Abstract
Background:
Social distancing strategies such as “stay-at-home” (SAH) orders can slow the transmission of contagious viruses like the SARS-CoV-2 virus, but require population adherence to be effective. This study explored adherence to SAH orders by young adults with hazardous drinking, and the role of alcohol consumption with in-person contacts in adherence to SAH orders.
Methods:
Analyses included young adults with hazardous drinking (i.e., AUDIT-C score ≥3/4 for women/men; n=50; ages 18–25) participating in a randomized trial in Pittsburgh, PA. Participants provided experience sampling reports on drinking twice per week from the week before “stay-at-home” SAH orders started on April 1, 2020 through 6 weeks during the SAH period. We examined how in-person contact with non-housemate friends changed over time and event-level relationships between alcohol consumption and in-person contacts.
Results:
The percentage of participants with any in-person contact in the week prior to SAH was 44% (95% CI 30%–59%), which decreased to 29% (95% CI 15%–43%) in the first SAH week and increased to 65% (95% CI 46%–85%) by SAH week 6. Controlling for average levels of alcohol consumption, on days when young adults drank, participants reported more in-person contacts compared to non-drinking days.
Conclusion:
Preliminary data indicate that, among young adults with hazardous drinking, adherence to public policies like SAH orders is sub-optimal, declines over time, and is associated with drinking events. Interventions aimed at enhancing young adults’ adherence to social distancing policies are urgently needed.
Keywords: young adult, alcohol, social distance
The SARS-CoV-2 virus, which causes COVID-19 illness, is highly contagious, spreading primarily through respiratory droplets, even among individuals who are pre- or non-symptomatic [1]. Social distancing strategies that involve reducing the number of between-person contacts such as “stay-at-home” (SAH) orders may help delay the exponential spread of the outbreak until effective vaccines become available or communities develop herd immunity [2].
Compliance is needed for social distancing strategies like SAH orders to be effective [3], which is especially difficult in the United States, which prizes individual freedom. Early evidence from tracking smartphones suggests that compliance with SAH orders across the US is sub-optimal, with only 35% of people staying home [4]. Compliance may be especially difficult for young adults. A recent survey of 7,355 respondents found that the youngest age group (18–31) reported the lowest compliance rate (52.4%) compared to the other age groups (all > 60%) [5].
In this study, we investigate in-person contacts with non-household friends by young adults with hazardous drinking (i.e. AUDIT-C score ≥3/4 for women/men), and the role of alcohol consumption on the frequency of these contacts, and number of friends involved in these contacts for time periods before and after mandated SAH. Given that 40% of young adults in the US have a history of hazardous drinking, the actions of this population have important public health implications [6]. We leveraged an on-going trial that collected experience sampling data twice per week from young adults with a history of hazardous drinking. We examined how in-person contact with friends (not housemates) changed over time and event-level relationships between alcohol consumption and in-person contacts. We hypothesized that young adults with a history of hazardous drinking would initially decrease their in-person contacts, but then tire of social distancing and increase in-person contacts (i.e. quarantine fatigue). Given the prominent role of alcohol consumption in socialization among young adults, particularly those with a history of hazardous drinking [7], we also hypothesized that most in-person contacts would occur with concurrent alcohol consumption (i.e. drinking) events. The use of experience sampling data allowed us to separate within-person and between-person factors associated with SAH order adherence (i.e. in-person contacts) [8]. Within-person analyses provide insights about how alcohol consumption on a given day, which differs from typical drinking for that individual, is associated with in-person contacts on that day. Given that models of viral infectivity suggest intermittent social distancing measures may be necessary until 2022 [9], it is imperative to identify key drivers and modifiable covariates related to compliance with social distancing policies among young adults.
