Abstract
Background:
Breathing frequency (breaths/min) differs among individuals and levels of physical activity. Particles enter respirators through two principle penetration pathways: faceseal leakage and filter penetration. However, it is unknown how breathing frequency affects the overall performance of N95 filtering facepiece respirators (FFRs) and surgical masks (SMs) against viral particles, as well as other health-relevant submicrometer particles.
Methods:
A FFR and SM were tested on a breathing manikin at four mean inspiratory flows (MIFs) (15, 30, 55 and 85 L/min) and five breathing frequencies (10, 15, 20, 25 and 30 breaths/min). Filter penetration (Pfilter) and total inward leakage (TIL) were determined for the tested respiratory protection devices against sodium chloride (NaCl) aerosol particles in the size range of 20 to 500 nm. “Faceseal leakage-to-filter” (FLTF) penetration ratios were calculated.
Results:
Both MIF and breathing frequency showed significant effects (p<0.05) on Pfilter and TIL. Increasing breathing frequency increased TIL for the N95 FFR whereas no clear trends were observed for the SM. Increasing MIF increased Pfilter and decreased TIL resulting in decreasing FLTF ratio. Most of FLTF ratios were >1, suggesting that the faceseal leakage was the primary particle penetration pathway at various breathing frequencies.
Conclusions:
Breathing frequency is another factor (besides MIF) that can significantly affect the performance of N95 FFRs, with higher breathing frequencies increasing TIL. No consistent trend of increase or decrease of TIL with either MIF or breathing frequency was observed for the tested SM. To potentially extend these findings beyond the manikin/breathing system used, future studies are needed to fully understand the mechanism causing the breathing frequency effect on the performance of respiratory protection devices on human subjects.
Keywords: breathing frequency, N95, respirator, surgical mask, manikin
INTRODUCTION
The National Institute for Occupational Safety and Health (NIOSH) certified N95 filtering facepiece respirators (FFRs) are widely used in various occupational environments to reduce the workers’ exposure to hazardous aerosols. In healthcare environments, N95 FFRs and surgical masks (SMs) are the most commonly used devices to prevent transmission of infectious diseases.(1, 2) N95 FFRs are certified by NIOSH in accordance with Title 42 of the Code of Federal Regulations.(3) The letter ‘N’ stands for non-oil-resistance, and the number ‘95’ denotes the filter efficiency of at least 95% when the filter is challenged with NaCl aerosols having a mass median aerodynamic particle diameter of 300 nm (the most penetrating particle size, MPPS, for mechanical filters) at a constant flow of 85 L/min.(4) Presently, the vast majority of FFRs are manufactured utilizing electrostatic fibers, which feature much smaller MPPS: 30 to 100 nm.(5–12) The latter range includes many viral species. SMs are not subject to NIOSH filter certification approval; instead they are regulated by the US Food and Drug Administration (FDA). Previous studies have shown that the filter efficiency for SMs is much lower than that for N95 FFRs.(5, 13–15)
Besides filter penetration, faceseal leakage can have a significant impact on the performance of N95 FFRs and SMs. One study showed that the efficiency of N95 FFRs was high when sealed to a manikin headform but decreased significantly due to faceseal leakage when the same respirators were tested on human subjects.(16) NIOSH has proposed total inward leakage (TIL) testing to assess respirator performance since it takes into account both penetration pathways.(17) Grinshpun and colleagues quantified the relative contributions of the two pathways for an N95 FFR and a SM by determining the filter penetration (Pfilter) and faceseal leakage penetration (Pleakage) using manikin-based and human subject-based experimental protocols.(13) The “faceseal leakage-to-filter” ratio (FLTF = Pleakage/Pfilter) was > 1, indicating a greater number of particles penetrated through faceseal leaks than the filter media.(13) While the quoted study addressed a wide range of particle sizes (30 – 1000 nm), it did not examine breathing frequency.
Exposure to viral particles is best characterized by the number or volume of inhaled particles rather than mass concentration(18, 19) Viral airborne particles (known as virions) are generally much smaller than airborne bacteria. Most naked viruses referenced in the literature are between 20 and 300 nm in diameter.(20) For instance, coronavirus, the causative agent of severe acute respiratory syndrome (SARS), has a primary physical size ranging from 80 to 140 nm; the avian influenza virus (H5N1 and H1N1) is between 80 to 120 nm.(21, 22) The size range of aerosol particles containing viruses (often referred to as “carriers”) found in an occupational setting is substantially larger as they may consist of respiratory secretions, dead cells, mucous, etc., in addition to single viruses or virus aggregates.(23–25) However, particles < 500 nm are capable of penetrating deeper in the respiratory tract during inhalation; this range also includes particles featuring the highest penetration through most of respiratory protection devices and filters. In addition, the differences in filtration performance between surgical masks and FFRs are less noticeable for the particles of around 1 μm or larger.(5, 13, 14) Therefore, this study was focused on particle sizes of < 500 nm.
