Abstract
We still have little understanding of short-term predictors of suicidal thoughts and behaviors (STBs). Prior research links increased negative affect to STBs, but the vast majority of earlier work is limited by measuring negative affect at one time point and aiming to predict STBs months or years in the future. Recently, intensive longitudinal studies have shown that negative affect is associated with suicidal thoughts over relatively short, clinically useful time periods; however, the specific patterns and types of negative affect that predict STBs remain unclear. Using ecological momentary assessment (EMA) data from psychiatric inpatients hospitalized for suicide risk (N = 83), this study sought to test whether the patterns (means and variability) of two types of negative affect (anxiety/agitation and shame/self-hatred, which were derived from a larger EMA battery) during hospitalization predict STBs in the four weeks after discharge: an extremely high-risk time for suicidal behavior. The mean – but not the variability – of both anxiety/agitation and shame/self-hatred during hospitalization predicted the number of days with suicidal thoughts after discharge. The mean and the variability of shame/self-hatred – but not anxiety/agitation – predicted post-discharge suicide attempt. We discuss implications for assessment and treatment of suicidal individuals and propose key directions for future research.
Keywords: suicide, suicidal thoughts and behaviors, negative affect, EMA
Suicide is a leading cause of death, with over 47,000 individuals dying by suicide each year in the United States (Centers for Disease Control, 2018). Nonfatal suicidal thoughts and behaviors (STBs) confer risk of future death by suicide (Ribeiro et al., 2016) and are associated with significant public health costs (Shepard et al., 2016). Despite decades of research, our ability to predict who will die by suicide is poor (Franklin et al., 2017). The factors that predict acute increases in suicidal thoughts and the transition from suicidal thoughts to behavior are especially unclear (e.g., Glenn & Nock, 2014). Very few studies focus on short-term risk; one recent meta-analysis of all studies on risk factors for STBs found that less than 1% of effect sizes capture a prediction window of one month or shorter (Franklin et al., 2017). This is a critical area in need of attention given that clinicians are most often tasked with determining whether patients will engage in suicidal behavior over short time windows: the coming hours, days, or weeks.
The weeks immediately after psychiatric hospitalization represent a short time period of extremely high risk for suicide (Olfson, 2017). Recent meta-analytic research shows that for psychiatric inpatients, the suicide rate during the first month after discharge is over 200 times the global rate (for the first week, 300 times) (Chung et al., 2019; Chung et al., 2017). Indeed, suicide risk has been shown to peak within the first week after discharge then steadily decrease over the following weeks and months (Qin & Nordentoft, 2005). Thus, improving the understanding of short-term risk factors for suicide during this high-risk time and the ability to predict which inpatients will make a suicide attempt after leaving the hospital is critical.
The central role of negative affect (NA) in the development and maintenance of STBs has long been theorized and observed clinically. Prominent theories posit that NA or constructs comprising intense NA – psychological pain (Shneidman, 1993), emotion dysregulation (Linehan, 1993), hopelessness (Abramson et al., 2000; Beck, 1967), and perceived burdensomeness (Joiner, 2005) – play a key role in conferring risk for STBs. For instance, suicide has long been conceptualized as escape from aversive intense NA (Baumeister, 1990; Maltsberger, 2004). Although a great deal of empirical work has demonstrated prospective associations between NA and STBs, nearly all prior studies used affective constructs measured at one time point to predict STBs many months or years in the future (Franklin et al., 2017). This approach is limited by treating NA states as static, trait-like phenomena and emphasizing distal, not short-term, suicide risk. To start to address these limitations, researchers have recently leveraged high-frequency, intensive longitudinal methods such as ecological momentary assessment (EMA) to capture momentary levels of NA and test short-term associations with momentary suicidal thoughts. These studies have generally shown that a wide range of momentary NA states predict suicidal thoughts over very short temporal windows (e.g., Ben-Zeev et al., 2012; Hallensleben et al., 2019; Humber et al., 2013; Husky et al., 2017; Kleiman et al., 2017; Mou et al., 2018).
It is not yet clear, however, whether certain within-person patterns of NA over time, such as the mean (average within-person intensity of NA) or variability (average within-person deviation from the mean), are better short-term predictors of STBs than others. For example, it has been proposed that variations in NA may confer greater risk for STBs than overall levels of NA, as unstable and rapidly fluctuating NA may be harder to tolerate than stable (even if high) NA and serve to increase the severity and frequency of suicidal thoughts over time (e.g., Palmier-Claus, Taylor, Varese, et al., 2012). A few intensive longitudinal studies support this hypothesis, showing that NA instability (a time-sensitive metric of variability; Trull et al., 2015) is associated with STBs when controlling for mean NA (e.g., Palmier-Claus, Taylor, Gooding, et al., 2012) and more recently, that both the mean and the variability of NA are associated with past-year and concurrent suicidal thoughts (Victor et al., in press), whereas other earlier work found that only mean NA (not metrics of variability) is associated with STBs (e.g., Links et al., 2007). These prior studies are limited, however, by generally assessing STBs retrospectively or concurrently (during the same reporting period as NA), not prospectively.
It also is not yet known whether different types of NA consistently confer greater risk for STBs than others. Prior work has shown that disorders characterized by high arousal NA such as severe anxiety or agitation (e.g., posttraumatic stress disorder, intermittent explosive disorder) confer risk specifically for transitioning from suicidal thoughts to behavior, whereas disorders primarily characterized by lower arousal NA such as sadness (e.g., major depressive disorder) do not (Nock et al., 2010). These findings align with theory that, among people already at elevated risk for suicide, the presence of acute, high arousal affective disturbances (e.g., agitation) may be a proximal marker of imminent suicidal behavior (Fawcett et al., 1990; Rogers et al., 2016), perhaps reflecting an associated action tendency to escape these aversive states. Other affective states that have been both conceptually and, at least preliminarily, empirically linked to STBs include guilt and shame, with theory suggesting that both suicidal and nonsuicidal self-injurious behavior may function to regulate these aversive, self-directed states (e.g., Cameron et al., 2020; Sheehy et al., 2019). With few notable exceptions (e.g., Palmier-Claus et al., 2013), however, prior intensive longitudinal studies on patterns of NA and STBs have largely collapsed across same-valenced affect items to form one NA construct (e.g., Victor et al., in press), rather than examining potentially nuanced associations between patterns of different types of NA and STBs.
Current Study
Here we examined the associations between EMA data on NA collected from suicidal psychiatric inpatients during hospitalization and follow-up data on STBs from the four weeks after discharge (following the inpatient EMA phase). Our first aim was to test whether patterns (specifically, the mean and variability) of two types of NA (“anxiety/agitation” and “shame/self-hatred,” which were derived from a larger EMA battery) during hospitalization predict the number of days with suicidal thoughts in the two weeks after discharge. We hypothesized that mean levels of both types of NA during hospitalization would predict suicidal thoughts after discharge; given mixed earlier findings, we also hypothesized that when controlling for mean NA, NA variability would not predict suicidal thoughts. Our second aim was to test whether patterns of NA during hospitalization predict suicide attempt in the four weeks after discharge. We again hypothesized that mean levels of both types of NA (but not variability of NA when controlling for the mean) during hospitalization would predict post-discharge suicide attempt.
