Abstract
Background:
Food insecurity dramatically increased due to the COVID-19 pandemic; however, little is known about pandemic-related food insecurity in households with dietary restrictions.
Objective:
Examine pre-pandemic rates of and pandemic-related change in food insecurity among households with and without dietary restrictions.
Methods:
Cross-sectional, panel-based survey of 3,200 U.S. women conducted in April 2020. Pre-pandemic food insecurity and early pandemic-related change in food insecurity were assessed using the adapted Hunger Vital Sign™. Weighted, multivariate logistic regression was used to model the odds of pre-pandemic food insecurity and the odds of incident or worsening pandemic-related food insecurity among households with and without dietary restrictions. In models predicting pandemic-related outcomes, interaction effects between race/ethnicity and dietary restrictions were examined.
Results:
Prior to the COVID-19 pandemic, households with self-reported food allergy (aOR 1.5, 95% CI 1.2–1.9), celiac disease (aOR 2.3, 95% CI 1.4–3.5), or both (aOR 2.1, 95% CI 1.2–3.6) were significantly more likely to be food insecure than households without restrictions. Households with dietary restrictions were also significantly more likely to experience incident or worsening food insecurity during the early pandemic (food allergy: aOR 1.6, 95% CI 1.3–2.1) (celiac disease: aOR 2.3, 95% CI 1.5–3.5) (both: aOR 2.0, 95% CI 1.2–3.4). Race/ethnicity was not a significant moderator of the relationship between dietary restrictions and pandemic-related food insecurity.
Conclusion:
Households with dietary restrictions were more likely to experience both pre-pandemic and pandemic-related incident or worsening food insecurity than households without restrictions. Clinical care for patients with dietary restrictions requires attention to food insecurity.
Keywords: food allergy, celiac disease, dietary restrictions, food insecurity, social determinants of health, COVID-19, pandemic, race/ethnicity
INTRODUCTION:
Food insecurity is a prevalent, yet preventable, social determinant of various health outcomes and healthcare utilization.1–4 Household food insecurity is defined as an economic and social condition in which households lack adequate or consistent access to food.5 Prior to the COVID-19 pandemic, 11.1% of the U.S. population was food insecure6 and households with food allergies were at higher risk of food insecurity than households without.7 During the COVID-19 pandemic, early analyses suggest rates of food insecurity have doubled overall and tripled among households with children.8 However, little is known about how the COVID-19 pandemic will further impact food insecurity among an already vulnerable population with dietary restrictions.
Individuals with food allergy (FA) or celiac disease (CeD) diagnoses face additional barriers to securing safe and adequate foods.9–13 FA is a chronic condition affecting 7% of U.S. children14 and 11% of U.S. adults15 characterized by an adverse immune-mediated response upon exposure to a given food. Dietary elimination of the allergen is essential to prevent life-threatening allergic reactions. CeD is an autoimmune disease affecting 1% of the U.S. population, in which consumption of gluten elicits an inflammatory response that damages the lining of the small intestine.16 Currently, a gluten-free diet is the only available treatment for patients with CeD. Both FA and CeD require dietary elimination of specific foods and expensive substitutions to maintain healthy nutrition and growth.9,10 Prior literature suggests that households with FA were more likely to experience food insecurity than households without;7 however, we find no studies examining the relationship between CeD and household food insecurity.
On March 11, 2020, the World Health Organization declared COVID-19 a global pandemic.17 As a result of the pandemic and efforts to contain it, the U.S. unemployment rate increased dramatically18 and negatively impacted people’s ability to purchase food.19 Moreover, both travel and business restrictions disrupted the transport and processing of food, resulting in increased delivery times and reduced global food availability.20 School closures are also suspected to exacerbate existing inequalities and have detrimental health consequences for children in households that rely on school meals to fill food gaps.21 Many families have turned to local charitable organizations for assistance, but food banks across the country are experiencing volunteer labor shortages and reduced donations.22 The COVID-19 crisis has exacerbated rates of food insecurity,8 but little is known about how the added restriction of a FA or CeD diagnosis may further impact food access.
Furthermore, it is likely that the burden of pandemic-related food insecurity in households with dietary restrictions is not equally distributed among racial or ethnic groups. Prior to the pandemic, not only were FA households more likely to be food insecure compared to non-restricted households, but Black children with food allergy were significantly more likely to experience low food security compared to White children with food allergy.7 There is also growing evidence that the COVID-19 crisis is widening existing racial disparities in food insecurity. Black and Hispanic households with children are nearly twice as likely as White families to struggle with food insecurity during the pandemic (41% and 37% versus 23%).23 One reason Black and Hispanic households may be at higher risk of food insecurity than White households is spatial inequality, or the unequal distribution of food stores across communities.24 With less options for supermarkets and fresh produce in communities of color compared to White neighborhoods,25–27 we hypothesized that race would moderate the relationship between dietary restrictions and pandemic-related incident or worsening food insecurity. In other words, the relationship between food insecurity and food restriction would be stronger among racial and ethnic minorities due to the compounding effects of structural inequities.
We used data from the National Women’s Health COVID-19 Study to examine differences in pre-pandemic prevalence of food insecurity among households with and without dietary restrictions. We also examined differences in incident or worsening food insecurity during the early phase of the pandemic among households with and without dietary restrictions. We hypothesized that, in the early phase of the pandemic, households with any type of dietary restriction would be more likely to experience incident or worsening food insecurity than households without dietary restrictions. As a secondary hypothesis, we predicted race/ethnicity would be a significant moderator of the relationship between household dietary restrictions and pandemic-related food insecurity.
METHODS:
Study Participants
The details of the survey sample for National Women’s Health COVID-19 Study have been previously described.28 Between April 10 and April 24, 2020, a U.S. national sample of adult women was recruited using the Opinions 4 Good (Op4G) Health Care Panel.29 Op4G is a philanthropic market research company whose panels of participants have been used in prior peer-reviewed studies.28,30,31 Op4G maintains sociodemographic and health characteristics for each panelist to facilitate targeted recruitment of eligible individuals for future studies. The Op4G Health Care Panel is comprised of 350,000+ members recruited pre-pandemic using a combination of methods including non-profit community partners, web campaigns, and word of mouth. A nested quota sampling strategy was used to ensure the sample distribution of age and educational attainment matched 2018 population estimates.32 The objective of the National Women’s Health COVID-19 Study was to examine the impact of the pandemic on women’s health and health related socioeconomic risks and if these impacts varied by racial and ethnic groups; to meet these objectives, the quota oversampled East/Southeast Asian women given the risk of potential disproportionate impacts to this particular population.33,34 Women who did not speak English or were <18 years old were excluded from the study. Of the 3,634 eligible persons contacted, the online survey was completed by 3,200 respondents (an 88% cooperation rate).35 Utilizing a research panel rather than other available survey methods allowed us to recruit a diverse sample, yield high participation rates, and quickly assess early pandemic-related changes. This study was approved by the University of Chicago Institutional Review Board (IRB20–0489). Informed consent was documented electronically using the online survey form and respondents received $4 in compensation.