The Institute of Medicine estimates that during an influenza pandemic, more than 13 million healthcare workers, patients, family members and friends may need respiratory protection devices to protect them from receiving or spreading infectious illness.(26) Among population groups (e.g., young vs. old, small vs. large, healthy vs. sick), breathing frequency (breaths/min) differs and will differ significantly with level of physical activity (e.g., at rest vs. active).(27, 28) In addition, studies examined the physiological impact of respirators on healthcare workers, reported that wearing a FFR did not impose any important physiological burden during one hour of use, at realistic clinical work rates (16 – 27 breaths/min at low to moderate work rates); the use of a surgical mask over the same period at a low-to-moderate work rate was not associated with clinically significant physiological impact or significant subjective perceptions of exertion or heat.(29–31) Human breathing has a cyclic flow pattern, which is primarily determined by mean inspiratory flow (MIF, L/min) and breathing frequency (breaths/min). Unlike the constant flow regime with a fixed flow rate, the cyclic regime features a constantly changing flow that depends on the level of the breathing frequency. Various studies have addressed the effect of flow rate on filter efficiency and faceseal leakage.(32–35) However, with the exception of our recent study in which an elastomeric half-mask respirator was tested,(36) no published study has evaluated the effect of breathing frequency on the performance of N95 FFRs and SMs when both filter and faceseal leakage penetration pathways are present.
Although the nature of an inert aerosol (e.g., NaCl) differs from that of bioaerosols, several studies have confirmed that filter performance against biological particles is consistent with that determined using non-biological particles of the same size.(5, 7, 16) This suggests that inert aerosol surrogates such as NaCl particles may generally be appropriate for predicting penetration of similarly sized virions. The present manikin-based study addresses the effects of breathing frequency and flow rate on the filter efficiency and faceseal leakage of an N95 FFR and a SM challenged with NaCl particles (20 – 500 nm), which represent many viral species, as well as other health-relevant particles (e.g., combustion generated or engineered nanoparticles). The tested N95 FFR/SM was sealed to plastic manikin headform to investigate filter performance. It was also donned without sealing to a different advanced manikin headform to quantify TIL. The advanced manikin utilized in this study was recently developed to mimic the properties of the human face.(37, 38) Faceseal leakage represents the difference between TIL and filter penetration. The hypothesis of this study was that the Pfilter as well as the TIL of FFRs and SMs are generally affected by MIF and breathing frequency.
MATERIALS AND METHODS
Tested N95 FFR and Surgical Mask
One N95 FFR and one SM were chosen for the study. Both models are commercially available and widely used in healthcare environments. The model of the N95 FFR was identical to the one tested in our previous studies.(5, 6) It has three principle layers with the middle layer composed of electrically charged polypropylene fibers to enhance filter capture efficiency.(5) The selected SM, according to the manufacturer, is fluid resistant and capable of providing at least 95% filter efficiency for 100 nm particles (not charge-neutralized).
For filter efficiency testing, the FFR/SM was sealed to the face of a hard plastic manikin headform. For the TIL tests, it was donned on an advanced manikin headform according to the FFR/SM manufacturer’s user instruction. After 20 tests, the tested FFR/SM was removed from the manikin and replaced with a new one to minimize the effect of NaCl loading on the filter media.
Challenge Aerosol
To produce the challenge agent (NaCl), a liquid salt solution was aerosolized using a particle generator (Model: 8026, TSI Inc., Shoreview, MN) and charge-equilibrated by passing through a 85Kr electrical charge equilibrator (Model: 3054, TSI Inc., Shoreview, MN) prior to being released inside the test chamber. Before each experiment, the particle generator operated for at least one hour to achieve a uniform NaCl concentration in the chamber; it continued operating during the testing to maintain a stable particle concentration level. The challenge aerosol was log normally distributed with a size range of 20 – 500 nm, a count geometric mean of 125.4 nm, and a geometric standard deviation of 1.68 as measured with a Nanoparticle Spectrometer (Nano-ID NPS500, Naneum Ltd., Kent, UK). This size range covers the size of individual and aggregate virus particles. The NaCl concentration inside the challenge chamber ranged from 30,000 to 60,000 particles/cm3 (such high ambient level was chosen to assure that enough particles would be detected inside the respirator).
Experimental Design and Test Conditions
Experiments were carried out in a room-size (24.3 m3) test chamber described in recent studies.(36, 39) Temperature and relative humidity inside the chamber were kept at 17–22 °C and 30–60 %, respectively. The headform was connected to a Breathing Recording and Simulation System (BRSS, Koken Ltd., Tokyo, Japan) with a HEPA filter placed in-between to keep particles from re-entering the respirator cavity during exhalation cycles. Details regarding the BRSS are described in our previous studies.(34, 36, 39, 40)
The experiments were conducted at four cyclic breathing flows (MIF =15, 30, 55 and 85 L/min) and five breathing frequencies (10, 15, 20, 25 and 30 breaths/min). Completely randomized factorial design was implemented for the breathing frequency and flow rate with three replicates. Particle size-independent (overall) concentrations inside and outside the FFR/SM were obtained using a condensation particle counter (Model: 3007, TSI Inc., Shoreview, MN) having a total sampling time of 3 min with a time resolution of 1 sec.
