Abstract
Introduction:
Cerebrovascular dysfunction, characterized by increased brain pulsatile flow, reduced cerebrovascular reactivity, and cerebral hypoperfusion precedes the onset of dementia and is linked to cognitive dysfunction. Autosomal dominant polycystic kidney disease (ADPKD) may increase the risk of dementia, and intracranial aneurysms are more prevalent in ADPKD patients. However, cerebrovascular function has not been previously characterized in patients with ADPKD.
Methods:
Using transcranial Doppler, we compared middle cerebral artery (MCA) pulsatility index (PI; cerebrovascular stiffness) and MCA blood velocity response to hypercapnia (normalized for blood pressure and end-tidal CO2; cerebrovascular reactivity) in patients with early-stage ADPKD vs. age-matched healthy controls. We also administered the NIH cognitive toolbox (cognitive function) and measured carotid-femoral pulse-wave velocity (PWV; aortic stiffness).
Results:
Fifteen participants with ADPKD (9F, 27±4 yrs, eGFR: 106±22 ml/min/1.73m2) were compared to 15 healthy controls (8F, 29±4 yrs, eGFR: 109±14 ml/min/1.73m2). MCA PI was unexpectedly lower in ADPKD (0.71±0.07) vs. controls (0.82±0.09 A.U.; p<0.001); however, normalized MCA blood velocity in response to hypercapnia did not differ between groups (2.0±1.2 vs. 2.1±0.8 %Δ/mmHg; p=0.85). Lower MCA PI was associated with a lower crystalized composite score (cognition), which persisted after adjustment for age, sex, eGFR, and education (β = 0.58, p=0.007). There was no association of MCA PI with carotid-femoral PWV (r=0.01, p=0.96), despite greater carotid-femoral PWV in ADPKD, suggesting MCA PI reflects vascular properties other than arterial stiffness (such as low wall shear stress) in ADPKD.
Discussion/Conclusion:
MCA PI is lower in patients with ADPKD. Follow-up research on this observation is merited, as low PI has been associated with intracranial aneurysm in other populations.
Keywords: ADPKD, cardiovascular, cerebrovascular, polycystic kidney disease
Introduction
Although the hallmark of autosomal dominant polycystic kidney disease (ADPKD) is the development and continued growth of multiple kidney cysts that results in end-stage kidney disease in the majority of patients [1], the leading causes of death are cardiovascular complications and disorders [2, 3]. We previously demonstrated that arterial dysfunction develops very early in the course of ADPKD (i.e., in young patients, prior to a decline in kidney function), as evidenced by impaired brachial artery flow-mediated dilation (a measure of endothelium-dependent dilation) and increased carotid-femoral pulse-wave velocity (PWV; a measure of large elastic artery stiffness) [4]. It is biologically plausible that arterial dysfunction may also occur in the cerebrovasculature in individuals with ADPKD. Research on patients with early-stage ADPKD has been recognized as an important priority, as early intervention may be necessary for the greatest benefit in this life-long, slowly progressive disease [5].
There has been increasing recognition of a kidney-brain axis; both organs have similar anatomical, functional, and vascular properties increasing vulnerability to vascular risk factors, including local autoregulation and high flow/low vascular resistance [6, 7]. Cerebrovascular dysfunction is strongly associated with cognitive dysfunction, precedes the clinical onset of dementia, and is characterized by cerebral hypoperfusion, reduced cerebrovascular reactivity, and increased pulsatile blood flow within the brain [8, 9]. In the setting of high aortic stiffness, blood flow is delivered to the brain with higher pulsatile pressure, inducing damage to small cerebral vessels, promoting structural changes, impairing cerebral microvascular function, and contributing to brain atrophy and cognitive impairment [10, 11]. The prevalence of intracranial aneurysm is higher in ADPKD patients compared to the general population, particularly in those with a positive family history, reflecting extrarenal disease complications [12]. Additionally, a recent retrospective cohort study observed an increased incidence of dementia in patients with ADPKD compared to propensity score matched controls [13].
The primary goal of this study was to assess middle cerebral artery (MCA) pulsatility index [PI; a measure of cerebrovascular stiffness] and change in mean blood velocity of the MCA [ΔMVMCA] in response to vasodilatory hypercapnia (a measure of cerebrovascular reactivity) in early-stage patients with ADPKD as compared to age- and sex-matched healthy controls. Additionally, we measured cognitive function, large-artery vascular function (carotid-femoral PWV, an index of aortic stiffness) and circulating markers, and their association with cerebrovascular function. We hypothesized that cerebrovascular dysfunction would be evident in participants with ADPKD and that it would associate with cognitive dysfunction, greater large-artery stiffness, and differences in circulating markers.
Material and Methods
Study Design and Participants
This was a physiological cross-sectional study assessing cerebrovascular function in adults with early-stage ADPKD and age- and sex-matched healthy controls. The associations of cerebrovascular function (PI and ΔMVMCA) with indices of cognitive function and carotid-femoral PWV were also assessed. Participants with early-stage ADPKD were recruited through a recruitment database at the University of Colorado Anschutz Medical Campus. Healthy controls were recruited for comparison to participants with ADPKD through community and university advertisements. Enrollment occurred between April 2019 and March 2022. The study was conducted at the University of Colorado Anschutz Medical Campus Division of Renal Diseases and Hypertension Clinical Vascular Physiology Laboratory. Analysts were blinded to group (ADPKD or healthy control) in all analyses.
Inclusion criteria for both the ADPKD and control group were: 18–35 years of age (to minimize co-morbidities), confirmation of a suitable temporal window for cerebrovascular assessments, an estimated glomerular filtration rate (eGFR) >60 ml/min/1.73 m2 using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [14], non-diabetic, and the ability to provide informed consent. Participants with ADPKD were required to have blood pressure controlled to <140/90 mmHg and a stable antihypertensive regimen (if applicable) at the time of testing. Control participants were free from hypertension (defined as current treatment or blood pressure ≥140/90 mmHg), as well as kidney diseases, cardiovascular disease, and other chronic diseases, as assessed by self-report, screening labs, medical history, and a physical exam (including a resting 12-lead electrocardiogram). Additional exclusion criteria in both groups were current diagnosis and treatment of major depression (based on DSM-IV-TR criteria for Major Depressive Episode), diagnosis of a major psychiatric disorder (e.g., psychosis, schizophrenia, mania, bipolar disorder), dementia, history of stroke, medications likely to affect central nervous system functions (e.g., long-active benzodiazepines), significant sensory or motor deficits that would interfere with cognitive testing, alcohol or other substance abuse (self-report or undergoing treatment), current tobacco or nicotine use or history of use in the last 12 months, oral contraceptives, active infection or antibiotic therapy, hospitalization in the last month, immunosuppressive therapy within the last year, pregnancy or lactation, cannabis use within 2 weeks prior to testing, omega-3 fatty acid and/or antioxidant use within 2 weeks prior to testing, and body mass-index >40 mg/m2 (for accuracy of vascular testing).