Survey Design and Measures
The self-administered, web-based survey collected basic sociodemographic and household characteristics. FA status was determined using the question: “does anyone in your household have a physician-diagnosed food allergy?” Similarly, CeD status was determined using the question: “Has a doctor or other health professional ever told anyone in your household that they have celiac (sele-ak) disease, also called sprue (sproo)?” For both questions, respondents could choose from the options: yes, no, don’t know, or refuse. Race/ethnicity was determined using two questions: “What race do you consider yourself to be? Please select one or more.” (White, Black or African American, American Indian or Alaskan Native, Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, other Asian, Pacific Islander or other) and “Do you consider yourself to be Hispanic, Latino/a/x or of Spanish origin” (yes or no). Women who selected American Indian or Alaskan Native, Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, other Asian, Pacific Islander, other, or multiple races were categorized as “Other.” Additional measures were included to assess respondent general and mental health.36,37
Pre-pandemic food insecurity was assessed using 2-items adapted from the validated Hunger Vital Sign™ (HVS) screener.38 The measures were preceded by the statement: “Some people have made the following statements about their food situation. Please answer whether the statements were often, sometimes, or never true for you and your household in the 12 months before the coronavirus pandemic.” Earlier in the survey, the start of the coronavirus pandemic was defined according to the World Health Organization declaration on March 12, 2020. HVS™ measures were individually modified (notated in bold) to probe specifically for pre-pandemic food insecurity: “In the 12 months before the coronavirus pandemic, you worried that your food would run out before you got money to buy more” and “In the 12 months before the coronavirus pandemic, the food you bought just didn’t last and you didn’t have money to get more.” A response of “often true” or “sometimes true” to either item was considered a positive screen. Change in food insecurity was determined using a single question adapted (in bold) from the HVS™: “How has your worry about food running out before you got money to buy more changed since the start of the coronavirus pandemic?” Responses were collected using a 5-point Likert scale (much more to much less worried) and dichotomized into more versus same or less. Responses were dichotomized to ensure adequate sample size and to specifically highlight worsening pandemic-related change in household food insecurity status. Nonresponse rates for individual measures ranged from 0 to 2.5% (median 0.2%).
Statistical Analysis
We adjusted sample weights using the raking-ratio method39 to correct for any imbalances in the marginal distributions of age group (18–24 years, 25–44 years, 45–64 years, ≥65 years), race (Asian, Black, Other, White), education (high school or less, more than high school), income category (<$25,000, $25,000-$49,000, $50,000-$99,999, ≥$100,000), and region (Midwest, Northeast, South, West) using 2018 U.S. population data for adult women.32 All analyses were performed using survey weights. Of the 3,200 survey respondents, 54 responses were excluded from analyses (24 respondents did not answer the income measure used to calculate survey weights and 30 respondents did not answer one or both of the FA/CeD measures). Respondents who answered yes to both the FA and CeD measures (n=97) were included in all three dietary restriction groups: FA, CeD, and both CeD and FA. Each dietary restriction group was compared to households with no dietary restrictions.
We described respondent sociodemographic, household, and health characteristics stratified by household dietary restriction status and used chi squared tests to examine bivariate associations between these characteristics and each type of household dietary restriction. Next, we used multivariate logistic regression to model: (1) the odds of pre-pandemic food insecurity, (2) the odds of early pandemic-related incident or worsening food insecurity, and (3) the odds of early pandemic-related incident or worsening food insecurity with race/ethnicity included as an interaction variable. In all models, the primary predictor of interest was household dietary restriction status, with no restrictions as the reference group. Models controlled for the following sociodemographic, household, and health characteristics: race/ethnicity, education, income, marital status, region, self-rated general health and mental health (categorical variables) and household size and number of children (continuous variables). Model results are presented as adjusted odds ratios (aOR) with 95% confidence intervals. All analyses were performed using Stata software, version 16.1.
RESULTS:
Sample Characteristics
Table I summarizes the weighted individual- and household-level characteristics of survey respondents by self-reported household dietary restriction status (see Table E1 in the Online Repository to compare weighted and unweighted demographic data). Of 3,146 respondents, 17% of women indicated someone in their household had a physician-diagnosed FA, 5% of women indicated someone in the household had a diagnosis of CeD, and 4% of women indicated both were true. In bivariate analyses, race/ethnicity, household size, number of household children, and respondent self-rated general and mental health were significantly associated with at least one of the household dietary restrictions (p<0.10).
TABLE I.
Weighted sample sociodemographic, household, and self-rated health characteristics
| No restriction |
FA |
CeD |
Both FA and CeD |
||||
|---|---|---|---|---|---|---|---|
| Characeteristic | N = 2577 (82.0%) | N = 522 (17.0%) | P | N = 140 (5.4%) | P | N = 97 (3.9%) | P |
| Race/ethnicity. n (%) | |||||||
| White | 1622 (67.6) | 274 (55.0) | <.01 | 68 (51.5) | <.01 | 50(55.5) | <.01 |
| Black | 309 (9.9) | 81 (14.0) | 15 (9.6) | 7 (6.6) | |||
| Hispanic | 290(12.6) | 92 (19.5) | 37 (26.0) | 25 (27.4) | |||
| Other | 356 (9.9) | 75(11.5) | 20(12.9) | 15 (10.5) | |||
| Education level. n (%) | |||||||
| High school or less | 986 (37.1) | 185 (37.0) | .93 | 56(45.1) | .10 | 39 (43.9) | .25 |
| More than high school | 1591 (62.9) | 337 (63.0) | 84 (54.9) | 58 (56.2) | |||
| Household income, n (%) | |||||||
| <25K | 597 (19.1) | 136(21.7) | .69 | 35 (21.7) | .68 | 23 (20.1) | .54 |
| 25K–49K | 839(21.4) | 154 (20.6) | 43 (20.0) | 26(17.1) | |||
| 50K–99K | 789 (30.2) | 160 (29.3) | 41 (26.1) | 31 (27.3) | |||
| ≥100K | 352 (29.3) | 72 (28.4) | 21 (32.5) | 17 (35.5) | |||
| Marital status, n (%) | |||||||
| Married/partnered | 1512 (62.9) | 292 (58.9) | .15 | 78 (58.5) | .48 | 55 (59.6) | .69 |
| Single | 1063 (37.1) | 229(41.1) | 62 (41.5) | 42 (40.4) | |||
| Household size, n (%) | |||||||
| Lives alone | 468 (16.2) | 69(12.4) | <.01 | 24(16.1) | <.10 | 16(17.7) | <.01 |
| Self + 1 | 886 (36.1) | 138 (15.9) | 35 (24.1) | 20(15.6) | |||
| Self + 2 or more | 1214 (47.8) | 313 (61.7) | 80 (59.8) | 60 (66.8) | |||
| No. of household children. n (%) | |||||||
| 0 children | 1152 (57.9) | 200 (45.5) | <.01 | 45 (38.8) | <.01 | 30 (36.2) | <.01 |
| 1 child | 437 (19.1) | 120 (25.0) | 34 (27.2) | 21 (23.6) | |||
| 2 or more children | 4% (23.1) | 127 (29.5) | 36 (34.0) | 29(40.2) | |||
| Region, n (%) | |||||||
| Midwest | 587 (21.2) | 103 (18.7) | .70 | 26 (14.3) | .45 | 17(13.3) | .42 |
| Northeast | 514(17.3) | 107 (16.8) | 25 (17.7) | 20(21.2) | |||
| South | 1024 (38.0) | 214(39.1) | 57 (41.5) | 37 (39.4) | |||
| West | 452 (23.6) | 98 (25.4) | 32 (46.5) | 23 (26.1) | |||
| Self-rated general health. n (%) | |||||||
| Excellent or very good | 1078 (45.1) | 185 (34.3) | <.01 | 55 (37.5) | .24 | 24 (33.3) | <.10 |
| Good | 999(37.1) | 202 (39.3) | 54 (39.3) | 37 (40.7) | |||
| Fair or poor | 494(17.8) | 132 (26.4) | 31 (23.2) | 36 (26.0) | |||
| Self-rated mental health. n (%) | |||||||
| Excellent or very good | 1246 (52.7) | 227 (43.4) | <.01 | 60 (43.2) | .12 | 43 (44.9) | .25 |
| Good | 841 (30.3) | 149 (28.6) | 45 (32.3) | 29 (30.0) | |||
| Fair or poor | 480(17.1) | 145 (28.0) | 35 (24.5) | 25 (25.1) |
Percentages were calculated using calibration weights generated based on the following variables: age, race, education, income, and region.