Filter Penetration (Pfilter) Test
The filter penetration (Pfilter) was determined as the ratio of concentrations inside [Cin_(Sealed)] and outside [Cout_(Sealed)] of the FFR/SM sealed to the plastic headform:
| (1) |
Total Inward Leakage (TIL) Test
For TIL, the same experimental protocol and test conditions were used except the FFR/SM was not sealed onto the advanced manikin headform. TIL values were determined as the ratio of concentrations inside [Cin_(Donned)] and outside [Cout_(Donned)] of the FFR/SM:
| (2) |
Faceseal Leakage to Filter (FLTF) Ratio
The TIL test measures total penetration through the filter and faceseal leakage (TIL = Pfilter + Pleakage). The FLTF ratio represents the relative contribution for each and was calculated as:
| (3) |
In this study, the FLTF ratio was calculated using the average TIL and Pfilter values over three replicates in order to identify the primary penetration pathway (leakage or filter penetration) for the entire particle size range of interest.
Data analysis
SAS version 9.3 (SAS Institute Inc., Cary, NC, USA) was used for data analysis. Normality of the data was checked prior to performing any statistical analyses. Two-way Analysis of Variance (ANOVA) was performed to analyze the effect of breathing frequency and flow rate on the filter penetration and TIL. All pairwise comparisons were conducted using Tukey’s range test. P-values < 0.05 were considered significant.
RESULTS AND DISCUSSION
1. N95 Filtering Facepiece Respirator
N95 Filter Penetration (Pfilter)
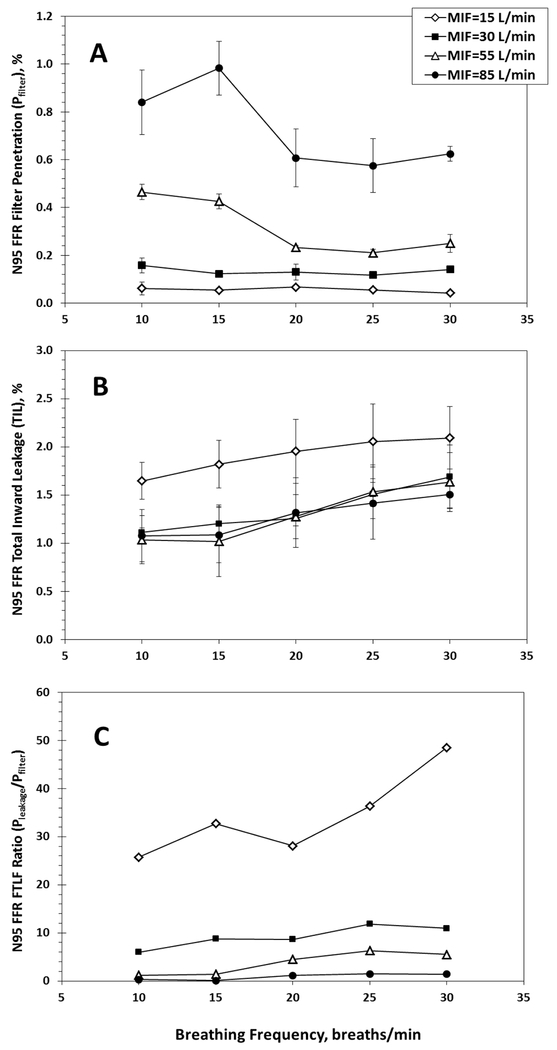
Filter penetration results for the N95 FFR are presented in Figure 1A. Filter penetration (Pfilter) consistently increased with increasing MIF. This result can be explained by the differences in linear air velocities. Penetration of very small particles, which deposit on filter fibers primarily due to diffusion, increases with a decreasing residence time (also known as removal time). Thus, small particles are more likely to penetrate the filter at higher breathing flows. At the higher flows (MIF = 55 and 85 L/min), the Pfilter curves are not flat, in contrast to those at the 15 and 30 L/min, suggesting that the effect of lower breathing frequencies are more pronounced at higher MIFs.
Fig 1.
Filter penetration (A), Total Inward Leakage (TIL) (B), and faceseal leakage-to-filter (FLTF) ratio (C) for an N95 FFR sealed to a plastic manikin’s face. Each data point in plot C represents the FLTF ratio calculated as the mean Pleakage (determined from 3 replicates) divided by the mean Pfilter (also determined from 3 replicates). Consequently, no error bars are presented in plot C.
Two-way ANOVA performed on the Pfilter data revealed that both the MIF and breathing frequency had a significant effect on filter penetration (p <0.0001, see Table I). Pairwise multiple comparison results (see Table I) show that the four MIFs produced four different Pfilter groups with the highest mean Pfilter (0.72%, Tukey grouping “A”) occurring at the highest MIF of 85 L/min, and the lowest mean Pfilter (0.05%, Tukey grouping “D”) occurring at the lowest MIF of 15 L/min. The breathing frequency comparisons show that 10 and 15 breaths/min produced higher values of Pfilter (0.39% and 0.38%, Tukey grouping “I”) than those observed at 20, 25 and 30 breaths/min (0.25%, 0.23% and 0.26%, respectively, Tukey grouping “II”).
TABLE I.
Pairwise multiple comparisons for mean Pfilter values among four MIFs and five breathing frequency groups (ANOVA with Tukey’s range test) for an N95 FFR
| Effect of MIF on Pfilter |
Effect of Breathing Frequency on Pfilter |
||||||
|---|---|---|---|---|---|---|---|
| MIF (L/min) | Tukey Groupinga | Meanb Pfilter (%) | p-valuec | Breathing Frequency (breaths/min) | Tukey Groupinga | Meanb Pfilter (%) | p-valued |
| 15 | D | 0.05 | <0.0001 | 10 | 0.38 | I | <0.0001 |
| 30 | C | 0.13 | 15 | 0.39 | I | ||
| 55 | B | 0.31 | 20 | 0.25 | II | ||
| 85 | A | 0.72 | 25 | 0.23 | II | ||
| 30 | 0.26 | II | |||||
Within each group of the MIF or the breathing frequency, means with the same letter are not significantly different (p-value > 0.05).