Procedures
Screening Measures
A fasted metabolic panel, lipid panel, complete blood count, and urine pregnancy test (women only) were performed. Medical history and demographics and were collected by self-report. Arterial blood pressure was measured in triplicate using an automated oscillometric machine while seated at rest.
Cerebrovascular Measurements
All vascular measurements followed standard recommendations, including an overnight fast [15]. Transcranial Doppler (TCD; Lucid M1 System, NovaSignal, Los Angeles, CA) was used to assess cerebrovascular reactivity, by measuring ΔMVMCA in response to a vasodilatory hypercapnic challenge (i.e., via CO2 breathing), as described previously [16, 17]. A 2-MHz TCD ultrasound probe positioned at the temporal window on the right side of the body and held in place by an adjustable headband to continuously assess MCA blood velocity (MCAv). The temporal window is the thinnest portion of the temporal bone and thus allows ideal access for Doppler ultrasonography of the circle of Willis arteries, including the MCA [18]. Following a baseline recording breathing room air, subjects breathed room air mixed with 5% CO2 (balanced nitrogen), which induces mild hypercapnia. Each condition was recorded for 5 minutes with paced breathing using a metronome in order to achieve a steady-state velocity. For each condition, MVMCA was determined by calculating the average MCAv over each cardiac cycle during the final minute. Percent ΔMVMCA was calculated as: [(hypercapnic MVMCA – normocapnic MVMCA)/(normocapnic MVMCA)]*100; this value was used to compare cerebrovascular reactivity between groups.
In order to normalize the MVMCA response to changes in arterial blood gas, breath-by-breath end-tidal partial pressure of CO2 (ETCO2) was continuously monitored (Vacumed, Ventura, CA) [18]. This measurement is noninvasive and strongly correlates with (invasive) serial blood measures of arterial blood gas [18]. Brachial artery blood pressure was measured during minute two of each condition using an automated cuff, and the MVMCA response was normalized for change in blood pressure. Relative cerebrovascular reactivity was calculated as %ΔMVMCA/(hypercapnia ETCO2 – normocapnic ETCO2). MVMCA / mean arterial pressure (vascular conductance; VC) was calculated for each condition. Percent Δ in MCA vascular conductance (VCMCA) was calculated as [(hypercapnic VCMCA – normocapnic VCMCA)/(normocapnic VCMCA)]*100. Relative VCMCA reactivity was calculated as % ΔVCMCA/(hypercapnia ETCO2 – resting ETCO2).
The Gosling PI was used to calculate pulsatile cerebrovascular velocity (PI = (MCAv(systolic) − MCAv(diastolic))/MVMCA), as described previously [19, 17]. PI positively associates with arterial stiffness [10]; a higher value reflects an impaired ability of the cerebral arteries to buffer a large increase in pressure delivered via the carotid arteries from the heart to the brain.
Cerebral blood flow (CBF) was assessed using extracranial high-resolution duplex ultrasound (Xario 200, Canon Medical Systems, USA) performed in the semi-seated position (45-degree hip angle) to capture both time-averaged mean blood velocity (MV) diameter of the right internal carotid artery (ICA) and right vertebral artery (VA) (i.e., the two primary arteries that supply the brain). ICA and VA diameter were measured during the diastolic phase of the cardiac cycle and averaged over a 30 second period. CBF was calculated as: CBF = MV × π(diameter/2)2 for each artery, as described previously [20, 17]. The sum of CBF calculated for the right ICA and VA was multiplied by two for a bilateral estimate of total CBF [20].
Arterial Stiffness
The assessment of PWV has been described in detail previously [21, 22]. Briefly, a transcutaneous custom tonometer was positioned at the carotid and femoral arteries to non-invasively assess carotid-femoral PWV (Noninvasive Hemodynamics Workstation [NIHem], Cardiovascular Engineering Inc., Norwood, MA).
Cognitive Function
The NIH Cognitive Toolbox is a validated multidimensional assessment of cognitive function designed to assess a wide range of cognitive subdomains in a brief amount of time [23]. Briefly, the NIH Toolbox-Cognition Battery entails seven computerized tests that assess five major cognitive subdomains, executive function (Dimensional Change Card Sort Test; Flanker Inhibitory Control and Attention Test), including processing speed (Pattern Comparison Processing Speed Test), working memory (List Sorting Working Memory Test), episodic memory (Picture Sequence Memory Test), and language (Picture Vocabulary Test; Oral Reading Recognition Test). The fluid composite cognition score is a combined score across subdomains assessing fluid cognitive ability: executive function, processing speed, working memory, and episodic memory. The crystallized cognition composite score is a combined score across the tests assessing language. The total cognitive function composite score (a measure of general cognitive function), is a combination of all test scores. A higher score indicates better cognitive performance. Additionally, we administered the Trail Making Test (parts A and B) as an indices of processing speed and executive function, respectively; a shorter time to complete the tests indicating better performance [24].
Circulating Markers
Fasting plasma samples were used to measure brain-derived neurotrophic factor (BDNF; a marker of blood-brain barrier disruption and key neurotrophic factor [25]), interleukin-6 (IL-6), IL-1β, tumor necrosis factor-α (TNF-α) (pro-inflammatory cytokines [26]), and monocyte chemoattractant protein (MCP-1; a chemokine regulating migration of monocytes and infiltration of macrophages [26]) (1:2 dilution, Customized U-Plex Metabolic Group 1, Meso Scale Discovery, Cat# K15052K-1, Lot# 356950). Fasting serum samples were used to measure soluble CD14 (sCD14; gut-blood barrier permeability marker [27]) (1:200 dilution; R&D Systems, Cat# DC140, Lot# P319505) and enolase 2 (neuron-specific marker of blood-brain barrier disruption [25]) (no dilution, R&D Systems, Cat# DENL20, lot P316287) by ELISA. Activity of the antioxidant enzyme superoxide dismutase (SOD) [28] was measured in fasting serum samples (1:4 dilution, Invitrogen, Cat# EIASODC, lot # 22SD001D).
