Key Points
Question
Did the prevalence of cardiovascular risk factors, as well as treatment and control rates, change among young adults from 2009 through March 2020?
Findings
In this serial cross-sectional study of 12 924 adults aged 20 to 44 years, there were increases in the prevalence of diabetes (from 3.0% to 4.1%) and obesity (from 32.7% to 40.9%), no improvement in the prevalence of hypertension (from 9.3% to 11.5%), and a decrease in the prevalence of hyperlipidemia (from 40.5% to 36.1%) from 2009-2010 to 2017-2020. Black young adults had the highest rates of hypertension over the study period, and increases in hypertension were observed among Mexican American and other Hispanic adults, while Mexican American adults experienced a significant rise in diabetes. Blood pressure control did not significantly change among young adults treated for hypertension, while glycemic control remained suboptimal throughout the study period.
Meaning
These data show a high and rising burden of most cardiovascular risk factors in young US adults, especially for Black, Hispanic, and Mexican American individuals.
Abstract
Importance
Declines in cardiovascular mortality have stagnated in the US over the past decade, in part related to worsening risk factor control in older adults. Little is known about how the prevalence, treatment, and control of cardiovascular risk factors have changed among young adults aged 20 to 44 years.
Objective
To determine if the prevalence of cardiovascular risk factors (hypertension, diabetes, hyperlipidemia, obesity, and tobacco use), treatment rates, and control changed among adults aged 20 to 44 years from 2009 through March 2020, overall and by sex and race and ethnicity.
Design, Setting, and Participants
Serial cross-sectional analysis of adults aged 20 to 44 years in the US participating in the National Health and Nutrition Examination Survey (2009-2010 to 2017–March 2020).
Main Outcomes and Measures
National trends in the prevalence of hypertension, diabetes, hyperlipidemia, obesity, and smoking history; treatment rates for hypertension and diabetes; and blood pressure and glycemic control in those receiving treatment.
Results
Among 12 924 US adults aged 20 to 44 years (mean age, 31.8 years; 50.6% women), the prevalence of hypertension was 9.3% (95% CI, 8.1%-10.5%) in 2009-2010 and 11.5% (95% CI, 9.6%-13.4%) in 2017-2020. The prevalence of diabetes (from 3.0% [95% CI, 2.2%-3.7%] to 4.1% [95% CI, 3.5%-4.7%]) and obesity (from 32.7% [95% CI, 30.1%-35.3%] to 40.9% [95% CI, 37.5%-44.3%]) increased from 2009-2010 to 2017-2020, while the prevalence of hyperlipidemia decreased (from 40.5% [95% CI, 38.6%-42.3%] to 36.1% [95% CI, 33.5%-38.7%]). Black adults had high rates of hypertension across the study period (2009-2010: 16.2% [95% CI, 14.0%-18.4%]; 2017-2020: 20.1% [95% CI, 16.8%-23.3%]), and significant increases in hypertension were observed among Mexican American adults (from 6.5% [95% CI, 5.0%-8.0%] to 9.5% [95% CI, 7.3%-11.7%]) and other Hispanic adults (from 4.4% [95% CI, 2.1%-6.8%] to 10.5% [95% CI, 6.8%-14.3%]), while Mexican American adults had a significant rise in diabetes (from 4.3% [95% CI, 2.3%-6.2%] to 7.5% [95% CI, 5.4%-9.6%]). The percentage of young adults treated for hypertension who achieved blood pressure control did not significantly change (from 65.0% [95% CI, 55.8%-74.2%] in 2009-2010 to 74.8% [95% CI, 67.5%-82.1%] in 2017-2020], while glycemic control among young adults receiving treatment for diabetes remained suboptimal throughout the study period (2009-2010: 45.5% [95% CI, 27.7%-63.3%]) to 2017-2020: 56.6% [95% CI, 39.2%-73.9%]).
Conclusions and Relevance
In the US, diabetes and obesity increased among young adults from 2009 to March 2020, while hypertension did not change and hyperlipidemia declined. There was variation in trends by race and ethnicity.
This study assesses the prevalence rates of cardiovascular risk factors (hypertension, diabetes, hyperlipidemia, obesity, and tobacco use), treatment, and control among adults aged 20 to 44 years from 2009 through March 2020, overall and by sex and race and ethnicity.
Introduction
In the US, declines in cardiovascular mortality have stagnated over the last decade. One concerning possibility behind these trends is that they may reflect changes in the burden of cardiovascular risk factors.1 Onset of cardiovascular risk factors early in life is associated with a higher risk of cardiovascular disease and events, resulting in substantial loss of disability-adjusted life-years and years of life.2,3 Therefore, a rise in the burden of cardiovascular risk factors among young adults could have major public health implications as the US population ages.
Despite emerging concerns about the cardiovascular health of young adults, little is known about how the prevalence of risk factors has changed in this segment of the population on a national scale. Prior studies examining cardiovascular risk factor prevalence in the US have not focused on adults aged 20 to 44 years nor changes by sex and race and ethnicity within this young population.4,5,6 Recent analyses suggest a rise in prediabetes among adolescents and obesity among the youngest adults (aged 18-25 years).7,8 In addition, shifts in guidelines from the American College of Cardiology and American Heart Association (ACC/AHA),9,10,11 along with health policy initiatives (eg, Medicaid expansion under the Affordable Care Act) that expanded access to insurance coverage and health care for young adults,12,13,14,15,16 have likely influenced population-level treatment rates and risk factor control. Understanding trends in cardiovascular risk factor prevalence, treatment, and control among young adults is critical from a public health standpoint given recent data suggesting that cardiovascular disease and death rates may now be increasing in this population.17,18,19
Therefore, in this study, we analyzed more than a decade of data from the National Health and Nutrition Examination Survey (NHANES) to answer 3 questions. First, how did the prevalence of cardiovascular risk factors (hypertension, diabetes, hyperlipidemia, obesity, and tobacco use) change among adults aged 20 to 44 years from 2009 through March 2020? Second, did these trends vary by sex and race and ethnicity? And third, did risk factor treatment rates and control improve or deteriorate over this period?
Methods
Study Population
We included data from NHANES survey cycles 2009-2010 to 2017–March 2020 (N = 55 999). NHANES uses a complex, multistage probability sampling design to generate nationally representative estimates of health in the noninstitutionalized US population. The survey is conducted in 2-year cycles by the Centers for Disease Control and Prevention (CDC). Data are collected through in-person interviews and medical examinations, which include physical examinations and laboratory measurements. Because NHANES was suspended during the COVID-19 pandemic, data were collected only until March 2020. To ensure nationally representative estimates, the CDC combined cycles 2017-2018 and 2019-2020.
We identified adults aged 20 to 44 years who participated in NHANES from January 2009 to March 2020. Age, sex, and race and ethnicity were determined by self-report to closed-ended questions. Races and ethnicities included non-Hispanic Asian, non-Hispanic Black, Mexican American, other Hispanic, and non-Hispanic White. Other Hispanic adults included those self-reporting as Hispanic but not as Mexican American. Individuals who did not identify as one of the aforementioned racial or ethnic groups, or who identified as multiracial, were recorded as other race or ethnicity in NHANES. Nationally representative estimates for Asian adults were made available by NHANES starting in 2011-2012. NHANES is approved by the National Center for Health Statistics Institutional Review Board. Written informed consent was obtained from participants. Data are made publicly available by the CDC.
Outcomes
We examined the prevalence of cardiovascular risk factors, including hypertension, diabetes, hyperlipidemia, obesity, and smoking history, based on medical examination data (systolic blood pressure, diastolic blood pressure, hemoglobin A1c, total cholesterol, and body mass index). Blood pressure was obtained by having participants rest quietly for 5 minutes, after which 3 measurements were taken. The mean of these 3 measurements was assigned as participants’ blood pressure. Hemoglobin A1c and total cholesterol were obtained by nonfasting laboratory measurement. Body mass index was obtained by measurement of weight and standing height and calculated as weight in kilograms divided by height in meters squared. Definitions for each cardiovascular risk factor were based on prior US Department of Health and Human Services and CDC reports to ensure consistency with prior health surveillance reports.20,21 Hypertension was defined as a systolic blood pressure of 140 mm Hg or greater, diastolic blood pressure of 90 mm Hg or greater, or a prescription for antihypertensive therapy.4,22 Diabetes was defined as a hemoglobin A1c of 6.5% or greater or a health care diagnosis of diabetes. Hyperlipidemia was defined as a total cholesterol of 200 mg/dL or greater or a health care diagnosis of high cholesterol. Obesity was defined as a body mass index of 30 or greater. Smoking history was defined as self-report of smoking at least 100 cigarettes ever. Uniform definitions for all outcomes were used over the study period.
