Abstract
Despite the large amounts of research currently being conducted and the high number of editorials warning about the potential mental health impacts, there is a stunning lack of longitudinal mental health data on the effects of the pandemic. Yet, the pandemic may have sizable long-term impacts on psychological distress and health behaviors—these effects may be long-lasting and may disproportionately affect some demographic groups more than others. Data came from a longitudinal international study of the impacts of the COVID-19 pandemic on adults’ psychological distress and wellbeing (N = 1567). We found high rates of depression (55% were diagnosable with probable depression at baseline), anxiety (65%), and risk for PTSD (51%). More than one-third of participants who reported that they drank alcohol indicated that their drinking had increased since the start of the pandemic. Over time, depressive symptoms and suicidal thoughts and behaviors increased significantly, but acute stress symptoms decreased. Specific demographic groups (people of color and sexual and gender minorities) appeared to be at high risk of distress across analyses. Our findings suggest high rates of depression, anxiety, acute stress, and other signs of distress like isolation, hopelessness, and use of substances to cope—even at five-month follow-up. Our findings suggest a need to prioritize availability of, and access to, mental health care during both the pandemic and the recovery.
1. Critical need for long-term mental health data during the COVID-19 pandemic
The COVID-19 pandemic has had resounding effects on social support, employment, healthcare, education and nearly every other aspect of daily life. Containment efforts critical for halting the spread of the virus have unfortunately increased social isolation, loneliness, relationship stress, and disconnection from communities. Many people have lost their usual sources of support as a result of disruptions to work, school, and not being able to safely get together with others. As a result, experts have issued grave warnings about mental health during the SARS-Cov-2 (COVID-19) pandemic (Pfefferbaum and North, 2020) and that the implications for mental and physical health will persist long after initial containment efforts (Brooks et al., 2020). Yet despite ample theorizing, there is a dearth of empirical data on the mental health effects of the pandemic, particularly longitudinal data. Limited data suggest high rates of psychological distress in the general population (McGinty et al., 2020; Holingue et al., 2020b; Czeisler et al., 2020) and that distress may increase over time (Keeter, 2020; Riehm et al., 2021). Data also suggests increases in unhealthy coping behaviors like alcohol use (Czeisler et al., 2020; Rodriguez et al., 2020).
Critically, data from previous pandemics suggest that there are not only acute mental health effects, but that psychological distress may persist long after the pandemic ceases (Brooks et al., 2020). In a review of research on the effects of quarantines in previous pandemics (e.g., SARS, Ebola), Brooks and colleagues (Brooks et al., 2020) reported longer-term psychological impacts of quarantining like acute stress, PTSD symptoms, depression, and alcohol abuse. Only one study (Keeter, 2020), however, in the review was longitudinal suggesting our understanding of the course of psychological distress during and after a pandemic is limited. Previous modern pandemics were also shorter, far less widespread, and had fewer socioeconomic implications. It is thus imperative to prospectively document the mental health consequences that may arise from the synergistic effects of economic precarity, unemployment, isolation, uncertainty, loss, and fear. Understanding how distress may, or may not, change across an unprecedented global pandemic is important for informing current prevention and intervention efforts, as well as planning for longer-term supports to halt worsening or chronicity of distress. Prospective research can also provide insights into predictors of distress and resilience during large-scale disasters (Chen and Bonanno, 2020).
Although nearly every person in the world is affected in some way by the pandemic because of containment efforts or the virus itself, there are likely particularly pernicious effects on marginalized populations (Kantamneni, 2020). Indeed, increasing evidence suggests that minority groups such as people of color and sexual and gender minorities are at increased risk of psychological distress during the pandemic due to the compounding effects of discrimination and stigma (Mattei et al., 2020; Goldberg, 2020; Romero et al., 2020). Marginalized groups may additionally be more vulnerable due to pre-COVID unemployment, workplace discrimination, poverty, housing and food insecurity, as well as other stressors (e.g., isolation, lack of legal protections) that are likely exacerbated during the pandemic (Conron and Goldberg, 2020; Gruberg and Madowitz, 2020; O’Neill, 2020; Wilson and Conron, 2020; Martin et al., 2020; Garcia et al., 2021; Gravlee, 2020).
To better understand the longer-term effects of the pandemic on mental health, we report longitudinal data on depression, suicide risk, and acute stress at two timepoints: April and September 2020. Finally, we test key demographic (age, race/ethnicity, gender, sexual identity, household composition, relationship status) and psychological factors (depression, previous mental health diagnosis, anxiety, using substances to cope, social support) associated with risks found in previous research (Holingue et al., 2020b; Riehm et al., 2020; Holingue et al., 2020a; Smail et al., n.d.).
2. Methods
Drawing on longitudinal data from an international convenience sample (N = 3358) of adults 18 or older living in every US state and more than 50 countries, we report on findings from validated psychological distress instruments, as well as measures of COVID-19-related concerns, and the effects of the pandemic on employment and food insecurity. Recruitment was conducted primarily through social media (i.e., twitter and facebook), listservs, social networks, websites aimed at the general population like Buzzfeed, and a research match website at Columbia University. Interested individuals were given links to the study webpage (in case they had more questions or wanted to contact a study team member) and were also given a direct link to the survey that included a brief description of the study; those who clicked through to the study were considered to have consented. The baseline survey had 146 questions and took approximately 30 min to complete; participants were not offered compensation for their time. In case anyone became distressed during the study, participants were provided with a list of resources (e.g., hotlines, counseling services) at three points in the survey: in the consent, immediately at the end of the section on suicide, and at the culmination of the survey. Participants who consented to be contacted again for follow-up surveys were sent an email at 5-month follow-up with a personalized link to the survey to allow linkages between waves of data for each participant. All study procedures were reviewed and approved by the Columbia University Irving Medical Center IRB (protocol #AAAS9704).