Calculated using the size-independent (overall) Pfilter values.
P-values were obtained from the two-way ANOVA performed to examine the effect of the MIF on the filter penetration.
P-values were obtained from the two-way ANOVA performed to examine the effect of the breathing frequency on the filter penetration.
N95 Total Inward Leakage (TIL)
Figure 1B presents the results obtained from the TIL measurements for the tested N95 FFR. It is seen that the MIF of 15 L/min produced the highest TILs. Interestingly, the TIL increased with increasing the breathing frequency, especially at MIF = 15 L/min. The exhaled particle-free air dilutes the aerosol in the respirator cavity. At a higher breathing frequency (given the same MIF), the dilution air volume per breathing cycle is lower, which results in a less efficient dilution and consequently increases the aerosol concentration inside the respirator. This explains why a higher breathing frequency produced a higher TIL.
Statistical analysis revealed significant effects of MIF (p =0.0019) and breathing frequency (p =0.0025) on TIL (see Table II). The pairwise multiple comparison results presented in Table II show that the lowest MIF (15 L/min) was associated with the highest mean TIL (1.93%, Tukey grouping “A”). The mean TIL values among the three higher MIFs (30, 55 and 85 L/min) were not significantly different from each other (1.37%, 1.31% and 1.29%, Tukey grouping “B”). The highest breathing frequency (30 breaths/min) produced the highest mean TIL (1.73%, Tukey grouping “I”) compared to the lowest mean TIL (1.22%, Tukey grouping “II”) with the lowest breathing frequency (10 breaths/min). The highest and lowest breathing frequencies were significantly different (Tukey groups I & II). As was pointed out in our previous study on elastomeric respirators,(36) higher MIF may create a higher sucking force that made a tighter contact between the respirator and the soft skin of the headform, possibly reducing the leak size. We anticipate that the quoted effect showed up when MIF increased to 30 L/min. The finding is consistent with previous FFR performance studies conducted using hard manikins and challenge aerosol particles above 500 nm.(32, 41, 42)
TABLE II.
Pairwise multiple comparisons for mean TIL values among four MIFs and five breathing frequency groups (ANOVA with Tukey’s range test) for an N95 FFR
| Effect of MIF on TIL |
Effect of Breathing Frequency TIL |
||||||
|---|---|---|---|---|---|---|---|
| MIF (L/min) | Tukey Groupinga | Meanb TIL (%) | p-valuec | Breathing Frequency (breaths/min) | Tukey Groupinga | Meanb TIL (%) | p-valued |
| 15 | A | 1.93 | 0.0019 | 10 | II | 1.22 | 0.0025 |
| 30 | B | 1.37 | 15 | II | 1.28 | ||
| 55 | B | 1.31 | 20 | I II | 1.45 | ||
| 85 | B | 1.29 | 25 | I II | 1.63 | ||
| 30 | I | 1.73 | |||||
Within each group of the MIF or the breathing frequency, means with the same letter are not significantly different (p-value > 0.05).
Calculated using the size-independent (overall) TIL values.
P-values were obtained from the two-way ANOVA performed to examine the effect of the MIF on the TIL.
P-values were obtained from the two-way ANOVA performed to examine the effect of the breathing frequency on the TIL.
N95 Faceseal Leakage-to-Filter (FLTF) Ratio
The size-independent (overall) FLTF ratios calculated by Eq. (3) are presented in Figure 1C as a function of the breathing frequency and MIF. Except for MIF = 85 L/min, all the FLTF ratios were > 1, which suggests that overall particle penetration through faceseal leaks exceeded N95 filter penetration at lower breathing rates. Remarkably, at the lowest MIF (15 L/min) the FLTF ratios ranged from 25 to 47, suggesting that the absolute majority of the measured virus-size aerosol particles penetrated through faceseal leaks. At MIF =15 L/min, increase in breathing frequency was generally associated with increase in FLTF ratio. However, the breathing frequency effect was not clearly seen for the three higher MIFs (30, 55 and 85 L/min).
It is seen that increasing MIF resulted in decreasing FLTF ratio. This finding agrees with two other N95 FFR studies.(13, 43) Grinshpun et al tested an N95 FFR using 25 human subjects, and reported that “deep breathing” produced higher FLTF ratios compared to “normal breathing”.(13) Rengasamy and Eimer also reported higher FLTF ratios occurred at higher flow rates when testing the N95 FFRs with artificially created leaks.(43) In both quoted studies, all the FLTF ratios exceeded the unity, indicating that the faceseal leakage was the primary penetration pathway for N95 FFRs.