We also examined cardiovascular risk factor treatment and control rates. Treatment in adults with hypertension was defined as a self-report of taking antihypertensive medications. Treatment in adults with diabetes was defined as a self-report of taking pills for diabetes or insulin. Control was assessed among adults receiving treatment for each respective condition, consistent with prior reports.4,15 Hypertension was considered controlled if systolic blood pressure was less than 140 mm Hg and diastolic blood pressure was less than 90 mm Hg. Because the 2017 ACC/AHA guidelines recently lowered blood pressure targets for young adults from less than 140/90 mm Hg to less than 130/80 mm Hg, we also assessed control rates using this more stringent goal. Diabetes was considered controlled if hemoglobin A1c was less than 7%.9,23 We did not assess treatment (or control) in young adults with hyperlipidemia given major changes in guideline recommendations over the study period that shifted away from lipid-level targets for treatment.10,24
Statistical Analysis
We first determined baseline characteristics of adults aged 20 to 44 years and estimated the annual prevalence of each cardiovascular risk factor, as well as treatment and control rates among those with a diagnosis of hypertension or diabetes, from survey cycles 2009-2010 to 2017–March 2020. Age-adjusted means of each outcome were determined with direct standardization using the 2010 US population as a reference (aged 20-32 years and aged 33-44 years). Trends in each age-adjusted outcomes were assessed with survey-weighted linear regression. We then repeated this analysis to estimate the prevalence of each cardiovascular risk factor by sex and race and ethnicity. To provide a contemporary assessment of the prevalence of risk factors by subgroups, we pooled the most recent NHANES cycles (2015-2016 and 2017–March 2020). We then fit multivariable logistic regression models to compare risk factor prevalence across subgroups of sex (after adjustment for age and race and ethnicity), as well as race and ethnicity (after adjustment for age and sex). Confidence intervals were determined by Taylor series linearization. For all analyses, NHANES survey weights, which account for the complex, cluster-stratified design of NHANES, were used to calculate nationally representative estimates.25
Complete case analysis by outcome was done, and imputation for missing values was not performed. Missingness rates were 8.9% for blood pressure, 5.9% for hemoglobin A1c, 6.9% for total cholesterol, less than 1% for body mass index, and less than 1% for smoking history. Age, sex, and race and ethnicity had no missing values. A 2-sided P < .05 was used for all analyses. Analyses were conducted in R version 4.2.1 (R Foundation) using the “survey” package.
Results
The study population included 12 924 young adults aged 20 to 44 years (mean age, 31.8 years; 50.6% women), of whom 12.8% were Black, 12.0% Mexican American, 8.0% other Hispanic, 57.2% White, and 10.0% other races and ethnicities (including Asian; these individuals were included as a separate category only starting in 2011). Baseline characteristics for these adults are presented in Table 1. Nationally representative estimates of blood pressure, hemoglobin A1c, total cholesterol, and body mass index for all young adults and key subgroups (sex and race and ethnicity) are shown in eFigures 1-3 in Supplement 1.
Table 1. Baseline Characteristics of the Study Population in the National Health and Nutrition Examination Survey (NHANES), 2009-2010 to 2017–March 2020a.
| Characteristics | NHANES cycle, % (95% CI) | ||||
|---|---|---|---|---|---|
| 2009-2010 (n = 2584) | 2011-2012 (n = 2328) | 2013-2014 (n = 2414) | 2015-2016 (n = 2324) | 2017–March 2020 (n = 3274) | |
| Age, median (IQR), y | 32 (26-39) | 32 (25-38) | 32 (25-38) | 31 (26-38) | 32 (25-38) |
| Sex | |||||
| Female | 50.7 (48.9-52.5) | 50.4 (48.3-52.5) | 50.8 (49.1-52.5) | 51.1 (49.2-52.9) | 50.1 (47.9-52.2) |
| Male | 49.3 (47.5-51.1) | 49.6 (47.5-51.7) | 49.2 (47.5-50.9) | 48.9 (47.1-50.8) | 49.9 (47.8-52.1) |
| Race and ethnicityb | |||||
| Asian | 6.1 (4.1-8.0) | 6.4 (4.7-8.0) | 7.0 (4.2-9.8) | 6.9 (4.8-9.0) | |
| Black | 12.5 (10.4-14.5) | 12.7 (8.2-17.2) | 12.7 (8.2-17.2) | 12.7 (8.8-16.6) | 13.1 (8.1-18.1) |
| Mexican American | 11.7 (6.8-16.6) | 11.6 (6.9-16.3) | 11.6 (6.9-16.3) | 12.8 (8.7-16.9) | 12.1 (6.4-17.8) |
| Other Hispanic | 6.7 (3.5-9.9) | 8.3 (4.8-11.8) | 8.3 (4.8-11.8) | 7.4 (4.7-10.2) | 8.3 (5.7-10.9) |
| White | 60.6 (53.1-68.1) | 58.3 (49.9-66.7) | 58.3 (49.9-66.7) | 56.9 (49.6-64.3) | 55.4 (46.7-64.1) |
| Other races and ethnicities | 8.6 (5.9-11.3) | 3.1 (2.1-4) | 3.8 (2.4-5.2) | 4.1 (3.3-4.9) | 4.4 (3.5-5.2) |
| Education | |||||
| High school or less | 39.1 (35.0-43.2) | 33.0 (26.6-39.5) | 36.3 (31.9-40.7) | 33.8 (28.6-39.0) | 35.9 (31.4-40.4) |
| Some college | 32.6 (30.7-34.5) | 36.1 (30.8-41.3) | 35.0 (32.9-37.1) | 33.6 (29.3-37.9) | 31.4 (28.8-34.1) |
| College graduate | 28.3 (24.7-31.9) | 30.9 (25.5-36.2) | 28.7 (24.4-33.1) | 32.6 (26.1-39.0) | 32.6 (27.4-37.9) |
| Health insurancec | |||||
| Private | 57.8 (55.2-60.4) | 57.3 (52.5-62.0) | 58.4 (54.6-62.2) | 59.0 (54.0-64.1) | 56.8 (53.3-60.3) |
| Medicare | 0.5 (0.3-0.7) | 1.2 (0.4-1.9) | 1.1 (0.4-1.7) | 1.0 (0.4-1.5) | 1.5 (1.1-1.9) |
| Medicaid | 5.9 (4.6-7.2) | 6.5 (4.4-8.7) | 8.4 (6.7-10.1) | 8.4 (5.6-11.1) | 12.5 (9.6-15.3) |
| Other | 5.9 (4.0-7.7) | 6.5 (4.4-8.6) | 5.9 (4.5-7.2) | 10.8 (9.3-12.2) | 9.5 (8.0-11.0) |
| Uninsured | 29.9 (27.0-32.7) | 28.5 (24.5-32.5) | 26.3 (23.1-29.5) | 20.9 (16.6-25.1) | 19.7 (16.5-23.0) |
| Ratio of family income to poverty, %d | |||||