METHODS
Participant Screening and Recruitment
This study includes a sub-sample of non-treatment seeking young adults (ages 18–25) who screened positive for hazardous alcohol consumption in an emergency department (ED) and enrolled in a randomized trial testing different text message interventions. Briefly, during the period of enrollment for this study, 128 young adults who presented to an urban ED and were not seeking help for drinking were screened for hazardous alcohol use. A total of 54 young adults reported a score of ≥3 for women or ≥4 for men on the Alcohol Use Disorder Identification Test for Consumption (AUDIT-C) [10] and reported at least one binge drinking episode (4+ drinks per day for women; 5+ drinks per day for men [11]) in the prior month. Four young adults were excluded for reporting past treatment for drug or alcohol use or current medical treatment for psychiatric disorders, resulting in a final sample of 50 participants. The study protocol was approved by the Institutional Review Board (IRB) at the University of Pittsburgh. The trial was pre-registered (NCT02918565). Full details of the screening, enrollment and intervention features are described in prior papers [12,13].
Procedures
Two days per week participants were prompted to report the number of alcoholic drinks consumed the prior day (i.e., drinking quantity; DQ). The day(s) of the week that a participant received assessments were based on an individual’s baseline drinking patterns as reported in the 30-day Time Line Follow-Back (TLFB) calendar at baseline. This design feature was intended to capture days with a higher probability of alcohol consumption and minimize assessment burden on non-drinking days. We made an IRB-approved modification to the text message protocol on March 23, 2020 to also assess the number of friends (not including housemates) the participants were with and the number of those friends who were drinking alcohol. Prompts and responses were provided and obtained via text messaging (i.e., SMS) and stored in a Microsoft Access database.
Measures
Day-Level Measures
Alcohol Consumption:
At 12pm on the 2 days per week an individual told us they typically drink, we asked: “How many drinks did you have yesterday?” The definition for standard drinks was provided in enrollment procedures. We examined drinking quantity (DQ) as a continuous (count) variable. We coded each day when a woman reported at least one day of consuming >4 or more standard drinks or a man reported >5 or more standard drinks as having a binge drinking day (BDD). We have successfuly used this single-item measure in prior studies, where responses were correlated with TLFB measures [14].
In-person Contacts:
If a participant reported not drinking the prior day, we asked: “How many friends were you with yesterday? (not including people you live with)”. If a participant reported drinking the prior day, they received the following question: “How many friends were you with while drinking? (not including people you live with)”. At the day-level, the in-person contacts variable was coded as a count variable representing the number of non-household friends with whom the participant spent time.
Weekend:
We coded assessments that occurred on a Friday or Saturday as weekend and Sunday through Thursday as non-weekend.
Week-Level Measures
In-person Contacts:
To understand how in-person contacts changed from the week prior to SAH orders through the SAH period, we created week-level variables related to in-person contacts. By summing the in-person contacts over days sampled, we created variables for any in-person contact in a given week (none=0; any=1) and maximum number of in-person contacts in a given week.
Person-level Measures
At baseline, participants reported age, sex (male=1; female=0), race (black=0, white=1, other=2), current college enrollment (yes=1; no=0), and living situation (by self=0; with other(s), same sex=1; with other(s), other sex=2; with family=3). We measured alcohol use severity using the AUDIT-C [10].
Analyses
We first examined patterns of missingness for the DQ and in-person contact assessments and assessed person-level (i.e. sex, race, college education, AUDIT-C score, living situation) and day-level covariates (i.e. weekend) for associations with missingness. To test our hypothesis that young adults would initially decrease their in-person contacts, but then tire of social distancing and increase them, we used general estimating equations (GEE) models with exchangeable correlation [15]. Independent variable was week (1 [pre-SAH week 1] to 6 [SAH week 5]). Covariates at the person-level (i.e. sex, race, college education, living situation) were tested in univariate models and only retained in the final model if they had significant univariate association.
