Abstract
Overdose Good Samaritan laws (GSLs) aim to reduce mortality by providing limited legal protections when a bystander to a possible drug overdose summons help. Most research into the impact of these laws is dated or potentially confounded by coenacted naloxone access laws. Lack of awareness and trust in GSL protections, as well as fear of police involvement and legal repercussions, remain key deterrents to help-seeking. These barriers may be unequally distributed by race/ethnicity due to racist policing and drug policies, potentially producing racial/ethnic disparities in the effectiveness of GSLs for reducing overdose mortality. We used 2015–2019 vital statistics data to estimate the effect of recent GSLs on overdose mortality, overall (8 states) and by Black/White race/ethnicity (4 states). Given GSLs’ near ubiquity, few unexposed states were available for comparison. Therefore, we generated an “inverted” synthetic control method (SCM) to compare overdose mortality in new-GSL states with that in states that had GSLs throughout the analytical period. The estimated relationships between GSLs and overdose mortality, both overall and stratified by Black/White race/ethnicity, were consistent with chance. An absence of effect could result from insufficient protection provided by the laws, insufficient awareness of them, and/or reticence to summon help not addressable by legal protections. The inverted SCM may be useful for evaluating other widespread policies.
Keywords: drug overdose, Good Samaritan laws, harm reduction, law enforcement, opioids, racial/ethnic disparities, substance use, synthetic control method
Abbreviations
- CI
confidence interval
- GSL
Good Samaritan law
- NAL
naloxone access law
- SCM
synthetic control method
Between May 2020 and April 2021, mortality from drug overdose in the United States rose by nearly 29% relative to the previous 12-month period, to an estimated 100,300 deaths (1). Overdose deaths have been increasing especially sharply among Black Americans in recent years, due in part to a greater relative increase in synthetic opioid-related overdose mortality among Black Americans as compared with White Americans (2–4). Overdose Good Samaritan laws (GSLs) are a common policy response to this ongoing crisis. Many people delay calling for assistance in a potential overdose situation due to fear of negative law enforcement or criminal legal system repercussions (5–7). As of December 2018, 46 states and the District of Columbia had passed a GSL in an effort to assuage those concerns (8). While their provisions vary by state, these laws typically provide limited legal protection from prosecution, charge, and/or arrest for low-level drug offenses such as possession of controlled substances (8). Some laws also provide limited immunity from violation of the conditions of probation or parole. Depending on the state, these protections apply to a person who experiences an overdose and/or to a person who witnesses it (9).
Initial evaluations of these laws suggest that they may increase willingness to call 911 (US emergency services) for some people likely to experience or witness an overdose (5, 10, 11). For example, Jakubowski et al. (10) found that, among 351 individuals receiving overdose prevention training at a syringe exchange program in New York City, the odds of calling 911 were 3 times higher among those who were familiar with New York State’s GSL than among those who were not. Increased willingness to call 911 may, in turn, reduce overdose death. Two national studies using National Vital Statistics System mortality data found that, by 2014, GSLs were associated with a 13%–16% reduction in opioid-related mortality; however, the 95% confidence intervals (CIs) in both studies overlapped with 0 (12, 13). The effects of these laws may also vary according to phases of the overdose crisis (e.g., the continued increase in use of synthetic opioids, including fentanyl) or with expansion of GSL protections (e.g., immunity from arrest and probation or parole violations). Findings from one recent study suggested that GSLs that protect people from arrest, in conjunction with naloxone access laws (NALs), are associated with a reduction in fatal overdose rates after a 1- to 2-year lag period, while GSLs without such protection are not (14). However, frequent enactment of GSLs and NALs concurrently or in quick succession has complicated efforts to isolate the effects of GSLs (14).
In addition, GSLs may benefit some groups more than others. The impact of a GSL on willingness to seek help and on overdose mortality may be shaped by a range of factors beyond the law’s particular provisions, and those may be patterned by race/ethnicity. In addition to fear of police involvement and legal repercussions as reasons for not calling 911, people also express concerns about consequences not covered by the GSL, including fear of police violence, stigmatization, eviction, and losing custody of children (5–7). Together, these fears may be more prevalent in Black populations, given the historical and current reality of racist policing and policies emerging from the “war on drugs”—including disproportionate search, arrest, incarceration, and sentencing of Black people. Because of these manifestations of structural racism, GSLs may reduce mortality less among Black people than among their White counterparts. The converse could also be true, however: Because Black communities have been disproportionately targeted by the “war on drugs,” they stand to gain more from the protections offered by a GSL (12, 15). Indeed, one study using data collected through 2014 found evidence that GSLs reduced overdose mortality more in non-Hispanic Black and Hispanic individuals than in non-Hispanic White individuals, although the 95% CIs overlapped for all 3 groups (12). Research on the performance of GSLs by race/ethnicity in the more recent policy and overdose context is needed.
The synthetic control method (SCM) is an increasingly popular approach for estimating the effect of policies enacted in a small number of geographic units (16). However, applying the SCM to estimate the effect of GSLs in recent years is complicated by a lack of comparison states: by December 2018, 46 states and the District of Columbia had passed a GSL (8). As a result, there were insufficient remaining states to form a well-fitting pre-GSL control group for the present analysis. We therefore used a novel strategy—what we term the “inverted SCM”—to estimate the effects of GSLs on drug overdose mortality, overall and by Black/White race/ethnicity, amid nearly ubiquitous GSLs nationwide. This method inverts the standard SCM so that states that had a GSL throughout the analytical period can serve as comparison units. As a result, the postintervention period functions as the matching period, during which the synthetic control is generated; the preintervention period, when no GSL was in effect in the intervention states, is used to estimate the effect of not having a GSL by comparing the observed and synthetic control outcomes. The inverted SCM may be useful in evaluating other policies for which few unexposed comparison states are available.