CeD, Celiac disease: FA, food allergy.
Pre-Pandemic Food Insecurity
Overall, 37% of households in our sample were food insecure. Households with dietary restrictions reported higher rates of pre-pandemic food insecurity (47% FA, 56% CeD, and 53% both) than households with no dietary restrictions (35%) and these differences were significant in bivariate analyses (p<0.01). Figure I illustrates the adjusted odds of experiencing food insecurity prior to the COVID-19 pandemic for households with FA, CeD, and both compared to households without dietary restrictions (see Table E2 in the Online Repository for full model). Overall, all three dietary restriction groups were significantly more likely to experience pre-pandemic food insecurity compared to households with no restriction (FA: aOR 1.5, 95% CI 1.2–1.9; CeD: aOR 2.3, 95% CI 1.4–3.5; Both: aOR 2.1, 95% CI 1.2–3.6).
FIGURE I.
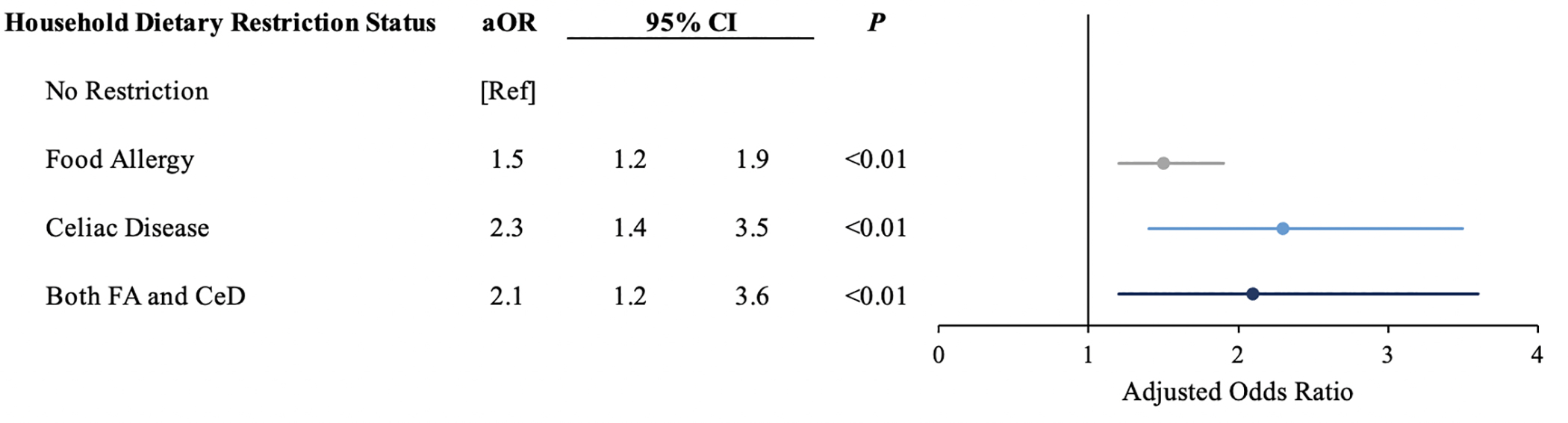
Odds of Pre-Pandemic Food Insecurity
Analyses are adjusted for race/ethnicity, education, household income, marital status, household size, number of household children, region, and respondent self-rated general and mental health.
Pandemic-Related Food Insecurity
Figure II depicts the likelihood of experiencing new or worsening food insecurity after the start of the COVID-19 pandemic by household dietary restriction type (see Table E3 in the Online Repository for full model). Households with FA (aOR 1.6, 95% CI 1.3–2.1), CeD (aOR 2.3, 95% CI 1.5–3.5), or diagnoses of both (aOR 2.0, 95% CI 1.2–3.4) were all significantly more likely to experience incident or worsening food insecurity when compared to households without restrictions. Race/ethnicity was not found to have a significant interaction effect with any of the three dietary restriction types (Table II).
FIGURE II.
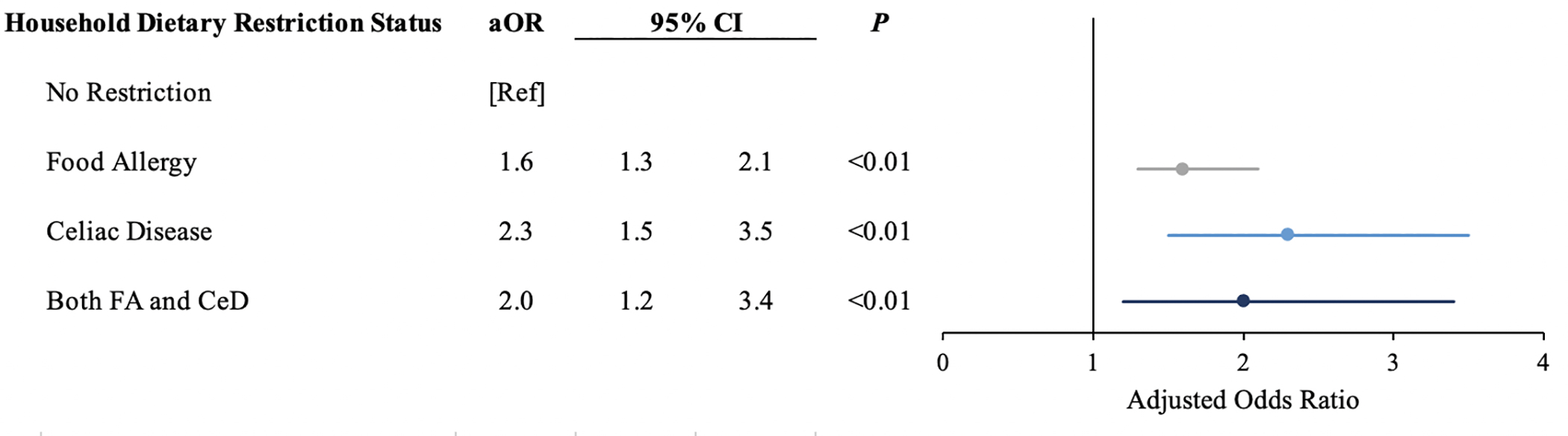
Odds of Pandemic-Related Incident or Worsening Food Insecurity
Analyses are adjusted for race/ethnicity, education, household income, marital status, household size, number of household children, region, and respondent self-rated general and mental health.