To test our hypothesis that in-person contacts would primarily occur with concurrent alcohol consumption (i.e. drinking) events, 412 days nested within 47 persons were analyzed using multilevel models. Outcomes of interest were any in-person contact and number of in-person contacts that day. The time-invariant person-level variable for usual alcohol consumption was calculated as the arithmetic mean across each individual’s repeated measures. Time-varying, day-level variables were calculated as deviations from those person-level means. Again, covariates at the person-level (i.e. sex, race, college education, living situation) and the day-level (i.e. weekend) were tested in univariate models and only retained in the final model if they had significant univariate association. Full information maximum likelihood (FIML) estimation was used to handle missing data [16]. Finally, to ensure models were not influenced by non-random missingness, we engaged multiple imputation procedures using sex and AUDIT-C score as predictors of missing values, Poisson distribution for DQ and friend counts, re-ran models and examined estimates from 10 imputations. Analyses were conducted using Stata 15.0 (StataCorp LLC, College Station, TX).
Results
Participant Characteristics:
Sample (N=50) mean age was 22.2 (SD=2.1), 64% were female, 22% self-identified as black race, 48% were in college, and 36% were living with friends (see Table 1 for baseline descriptive statistics). At enrollment (baseline), the mean AUDIT-C score was 5.9 (SD 1.7; range 3 to 10) and in the past month participants reported a mean of 2 BDD. (see Table 1)
Table 1:
Baseline Characteristics
| Characteristics | Analyzed (n=50) |
|---|---|
| Age, mean (SD) | 22.2 (2.1) |
| Female | 32 (64%) |
| Race | |
| White | 38 (76%) |
| Black | 11 (22%) |
| Asian | 1 (2%) |
| Hispanic ethnicity | 4 (8%) |
| Current college enrollment | 24 (48%) |
| Living situation | |
| Alone | 11 (22%) |
| Friends, same sex | 10 (20%) |
| Friends, other sex | 8 (16%) |
| Family | 21 (42%) |
| Employment | |
| None | 11 (22%) |
| Part-time | 16 (32%) |
| Full-time | 23 (46%) |
| Alcohol Use | |
| AUDIT-C score, median (IQR) | 6 (5,7) |
| BDD | 2.0 (2.6) |
Results are presented as mean (SD) unless specified otherwise. Abbreviations: AUDIT-C= alcohol use disorders identification test for consumption; BDD=binge drinking days
Assessment Characteristics:
In this study, 76.3% of assessments were sent on the weekend and 23.7% on non-weekend days. 22.4% of DQ assessments were missing and 32.4% of in-person contact assessments were missing. Male sex was associated with missingness for DQ (OR=2.86; 95% CI 1.93, 4.22) and missingness for in-person contacts (OR=1.18; 95% CI 1.26, 2.57).
Drinking and In-person Contact Characteristics:
On drinking days (42.2% of all days assessed, with 83% of participants having at least one drinking day), participants drank an average of 3.1 drinks (SD= 2.8; range = 1 to 20). When drinking, there was in-person contact on 48.0% of days. 40.0% of the times when in-person contact occurred, it was with one person (range 1–20). When not drinking, there was in-person contact on 20.9% of days. 65.3% of the times when in-person contact occurred when not drinking, it was with one person (range 1–6). There were BDD on 9.9% of all days assessed, with 48.9% of participants having at least one BDD.
In-person Contact over Time:
Over the entire sampling period, of the 412 days assessed, any in-person contact occurred on 134 days (32.5%). The percentage of participants with any in-person contact in the week prior to SAH orders was 44% (95% CI 30%–59%), which decreased to 29% (95% CI 15%–43%) in the first week of the SAH period and increased to 65% (95% CI 46%–85%) by week 6 of the SAH period (see Figure 1). The GEE models examining the effect of time (week) on any in-person contact and maximum number of in-person contacts are shown in Table 2. Compared to the pre-SAH week, there were significant increases in the probability of any in-person contact by SAH week 6 (beta=0.20; SE=0.08; Table 2, panel a).
Figure 1: Proportion of Participants with Any In-Person Contact by Week.