Statistical Analyses and Power Calculations
Independent samples t-tests, Chi-square tests, or Fisher’s exact tests were used to assess differences in variables between groups. Non-normally distributed variables were log-transformed prior to analysis. ANCOVA was used to adjust for education when comparing cognitive function between groups. Pearson’s bivariate correlations and multiple linear regression were used to evaluate a group * sex interaction, as well as associations between variables. Analyses were performed using SPSS 27 and statistical significance was set at p<0.05 with a two-sided alpha. All data were considered physiological and hypothesis-generating; thus, adjustment was not made for multiple comparisons. Data are reported as means+S.D or medians (interquartile range).
A previous cross-sectional study comparing patients with anemia secondary to kidney failure and healthy controls [29] was used to calculate an effect size for the primary outcome of cerebrovascular reactivity. Calculations were performed based on an independent samples t-test using G-power 3.1. An effect size of 2.20 was calculated based on a value of 5.3±0.82 in the control group and 2.6±1.18 in the kidney failure group. Based on this effect size, 10 participants would be needed per group with 80% power and an α-level of 0.05. As we anticipated that the effect size in patients with earlier-stage ADPKD vs. healthy control may not be as large as difference between patients with kidney failure and controls, we increased the number of participants needed to complete the study to 15 per group (50% increase).
Study Approval
All procedures were approved by the Colorado Multiple Institutional Review Board (17–2135) and adhere to the Declaration of Helsinki. The nature, benefits and risks of the study were explained to the volunteers and their written informed consent was obtained prior to participation.
Data Availability Statement
De-identified human data have been deposited at Zenodo (accession number https://doi.org/10.5281/zenodo.6632690). Access to the deposited data isavailable from the corresponding author (KLN), upon reasonable request.
Results
Demographics and Clinical Characteristics
Twenty-three participants with ADPKD were assessed for eligibility and 8 were excluded from enrollment (7 did not meet inclusion/exclusion criteria, 1 declined to participate), for a total ADPKD cohort of 15 participants completing the study. Twenty-four control participants were assessed for eligibility and 9 were excluded from enrollment (5 did not meet inclusion/exclusion criteria, 4 declined to participate), for a total control cohort of 15 participants completing the study. Healthy control participants had a lower average body mass index than participants with ADPKD (Table 1). The majority of ADPKD patients had hypertension, which was an exclusion for healthy controls, and were treated with anti-hypertensive agents (not used by controls). Despite adequate blood pressure control on average, systolic and diastolic blood pressure were higher in the ADPKD group than in controls. No participants had hyperlipidemia; however, three participants with ADPKD were prescribed a statin based on the results from a previous study in ADPKD [30], rather than for lipid lowering. Healthy control participants tended to have more education than participants with ADPKD (p=0.06).
Table 1.
Demographics and Clinical Characteristics of Autosomal Dominant Polycystic Kidney Disease and Control Participants
| Variable | ADPKD (n=15) |
Control (n=15) |
P-Value |
|---|---|---|---|
| Age, y | 27±4 | 29±4 | |
| Sex, n (%) Male | 6 (40%) | 7 (47%) | 1.00 |
| Race/Ethnicity, (%) Non-Hispanic White | 12 (80%) | 15 (100%) | 0.24 |
| Education, n (%) | 0.059 | ||
| High school or some high school | 4 (27%) | 0 (0%) | |
| Some college | 3 (20% | 1 (7%) | |
| College graduate | 6 (40%) | 7 (47%) | |
| Advanced degree | 2 (13%) | 7 (47%) | |
| BMI, kg/m2 * | 28.1±6.9 | 22.5±4.1 | 0.011 |
| Systolic BP, mmHg * | 118±10 | 107±11 | 0.005 |
| Diastolic BP, mmHg * | 81±9 | 67±7 | <0.001 |
| Resting heart rate, beats/min | 66±13 | 73±6 | 0.064 |
| eGFR, ml/min/1.73m2 | 106±22 | 109±14 | 0.62 |
| Glucose, mg/dL | 90±9 | 90±9 | 0.82 |
| LDL Cholesterol, mg/dL | 91±20 | 90±21 | 0.88 |
| HDL Cholesterol, mg/dL | 48±15 | 54±8 | 0.15 |
| Total Cholesterol, mg/dL | 156±23 | 158±25 | 0.75 |
| Triglycerides, mg/dL | 99±56 | 69±27 | 0.070 |
| Hematocrit, % | 41.5±3.6 | 43.6±2.1 | 0.082 |
| Hemoglobin, g/dL | 14.1±1.4 | 14.8±0.83 | 0.089 |
| Hypertension, n (%) * | 9 (60%) | 0 (0%) | <0.001 |
| ACEi/ARB, n (%) * | 8 (53%) | 0 (0%) | 0.002 |
| Diuretic, n (%) | 1 (7%) | 0 (0%) | 1.00 |
| IUD or implantable contraceptive, n (%) | 4 (27%) | 5 (33%) | 1.00 |
| Statin, n (%) | 3 (20%) | 0 (0%) | 0.22 |
| Antianxiety Medication, n (%) | 2 (13%) | 0 (0%) | 0.48 |
| Migraine medication, n (%) | 2 (13%) | 0 (0%) | 0.48 |
Data are mean±S.D. or n (%).
p<0.05 by Chi-square or Fisher’s exact tests for categorical data and an independent samples t-test for continuous variables. ADPKD, autosomal dominant polycystic kidney disease; BMI, body mass index; BP, blood pressure (seated position); eGFR; estimated glomerular filtration rate (by the Chronic Kidney Disease Epidemiology Collaboration equation); LDL, low density lipoprotein; HDL, high density lipoprotein; ACEi, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; IUD, intrauterine device. Resting heart rate was measured in the seated position.