TABLE II.
Interaction effects between race/ethnicity and household dietary restriction status in models predicting pandemic-related incident or worsening food insecurity
| Race/ethnicity | Household dietary restriction |
|||||
|---|---|---|---|---|---|---|
| FA |
CeD |
Both FA and CeD |
||||
| aOR (95% Cl) | P | aOR (95% Cl) | P | aOR (95% Cl) | P | |
| White | [Ref] | [Ref] | [Ref] | |||
| Black | 1.1 (0.6–2.3) | .72 | 1.1 (0.3–4.1) | .91 | 1.2 (0.2–10.3) | .84 |
| Hispanic | 1.8 (0.9–3.5) | .11 | 0.9 (0.3–2.8) | .88 | 0.6 (0.2–2.4) | .50 |
| Other | 1.3 (0.6–2.7) | .45 | 3.6 (1.0–13.6) | .06 | 2.3 (0.5–9.7) | .26 |
Analyses are adjusted for race/ethnicity, education, household income, marital status, household size, number of household children, region, and respondent self-rated general and mental health.
aOR, Adjusted odds ratio; CeD, celiac disease; CI, confidence interval; FA, food allergy.
DISCUSSION:
These national data show that in the early phase of the COVID-19 pandemic, households with each type of dietary restriction (FA, CeD, and both) were significantly more likely than households without dietary restrictions to experience pandemic-related incident or worsening food insecurity. Race/ethnicity was not found to be a significant moderator of this relationship. Our study provides an early look at the impact of COVID-19 on households with food restrictions, while also filling important knowledge gaps about the pre-pandemic prevalence of food insecurity in households with restrictions. We found that prior to the pandemic, households with FA, CeD, or both were all more likely to be food insecure than households without restrictions.
Brown et al.40 outlines important shortcomings in federal and state nutrition policy that help explain our key pandemic-related findings. Despite efforts made through the Families First Coronavirus Response Act to expand nutrition benefits offered by the Supplemental Nutrition Assistance Program (SNAP) and the Special Supplemental Nutrition Program for Women, Infants and Children (WIC), this policy failed to address the increased cost and decreased availability of allergen/gluten-free products.9,11,12 On a local level, families relying on emergency assistance programs, such as food pantries or soup kitchens, were limited by temporary location closures and lack of allergen/gluten-free options. Brown et. al noted that of the 60,000 food pantries and soup kitchens around the country, only 4 consistently stock allergen-free foods and only 2 were operational during the early months of the pandemic.40 Many organizations are also implementing boxed food distribution protocols,40 further limiting options for families and resulting in unnecessary food waste in resource-limited setting. Many families with restrictions also rely on online shopping and delivery to purchase necessary specialty items. Early in the pandemic, postal package delivery and grocery delivery services were inundated with orders; this resulted in increased shipping delays and further restricted access to food.41,42 The COVID-19 pandemic compromised our national food system in ways that uniquely disadvantaged families with dietary restrictions.
We hypothesized that, given structural inequities such as the limited distribution of supermarkets in communities of color compared to White neighborhoods,25–27 race and ethnicity would moderate the relationship between household food restriction and pandemic-related food insecurity. However, we were surprised to find that the relationship between household dietary restrictions and pandemic-related food insecurity was similar across all racial and ethnic subgroups. One possible explanation is that households who are food insecure have similarly limited access to food in their communities, regardless of race or ethnicity. It is also possible that our secondary analyses had insufficient power to detect small, but important moderation effects. Despite our findings, we argue that race and ethnicity should be considered when addressing food insecurity among those with food restrictions. After controlling for other social and economic factors, people identifying with minority racial and ethnic groups are still at higher risk of experiencing food insecurity compared to Whites.43 Prior studies have outlined that ways in which race- and ethnicity-based discrimination and racism within our systems of housing, criminal justice, and employment contribute to disparities in rates of food insecurity.44,45 Though our data did not demonstrate a moderating effect by race, these structural factors cannot be overlooked in the treatment of patients with dietary restrictions.
In addition to describing pandemic-related changes in food insecurity, our findings support prior pre-pandemic studies of FA7 and uncover a similar trend in CeD households. To our knowledge, no other studies have examined the relationship between CeD and food insecurity. In fact, a number of studies suggest CeD diagnoses are more common in high socioeconomic households.46,47 However, the data regarding socioeconomic status and formal CeD diagnosis are conflicting.48,49 Our study showed no significant bivariate relationship between household income, educational attainment, or marital status with any of the household dietary restriction types. Studies analyzing administrative claims data have documented that families accrue significant costs associated with diagnosis, treatment, and follow-up for CeD when compared to matched controls.50–52 These costs are in addition to those acquired from adhering to a gluten-free diet.13 It is possible the added financial strain associated with CeD diagnosis and treatment makes it harder for households to afford food.
Further research is needed to understand the unique barriers FA and CeD households encounter in accessing safe foods. Many studies evaluating food insecurity intervention outcomes fail to collect data from their sample regarding dietary restrictions.53–55 Without data, it becomes impossible to evaluate whether food insecurity interventions are equally as effective for food restricted households as they are for households without restrictions. Moreover, some studies exclude FA patients entirely from their intervention.56 Our data suggest that excluding food restricted patients from intervention studies may disadvantage people who are at highest risk of food insecurity.