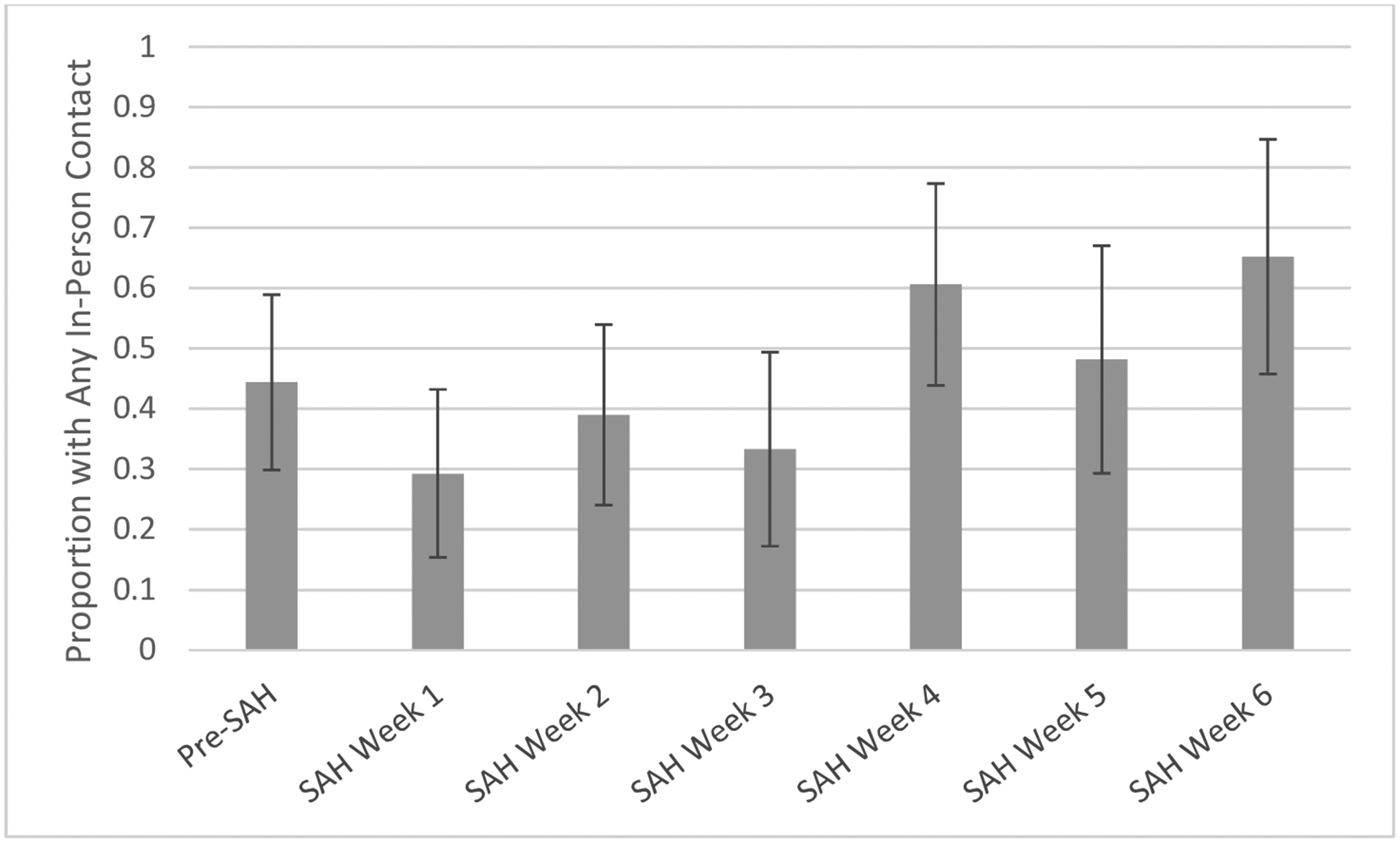
Abbreviations: SAH= “stay-at-home” orders
Table 2.