Here we focus on respondents (N = 1567) who completed baseline surveys during the weeks of April 5–19, 2020 (i.e., after 43 states issued statewide stay-at-home orders) and the five-month follow-up (August 28–September 11, 2020). The survey was open to anyone who was age 18 or older (with no additional inclusion or exclusion criteria) and the current analyses are inclusive of anyone irrespective of country of residence.
2.1. Measures
2.1.1. Demographics
Participants were asked their age (categorized as: 18–30, 31–40, 41–50, 51–65, and 66+), race/ethnicity (categorized as Asian, Black, Latinx, and White), gender (woman, man), and whether they are a sexual or gender minority (SGM; e.g., lesbian, gay, bisexual, transgender, nonbinary). We also include 5-month follow-up household composition (coded as living alone, living with partner, living with partner and kids, living with kids but no partner, or other living arrangements), relationship status (single or in a committed relationship), and whether they had lost a job or had been laid off or furloughed at any point in the study.
2.1.2. COVID worries
Participants were asked to rate how worried they felt about factors related to the pandemic on a scale of 0 (not worried) to 100 (extremely worried). Participants were asked whether they were worried about the following related to COVID-19: 1) the coronavirus itself; 2) their own health; 3) becoming sick and dying from the virus; 4) their future; and 5) managing child care and work. Each worry was included separately.
2.1.3. Psychological distress
Our measures of depression and acute stress/PTSD symptoms were chosen to be consistent with measures used in previous pandemics to support comparisons across studies (Brooks et al., 2020).
Depression was measured using the Center for Epidemiologic Studies Depression (CES-D) (Radloff, 1977); scale is a short self-report scale designed to measure depressive symptoms in large-scale surveys and been found to have high specificity and sensitivity (Radloff, 1977). We used an 11-item version of the CES-D that has comparable psychometric properties to the original version and reduces respondent burden (Kohout et al., 1993). Participants were asked to indicate how often they have experienced each of the 11 items (e.g., felt depressed) during the past week on a 4-point scale (0 = rarely or none of the time, 3 = most of the time). A score of 10 or higher was considered to signify a probable diagnosis of depression. The internal consistency for the 11-item version based on the current sample at baseline assessment was 0.850.
Suicide risk was measured using the Suicidal Ideation Attributes Scale (SIDAS) which measures thoughts and behaviors and provides an assessment of risk (scores of 21 or higher are considered severe risk and 10 or higher is considered to be some risk) (van Spijker et al., 2014).
Acute stress/risk for PTSD was measured using a modified version of the Impact of Event Scale (Horowitz et al., 1979) which is a 15-item questionnaire measuring subjective distress related to a specific event. The scale was adapted in order to measure acute peritraumatic stress (i.e., the tense of all items was changed from the past to the present tense to examine PTSD symptoms at the time of the potentially traumatic event) and participants were specifically asked to rate their levels of stress related to COVID-19 (e.g., I have dreams about [COVID-19]). Participants were asked to rate each of the items on a 4-point scale (0 = not at all, 5 = often) according to how they have experienced each item in the past 7 days. The IES has commonly been used to screen for PTSD in clinical and research settings (Rash et al., 2008; Hosey et al., 2020; Coffey et al., 2006). Previous literature has reported strong criterion validity and convergent validity of IES. The internal consistency of the overall IES scores based on the modified version among the current sample at the first assessment was excellent (α = 0.942). Potential risk for PTSD was determined using a cutoff score of 11, which gives sensitivity of 0.72 and specificity of 0.94 (Thoresen et al., 2010).
Anxiety was measured with the Generalized Anxiety Disorder 7-item (GAD-7) scale (Spitzer et al., 2006). In the GAD, participants are asked to indicate how often, over the past two weeks, they have been bothered with anxiety-related symptoms like worrying, feeling nervous, feeling restless or irritable. Scores of 10 or greater are considered to indicate a severity of anxiety symptoms that require clinical assessment. Internal consistency at 5-month follow-up (the first timepoint at which the GAD was used) was 0.909. At baseline, participants were solely asked how often they felt anxious or worried (response options ranged from rarely to much/most of the time).
2.1.3.1. Previous mental health diagnosis.
Participants were asked if they had ever been diagnosed with specific mental health issues including depression, anxiety, PTSD, eating disorders, and ADD/ADHD. Participants who reported depression, anxiety, or PTSD were considered to have a previous relevant mental health diagnosis. Of note, everyone who indicated other mental health diagnoses (e.g., ADHD or eating disorders) also reported having been diagnosed with depression, anxiety, or PTSD.
2.1.3.2. Using substances to cope.
Participants were asked if they currently “use alcohol or other drugs to help [them] get through it.” Response options ranged from not at all to a lot.
2.2. Social support
Social support at 5-month follow-up was measured in three ways. First, using an item from the Behavioral Risk Factor Surveillance System (BRFSS), participants were asked “How often can you get the social and emotional support you need (response options: usually, often some-times, rarely) as a measure of the availability of support. Second, participants were asked “Have there been any changes in the amount you are reaching out to others for support since the beginning of the pandemic?” (response options: I’m reaching out more, less, about the same, or I have not needed support) to determine whether there had been changes in support seeking since the start of the pandemic. Finally, participants were asked how much they agreed with the statement, “I feel isolated” on a 1 (strongly disagree) to 7 (strongly agree) scale as a measure of isolation.