Method
Participants
Participants in this study were 104 adult inpatients hospitalized on an adult psychiatric inpatient unit at the Massachusetts General Hospital for a recent suicide attempt or severe suicidal thoughts who agreed to participate in a smartphone monitoring study during their inpatient stay. Inclusion criteria were admission to the inpatient unit due to recent suicide attempt or severe suicidal thoughts, fluency in English, and permission from an inpatient provider to approach the patient for participation. Exclusion criteria included anything that would impair participants from understanding the study instructions and providing informed consent (e.g., cognitive impairment). We did not require a minimum length of hospital stay for participation.
For this report, we only included the 83 participants (79.8% of the original sample) who completed at least 3 EMA surveys during hospital stay. Study data were collected in two waves; the first wave (from January 2016 to January 2017) had 37 (of 44; 84.1%) participants1 with at least three EMA surveys and the second wave (from May 2017 to December 2018) had 46 (of 60; 76.7%) participants with at least three EMA surveys. The only differences between the two waves of the study were the smartphone platform used to collect EMA data and the number of EMA prompts per day (described below); all other methods and assessments were equivalent.
Procedure
This study included five parts: (1) recruitment and a baseline assessment that occurred as close to a participant’s inpatient admission as possible, (2) an EMA period that lasted the duration of the participants’ hospital stays (M = 8.52 days, SD = 5.73; range: 2 to 46), (3) a discharge assessment at the end of hospital stay, (4) post-hospitalization follow-up retrospective assessments (via online surveys) at two- and four-weeks after hospital discharge, and (5) extraction of relevant post-discharge outcomes (e.g., suicide attempt) from the hospital’s electronic health record (EHR), which is shared by other hospitals within the healthcare system and has access to other regional and national institutions. In this report, we focus only on the inpatient EMA period, post-hospitalization retrospective assessments, and EHR outcomes. During the inpatient period, participants were compensated with $10 per day for their participation (regardless of number of EMA prompts completed). All study procedures were approved by the Institutional Review Board at the Massachusetts General Hospital (under protocol #2015P000598) with reliance agreements with other involved institutions (under SMART IRB protocol #2255).
Measures
Inpatient EMA Battery
Smartphone-based EMA was used to assess momentary NA. In the first study wave, MovisensXS, an EMA app for Android phones, was used to send surveys four times per day randomly within pre-defined windows between 8am and 8pm. We provided loaner phones to those who had an iOS device or no phone. In the second wave, Beiwe, a digital phenotyping platform for Android and iOS phones, was used to send surveys six times per day randomly within pre-defined windows, also between 8am and 8pm. Participants were asked to rate how much they were currently feeling 14 NA or cognitive-affective states at the time of the survey on a ten-point scale. NA states were taken from the Positive and Negative Affect Schedule (PANAS) (Watson et al., 1988) as well as broader cognitive-affective states associated with risk for suicide (e.g., hopeless, abandoned). The 14 NA states assessed were: desperate, hopeless, abandoned, self-hate, rage, anxious, lonely, guilty, humiliated, upset, ashamed, nervous, afraid, and fatigued. See Data Processing for the approach used to generate two NA categories from a subset of the 14 total EMA items: anxious, nervous, upset, and rage (“anxiety/agitation” category), and ashamed, guilty, humiliated, and self-hate (“shame/self-hatred” category).
Post-Discharge Follow-Up Surveys
At two and four weeks after discharge, participants were asked to complete an online follow-up survey of STBs that occurred since discharge. Participants who did at least one follow-up survey (n = 65 [78.3%], of which 31 [83.8%] were in the first study wave and 34 [73.9%] were in the second wave) did not differ (all ps > .10) from those who did not complete a follow-up survey in terms of STB history (recent and lifetime), baseline measures of depression and anxiety symptom severity, or length of inpatient hospitalization.
Post-Discharge Suicidal Thoughts.
Days with suicidal thoughts were assessed with the following question sequence in the two-week follow-up survey. First, participants were asked “In the past two weeks, did you have thoughts of killing yourself?” If yes, they were then asked, “About how many days in the past two weeks did you think of killing yourself?” In the four-week follow-up survey, participants were asked the same question sequence but with a “past four weeks” time frame (thus also encompassing the first two weeks after discharge).2 The analysis of post-discharge suicidal thoughts focused on the number of days with active suicidal thoughts in the two weeks after discharge. The 59 participants (71.1%) who provided data about number of days with suicidal thoughts in the two-week follow-up survey (n = 54) or did not complete the two-week follow-up survey but responded “no” to the first four-week survey question about presence of suicidal thoughts in the past two weeks (n = 5) were included in this analysis.
Post-Discharge Suicidal Behavior.
Consistent with prior work by our team on predicting suicidal behavior (e.g., Nock et al., 2010), we used two methods to assess suicide attempt in the month after discharge. From the two- and four-week follow-up surveys, we categorized participants as having made a suicide attempt if they (1) reported being re-admitted to the hospital and in response to the follow-up question “What was the reason for your admission overnight to a hospital for mental health care?”, responded “tried to kill yourself”, or (2) responded affirmatively to “In the past two (four) weeks (that is, since you left the unit), did you make a suicide attempt (that is, purposefully hurt yourself with at least some intent to die)?”. We also reviewed participants’ charts in the EHR for documented suicide attempts (e.g., the participant visited a hospital for suicide attempt) in the four weeks after discharge. This yielded a categorical suicide attempt variable, where 1 = attempt and 0 = no attempt. The 64 participants who provided information about suicide attempt in at least one follow-up survey (including the 5 participants who denied making a suicide attempt in the two-week follow-up survey and subsequently did not complete the four-week survey) or had a documented suicide attempt in the EHR were included in this analysis. Nine (14.1%) participants made a suicide attempt.
Data Processing
Data processing and analysis were conducted in R (version 3.5.3; R Core Team, 2019). To calculate intraindividual metrics using EMA affect data, it is standard practice to compute a composite score for each measurement occasion by taking the average of all same-valenced affect items. This approach, however, ignores conceptual differences between individual affect items (e.g., in terms of the arousal dimension or associated behavioral tendencies) (Dejonckheere et al., 2019). Thus, given the wide range of NA and cognitive-affective states included in our EMA battery (e.g., rage, hopeless, afraid), we used an empirical approach (principal components analysis [PCA] of all 14 NA items followed by multilevel confirmatory factor analysis [CFA]; see Supplemental Material for details) to identify two categories of NA, each of which comprised four conceptually similar individual NA items. The two categories identified were “anxiety/agitation” (made up of anxious, nervous, upset, and rage – all prototypical high arousal NA states characterized by anxiety or agitation) and “shame/self-hatred” (ashamed, guilty, humiliated, and self-hate – all self-directed NA or cognitive-affective states characterized by shame, guilt, or hatred). The remaining six EMA NA items (desperate, hopeless, abandoned, lonely, afraid, and fatigued) were not included in subsequent analyses.
We then computed composite anxiety/agitation (average of anxious, nervous, upset, and rage items) and shame/self-hatred (average of ashamed, guilty, humiliated, and self-hate items) scores for each EMA observation. To calculate within-person patterns of NA, we computed the mean and variability (the standard deviation [SD]) of each participant’s anxiety/agitation and shame/self-hatred scores, resulting in four variables for each participant: anxiety/agitation mean, anxiety/agitation variability (SD), shame/self-hatred mean, and shame/self-hatred variability (SD).3 Missing EMA observations were excluded as a function of listwise deletion.