Cerebrovascular Measurements
Participants with ADPKD had a 12% lower MCA PI compared to healthy controls (ADPKD: 0.71±0.07 A.U.; control: 0.81±0.09 A.U.; p<0.001 Figure1A). This group difference remained significant when co-varying for the presence of hypertension, anti-hypertensive medications, statin usage, or body mass index (p<0.01). Resting MVMCA did not differ between groups (ADPKD: 60.0±9.9 cm/sec; control: 58.7±7.1 cm/sec; p=0.67). There was no difference in cerebrovascular reactivity between participants with ADPKD and healthy controls, whether expressed as %ΔMVMCA (ADPKD: 29.4±14.4 %Δ; control: 28.4±14.5 %Δ; p=0.86; Figure 1B), relative cerebrovascular reactivity (ADPKD: 2.6±0.81 %Δ/mmHg; control: 2.6±1.2 %Δ/mmHg; p=0.95; Figure1C), %Δ VCMCA (ADPKD: 23.6±13.5 %Δ; control: 22.9±13.1 %Δ; p=0.88; Figure1D), or relative VCMCA reactivity (ADPKD: 2.1±0.80 %Δ/mmHg; control: 2.0±1.2 %Δ/mmHg; p=0.85; Figure1E). Peak ETCO2 did not differ between groups (ADPKD: 42±4 mmHg; control: 43±3 mmHg, p=0.29). Total CBF velocity did not differ between groups (ADPKD: 1150±260 ml/min; control: 1189±353 ml/min; p=0.74; Figure1F).
Figure 1.
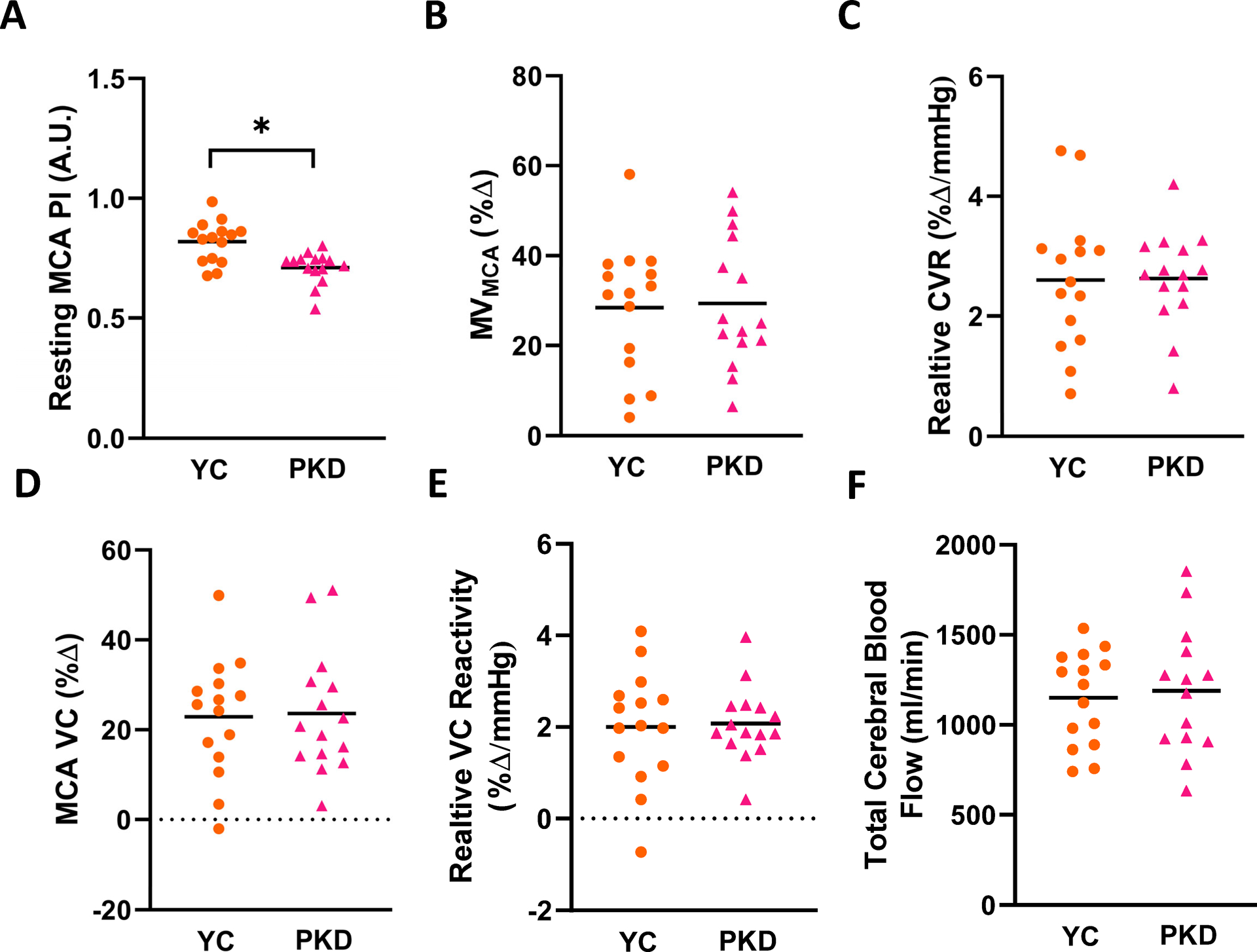
Resting pulsatility index (PI) of the middle cerebral artery (MCA), calculated as (MCA velocity systole – MCA velocity diastole)/(MCA velocity mean) in younger healthy control (orange circles) and early-stage autosomal dominant polycystic kidney disease (ADPKD; pink triangles) participants (A). Percent change in mean flow velocity of the MCA (MVMCA) in response to hypercapnia (B). Relative cerebrovascular reactivity (CVR), calculated as percent change in MVMCA normalized to absolute change in end-tidal CO2 in response to hypercapnia (C). Percent change in vascular conductance (VC; MVMCA / mean arterial pressure) (D). Percent change in relative VC, calculated as percent change in VC normalized to absolute change in end-tidal CO2 in response to hypercapnia (E). Total cerebral blood flow, calculated as right internal carotid blood flow × 2 + right vertebral artery blood flow × 2 (F). Lines represent mean and circles/triangles represent individual participants. * p<0.05 by an independent samples t-test.
There was a significant group * sex interaction (p=0.002) for PI. The group difference in PI was more pronounced in females (ADPKD: 0.68±0.07 A.U. [n=8]; control: 0.81±0.09 A.U. [n=9]; p=0.004) than in males (ADPKD: 0.75±0.03 A.U. [n=7]; control: 0.83±0.09 A.U. [n=6]; p=0.06).
Arterial Stiffness
Consistent with previous reports, carotid-femoral PWV was greater in participants with ADPKD (592±104 cm/sec) as compared to healthy controls (518±89 cm/sec; p<0.05). There was no association of MCA PI with carotid-femoral PWV (r = 0.01, p=0.96; Figure 2 A), suggesting MCA PI reflects vascular properties other than arterial stiffness in this population.