METHODS
Outcome data and variables
We examined state-level overdose mortality using 2015–2019 vital statistics data from the National Center for Health Statistics (17). We modeled 3 outcomes for each intervention state: 1) overall drug overdose mortality (International Classification of Diseases, Tenth Revision, codes X40–44, X60–64, X85, and Y10–Y14) (per 100,000 population); 2) Hispanic Black and non-Hispanic Black (“Black”) drug overdose mortality (per 100,000 Black population); and 3) non-Hispanic White drug overdose mortality (per 100,000 White population). We grouped Hispanic Black and non-Hispanic Black mortality together because 1) sociodemographic profiles and health outcomes among Hispanic Black individuals may be more similar to those of non-Hispanic Black individuals than to Hispanic non-Black individuals (18–20) and 2) Hispanic Black and non-Hispanic Black individuals may experience similar anti-Black racism.
Selection of intervention states of interest
We estimated the overall effects of GSLs in the 7 states (Ohio, Oregon, Michigan, Missouri, Nebraska, South Carolina, South Dakota) for which the following criteria were satisfied:
A GSL came into effect in 2016 or 2017, enabling evaluation of recent laws while providing at least a 12-month post-GSL period following a 12-month implementation period (12).
The state did not change from having an NAL to not having an NAL (or vice versa) within 12 months of the GSL effective date. This was to avoid confounding by a policy that is frequently coenacted with GSLs and potentially also likely to reduce overdose mortality through improved overdose response (13, 21). Ultimately, all selected states had an NAL at least 12 months prior to having a GSL.
We separately estimated the effects of GSLs in the Black and White populations in the 4 states that also met the following criterion:
3. Overdose mortality in the Black population was sufficient to enable modeling for that group, i.e., non-0 overdose mortality among Black people in at least 80% of evaluated months. This excluded Nebraska, Oregon, and South Dakota.
Web Figure 1 (available at https://doi.org/10.1093/aje/kwac122) presents overdose mortality trends, overall and by Black/White race/ethnicity, in the selected states.
Selection of comparison (donor) states
To model overall overdose mortality, we created a pool of 20 donor states that met the following criteria (Table 1):
Table 1.
Weights Applied to Donor States to Create a Synthetic Control for Each Intervention State in Order to Estimate the Effect of Implementation of Good Samaritan Laws on Overall (All Races/Ethnicities) Drug Overdose Mortality, United States, 2015–2019
| Intervention State | |||||||
|---|---|---|---|---|---|---|---|
| Donor State a | Michigan | Missouri | Nebraska | Ohio | Oregon | South Dakota | South Carolina |
| California | 0b,c | 0 | 0 | 0 | 0.10 | 0 | 0 |
| Colorado | 0 | 0 | 0 | 0 | 0 | 0.40 | 0.03 |
| Connecticut | 0.22 | 0 | 0 | 0 | 0.04 | 0 | 0 |
| Washington, DC | 0 | 0.01 | 0 | 0 | 0 | 0.04 | 0.18 |
| Delaware | 0 | 0 | 0 | 0.19 | 0.06 | 0 | 0.01 |
| Georgia | 0 | 0 | 0 | 0.43 | 0 | 0 | 0 |
| Illinois | 0.30 | 0 | 0 | 0 | 0.10 | 0.35 | 0.30 |
| Massachusetts | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Maryland | 0 | 0 | 0.12 | 0 | 0 | 0.06 | 0.10 |
| Minnesota | 0.08 | 0 | 0 | 0.12 | 0 | 0 | 0.29 |
| North Carolina | 0 | 0 | 0.14 | 0 | 0 | 0 | 0 |
| New Jersey | 0 | 0.30 | 0.10 | 0 | 0 | 0 | 0.05 |
| New Mexico | 0.17 | 0 | 0 | 0.03 | 0 | 0 | 0.04 |
| New York | 0 | 0 | 0 | 0 | 0.40 | 0 | 0 |
| Pennsylvania | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Rhode Island | 0 | 0.05 | 0.05 | 0 | 0 | 0 | 0 |
| Utah | 0.23 | 0 | 0.55 | 0 | 0.22 | 0.07 | 0 |
| Vermont | 0 | 0.16 | 0.03 | 0.15 | 0.01 | 0.04 | 0 |
| Washington | 0 | 0.48 | 0 | 0 | 0 | 0.04 | 0 |
| Wisconsin | 0 | 0 | 0 | 0.07 | 0.07 | 0 | 0 |
Abbreviation: DC, District of Columbia.
a The synthetic control method selects a subset of donor states and creates a weighted average of those states to generate a counterfactual postpolicy trend for each state and population.
b “0” indicates a weight with an absolute value less than 0.0001.
c Weights sum to 1.
1. A GSL was in effect throughout the analytical period (2015–2019).
2. An NAL was in effect throughout the analytical period.
To model race/ethnicity-stratified mortality, we used the subset of donor states in which the above criteria were met and overdose mortality in the Black population was non-0 in at least 80% of evaluated months (n = 17 states). This disqualified New Mexico, Utah, and Vermont.
Covariates
In the SCM, using covariates may improve the match between the outcomes predicted by the synthetic control and the observed outcomes in the matching period. For each model, we tested whether inclusion of a set of 1) sociodemographic and/or 2) policy covariates improved fit beyond inclusion of matching period outcomes alone (Web Appendix). However, including covariates did not improve fit in any model, so they were not included. (Other studies have also encountered worsening fit with covariate inclusion (22) or have simply used the augmented SCM without considering inclusion of covariates (23, 24).)