2.3. Analytic plan
We compared psychological distress indicators (depression, suicide risk, anxiety, and acute stress/PTSD) at baseline to five-month follow-up (N = 1567). To do so, we first conducted general linear models to examine changes from baseline to five-month follow-up using continuous scores for depression, suicide risk, and acute stress as the outcomes. Specific demographics (age, race/ethnicity, gender, SGM identity, relationship status, and household composition) were included in the models to test within-group changes over time. To examine predictors of potentially clinically significant levels of distress at 5-month follow-up, using logistic regression models models we controlled for baseline levels of distress for each variable (depression, suicide, PTSD risk) to test odds of a probable diagnosis of depression, risk of suicide (some risk to severe risk), and potential risk for PTSD. In Model 1, we included just baseline scores as the independent variable. In Model 2, we added in demographics (age, race/ethnicity, gender, SGM, household composition, relationship status, work loss at any wave) controlling for baseline scores. In Model 3 we added mental health and health behavior variables [baseline depression, whether or not they had ever received a mental health diagnosis, current anxiety, using substances to cope]. In Model 4, we added social support variables (availability of social support, changes in reaching out for social support, and isolation). In Model 5 we added COVID-related worries (worries related to the virus itself, worries about their health, worries about dying from the virus, worries about the future, and worries about managing work and children’s needs). As the strengths of associations varied very little across models, we report in tables solely the data from the final model (Model 5). Data from the other models is available upon request. All analyses were conducted using SPSS version 27.
3. Results
3.1. Baseline descriptives
More than 20% of the baseline sample reported at least one COVID-related symptom (e.g., shortness of breath, fever) at the time of the survey, and at five-month follow-up 22% reported knowing someone who had died of COVID-19. Among those who were employed prior to the pandemic, at baseline 30% had either lost a job, had work hours reduced, or had been furloughed. Almost 15% of respondents reported no longer getting paid. Food insecurity was a concern with 19% worrying they might run out of food and 16% worrying they could not adequately feed their children at baseline.
Together these factors likely increase risks for clinically significant distress. And indeed, more than half of respondents at baseline had CESD scores consistent with a probable diagnosis of depression (55.4%; See Fig. 1); of those, one-quarter reported no previous diagnosis of depression. Among the entire sample, 7.1% at baseline were at some or high risk of suicide. More than half (65.1%) of all participants reported feeling anxious three or more days a week. More than half of all respondents (56.7%) reported feeling at least somewhat isolated. (See Table 1.)
Fig. 1.
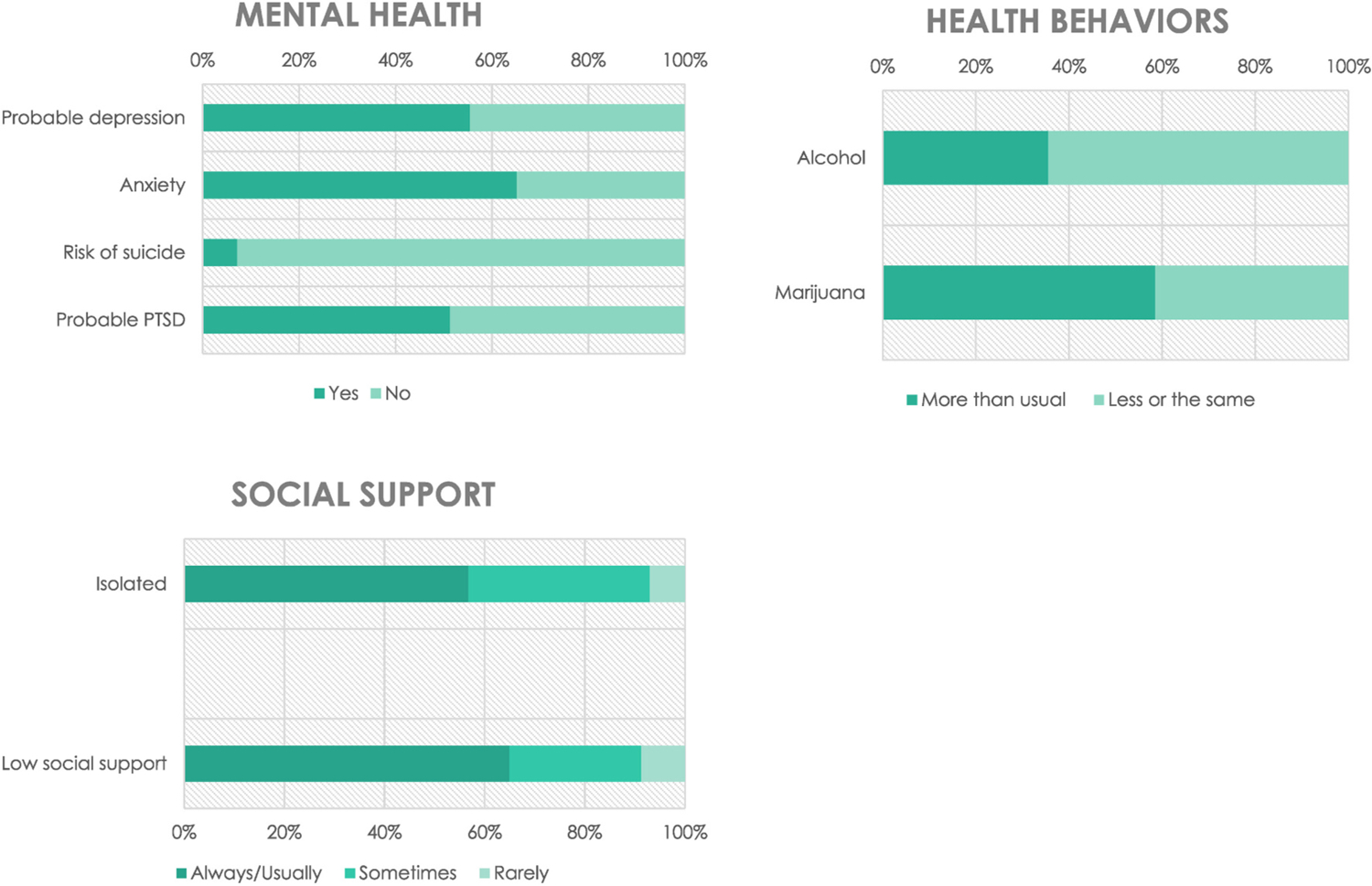
Baseline rates (from April 2020) of psychological distress concerns, social support, health behaviors, and sleep difficulties (N = 1567).