| <100 | 19.5 (16.7-22.2) | 23.2 (17.5-28.9) | 20.2 (16.4-24.1) | 17.1 (14.0-20.2) | 15.9 (13.4-18.3) |
| 100-199 | 21.1 (18.9-23.4) | 22.0 (19.0-25.0) | 22.4 (20.4-24.4) | 23.1 (19.6-26.6) | 20.3 (17.1-23.5) |
| 200-299 | 15.6 (13.5-17.7) | 13.0 (10.8-15.3) | 16.2 (13.8-18.6) | 19.7 (16.2-23.3) | 15.7 (13.3-18.0) |
| ≥300 | 43.8 (41.6-46.0) | 41.7 (35.1-48.4) | 41.1 (35.7-46.6) | 40.1 (33.9-46.3) | 48.2 (43.5-52.8) |
| Regular exercisee | 33.0 (29.3-36.7) | 37.3 (31.3-43.3) | 34.7 (31.9-37.6) | 41.4 (37.6-45.2) | 40.8 (37.2-44.5) |
| Recent weight gainf | 40.2 (37.6-42.7) | 38.0 (34.9-41.2) | 39.5 (36.6-42.4) | 40.1 (37.3-42.8) | 40.0 (38.1-41.9) |
| Recent dietingf | 19.9 (17.8-21.9) | 19.8 (17.4-22.2) | 22.3 (20.6-24.0) | 24.4 (22.6-26.3) | 26.6 (24.1-29.0) |
| Body mass indexg | |||||
| <18.5 (Underweight) | 1.9 (1.4-2.5) | 2.4 (1.7-3.1) | 1.6 (1.1-2.1) | 2.0 (1.4-2.7) | 2.0 (1.3-2.7) |
| 18.5-24.9 (Normal) | 34.3 (30.8-37.8) | 34.3 (29.2-39.5) | 32.2 (29.6-34.8) | 31.3 (27.8-34.9) | 29.4 (26.4-32.3) |
| 25-29.9 (Overweight) | 30.9 (28.8-33.0) | 31.0 (27.3-34.7) | 30.0 (28.7-31.4) | 29.1 (27.1-31) | 27.6 (25.9-29.3) |
| ≥30 (Obese) | 32.8 (30.2-35.5) | 32.3 (29.2-35.4) | 36.2 (33.5-38.9) | 37.6 (33.7-41.5) | 41.0 (37.6-44.4) |
| Blood pressure, mm Hgh | |||||
| Systolic | |||||
| <120 | 69.2 (67.1-71.3) | 67.2 (63.8-70.6) | 69.3 (66.7-71.9) | 62.8 (59.7-65.9) | 68.9 (66.2-71.6) |
| 120-139 | 26.9 (24.6-29.3) | 29.1 (26.4-31.9) | 26.1 (23.2-29.0) | 32.9 (30.0-35.8) | 27.7 (25.2-30.3) |
| ≥140 | 3.9 (3-4.8) | 3.7 (2.8-4.6) | 4.6 (3.6-5.6) | 4.3 (3.2-5.3) | 3.4 (2.8-4.0) |
| Diastolic | |||||
| <80 | 83.0 (80.4-85.5) | 80.9 (77.6-84.1) | 86.8 (85.8-87.8) | 84.4 (81.4-87.5) | 76.5 (73.9-79.2) |
| 80-89 | 13.3 (11.2-15.5) | 15.0 (12.0-18.0) | 10.2 (9.1-11.4) | 12.1 (9.3-14.8) | 17.6 (15.6-19.6) |
| ≥90 | 3.7 (2.9-4.5) | 4.1 (3.2-5) | 3 (2.3-3.6) | 3.5 (2.6-4.5) | 5.9 (4.7-7.0) |
| Hemoglobin A1c, %h,i | |||||
| <6.5 | 97.7 (96.9-98.5) | 96.8 (95.9-97.7) | 97.2 (96.6-97.9) | 96.8 (95.8-97.8) | 97.2 (96.6-97.8) |
| 6.5-7.9 | 1.1 (0.6-1.6) | 1.3 (0.9-1.8) | 1.5 (0.8-2.1) | 1.6 (1-2.2) | 1.6 (1.2-1.9) |
| ≥8.0 | 1.2 (0.7-1.7) | 1.9 (1.1-2.6) | 1.3 (0.9-1.7) | 1.6 (1-2.2) | 1.2 (0.8-1.7) |
| Total cholesterol, mg/dLh,i | |||||
| <200 | 64.4 (62.8-66.1) | 66.3 (63.5-69.1) | 69.0 (65.4-72.6) | 70.4 (67.7-73) | 71.9 (69.4-74.4) |
| 200-239 | 26.2 (24.4-28.1) | 25.4 (22.6-28.3) | 22.1 (19-25.2) | 21.6 (19.7-23.4) | 21.5 (19.6-23.4) |
| ≥240 | 9.3 (8.0-10.6) | 8.2 (6.9-9.5) | 8.9 (7.5-10.3) | 8.1 (6.5-9.7) | 6.6 (5.3-7.9) |
SI conversion: To convert total cholesterol to millimoles per deciliter, multiply by 0.0259.
Nationally representative estimates of US adults aged 20 to 44 years from NHANES, 2009 to March 2020. Age, sex, education, health insurance coverage, and smoking history are based on self-report.
Race and ethnicity were based on self-report to closed-ended questions. Asian, Black, and White adults included only those self-reporting as non-Hispanic. Participants were able to self-identify as multiple races. Other races and ethnicities included participants responding as multiracial or as a race or ethnicity group that was not listed. Other races and ethnicities included Asian adults prior to 2011-2012; NHANES began separately reporting this group only from 2011-2012 onward.
Health insurance was based on self-report. Other health insurance category includes Medigap, State Children’s Health Insurance Program, military health care, Indian Health Service, state-sponsored health plans, other government, single service, and unknown insurance plans.
Family income was based on self-report. The federal poverty level for a family of 4 was $26 200 in 2020.
Defined as affirmative response to engaging in vigorous exercise within a typical week.
Defined as an affirmative response within the last year.
Body mass index was based on physical examination of height and weight, defined as weight in kilograms divided by height in meters squared. Categories (underweight, normal weight, overweight, and obese weight) were based on standard Centers for Disease Control and Prevention classifications.
Blood pressure, hemoglobin A1c, and total cholesterol were based on physical or laboratory measurements.
Diabetes is defined as a hemoglobin A1c of ≥6.5% and hyperlipidemia as a total cholesterol level of ≥200 mg/dL.
Prevalence of Cardiovascular Risk Factors
The age-adjusted prevalence of hypertension among adults aged 20 to 44 years was 9.3% (95% CI, 8.1%-10.5%) in 2009-2010 and 11.5% (95% CI, 9.6%-13.4%) in 2017-2020 (P = .09 for linear trend). In addition, the prevalence of diabetes increased significantly over this period, from 3.0% (95% CI, 2.2%-3.7%) in 2009-2010 to 4.1% (95% CI, 3.5%-4.7%) in 2017-2020 (P = .01 for trend), as did obesity (from 32.7% [95% CI, 30.1%-35.3%] in 2009-2010 to 40.9% [95% CI, 37.5%-44.3%] in 2017-2020; P < .001 for trend). In contrast, the prevalence of hyperlipidemia significantly decreased from 40.5% (95% CI, 38.6%-42.3%) in 2009-2010 to 36.1% (95% CI, 33.5%-38.7%) in 2017-2020 (P = .002 for trend), while there was no change in smoking history (P = .99 for linear trend) (Figure 1).
Figure 1. Age-Adjusted Trends in the Prevalence of Hypertension, Diabetes, Hyperlipidemia, Obesity, and Smoking History Among US Adults Aged 20 to 44 Years, 2009-2010 to 2017–March 2020.
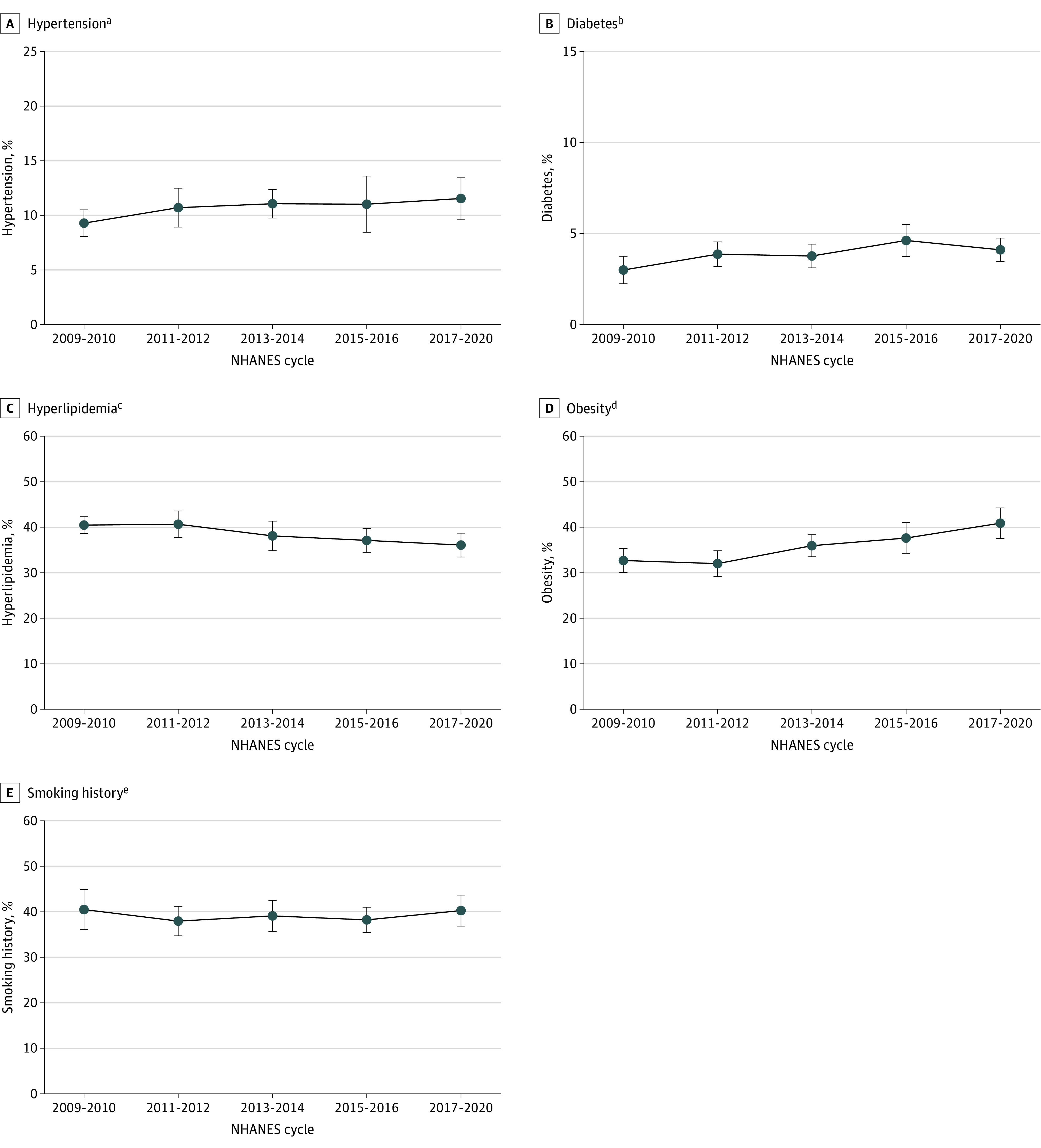
Nationally representative estimates of the prevalence of cardiovascular risk factors among US adults aged 20 to 44 years from the National Health and Nutrition Examination Survey (NHANES), 2009 to March 2020. Whiskers indicate 95% confidence intervals.