Statistical analysis
Overview of the classic, inverted, and augmented SCMs.
Standard SCM.
The SCM is a popular method for estimating the effects of interventions that occurred in a small number of units. By generating a synthetic pre- and postintervention counterfactual, this method avoids the often-implausible parallel trends assumption required by the commonly used difference-in-differences approach. For a given intervention unit, the synthetic control—or estimated counterfactual—is a weighted average of the outcomes in untreated comparison, or “donor,” units. In standard SCM, the selected weights are positive weights that maximize preintervention fit of the synthetic control to the observed outcomes, i.e., that minimize the root mean squared prediction error of the synthetic control. Those weights are then applied to the postintervention period outcome data from the donor units to estimate the counterfactual outcome in the intervention unit(s), absent the intervention. For a given postintervention time point, the estimated “effect” is defined as the difference between the observed and estimated counterfactual outcomes (Figure 1A). This enables the estimation of time-varying effects, which is useful when an intervention’s effects may be lagged or attenuate over time.
Figure 1.
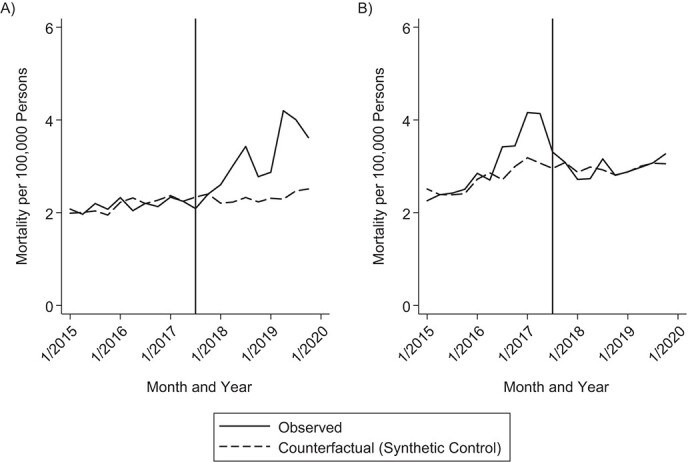
Illustrative examples of the standard and inverted forms of the synthetic control method (SCM). A) Standard SCM. In this example, we estimate the effect of hypothetical Good Samaritan laws (GSLs) on drug overdose mortality in the United States. States without a GSL in effect comprise the donor pool. The synthetic control is generated using data from the preintervention period (matching period); the postintervention period is used to estimate the effect of the intervention (evaluation period). B) Inverted SCM. Here, we use an inverted SCM to estimate the effect of Ohio’s GSL on overdose mortality. States with a GSL in effect comprise the donor pool. In contrast with the standard SCM, the synthetic control is generated using data from the post-intervention period, while the preintervention period—during which the donor states but not Ohio had a GSL—is used to estimate the effect of an absence of the intervention. In this example, we would expect observed overdose mortality to be greater than the counterfactual scenario in which Ohio had a GSL throughout 2015–2019.
The standard approach for evaluating whether an estimated effect was likely to have occurred by chance is to conduct a series of placebo tests in which each donor unit is successively treated as an intervention unit; the researcher evaluates the proportion of placebo trials in which the effect is at least as large as that for the intervention unit of interest (as the number of donor states increases, so too does the precision of this estimate). If the estimated effect of interest is larger than in most of the placebo trials, then that provides evidence that the difference is likely not due to chance.
The SCM requires that there be no spillover from intervention units to donor units, which would contaminate the donor units; that is, the intervention should not have an effect on untreated units. It also assumes an absence of confounding events in the postintervention period, such as an additional intervention that affects the outcome of interest. Donor units should be judged similar to the intervention units on characteristics relevant to the outcome, and should not experience idiosyncratic shocks to the outcome that do not affect the intervention units, as this could result in interpolation errors.
Inverted SCM.
We propose the inverted SCM, in which the donor pool comprises treated rather than untreated units. This may be useful when a near-ubiquitous intervention leaves few untreated units to include in a standard donor pool. To estimate the effect of the intervention, then, the time variable must be inverted so that the units of interest (i.e., those that receive the intervention during the analytical time period) appear to switch from having the intervention to not having the intervention. The counterfactual is then generated using the postperiod data, which we refer to as the “matching period,” during which both the intervention and donor units all have the intervention. The effect is estimated using data from what is actually the preintervention period (we call this the “evaluation period”), during which the donor units have the intervention but the intervention units of interest do not. Figure 1B helps to visualize this.
Augmented SCM with partially pooled estimates.
Because of the staggered timing of GSL enactment, estimation of an average treatment effect across intervention states required the use of an SCM approach appropriate for staggered adoption; we chose to use augmented, partially pooled SCM. Augmented SCM was developed as an extension of standard SCM; it can improve the fit of the synthetic control outcomes to the observed, matching period outcomes by relaxing the requirement that donor weights be nonnegative (25). To minimize extrapolation from the convex hull, augmented SCM uses a ridge regression with a regularization parameter that penalizes increasing departure from the nonnegative weights selected by standard SCM (25). Partially pooled SCM can account for staggered interventions through partial pooling of the intervention-unit–specific models. Partially pooled models minimize a weighted average of 2—rather than just 1—measures of imbalance, or fit: 1) the unit-specific imbalance (i.e., when each intervention unit is modeled separately) and 2) the imbalance for the average of the intervention units (i.e., when all units are pooled), where imbalance is estimated as the root mean squared prediction error in the matching period (26). The parameter  , bounded by 0 and 1, determines the weight given to the pooled imbalance. As with standard SCM for single interventions, augmented SCM with staggered interventions models the interventions with respect to calendar time to account for secular trends.