Table 1.
Description of the sample (N = 1567).
| % | |
|---|---|
| Age | |
| 18–30 | 38.0 |
| 31–40 | 31.8 |
| 41–50 | 14.2 |
| 51–65 | 12.3 |
| 66+ | 3.7 |
| Race/ethnicity | |
| White | 85.2 |
| Black | 1.7 |
| Latinx | 6.0 |
| Asian | 6.9 |
| Bi/multiracial | 0.2 |
| Gender | |
| Men | 11.8 |
| Women | 88.2 |
| Sexual or gender minority identity | 41.7 |
| Household composition | |
| Alone | 18.5 |
| With partner | 35.4 |
| With partner and children | 25.4 |
| Children, no partner | 4.7 |
| Other | 16.4 |
| Relationship status | |
| Single | 33.0 |
| Committed relationship | 67.0 |
| Lost job, laid off, furloughed (across all waves) | 33.1 |
| Ever received a mental health diagnosis | 58.9 |
Health behaviors were also impacted. More than one-third of all respondents (35%) reported currently using drugs or alcohol to help them cope. Of those who had drunk alcohol in the past week, more than one-third (35.6%) reported drinking alcohol more than usual and of those who reported past week marijuana use, more than half (55.1%) reported smoking more than usual.
3.2. Changes over time
We examined changes from baseline to five-month follow-up (see Figs. 2–4). There was a significant increase in depressive symptoms from baseline (M = 9.9, SE = 0.62) to 5-month follow-up (M = 11.2, SE = 0.654, p < .05) There were no significant within-group differences, however there was a possible trend in change over time by race/ethnicity (p = .072) and household composition (p = .079). There was a significant increase over time in suicidal thoughts and behaviors from baseline (M = 2.6, SE = 0.72) to 5-month follow-up (M = 4.89, SE = 0.91; p < .05). There were no significant differences in within-group effects of time on suicidal thoughts and behaviors, however there was a possible trend in change over time by race/ethnicity (p = .07). Using the modified version of the Impact of Events Scale-6 (Thoresen et al., 2010), we examined acute stress symptoms. We found that the average acute stress score decreased significantly from baseline (M = 9.7, SE = 0.511) to two-week follow-up (M = 8.5, SE = 0.526, p < .01). There were no within-group effects of time on IES scores.
Fig. 2.

Change in depression rates from baseline (April 2020) to 5-month follow-up (September 2020) by demographics (N = 1567).
Fig. 4.

Change in suicide risk from baseline (April 2020) to 5-month follow-up (September 2020) by demographics (N = 1567).
3.3. Predictors of distress at 5-month follow-up
3.3.1. Depression
See Table 2 for models examining 5-month mental health outcomes. Having CESD scores that could be indicative of a probable diagnosis of depression at baseline was associated with a five times higher odds of probable depression at 5-month follow-up (aOR 5.426, 95%CI 4.24, 6.94). This association was attenuated and no longer significant when all other variables were included in the model (aOR 2.047, 95% 0.794, 5.23). In the final model, the only significant predictors of 5-month depression were anxiety at 5-month follow-up (aOR 1.371; 95%1.20, 1.56); higher anxiety was associated with increased odds of depression and higher levels of worries about participants’ own health were associated with higher odds of depression (aOR 1.035, 95%CI 1.01, 1.06). Of note, in Model 2, participants who identified as SGM had higher odds of depression at 5-month follow-up (aOR 1.760, 95%CI 136, 2.28) and the higher odds for SGM individuals persisted across models until the social support at 5-month follow-up variables were added to the model. In Model 3, hopelessness was associated with higher odds of depression (aOR 1.189, 95%CI 1.13, 1.25) and being able to get needed social support was associated with lower odds of depression (aOR 0.226, 95% CI 0.09, 0.57). Interestingly, reporting that you neither agree nor disagree with the statement “I feel isolated” was associated with higher odds of depression, (aOR 1.1822, 95%CI 1.03, 3.22), but agreeing with the statement was not associated with higher odds of depression. This association was no longer significant when COVID-related worries at 5-month follow-up were added to the model.
Table 2.
Final logistic regression models of demographics, mental health, social support, and COVID-related worries on probable depression, suicide risk, and PTSD risk (N = 1567).
