Figure 1.
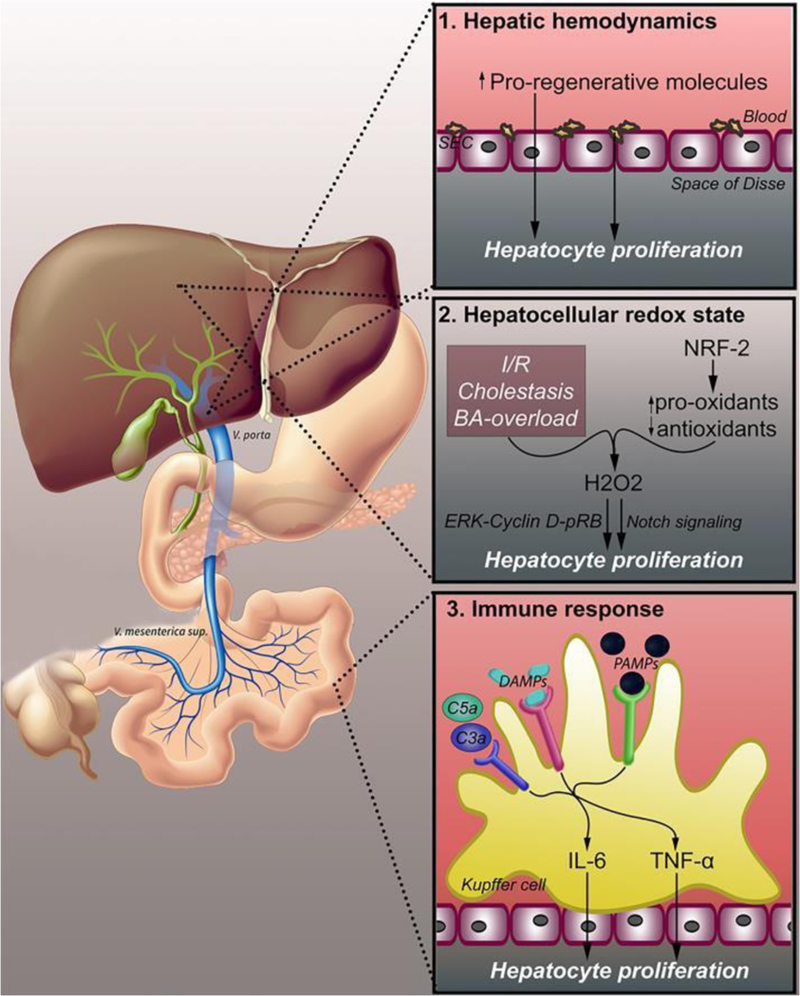
Changes in hepatic hemodynamics that lead to liver regeneration. Three physiological changes following PHx trigger liver regeneration. Altered hepatic hemodynamics (1) lead to increased hepatic exposure to pro-regenerative factors originating from the portal circulation. Additionally, platelets accumulate in the space of Disse and release pro- regenerative molecules. The hepatocellular redox state (2) shifts to a pro- oxidative state due to ischemia/reperfusion, cholestasis, and bile acid overload. NRF-2 and other redox-active enzymes upregulate pro-oxidant enzymes and downregulates antioxidant enzymes, leading to increased levels of H2O2, which promotes cell proliferation through both ERK-cyclin D1-p-RB and Notch signaling. PHx induces hepatocyte proliferation through an immune response (3), resulting from endotoxemia, intestine- derived PAMPs, and damaged cells leaking DAMPs. PAMPs and DAMPs bind PRRs on Kupffer cells, triggering the release of cytokines such as TNF-α and IL-6. Complement factors C3a and C5a are also triggered by the immune response and activate TNF-α and IL-6 release through complement receptors. Abbreviations: SEC, sinusoidal endothelial cell; BA, bile acid; NRF-2, nuclear factor (erythroid-derived 2)-like 2; H2O2, hydrogen peroxide; ERK, extracellular signal-regulated kinase; pRB, phosphorylated retinoblastoma protein; DAMPs, damage-associated molecular patterns; PRR, pattern recognition receptor; PAMPs, pathogen- associated molecular patterns; IL-6, interleukin 6; TNF-α, tumor necrosis factor alpha.