aHypertension was defined as systolic blood pressure of ≥140 mm Hg, diastolic blood pressure of ≥90 mm Hg, or a prescription for antihypertensive therapy.
bDiabetes was defined as a hemoglobin A1c of ≥6.5% or a health care diagnosis of diabetes.
cHyperlipidemia was defined as total cholesterol level of ≥200 mg/dL or a health care diagnosis of high cholesterol.
dObesity was defined as body mass index of ≥30 (calculated as weight in kilograms divided by height in meters squared).
eSmoking history was defined as self-report of smoking at least 100 cigarettes ever.
Trends in the prevalence of cardiovascular risk factors were largely similar for women and men (eFigure 4 in Supplement 1), but there was variation by race and ethnicity (Figure 2). Black adults experienced the highest rates of hypertension (2009-2010: 16.2% [95% CI, 14.0%-18.4%]; 2017-2020: 20.1% [95% CI, 16.8%-23.3%]; P = .24 for trend), while increases were observed from 2009-2010 to 2017-2020 among Mexican American adults (from 6.5% [95% CI, 5.0%-8.0%] to 9.5% [95% CI, 7.3%-11.7%]; P = .05 for trend) and other Hispanic adults (from 4.4% [95% CI, 2.1%-6.8%] to 10.5% [95% CI, 6.8%-14.3%]; P = .01 for trend). Mexican American adults also experienced a significant increase in diabetes (from 4.3% [95% CI, 2.3%-6.2%] to 7.5% [95% CI, 5.4%-9.6%]; P = .007 for trend). The prevalence of obesity did not change in Black adults but significantly increased across all other racial and ethnic groups (Figure 2).
Figure 2. Age-Adjusted Trends in the Prevalence of Hypertension, Diabetes, Hyperlipidemia, Obesity, and Smoking History Among US Adults Aged 20 to 44 Years by Race and Ethnicity, 2009-2010 to 2017–March 2020.
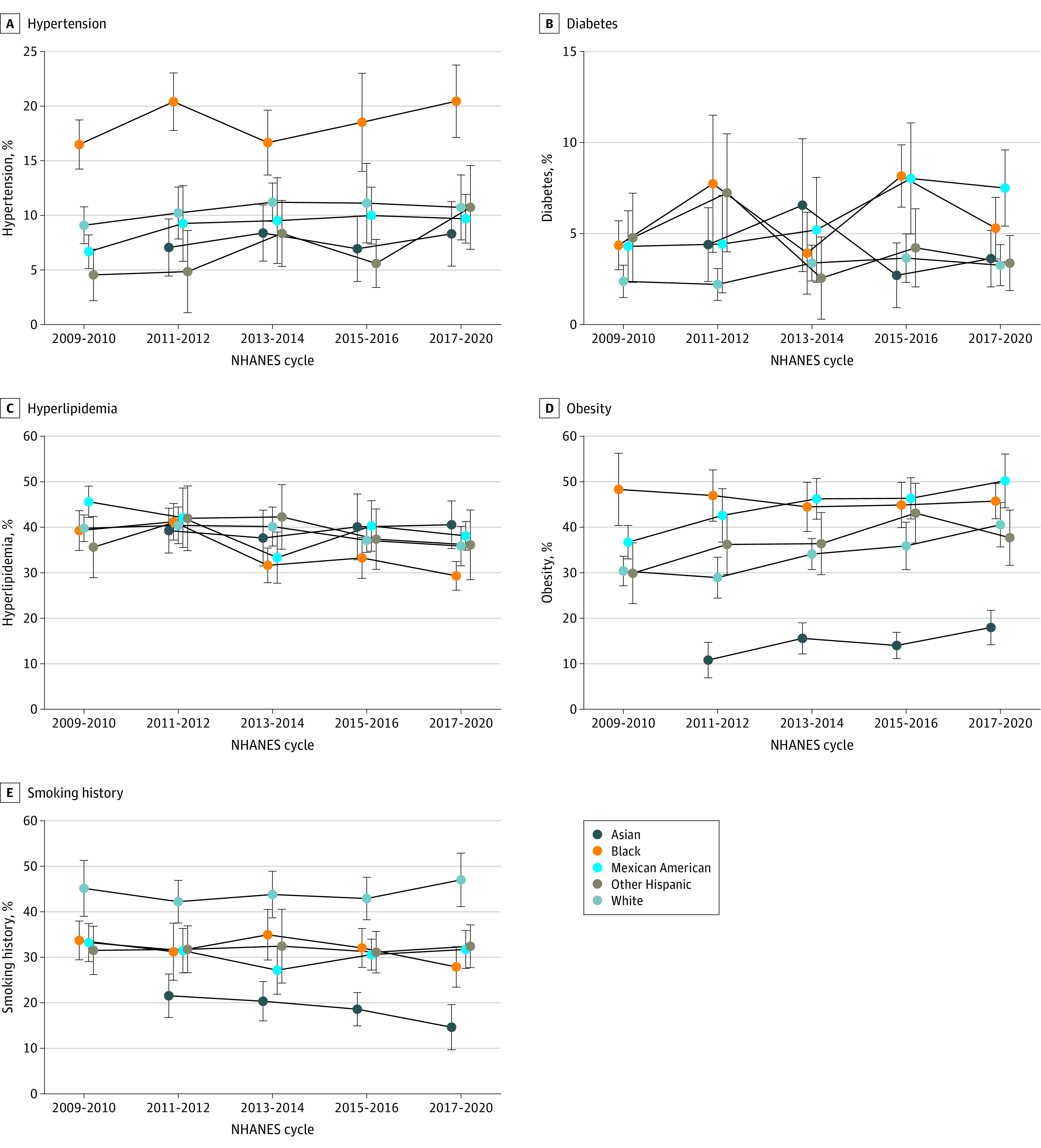
Nationally representative estimates of US adults aged 20 to 44 years from the National Health and Nutrition Examination Survey (NHANES), 2009 to March 2020. Estimates are shown by race and ethnicity; whiskers indicate 95% confidence intervals. Race and ethnicity were based on self-report to closed-ended questions. Asian, Black, and White adults included only those self-reporting as non-Hispanic. Other Hispanic adults included those self-reporting as Hispanic but not as Mexican American. Data for Asian adults were collected only from 2011 onward. For definitions of hypertension, diabetes, hyperlipidemia, obesity, and smoking history, see Figure 1 legend.