| Depression |
Suicide risk |
PTSD |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| aOR | 95% CI |
p |
aOR | 95% CI |
p |
aOR | 95% CI |
p |
||||
| Lower | Upper | Lower | Upper | Lower | Upper | |||||||
| Baseline mental health | 2.047 | 0.794 | 5.273 | 0.14 | 5.123 | 1.386 | 18.94 | 0.014 | 7.861 | 2.924 | 21.14 | 0 |
| Demographics | ||||||||||||
| Age | ||||||||||||
| 18–40 | 1 | 1 | 1 | |||||||||
| 41 and above | 1.96 | 0.792 | 4.849 | 0.15 | 1.809 | 0.421 | 7.766 | 0.425 | 1.783 | 0.705 | 4.511 | 0.222 |
| Race/ethnicity | ||||||||||||
| White | 1 | 1 | 1 | |||||||||
| Person of color | 2.021 | 0.347 | 11.76 | 0.43 | 0.09 | 0.015 | 0.554 | 0.009 | 0.516 | 0.108 | 2.471 | 0.408 |
| Gender | ||||||||||||
| Men | 1 | 1 | 1 | |||||||||
| Women | 0.27 | 0.046 | 1.57 | 0.15 | 0.463 | 0.038 | 5.623 | 0.545 | 0.237 | 0.042 | 1.325 | 0.101 |
| SGM (reference: Not SGM) | 0.858 | 0.337 | 2.185 | 0.75 | 0.485 | 0.138 | 1.711 | 0.261 | 1.272 | 0.896 | 1.807 | 0.179 |
| Household composition | ||||||||||||
| Alone | 1 | 1 | 1 | |||||||||
| With partner | 0.551 | 0.263 | 1.152 | 0.11 | 4.779 | 0.315 | 72.4 | 0.259 | 0.707 | 0.34 | 1.47 | 0.353 |
| With partner and kids | 1.011 | 0.463 | 2.208 | 0.98 | 0.205 | 0.012 | 3.465 | 0.272 | 0.826 | 0.38 | 1.794 | 0.629 |
| Kids, no partner | 0.8 | 0.317 | 2.018 | 0.64 | 3.783 | 0.476 | 30.05 | 0.208 | 1.911 | 0.76 | 4.805 | 0.169 |
| Other | 0.982 | 0.492 | 1.957 | 0.96 | 0.882 | 0.143 | 5.436 | 0.893 | 1.165 | 0.581 | 2.333 | 0.667 |
| Relationship status | ||||||||||||
| Single | 1 | 1 | 1 | |||||||||
| Committed relationship | 4.087 | 0.41 | 40.76 | 0.23 | 1.044 | 0.1 | 10.95 | 0.971 | 1.811 | 0.119 | 27.63 | 0.669 |
| Lost job, laid off, furloughed | 1.324 | 0.503 | 3.489 | 0.57 | 0.651 | 0.201 | 2.109 | 0.474 | 0.958 | 0.349 | 2.63 | 0.933 |
| Mental health | ||||||||||||
| Time 1 probable depression (reference: No depression) | 1.056 | 0.741 | 1.505 | 0.76 | 2.349 | 0.367 | 15.05 | 0.368 | 1.758 | 0.625 | 4.939 | 0.285 |
| Ever MH diagnosis (reference: No MH diagnosis ever) | 1.262 | 0.519 | 3.068 | 0.61 | 53.49 | 2.193 | 1304 | 0.015 | 0.518 | 0.193 | 1.384 | 0.19 |
| Hopelessness | 1.154 | 0.983 | 1.355 | 0.08 | 1.606 | 1.27 | 2.031 | 0 | 1.039 | 0.874 | 1.236 | 0.662 |
| Use substances to cope (reference: Does not use to cope) | 0.15 | 0.637 | 0.344 | 1.18 | 0.099 | 1.6 | 0.915 | 2.798 | 0.695 | 1.128 | 0.619 | 2.055 |
| Anxiety | 1.371 | 1.203 | 1.563 | 0 | 1.208 | 1.049 | 1.391 | 0.009 | 1.264 | 1.106 | 1.445 | 0.001 |
| Social support | ||||||||||||
| How often can you get the social and emotional support you need RIGHT NOW? | ||||||||||||
| Always | 1 | 1 | 1 | |||||||||
| Usually | 1.08 | 0.145 | 8.07 | 0.94 | 2.635 | 0.37 | 18.78 | 0.334 | 0.304 | 0.025 | 3.725 | 0.352 |
| Sometimes | 2.029 | 0.288 | 14.28 | 0.48 | 0.494 | 0.059 | 4.125 | 0.515 | 0.158 | 0.012 | 2.025 | 0.156 |
| Rarely | 0.621 | 0.054 | 7.198 | 0.7 | 0.85 | 0.357 | 2.024 | 0.714 | 0.593 | 0.037 | 9.544 | 0.713 |
| Isolation | ||||||||||||
| No | 1 | 1 | 1 | |||||||||
| Yes | 0.476 | 0.105 | 2.157 | 0.34 | 1.208 | 0.191 | 7.65 | 0.841 | 0.083 | 0.016 | 0.446 | 0.004 |
| Neither | 1.405 | 0.321 | 6.154 | 0.65 | 2.269 | 0.205 | 25.12 | 0.504 | 0.15 | 0.029 | 0.781 | 0.024 |
| Changes in the amount reaching for support | ||||||||||||
| More | 1 | 1 | 1 | |||||||||
| The same | 0.794 | 0.278 | 2.267 | 0.67 | 0.449 | 0.103 | 1.955 | 0.286 | 0.733 | 0.244 | 2.196 | 0.579 |
| Less | 0.934 | 0.277 | 3.145 | 0.91 | 1.132 | 0.29 | 4.426 | 0.859 | 0.392 | 0.108 | 1.424 | 0.155 |
| COVID-related worries | 0.984 | 0.961 | 1.008 | 0.19 | 0.974 | 0.945 | 1.004 | 0.091 | 1.001 | 0.977 | 1.025 | 0.94 |
| Virus-related worries | ||||||||||||
| Health worries | 1.035 | 1.011 | 1.059 | 0 | 1.002 | 0.976 | 1.03 | 0.857 | 0.996 | 0.973 | 1.019 | 0.708 |
| Worries about death | 0.992 | 0.974 | 1.009 | 0.36 | 0.999 | 0.978 | 1.02 | 0.924 | 1.009 | 0.992 | 1.027 | 0.289 |
| Future worries | 0.998 | 0.98 | 1.017 | 0.87 | 1.017 | 0.993 | 1.042 | 0.175 | 1.001 | 0.982 | 1.021 | 0.897 |
| Managing children and work | 1.004 | 0.991 | 1.017 | 0.56 | – | – | – | – | 0.998 | 0.985 | 1.011 | 0.757 |
NOTE: In the final model for suicide risk, worries related to managing child and work failed to work in the model and was deleted.
