Figure 1. Anaplastic myxopapillary ependymomas with aggressive clinical features.
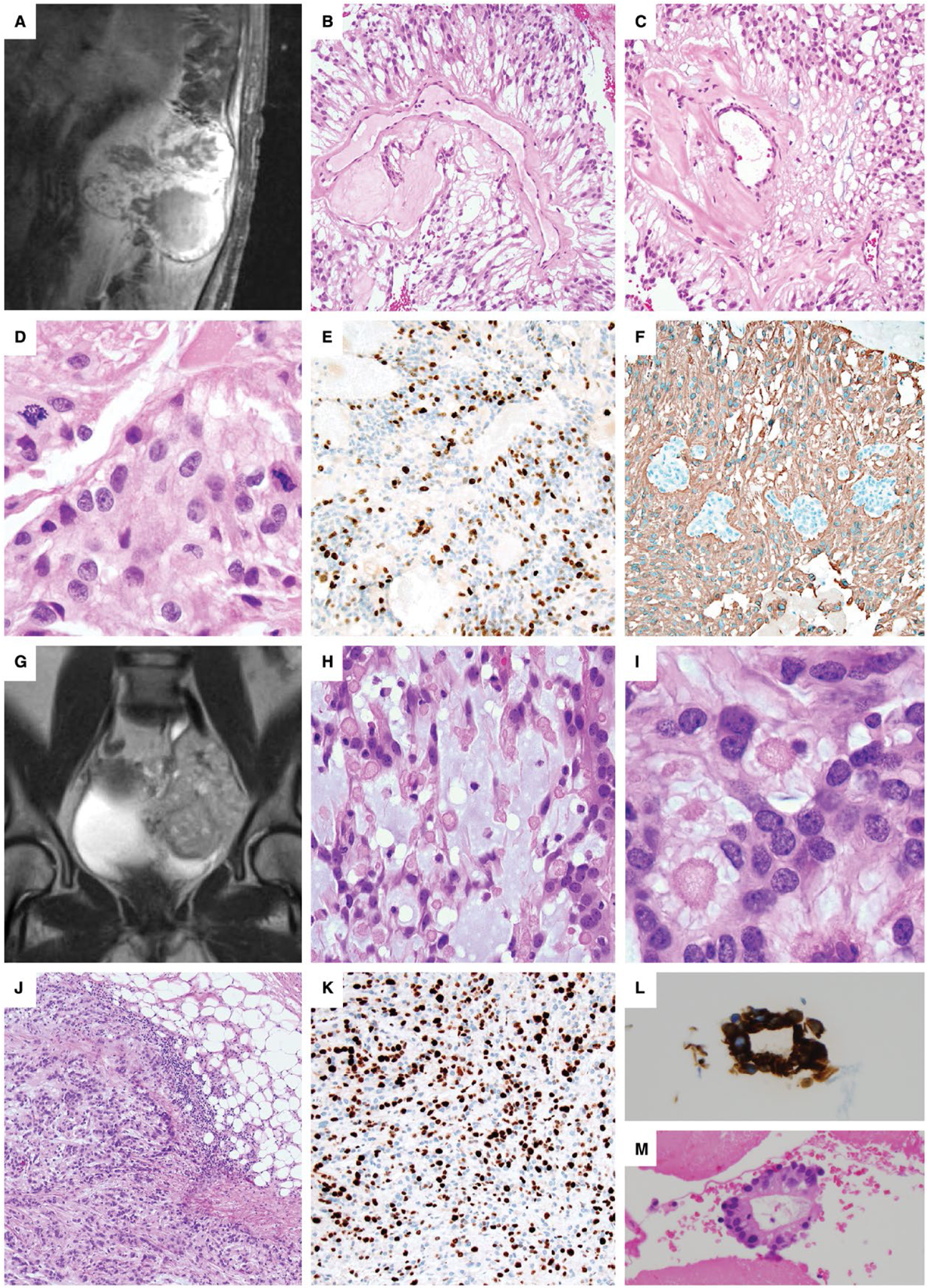
A–F. Case #12: A 45-year-old man underwent subtotal resection and radiation of an 11.5 cm T11-L2 MPE. (A). Recurrence detected by MRI 12 years later showed destruction of the L1 vertebrae with invasion into the paraspinal soft tissues. Areas of classic MPE histology were present (B,C), but were accompanied by anaplastic features, including increased mitotic activity of 17 mitoses per 10 HPF (D), Ki-67 LI up to 26% and prominent microvascular proliferation (MVP). There were foci of non-palisading necrosis in this patient that had previously received radiation therapy. A representative area of increased Ki-67 staining is shown (E), and foci of MVP are seen among GFAP-positive neoplastic cells (F). G–M. Case #10: A 10-cm pelvic recurrence on MR imaging (G) was found in a 45-year-old woman 14 years after resection and radiation of a sciatic notch MPE. Careful review of the medical record could not establish if the original mass was intradural or extradural in origin, or if it arose as an extraspinal primary soft tissue MPE. The recurrence contained areas of classic MPE with increased mucin and collagen balloons H–I. The mass was invasive into the adjacent soft tissues (J), with a Ki-67 LI up to 40% (K), a mitotic index of 7/10 HPF, MVP and palisading necrosis. As the patient had received radiation therapy, the palisading necrosis was not considered an anaplastic feature. The patient was concurrently found to have multiple pulmonary nodules, a large left-sided pleural effusion and an enhancing pleural-based mass. Evaluation of the pleural fluid, shown here with GFAP immunostaining (L), and a pleural biopsy (M) demonstrated metastatic MPE. At the time of the pelvic recurrence, a sacral mass was also present, which was resected 4 months later in a separate surgery.
