024–1.072, p<0.001) and a decreasing trend in the other age groups (mortality rate ratio=0.956 per 100,000 persons, 95% CI=0.928–0.997, p<0.001) each year (Fig. 4A). Compared with the reference year (2005), the age-specific PM showed a modest increasing tendency among those aged 55–74 years (mortality rate ratio=1.034, 95% CI=1.023–1.045, p<0.001) and 75 years or older (mortality rate ratio=1.059, 95% CI=1.047–1.072, p<0.001), and a decreasing tendency in the other age groups (mortality rate ratio=0.985, 95% CI=0.978–0.991, p<0.001) each year (Fig. 4B).
Fig. 4. Annual trend of age-specific mortality caused by epilepsy between 1993 and 2019. The age-specific mortality rate (A) showed an increasing tendency over time in those aged 75 years and older and a decreasing tendency in the other age groups each year since 2005. The age-specific proportional mortality (B) showed a modest increasing tendency over time in those aged 55–74 years and 75 years or older, and a decreasing tendency in the other age groups each year.
DISCUSSION
This was the first study to use the statistics of epilepsy-related mortality in Korea and one of few studies to analyze its time trend. The results of our study were consistent with those for previous studies from other countries. The CMR was 0.71 to 1.50 per 100,000 persons in Cuba between 1982 and 2010, and 1.45 to 2.03 per 100,000 persons in England and Wales.14 The worldwide ASMR was 1.7 (95% CI=1.6–1.8) per 100,000 persons in 2015.15
We estimated that epilepsy was the 23rd most common cause of death in those aged 1–9 years in 2019 among 236 causes of deaths according to ICD-10. Epilepsy imposed a larger burden on children and young adults than any other neurological condition, as estimated by a study based on the GBD.16 Population-based studies indicated that SMRs are considerably higher in epilepsy, ranging from 6.4 to 7.5 in children.8 Underlying diseases increase the risk of premature mortality among infants or children with epilepsy, such as brain injury or hypoxic encephalopathy at birth, epileptic encephalopathy, inborn metabolism dysfunction, and congenital brain malformation.8,17
Epilepsy-related mortality measured in this study was affected not only by the relative risk of death but also by the prevalence of epilepsy. The SMR was lower in HICs than in low- and middle-income countries, which is due to improved access and increased adherence to medical management with antiseizure medications decreasing the risk of fatal medical- or injury-related complications from frequent seizures for PWE.8,18 The prevalence of epilepsy has also been reported to be lower in HICs.19 However, the overall prevalence of epilepsy has recently escalated in Korea due to an increasing incidence among the rapidly growing elderly population.5
A decreasing trend of the CMR in the 2000s might indicate an improvement in epilepsy care. The increased CMR in the elderly population contributed to a recent increase in the overall CMR, and the aging of the population is accompanied by a decreasing tendency in ASMR. The reason for the steep increase in both the CMR and PM during 1999–2002 is unclear. One of the probable explanations is increased registration in death certificates due to the recognition of epilepsy improving during this period. Also, new antiseizure medications and epilepsy surgeries were actively introduced in Korea in the late 1990s.
In our study, CMR and PM values were higher in males than in females, which meant that the prevalence and incidence of epilepsy were both higher in males.20,21,22 The SMR was also slightly higher in males than in females in previous studies.8 The increased mortality rate for males is partially attributable to excess mortality from accidental causes and suicides.21
This study was subject to several limitations. We did not include ICD-10 code R56 (convulsion) because of its diagnostic uncertainty. However, some deaths caused by epilepsy or SE could be coded as R56. SUDEP or death caused by unintentional injuries and suicides in PWE might not be coded as epilepsy.
In conclusion, in Korea there has been a decreasing tendency of mortality caused by epilepsy and SE in the overall population. However, epilepsy is still one of the notable causes of death in children, and epilepsy-related death had an increasing trend in the elderly population. This indicates the need for further research into epilepsy and the development of care systems in a superaging society.
Footnotes
- Conceptualization: Seul Gi Moon, Hyun Kyung Kim, Seo-Young Lee.
- Data curation: Seul Gi Moon, Jung-Kyeom Kim.
- Formal analysis: Seul Gi Moon, Hyun Kyung Kim, Seo-Young Lee.
- Investigation: Seul Gi Moon, Seo-Young Lee.
- Methodology: Seul Gi Moon, Jung-Kyeom Kim, Seo-Young Lee.
- Project administration: Seo-Young Lee.
- Resources: Seul Gi Moon, Jung-Kyeom Kim.
- Supervision: Hyun Kyung Kim, Seo-Young Lee.
- Validation: Hyun Kyung Kim, Seo-Young Lee.
- Visualization: Seul Gi Moon, Seo-Young Lee.
- Writing—original draft: Seul Gi Moon, Seo-Young Lee.
- Writing—review & editing: Seul Gi Moon, Hyun Kyung Kim, Seo-Young Lee.
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
Funding Statement: None
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.3988/jcn.2022.0119.