3.3.2. Suicide risk
Baseline risk for suicide was associated with a 12 times higher odds of risk for suicide at 5-month follow-up (aOR 12.287, 95%CI 5.697, 26.499) and this was attenuated but still significant at 5-month follow-up (aOR 9.862, 95%CI 3.245, 29.973). Of the mental health variables, ever having received a mental health diagnosis (aOR 7.402, 95%CI 1.20, 45.56), hopelessness at 5-month follow-up (aOR 1.606, 95%CI 1.27, 2.03), and 5-month follow-up anxiety (aOR 1.208, 95%CI 1.05, 1.39) were associated with suicide risk at 5-month follow-up. Notably, none of the social support or COVID-related worries were significantly associated with suicide risk. Using substances to cope (aOR 1.603, 95%CI 1.01, 2.55) was associated with significantly higher odds of suicide risk when mental health variables were added in and remained significant when social support was added, but was attenuated and no longer significant when COVID-related worries were added. Of note, in Model 2 (just demographics), participants who identified as people of color had lower odds of suicide risk compared to White participants (aOR 0.357, 95%CI 0.15, 0.84), this association was attenuated and marginally significant (p = .052) when the mental health variables were added in, and then no longer significant when the social support variables were added.
3.3.3. Risk for PTSD
Participants who were at probable risk for PTSD at baseline had almost eight times higher odds of risk for PTSD at 5-month follow-up (aOR 7.745 95%CI: 5.87, 10.22). In Model 5, risk for PTSD had increased (aOR 9.973, 95%CI 3.42, 29.06)tand was still significant. Controlling for baseline PTSD risk, higher levels of anxiety were associated with higher risk for PTSD (aOR 1.264, 95%CI 1.12, 1.46). Feeling isolated was associated with lower odds of PTSD risk, (aOR 0.083, 95% CI 0.16, 0.45). In Model 3, when the mental health variables were added in, using substances to cope (aOR 1.214, 95%CI 1.01, 1.46) was associated with higher odds of PTSD risk compared to participants who did not use substances to cope. This association was no longer significant when social support was added into the model. Identifying as a sexual or gender minority was associated with significantly higher odds of PTSD risk (aOR 1.476, 95%CI 1.12, 1.95) compared to participants who identified as cisgender and strictly heterosexual. This association was no longer significant when the mental health variables were added into the model.
4. Discussion
Together, our findings suggest high rates of depression, anxiety, acute stress, and other signs of distress like isolation, social support, and use of substances to cope. Although acute stress symptoms attenuated at five-month follow-up, depressive symptoms and suicidal thoughts and behaviors increased. Notably, at five-month follow up, even attenuated rates of distress were still alarmingly high.
Determining who is at highest risk—both acutely and over the longer term—is essential for prevention of distress and intervention to reduce risk of worsening or chronicity (Chen and Bonanno, 2020). Within-subject analyses show no significant demographic differences, however across models there is some suggestion of potentially elevated rates of distress such that sexual and gender minorities and people of color may be at higher risk, but more research is needed. Notably, during the study period, the Centers for Disease Control released their report that highlighted the racial/ethnic disparities in hospitalizations due to COVID, and that these disparities disproportionately affected Black and Latinx communities (Garg et al., 2020). Our findings may suggest that not only does COVID worsen racial/ethnic disparities in physical health, it may also heighten racial/ethnic disparities in mental health. It will be important to document changes over time, particularly how events like George Floyd’s and Breonna Taylor’s killings (as well as the killings of other people of color, particularly Black people), the protests, and the increased attention to injustice and inequality may impact wellbeing and potentially interact with the effects of the pandemic.
Our findings also suggest that specific factors may increase or decrease risks. Hopelessness, previous mental health diagnoses, using substances to cope, and anxiety may be associated with increased mental health risks, whereas having a usual source of support may serve as a buffer. These findings suggest modifiable targets for intervention such as helping people develop healthy coping skills and how to find hope during a global disaster.
Our study uses a convenience sample of respondents largely recruited through social media and may not be generalizable to the general population; nevertheless, these data provide a window into the state of psychological distress during the COVID-19 pandemic. Our findings suggest that because distress appears to have increased, there is a need to prioritize availability of, and access to, mental health care during both the pandemic and the recovery. Previous research on the long-term effects of pandemics and quarantining suggests that the end of the crisis does not necessarily bring an end to deleterious mental health effects (Brooks et al., 2020). Those affected may experience pandemic-related PTSD, depression, suicidality, and anxiety months—or even years—after the pandemic ends. Longitudinal research is critical for monitoring whether psychological distress abates, remains static, or worsens over time. It will also be important to measure social support and isolation in order to understand how these important buffers against stress may be undermined, or enhanced, by the pandemic and efforts at containing the pandemic.