, bounded by 0 and 1, determines the weight given to the pooled imbalance. As with standard SCM for single interventions, augmented SCM with staggered interventions models the interventions with respect to calendar time to account for secular trends.
Implementation of inverted SCM with partially pooled models in the present study.
Given the near ubiquity of GSLs in the United States, too few untreated states were available to form a well-fitting control group using standard SCM. We therefore used inverted SCM, enabling estimation of the effect of a change from post-GSL (“matching period”) to pre-GSL (“evaluation period”) status in the intervention states, compared with the donor pool of states that did have a GSL throughout the analytical period. For each intervention state and group, we compared the observed mortality rate in the evaluation (pre-GSL) period with that predicted by the synthetic control; following the synthetic control literature, we refer to the difference between these as the estimated effect of not having a GSL (16, 27). Staggered adoption of GSLs across intervention states required use of partially pooled models (26). Following the approach of Ben-Michael et al. (26), we set  to equal the ratio of the pooled fit to the average state-level fit. All analyses were conducted using the multisynth function within the augsynth package in R (R Foundation for Statistical Computing, Vienna, Austria) (26).
to equal the ratio of the pooled fit to the average state-level fit. All analyses were conducted using the multisynth function within the augsynth package in R (R Foundation for Statistical Computing, Vienna, Austria) (26).
The effects of a GSL may be gradual—for instance, as law enforcement and laypeople grow familiar with its protections—and matching the synthetic control to observed data during this implementation period could result in biased estimates (12, 14). We therefore treated the intervention as beginning 12 months after the effective date. In addition, intervention state data were left-truncated at the NAL’s effective date, so that a NAL was in place throughout the analyzed months. This aimed to reduce confounding from a NAL coming into effect (left-truncating at 12 months after a NAL came into effect, to account for potential lagged effects of NALs, did not affect the substantive conclusions). This enabled us to include a 15-month matching period (post-GSL) and a 24-month evaluation period (pre-GSL) for each state. Web Table 1 presents the GSL and NAL effective dates for each state, lagged GSL dates, and the months analyzed in the main analysis.
Staggered implementation precludes standard placebo checks to assess the likelihood that estimated effects occurred by chance. Following the approach of Ben-Michael et al. (26), we used a range of alternative approaches to evaluate whether effect estimates could be due to chance. First, we generated 95% CIs via the wild bootstrap (26). Because these CIs may be conservative under some conditions (26), we also conducted a series of robustness checks. First, we successively set the parameter  to 0 (i.e., conducted separate SCM for each intervention state and took the average of the estimated effects) and to 1 (i.e., pooled all intervention states and estimated the average effect). Second, we altered the definition of the intervention dates in 2 ways: 1) assuming no lagged effects, i.e., the implementation date equals the GSL effective date; and 2) assuming a 2-year lag, i.e., the implementation date equals 2 years after the GSL effective date, following recent literature (14). Third, we evaluated whether removal of the state with the worst matching period fit affected the results (Missouri; Web Table 2). Finally, we removed South Carolina, the only intervention state whose GSL protects people from prosecution and charge but not arrest (8); prior evidence suggests that protection from arrest may be necessary for GSL effectiveness (14).
to 0 (i.e., conducted separate SCM for each intervention state and took the average of the estimated effects) and to 1 (i.e., pooled all intervention states and estimated the average effect). Second, we altered the definition of the intervention dates in 2 ways: 1) assuming no lagged effects, i.e., the implementation date equals the GSL effective date; and 2) assuming a 2-year lag, i.e., the implementation date equals 2 years after the GSL effective date, following recent literature (14). Third, we evaluated whether removal of the state with the worst matching period fit affected the results (Missouri; Web Table 2). Finally, we removed South Carolina, the only intervention state whose GSL protects people from prosecution and charge but not arrest (8); prior evidence suggests that protection from arrest may be necessary for GSL effectiveness (14).
RESULTS
Overall estimated effects of the GSL
Table 1 provides the weights applied to each donor state to form the synthetic controls. Figure 2 displays month-specific estimated effects of GSLs on overall overdose mortality in both the matching and evaluation periods. In the matching period, estimated effects closer to 0 correspond to a better-fitting synthetic control.
Figure 2.
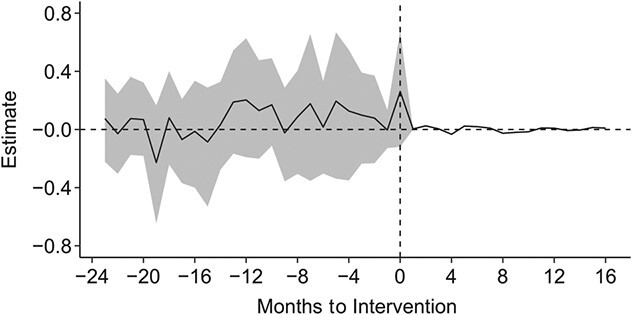
Estimated effects of Good Samaritan laws (GSLs) on overall (all races/ethnicities) drug overdose mortality in the United States, 2015–2019. The estimated effect was measured as the difference (observed minus counterfactual) in mortality per 100,000 population. The vertical dashed line indicates the intervention date, defined as 1 year after the GSL effective date. Months to the right of this line (postintervention) indicate the matching period, during which the synthetic control is generated; months to the left (preintervention) indicate the evaluation period, during which the observed and counterfactual estimates are compared. An estimated effect closer to 0 during the matching period indicates a better-fitting synthetic control. The intervention states were Ohio, Oregon, Michigan, Missouri, Nebraska, South Carolina, and South Dakota. The gray shading represents 95% confidence intervals.