We acknowledge limitations to these findings. Although our dataset closely resembles U.S. population data for women,28 our findings are limited in generalizability by the use of a panel-based, quota sample rather than a probability sample. Our use of an online survey may underestimate food insecurity by excluding a small subset of households with limited internet access – a more prevalent condition among Black and Hispanic households than in White and Asian households.57 At the same time, our findings may overestimate the prevalence of food insecurity in the general population as single woman-headed households have higher rates of food insecurity than their male counterparts.6 To mitigate this limitation, we accounted for marital status, household size, and number of children in all multivariate analyses. The timing of the survey, which was relatively early in the pandemic, April 2020, may be a limitation in this study as an increasing number of households may experience food insecurity as the pandemic continues. In addition, dietary restriction status was determined by respondent self-reporting a medical diagnosis. Self-report of a medical diagnosis may over- or underestimate the true prevalence of these conditions.58 Since we are considering household-level estimates rather than individual-level estimates, we anticipated our estimates would be higher than previously reported individual-level estimates for the average U.S. adult.15,16,59 Our study may be limited by sample size, in particular for analyses with smaller subgroups; the overall study was designed to ensure reasonably precise estimates in subgroups of interest for the primary objectives of the National Women’s COVID Health Study (i.e., racial/ethnic groups).28 However, in a post-hoc analysis calculating the minimally detectable difference between those with no food restriction and those with both food allergy and celiac disease (our smallest comparison group), given 35% of the sample with no food restrictions were food insecure, we were powered to detect a difference in proportion of food insecurity between groups of 14% (power=0.80, alpha=0.05). Similarly, for the subgroup of the sample with celiac disease (5.4%), we calculate a minimally detectable difference between households with no food restrictions and those with celiac disease of 12%. All analyses are weighted based on age, race, education, income, and region to reduce the effects of selection bias in the sample. We also did not collect data on the type or number of household food allergies, which might modulate food accessibility or financial burden of the restriction.60
In summary, we have demonstrated that households with dietary restrictions were more susceptible to both pre-pandemic food insecurity and pandemic-related new or worsening food insecurity when compared to households without restrictions. This study has important policy implications regarding how best to minimize the impact of the COVID-19 pandemic and create equitable food assistance programs. Our study also underscores the importance of addressing food insecurity among FA and CeD patients, as the economic burden of an allergen/gluten-free diet may be underestimated.
HIGHLIGHTS BOX:
1. What is already known about this topic?
A food allergy or celiac disease diagnosis requires dietary elimination of specific foods and creates unique barriers to obtaining adequate nutrition.
2. What does this article add to our knowledge?
This is the first study to examine patterns of food insecurity by household dietary restriction status in the context of a global pandemic.
3. How does this study impact current management guidelines?
Our findings reinforce the importance of routine household food insecurity screening among patients diagnosed with food allergy or celiac disease.
ACKNOWLEDGEMENTS:
We acknowledge the following individuals from the University of Chicago for their role in the development of U.S. Women’s Health COVID19 Survey: Stacy Tessler Lindau, MD, MAPP; Kate E. Doyle, MPH; Kelly Boyd, BS; Sadia Haider, MD, MPH; Nita Karnik Lee, MD, MPH; Jennifer Makelarski, PhD, MPH; El Pinkerton, MPH; L. Philip Schumm, MA; Marie Tobin, MD; Kristen Wroblewski, MS; Ernst Lengyel, MD, PhD.
Funding: This work was supported by the Pritzker Summer Research Program, Paul and Mary Yovovich, and grants 5R01AG064949 (ST Lindau and E Huang, PIs) and 5R01MD012630 (ST Lindau, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Material support for this survey was provided by the Joseph B. De Lee Endowment to the University of Chicago Department of Obstetrics and Gynecology.
Conflicts of Interest: S.T.L. directed a Center for Medicare and Medicaid Innovation Health Care Innovation Award (1C1CMS330997–03) called CommunityRx. This award required development of a sustainable business model to support the model test after award funding ended. To this end, S. T. Lindau is founder and co-owner of NowPow, LLC. Neither the University of Chicago nor the University of Chicago Medicine is endorsing or promoting any NowPow entity or its business, products, or services. Dr. Lindau is also a contributor to UpToDate, Inc. The rest of the authors declare that they have no relevant conflicts of interest.
ABBREVIATIONS:
- FA
Food Allergy
- CeD
Celiac Disease
- Op4G
Opinions for Good
- HVS
Hunger Vital Sign™
- aOR
Adjusted Odds Ratio
Appendix
E1.
Sociodemographic, household, and self-rated health characteristics for unweighted and weighted sample
| Unweighted Sample N=2577 |
Weighted Sample N=2577 |
||
|---|---|---|---|
|
| |||
| N | % | % | |
|
| |||
| Race/Ethnicity | |||
| White | 1914 | 60.9 | 62.3 |
| Black | 398 | 12.7 | 10.6 |
| Hispanic | 394 | 12.5 | 13.9 |
| Other | 436 | 13.9 | 10.3 |
| Education level | |||
| High school or less | 1188 | 37.8 | 37.2 |
| More than high school | 1954 | 62.2 | 62.8 |
| Household income | |||
| < 25K | 745 | 23.7 | 19.6 |
| 25K – 49K | 1010 | 32.2 | 21.3 |
| 50K – 99K | 959 | 30.5 | 30.0 |
| ≥ 100K | 428 | 13.6 | 29.1 |
| Marital status | |||
| Married/P artnered | 1827 | 58.2 | 62.2 |
| Single | 1312 | 41.8 | 37.8 |
| Household size | |||
| Lives alone | 545 | 17.4 | 15.5 |
| Self+1 | 1039 | 33.2 | 34.5 |
| Self+2 or more | 1547 | 49.4 | 50.0 |
| Number of Household Children | |||
| 0 children | 1367 | 53.3 | 55.6 |
| 1 child | 570 | 22.2 | 20.3 |
| 2 or more children | 630 | 24.5 | 24.1 |
| Region | |||
| Midwest | 699 | 22.3 | 20.7 |
| Northeast | 626 | 19.9 | 17.1 |
| South | 1258 | 40.0 | 38.3 |
| West | 559 | 17.8 | 23.9 |
| Self-rated general health | |||
| Excellent or Very Good | 1282 | 40.9 | 43.3 |
| Good | 1218 | 38.9 | 37.5 |
| Fair or Poor | 635 | 20.3 | 19.3 |
| Self-rated mental health | |||
| Excellent or Very Good | 1490 | 47.6 | 50.9 |
| Good | 1006 | 32.1 | 30.1 |
| Fair or Poor | 635 | 20.3 | 19.0 |
E2.