2. Surgical Mask
SM Filter Penetration (Pfilter)
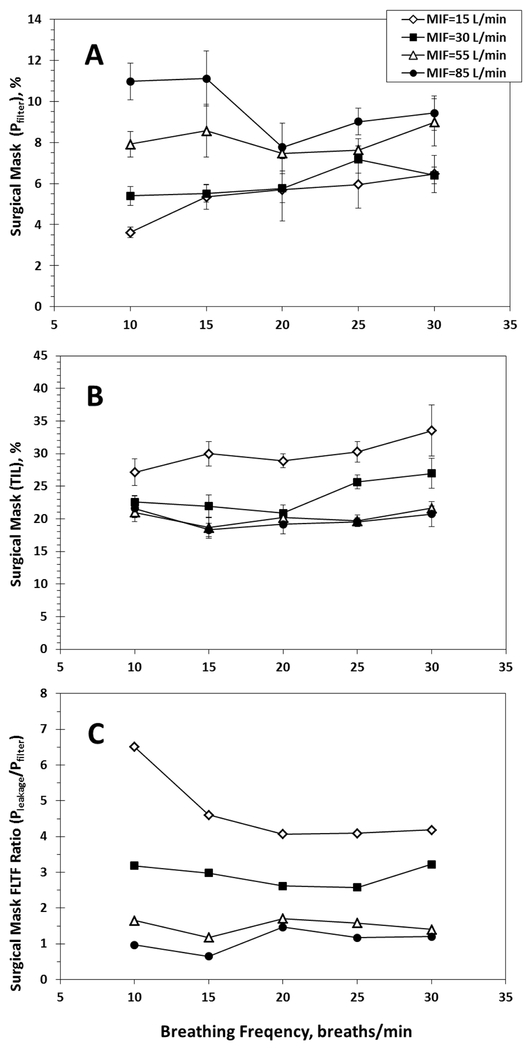
The data on filter penetrations (Pfilter) for the tested SM are shown in Figure 2A. Compared to the N95 FFR, the SM had a much higher filter penetration. This is not surprising given the less stringent filter penetration test requirements for SMs. In fact, previous studies have reported SMs providing much lower levels of respiratory protection than N95 FFRs when challenged with biological or non-biological particles.(5, 13–15) Increasing MIF frequently resulted in an increase in filter penetration, especially at the lowest breathing frequency. Statistical analysis suggests that the effects of MIF and breathing frequency on the Pfilter were both significant (p <0.05; see Table III). The pairwise multiple comparisons (see Table III) show the highest MIF (85 L/min) produced the highest mean Pfilter (9.65%, Tukey grouping “A”), whereas the lowest Pfilter (5.41%, Tukey grouping “C”) occurred at the lowest MIF (15 L/min). Table III also shows that the mean Pfilter = 7.81% (Tukey grouping “I”) obtained at 30 breaths/min was significantly higher (p <0.05) than Pfilter = 6.67% (Tukey grouping “II”) obtained at 20 breaths/min. However, no consistent trend was identified throughout the frequency scale.
Fig 2.
Filter penetration (A), Total Inward Leakage TIL (B), and faceseal leakage-to-filter (FLTF) ratio (C) for a surgical mask sealed to a plastic manikin’s face. Each data point in plot C represents the FLTF ratio calculated as the mean Pleakage (determined from 3 replicates) divided by the mean Pfilter (also determined from 3 replicates). Consequently, no error bars are presented in plot C.
TABLE III.
Pairwise multiple comparisons for mean Pfilter values among four MIFs and five breathing frequency groups (ANOVA with Tukey’s range test) for a surgical mask
| Effect of MIF on Pfilter |
Effect of Breathing Frequency on Pfilter |
||||||
|---|---|---|---|---|---|---|---|
| MIF (L/min) | Tukey Groupinga | Meanb Pfilter (%) | p-valuec | Breathing Frequency (breaths/min) | Tukey Groupinga | Meanb Pfilter (%) | p-valued |
| 15 | C | 5.41 | <0.0001 | 10 | I II | 6.97 | <0.0143 |
| 30 | C | 6.04 | 15 | I II | 7.63 | ||
| 55 | B | 8.11 | 20 | II | 6.67 | ||
| 85 | A | 9.65 | 25 | I II | 7.43 | ||
| 30 | I | 7.81 | |||||
Within each group of the MIF or the breathing frequency, means with the same letter are not significantly different (p-value > 0.05).
Calculated using the size-independent (overall) Pfilter values.
P-values were obtained from the two-way ANOVA performed to examine the effect of the MIF on the filter penetration.
P-values were obtained from the two-way ANOVA performed to examine the effect of the breathing frequency on the filter penetration.
SM Total Inward Leakage (TIL)
TIL results for the SM are presented in Figure 2B. The average TIL values ranged from 17% to 35% compared to filter penetrations of 3 – 12%, suggesting that faceseal leakage had a greater effect on the mask performance. Increasing MIF caused the mean TIL to decrease (see Table IV), which is in agreement with the finding reported for the N95.
TABLE IV.
Pairwise multiple comparisons for mean TIL values among four MIFs and five breathing frequency groups (ANOVA with Tukey’s range test) for a surgical mask
| Effect of MIF on TIL |
Effect of Breathing Frequency TIL |
||||||
|---|---|---|---|---|---|---|---|
| MIF (L/min) | Tukey Groupinga | Meanb TIL (%) | p-valuec | Breathing Frequency (breaths/min) | Tukey Groupinga | Meanb TIL (%) | p-valued |
| 15 | A | 1.93 | 0.0019 | 10 | I II | 23.1 | 0.0316 |
| 30 | B | 1.37 | 15 | II | 22.2 | ||
| 55 | B | 1.31 | 20 | I II | 22.3 | ||
| 85 | B | 1.29 | 25 | I II | 23.8 | ||
| 30 | I | 25.7 | |||||
Within each group of the MIF or the breathing frequency, means with the same letter are not significantly different (p-value > 0.05).