Data Analyses
Preliminary Analyses
We first computed descriptive statistics (means and SDs) of the mean and variability of anxiety/agitation and shame/self-hatred, and used paired t-tests to test for differences between the two NA categories. We computed the repeated measures correlation of momentary anxiety/agitation and shame/self-hatred using the rmcorr package (Bakdash & Marusich, 2020), followed by the intraclass correlations (ICCs) to describe the proportion of variance attributed to within- versus between-person variance for each NA type, using the ICC package (Wolak, 2017).
Bayesian Modeling
All regression models described below were estimated within a Bayesian modeling framework (Gelman et al., 2014; Kruschke & Liddell, 2018) using the brms package (Bürkner, 2017). We used Bayesian estimation over traditional frequentist methods for two main reasons. First, Bayesian statistics are better suited than frequentist methods to modeling data with relatively small sample sizes (Depaoli & van de Schoot, 2017). Second, Bayesian models provide posterior distributions that represent uncertainty of the resultant beta values, which (unlike confidence intervals in frequentist methods) have an intuitive interpretation (Kruschke, 2015). Specifically, the credible interval (also referred to as the highest density interval [HDI]) summarizes the central portion of the posterior distribution that contains a certain percentage (often, 95%) of probable beta values (Kruschke & Liddell, 2018). Thus, a 95% HDI of 0.25 to 0.50, for example, allows one to conclude with 95% certainty that the population value lies between 0.25 and 0.50 (e.g., Makowski, Ben-Shachar, & Lüdecke, 2019).
All Bayesian models described below were estimated using Markov Chain Monte Carlo (MCMC) simulation, with 4 chains per model and 10,000 iterations per chain, and non-informative prior distributions. Results were interpreted by summarizing the 95% HDIs around the median (as a measure of centrality) (Kruschke & Liddell, 2018). We also calculated the probability of direction (pd) values as an index of effect existence for each parameter using the bayestestR package (Makowski, Ben-Shachar, & Lüdecke, 2019). Ranging from 50% to 100%, the pd represents the certainty with which an effect is reliably positive or negative. For example, if 99% of beta values in the posterior distribution are above 0, then we would have high certainty that the data suggest that the true relationship is positive. The pd value is similar to frequentist p values (Makowski, Ben-Shachar, Chen, et al., 2019). Thus, although we focus on HDIs, for those that prefer a strict cutoff, parameters with pd values greater than or equal to 97.5% (corresponding to a two-sided p value of .05) may be considered “significant” (Makowski, Ben-Shachar, Chen, et al., 2019). The sjPlot (Lüdecke, 2020) package was used to generate plots of such “significant” effects in the final models. Posterior predictive checks were conducted for all models to confirm concordance of observed and simulated data (Kruschke, 2015).
Predicting Post-Discharge Suicidal Thoughts.
To test whether NA during hospitalization predicted the number of days with suicidal thoughts in the two weeks after discharge, we began with fitting four zero-inflated binomial models using the logit link function with each NA variable (mean of anxiety/agitation, variability of anxiety/agitation, mean of shame/self-hatred, and variability of shame/self-hatred) as the sole predictor. We then fit a final model that included all NA variables that predicted (based on HDIs and pd) days with suicidal thoughts in the four bivariate models to test whether, for example, NA variability predicted suicidal thoughts when controlling for mean NA. We chose zero-inflated binomial models because the outcome was an upper-bounded count variable with excess zeroes (Hall, 2000).
Predicting post-discharge suicide attempt.
To test whether NA predicted suicide attempt in the four weeks after discharge, we again began with fitting four bivariate logistic regression models using the logic link function with each NA variable as the sole predictor of suicide attempt. We then fit a multiple regression model including all the NA variables that predicted suicide attempt in the four bivariate models as predictors.
Results
Preliminary Analyses
Overall, participants in this study completed a total of 1,374 surveys (median = 18.5 per participant, SD = 15.1, range = 3 – 120) during the inpatient EMA phase (M = 5.9 days, SD = 5.7, range = 2 – 44). The mean time interval between completed surveys was 7.7 hours (SD = 8.2 hours, range = 0.0 – 101.7); 10% of surveys had an interval of one hour or less and 2.7% had an interval of 24 hours or more. The number of completed EMA surveys did not differ by study wave. The overall EMA compliance rate was 52.2% (58.5% in the first wave which used four prompts/day and 47.1% in the second wave which used six prompts/day; p < .010). Length of hospital stay was correlated with the number of completed EMA surveys (r = .84 [95% CI: .77, .90], p < .001) but not EMA compliance (r = .08, p = 0.440).
The average age of the sample was 38.43 years (SD = 13.64, range = 18 to 68); participants in the first study wave (M = 43.14 years) were slightly older than those in the second wave (M = 34.56 years) (p < .010). Of the 83 participants included, 43 identified as male, 35 as female, three as transgender, two as another gender identity. A total of 69 participants self-identified as being of European decent, four as Black/African-American, four as Asian, and five as another race (one participant did not answer this question). A total of 76 participants self-identified as non-Hispanic/Latinx, and seven participants identified as Hispanic/Latinx. There were no significant differences in gender or race/ethnicity between the two waves.
Descriptive statistics (sample means and SDs) of predictor (mean and variability of anxiety/agitation and shame/self-hatred) and dependent variables (post-discharge STBs) are presented in Table 1. NA and post-discharge STBs did not vary by number of completed EMA surveys, length of hospital stay, or study wave. The mean and variability of anxiety/agitation did not differ significantly from the mean and variability of shame/self-hatred. The repeated measures correlation for momentary anxiety/agitation and shame/self-hatred was 0.51 (95% CI: 0.46 – 0.55). ICCs indicated that most of the variability in the NA categories was due to between-person variance, with 28% of variance in anxiety/agitation and 18% in shame/self-hatred occurring within-person. See Supplemental Material for ICCs (ranging from .54 [“upset”] to .77 [“self-hate”]) of the eight EMA items used to generate the two NA categories.
Table 1.
Descriptive statistics for inpatient NA and post-discharge STBs
| Mean | Variability | ICC [95% CI] | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Inpatient NA | Mean | SD | Mean | SD | |||
|
| |||||||
| Anxiety/agitation | 4.53 | 1.95 | t(82) = 0.41, p = .68 | 1.10 | 0.59 | t(82) = 0.70, p = .48 | .72 [.66, .78] |
| Shame/self-hatred | 4.44 | 2.37 | 1.06 | 0.61 | .82 [.77, .86] | ||
|
| |||||||
| Post-discharge STBs | Mean | SD | Range | n (%) | |||
|
| |||||||
| Days with suicidal thoughts (two weeks after discharge) | 2.97 | 3.80 | 0 – 14 | -- | |||
| Suicide attempt | -- | -- | 9 (14.1%) | ||||
Note. SD = standard deviation. Inpatient NA: n = 83 with at least 3 EMA surveys; Days with suicidal thoughts in two weeks after discharge: n = 59 with follow-up survey data; Suicide attempt in four weeks after discharge: n = 64 with follow-up survey or EHR data.