Full models predicting odds of pre-pandemic food insecurity
| Household Dietary Restriction |
|||
|---|---|---|---|
| Food Allergy |
Celiac Disease |
Both FA & CeD |
|
| aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | |
| Household Dietary Restriction Status | |||
| No Restriction | [Ref] | [Ref] | [Ref] |
| Restriction | 1.5 (1.2–1.9) | 2.3 (1.4–3.5) | 2.1 (1.2–3.6) |
| Race/Ethnicity | |||
| White | [Ref] | [Ref] | [Ref] |
| Black | 1.6 (1.2–2.2) | 1.7 (1.3–2.3) | 1.6 (1.2–2.2) |
| Hispanic | 1.6 (1.2–2.1) | 1.4 (1.0–1.9) | 1.3 (1.0–1.8) |
| Other | 1.5 (1.1–2.0) | 1.6 (1.1–2.2) | 1.5 (1.1–2.1) |
| Education level | |||
| High school or less | [Ref] | [Ref] | [Ref] |
| More than high school | 0.8 (0.7–0.9) | 0.8 (0.7–0.9) | 0.8 (0.7–0.9) |
| Household income | |||
| < 25K | 6.6 (4.6–9.3) | 7.1 (4.9–10.5) | 7.2 (4.9–10.6) |
| 25K – 49K | 3.4 (2.5–4.7) | 3.6 (2.5–5.0) | 3.4 (2.4–4.9) |
| 50K – 99K | 2.4 (1.7–3.3) | 2.5 (1.8–3.6) | 2.5 (1.8–3.5) |
| ≥ 100K | [Ref] | [Ref] | [Ref] |
| Marital status | |||
| Married/Partnered | [Ref] | [Ref] | [Ref] |
| Single | 1.0 (0.8–1.2) | 1.0 (0.8–1.2) | 1.0 (0.8–1.2) |
| Household size | 1.1 (1.0–1.2) | 1.1 (1.0–1.2) | 1.1 (1.0–1.2) |
| Number of Household Children | 1.2 (1.0–1.3) | 1.2 (1.0–1.4) | 1.2 (1.0–1.4) |
| Region | |||
| Midwest | [Ref] | [Ref] | [Ref] |
| Northeast | 1.4 (1.0–1.8) | 1.3 (1.0–1.7) | 1.3 (1.0–1.7) |
| South | 1.4 (1.1–1.8) | 1.5 (1.2–1.9) | 1.5 (1.2–1.9) |
| West | 1.7 (1.3–2.3) | 1.9 (1.4–2.6) | 1.9 (1.4–2.6) |
| Self-rated general health | |||
| Excellent or Very Good | [Ref] | [Ref] | [Ref] |
| Good | 1.1 (0.9–1.4) | 1.1 (0.8–1.3) | 1.1 (0.8–1.3) |
| Fair or Poor | 1.3 (1.0–1.8) | 1.2 (0.9–1.6) | 1.2 (0.9–1.6) |
| Self-rated mental health | |||
| Excellent or Very Good | [Ref] | [Ref] | [Ref] |
| Good | 1.1 (0.9–1.4) | 1.1 (0.9–1.4) | 1.1 (0.9–1.4) |
| Fair or Poor | 1.6 (1.3–2.2) | 1.7 (1.3–2.3) | 1.7 (1.2–2.2) |
E3.
Full models predicting odds of pandemic-related incident or worsening food insecurity
| Household Dietary Restriction |
|||
|---|---|---|---|
| Food Allergy |
Celiac Disease |
Both FA & CeD |
|
| aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | |
| Household Dietary Restriction Status | |||
| No Restriction | [Ref] | [Ref] | [Ref] |
| Restriction | 1.6 (1.3–2.1) | 2.3 (1.5–3.5) | 2.0 (1.2–3.4) |
| Race/Ethnicity | |||
| White | [Ref] | [Ref] | [Ref] |
| Black | 1.1 (0.8–1.5) | 1.1 (0.8–1.5) | 1.1 (0.8–1.5) |
| Hispanic | 1.4 (1.1–1.8) | 1.2 (0.9–1.6) | 1.2 (0.9–1.6) |
| Other | 1.4 (1.1–1.9) | 1.4 (1.0–1.9) | 1.3 (1.0–1.8) |
| Education level | |||
| High school or less | [Ref] | [Ref] | [Ref] |
| More than high school | 0.9 (0.8–1.0) | 0.9 (0.8–1.0) | 1.0 (0.9–1.1) |
| Household income | |||
| < 25K | 1.8 (1.3–2.5) | 2.0 (1.5–2.9) | 2.1 (1.4–2.9) |
| 25K – 49K | 1.8 (1.4–2.4) | 2.1 (1.5–2.8) | 2.0 (1.5–2.8) |
| 50K – 99K | 1.2 (0.9–1.5) | 1.3 (1.0–1.7) | 1.3 (0.9–1.7) |
| ≥ 100K | [Ref] | [Ref] | [Ref] |
| Marital status | |||
| Married/Partnered | [Ref] | [Ref] | [Ref] |
| Single | 1.0 (0.9–1.3) | 1.0 (0.8–1.2) | 1.0 (0.8–1.2) |
| Household size | 1.0 (0.9–1.1) | 1.1 (1.0–1.2) | 1.1 (1.0–1.2) |
| Number of Household Children | 1.2 (1.0–1.3) | 1.2 (1.0–1.3) | 1.2 (1.0–1.3) |
| Region | |||
| Midwest | [Ref] | [Ref] | [Ref] |
| Northeast | 1.4 (1.1–1.9) | 1.4 (1.1–1.9) | 1.5 (1.1–2.0) |
| South | 1.3 (1.0–1.6) | 1.4 (1.1–1.7) | 1.3 (1.0–1.7) |
| West | 1.2 (0.9–1.6) | 1.3 (1.0–1.8) | 1.3 (1.0–1.8) |
| Self-rated general health | |||
| Excellent or Very Good | [Ref] | [Ref] | [Ref] |
| Good | 1.1 (0.9–1.4) | 1.1 (0.9–1.4) | 1.1 (0.9–1.4) |
| Fair or Poor | 1.4 (1.0–1.8) | 1.5 (1.1–1.9) | 1.5 (1.1–2.0) |
| Self-rated mental health | |||
| Excellent or Very Good | [Ref] | [Ref] | [Ref] |
| Good | 1.1 (1.0–1.5) | 1.2 (0.9–1.5) | 1.2 (0.9–1.5) |
| Fair or Poor | 2.0 (1.5–2.5) | 2.0 (1.5–2.7) | 2.0 (1.5–2.7) |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Jessica D. Guillaume, The University of Chicago, Pritzker School of Medicine, Chicago, IL.
Jyotsna S. Jagai, The University of Chicago, Department of Obstetrics and Gynecology, Chicago, IL and University of Illinois at Chicago, School of Public Health, Chicago, IL.
Jennifer A. Makelarski, The University of Chicago, Department of Obstetrics and Gynecology, Chicago, IL.
Emily M. Abramsohn, The University of Chicago, Department of Obstetrics and Gynecology, Chicago, IL.
Stacy Tessler Lindau, The University of Chicago, Departments of Obstetrics and Gynecology and Medicine-Geriatrics, Chicago, IL.
Ritu Verma, The University of Chicago, Department of Pediatric Gastroenterology, Hepatology, and Nutrition, Chicago, IL.
Christina E. Ciaccio, The University of Chicago, Department of Pediatric Allergy and Immunology, Chicago, IL.