Despite the strengths of this study, there are several limitations to consider when evaluating its generalizability. First, as noted above, this study relied on a convenience sample recruited largely through social media. As a result, the sample is less diverse than the general population and may be more distressed given that they were motivated to take part in a study on COVID-19 and wellbeing with no compensation for their participation. The latter also likely impacted our retention rates. The instruments were all self-report and thus objective measurements of distress and wellbeing were not captured; reports of distress may be influenced by some biases like social desirability. We chose to use the Impact of Events scale to be consistent with measurement of PTSD symptoms in previous studies on mental health during pandemics. However, because we were unable to find a relevant measure of peritraumatic PTSD (i.e., PTSD developing at the time of the potentially traumatic event), we decided to modify the scale to measure current distress related to COVID-19. Thus our scores may, or may not, be comparable to those from other studies. One strength of the study was that we were able to include whether participants had received a previous mental health diagnosis. We could not, however, account for whether they had a pre-pandemic substance use disorder which could have an influence on current substance use. We also, as the pandemic evolved, shifted our survey to include better measurement of concerns that seemed to be emerging, such as anxiety, sleep, and concentration. Thus, we could not test changes over time in anxiety as it was assessed solely with a single item at baseline and with the GAD at 5-month follow-up. There may be some overlap between symptoms of psychological distress and COVID. For example, difficulty breathing could be an indicator of COVID-19 or potentially of anxiety which may lead to a conflation of the reasons for symptoms. Our outcomes may also have bidirectional associations. For example, increased substance use may affect mood or suicidal thoughts and behaviors. In turn, feeling depressed may increase the likelihood of using substances to cope.
5. Conclusion
Any interventions created in response to the pandemic must include longer-term follow-up and must be accessible to those who have lost (or did not have) health insurance—as well as those with limited economic resources (Blunt et al., 2020; Walker et al., 2015; Saloner et al., 2017). Importantly, our data suggest that distress in the wake of the pandemic and associated unprecedented levels of uncertainty and loss is fairly ubiquitous and may be long-lasting. We would thus argue that psychological distress should not be treated as an individual-level issue (Veldhuis et al., 2021). Broad structural-level interventions to address the root causes of distress such as financial impacts, job loss, isolation, loss of childcare and school, loss of friends and family members to the virus, as well as the high levels of uncertainty (Brooks et al., 2020) about the future and anxiety about transmission should be addressed through universal screening, interventions, and policy initiatives (Veldhuis et al., 2021; Torous and Wykes, 2020; Shore et al., 2020; Gunnell et al., 2020; Campion et al., 2020).
Fig. 3.

Change in acute stress/probable PTSD rates baseline (April 2020) to 5-month follow-up (September 2020) by demographics (N = 1567).
Acknowledgements
Dr. Veldhuis’ work on this manuscript was supported by an NIH/ NIAAA Pathway to Independence Award (K99AA028049; C.B. Veldhuis, Principal Investigator). Dr. Nesoff’s work on this manuscript was supported by an NIH/NIDA grant (K01DA049900; E.D. Nesoff, Principal Investigator).
References
- Blunt EO, Maclean JC, Popovici I, Marcus SC, 2020. Public insurance expansions and mental health care availability. Health Serv. Res 55 (4), 615–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks SK, Webster RK, Smith LE, et al. , 2020. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395 (10227), 912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campion J, Javed A, Sartorius N, Marmot M, 2020. Addressing the public mental health challenge of COVID-19. Lancet Psychiatry 7 (8), 657–659. S2215036620302406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S, Bonanno GA, 2020. Psychological adjustment during the global outbreak of COVID-19: a resilience perspective. Psychol. Trauma Theory Res. Pract. Policy 12 (S1), S51–S54. [DOI] [PubMed] [Google Scholar]
- Coffey SF, Gudmundsdottir B, Beck JG, Palyo SA, Miller L, 2006. Screening for PTSD in motor vehicle accident survivors using the PSS-SR and IES*. J. Trauma. Stress 19 (1), 119–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conron KJ, Goldberg SK, 2020. LGBT people in the US not protected by state nondiscrimination statutes [Internet] In: UCLA School of Law Williams Institute. Available from: https://williamsinstitute.law.ucla.edu/wp-content/uploads/LGBT-Nondiscrim-Statutes-Mar-2019.pdf. [Google Scholar]
- Czeisler MÉ, Lane RI, Petrosky E, et al. , 2020. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. MMWR Morb. Mortal. Wkly Rep 69 (32), 1049–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia MA, Homan PA, García C, Brown TH, 2021. The color of COVID-19: structural racism and the disproportionate impact of the pandemic on older black and Latinx Adults. J. Gerontol. Ser. B 76 (3), e75–e80. 10.1093/geronb/gbaa114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg S, Kim L, Whitaker M, et al. , 2020. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 — COVID-NET, 14 states, march 1–30, 2020. MMWR Morb. Mortal. Wkly Rep 69 (15), 458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, 2020. COVID-19 and LGBT rights. Columbia Law Sch. Schol. Arch 99–108.
- Gravlee CC, 2020. Systemic racism, chronic health inequities, and COVID-19: A syndemic in the making? Am. J. Hum. Biol. [Internet] 32 (5). 10.1002/ajhb.23482. Available from:. [cited 2020 Nov 20]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruberg S, Madowitz M. Same-sex couples experience higher unemployment rates throughout an economic recovery [Internet]. Center for American Progress. LGBT Rights: 2020. Available from: https://www.americanprogress.org/issues/lgbtq-rights/news/2020/05/05/484547/sex-couples-experience-higher-unemployment-rates-throughout-economic-recovery/.