Treatment and Control Rates
Among adults aged 20 to 44 years with hypertension, age-adjusted treatment rates did not significantly change, from 56.5% (95% CI, 47.7%-65.3%) in 2009-2010 to 53.7% (95% CI, 47.6%-59.8%) in 2017-2020 (P = .80 for trend) (Figure 3A). Among those receiving treatment, age-adjusted blood pressure control rates did not significantly change, from 65.0% (95% CI, 55.8%-74.2%) in 2009-2010 to 74.8% (95% CI, 67.5%-82.1%) in 2017-2020 (P = .91 for trend) (Figure 3B). Treatment and control rates for hypertension were lower across all years when defined using new blood pressure targets from the recent 2017 ACC/AHA guidelines, although trends over time were similar (eFigure 5 in Supplement 1). For adults with diabetes, treatment rates did not significantly change over the study period, from 62.4% (95% CI, 51.2%-73.6%) in 2009-2010 to 54.5% (95% CI, 42.3%-66.7%) in 2017-2020 (P = .38 for trend) (Figure 3A). Among those receiving treatment for diabetes, glycemic control rates did not significantly improve from 2009-2010 (45.5% [95% CI, 27.7%-63.3%]) to 2017-2020 (56.6% [95% CI, 39.2%-73.9%]) (P = .22 for trend) (Figure 3B). Treatment and control rates by sex were largely similar for both conditions and are shown in eFigure 6 in Supplement 1, but could not be examined by race and ethnicity due to small sample size. We also evaluated treatment rates specifically among adults who were aware of their diagnosis (hypertension or diabetes), which are shown in eFigure 7 in Supplement 1.
Figure 3. Age-Adjusted Trends in Hypertension and Diabetes Treatment and Control Among US Adults Aged 20 to 44 Years, 2009-2010 to 2017–March 2020.
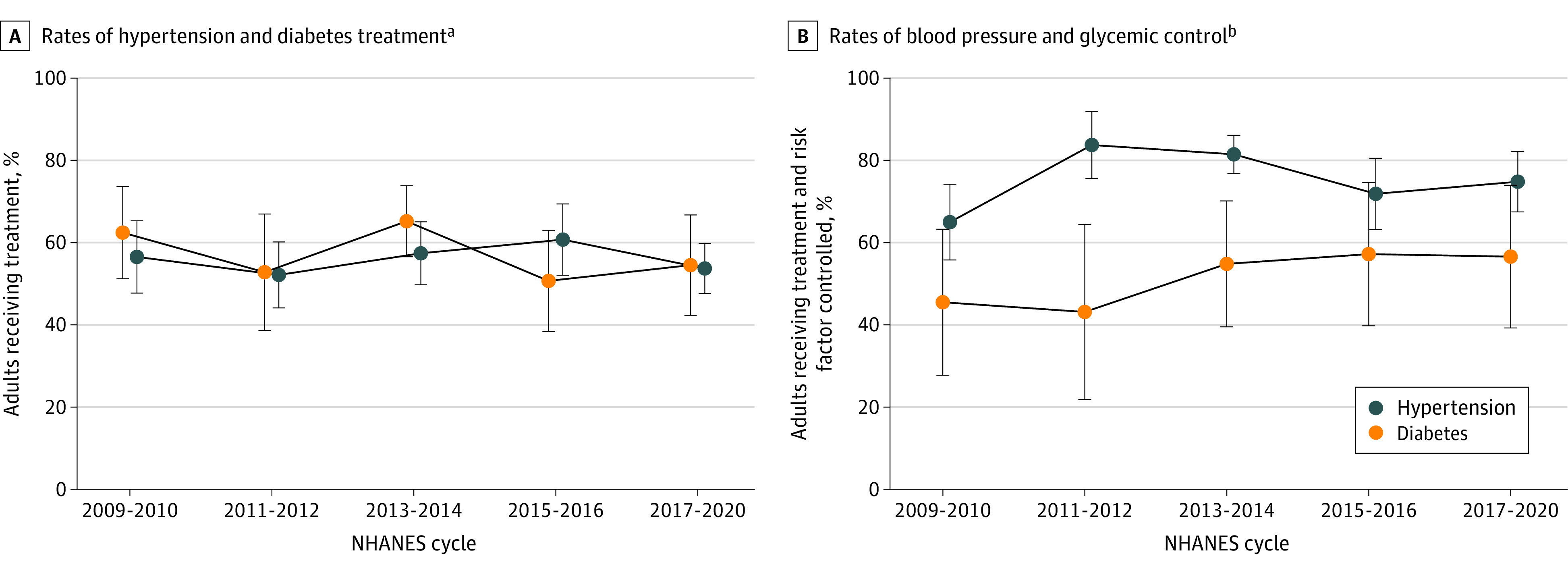
Nationally representative estimates of US adults aged 20 to 44 years from the National Health and Nutrition Examination Survey (NHANES), 2009 to March 2020. Whiskers indicate 95% confidence intervals.
aTreatment of hypertension was defined as a self-report of taking medications for blood pressure and was assessed among adults with hypertension (n = 1408). Treatment of diabetes was defined as a self-report of taking diabetes pills or insulin and was assessed among adults with diabetes (n = 631).
bControl was assessed among adults receiving treatment, consistent with prior reports (n = 693 for hypertension and n = 350 for diabetes).12,13 Hypertension was considered controlled if systolic blood pressure was <140 mm Hg and <90 mm Hg, diabetes was considered controlled if hemoglobin A1c was <7%.
Comparison of Cardiovascular Risk Factor Prevalence by Sex and by Race and Ethnicity
From 2015 to 2020, the adjusted prevalence of hypertension was higher in men compared with women (14.1% vs 8.6%; adjusted odds ratio [OR], 1.88 [95% CI, 1.55-2.29]; P < .001), as was hyperlipidemia (40.5% vs 32.6%; OR, 1.47 [95% CI, 1.26-1.71]; P < .001) and smoking history (46.6% vs 32.7%; OR, 1.86 [95% CI, 1.61-2.16]; P < .001). However, there was no significant differences in the prevalence of diabetes or obesity between men and women (Table 2).
Table 2. Association of Sex and Race and Ethnicity With Prevalence of Hypertension, Diabetes, Hyperlipidemia, Obesity, and Smoking History Among US Adults Aged 20 to 44 Years, 2015–March 2020a.
| No. | Hypertensionb | Diabetesc | Hyperlipidemiad | Obesitye | Smoking historyf | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Prevalence, % (95% CI) | Adjusted OR (95% CI) | Prevalence, % (95% CI) | Adjusted OR (95% CI) | Prevalence, % (95% CI) | Adjusted OR (95% CI) | Prevalence, % (95% CI) | Adjusted OR (95% CI) | Prevalence, % (95% CI) | Adjusted OR (95% CI) | ||
| Sexg | |||||||||||
| Female | 2990 | 8.6 (7.3-10.0) | 1 [Reference] | 4.5 (3.5-5.4) | 1 [Reference] | 32.6 (30.1-35.1) | 1 [Reference] | 39.6 (37.0-42.2) | 1 [Reference] | 32.7 (29.7-35.7) | 1 [Reference] |
| Male | 2608 | 14.1 (11.9-16.3) | 1.88 (1.55-2.29) | 4.1 (3.2-5.1) | 0.96 (0.65-1.41) | 40.5 (37.9-43.1) | 1.47 (1.26-1.71) | 39.7 (35.7-43.7) | 1.01 (0.83-1.22) | 46.6 (43.8-49.3) | 1.86 (1.61-2.16) |
| Race and ethnicityh | |||||||||||
| Asian | 773 | 7.6 (5.5-9.7) | 0.65 (0.43-0.98) | 3.3 (2.1-4.4) | 0.92 (0.59-1.44) | 40.4 (36.1-44.6) | 1.16 (0.93-1.45) | 16.5 (13.9-19.1) | 0.30 (0.24-0.38) | 16.1 (12.7-19.6) | 0.22 (0.16-0.29) |
| Black | 1371 | 19.3 (16.7-21.9) | 2.12 (1.57-2.86) | 6.4 (5.1-7.6) | 1.91 (1.28-2.86) | 30.8 (28.2-33.4) | 0.77 (0.65-0.92) | 45.4 (42.3-48.5) | 1.31 (1.08-1.60) | 29.5 (26.3-32.7) | 0.50 (0.39-0.63) |
| Mexican American | 899 | 9.6 (7.9-11.3) | 0.89 (0.63-1.26) | 7.7 (6.0-9.4) | 2.48 (1.6-3.82) | 38.9 (36.1-41.8) | 1.15 (0.95-1.39) | 48.7 (44.7-52.7) | 1.52 (1.24-1.86) | 31.3 (28.4-34.2) | 0.53 (0.42-0.67) |
| Other Hispanic | 644 | 8.7 (6.2-11.2) | 0.77 (0.51-1.15) | 3.7 (2.4-4.9) | 1.07 (0.69-1.64) | 36.6 (31.1-42.1) | 1.01 (0.75-1.36) | 39.6 (35.0-44.2) | 1.04 (0.84-1.3) | 32.0 (28.5-35.4) | 0.55 (0.42-0.72) |
| White | 1617 | 10.7 (8.4-12.9) | 1 [Reference] | 3.4 (2.5-4.3) | 1 [Reference] | 36.3 (33.5-39.2) | 1 [Reference] | 38.8 (35.2-42.4) | 1 [Reference] | 45.4 (41.4-49.5) | 1 [Reference] |
Abbreviation: OR, odds ratio.