Calculated using the size-independent (overall) TIL values.
P-values were obtained from the two-way ANOVA performed to examine the effect of the MIF on the TIL.
P-values were obtained from the two-way ANOVA performed to examine the effect of the breathing frequency on the TIL.
While ANOVA revealed that both MIF and breathing frequency had a significant effect on the TIL (p <0.05; see Table IV), no consistent trend of increase or decrease of TIL with breathing frequency was observed. For instance, increasing the breathing frequency from 10 to 15 breaths/min was associated with a decrease in TIL, whereas changing the frequency from 10 to 30 breaths/min at MIF = 55 or 85 L/min resulted in essentially no change in TIL. When comparing the mean TIL values among the five breathing frequencies, the highest mean TIL (25.7%, Tukey grouping “I”) occurred at 30 breaths/min, and the lowest mean TIL (22.2%, Tukey grouping “II”) at 15 breaths/min.
At the same time, the data produced by a pairwise comparison presented in Table IV demonstrate that increasing MIF indeed decreased the TIL with MIF = 15 L/min generating the highest mean TIL (30%, Tukey grouping “A”) and 85 L/min producing the lowest mean TIL (19.9%, Tukey grouping “C”).
SM Faceseal Leakage-To-Filter (FLTF) Ratio
The FLTF ratios calculated from the overall Pfilter and the TIL data are presented in Figure 2C. It is seen that increasing MIF from 15 to 55 L/min resulted in a decrease in FLTF, with most of the FLTF ratios were > 1 (which means Pleakage > Pfilter). Increasing MIF from 55 to 85 L/min had less effect, with FLTF ratios < 2 and even < 1 at the highest MIF (85 L/min) for the two lowest frequencies of 10 and 15 breaths/min. The results had a similar pattern to those presented for the N95 FFR. However, the FLTF ratios for the SM were lower. For example, at MIF =15 L/min, the FLTF ratios for the SM were between 4 and 7 while those found for the N95 FFR ranged from 24 to 50. This difference is attributed to much higher filter penetration of the SM as compared to the N95 FFR.(13)
No clear trend was identified between the breathing frequency and the FLTF ratio for the three highest flows (MIF = 30, 55 and 85 L/min), where the curves are relatively flat (Figure 2C). For the lowest flow rate (15 L/min), increasing breathing frequency initially decreased FLTF, but this too leveled off.
CONCLUSIONS
Breathing frequency was found to be another factor (in addition to MIF) that can significantly affect the performance of N95 FFRs and SMs. However, the filter mechanism causing Pfilter to change as a function of breathing frequency is complex and not fully understood at this time. For the tested N95 FFR, the increase of breathing frequency caused an increase in TIL. No consistent trend of increase or decrease of TIL with either MIF or breathing frequency was observed for the tested SM. To potentially extend these findings beyond the manikin/breathing system used, future studies are needed to fully understand the mechanism causing the breathing frequency effect on the performance of FFRs and SMs on human subjects. The FLTF ratios obtained for the N95 FFR were generally higher than those for the SM for all tested breathing frequencies and MIFs. It is primarily because of the higher efficiency of the N95 filter. Increasing MIF was also generally associated with decreasing FLTF ratio for the tested FFR/SM. Except for MIF = 85 L/min, all the calculated FLTF ratios were > 1, suggesting that the faceseal leakage was the primary particle penetration pathway for the tested FFR/SM at various breathing frequencies.
ACKNOWLEDGEMENT
This research was supported by the NIOSH Targeted Research Training Program and Pilot Research Project Training Program (University of Cincinnati, Education and Research Center, Grant 5T42/OH008432). The BRSS was made available thanks to courtesy of Koken Ltd. (Tokyo, Japan); the advanced manikin headform was provided by Mr. Michael S. Bergman, and Dr. Ziqing Zhuang of NIOSH.
Footnotes
Publisher's Disclaimer: Disclaimer: This is a version of an unedited manuscript that has been accepted for publication. As a service to authors and researchers we are providing this version of the accepted manuscript (AM). Copyediting, typesetting, and review of the resulting proof will be undertaken on this manuscript before final publication of the Version of Record (VoR). During production and pre-press, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal relate to this version also.
REFERENCES
- 1.OSHA: Occupational Safety & Health Administration. Pandemic Influenza Preparedness and Response Guidance for Healthcare Workers and Healthcare Employers(2007). [Google Scholar]
- 2.Noti JD, Lindsley WG, Blachere FM, Cao G, Kashon ML, Thewlis RE et al. : Detection of Infectious Influenza Virus in Cough Aerosols Generated in a Simulated Patient Examination Room. Clin. Infect. Dis 54(11): 1569–1577 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CFR: Code of Federal Regulations Title 42, Part 84. “Respirator Protection”(1995. pp.30382–30383).