Figure 2.
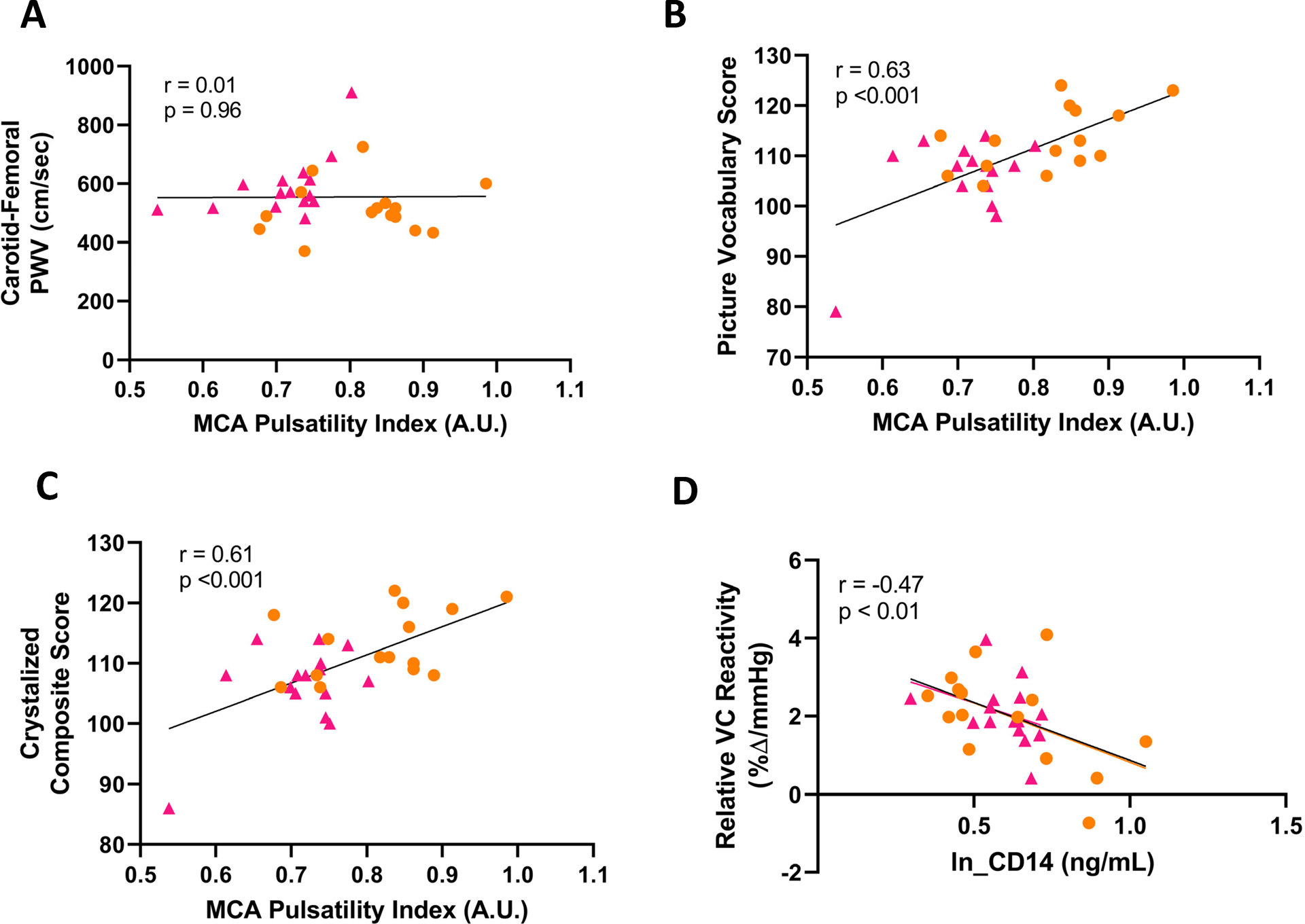
Association of middle cerebral artery pulsatility index with carotid-femoral pulse-wave velocity (PWV) (A), middle cerebral artery pulsatility index with picture vocabulary score (B), middle cerebral artery pulsatility index with crystalized composite score (C), and log-transformed soluble CD14 with middle cerebral artery relative vascular conductance (VC) reactivity (D). Controls are shown in orange circles and participants with early-stage autosomal dominant polycystic kidney disease are shown in pink triangles.
Cognitive Function
Participants with ADPKD had a slower time on the trail making part B test and lower NIH Toolbox picture vocabulary, reading recognition, crystallized composite, and total composite scores as compared to healthy controls (Table 2). When adjusted for education (ANCOVA), the group differences in reading recognition score (p=0.03) and crystalized composite score (p=0.04) remained significantly different, but not trail making part B time (p=0.22), picture vocabulary score (p=0.08), and total composite score (p=0.09). Pulsatility index was positivity correlated with picture vocabulary score (r=0.63, p<0.001; Figure 2B) and crystalized composite score (r=0.61, p<0.001; Figure 2C). These associations persisted after adjustment for age, sex, eGFR, and education (picture vocabulary score: β=0.58, p=0.002; crystalized composite score (β=0.58, p=0.007).
Table 2.
Cognitive Function in Autosomal Dominant Polycystic Disease and Control Participants
| Variable | ADPKD (n=15) |
Control (n=15) |
P-Value |
|---|---|---|---|
| Trails A, sec | 19.5±4.1 | 16.1±5.2 | 0.057 |
| Trails B, sec * | 44.7±16.0 | 34.0±10.7 | 0.040 |
| Picture Vocabulary, score * | 105.7±8.6 | 113.2±6.3 | 0.011 |
| Flanker, score | 100.5±8.1 | 104.3±6.9 | 0.18 |
| List Sort, score | 109.2±9.7 | 112.2±8.6 | 0.38 |
| Dimensional Card Sort, score | 108.3±10.3 | 113.2±6.7 | 0.14 |
| Processing Speed, score | 113.3±19.9 | 119.5±23.4 | 0.44 |
| Sequence Memory, score | 114.4±14.9 | 118.5±15.5 | 0.47 |
| Reading Recognition, score * | 106.9±6.2 | 112.4±5.0 | 0.012 |
| Fluid Composite, score | 111.3±15.2 | 117.5±12.1 | 0.22 |
| Crystallized Composite, score * | 106.3±7.0 | 113.3±5.6 | 0.005 |
| Total Composite, score * | 109.9±11.7 | 118.0±8.7 | 0.040 |
Data are mean±S.D.
p<0.05 by an independent samples t-test. ADPKD, autosomal dominant polycystic kidney disease; Trails A, trail making test part A; trails B, trail making test part B. A shorter time to complete the test indicates better performance. The NIH toolbox scores are uncorrected. A higher score indicates better performance (mean = 100, SD = 15).