Nationally representative estimates of US adults aged 20 to 44 years from the National Health and Nutrition Examination Survey (NHANES). Estimates are from the most recent NHANES cycles to provide contemporaneous estimates of prevalence by sex as well as by race and ethnicity (2015 to March 2020).
Hypertension was defined as a systolic blood pressure of ≥140 mm Hg, a diastolic blood pressure of ≥90 mm Hg, or a prescription for antihypertensive therapy.
Diabetes was defined as a hemoglobin A1c of ≥6.5% or a health care diagnosis of diabetes.
Hyperlipidemia was defined as a total cholesterol level of ≥200 mg/dL or a health care diagnosis of high cholesterol.
Obesity was defined as a body mass index of ≥30 (calculated as weight in kilograms divided by height in meters squared).
Smoking history was defined as self-report of smoking at least 100 cigarettes ever.
Comparisons by sex were performed using logistic regression models that adjusted for age and race and ethnicity. Sex was determined by self-report.
Comparisons by race and ethnicity were performed using logistic regression models that adjusted for age and sex. Race and ethnicity were based on self-report to closed-ended questions. Asian, Black, and White adults included only those self-reporting as non-Hispanic. Other Hispanic adults included those self-reporting as Hispanic but not as Mexican American. Data for Asian adults were collected only from 2011 onward. Other races and ethnicities were not included due to small sample size (n = 294).
Across racial and ethnic subpopulations, the adjusted prevalence of hypertension was significantly higher among Black adults compared with White adults (19.3% vs 10.7%; OR, 2.12 [95% CI, 1.57-2.86]; P < .001), while Mexican American adults and other Hispanic adults had similar prevalence rates. In addition, when compared with White adults, the prevalence of diabetes was higher among Black adults (6.4% vs 3.4%; OR, 1.91 [95% CI, 1.28-2.86]; P = .003) and Mexican American adults (7.7% vs 3.4%; OR, 2.48 [95% CI, 1.60-3.82]; P < .001), as was the prevalence of obesity (Black adults, 45.4%, vs White adults, 38.8%; OR, 1.31 [95% CI, 1.08-1.60]; P = .01; Mexican American adults, 48.7%, vs White adults, 38.8%; OR, 1.52 [95% CI, 1.24-1.86]; P < .001). In contrast, the prevalence of hyperlipidemia was similar across all racial and ethnic subpopulations, while White adults were more likely to have a smoking history than all other racial and ethnic groups (Table 2).
Discussion
In the US, the prevalence of diabetes and obesity increased among adults aged 20 to 44 years from 2009 to March 2020, while the prevalence of hypertension did not improve. In contrast, the prevalence of hyperlipidemia decreased over the study period. Black adults consistently experienced the highest rates of hypertension, and significant increases were observed among Mexican American adults and other Hispanic adults, while Mexican American adults also experienced a significant rise in diabetes. Although rates of medical treatment for hypertension and diabetes did not improve among young adults, blood pressure control was stable, while glycemic control remained suboptimal throughout the study period.
The national increases in diabetes and obesity among young adults in the US have major public health implications. The rise in obesity—to more than 40% in young adults18,19—corresponds with increases in sedentary behaviors over the same period and likely contributed to other cardiometabolic trends observed in our study.26 The prevalence rates for hypertension also increased from 9.3% to 11.5%, although this change did not reach statistical significance (P = .09). In contrast, there was a decrease in the prevalence of hyperlipidemia, potentially reflecting greater regulation on the use of trans-fatty acids and other partially hydrogenated oils.27,28 Overall, our findings highlight the need to intensify public health and clinical interventions focused on primordial and primary prevention for young adults,1,29 given evidence that cardiovascular disease mortality may now be rising in this population, as well as the potential adverse long-term public health impact of these trends in risk factors on lifetime rates of acute myocardial infarction, stroke, and heart failure.17,18,19,30
We also observed significant variation in cardiovascular risk factors across racial and ethnic groups. For example, hypertension prevalence in young Black adults was more than 2 times higher than in all other racial and ethnic groups, with no improvement over the study period. Black adults have high rates of stroke, heart failure, and hypertensive kidney disease,31,32,33 as well as the highest premature cardiovascular mortality rates in the country, in part due to a high burden of hypertension.34 The etiology of these inequities is multifactorial but likely includes disparities in early-life exposures, access to health care, and other factors rooted in structural racism.35 Scalable and realistic solutions are needed. The expansion of tailored community-based programs (eg, pharmacist-led interventions in Black barbershops)36 and large-scale health system initiatives that screen for and treat uncontrolled blood pressure for young Black adults,37 in combination with efforts to address socioeconomic factors (eg, poverty), community factors (eg, access to primary care), and environmental factors (eg, green space for regular exercise), could help reduce disparities in hypertension for this population.38,39,40,41,42
Mexican American young adults and other Hispanic young adults experienced a significance increase in the prevalence of hypertension over the study period. One potential explanation for these trends is that food insecurity is common in these groups,43 resulting in very high sodium intake.44 Mexican American adults also experienced a rise in diabetes,43 which is especially concerning because rates of undiagnosed diabetes are high in this population.45 These patterns likely reflect the high and rising burden of obesity in this population, large increases in the consumption of ultraprocessed foods,46 and socioeconomic factors, including barriers in access to insurance and healthy foods.43,47,48 Community-informed, culturally appropriate public health efforts to address the rise in diabetes among Mexican American adults are needed, given that the onset of diabetes at a young age is associated with higher rates of complications (eg, cardiovascular disease, kidney disease, retinopathy) and poorer quality of life.49
Only approximately 55% of young adults with hypertension were receiving antihypertensive treatment at both the beginning and end of the study period, while blood pressure control among those receiving treatment did not change. Nearly 1 in 4 young adults treated for hypertension were unable to achieve a blood pressure target less than 140/90 mm Hg, suggesting inadequate intensification of treatment.50 In addition, a 2017 guideline statement by the ACC/AHA changed blood pressure targets for young adults to lower thresholds (<130/80 mm Hg).51 The proportion of adults with uncontrolled hypertension based on newer guidelines was substantially higher (>75% in 2017–March 2020), and achieving these lower blood pressure goals will require large increases in screening, treatment, and monitoring.
Similar to hypertension, treatment rates for diabetes were suboptimal, with about 1 in 2 young adults with diabetes on therapy. This may partially reflect that guidelines have historically emphasized an age-based approach to diabetes screening and often have not recommended screening for adults until age 35 years, resulting in undiagnosed diabetes.52 We found that nearly half of young adults receiving treatment for diabetes had poor glycemic control (hemoglobin A1c >7%). Given the high rates of diabetes complications in the US, identifying and mitigating risk in younger adults could have downstream implications for cardiovascular health53 as well as other diabetes-related illnesses such as kidney disease, infection, and cancer.