- 4.NIOSH: National Institute for Occupational Safety and Health. US DHHS, Public Health Service. “Respiratory Protective Devices; Final Rules and Notices” Federal Register 60:110, pp. 30335–30393. (1995). [Google Scholar]
- 5.Ba³azy A, Toivola M, Adhikari A, Sivasubramani SK, Reponen T, and Grinshpun SA: Do N95 Respirators Provide 95% Protection Level against Airborne Viruses, and How Adequate Are Surgical Masks? Am. J. Infect. Control 34(2): 51–57 (2006). [DOI] [PubMed] [Google Scholar]
- 6.Ba³azy A, Toivola M, Reponen T, Podgorski A, Zimmer A, and Grinshpun SA: Manikin-Based Performance Evaluation of N95 Filtering-Facepiece Respirators Challenged with Nanoparticles. Ann. Occup. Hyg 50(3): 259–269 (2006). [DOI] [PubMed] [Google Scholar]
- 7.Eninger RM, Honda T, Adhikari A, Heinonen-Tanski H, Reponen T, and Grinshpun SA: Filter Performance of N99 and N95 Facepiece Respirators against Viruses and Ultrafine Particles. Ann. Occup. Hyg 52(5): 385–396 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grafe T, Gogins M, Barris M, Schaefer J, and Canepa R: “Nanofibers in Filtration Applications in Transportation”. Filtration 2001 Conference Proceedings, Chicago, IL; 1–15 (2001). [Google Scholar]
- 9.Martin SB, and Moyer ES: Electrostatic Respirator Filter Media: Filter Efficiency and Most Penetrating Particle Size Effects. Appl. Occup. Environ. Hyg 15(8): 609–617 (2000). [DOI] [PubMed] [Google Scholar]
- 10.Rengasamy S, King WP, Eimer BC, and Shaffer RE: Filtration Performance of Niosh-Approved N95 and P100 Filtering Facepiece Respirators against 4 to 30 Nanometer-Size Nanoparticles. J. Occup. Environ. Hyg 5(9): 556–564 (2008). [DOI] [PubMed] [Google Scholar]
- 11.Cho KJ, Jones S, Jones G, McKay R, Grinshpun SA, Dwivedi A et al. : Effect of Particle Size on Respiratory Protection Provided by Two Types of N95 Respirators Used in Agricultural Settings. J. Occup. Environ. Hyg 7(11): 622–627 (2010). [DOI] [PubMed] [Google Scholar]
- 12.Zuo Z, Kuehn TH, and Pui DYH: Performance Evaluation of Filtering Facepiece Respirators Using Virus Aerosols. Am. J. Infect. Control 41(1): 80–82 (2013). [DOI] [PubMed] [Google Scholar]
- 13.Grinshpun SA, Haruta H, Eninger RM, Reponen T, McKay RT, and Lee SA: Performance of an N95 Filtering Facepiece Particulate Respirator and a Surgical Mask During Human Breathing: Two Pathways for Particle Penetration. J. Occup. Environ. Hyg 6(10): 593–603 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee SA, Grinshpun SA, and Reponen T: Respiratory Performance Offered by N95 Respirators and Surgical Masks: Human Subject Evaluation with Nacl Aerosol Representing Bacterial and Viral Particle Size Range. Ann Occup Hyg 52(3): 177–185 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Willeke K, Qian Y, Donnelly J, Grinshpun S, and Ulevicius V: Penetration of Airborne Microorganisms through a Surgical Mask and a Dust/Mist Respirator. Am. Ind. Hyg. Assoc. J 57(4): 348–355 (1996). [DOI] [PubMed] [Google Scholar]
- 16.Qian Y, Willeke K, Grinshpun SA, Donnelly J, and Coffey CC: Performance of N95 Respirators: Filtration Efficiency for Airborne Microbial and Inert Particles. Am. Ind. Hyg. Assoc. J 59(2): 128–132 (1998). [DOI] [PubMed] [Google Scholar]
- 17.NIOSH/CDC: National Institute for Occupational Safety and Health. US DHHS, Public Health Service. “Total Inward Leakage for Half-Mask Air-Purifying Respirators”(2009). [Google Scholar]
- 18.Kulkarni P, Baron PA, and Willeke K: Aerosol Measurement - Principles, Techniques, and Applications, 3rd Edition John Wiley & Sons, New Jersey: (2011). [Google Scholar]
- 19.Zuo Z, Kuehn TH, Verma H, Kumar S, Goyal SM, Appert J et al. : Association of Airborne Virus Infectivity and Survivability with Its Carrier Particle Size. Aerosol Science and Technology 47(4): 373–382 (2012). [Google Scholar]
- 20.Collier L, Balows A, and Sussman M: Topley and Wilson’s Microbiology and Microbial Infections, Volume 1, Virology: Hodder Arnold Publishers, 1998. [Google Scholar]
- 21.Ksiazek TG, Erdman D, Goldsmith CS, Zaki SR, Peret T, Emery S et al. : A Novel Coronavirus Associated with Severe Acute Respiratory Syndrome. N. Engl. J. Med 348(20): 1953–1966 (2003). [DOI] [PubMed] [Google Scholar]
- 22.Mandell GL, Bennett JE, and Dolin RD: Principles and Practice of Infectious Diseases. New York: Churchill Livingstone, 1995. [Google Scholar]
- 23.Lindsley WG, Blachere FM, Davis KA, Pearce TA, Fisher MA, Khakoo R et al. : Distribution of Airborne Influenza Virus and Respiratory Syncytial Virus in an Urgent Care Medical Clinic. Clin. Infect. Dis 50(5): 693–698 (2010). [DOI] [PubMed] [Google Scholar]