Circulating Markers
There were no group differences in sCD14, enolase 2, BDNF, IL-1β, IL-6, MCP-1, TNFα, or SOD activity (Supplementary Figure 1). Greater (log-transformed) sCD14 was associated with worse relative cerebrovascular reactivity (r=−0.47, p=0.009; Figure 2D). This association persisted after adjustment for age, sex, and eGFR (β=−0.56, p=0.01).
Discussion / Conclusion
In this physiological cross-sectional study, we observed a consistently lower MCA PI in participants with early-stage ADPKD as compared to healthy controls, which was not explained by the presence of hypertension or the use of antihypertensive agents. This was unexpected, as we had hypothesized that MCA PI would be greater in the ADPKD group, reflecting greater arterial stiffness. Indeed, there was no correlation between MCA PI and carotid-femoral PWV, the gold-standard measure of large-artery stiffness, despite a higher carotid-femoral PWV in the ADPKD group, suggesting that the lower MCA PI in the ADPKD group may reflect physiological parameters other than arterial stiffness. In addition to mirroring cerebrovascular resistance, MCA PI is also influenced by cerebral perfusion pressure, cerebral arterial compliance, and heart rate [31]. Decreased MCA PI could also indicate stenosis of the internal carotid artery; however, no participants has evidence of internal carotid artery stenosis [32]. Interestingly, lower MCA PI was associated with worse performance on two indices of cognitive function, independent of age, sex, eGFR, and education. In contrast, we observed no differences in MCA cerebrovascular reactivity indices between the ADPKD group and healthy controls,
The prevalence of intracranial aneurysm is higher in patients with ADPKD as compared to the general population. For example, in a systematic review and meta-analysis, the pooled prevalence of intracranial aneurysm in participants with ADPKD was 10% (95% confidence interval: 7–13%) as compared to ~2–3% in the general population [33]. Recent studies report an inverse association between PI and aneurysm risk in non-ADPKD populations. In a recent observational study including 1,276 healthy middle-aged and older Japanese adults without prevalent cerebrovascular or cardiovascular disease who underwent magnetic resonance angiography as part of health screening, 5.7% had a finding of incidental unruptured intracranial aneurysm (UIA) [34]. After adjustment for age, sex, and hypertension, there was a significant association of lower carotid artery PI with the presence of incidental UIA. The authors suggested that low PI may reflect low wall shear stress, which may be involved in UIA formation via inflammatory cell-mediated arterial wall remodeling and thickening. Similarly, in another recent, observational study, which included 96 patients with unruptured MCA aneurysm and 94 age- and sex-matched controls, MCA PI was significantly lower in the aneurysm group [35]. Given the lower MCA PI observed in the ADPKD as compared to healthy control group in the current study, it is plausible that a lower MCA PI may be associated with an increased aneurysm risk in patients with ADPKD. Following completion of the study and observing lower MCA PI index in the ADPKD group, we contacted the ADPKD participants to inquire about family history of intracranial aneurysm. Four of the 15 participants reported a family history of intracranial aneurysm, although only one of the four participants noted that this history was in a family member with a known ADPKD diagnosis.
In contrast to MCA PI, cerebrovascular reactivity did not differ between patients with ADPKD and healthy controls in this study. A very recent publication supports that cerebrovascular reactivity to hypercapnia is only partially nitric oxide dependent, and nitric oxide is not obligatory for cerebrovascular reactivity to CO2 [36]. Thus, despite evidence of reduced nitric oxide bioavailability in ADPKD [37, 38], other compensatory vasodilators may maintain CBF during a hypercapnia challenge, given the critical importance of CBF. Additionally, we did not observe evidence of increased levels of circulating markers of oxidative stress or inflammation in this small cohort of early-stage ADPKD patients, both of which are contributors to nitric oxide bioavailability [39]. Interestingly, there was a correlation between sCD14 and relative VCMCA reactivity across pooled participants, suggesting a potential role of gut barrier permeability [27] in cerebrovascular reactivity. Anemia may also promote increased MCA mean flow velocity [40]; hematocrit and hemoglobin levels tended to be lower in ADPKD patients, although not statistically different.
We observed group differences in several indices of cognitive function. These were at least in part due to differing levels of education between groups. However, two indices remained significantly different between groups after statistical correction for level of education (reading recognition and crystalized composite). Both of these measures are dependent upon past learning experiences and are considered consistent across the adult lifespan. Thus, there may be residual confounding between groups even after correction for level of education, which is considered to be a proxy for socioeconomic status. Interestingly, across pooled groups, MCA PI was correlated with each of these cognitive indices, and this association persisted after correction for age, sex, eGFR, and education. Increased PI has been previously shown to independently associate with reduced cognitive function (memory, speed, and executive function) in older adults without stroke or dementia [10]. Similar directionality of increased MCA PI and cognitive impairment has been described in other middle-aged to older adult populations [41, 42]. However, in our current young cohort, PI was positively rather than inversely correlated with cognitive function, consistent with and driven by the lower observed MCA PI in the ADPKD group.
There are several limitations to this study. Most notably, our sample size was small. However, we performed comprehensive physiological assessments and cognitive testing, and we were appropriately powered for our a priori primary outcome of cerebrovascular reactivity. Additionally, the observed difference in MCA PI was consistent across participants. Another limitation is that group differences between the ADPKD and healthy control group other than the primary disease process, such as differences in body mass index, the presence of hypertension, or medication usage, may have accounted for the observed results rather than ADPKD per se. Although the observed group differences in MCA PI persisted after statistical adjustments were made for such parameters, there may be residual confounding, and future research is needed to compare patients with ADPKD to controls who also have hypertension and antihypertensive medication usage. However, importantly, such comorbidities are very common in patients with kidney diseases, thus may contribute to phenotypic changes observed in patients with ADPKD, and even if beyond the effects of genetic mutation alone, are critical to the clinical presentation of this patient population. Hypertension is extremely common in patients with ADPKD, occurring at a young age and prior to the loss of kidney function [1]. An additional limitation is that normative values for MCA PI in young adults are not readily available. Furthermore, due to time and/or budgetary constraints, we were unable to assess total kidney volume in this cohort as an index of disease severity or beat-to-beat blood pressure. However, the major strength of our study is that to our knowledge, this is the first study to assess cerebrovascular function in patients with ADPKD.