Limitations
There are limitations to this study. First, the response rate for NHANES declined over the study period. However, NHANES sampling weights account for nonresponse bias and were used in our study. Second, treatment data were based on self-report, which is subject to recall bias and thus could lead to underestimation of treatment rates. Third, because of the relatively small sample size for analyses of treatment and control rates, the study may have lacked power to detect small changes. Fourth, we were unable to perform some subgroup analyses of treatment and control by race or ethnicity due to small sample sizes, which remains an important area for future research. Fifth, although we defined risk factor control using targets from recent clinical guidelines, recommendations for hypertension changed in 2017, which may have affected both diagnosis and treatment in clinical practice. However, we observed no significant changes in the prevalence, treatment, or control of hypertension in 2017-2020 compared with the preceding 2015-2016 NHANES cycle. We also performed additional analyses assessing treatment and control rates using lower blood pressure targets defined by the 2017 ACC/AHA guidelines, which demonstrated trends consistent with our main results.9 Sixth, we report trends through March 2020, and it is unclear whether these patterns have continued through 2022, given the impact of the COVID-19 pandemic on health behaviors and disruptions in care.54,55,56
Conclusions
In the US, diabetes and obesity increased among young adults from 2009 to March 2020, while hypertension did not change and hyperlipidemia declined. There was variation in trends by race and ethnicity.
eFigure 1. Age-Adjusted Trends in Mean Blood Pressure, Hemoglobin A1c, Total Cholesterol Levels, and Body Mass Index for US Adults Age 20 to 44 Years, 2009-2010 to 2017-March 2020
eFigure 2. Age-Adjusted Trends in Mean Blood Pressure, Hemoglobin A1c, Total Cholesterol Levels, and Body Mass Index for US Adults Age 20 to 44 Years by Sex, 2009-2010 to 2017-March 2020
eFigure 3. Age-Adjusted Trends in Mean Blood Pressure, Hemoglobin A1c, Total Cholesterol Levels, and Body Mass Index for US Adults Age 20 to 44 Years by Race and Ethnicity, 2009-2010 to 2017-March 2020
eFigure 4. Age-Adjusted Trends in the Prevalence of Hypertension, Diabetes, Hyperlipidemia, Obesity, and Smoking History Among US Adults Age 20 to 44 Years by Sex, 2009-2010 to 2017-March 2020
eFigure 5. Age-Adjusted Trends in Hypertension Treatment and Control Rates Among US Adults Aged 20 to 44 Years Using a Lower Blood Pressure Target (<130/80mmHg), 2009-2010 to 2017-March 2020
eFigure 6. Age-Adjusted Trends in Hypertension and Diabetes Treatment and Control Rates Among US Adults Aged 20 to 44 Years by Sex, 2009-2010 to 2017-March 2020
eFigure 7. Age-Adjusted Trends in Hypertension and Diabetes Treatment and Control Rates Among US Adults Aged 20 to 44 Years Aware They Had the Condition, 2009-2010 to 2017-March 2020
Data Sharing Statement
References
- 1.Gooding HC, Gidding SS, Moran AE, et al. Challenges and opportunities for the prevention and treatment of cardiovascular disease among young adults: report from a National Heart, Lung, and Blood Institute working group. J Am Heart Assoc. 2020;9(19):e016115. doi: 10.1161/JAHA.120.016115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Armstrong AC, Jacobs DR Jr, Gidding SS, et al. Framingham score and LV mass predict events in young adults: CARDIA study. Int J Cardiol. 2014;172(2):350-355. doi: 10.1016/j.ijcard.2014.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jacobs DR Jr, Woo JG, Sinaiko AR, et al. Childhood cardiovascular risk factors and adult cardiovascular events. N Engl J Med. 2022;386(20):1877-1888. doi: 10.1056/NEJMoa2109191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muntner P, Hardy ST, Fine LJ, et al. Trends in blood pressure control among US adults with hypertension, 1999-2000 to 2017-2018. JAMA. 2020;324(12):1190-1200. doi: 10.1001/jama.2020.14545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang L, Li X, Wang Z, et al. Trends in prevalence of diabetes and control of risk factors in diabetes among US adults, 1999-2018. JAMA. 2021;326(8):1-13. doi: 10.1001/jama.2021.9883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.He J, Zhu Z, Bundy JD, Dorans KS, Chen J, Hamm LL. Trends in cardiovascular risk factors in US adults by race and ethnicity and socioeconomic status, 1999-2018. JAMA. 2021;326(13):1286-1298. doi: 10.1001/jama.2021.15187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andes LJ, Cheng YJ, Rolka DB, Gregg EW, Imperatore G. Prevalence of prediabetes among adolescents and young adults in the United States, 2005-2016. JAMA Pediatr. 2020;174(2):e194498. doi: 10.1001/jamapediatrics.2019.4498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ellison-Barnes A, Johnson S, Gudzune K. Trends in obesity prevalence among adults aged 18 through 25 years, 1976-2018. JAMA. 2021;326(20):2073-2074. doi: 10.1001/jama.2021.16685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13-e115. [DOI] [PubMed] [Google Scholar]
- 10.Stone NJ, Robinson JG, Lichtenstein AH, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines . 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25)(suppl 2):S1-S45. doi: 10.1161/01.cir.0000437738.63853.7a [DOI] [PubMed] [Google Scholar]
- 11.Yano Y, Reis JP, Colangelo LA, et al. Association of blood pressure classification in young adults using the 2017 American College of Cardiology/American Heart Association blood pressure guideline with cardiovascular events later in life. JAMA. 2018;320(17):1774-1782. doi: 10.1001/jama.2018.13551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miller S, Wherry LR. Health and access to care during the first 2 years of the ACA Medicaid expansions. N Engl J Med. 2017;376(10):947-956. doi: 10.1056/NEJMsa1612890 [DOI] [PubMed] [Google Scholar]
- 13.Wadhera RK, Bhatt DL, Wang TY, et al. Association of state Medicaid expansion with quality of care and outcomes for low-income patients hospitalized with acute myocardial infarction. JAMA Cardiol. 2019;4(2):120-127. doi: 10.1001/jamacardio.2018.4577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wadhera RK, Joynt Maddox KE, Fonarow GC, et al. Association of the Affordable Care Act’s Medicaid expansion with care quality and outcomes for low-income patients hospitalized with heart failure. Circ Cardiovasc Qual Outcomes. 2018;11(7):e004729. doi: 10.1161/CIRCOUTCOMES.118.004729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aggarwal R, Bhatt DL, Rodriguez F, Yeh RW, Wadhera RK. Trends in lipid concentrations and lipid control among US adults, 2007-2018. JAMA. 2022;328(8):737-745. doi: 10.1001/jama.2022.12567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wadhera RK, Bhatt DL. Toward precision policy—the case of cardiovascular care. N Engl J Med. 2018;379(23):2193-2195. doi: 10.1056/NEJMp1806260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jain V, Minhas AMK, Morris AA, et al. Demographic and regional trends of heart failure-related mortality in young adults in the US, 1999-2019. JAMA Cardiol. 2022;7(9):900-904. doi: 10.1001/jamacardio.2022.2213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mehta NK, Abrams LR, Myrskylä M. US life expectancy stalls due to cardiovascular disease, not drug deaths. Proc Natl Acad Sci U S A. 2020;117(13):6998-7000. doi: 10.1073/pnas.1920391117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ariss RW, Minhas AMK, Lang J, et al. Demographic and regional trends in stroke-related mortality in young adults in the United States, 1999 to 2019. J Am Heart Assoc. 2022;11(18):e025903. doi: 10.1161/JAHA.122.025903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Office of Disease Prevention and Health Promotion . Healthy People 2020. Accessed June 30, 2020. https://www.healthypeople.gov/2020/About-Healthy-People
- 21.Centers for Disease Control and Prevention . Cholesterol information. Published 2021. Accessed March 1, 2022. https://www.cdc.gov/cholesterol/index.htm
- 22.National Center for Health Statistics, Centers for Disease Control and Prevention . Hypertension prevalence and control among adults: United States, 2015-2016. Published October 2017. Accessed July 1, 2020. https://www.cdc.gov/nchs/products/databriefs/db289.htm
- 23.American Diabetes Association Professional Practice Committee . Glycemic targets: standards of medical care in diabetes—2022. Diabetes Care. 2022;45(suppl 1):S83-S96. doi: 10.2337/dc22-S006 [DOI] [PubMed] [Google Scholar]
- 24.Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139(25):e1082-e1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Center for Health Statistics, Centers for Disease Control and Prevention . NHANES survey methods and analytic guidelines. Published 2020. Accessed July 1, 2020. https://wwwn.cdc.gov/nchs/nhanes/analyticguidelines.aspx#analytic-guidelines
