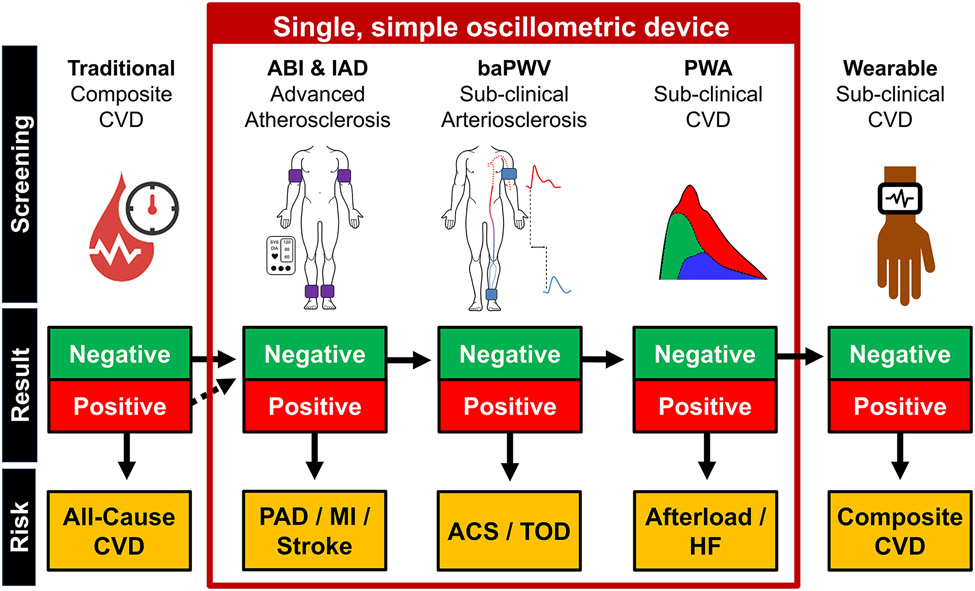
FIGURE 3.
Example of a potential future clinical practice model in the form of a decision tree. In this example, traditional risk factors will be measured and used to stratify all-cause cardiovascular disease (CVD) risk. Subsequently, ankle brachial index (ABI) and systolic interarm blood pressure difference (IAD) are measured. Positive ABI and/or IAD (i.e., unhealthy, ABI score < 0.9 or > 1.4 and/or IAD ≥ 10 mmHg) scores indicates peripheral arterial disease (PAD) and increased myocardial infarction and stroke risk. If the ABI and IAD scores are negative (i.e. healthy, ABI: between 0.9 and 1.4; IAD < 10 mmHg), the additional information provided by brachial-ankle pulse wave velocity (baPWV) and pulse wave analysis (PWA) will be considered. A positive baPWV indicates increased risk for all-cause cardiovascular events, acute coronary syndrome (ACS) and/or target organ damage (TOD) risk. A positive PWA score may indicate increased afterload and increased heart failure (HF) risk. If both the baPWV and PWA scores are negative, the participant is sent home with a wearable device to collect ambulatory PWA and baPWV data, from which a composite CVD risk score is derived.