Predictors of In-Person Contact
| a. Any In-Person Contact | |||
|---|---|---|---|
| beta | SE | p-value | |
| Week | |||
| Pre-SAH | REF | ||
| SAH Week 1 | −0.15 | 0.08 | 0.07 |
| SAH Week 2 | −0.03 | 0.09 | 0.7 |
| SAH Week 3 | −0.11 | 0.1 | 0.27 |
| SAH Week 4 | 0.16 | 0.08 | 0.05 |
| SAH Week 5 | 0.01 | 0.1 | 0.96 |
| SAH Week 6 | 0.2 | 0.08 | 0.01 |
| College enrollment | |||
| Yes | REF | ||
| No | 0.17 | 0. 1 | 0.07 |
| b. Max Number of In-Person Contacts | |||
| beta | SE | p-value | |
| Week | |||
| Pre-SAH | REF | ||
| SAH Week 1 | −0.64 | 0.18 | <0.0001 |
| SAH Week 2 | −0.28 | −0.19 | 0.15 |
| SAH Week 3 | −0.29 | 0.2 | 0.15 |
| SAH Week 4 | 0.56 | 0.25 | 0.03 |
| SAH Week 5 | 0.67 | 0.28 | 0.02 |
| SAH Week 6 | 1.03 | 0.31 | 0.001 |
| College enrollment | |||
| Yes | REF | ||
| No | 0.95 | 0. 2 | <0.0001 |
Abbreviations: SE= standard error; SAH=”stay-at-home” orders; REF=reference
Over the entire assessment period, on days with any in-person contact, the mean number of max in-person contacts was 3.8 (SD 2.8).Compared to the pre-SAH week, there were significant reductions in the number of max in-person contacts in SAH week 1 (beta=−0.64; SE=0.18) and significant increases in the number of max in-person contacts in week 4 (beta−0.56; SE=0.25) through 6 (beta=1.03; SE=0.31) (Table 2, panel b). Controlling for weeks, not being enrolled in college was associated with greater max in-person contacts (beta=0.95; SE=0.20). Model estimates for any and max number of in-person contact were similar when using multiple imputation datasets.
In-person Contact and Drinking:
Mixed-effect model results for the within- and between- person effect of any drinking and binge drinking on in-person contacts are shown in Tables 3 and 4. Within-person (adjusting for an individual’s typical drinking) there were greater odds of any in-person contact when participants reported any drinking (OR=6.6; Table 3) or binge drinking (OR=8.6; Table 4) on a given day. There were also within-person associations between number of in-person contacts and any drinking (beta=1.32; Table 3) and binge drinking (beta=1.6; Table 4). Similar associations also existed between-person. In these multi-level models, no level-2 (between-person) covariates (e.g. sex or college enrollment) nor within-person covariate (i.e. weekend) were associated with in-person contact. Model estimates were similar when using multiple imputation datasets.
Table 3.
Association of Any Drinking with In-Person Contacts
| Any In-Person Contact | Odds Ratio | SE | p-value |
|---|---|---|---|
| Intercept | 0.17 | 0.07 | <0.0001 |
| Any drinking (between-person) | 7.92 | 6.88 | 0.02 |
| Any drinking (within-person) | 6.58 | 2.33 | <0.0001 |
| Weekend | 2.18 | 0.89 | 0.06 |
| Level 1 residual variance | 2.23 | 0.84 | |
| # In-Person Contacts | beta | SE | p-value |
| Intercept | −1.09 | 0.25 | <0.0001 |
| Any drinking (between-person) | 2.34 | 0.6 | <0.0001 |
| Any drinking (within-person) | 1.32 | 0.15 | <0.0001 |
| Weekend | 0.18 | 0.18 | 0.32 |
| Level 1 residual variance | 1.44 | 0.46 |
Abbreviations: SE= standard error
Table 4.