Predicting Post-Discharge Suicidal Thoughts
Fixed effects for the bivariate zero-inflated binomial models (using each of the four NA variables to predict the number of days with suicidal thoughts in the two weeks after discharge) are presented in the top part of Table 2 (n = 59). Mean levels of both anxiety/agitation and shame/self-hatred predicted the number of days with suicidal thoughts, but variability in anxiety/agitation and shame/self-hatred did not. In the multiple regression model, each type of mean NA (mean anxiety/agitation and shame/self-hatred) predicted days with suicidal thoughts when controlling for the other (bottom part of Table 2; Figure 1). These findings held when controlling for the number of completed EMA surveys, % EMA compliance, length of hospital stay, and study wave.4
Table 2.
Fixed effects from zero-inflated binomial models predicting number of days with suicidal thoughts after discharge
| Bivariate models | Main Effects |
|||
|---|---|---|---|---|
| Median | 95% HDI | pd | Odds ratio | |
|
| ||||
| (Intercept) | −1.69 | [−2.35, −1.05] | 100.0% | 0.18 |
| (Zero-inflated intercept) | −0.19 | [−0.71, 0.31] | 77.0% | 0.83 |
| Anxiety/agitation mean | 0.26 | [0.13, 0.39] | 100.0%* | 1.30 |
|
| ||||
| (Intercept) | −0.16 | [−0.60, 0.29] | 74.8% | 0.85 |
| (Zero-inflated intercept) | −0.17 | [−0.69, 0.32] | 74.0% | 0.84 |
| Anxiety/agitation variability | −0.26 | [−0.62, 0.10] | 92.2% | 0.77 |
|
| ||||
| (Intercept) | −1.68 | [−2.24, −1.16] | 100.0% | 0.19 |
| (Zero-inflated intercept) | −0.21 | [−0.72, 0.31] | 78.7% | 0.81 |
| Shame/self-hatred mean | 0.26 | [0.16, 0.36] | 100.0%* | 1.30 |
|
| ||||
| (Intercept) | −0.33 | [−0.76, 0.14] | 92.4% | 0.72 |
| (Zero-inflated intercept) | −0.17 | [−0.68, 0.34] | 73.6% | 0.84 |
| Shame/self-hatred variability | −0.12 | [−0.51, 0.27] | 72.4% | 0.89 |
|
| ||||
| Multiple regression model | ||||
|
| ||||
| (Intercept) | −2.40 | [−3.18, −1.61] | 100.0% | 0.09 |
| (Zero-inflated intercept) | −0.25 | [−0.80, 0.29] | 82.1% | 0.78 |
| Anxiety/agitation mean | 0.18 | [0.05, 0.33] | 99.6%* | 1.20 |
| Shame/self-hatred mean | 0.23 | [0.12, 0.33] | 100.0%* | 1.26 |
Note. The top part of the table presents results from four separate bivariate models using each NA variable as the sole predictor, and the bottom part presents results from the multiple regression model including only those NA variables that predicted days with suicidal thoughts in the bivariate models. The zero-inflated intercept corresponds to the discrete distribution portion of the model (i.e., predicting excess zeroes), whereas the intercept is for the beta distribution portion of the model (i.e., predicting values greater than zero). HDI = Highest Density Interval. pd = probability of direction (“significant” effects are marked with a *). N = 59 participants.
Figure 1.
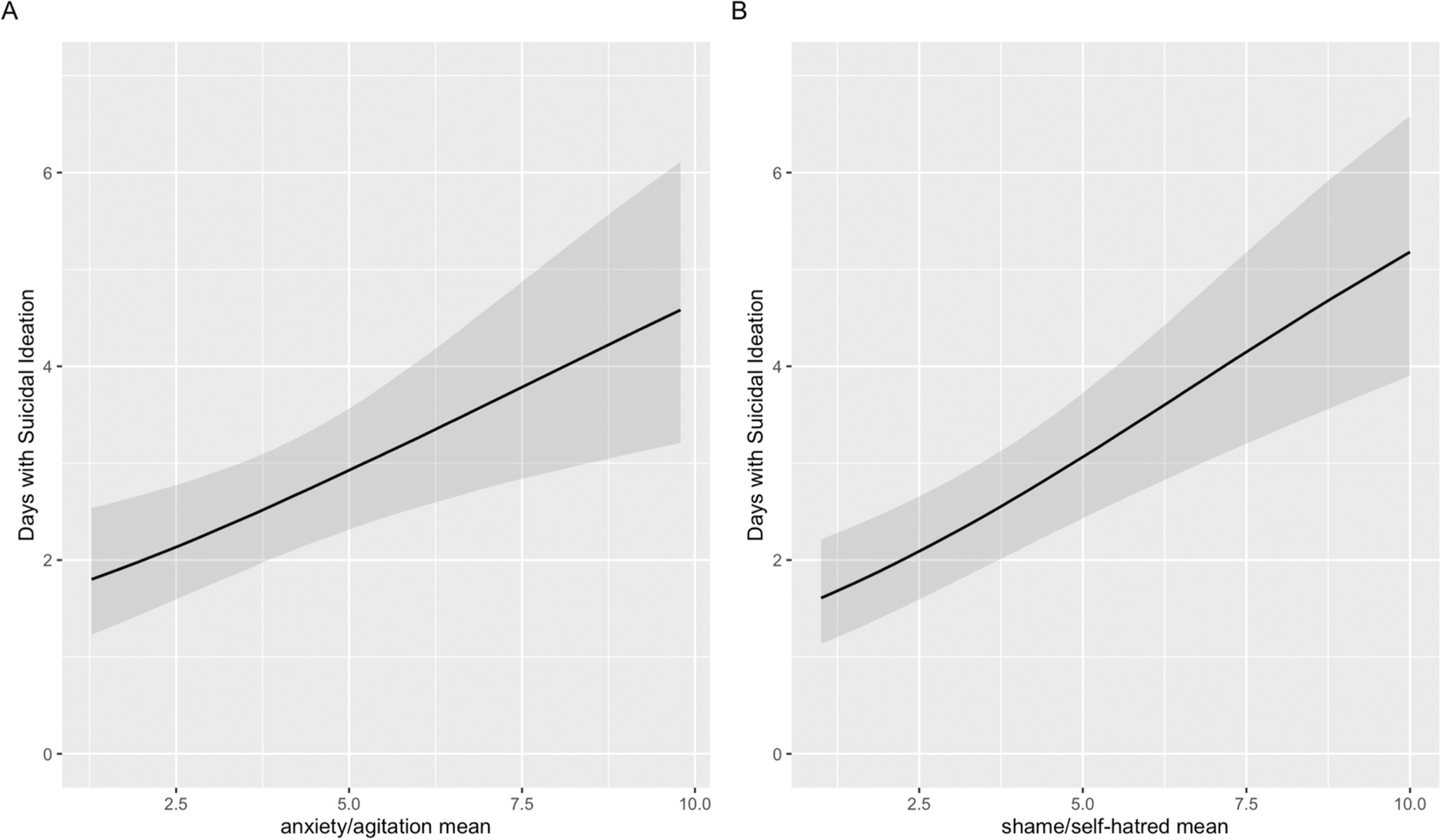
Means of anxiety/agitation (1A) and shame/self-hatred (1B) during hospitalization both predict the number of days with suicidal thoughts after discharge in a zero-inflated binomial multiple regression model with these two NA variables as predictors.