Statistics of death caused by epilepsy or SE according to age in 2019
Trend of mortality caused by epilepsy or SE during 1993–2019
References
- 1.Beghi E. The epidemiology of epilepsy. Neuroepidemiology. 2020;54:185–191. doi: 10.1159/000503831. [DOI] [PubMed] [Google Scholar]
- 2.GBD 2015 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1603–1658. doi: 10.1016/S0140-6736(16)31460-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee SY, Chung SE, Kim DW, Eun SH, Kang HC, Cho YW, et al. Estimating the prevalence of treated epilepsy using administrative health data and its validity: ESSENCE study. J Clin Neurol. 2016;12:434–440. doi: 10.3988/jcn.2016.12.4.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jeon JY, Lee H, Shin JY, Moon HJ, Lee SY, Kim JM. Increasing trends in the incidence and prevalence of epilepsy in Korea. J Clin Neurol. 2021;17:393–399. doi: 10.3988/jcn.2021.17.3.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Linehan C, Berg AT. In: Wyllie’s Treatment of Epilepsy: Principles and Practice. 7th ed. Wyllie E, editor. Philadelphia, PA: Lippincott Williams & Wilkins; 2021. Epidemiologic aspects of epilepsy; pp. 1–12. [Google Scholar]
- 7.Watila MM, Balarabe SA, Ojo O, Keezer MR, Sander JW. Overall and cause-specific premature mortality in epilepsy: a systematic review. Epilepsy Behav. 2018;87:213–225. doi: 10.1016/j.yebeh.2018.07.017. [DOI] [PubMed] [Google Scholar]
- 8.Thurman DJ, Logroscino G, Beghi E, Hauser WA, Hesdorffer DC, Newton CR, et al. The burden of premature mortality of epilepsy in high-income countries: a systematic review from the Mortality Task Force of the International League Against Epilepsy. Epilepsia. 2017;58:17–26. doi: 10.1111/epi.13604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Korean Statistical Information Service. Cause of death statistics [Internet] Daejeon: KOSIS; [cited 2021 Jul 5]. Available from: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B34E07&conn_path=I2 . [Google Scholar]
- 10.Vital Statistics Division, Statistics Korea. Shin HY, Lee JY, Kim JE, Lee S, Youn H, et al. Cause-of-death statistics in 2016 in the Republic of Korea. J Korean Med Assoc. 2018;61:573–584. [Google Scholar]
- 11.Korean Statistical Information Service. Total population of year [Internet] Daejeon: KOSIS; [cited 2021 Jul 5]. Available from: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B040M5&conn_path=I2 . [Google Scholar]
- 12.Fiest KM, Sauro KM, Wiebe S, Patten SB, Kwon CS, Dykeman J, et al. Prevalence and incidence of epilepsy: a systematic review and meta-analysis of international studies. Neurology. 2017;88:296–303. doi: 10.1212/WNL.0000000000003509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJL, Lozano R, Inoue M. Age Standardization of Rates: A New WHO Standard (GPE Discussion Paper Series: no. 31) Geneva: World Health Organization; 2001. [Google Scholar]
- 14.Suárez-Medina R, Morales-Chacón LM, Venero-Fernández SJ, Liu C, Fogarty AW, Neligan A. Epilepsy mortality trends in Cuba compared with England and Wales: 1987-2010. Epilepsy Behav. 2018;85:72–75. doi: 10.1016/j.yebeh.2018.04.031. [DOI] [PubMed] [Google Scholar]
- 15.Tomson T, Walczak T, Sillanpaa M, Sander JW. Sudden unexpected death in epilepsy: a review of incidence and risk factors. Epilepsia. 2005;46 Suppl 11:54–61. doi: 10.1111/j.1528-1167.2005.00411.x. [DOI] [PubMed] [Google Scholar]
- 16.GBD 2015 Neurological Disorders Collaborator Group. Global, regional, and national burden of neurological disorders during 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 2017;16:877–897. doi: 10.1016/S1474-4422(17)30299-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gallentine WB. In: Practical Epilepsy. Husain AM, editor. New York: Demos Medical Publishing; 2015. Neonatal seizures; pp. 54–58. [Google Scholar]
- 18.Levira F, Thurman DJ, Sander JW, Hauser WA, Hesdorffer DC, Masanja H, et al. Premature mortality of epilepsy in low- and middle-income countries: a systematic review from the Mortality Task Force of the International League Against Epilepsy. Epilepsia. 2017;58:6–16. doi: 10.1111/epi.13603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Banerjee PN, Filippi D, Allen Hauser W. The descriptive epidemiology of epilepsy-a review. Epilepsy Res. 2009;85:31–45. doi: 10.1016/j.eplepsyres.2009.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McHugh JC, Delanty N. Epidemiology and classification of epilepsy: gender comparisons. Int Rev Neurobiol. 2008;83:11–26. doi: 10.1016/S0074-7742(08)00002-0. [DOI] [PubMed] [Google Scholar]
- 21.Rafnsson V, Olafsson E, Hauser WA, Gudmundsson G. Cause-specific mortality in adults with unprovoked seizures. A population-based incidence cohort study. Neuroepidemiology. 2001;20:232–236. doi: 10.1159/000054795. [DOI] [PubMed] [Google Scholar]
- 22.Neligan A, Hauser WA, Sander JW. The epidemiology of the epilepsies. Handb Clin Neurol. 2012;107:113–133. doi: 10.1016/B978-0-444-52898-8.00006-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Statistics of death caused by epilepsy or SE according to age in 2019
Trend of mortality caused by epilepsy or SE during 1993–2019
Data Availability Statement
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.