If the GSL had the intended effect of reducing mortality, we would expect estimated effects of not having a GSL to be greater than 0. That is, observed mortality in the (pre-GSL) evaluation period would be higher than predicted mortality. While observed overdose mortality tended to be greater than predicted during the year of the evaluation period most proximal to the intervention, the 95% CIs consistently overlapped with 0—suggesting that these results were consistent with chance (Figure 2, Table 2). For the entire evaluation period, for example, the estimated average treatment effect in the treated (i.e., the estimated reduction in deaths if a GSL had been in effect throughout the analytical period) was 0.067 per 100,000 population (95% CI: −0.151, 0.283). Similarly, the effect estimates in each of the intervention states individually were small, with wide CIs spanning the null (Web Table 3).
Table 2.
Estimated Effects of Good Samaritan Laws on Drug Overdose Mortality, Overall (All Races/Ethnicities) and by Black/White Race/Ethnicity, United States, 2015–2019
| Race/Ethnicity | ||||||
|---|---|---|---|---|---|---|
| Overall (All Races/Ethnicities) a | Black | White | ||||
| Comparison(Pre-GSL)Month | Estimate b | 95% CI c | Estimate | 95% CI | Estimate | 95% CI |
| Average across months | 0.07 | −0.15, 0.28 | 0.09 | −0.29, 0.51 | 0.10 | −0.33, 0.49 |
| 0d | 0.26 | −0.13, 0.66 | 1.21 | −1.05, 3.52 | 0.22 | −0.29, 0.81 |
| 1 | 0.00 | −0.13, 0.14 | 0.24 | −0.33, 0.85 | −0.02 | −0.21, 0.18 |
| 2 | 0.08 | −0.21, 0.37 | 0.58 | −0.73, 2.22 | 0.39 | −0.39, 1.18 |
| 3 | 0.10 | −0.24, 0.41 | 0.45 | −0.41, 1.45 | 0.19 | −0.46, 0.87 |
| 4 | 0.13 | −0.32, 0.55 | 0.85 | −0.78, 2.67 | 0.40 | −0.45, 1.31 |
| 5 | 0.20 | −0.31, 0.67 | 0.51 | −0.78, 1.86 | 0.33 | −0.62, 1.27 |
| 6 | 0.02 | −0.28, 0.34 | −0.04 | −0.55, 0.54 | 0.19 | −0.47, 0.85 |
| 7 | 0.18 | −0.38, 0.63 | −0.54 | −1.94, 0.76 | 0.28 | −0.87, 1.25 |
| 8 | 0.09 | −0.30, 0.40 | 0.17 | −0.78, 1.19 | 0.20 | −0.47, 0.81 |
| 9 | −0.02 | −0.33, 0.26 | −0.07 | −1.00, 0.95 | −0.02 | −0.44, 0.35 |
| 10 | 0.17 | −0.10, 0.46 | −0.23 | −0.84, 0.40 | 0.16 | −0.34, 0.73 |
| 11 | 0.13 | −0.20, 0.47 | −0.08 | −0.79, 0.62 | 0.11 | −0.47, 0.71 |
| 12 | 0.20 | −0.20, 0.62 | 0.78 | −0.78, 2.53 | 0.12 | −0.48, 0.64 |
| 13 | 0.19 | −0.16, 0.60 | 0.13 | −0.51, 0.68 | 0.33 | −0.41, 1.12 |
| 14 | 0.03 | −0.28, 0.34 | −0.11 | −0.96, 0.80 | −0.09 | −0.74, 0.37 |
| 15 | −0.09 | −0.51, 0.27 | 0.04 | −1.12, 1.25 | −0.22 | −0.90, 0.43 |
| 16 | −0.01 | −0.41, 0.34 | −0.54 | −1.97, 1.02 | −0.08 | −0.47, 0.33 |
| 17 | −0.07 | −0.35, 0.20 | −0.13 | −0.92, 0.62 | −0.12 | −0.44, 0.17 |
| 18 | 0.08 | −0.26, 0.41 | −0.55 | −1.76, 0.57 | 0.23 | −0.33, 0.83 |
| 19 | −0.23 | −0.65, 0.16 | −0.35 | −1.32, 0.63 | −0.36 | −1.13, 0.41 |
| 20 | 0.07 | −0.19, 0.33 | −0.17 | −1.08, 0.61 | 0.08 | −0.27, 0.43 |
| 21 | 0.07 | −0.21, 0.35 | −0.30 | −1.33, 0.65 | −0.02 | −0.46, 0.36 |
| 22 | −0.03 | −0.31, 0.25 | 0.47 | −0.65, 1.71 | −0.11 | −0.61, 0.37 |
| 23 | 0.07 | −0.25, 0.38 | −0.31 | −1.19, 0.57 | 0.12 | −0.29, 0.53 |
Abbreviations: CI, confidence interval; GSL, Good Samaritan law.
a The overall results cannot be directly compared with the race/ethnicity-stratified results, as they were produced by a distinct set of intervention states, donor states, and weights.
b The estimated effect was measured as the difference (observed minus counterfactual) in mortality per 100,000 population (all races/ethnicities, Black, and White).
c 95% CIs were generated via the wild bootstrap.
d Comparison month 0 refers to 1 month prior to the intervention date, where the intervention date is defined as 1 year after the GSL effective date to allow for lagged effects.