Association of Binge Drinking with In-Person Contacts
| Any In-Person Contact | Odds Ratio | SE | p-value |
|---|---|---|---|
| Intercept | 0.17 | 0.07 | <0.0001 |
| Binge drinking (between-person) | 22.6 | 42.9 | 0.1 |
| Binge drinking (within-person) | 8.56 | 3.79 | <0.0001 |
| Weekend | 2.06 | 0.83 | 0.07 |
| Level 1 residual variance | 2.02 | 0.76 | |
| # In-Person Contacts | beta | SE | p-value |
| Intercept | −1.12 | 0.24 | <0.0001 |
| Binge drinking (between-person) | 4.15 | 1.34 | 0.002 |
| Binge drinking (within-person) | 1.64 | 0.13 | <0.0001 |
| Weekend | 0.33 | 0.17 | 0.06 |
| Level 1 residual variance | 1.44 | 0.46 |
Abbreviations: SE= standard error
Discussion
In this exploratory study, we found that many at-risk young adults with past hazardous drinking do not strictly adhere to SAH orders. Overall, in the first 6 weeks of SAH orders, 44% of young adults reported in-person contacts with non-housemate friends, and there was an average number of 3.8 in-person contacts per social event, nearly identical to the week prior to SAH orders. When viewed at this level, it appears that SAH orders did not influence in-person social interactions with non-housemate friends among study participants, who were young adults with a history of hazardous alcohol drinking. However, when viewed by week, we found an initial dip in the prevalence and number of in-person contacts, which rebounded and increased above the pre-SAH week by week 4 of SAH orders. These findings are consistent with prior studies demonstrating the lower prevalence of social distancing among young adults [5], and concern in the lay press regarding quarantine fatigue. Study results also suggest that, among young adult hazardous drinkers, public policies need to consider the potential for rebound effects of social distancing for certain at-risk subgroups.
We found that there is a strong association between drinking events and in-person contacts. Overall, in the SAH order period, 63% of days with in-person contact occurred during drinking events. Individuals with greater overall probability of drinking, and binge drinking, had higher odds of any in-person contact and reported higher in-person contact with non-housemate friends. On any given day, controlling for their typical drinking, individuals who drank at all or who had a binge drinking episode had both greater odds of any in-person contact and reported a greater number of in-person social contacts.
Social-ecological models suggest that interpersonal processes, social networks, social context, and social infrastructures all play a role in individuals’ behavior and how it changes over time – sometimes in conflicting ways. The findings of this study fit with potential social network-level effects as described in social-ecological models of alcohol use in young adults [17], prior research showing the influence of peers on alcohol consumption [7], and that the number of friends present at a social occasion is directly associated with drinking quantity [18]. Our findings extend prior work by showing that these interpersonal-level factors continue to play a role in young adult drinking behavior despite environmental restrictions such as SAH orders and related fears around person-to-person viral transmission. Drinking excessively could put individuals at additional viral transmission risk due to loss of inhibition and increased interpersonal contacts [19]. In addition, depressed immune function related to binge drinking could compound risk of infection [20].
We did not find that sex, race, employment or living situation were associated with in-person contacts (and thus were not included in final model outputs). We did find, however, that not being enrolled in college was associated with higher probability of social contacts over time (i.e., during the SAH order period). This result suggests that there may be educational barriers to compliance with public policies and young adults not in college may lack health education available to those in college. It is somewhat surprising that drinking-related social events were as common as they were in young adults. Given statewide closures of college campuses, bars and restaurants, certain opportunities for socialization are curtailed. With many college students (48% of our sample) presumably moving home with parents, we expected increases in parental oversight of young adult behaviors to potentially result in curtailed drinking [21] and support of SAH orders.