Predicting Post-Discharge Suicide Attempt
Results for the four bivariate logistic regression models using each NA variable to predict suicide attempt after discharge are presented in the top part of Table 3 (n = 64). The mean and variability of shame/self-hatred predicted suicide attempt, whereas the mean and variability of anxiety/agitation did not. In the multiple regression model, when controlling for mean levels of shame/self-hatred, variability of shame/self-hatred (and vice-versa) predicted suicide attempt (bottom part of Table 3; Figure 2). These findings held when controlling for the number of completed EMA surveys, % EMA compliance, length of hospital stay, and/or study wave.5
Table 3.
Fixed effects from the logistic regression models predicting suicide attempt after discharge
| Bivariate models | Main Effects |
|||
|---|---|---|---|---|
| Median | 95% HDI | pd | Odds ratio | |
|
| ||||
| (Intercept) | −2.88 | [−4.85, −0.99] | 100.0% | 0.06 |
| Anxiety/agitation mean | 0.22 | [−0.14, 0.57] | 89.4% | 1.25 |
|
| ||||
| (Intercept) | −2.53 | [−4.17, −0.98] | 99.9% | 0.08 |
| Anxiety/agitation variability | 0.63 | [−0.58, 1.82] | 84.9% | 1.88 |
|
| ||||
| (Intercept) | −3.86 | [−6.01, −1.99] | 100.0% | 0.02 |
| Shame/self-hatred mean | 0.41 | [0.07, 0.74] | 99.4%* | 1.51 |
|
| ||||
| (Intercept) | −3.38 | [−5.23, −1.61] | 100.0% | 0.03 |
| Shame/self-hatred variability | 1.36 | [0.06, 2.74] | 98.4%* | 3.90 |
|
| ||||
| Multiple regression model | ||||
|
| ||||
| (Intercept) | −6.29 | [−10.27, −3.12] | 100.0% | 0.00 |
| Shame/self-hatred mean | 0.52 | [0.11, 0.96] | 99.6%* | 1.68 |
| Shame/self-hatred variability | 1.56 | [0.17, 3.11] | 98.9%* | 4.76 |
Note. The top part of the table presents results from four bivariate models using each NA variable as the sole predictor, and the bottom part presents results from the multiple regression model including only those NA variables that predicted suicide attempt in the bivariate models. HDI = Highest Density Interval. pd = probability of direction (“significant” effects are marked with a *). n = 64 participants.
Figure 2.
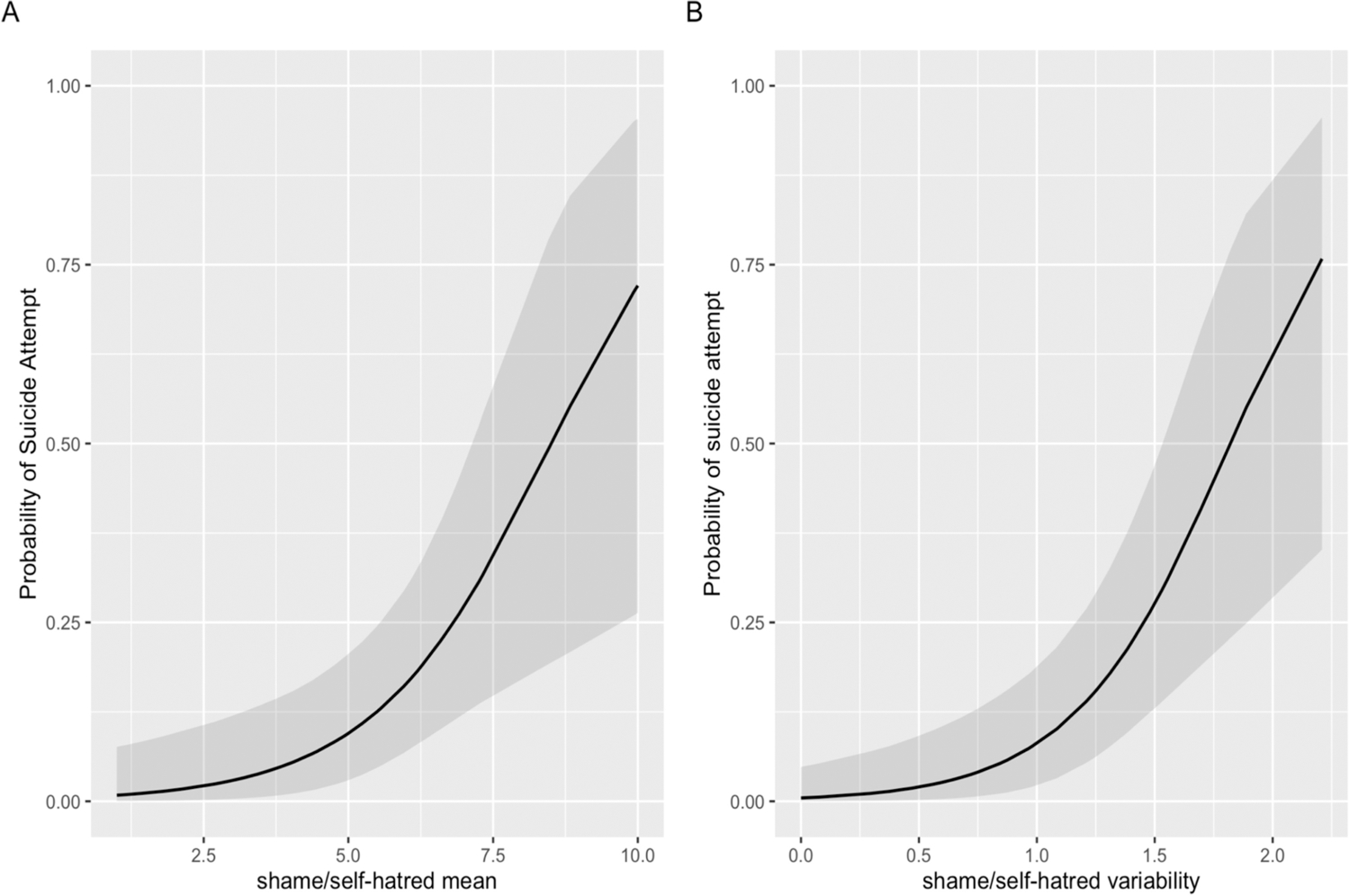
Shame/self-hatred mean (2A) and variability (2B) during hospitalization predict probability of suicide attempt after discharge in a multiple logistic regression model with these two NA variables as predictors.
Discussion
The associations between patterns of NA and STBs over short, clinically useful timeframes are not well-understood. In this study, we observed different associations between patterns of two types of NA during psychiatric hospitalization and post-discharge STBs. Mean levels (but not the variability) of anxiety/agitation and shame/self-hatred during hospitalization predicted days with suicidal thoughts after discharge, whereas the mean and variability of shame/self-hatred (but not anxiety/agitation) predicted post-discharge suicide attempt.
