Figure 2. The protective versus pathogenic adaptive immune responses in COVID-19.
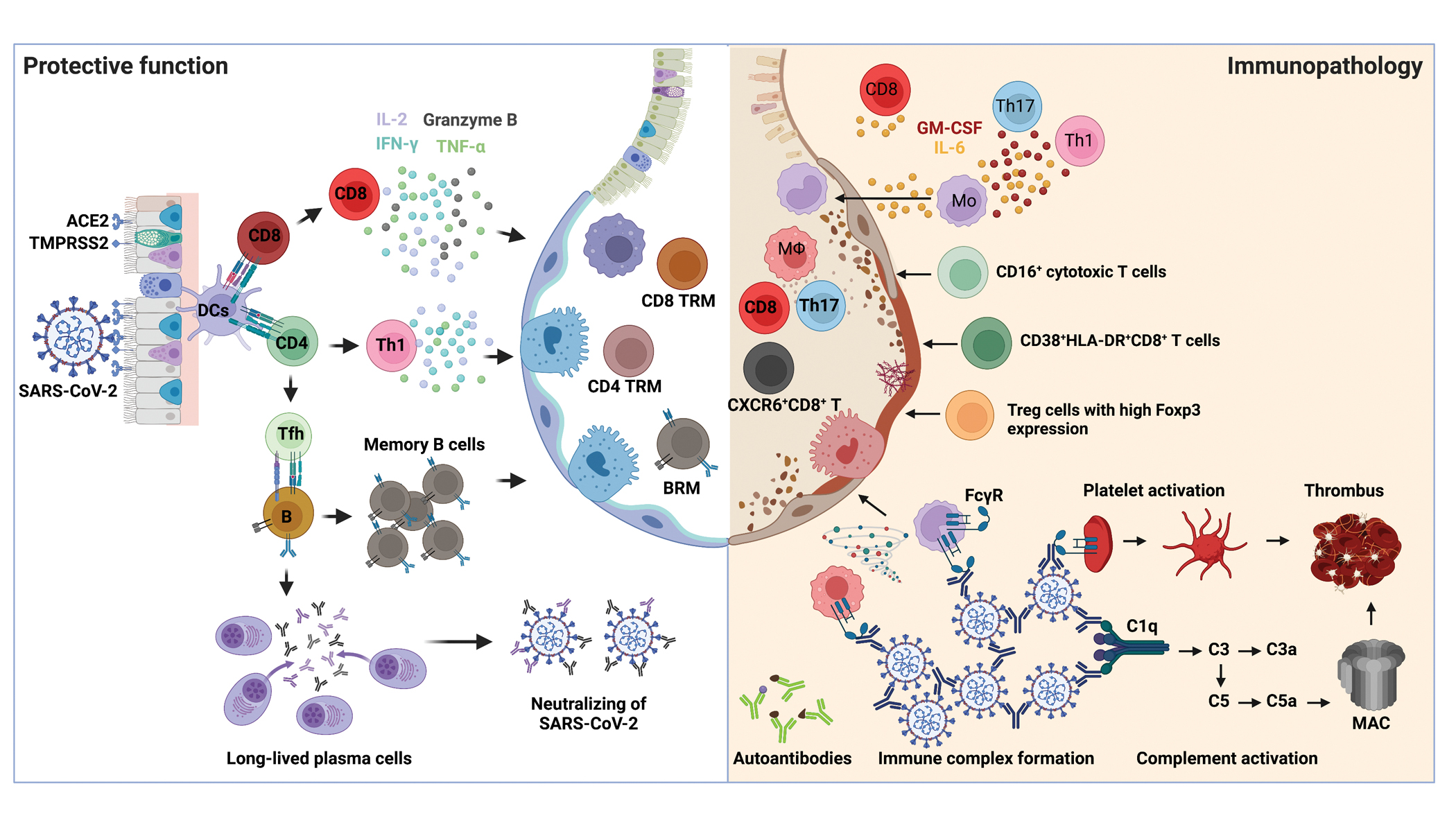
Left: when SARS-CoV-2 invading host respiratory tract, viral antigen can be detected and presented by DCs to either CD4+ T or CD8+ T cells for their activation. Naïve CD4+ T cells mainly differentiate into T helper 1 (Th1) and T follicular helper cells (Tfh). Th1 cells possess antiviral effects by producing higher levels of IFN-γ, TNF and IL-2. Tfh cells providing help to B cells for somatic hypermutations and affinity maturation of germinal center reactions to generate memory B cells and long-lived antibody-producing plasma cells. The viral specific antibodies secreted by plasma cells play a protective role by neutralizing virus. Activated CD8+ T cells producing effector cytokines and cytotoxic molecules, including IFN-γ, TNF, IL-2 and granzyme B, controlling viral infections. After viral clearance, memory CD4+ T, CD8+ T and B cells are developed in the circulation and lungs to protect against secondary infections. Right: excessive T cell responses are associated with severe COVID-19, including IL-6- and GM-CSF-producing Th1 or Th17 cells, CD16+ cytotoxic T cells, CXCR6+ CD8+ T cells, as well as dysregulated Treg cells. On the other hand, the production of autoantibodies, the formation of immune complexes, and complement activation also contribute to the disease progression of COVID-19.