Findings highlight challenges with social distancing among young adults. There are numerous factors that can affect compliance with social distancing policies. On one level, compliance requires awareness or understanding of the rules and trust toward the authorities that enact them. On another level, compliance requires a belief that one could put oneself and/or others at risk by not following social or physical distancing guidelines. Young adults may have difficulty with compliance with “stay-at-home” orders due to a combination of lack of concern for getting themselves (due to perceived lack of vulnerability) or others sick (due to lack of awareness of asymptomatic transmission). Early reports of norms-based interventions were not effective at increasing social distancing during the COVID-19 pandemic, but illustrate that fear of missing out on social events was a key target [22]. This suggests that platforms that provide a way for young adults to meaningfully socialize remotely could help reduce in-person contacts.
There are several limitations that should be considered. First, we were only able to study a relatively small sample of young adults with hazardous drinking histories and results may not be representative of other populations of young adults. All measures were self-report and subject to reporting biases. We were not able to assess more detailed event-level factors such as drinking context and perceived peer norms. Finally, we have limited data on alcohol availability. Strengths of this study include the following. We recruited a socio-demographically diverse cohort of young adults not seeking treatment for alcohol use. We used experience sampling methods to understand this event-level relationship, which reduces recall biases and allows us to make inferences about temporality [23]. Finally, we used models accounting for clustering of data within individuals and included relevant covariates, which reduces the possibility of confounding.
Conclusions
We found preliminary evidence that young adults’ adherence to public policies like “stay-at-home” orders is sub-optimal, declines over time, and is associated with drinking events. Interventions that address the role of alcohol with in-person contacts among young adults are needed.
Implications and Contribution:
This study shows how alcohol consumption is associated with non-compliance with social distancing during a pandemic among young adults with hazardous drinking.
Funding:
This work was supported by the National Institutes of Health (R01 AA023650).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Citations
- 1.Hsueh SC, Yen MY, Ko WC, & Hsueh PR (2020). Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): Facts and myths. Journal of microbiology, immunology, and infection, 53(3), 404–412. 10.1016/j.jmii.2020.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sen S, Karaca-Mandic P, & Georgiou A (2020). Association of Stay-at-Home Orders With COVID-19 Hospitalizations in 4 States. JAMA, 10.1001/jama.2020.9176. Advance online publication. 10.1001/jama.2020.9176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maharaj S, & Kleczkowski A (2012). Controlling epidemic spread by social distancing: do it well or not at all. BMC public health, 12, 679 10.1186/1471-2458-12-679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gao S, Rao J, Kang Y, Liang Y & Kruse J Mapping county-level mobility pattern changes in the United States in response to COVID-19. Available at SSRN 3570145 (2020). [Google Scholar]
- 5.Park CL, Russell BS, Fendrich M, Finkelstein-Fox L, Hutchison M, & Becker J (2020). Americans’ COVID-19 Stress, Coping, and Adherence to CDC Guidelines. Journal of general internal medicine, 1–8. Advance online publication. 10.1007/s11606-020-05898-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wechsler H, Lee JE, Kuo M, Seibring M, Nelson TF, Lee H. Trends in college binge drinking during a period of increased prevention efforts. Findings from 4 Harvard School of Public Health College Alcohol Study surveys: 1993–2001 [published correction appears in J Am Coll Health 2002 Jul;51(1):37]. J Am Coll Health. 2002;50(5):203–217. doi: 10.1080/07448480209595713 [DOI] [PubMed] [Google Scholar]