Higher overall levels of both anxiety/agitation and shame/self-hatred during hospitalization predicted more days with suicidal thoughts in the two weeks post-discharge. These findings align with the wealth of theory associating a wide range of NA or related cognitive-affective experiences to STBs (e.g., Beck, 1967; Joiner, 2005; Linehan, 1993), as well as increasing recent EMA work demonstrating that many different momentary NA states prospectively predict momentary suicidal thoughts (e.g., Ben-Zeev et al., 2012; Hallensleben et al., 2019; Kleiman et al., 2017). To the extent that suicidal thoughts function to regulate or relieve aversive NA states (e.g., Kleiman et al., 2018), one would expect more intense levels of NA during hospitalization to increase the frequency of suicidal thoughts after discharge.
Perhaps more surprising is that neither the variability of anxiety/agitation nor shame/self-hatred predicted suicidal thoughts, even in bivariate models. These results are consistent with some (e.g., Links et al., 2007), but not all (e.g., Palmier-Claus, Taylor, Gooding, et al., 2012; Victor et al., in press), prior work on patterns of NA and STBs. In our study, the vast majority of variance in NA during hospitalization occurred between (not within) people, which may be attributed to unique characteristics of the in-hospital monitoring period: a secure, treatment-intensive environment that may result in more stable NA than what unfolds in the “real-world.” Ultimately this may have restricted the potential to observe prospective associations between NA variability during hospitalization and post-discharge suicidal thoughts. Future work that examines more complex or time-sensitive metrics of variability that typically require more (and ideally, shorter intervals between) EMA observations than our data to be estimated reliably (e.g., Dejonckheere et al., 2020; Ebner-Priemer & Sawitzki, 2007) will help shed light on whether and in what contexts specific types of variations in NA predict suicidal thoughts. Probability of acute change, for example, may be one promising temporal metric (Berner et al., 2017).
Both the mean and the variability of shame/self-hatred predicted post-discharge suicide attempt. This finding contributes to growing empirical support (e.g., Sheehy et al., 2019) for the role of shame in STBs (Hastings et al., 2000; Maltsberger et al., 2011; Shneidman, 1993). Shame and self-hatred may be particularly important in suicidal behavior due to how closely linked these aversive affective experiences are to how individuals perceive themselves; self-injurious behavior may then serve as a relevant way to regulate such self-directed emotions (Sheehy et al., 2019). Our findings suggest that not only higher levels of, but also greater variations in, these emotions predict suicidal behavior. Studies testing interventions aimed to reduce overall levels of, as well as stabilize, shame/self-hatred (e.g., cognitive processing, self-compassion) on STBs may be useful for both shedding light on whether a causal relationship between shame/self-hatred and STBs exists, and informing clinical practice during high-risk periods.
That neither the mean nor the variability of anxiety/agitation during hospitalization predicted suicide attempt (even in bivariate models) was unexpected given accumulating evidence that both associates disorders characterized by severe anxiety or agitation with the transition from suicidal thoughts to behavior (e.g., Nock et al., 2010) and implicates agitation as a short-term predictor of suicide attempt (e.g., Fawcett et al., 1990; Rogers et al., 2016). It may be that the experience of anxiety/agitation is most relevant for predicting suicidal behavior over even shorter time windows (e.g., minutes, hours, days) than the four weeks captured here.
Regarding study limitations, the duration of the EMA period corresponded to length of inpatient stay and thus was inconsistent across participants and relatively short. Coupled with just over 50% compliance, which was likely due to the severe patient population, compensation for each day of participation (not EMA surveys), and that participants were instructed not to respond to EMA prompts while in treatment sessions, this resulted in fewer observations compared to other EMA NA studies (Dejonckheere et al., 2019). As about 20% of the original sample did fewer than 3 EMA surveys (and were not included the present analyses) and about 22% of included participants did not complete a follow-up survey after discharge, it is possible that remaining participants differed from the general population of suicidal psychiatric inpatients on relevant characteristics (e.g., functioning) that we did not measure. Other limitations are the small number of suicide attempts (potentially resulting in unstable model parameters), retrospective nature of follow-up surveys, and that we combined data from two study waves that used a different number of EMA prompts per day, which may have introduced bias and reduced precision in estimates of NA patterns.
Despite these limitations, this study extends previous work on the role of patterns and types of NA in predicting STBs. Future studies that advance the frequency, duration, and types (e.g., physiological) of data streams to collect information on NA have the potential to uncover nuanced relationships between patterns and types of affective experience and STBs, including what may be key individual- and contextual-level differences. This line of inquiry has the potential to inform the development of novel emotion-focused interventions for suicidal individuals, perhaps using scalable digital formats that deliver real-time support in response to individuals’ ever-fluctuating affective states (e.g., Nahum-Shani et al., 2018).
Supplementary Material
Funding:
This research was funded by grant K23 MH120436 (KHB) from the National Institute of Mental Health, and the Chet and Will Griswold Suicide Prevention Fund (MKN).
Footnotes
Financial interests: The authors have no relevant financial or non-financial interests to disclose.
Data, material, and code availability: The data generated during and analyzed during the current study are not publicly available due the sensitive nature of these data and vulnerable nature of the study sample but are available from the corresponding author on reasonable request. Code is available from the corresponding author on request.
Preregistration: The analyses conducted here were not formally pre-registered.
Ethics approval: All procedures performed in this study involving human participants were approved by the Institutional Review Board at the Massachusetts General Hospital (IRB# 2015P000598) with reliance agreements established with other involved institutions.
Consent: Informed consent was obtained from all individual participants included in the study.
Data from the first wave of this study have been reported in two publications (for which aims and analyses do not overlap with this report): Mou et al. (2018), which used 35 of 37 participants and Kleiman et al. (2017; Study 2), which used 36 of 37 participants.
In both study waves, the second question of the four-week follow-up survey (“about how many days in the past four weeks did you think of killing yourself?”) had an error such that the maximum number of days participants could enter was 14 (not 28). Thus, we did not analyze the “how many days” question from the four-week follow-up.
We operationalized variability with SD instead of RMSSD or other more complex metrics for two reasons. (1) The convention is to require more data points (e.g., 20 in Dejonckheere et al., 2019) than we had here to calculate more complex, time-dependent affective metrics, whereas SD is not time-dependent (Trull et al., 2015). To reliably estimate the RMSSD, we would have needed to restrict to only those participants who completed higher numbers of EMA surveys which would have biased our sample and considerably reduced our N. (2) SD and RMSSD overlap and are highly correlated (e.g., Hisler et al., 2020; Wendt et al., 2019), and we were more interested in the relationship of NA variability with STBs rather than the unique effects of one index of variability when controlling for another.
In two additional sensitivity analyses, (1) when excluding the 5 participants who did not complete the two-week follow-up but denied suicidal thoughts since discharge on the four-week follow-up, the same findings also held. (2) When excluding participants who completed fewer than 10 EMA surveys, only mean levels of shame/self-hatred (not anxiety/agitation) predicted days with suicidal thoughts.
When excluding the 5 participants coded as non-attempters based only on two-week (not four-week) follow-up survey data, and when excluding participants who completed fewer than 10 EMA surveys, the same findings held.