REFERENCES:
- 1.Cook JT, Frank DA, Berkowitz C, Black MM, Casey PH, Cutts DB, et al. Food insecurity is associated with adverse health outcomes among human infants and toddlers. J Nutr. 2004;134(6):1432–8. [DOI] [PubMed] [Google Scholar]
- 2.Cook JT, Frank DA, Levenson SM, Neault NB, Heeren TC, Black MM, et al. Child food insecurity increases risks posed by household food insecurity to young children’s health. J Nutr. 2006;136(4):1073–6. [DOI] [PubMed] [Google Scholar]
- 3.Stuff JE, Casey PH, Szeto KL, Gossett JM, Robbins JM, Simpson PM, et al. Household food insecurity is associated with adult health status. J Nutr. 2004;134(9):2330–5. [DOI] [PubMed] [Google Scholar]
- 4.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: Results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med. 2007;22(7):1018–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Council NR. Food Insecurity and Hunger in the United States: An Assessment of the Measure. Wunderlich GS, Norwood JL, editors. Washington, DC: The National Academies Press; 2006. [Google Scholar]
- 6.Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States in 2018. Economic Research Report Number 270. Washington, DC: U.S. Department of Agriculture, Economic Research Service; 2019. [Google Scholar]
- 7.Johns CB, Savage JH. Access to health care and food in children with food allergy. J Allergy Clin Immunol. 2014;133(2):582–585.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schanzenbach D, Pitts A. How Much Has Food Insecurity Risen? Evidence from the Census Household Pulse Survey. Chicago (IL); Institute for Policy Research Rapid Research Report; 2020. Available at: https://www.ipr.northwestern.edu/documents/reports/ipr-rapid-researchreports-pulse-hh-data-10-june-2020.pdf. Accessed December 5, 2020. [Google Scholar]
- 9.Lee AR, Ng DL, Zivin J, Green PHR. Economic burden of a gluten-free diet. J Hum Nutr Diet. 2007;20(5):423–30. [DOI] [PubMed] [Google Scholar]
- 10.Gupta R, Holdford D, Bilaver L, Dyer A, Holl JL, Meltzer D. The economic impact of childhood food allergy in the United States. JAMA Pediatr. 2013;167(11): 1026–31. [DOI] [PubMed] [Google Scholar]
- 11.Bilaver LA, Chadha AS, Doshi P, O’Dwyer L, Gupta RS. Economic burden of food allergy: A systematic review. Ann Allergy, Asthma Immunol. 2019;122(4):p373–380.e1. [DOI] [PubMed] [Google Scholar]
- 12.Dyer A, Negris O, Gupta R, Bilaver L. Food allergy: how expensive are they? Curr Opin Allergy Clin Immunol. 2020;20(2):188–93. [DOI] [PubMed] [Google Scholar]
- 13.Lee AR, Wolf RL, Lebwohl B, Ciaccio EJ, Green PHR. Persistent economic burden of the Gluten free diet. Nutrients. 2019;11(2):399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta RS, Warren CM, Smith BM, Blumenstock JA, Jiang J, Davis MM, et al. The public health impact of parent-reported childhood food allergies in the United States. Pediatrics. 2018;142(6):e20181235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta RS, Warren CM, Smith BM, Jiang J, Blumenstock JA, Davis MM, et al. Prevalence and Severity of Food Allergies Among US Adults. JAMA Netw open. 2019;2(1):e185630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rubio-Tapia A, Ludvigsson JF, Brantner TL, Murray JA, Everhart JE. The prevalence of celiac disease in the United States. Am J Gastroenterol. 2012;107(10):1538–44. [DOI] [PubMed] [Google Scholar]
- 17.WHO Director-General’s opening remarks at the media briefing on COVID-19. World Health Organization; 2020. Available at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-−−11-march-2020. Accessed December 5, 2020.
- 18.The Employment Situation - May 2020. Bureau of Labor Statistics; 2020. Available at: https://www.bls.gov/news.release/pdf/empsit.pdf. Accessed December 5, 2020. [Google Scholar]
- 19.Silva C Food Insecurity In The U.S. By The Numbers. NPR; 2020. Available at: https://www.npr.org/2020/09/27/912486921/food-insecurity-in-the-u-s-by-the-numbers. Accessed December 5, 2020.
- 20.Food Security Information Network. 2020 Global Report on Food Crises: Joint Analysis for Better Decisions. Rome, Italy and Washington, DC: Food and Agriculture Organization (FA); World Food Programme (WFP); and International Food Policy Research Institute (IFPRI); 2020. Available at: https://www.fsinplatform.org/global-report-food-crises-2020. Accessed December 5, 2020. [Google Scholar]
- 21.Van Lancker W, Parolin Z. COVID-19, school closures, and child poverty: a social crisis in the making. Lancet Public Heal. 2020;5(5):e243–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kulish N ‘Never Seen Anything Like It’: Cars Line Up for Miles at Food Banks. New York Times; 2020. Available at: https://www.nytimes.com/2020/04/08/business/economy/coronavirus-food-banks.html. Accessed December 5, 2020. [Google Scholar]
- 23.Schanzenbach D, Pitts A. Food Insecurity during COVID-19 in households with children: Results by racial and ethnic groups. Chicago (IL); Institute for Policy Research Rapid Research Report; 2020. Available at: https://www.ipr.northwestern.edu/documents/reports/ipr-rapid-research-reports-pulse-hh-data-9-july-2020-by-race-ethnicity.pdf. Accessed December 5, 2020. [Google Scholar]
- 24.Myers AMC, Painter MA. Food insecurity in the United States of America: an examination of race/ethnicity and nativity. Food Secur. 2017;9:1419–1432. [Google Scholar]
- 25.Larson NI, Story MT, Nelson MC. Neighborhood Environments. Disparities in Access to Healthy Foods in the U.S. American Journal of Preventive Medicine. 2009;36(1):74–81. [DOI] [PubMed] [Google Scholar]
- 26.Bower KM, Thorpe RJ, Rohde C, Gaskin DJ. The intersection of neighborhood racial segregation, poverty, and urbanicity and its impact on food store availability in the United States. Prev Med. 2014;58:33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gordon C, Purciel-Hill M, Ghai NR, Kaufman L, Graham R, Van Wye G. Measuring food deserts in New York City’s low-income neighborhoods. Heal Place. 2011;17(1):696–700. [DOI] [PubMed] [Google Scholar]
- 28.Lindau ST, Makelarski JA, Boyd K, Doyle KE, Haider S, Kumar S, et al. Change in Health-Related Socioeconomic Risk Factors and Mental Health during the Early Phase of the COVID-19 Pandemic: A National Survey of U.S. Women. J Women’s Heal. April5, 2021. Ahead of Print: 10.1089/jwh.2020.8879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Health Care Panel. Opinions 4 Good; 2020. Available at: https://op4g.com/our-panel/health-care-panel/. Accessed December 5, 2020. [Google Scholar]
- 30.Forrest CB, Bevans KB, Pratiwadi R, Moon J, Teneralli RE, Minton JM, et al. Development of the PROMIS® pediatric global health (PGH-7) measure. Qual Life Res. 2014;23(3):1221–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gruber-Baldini AL, Velozo C, Romero S, Shulman LM. Validation of the PROMIS® measures of self-efficacy for managing chronic conditions. Qual Life Res. 2017;26(7):1915–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.U.S. Census Bureau. 2018American Community Survey 1-year estimates. 2018.Available at: https://www2.census.gov/programs-surveys/acs/summary_file/2018/data/?#. Accessed May 15, 2020. [Google Scholar]
- 33.Jeung R, Nham K. Incidents of Coronavirus-Related Discrimination. Asian Pacific Policy and Planning Council; 2020. Available at: https://a1w.90d.myftpupload.com/wp-content/uploads/2020/10/Stop_AAPI_Hate_Monthly_Report_200423.pdf. Accessed December 4, 2020.