In conclusion, we have provided novel and unexpected evidence that MCA PI is reduced, but cerebrovascular reactivity is preserved in early-stage ADPKD. The former observation merits further research, as low PI could potentially be a risk factor for cerebral aneurysm, a more frequent event in patients with ADPKD as compared to the general population, although association does not imply causality. It does not appear that MCA PI reflects cerebrovascular stiffness in young ADPKD patients; thus, further research is needed to further evaluate changes in the cerebrovasculature, such as potential low wall shear stress.
Supplementary Material
Acknowledgments
The authors acknowledge Christopher Martens for his technical assistance.
Funding Sources:
This study was supported by the Baltimore PKD Research and Clinical Core Center Pilot and Feasibility Program (P30DK090868; National Institute of Diabetes and Digestive and Kidney Diseases [NIDDK]). Kristen Nowak was also supported by NIDDK, K01DK103678. Cortney Steele and Ester Oh were supported by NIDDK (grant 5T32DK007135-46). Additional funding was provided by the Zell Family Foundation.
Footnotes
Statement of Ethics
All procedures were approved by the Colorado Multiple Institutional Review Board (17–2135) and adhere to the Declaration of Helsinki. The nature, benefits and risks of the study were explained to the volunteers and their written informed consent was obtained prior to participation.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The results presented in this paper have not been published previously in whole or part, except in abstract format.
Data Availability Statement:
De-identified human data have been deposited at Zenodo (accession number https://doi.org/10.5281/zenodo.6632690).
Access to the deposited data is available from the corresponding author (KLN), upon reasonable request.
References
- 1.Cornec-Le Gall E, Alam A, Perrone RD. Autosomal dominant polycystic kidney disease. Lancet. 2019;393(10174):919–35. [DOI] [PubMed] [Google Scholar]
- 2.Fick GM, Johnson AM, Hammond WS, Gabow PA. Causes of death in autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 1995;5(12):2048–56. [DOI] [PubMed] [Google Scholar]
- 3.Ecder T, Schrier RW. Cardiovascular abnormalities in autosomal-dominant polycystic kidney disease. Nat Rev Nephrol. 2009;5(4):221–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nowak KL, Farmer H, Cadnapaphornchai MA, Gitomer B, Chonchol M. Vascular dysfunction in children and young adults with autosomal dominant polycystic kidney disease. Nephrol Dial Transplant. 2016;17:1555–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mekahli D, Womack H, Dahl NK. Perspectives on drug development in early ADPKD. Clin J Am Soc Nephrol. 2022;17(10):1555–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lau WL, Huisa BN, Fisher M. The cerebrovascular-chronic kidney disease connection: perspectives and mechanisms. Transl Stroke Res. 2017;8(1):67–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lu R, Kiernan MC, Murray A, Rosner MH, Ronco C. Kidney-brain crosstalk in the acute and chronic setting. Nat Rev Nephrol. 2015;11(12):707–19. [DOI] [PubMed] [Google Scholar]
- 8.Stone J, Johnstone DM, Mitrofanis J, O’Rourke M. The mechanical cause of age-related dementia (Alzheimer’s disease): the brain is destroyed by the pulse. J Alzheimers Dis. 2015;44(2):355–73. [DOI] [PubMed] [Google Scholar]
- 9.Nation DA, Wierenga CE, Clark LR, Dev SI, Stricker NH, Jak AJ, et al. Cortical and subcortical cerebrovascular resistance index in mild cognitive impairment and Alzheimer’s disease. J Alzheimers Dis. 2013;36(4):689–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mitchell GF, van Buchem MA, Sigurdsson S, Gotal JD, Jonsdottir MK, Kjartansson O, et al. Arterial stiffness, pressure and flow pulsatility and brain structure and function: the Age, Gene/Environment Susceptibility--Reykjavik study. Brain. 2011;134(Pt 11):3398–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cooper LL, Woodard T, Sigurdsson S, van Buchem MA, Torjesen AA, Inker LA, et al. Cerebrovascular damage mediates relations between aortic stiffness and memory. Hypertension. 2016;67(1):176–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chapman AB, Rubinstein D, Hughes R, Stears JC, Earnest MP, Johnson AM, et al. Intracranial aneurysms in autosomal dominant polycystic kidney disease. New Engl J Med. 1992;327(13):916–20. [DOI] [PubMed] [Google Scholar]
- 13.Yu TM, Chuang YW, Sun KT, Yu MC, Kung SC, Lee BK, et al. Polycystic kidney disease is significantly associated with dementia risk. Neurology. 2017;89(14):1457–63. [DOI] [PubMed] [Google Scholar]
- 14.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harris RA, Nishiyama SK, Wray DW, Richardson RS. Ultrasound assessment of flow-mediated dilation. Hypertension. 2010;55(5):1075–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zuj KA, Arbeille P, Shoemaker JK, Blaber AP, Greaves DK, Xu D, et al. Impaired cerebrovascular autoregulation and reduced CO(2) reactivity after long duration spaceflight. Am J Physiol Heart Circ Physiol. 2012;302(12):H2592–8. [DOI] [PubMed] [Google Scholar]
- 17.Oh ES, Freeberg KA, Steele CN, Wang W, Farmer-Bailey H, Coppock ME, et al. Cerebrovascular pulsatility index is higher in chronic kidney disease. Physiol Rep. 2023;11(1):e15561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Purkayastha S, Sorond F. Transcranial Doppler ultrasound: technique and application. Semin Neurol. 2012;32(4):411–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brar I, Robertson AD, Hughson RL. Increased central arterial stiffness and altered cerebrovascular haemodynamic properties in South Asian older adults. J Hum Hypertens. 2016;30(5):309–14. [DOI] [PubMed] [Google Scholar]
- 20.Robertson AD, Tessmer CF, Hughson RL. Association between arterial stiffness and cerebrovascular resistance in the elderly. J Hum Hypertens. 2010;24(3):190–6. [DOI] [PubMed] [Google Scholar]
