Fig. 10: Model of factors contributing to HCA-induced placental and fetal lung inflammation.
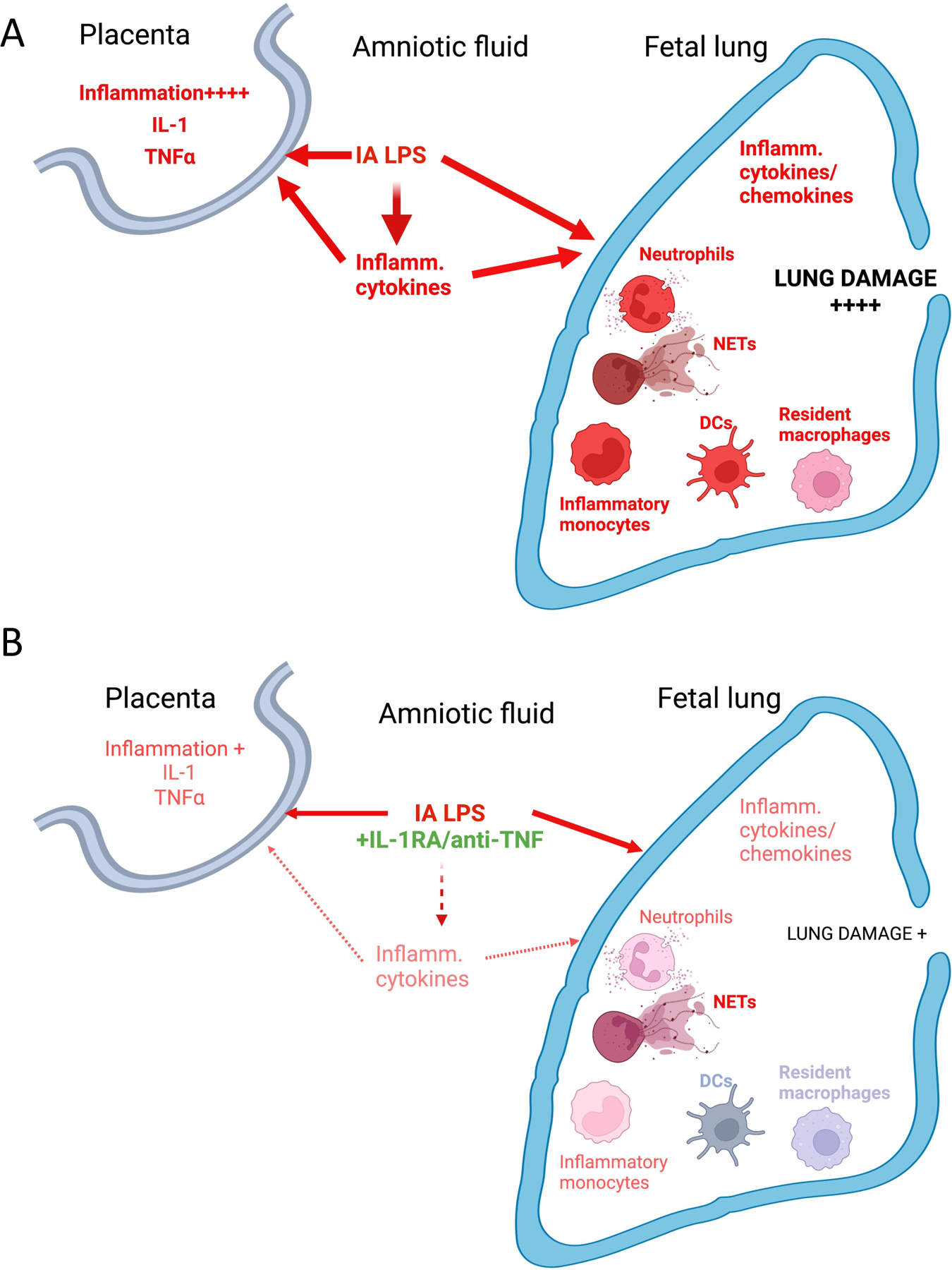
(A) IA LPS injection induces a mixture of TLR-dependent, and IL-1/TNFα signaling pathway-mediated activation in the placenta (described in more detail in 33,35). In the lung, IA LPS induces production of inflammatory cytokines/chemokines, recruitment of activated neutrophils and monocytes, as well as activation of resident myeloid cells (macrophages and DCs). Together, these changes contribute to the extensive lung damage observed in HCA-exposed fetuses (described in more detail in 46). (B) Co-administration of IL-1RA and anti TNFα in the context of LPS exposure blunts placental inflammation. Although inflammatory cell recruitment and NET formation is not significantly diminished, production of inflammatory cytokines/chemokines, activation of recruited and resident myeloid cells is blunted. Lung damage is also significantly decreased by co-administration of IL-1 and TNFα blocking agents. Created with BioRender.com.