References
- Abramson LY, Alloy LB, Hogan ME, Whitehouse WG, Hankin BL, & Cornette MM (2000). The hopelessness theory of suicidality. In In Joiner TE & Rudd MD (Eds.), Suicide science: Expanding the boundaries (pp. 17–32). Kluwer Academic/Plenum Publishers. [Google Scholar]
- Bakdash JZ, & Marusich LR (2020). Repeated Measures Correlation (0.4.1) [Computer software]. [DOI] [PMC free article] [PubMed]
- Baumeister RF (1990). Suicide as escape from self. Psychological Review, 97(1), 90–113. 10.1037/0033-295X.97.1.90 [DOI] [PubMed] [Google Scholar]
- Beck AT (1967). Depression: Clinical, Experimental, and Theoretical Aspects. Harper & Row. [Google Scholar]
- Ben-Zeev D, Young MA, & Depp CA (2012). Real-time predictors of suicidal ideation: Mobile assessment of hospitalized depressed patients. Psychiatry Research, 197(1–2), 55–59. 10.1016/j.psychres.2011.11.025 [DOI] [PubMed] [Google Scholar]
- Berner LA, Crosby RD, Cao L, Engel SG, Lavender JM, Mitchell JE, & Wonderlich SA (2017). Temporal associations between affective instability and dysregulated eating behavior in bulimia nervosa. Journal of Psychiatric Research, 92, 183–190. 10.1016/j.jpsychires.2017.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bürkner P-C (2017). brms: An R Package for Bayesian Multilevel Models Using Stan. Journal of Statistical Software, 80(1). 10.18637/jss.v080.i01 [DOI] [Google Scholar]
- Busch KA, Fawcett J, & Jacobs DG (2003). Clinical correlates of inpatient suicide. The Journal of Clinical Psychiatry, 64(1), 14–19. [DOI] [PubMed] [Google Scholar]
- Cameron AY, Shea MT, & Randall AB (2020). Acute Shame Predicts Urges for Suicide but not for Substance Use in a Veteran Population. Suicide and Life-Threatening Behavior, 50(1), 292–299. 10.1111/sltb.12588 [DOI] [PubMed] [Google Scholar]
- Chung D, Hadzi-Pavlovic D, Wang M, Swaraj S, Olfson M, & Large M (2019). Meta-analysis of suicide rates in the first week and the first month after psychiatric hospitalisation. BMJ Open, 9(3), e023883. 10.1136/bmjopen-2018-023883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung DT, Ryan CJ, Hadzi-Pavlovic D, Singh SP, Stanton C, & Large MM (2017). Suicide Rates After Discharge From Psychiatric Facilities: A Systematic Review and Meta-analysis. JAMA Psychiatry, 74(7), 694. 10.1001/jamapsychiatry.2017.1044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dejonckheere E, Mestdagh M, Houben M, Rutten I, Sels L, Kuppens P, & Tuerlinckx F (2019). Complex affect dynamics add limited information to the prediction of psychological well-being. Nature Human Behaviour, 3(5), 478–491. 10.1038/s41562-019-0555-0 [DOI] [PubMed] [Google Scholar]
- Dejonckheere E, Mestdagh M, Kuppens P, & Tuerlinckx F (2020). Reply to: Context matters for affective chronometry. Nature Human Behaviour. 10.1038/s41562-020-0861-6 [DOI] [PubMed] [Google Scholar]
- Depaoli S, & van de Schoot R (2017). Improving transparency and replication in Bayesian statistics: The WAMBS-Checklist. Psychological Methods, 22(2), 240–261. 10.1037/met0000065 [DOI] [PubMed] [Google Scholar]
- Ebner-Priemer UW, & Sawitzki G (2007). Ambulatory Assessment of Affective Instability in Borderline Personality Disorder. European Journal of Psychological Assessment, 23(4), 238–247. 10.1027/1015-5759.23.4.238 [DOI] [Google Scholar]
- Fawcett J, Scheftner WA, Fogg L, Clark DC, Young MA, Hedeker D, & Gibbons R (1990). Time-related predictors of suicide in major affective disorder. The American Journal of Psychiatry, 147(9), 1189–1194. 10.1176/ajp.147.9.1189 [DOI] [PubMed] [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, & Nock MK (2017). Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin, 143(2), 187–232. 10.1037/bul0000084 [DOI] [PubMed] [Google Scholar]
- Gelman A, Carlin JB, Stern HS, Dunson DB, Vehtari A, & Rubin D (2014). Bayesian data analysis (Vol. 2). CRC Press. [Google Scholar]
- Glenn CR, & Nock MK (2014). Improving the Short-Term Prediction of Suicidal Behavior. American Journal of Preventive Medicine, 47(3 Suppl 2), S176. 10.1016/j.amepre.2014.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall DB (2000). Zero-Inflated Poisson and Binomial Regression with Random Effects: A Case Study. Biometrics, 56(4), 1030–1039. 10.1111/j.0006-341X.2000.01030.x [DOI] [PubMed] [Google Scholar]
- Hall RCW, Platt DE, & Hall RCW (1999). Suicide Risk Assessment: A Review of Risk Factors for Suicide in 100 Patients Who Made Severe Suicide Attempts. Psychosomatics, 40(1), 18–27. 10.1016/S0033-3182(99)71267-3 [DOI] [PubMed] [Google Scholar]
- Hallensleben N, Glaesmer H, Forkmann T, Rath D, Strauss M, Kersting A, & Spangenberg L (2019). Predicting suicidal ideation by interpersonal variables, hopelessness and depression in real-time. An ecological momentary assessment study in psychiatric inpatients with depression. European Psychiatry, 56(1), 43–50. 10.1016/j.eurpsy.2018.11.003 [DOI] [PubMed] [Google Scholar]
- Hastings ME, Northman LM, & Tangney JP (2000). Shame, guilt, and suicide. In Suicide science: Expanding the boundaries. (In: Joiner T, Rudd DM, editors., pp. 67–79). Kluwer Academic/Plenum Publishers. [Google Scholar]
- Hisler GC, Krizan Z, DeHart T, & Wright AGC (2020). Neuroticism as the intensity, reactivity, and variability in day-to-day affect. Journal of Research in Personality, 87, 103964. 10.1016/j.jrp.2020.103964 [DOI] [Google Scholar]
- Humber N, Emsley R, Pratt D, & Tarrier N (2013). Anger as a predictor of psychological distress and self-harm ideation in inmates: A structured self-assessment diary study. Psychiatry Research, 210(1), 166–173. 10.1016/j.psychres.2013.02.011 [DOI] [PubMed] [Google Scholar]
- Husky M, Swendsen J, Ionita A, Jaussent I, Genty C, & Courtet P (2017). Predictors of daily life suicidal ideation in adults recently discharged after a serious suicide attempt: A pilot study. Psychiatry Research, 256, 79–84. 10.1016/j.psychres.2017.06.035 [DOI] [PubMed] [Google Scholar]
- Joiner T (2005). Why people die by suicide. Harvard University Press. [Google Scholar]
- Kleiman EM, Coppersmith DDL, Millner AJ, Franz PJ, Fox KR, & Nock MK (2018). Are suicidal thoughts reinforcing? A preliminary real-time monitoring study on the potential affect regulation function of suicidal thinking. Journal of Affective Disorders, 232, 122–126. 10.1016/j.jad.2018.02.033 [DOI] [PubMed] [Google Scholar]
- Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, & Nock MK (2017). Examination of real-time fluctuations in suicidal ideation and its risk factors: Results from two ecological momentary assessment studies. Journal of Abnormal Psychology, 126(6), 726–738. 10.1037/abn0000273 [DOI] [PubMed] [Google Scholar]