- 7.Borsari B, Carey KB Peer influences on college drinking: a review of the research. J Subst Abuse 2001; 13: 391–424. [DOI] [PubMed] [Google Scholar]
- 8.Curran PJ, Bauer DJ. The disaggregation of within-person and between-person effects in longitudinal models of change. Annu Rev Psychol. 2011;62:583–619. doi: 10.1146/annurev.psych.093008.100356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kissler SM, Tedijanto C, Goldstein E, Grad YH, & Lipsitch M (2020). Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science (New York, N.Y.), 368(6493), 860–868. 10.1126/science.abb5793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, & Kivlahan DR (2007). AUDIT-C as a brief screen for alcohol misuse in primary care. Alcoholism, clinical and experimental research, 31(7), 1208–1217. 10.1111/j.1530-0277.2007.00403.x [DOI] [PubMed] [Google Scholar]
- 11.SAMHSA. 2018. National Survey on Drug Use and Health. Table 7.16A—Alcohol Use in Lifetime, Past Year, and Past Month among Persons Aged 12 to 20, by Gender: Numbers in Thousands, 2002–2018 Available at: https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHDetailedTabs2018R2/NSDUHDetTabsSect7pe2018.htm#tab7-16a. Accessed 6/4/20
- 12.Suffoletto B, Kirisci L, Clark DB, & Chung T (2019). Which behavior change techniques help young adults reduce binge drinking? A pilot randomized clinical trial of 5 text message interventions. Addictive behaviors, 92, 161–167. 10.1016/j.addbeh.2019.01.006 [DOI] [PubMed] [Google Scholar]
- 13.Suffoletto B, Huber J, Kirisci L, Clark D, & Chung T (2020). The effect of SMS behavior change techniques on event-level desire to get drunk in young adults. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors, 34(2), 320–326. 10.1037/adb0000534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suffoletto B, Callaway C, Kristan J, Kraemer K, & Clark DB (2012). Text-message-based drinking assessments and brief interventions for young adults discharged from the emergency department. Alcoholism, clinical and experimental research, 36(3), 552–560. 10.1111/j.1530-0277.2011.01646.x [DOI] [PubMed] [Google Scholar]
- 15.Zeger SL, & Liang KY (1992). An overview of methods for the analysis of longitudinal data. Statistics in medicine, 11(14–15), 1825–1839. 10.1002/sim.4780111406 [DOI] [PubMed] [Google Scholar]
- 16.Mazza GL, Enders CK, & Ruehlman LS (2015). Addressing Item-Level Missing Data: A Comparison of Proration and Full Information Maximum Likelihood Estimation. Multivariate behavioral research, 50(5), 504–519. 10.1080/00273171.2015.1068157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sudhinaraset M, Wigglesworth C, & Takeuchi DT (2016). Social and Cultural Contexts of Alcohol Use: Influences in a Social-Ecological Framework. Alcohol research : current reviews, 38(1), 35–45. [PMC free article] [PubMed] [Google Scholar]
- 18.Thrul J, & Kuntsche E (2016). Interactions Between Drinking Motives and Friends in Predicting Young Adults’ Alcohol Use. Prevention science : the official journal of the Society for Prevention Research, 17(5), 626–635. 10.1007/s11121-016-0660-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Field M, Wiers RW, Christiansen P, Fillmore MT, & Verster JC (2010). Acute alcohol effects on inhibitory control and implicit cognition: implications for loss of control over drinking. Alcoholism, clinical and experimental research, 34(8), 1346–1352. 10.1111/j.1530-0277.2010.01218.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bala S, Marcos M, Gattu A, Catalano D, & Szabo G (2014). Acute binge drinking increases serum endotoxin and bacterial DNA levels in healthy individuals. PloS one, 9(5), e96864 10.1371/journal.pone.0096864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Evans-Polce RJ, Maggs JL, Staff J, & Lanza ST (2017). The Age-Varying Association of Student Status with Excessive Alcohol Use: Ages 18 to 30 Years. Alcoholism, clinical and experimental research, 41(2), 407–413. 10.1111/acer.13294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leary A, Dvorak R, De Leon A, Peterson R, & Troop-Gordon W (2020, May 13). COVID-19 Social Distancing. 10.31234/osf.io/mszw2 [DOI]
- 23.Shiffman S (2009). Ecological momentary assessment (EMA) in studies of substance use. Psychological assessment, 21(4), 486–497. 10.1037/a0017074 [DOI] [PMC free article] [PubMed] [Google Scholar]