- Gunnell D, Appleby L, Arensman E, et al. , 2020. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry 7 (6), 468–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holingue C, Badillo-Goicoechea E, Riehm KE, et al. , 2020a. Mental distress during the COVID-19 pandemic among US adults without a pre-existing mental health condition: findings from American trend panel survey. Prev. Med 139, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holingue C, Kalb LG, Riehm KE, et al. , 2020b. Mental distress in the United States at the beginning of the 2019 Coronavirus Disease (COVID-19) pandemic. Am J Public Health 110, 1628–1634. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, Alvarez W, 1979. Impact of event scale: a measure of subjective stress. Psychosom. Med 41 (3), 209–218. [DOI] [PubMed] [Google Scholar]
- Hosey MM, Leoutsakos JMS, Li X, et al. , 2020. Screening for posttraumatic stress disorder in ARDS survivors: validation of the impact of event Scale-6 (IES-6) ( 10.1186/s13054-019-2553-z). Crit. Care 24 (1), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kantamneni N, 2020. The impact of the COVID-19 pandemic on marginalized populations in the United States: a research agenda. J. Vocat. Behav 119, 103439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keeter S, 2020. People financially affected by COVID-19 outbreak are experiencing more psychological distress than others. Pew Research Center
- Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J, 1993. Two shorter forms of the CES-D depression symptoms index. J. Aging Health 5 (2), 179–193. [DOI] [PubMed] [Google Scholar]
- Martin A, Markhvida M, Hallegatte S, Walsh B, 2020. Socio-economic impacts of COVID-19 on household consumption and poverty. Econ. Disast. Clim. Change 4 (3), 453–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattei G, Russo T, Addabbo T, Galeazzi GM, 2020. The COVID-19 Recession Might Increase Discriminating Attitudes Toward LGBT People and Mental Health Problems Due to Minority Stress, p. 2. [DOI] [PubMed]
- McGinty EE, Presskreischer R, Han H, Barry CL, 2020. Psychological Distress and Loneliness Reported by US Adults in 2018 and April 2020. JAMA [Internet] 324 (1), 93–94 [cited 2020 Jun 22];Available from: https://jamanetwork.com/journals/jama/fullarticle/2766941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Neill K, 2020. Economic vulnerabilities to COVID-19 among LGBT adults in California. [Internet]. UCLA School of Law Williams Institute Available from: https://williamsinstitute.law.ucla.edu/publications/covid-economics-lgbt-ca/.
- Pfefferbaum B, North CS, 2020. Mental health and the Covid-19 pandemic. N. Engl. J. Med 3. [DOI] [PubMed] [Google Scholar]
- Radloff LS, 1977. The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas 1 (3), 385–401. [Google Scholar]
- Rash CJ, Coffey SF, Baschnagel JS, Drobes DJ, Saladin ME, 2008. Psychometric properties of the IES-R in traumatized substance dependent individuals with and without PTSD. Addict. Behav 33 (8), 1039–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riehm KE, Holingue C, Kalb LG, et al. , 2020. Associations between media exposure and mental distress among U.S. adults at the beginning of the COVID-19 pandemic. Am. J. Prev. Med 55, 1–10. S0749379720302749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riehm KE, Holingue C, Smail EJ, et al. , 2021. Trajectories of mental distress among U.S. adults during the COVID-19 pandemic. Ann. Behav. Med 1–10. [DOI] [PMC free article] [PubMed]
- Rodriguez LM, Litt DM, Stewart SH, 2020. Drinking to cope with the pandemic: the unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women. Addict. Behav 110, 106532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romero AP, Goldberg SK, Vasquez LA, 2020. LGBT People and Housing Affordability, Discrimination, and Homelessness. UCLA School of Law Williams Institute
- Saloner B, Bandara S, Bachhuber M, Barry CL, 2017. Insurance coverage and treatment use under the affordable care act among adults with mental and substance use disorders. Psychiatr. Serv 68 (6), 542–548. [DOI] [PubMed] [Google Scholar]
- Shore JH, Schneck CD, Mishkind MC, 2020. Telepsychiatry and the coronavirus disease 2019 pandemic—current and future outcomes of the rapid virtualization of psychiatric care. JAMA Psychiatry [Internet] 77 (12), 1211–1212 [cited 2020 Jun 24]; Available from: https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2765954. [DOI] [PubMed] [Google Scholar]
- Smail EJ, Riehm KE, Veldhuis CB, et al. , 2020. Associations of family structure and presence of children in the household with mental distress during the COVID-19 pandemic. PsyArxiv [Internet] 1–28. Available from: https://psyarxiv.com/8qm7s/. [DOI] [PMC free article] [PubMed]
- Spitzer RL, Kroenke K, Williams JBW, Löwe B, 2006. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med 166 (10), 1092. [DOI] [PubMed] [Google Scholar]
- Thoresen S, Tambs K, Hussain A, Heir T, Johansen VA, Bisson JI, 2010. Brief measure of posttraumatic stress reactions: impact of event Scale-6. Soc. Psychiatry Psychiatr. Epidemiol. 45 (3), 405–412. [DOI] [PubMed] [Google Scholar]
- Torous J, Wykes T, 2020. Opportunities from the Coronavirus Disease 2019 pandemic for transforming psychiatric care with telehealth. JAMA Psychiatry [Internet] 77, 1205–1206 [cited 2020 Jun 24];Available from: https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2765953. [DOI] [PubMed] [Google Scholar]
- van Spijker BAJ, Batterham PJ, Calear AL, et al. , 2014. The suicidal ideation attributes scale (SIDAS): community-based validation study of a new scale for the measurement of suicidal ideation. Suicide Life Threat. Behav 44 (4), 408–419. [DOI] [PubMed] [Google Scholar]
- Veldhuis CB, Stuart E, Fallin MD, 2021. Five urgent public health policies to combat the mental health effects of COVID-19 [Internet]. Health Affairs Blog 10.1377/hblog20210122.959001/full/ [cited 2021 Feb 12]; Available from: [DOI]
- Walker ER, Cummings JR, Hockenberry JM, Druss BG, 2015. Insurance status, use of mental health services, and unmet need for mental health Care in the United States. Psychiatr. Serv 66 (6), 578–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson BDM, Conron KJ, 2020. National Estimates of Food Insecurity: LGBT People and COVID-19. UCLA School of Law, The Williams Institute. [Google Scholar]