- 26.Yang L, Cao C, Kantor ED, et al. Trends in sedentary behavior among the US population, 2001-2016. JAMA. 2019;321(16):1587-1597. doi: 10.1001/jama.2019.3636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.US Food and Drug Administration . Final determination regarding partially hydrogenated oils (removing trans fat). Published 2018. Accessed November 22, 2022. https://www.fda.gov/food/food-additives-petitions/final-determination-regarding-partially-hydrogenated-oils-removing-trans-fat
- 28.Brownell KD, Pomeranz JL. The trans-fat ban—food regulation and long-term health. N Engl J Med. 2014;370(19):1773-1775. doi: 10.1056/NEJMp1314072 [DOI] [PubMed] [Google Scholar]
- 29.Leopold JA, Antman EM. Ideal cardiovascular health in young adults with established cardiovascular diseases. Front Cardiovasc Med. 2022;9:814610. doi: 10.3389/fcvm.2022.814610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Allen NB, Siddique J, Wilkins JT, et al. Blood pressure trajectories in early adulthood and subclinical atherosclerosis in middle age. JAMA. 2014;311(5):490-497. doi: 10.1001/jama.2013.285122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Howard G, Lackland DT, Kleindorfer DO, et al. Racial differences in the impact of elevated systolic blood pressure on stroke risk. JAMA Intern Med. 2013;173(1):46-51. doi: 10.1001/2013.jamainternmed.857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pinheiro LC, Reshetnyak E, Sterling MR, Levitan EB, Safford MM, Goyal P. Multiple vulnerabilities to health disparities and incident heart failure hospitalization in the REGARDS study. Circ Cardiovasc Qual Outcomes. 2020;13(8):e006438. doi: 10.1161/CIRCOUTCOMES.119.006438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bock F, Stewart TG, Robinson-Cohen C, et al. Racial disparities in end-stage renal disease in a high-risk population: the Southern Community Cohort Study. BMC Nephrol. 2019;20(1):308. doi: 10.1186/s12882-019-1502-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kyalwazi AN, Loccoh EC, Brewer LC, et al. Disparities in cardiovascular mortality between Black and White adults in the United States, 1999 to 2019. Circulation. 2022;146(3):211-228. doi: 10.1161/CIRCULATIONAHA.122.060199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hermes Z, Joynt Maddox KE, Yeh RW, Zhao Y, Shen C, Wadhera RK. Neighborhood socioeconomic disadvantage and mortality among Medicare beneficiaries hospitalized for acute myocardial infarction, heart failure, and pneumonia. J Gen Intern Med. 2022;37(8):1894-1901. doi: 10.1007/s11606-021-07090-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Victor RG, Lynch K, Li N, et al. A cluster-randomized trial of blood-pressure reduction in Black barbershops. N Engl J Med. 2018;378(14):1291-1301. doi: 10.1056/NEJMoa1717250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood pressure control associated with a large-scale hypertension program. JAMA. 2013;310(7):699-705. doi: 10.1001/jama.2013.108769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carnethon MR, Pu J, Howard G, et al. ; American Heart Association Council on Epidemiology and Prevention, Council on Cardiovascular Disease in the Young, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, Council on Functional Genomics and Translational Biology, and Stroke Council . Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136(21):e393-e423. doi: 10.1161/CIR.0000000000000534 [DOI] [PubMed] [Google Scholar]
- 39.Howard G, Cushman M, Moy CS, et al. Association of clinical and social factors with excess hypertension risk in Black compared with White US adults. JAMA. 2018;320(13):1338-1348. doi: 10.1001/jama.2018.13467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kershaw KN, Robinson WR, Gordon-Larsen P, et al. Association of changes in neighborhood-level racial residential segregation with changes in blood pressure among Black adults: the CARDIA study. JAMA Intern Med. 2017;177(7):996-1002. doi: 10.1001/jamainternmed.2017.1226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aggarwal R, Chiu N, Loccoh EC, Kazi DS, Yeh RW, Wadhera RK. Rural-urban disparities: diabetes, hypertension, heart disease, and stroke mortality among Black and White adults, 1999-2018. J Am Coll Cardiol. 2021;77(11):1480-1481. doi: 10.1016/j.jacc.2021.01.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Erqou S, Clougherty JE, Olafiranye O, et al. Particulate matter air pollution and racial differences in cardiovascular disease risk. Arterioscler Thromb Vasc Biol. 2018;38(4):935-942. doi: 10.1161/ATVBAHA.117.310305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rabbitt MP, Smith MD, Coleman-Jensen A. Food security among Hispanic adults in the United States, 2011-2014. Econ Inf Bull. 2016;153:42. [Google Scholar]
- 44.Elfassy T, Sotres-Alvarez D, Van Horn L, et al. Daily intake of sodium and potassium among diverse US Hispanics/Latinos: the Hispanic Community Health Study/Study of Latinos. Am J Hypertens. 2019;32(9):868-879. doi: 10.1093/ajh/hpz073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Aggarwal R, Bibbins-Domingo K, Yeh RW, et al. Diabetes screening by race and ethnicity in the United States: equivalent body mass index and age thresholds. Ann Intern Med. 2022;175(6):765-773. doi: 10.7326/M20-8079 [DOI] [PubMed] [Google Scholar]
- 46.Rehm CD, Peñalvo JL, Afshin A, Mozaffarian D. Dietary intake among US adults, 1999-2012. JAMA. 2016;315(23):2542-2553. doi: 10.1001/jama.2016.7491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stokes M. Health and health care experiences of Hispanic adults. Kaiser Family Foundation. Published July 14, 2021. Accessed November 22, 2022. https://www.kff.org/coronavirus-covid-19/poll-finding/health-and-health-care-experiences-of-hispanic-adults/
- 48.National Center for Health Statistics, Centers for Disease Control and Prevention . Health of Mexican American population. Published 2022. Accessed November 22, 2022. https://www.cdc.gov/nchs/fastats/mexican-health.htm
- 49.Lascar N, Brown J, Pattison H, Barnett AH, Bailey CJ, Bellary S. Type 2 diabetes in adolescents and young adults. Lancet Diabetes Endocrinol. 2018;6(1):69-80. doi: 10.1016/S2213-8587(17)30186-9 [DOI] [PubMed] [Google Scholar]
- 50.Mu L, Mukamal KJ. Treatment intensification for hypertension in US ambulatory medical care. J Am Heart Assoc. 2016;5(10):e004188. doi: 10.1161/JAHA.116.004188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wright JT Jr, Williamson JD, Whelton PK, et al. ; SPRINT Research Group . A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103-2116. doi: 10.1056/NEJMoa1511939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Davidson KW, Barry MJ, Mangione CM, et al. ; US Preventive Services Task Force . Screening for prediabetes and type 2 diabetes: US Preventive Services Task Force recommendation statement. JAMA. 2021;326(8):736-743. doi: 10.1001/jama.2021.12531 [DOI] [PubMed] [Google Scholar]
- 53.Fang M, Selvin E. Thirty-year trends in complications in US adults with newly diagnosed type 2 diabetes. Diabetes Care. 2021;44(3):699-706. doi: 10.2337/dc20-2304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wadhera RK, Shen C, Gondi S, Chen S, Kazi DS, Yeh RW. Cardiovascular deaths during the COVID-19 pandemic in the United States. J Am Coll Cardiol. 2021;77(2):159-169. doi: 10.1016/j.jacc.2020.10.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wadhera RK, Figueroa JF, Rodriguez F, et al. Racial and ethnic disparities in heart and cerebrovascular disease deaths during the COVID-19 pandemic in the United States. Circulation. 2021;143(24):2346-2354. doi: 10.1161/CIRCULATIONAHA.121.054378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ahmed A, Song Y, Wadhera RK. Racial/ethnic disparities in delaying or not receiving medical care during the COVID-19 pandemic. J Gen Intern Med. 2022;37(5):1341-1343. doi: 10.1007/s11606-022-07406-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Age-Adjusted Trends in Mean Blood Pressure, Hemoglobin A1c, Total Cholesterol Levels, and Body Mass Index for US Adults Age 20 to 44 Years, 2009-2010 to 2017-March 2020
eFigure 2. Age-Adjusted Trends in Mean Blood Pressure, Hemoglobin A1c, Total Cholesterol Levels, and Body Mass Index for US Adults Age 20 to 44 Years by Sex, 2009-2010 to 2017-March 2020
eFigure 3. Age-Adjusted Trends in Mean Blood Pressure, Hemoglobin A1c, Total Cholesterol Levels, and Body Mass Index for US Adults Age 20 to 44 Years by Race and Ethnicity, 2009-2010 to 2017-March 2020
eFigure 4. Age-Adjusted Trends in the Prevalence of Hypertension, Diabetes, Hyperlipidemia, Obesity, and Smoking History Among US Adults Age 20 to 44 Years by Sex, 2009-2010 to 2017-March 2020
eFigure 5. Age-Adjusted Trends in Hypertension Treatment and Control Rates Among US Adults Aged 20 to 44 Years Using a Lower Blood Pressure Target (<130/80mmHg), 2009-2010 to 2017-March 2020
eFigure 6. Age-Adjusted Trends in Hypertension and Diabetes Treatment and Control Rates Among US Adults Aged 20 to 44 Years by Sex, 2009-2010 to 2017-March 2020
eFigure 7. Age-Adjusted Trends in Hypertension and Diabetes Treatment and Control Rates Among US Adults Aged 20 to 44 Years Aware They Had the Condition, 2009-2010 to 2017-March 2020
Data Sharing Statement


