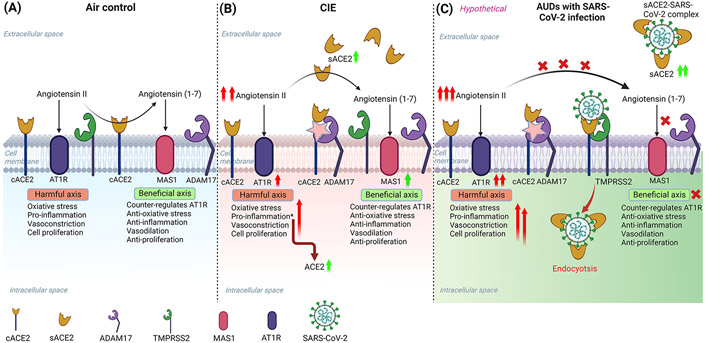
Figure 11: Schematic overview of the possible mechanism for increased susceptibility to SARS-CoV-2 infection in alcohol use disorder patients.
(A) Baseline mechanism: Angiotensin-converting enzyme 2 (ACE2) is a key regulator of the Renin-angiotensin system (RAS) that controls the hyperactivation of the Angiotensin II-AT1R pathway by converting Angiotensin II to Angiotensin (1-7) and activating MAS1 receptor-mediated pathway. (B) RAS perturbation by ethanol intake: After ethanol intoxication, the homeostatic balance of the RAS in the CNS is disturbed due to higher Angiotensin II levels, and the hyperactivation of the Angiotensin II-AT1R axis leads to neuroinflammation. A soluble form of ACE2 (sACE2) levels are increased after ethanol due to higher levels of ADAM17 (ACE2 sheddase) in the CNS, to cope with Angiotensin II triggered inflammation. (C) A hypothetical model explaining the susceptibility of AUDs to increased risk for SARS-CoV-2 infection: Ethanol exacerbates the levels of sACE2 to compensate for the harmful effects of Angiotensin II in the CNS. However, after infection with SARS-CoV-2, the virus hijacks the sACE2 and gets internalized into the cell by endocytosis, thereby reducing the circulating sACE2 and perturbing the homeostasis in the RAS leading to neuroinflammation and other pathological complications. The illustration was created in BioRender (BioRender.com).