Estimated effects of the GSL by Black/White race/ethnicity
As for the overall population, large CIs suggested that, for the Black and White populations separately, the overall and monthly estimated effects in the evaluation period were consistent with chance, although the point estimates for the evaluation period months most proximal to GSL enactment were in the expected direction (Figure 3, Web Table 4). For the entire evaluation period, the estimated average treatment effect in the treated was 0.085 per 100,000 (95% CI: −0.292, 0.514) in the Black population and 0.095 per 100,000 (95% CI: −0.332, 0.493) in the White population. While the point estimates during the 6 months of the evaluation period most proximal to the intervention were larger in the Black population than in the White population (consistent with larger GSL-associated reductions in mortality in the Black population), the CIs consistently overlapped.
Figure 3.
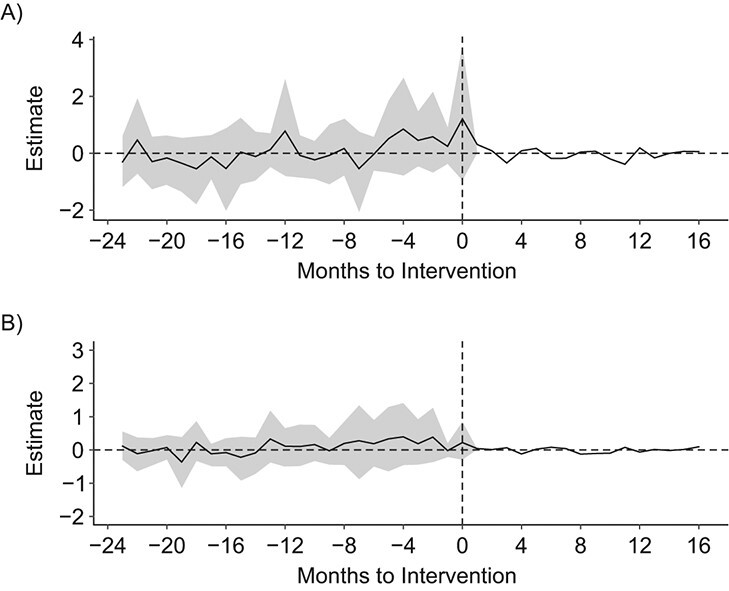
Estimated effects of Good Samaritan laws (GSLs) on drug overdose mortality according to Black/White race/ethnicity, United States, 2015–2019. The estimated effect was measured as the difference (observed minus counterfactual) in mortality per 100,000 population. A) Black overdose mortality; B) White overdose mortality. Vertical dashed lines indicate the intervention date, defined as 1 year after the GSL effective date. Months to the right of this line (postintervention) indicate the matching period, during which the synthetic control is generated; months to the left (preintervention) indicate the evaluation period, during which the observed and counterfactual estimates are compared. An estimated effect closer to 0 during the matching period indicates a better-fitting synthetic control. The intervention states were Ohio, Michigan, Missouri, and South Carolina. The gray shading represents 95% confidence intervals.
Robustness checks
For both overall and race/ethnicity-stratified overdose mortality, setting the weight given to the pooled imbalance (the parameter  ) to both 0 and 1, setting the lag period to both 0 and 2 years, and excluding the state with the worst matching period fit (Missouri) and the state that did not protect against arrest (South Carolina) did not change the substantive conclusions (Web Figures 2–4; results not shown for race/ethnicity-stratified models).
) to both 0 and 1, setting the lag period to both 0 and 2 years, and excluding the state with the worst matching period fit (Missouri) and the state that did not protect against arrest (South Carolina) did not change the substantive conclusions (Web Figures 2–4; results not shown for race/ethnicity-stratified models).
DISCUSSION
Amid a shifting landscape of overdose mortality and related policy, this study provides a rigorous, updated evaluation of one popular policy response, GSLs, paying particular attention to potential racial/ethnic disparities in the effects of these laws. We have proposed a novel implementation of traditional SCM, what we call the inverted SCM, to estimate the effect of recently enacted GSLs on drug overdose mortality, both overall and by Black/White race/ethnicity, in states that did not coenact an NAL. In this method, units in which the policy is in effect throughout the analytical period—rather than those in which it is absent—become comparison units. By inverting time, the synthetic control is generated for the postpolicy period rather than the prepolicy period, and the estimated effect is that of a change from having a policy to not having a policy. This approach may be useful in other research in which a policy of interest is nearly ubiquitous.
While we hypothesized that recent GSLs would be associated with lower overdose mortality overall and that the association would be larger in White people than in Black people, we estimated small effects with very wide CIs spanning the null—compatible with no effects in the overall population or in either subgroup. Some prior research has suggested that GSLs can increase 911 calling (10, 28) and reduce overdose mortality (12, 14), although the CIs in 2 of these studies were compatible with no effect at the conventional 95% level (12, 28). These findings, taken together with our and others’ (13) generally null findings, could reflect an overall lack of effect of GSLs or could indicate heterogeneity in effects by state, implementation timing, or other factors. State heterogeneity could result in part from wide variation in the protections provided by GSLs. For example, while in 2018 the GSL in 43 states provided protection from prosecution for drug possession, it only provided protection from both prosecution and arrest in 22 states (29). GSLs with broader protections could be more effective at encouraging 911 calling during overdose events (14), but nuances in the law may work to undermine even those. For instance, while the GSL in one state of interest, Ohio, provides protection from arrest and lesser sanctions for violating probation or parole, it requires that the benefiting individual present an addiction treatment referral within 30 days of the overdose event (29). Moreover, Ohio’s law includes a caveat that a person cannot benefit from the GSL more than twice (29). Given these barriers, it is perhaps not surprising that we did not find clear evidence of a meaningful effect in Ohio. Further research is needed to identify which individual or combinations of GSL provisions, if any, are associated with reduced overdose mortality.