- 24.Lindsley WG, Pearce TA, Hudnall JB, Davis KA, Davis SM, Fisher MA et al. : Quantity and Size Distribution of Cough-Generated Aerosol Particles Produced by Influenza Patients During and after Illness. J. Occup. Environ. Hyg 9(7): 443–449 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang W, Elankumaran S, and Marr LC: Concentrations and Size Distributions of Airborne Influenza a Viruses Measured Indoors at a Health Centre, a Day-Care Centre and on Aeroplanes. J Royal Soc Interface 8(61): 1176–1184 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.IOM: Institute of Medicine. Preparing for an Influenza Pandemic: Personal Protective Equipment for Healthcare Workers(2008). [Google Scholar]
- 27.Sherwood L: Fundamentals of Physiology: A Human Perspective. Thomson Brooks/Cole, p.380 (2006). [Google Scholar]
- 28.Tortora GJ, and Anagnostakos NP: Principles of Anatomy and Physiology, 6th Edition, New York: Harper-Collins; P.707 (1990). [Google Scholar]
- 29.Roberge RJ, Coca A, Williams WJ, Powell JB, and Palmiero AJ: Physiological Impact of the N95 Filtering Facepiece Respirator on Healthcare Workers. Respir. Care 55(5): 569–577 (2010). [PubMed] [Google Scholar]
- 30.Kim J-H, Benson SM, and Roberge RJ: Pulmonary and Heart Rate Responses to Wearing N95 Filtering Facepiece Respirators. Am. J. Infect. Control 41(1): 24–27 (2013). [DOI] [PubMed] [Google Scholar]
- 31.Roberge RJ, Kim J-H, and Benson SM: Absence of Consequential Changes in Physiological, Thermal and Subjective Responses from Wearing a Surgical Mask. Respir Physiol Neurobiol 181(1): 29–35 (2012). [DOI] [PubMed] [Google Scholar]
- 32.Cho KJ, Reponen T, McKay R, Shukla R, Haruta H, Sekar P et al. : Large Particle Penetration through N95 Respirator Filters and Facepiece Leaks with Cyclic Flow. Ann. Occup. Hyg 54(1): 68–77 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eshbaugh JP, Gardner PD, Richardson AW, and Hofacre KC: N95 and P100 Respirator Filter Efficiency under High Constant and Cyclic Flow. J. Occup. Environ. Hyg 6(1): 52–61 (2008). [DOI] [PubMed] [Google Scholar]
- 34.Haruta H, Honda T, Eninger RM, Reponen T, McKay R, and Grinshpun SA: Experimental and Theoretical Investigation of the Performance of N95 Respirator Filters against Ultrafine Aerosol Particles Tested at Constant and Cyclic Flows. J. Int. Soc. Resp. Prot 25: 75–88 (2008). [Google Scholar]
- 35.Myers WR, Kim H, and Kadrichu N: Effect of Particle Size on Assessment of Faceseal Leakage. J. Int. Soc. Resp. Prot (9): 6–21 (1991). [Google Scholar]
- 36.He X, Grinshpun SA, Reponen T, McKay R, Bergman SM, and Zhuang Z: Effect of Breathing Frequency on the Total Inward Leakage of an Elastomeric Half-Mask Donned on an Advanced Manikin Headform. (in Press). Ann. Occup. Hyg (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bergman MS, Zhuang Z, Wander J, Hanson D, Heimbuch BK, McDonald M et al. : Development of an Advanced Respirator Fit Test Headform. (in Press). J. Occup. Environ. Hyg (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hanson D, Bergs R, Tadesse Y, White V, and Priya S: Enhancement of Eap Actuated Facial Expressions by Designed Chamber Geometry in Elastomers. Proc. Spie’s Electroactive Polymer Actuators and Devices Conf., 10th Smart Structures and Materials Symposium, San Diego (2006). [Google Scholar]
- 39.He X, Grinshpun SA, Reponen T, Yermakov M, McKay R, Haruta H et al. : Laboratory Evaluation of the Particle Size Effect on the Performance of an Elastomeric Half-Mask Respirator against Ultrafine Combustion Particles. (in Press). Ann. Occup. Hyg (2013). [DOI] [PubMed] [Google Scholar]
- 40.He X, Yermakov M, Reponen T, McKay R, James K, and Grinshpun SA: Manikin-Based Performance Evaluation of Elastomeric Respirators against Combustion Particles. J. Environ. Occup. Hyg 10: 203–212 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen CC, Ruuskanen J, Pilacinski W, and Willeke K: Filter and Leak Penetration Characteristics of a Dust and Mist Filtering Facepiece. Am. Ind. Hyg. Assoc. J 51(12): 632–639 (1990). [DOI] [PubMed] [Google Scholar]
- 42.Huang S-H, Chen C-W, Chang C-P, Lai C-Y, and Chen C-C: Penetration of 4.5 nm to Aerosol Particles through Fibrous Filters. J. Aerosol. Sci 38(7): 719–727 (2007). [Google Scholar]
- 43.Rengasamy S, and Eimer BC: Total Inward Leakage of Nanoparticles through Filtering Facepiece Respirators. Ann. Occup. Hyg 55(3): 253–263 (2011). [DOI] [PubMed] [Google Scholar]