- 21.Nowak KL, Gitomer B, Farmer-Bailey H, Wang W, Malaczewski M, Klawitter J, et al. Mineralocorticoid Antagonism and vascular function in early autosomal dominant polycystic kidney disease: a randomized controlled trial. Am J Kidney Dis. 2019;74(2):213–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nowak KL, Wang W, Farmer-Bailey H, Gitomer B, Malaczewski M, Klawitter J, et al. Vascular dysfunction, oxidative stress, and inflammation in autosomal dominant polycystic kidney disease. Clin J Am Soc Nephrol. 2018;13(10):1493–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gershon RC, Wagster MV, Hendrie HC, Fox NA, Cook KF, Nowinski CJ. NIH toolbox for assessment of neurological and behavioral function. Neurology. 2013;80(11 Suppl 3):S2–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kurella M, Chertow GM, Luan J, Yaffe K. Cognitive impairment in chronic kidney disease. J Am Geriatr Soc. 2004;52(11):1863–9. [DOI] [PubMed] [Google Scholar]
- 25.Lau WL, Savoj J, Nakata MB, Vaziri ND. Altered microbiome in chronic kidney disease: systemic effects of gut-derived uremic toxins. Clin Sci (Lond). 2018;132(5):509–22. [DOI] [PubMed] [Google Scholar]
- 26.Ta MH, Harris DC, Rangan GK. Role of interstitial inflammation in the pathogenesis of polycystic kidney disease. Nephrology (Carlton). 2013;18(5):317–30. [DOI] [PubMed] [Google Scholar]
- 27.Hernandez L, Ward LJ, Arefin S, Ebert T, Laucyte-Cibulskiene A, Collaborators G-F, et al. Blood-brain barrier and gut barrier dysfunction in chronic kidney disease with a focus on circulating biomarkers and tight junction proteins. Sci Rep. 2022;12(1):4414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Akiyama S, Inagaki M, Tsuji M, Gotoh H, Gotoh T, Gotoh Y, et al. mRNA study on Cu/Zn superoxide dismutase induction by hemodialysis treatment. Nephron Clin Pract. 2005;99(4):c107–14. [DOI] [PubMed] [Google Scholar]
- 29.Kuwabara Y, Sasaki M, Hirakata H, Koga H, Nakagawa M, Chen T, et al. Cerebral blood flow and vasodilatory capacity in anemia secondary to chronic renal failure. Kidney Int. 2002;61(2):564–9. [DOI] [PubMed] [Google Scholar]
- 30.Cadnapaphornchai MA, George DM, McFann K, Wang W, Gitomer B, Strain JD, et al. Effect of pravastatin on total kidney volume, left ventricular mass index, and microalbuminuria in pediatric autosomal dominant polycystic kidney disease. Clin J Am Soc Nephrol. 2014;9(5):889–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.de Riva N, Budohoski KP, Smielewski P, Kasprowicz M, Zweifel C, Steiner LA, et al. Transcranial Doppler pulsatility index: what it is and what it isn’t. Neurocrit Care. 2012;17(1):58–66. [DOI] [PubMed] [Google Scholar]
- 32.Blohme L, Pagani M, Parra-Hoyos H, Olofsson P, Takolander R, Swedenborg J. Changes in middle cerebral artery flow velocity and pulsatility index after carotid endarterectomy. Eur J Vasc Surg. 1991;5(6):659–63. [DOI] [PubMed] [Google Scholar]
- 33.Zhou Z, Xu Y, Delcourt C, Shan J, Li Q, Xu J, et al. Is regular screening for intracranial aneurysm necessary in patients with autosomal dominant polycystic kidney disease? A systematic review and meta-analysis. Cerebrovasc Dis. 2017;44(1–2):75–82. [DOI] [PubMed] [Google Scholar]
- 34.Igase M, Igase K, Okada Y, Ochi M, Tabara Y, Sadamoto K, et al. Low carotid flow pulsatility index correlates with the presence of unruptured intracranial aneurysms. J Am Heart Assoc. 2021;10(13):e018626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaspera W, Cmiel-Smorzyk K, Wolanski W, Kawlewska E, Hebda A, Gzik M, et al. Morphological and hemodynamic risk factors for middle cerebral artery aneurysm: a case-control study of 190 patients. Sci Rep. 2020;10(1):2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hoiland RL, Caldwell HG, Carr J, Howe CA, Stacey BS, Dawkins T, et al. Nitric oxide contributes to cerebrovascular shear-mediated dilatation but not steady-state cerebrovascular reactivity to carbon dioxide. J Physiol. 2022;600(6):1385–403. [DOI] [PubMed] [Google Scholar]
- 37.Wang D, Iversen J, Wilcox CS, Strandgaard S. Endothelial dysfunction and reduced nitric oxide in resistance arteries in autosomal-dominant polycystic kidney disease. Kidney Int. 2003;64(4):1381–8. [DOI] [PubMed] [Google Scholar]
- 38.Wang D, Iversen J, Strandgaard S. Contractility and endothelium-dependent relaxation of resistance vessels in polycystic kidney disease rats. Journal Vasc Res. 1999;36(6):502–9. [DOI] [PubMed] [Google Scholar]
- 39.El Assar M, Angulo J, Rodriguez-Manas L. Oxidative stress and vascular inflammation in aging. Free Radic Biol Med. 2013;65:380–401. [DOI] [PubMed] [Google Scholar]
- 40.Brass LM, Pavlakis SG, DeVivo D, Piomelli S, Mohr JP. Transcranial Doppler measurements of the middle cerebral artery. Effect of hematocrit. Stroke. 1988;19(12):1466–9. [DOI] [PubMed] [Google Scholar]
- 41.Harris S, Reyhan T, Ramli Y, Prihartono J, Kurniawan M. Middle cerebral artery pulsatility index as predictor of cognitive impairment in hypertensive patients. Front Neurol. 2018;9:538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Crespo-Cuevas AM, Canento T, Hernandez-Perez M, Caceres C, Gonzalez A, Ispierto L, et al. The Barcelona-Asymptomatic Intracranial Atherosclerosis (AsIA) study: Subclinical cervico-cerebral stenosis and middle cerebral artery pulsatility index as predictors of long-term incident cognitive impairment. Atherosclerosis. 2020;312:104–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
De-identified human data have been deposited at Zenodo (accession number https://doi.org/10.5281/zenodo.6632690). Access to the deposited data isavailable from the corresponding author (KLN), upon reasonable request.
De-identified human data have been deposited at Zenodo (accession number https://doi.org/10.5281/zenodo.6632690).
Access to the deposited data is available from the corresponding author (KLN), upon reasonable request.