Beyond the explicit protections provided by a GSL, other factors may present barriers to these laws’ effectiveness at reducing overdose mortality. First, familiarity with the GSL and its provisions is often lacking among people who use drugs, likely limiting their ability to take the protections into account when deciding whether to call 911 (30). Given that GSL protections are often contingent on the nature of the drug violation—e.g., the amount of a given substance possessed (29)—even individuals broadly familiar with the GSL may lack confidence that its protections apply to their situation, and in turn hesitate to call 911. Moreover, aversion to calling 911 may be challenging to overcome with legal protections alone. Qualitative research has shown that general distrust of police, expected stigmatization by first responders, and fear of losing housing or custody of children are among the reasons some overdose witnesses decide not to call 911—issues not addressed by GSLs (5–7).
This study had limitations. First, provision of theoretical support for a proposed inverted SCM remains an area for future work. Second, we estimated the relationship between GSLs and overdose mortality because that is the outcome GSLs ultimately aim to influence. However, by not looking at more proximate outcomes, such as emergency medical services activations, we were unable to discern the mechanisms underlying the potential absence of effects in the evaluated states. Similarly, while we conducted state-level analysis because GSLs are enacted at the state level, the analysis could be subject to ecological bias if GSL implementation varies by locality; local-level analyses are warranted to test whether local contextual factors lead to heterogenous effects. Fourth, to avoid confounding due to a frequently coenacted policy likely to influence mortality via a similar mechanism as GSLs (21), we selected intervention and donor states that had NALs throughout the analytical period. Some states updated their NALs during this period, creating the possibility of some residual confounding; these changes have not been fully documented, limiting our ability to account for them (31). Similarly, it was not feasible to apply the same approach for all drug-related policies implemented during the study period. As states continue to implement a range of supply-side, demand-side, and harm reduction policies to address the ongoing overdose crisis, this remains a persistent challenge for drug policy evaluation (32). Continued research to evaluate the individual and joint effects of drug-related policies, and to improve methodological approaches to account for multiple cooccurring policies, is needed.
Implementation and scale-up of evidence-based policy requires rigorous real-world evaluation, but myriad factors complicate efforts to establish that evidence base (32). We inverted the typical SCM to address one important challenge: an insufficient number of satisfactory unexposed comparison units—for instance, due to a ubiquitous policy—in evaluating GSLs enacted during the third wave of the ongoing overdose crisis. This method may be useful in other policy contexts in which unexposed comparison units are lacking.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Center for Opioid Epidemiology and Policy, Division of Epidemiology, Department of Population Health, Grossman School of Medicine, New York University, New York, New York, United States (Tarlise N. Townsend, Leah K. Hamilton, Ariadne Rivera-Aguirre, Corey S. Davis, John R. Pamplin II, Magdalena Cerdá); Behavioral Sciences Training in Drug Abuse Research Program, Rory Meyers College of Nursing, New York University, New York, New York, United States (Tarlise Townsend); Kaiser Permanente Washington Health Research Institute, Seattle, Washington, United States (Leah K. Hamilton); Network for Public Health Law, Edina, Minnesota, United States (Corey S. Davis); Center for Urban Science and Progress, New York University, New York, New York, United States (John R. Pamplin II); Department of Biostatistics and Data Sciences, Division of Public Health Sciences, Wake Forest School of Medicine, Winston-Salem, North Carolina, United States (David Kline); and Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, New York, United States (Kara E. Rudolph, John R. Pamplin II).
K.E.R. and M.C. are joint senior authors.
This work was supported by the National Institute on Drug Abuse (grant 5T32DA007233-37) and the New York University Center for Opioid Epidemiology and Policy.
We do not have permission to share the restricted-use mortality data used in this study. The data are available upon request on the website of the National Center for Health Statistics (https://www.cdc.gov/nchs/nvss/nvss-restricted-data.htm). Data from the American Community Survey, the Prescription Drug Abuse Policy System, and the Network for Public Health Law are publicly available.
We thank Lesly-Marie Buer, Donald Davis, Maya Doe-Simkins, and DeWayne Holman for their contributions to this study.
This work was presented at the 54th Annual Meeting of the Society for Epidemiologic Research (virtual), June 22–25, 2021.
Conflict of interest: none declared.
REFERENCES
- 1. Ahmad F, Rossen L, Sutton P. Provisional drug overdose death counts. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm#citation. Published 2021. Reviewed July 13, 2022. Accessed December 14, 2021.
- 2. Wilson N, Kariisa M, Seth P, et al. Drug and opioid-involved overdose deaths—United States, 2017–2018. MMWR Morb Mortal Wkly Rep. 2020;69(11):8–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kaiser Family Foundation . Opioid overdose deaths by race/ethnicity. (Opioid overdose death data for 1999–2019). https://www.kff.org/other/state-indicator/opioid-overdose-deaths-by-raceethnicity. Published 2022. Accessed May 2, 2022.
- 4. Drake J, Charles C, Bourgeois JW, et al. Exploring the impact of the opioid epidemic in Black and Hispanic communities in the United States. Drug Sci Policy Law. 2020;6:205032452094042. [Google Scholar]
- 5. Latimore AD, Bergstein RS. “Caught with a body” yet protected by law? Calling 911 for opioid overdose in the context of the Good Samaritan Law. Int J Drug Policy. 2017;50:82–89. [DOI] [PubMed] [Google Scholar]
- 6. Zadoretzky C, McKnight C, Bramson H, et al. The New York 911 Good Samaritan Law and opioid overdose prevention among people who inject drugs. World Med Health Policy. 2017;9(3):318–340. [Google Scholar]
- 7. Koester S, Mueller SR, Raville L, et al. Why are some people who have received overdose education and naloxone reticent to call emergency medical services in the event of overdose? Int J Drug Policy. 2017;48:115–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. The Network for Public Health Law . Legal Interventions to Reduce Overdose Mortality: Naloxone Access and Overdose Good Samaritan Laws. Edina, MN: The Network for Public Health Law; 2018. [Google Scholar]
- 9. Prescription Drug Abuse Policy System . Good Samaritan overdose prevention laws. https://pdaps.org/datasets/good-samaritan-overdose-laws-1501695153. Published June 1, 2021. Accessed November 15, 2021.