- Kruschke JK (2015). Doing Bayesian Data Analysis: A Tutorial with R, JAGS, and Stan (2nd ed.). Elsevier Inc. [Google Scholar]
- Kruschke JK, & Liddell TM (2018). The Bayesian New Statistics: Hypothesis testing, estimation, meta-analysis, and power analysis from a Bayesian perspective. Psychonomic Bulletin & Review, 25(1), 178–206. 10.3758/s13423-016-1221-4 [DOI] [PubMed] [Google Scholar]
- Linehan M (1993). Cognitive-behavioral treatment of borderline personality disorder. Guilford Press. [Google Scholar]
- Links PS, Eynan R, Heisel MJ, Barr A, Korzekwa M, McMain S, & Ball JS (2007). Affective Instability and Suicidal Ideation and Behavior in Patients with Borderline Personality Disorder. Journal of Personality Disorders, 21(1), 72–86. 10.1521/pedi.2007.21.1.72 [DOI] [PubMed] [Google Scholar]
- Lüdecke D (2020). sjPlot: Data Visualization for Statistics in Social Science (2.8.4) [Computer software]. https://CRAN.R-project.org/package=sjPlot
- Makowski D, Ben-Shachar M, & Lüdecke D (2019). bayestestR: Describing Effects and their Uncertainty, Existence and Significance within the Bayesian Framework. Journal of Open Source Software, 4(40), 1541. 10.21105/joss.01541 [DOI] [Google Scholar]
- Makowski D, Ben-Shachar MS, Chen SHA, & Lüdecke D (2019). Indices of Effect Existence and Significance in the Bayesian Framework. Frontiers in Psychology, 10. 10.3389/fpsyg.2019.02767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maltsberger JT (2004). The descent into suicide. The International Journal of Psychoanalysis, 85(3), 653–668. 10.1516/3C96-URET-TLWX-6LWU [DOI] [PubMed] [Google Scholar]
- Maltsberger JT, Goldblatt MJ, Ronningstam E, Weinberg I, & Schechter M (2011). Traumatic Subjective Experiences Invite Suicide. The Journal of the American Academy of Psychoanalysis and Dynamic Psychiatry, 39(4), 671–693. 10.1521/jaap.2011.39.4.671 [DOI] [PubMed] [Google Scholar]
- Mou D, Kleiman EM, Fedor S, Beck S, Huffman JC, & Nock MK (2018). Negative affect is more strongly associated with suicidal thinking among suicidal patients with borderline personality disorder than those without. Journal of Psychiatric Research, 104, 198–201. 10.1016/j.jpsychires.2018.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahum-Shani I, Smith SN, Spring BJ, Collins LM, Witkiewitz K, Tewari A, & Murphy SA (2018). Just-in-Time Adaptive Interventions (JITAIs) in Mobile Health: Key Components and Design Principles for Ongoing Health Behavior Support. Annals of Behavioral Medicine, 52(6), 446–462. 10.1007/s12160-016-9830-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson NA, & Kessler RC (2010). Mental disorders, comorbidity and suicidal behavior: Results from the National Comorbidity Survey Replication. Molecular Psychiatry, 15(8), 868–876. 10.1038/mp.2009.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Park JM, Finn CT, Deliberto TL, Dour HJ, & Banaji MR (2010). Measuring the Suicidal Mind: Implicit Cognition Predicts Suicidal Behavior. Psychological Science, 21(4), 511–517. 10.1177/0956797610364762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson M (2017). Suicide Risk After Psychiatric Hospital Discharge. JAMA Psychiatry, 74(7), 669. 10.1001/jamapsychiatry.2017.1043 [DOI] [PubMed] [Google Scholar]
- Palmier-Claus JE, Taylor PJ, Gooding P, Dunn G, & Lewis SW (2012). Affective variability predicts suicidal ideation in individuals at ultra-high risk of developing psychosis: An experience sampling study: Affective variability as a predictor of suicidal ideation. British Journal of Clinical Psychology, 51(1), 72–83. 10.1111/j.2044-8260.2011.02013.x [DOI] [PubMed] [Google Scholar]
- Palmier-Claus JE, Taylor PJ, Varese F, & Pratt D (2012). Does unstable mood increase risk of suicide? Theory, research and practice. Journal of Affective Disorders, 143(1–3), 5–15. 10.1016/j.jad.2012.05.030 [DOI] [PubMed] [Google Scholar]
- Qin P, & Nordentoft M (2005). Suicide Risk in Relation to Psychiatric Hospitalization: Evidence Based on Longitudinal Registers. Archives of General Psychiatry, 62(4), 427. 10.1001/archpsyc.62.4.427 [DOI] [PubMed] [Google Scholar]
- R Core Team. (2019). R: A language and environment for statistical computing. R Foundation for Statistical Computing. [Google Scholar]
- Ribeiro JD, Franklin JC, Fox KR, Bentley KH, Kleiman EM, Chang BP, & Nock MK (2016). Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: A meta-analysis of longitudinal studies. Psychological Medicine, 46(2), 225. 10.1017/S0033291715001804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers ML, Ringer FB, & Joiner TE (2016). A meta-analytic review of the association between agitation and suicide attempts. Clinical Psychology Review, 48, 1–6. 10.1016/j.cpr.2016.06.002 [DOI] [PubMed] [Google Scholar]
- Sheehy K, Noureen A, Khaliq A, Dhingra K, Husain N, Pontin EE, Cawley R, & Taylor PJ (2019). An examination of the relationship between shame, guilt and self-harm: A systematic review and meta-analysis. Clinical Psychology Review, 73, 101779. 10.1016/j.cpr.2019.101779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepard DS, Gurewich D, Lwin AK, Reed GA, & Silverman MM (2016). Suicide and Suicidal Attempts in the United States: Costs and Policy Implications. Suicide and Life-Threatening Behavior, 46(3), 352–362. 10.1111/sltb.12225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shneidman ES (1993). Commentary: Suicide as Psychache: The Journal of Nervous and Mental Disease, 181(3), 145–147. 10.1097/00005053-199303000-00001 [DOI] [PubMed] [Google Scholar]
- Statistics|Suicide|Violence Prevention|Injury Center|CDC. (2018, September 7). https://www.cdc.gov/violenceprevention/suicide/statistics/index.html
- Trull TJ, Lane SP, Koval P, & Ebner-Priemer UW (2015). Affective Dynamics in Psychopathology. Emotion Review, 7(4), 355–361. 10.1177/1754073915590617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victor SE, Brown SL, & Scott LN (in press). Prospective and concurrent affective dynamics in self-injurious thoughts and behaviors: An examination in young adult women. Behavior Therapy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Wendt LP, Wright AGC, Pilkonis PA, Woods WC, Denissen JJA, Kühnel A, & Zimmermann J (2019). Indicators of affect dynamics: Structure, reliability, and personality correlates [Preprint]. PsyArXiv. 10.31234/osf.io/nyqst [DOI]
- Wolak M (2017). Facilitating Estimation of the Intraclass Correlation Coefficient. https://github.com/matthewwolak/ICC
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