- 34.Margolin J FBI warns of potential surge in hate crimes against Asian Americans amid coronavirus. ABC News; 2020. Available at: https://abcnews.go.com/US/fbi-warns-potential-surge-hate-crimes-asian-americans/story?id=69831920. Accessed January 5, 2021.
- 35.The American Association for Public Opinion Research. Standard definitions: Final dispositions of case codes and outcome rates for surveys. 9th edition. AAPOR; 2016. Available at: https://www.aapor.org/AAPOR_Main/media/publications/Standard-Definitions20169theditionfinal.pdf. Accessed May 27, 2017. [Google Scholar]
- 36.Ware JE, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: Construction of Scales and Preliminary Tests of Reliability and Validity. Med Care. 1996;34(3):220–33. [DOI] [PubMed] [Google Scholar]
- 37.Hays RD, Schalet BD, Spritzer KL, Cella D . Two-item promis® global physical and mental health scales. J Patient-Reported Outcomes 2017;1(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hager ER, Quigg AM, Black MM, Coleman SM, Heeren T, Rose-Jacobs R, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics 2010;126(1):e26–32. [DOI] [PubMed] [Google Scholar]
- 39.Deville JC, Särndal CE, Sautory O. Generalized raking procedures in survey sampling. J Am Stat Assoc. 1993;88(423):1013–20. [Google Scholar]
- 40.Brown E, Das R, Brewer AG, Martinez E, Bilaver LA, Gupta RS. Food Insecure and Allergic in a Pandemic: A Vulnerable Population. J Allergy Clin Immunol Pract. 2020;8(7):2149–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Corkey M, Yaffe-Bellany D. U.S. Food Supply Chain Is Strained as Virus Spreads. The New York Times; 2020. Available at: https://www.nytimes.com/2020/04/13/business/coronavirus-food-supply.html. Accessed December 5, 2020. [Google Scholar]
- 42.Smith J Postal Package Deliveries ‘Bogged Down’ With Delays, Backlogs. The Wall Sreet Journal; 2020. Available at: https://www.wsj.com/articles/postal-package-deliveries-bogged-down-with-delays-backlogs-11590836400. Accessed December 5, 2020. [Google Scholar]
- 43.Burke MP, Jones SJ, Frongillo EA, Fram MS, Blake CE, Freedman DA. Severity of household food insecurity and lifetime racial discrimination among African-American households in South Carolina. Ethn Heal. 2018;23(3):176–292. [DOI] [PubMed] [Google Scholar]
- 44.Odoms-Young A, Bruce MA. Examining the Impact of Structural Racism on Food Insecurity: Implications for Addressing Racial/Ethnic Disparities. Fam Community Health. 2018;41:S3–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Phojanakong P, Weida EB, Grimaldi G, Lê-Scherban F, Chilton M. Experiences of racial and ethnic discrimination are associated with food insecurity and poor health. Int J Environ Res Public Health. 2019;16(22):4369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Whyte LA, Kotecha S, Watkins WJ, Jenkins HR. Coeliac disease is more common in children with high socio-economic status. Acta Paediatr Int J Paediatr. 2014;103(3):289–94. [DOI] [PubMed] [Google Scholar]
- 47.Olén O, Bihagen E, Rasmussen F, Ludvigsson JF. Socioeconomic position and education in patients with coeliac disease. Dig Liver Dis. 2012;44(6):471–6. [DOI] [PubMed] [Google Scholar]
- 48.Ludvigsson JF. Socio-economic characteristics in children with coeliac disease. Acta Paediatr Int J Paediatr. 2005;94(1):107–13. [DOI] [PubMed] [Google Scholar]
- 49.Norström F, Namatovu F, Carlsson A, Hogberg L, Ivarsson A, Myléus A. Family socio-economic status and childhood coeliac disease seem to be unrelated—A cross-sectional screening study. Acta Paediatr Int J Paediatr. 2020;00:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cappell K, Taylor A, Johnson BH, Gelwicks S, Wang S, Gerber M, et al. Healthcare Resource Utilization and Costs in Celiac Disease : A US Claims Analysis. Am J Gastroenterol. 2020;115(11):1821–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Guandalini S, Tundia N, Thakkar R, Macaulay D, Essenmacher K, Fuldeore M. Direct Costs in Patients with Celiac Disease in the USA: A Retrospective Claims Analysis. Dig Dis Sci. 2016;61(10):2823–30. [DOI] [PubMed] [Google Scholar]
- 52.Long K, Rubio-Tapia A, Wagie A, Melton L, Lahr B, Van Dyke C, et al. The economics of coeliac disease: A population-based study. Aliment Pharmacol Ther. 2010;32(2):261–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: A cluster RCT. Pediatrics. 2015;135(2):e296–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cavanagh M, Jurkowski J, Bozlak C, Hastings J, Klein A. Veggie Rx: An outcome evaluation of a healthy food incentive programme. Public Health Nutr. 2017;20(14):2636–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Patel MR, Resnicow K, Lang I, Kraus K, Heisler M. Solutions to Address Diabetes-Related Financial Burden and Cost-Related Nonadherence: Results From a Pilot Study. Heal Educ Behav. 2018;45(1): 101–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Berkowitz SA, Delahanty LM, Terranova J, Steiner B, Ruazol MP, Singh R, et al. Medically Tailored Meal Delivery for Diabetes Patients with Food Insecurity: a Randomized Cross-over Trial. J Gen Intern Med. 2019;34(3):396–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ryan C. Computer and Internet Use in the United States: 2016. American Community Survey Report Number 39. Washington, DC: U.S. Census Bureau; 2017. Available at: https://www.census.gov/content/dam/Census/library/publications/2018/acs/ACS-39.pdf. Accessed Feburary 13, 2021. [Google Scholar]
- 58.Van Den Akker M, Van Steenkiste B, Krutwagen E, Metsemakers JFM. Disease or no disease? Disagreement on diagnoses between self-reports and medical records of adult patients. Eur J Gen Pract. 2015;21(1):45–51. [DOI] [PubMed] [Google Scholar]
- 59.Savage J, Sicherer S, Wood R. The Natural History of Food Allergy. J Allergy Clin Immunol Pract. 2016;4(2):196–203. [DOI] [PubMed] [Google Scholar]
- 60.Dilley MA, Rettiganti M, Christie L, O’Brien E, Patterson M, Weeks C, et al. Impact of food allergy on food insecurity and health literacy in a tertiary care pediatric allergy population. Pediatr Allergy Immunol. 2019;30(3):363–369. [DOI] [PubMed] [Google Scholar]