- 10. Jakubowski A, Kunins HV, Huxley-Reicher Z, et al. Knowledge of the 911 Good Samaritan Law and 911-calling behavior of overdose witnesses. Subst Abus. 2018;39(2):233–238. [DOI] [PubMed] [Google Scholar]
- 11. Watson DP, Ray B, Robison L, et al. Lay responder naloxone access and Good Samaritan law compliance: postcard survey results from 20 Indiana counties. Harm Reduct J. 2018;15(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McClellan C, Lambdin BH, Ali MM, et al. Opioid-overdose laws association with opioid use and overdose mortality. Addict Behav. 2018;86:90–95. [DOI] [PubMed] [Google Scholar]
- 13. Rees DI, Sabia JJ, Argys LM, et al. With a Little Help From My Friends: The Effects of Naloxone Access and Good Samaritan Laws on Opioid-Related Deaths. (NBER working paper 23171). Cambridge, MA: National Bureau of Economic Research; 2017. http://www.nber.org/papers/w23171.pdf. Accessed April 20, 2019. [Google Scholar]
- 14. Hamilton L, Davis CS, Kravitz-Wirtz N, et al. Good Samaritan laws and overdose mortality in the United States in the fentanyl era. Int J Drug Policy. 2021;97:103294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Alexander M. The New Jim Crow: Mass Incarceration in the Age of Colorblindness. 10th anniv. ed. New York, NY: The New Press; 2020. [Google Scholar]
- 16. Abadie A, Diamond A, Hainmueller J. Synthetic control methods for comparative case studies: estimating the effect of California’s tobacco control program. J Am Stat Assoc. 2010;105(490):493–505. [Google Scholar]
- 17. National Center for Health Statistics . Detailed Mortality—All County Files 2000–2018 as Compiled From Data Provided by the 57 Vital Statistics Jurisdictions Through the Vital Statistics Cooperative Program. Hyattsville, MD: National Center for Health Statistics; 2019. [Google Scholar]
- 18. Marquez-Velarde G, Jones NE, Keith VM. Racial stratification in self-rated health among Black Mexicans and White Mexicans. SSM Popul Health. 2020;10:100509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Borrell LN, Crawford ND. Race, ethnicity, and self-rated health status in the Behavioral Risk Factor Surveillance System Survey. Hisp J Behav Sci. 2006;28(3):387–403. [Google Scholar]
- 20. Logan JR. How Race Counts for Hispanic Americans. Albany, NY: Lewis Mumford Center for Comparative Urban and Regional Research, State University of New York at Albany; 2003. [Google Scholar]
- 21. Cataife G, Dong J, Davis CS. Regional and temporal effects of naloxone access laws on opioid overdose mortality. Subst Abus. 2020;42(3):329–338. [DOI] [PubMed] [Google Scholar]
- 22. Zimmerman SC, Matthay EC, Rudolph KE, et al. California’s Mental Health Services Act and mortality due to suicide, homicide, and acute effects of alcohol: a synthetic control application. Am J Epidemiol. 2021;190(10):2107–2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cole MA, Elliott RJR, Liu B. The impact of the Wuhan Covid-19 lockdown on air pollution and health: a machine learning and augmented synthetic control approach. Environ Resource Econ. 2020;76(4):553–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Opatrny M. The impact of the Brexit vote on UK financial markets: a synthetic control method approach. Empirica. 2021;48(2):559–587. [Google Scholar]
- 25. Ben-Michael E, Feller A, Rothstein J. The augmented synthetic control method. J Am Stat Assoc. 2021;116(536):1789–1803. [Google Scholar]
- 26. Ben-Michael E, Feller A, Rothstein J. Synthetic Controls With Staggered Adoption. (NBER working paper 28886). Cambridge, MA: National Bureau of Economic Research; 2021. http://www.nber.org/papers/w28886.pdf. Accessed July 9, 2021. [Google Scholar]
- 27. Galiani S, Quistorff B. The synth_runner package: utilities to automate synthetic control estimation using synth. Stata J. 2017;17(4):834–849. [Google Scholar]
- 28. Nguyen H, Parker BR. Assessing the effectiveness of New York’s 911 Good Samaritan law—evidence from a natural experiment. Int J Drug Policy. 2018;58:149–156. [DOI] [PubMed] [Google Scholar]
- 29. Beasley School of Law, Temple University . Prescription Drug Abuse Policy System (PDAPS). http://pdaps.org. Published 2020. Updated November 2021. Accessed January 15, 2020.
- 30. Moallef S, Hayashi K. The effectiveness of drug-related Good Samaritan laws: a review of the literature. Int J Drug Policy. 2020;90:102773. [DOI] [PubMed] [Google Scholar]
- 31. The Network for Public Health Law . Legal Interventions to Reduce Overdose Mortality: Naloxone Access Laws. Edina, MN: Network for Public Health Law; 2021. [Google Scholar]
- 32. Schuler MS, Griffin BA, Cerdá M, et al. Methodological challenges and proposed solutions for evaluating opioid policy effectiveness. Health Serv Outcomes Res Method. 2021;21(1):21–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


