Abstract
Background
Although family-based, behavioral interventions for pediatric obesity require caregivers to make major changes to dietary intake and the family meal, few studies have examined family functioning, and specifically, mealtime behaviors among families of treatment-seeking obese children. The current study compared mealtime family functioning of treatment-seeking obese children and nonobese demographically matched comparisons using a multimethod design.
Methods
Participants included the families of 27 obese children (BMI ≥95th percentile; M body mass index (BMI) z-score values [M zBMI] = 2.55) at the time of treatment initiation and 27 families of nonobese children (M zBMI = 0.17). Each family’s evening meal was videotaped and coded for observed family functioning using the Mealtime Interaction Coding System (MICS). Caregivers completed a demographics form and a measure of family mealtime climate.
Results
Caregivers of obese children self-reported greater mealtime challenges and a less positive meal environment than non-obese comparisons. There were no significant group differences in observed family mealtime interactions.
Conclusion
Interestingly, although group means on the observational measure of mealtime family functioning were not significantly different, caregivers of obese children reported greater mealtime stress. Accordingly, it is important in the context of treatment to address caregiver perceptions of mealtime challenges and to examine the extent to which these self-reported challenges affect implementation of treatment recommendations and treatment outcomes.
Introduction
Empirically supported pediatric obesity treatment approaches are typified by family-based interventions that rely on long-term parental involvement and monitoring.1 Unfortunately, we know very little about family functioning in the context of pediatric obesity and its treatment. Existing research suggests that the families of obese children that are seeking treatment struggle at mealtimes, with obese children exhibiting behaviors that can be challenging for families to manage. Zeller and colleagues2 found that mothers of treatment-seeking obese youth reported higher levels of family conflict and lower cohesion and structure as well as greater mealtime challenges (e.g., arguing about eating, need to monitor closely) as compared to mothers of non-overweight children. Furthermore, both mothers and fathers described less positive mealtime interactions than comparison parents. In a related study, obese children were described by mothers as having a more difficult temperament than non-overweight children, with their mothers reporting a parenting style lower in behavioral control (e.g., fewer rules, less strict).3 Taken together, these predominantly mother-reported data highlight the need to examine family processes during mealtimes more closely. This is especially salient given that the major focus of pediatric obesity treatment is decreasing youth caloric intake, in part, by increasing caregiver monitoring and behavior management.
Observational assessments provide rich contextual data on how family members interact, support, and work together to achieve a goal, thus providing a measure of family functioning that may be less biased by caregiver self-report.4 The Mealtime Interaction Coding System (MICS)5,6 is a direct observational measure that assesses qualities of family interactions (e.g., communication, task accomplishment) occurring in the unstructured, naturalistic setting of family meals. Investigators have used the MICS to compare family functioning among families with healthy children versus children with various chronic conditions requiring significant dietary intervention (e.g., cystic fibrosis7,8 and diabetes9), noting that families with chronically ill children demonstrate poorer family functioning at mealtimes than families with healthy children. To date, however, only two groups of investigators have used observational methods to examine family functioning in school-aged children who are overweight and obese.10,11
Additional research is needed to examine potentially modifiable family behaviors that may relate to a family’s ability to implement weight management strategies successfully. The primary purpose of the current study was to assess family functioning in families of treatment-seeking obese children (BMI ≥95th percentile; ages 5–12) and compare them with a demographically matched, non-obese (BMI <95th percentile) comparison group. Given the associations of familial variables with child BMI and differences in family functioning when a pediatric chronic medical condition has high mealtime demands,12–14 it was hypothesized that family functioning would be more impaired at mealtimes in families of treatment-seeking obese children relative to families without an obese child. A secondary, exploratory aim was to examine the relations between family functioning and mealtime climate.
Methods
Participants
Participants included 27 treatment-seeking obese children (BMI ≥95lh percentile; M body mass index (BMI) z-score values [M zBMI] = 2.55) and 27 nonobese children (BMI <95th percentile; M zBMI = 0.17) and their families. The mean age of the target child was 9.5 years (standard deviation [SD] = 2.06); 65% were female and 47% were African American. The majority of caregiver respondents were mothers/stepmothers (83%) and approximately half were married/remarried (51%).
Inclusion/exclusion criteria
Target children were between the ages of 5 and 12 at the time of enrollment. Children with significant reading disabilities or who were developmentally delayed (by caregiver report) were excluded. Inclusion into the obese group was indicated by a BMI greater than or equal to the 95th percentile. Children in the nonobese demographically matched comparison group could not be obese (BMI <95th percentile), have a chronic medical condition, or have siblings who were obese.
Of the 70 families approached, 6 in the obese group and 5 in the comparison group declined participation (primary reason given was schedule/work schedule too busy for home visit). Fifty-nine families were recruited; however, five families were excluded from the final analyses (n = 3 comparison group families due to children having a BMI ≥95th percentile at time of data collection, and n = 2 obese group families due to rating their meal as atypical and thus the observed meal being unrepresentative of mealtime functioning). The final sample used for analyses included 27 families with an obese child and 27 nonobese matched comparisons.
Procedures
Institutional Review Board approval was obtained prior to study initiation. Families referred to a pediatric weight management clinic were sent a letter describing the present study. Families meeting inclusion criteria were approached at their medical screening/initial evaluation visit to further discuss the study and assess interest. If the family agreed to participate, a home visit was scheduled within 2 weeks and prior to their first treatment session.
Matched nonobese comparisons were selected based on same gender, race, and ±1 year of age. Comparisons were identified in three ways. First, data from a clinical trials database, which includes families who have volunteered to participate in research studies at our institution and given permission to be contacted, was used. Families with a child who met gender and age criteria were sent a letter and brochure explaining the study. Second, a recruitment e-mail was sent to all hospital staff. Finally, children attending regular pediatrician outpatient appointments through the Pediatric Primary Care Clinic were approached prior to their medical visit to assess interest and match.
Two research staff attended each home visit. Consent from caregivers and assent from children was obtained. All meals taped were dinner/evening meals. Prior to the meal, height and weight measurements were obtained for all family members present for the meal, and parents completed self-report measures. A video camera was set up based on the family’s typical location for dinner and started. Research staff left the room or house to reduce distraction and social desirability during the meal. Following completion of the meal, the primary caregiver completed meal typicality form. Families were reimbursed for their time.
Measures
Demographic questionnaire
This instrument assessed demographic characteristics, including caregiver race, marital status, level of education, income, and the number of children living in the home. From this information, the Revised Duncan15 score was calculated to measure socio-economic status (SES) for each family. This occupational-based measure of SES ranges from 15 to 97, with higher scores representing greater occupational attainment.
Weight and height
Weight was measured (0.1 kg) on a portable Seca digital scale (Seca, Hamburg, Germany). Standing height was measured (0.1 cm) using a calibrated custom portable stadiometer (Creative Health Products, Plymouth, MI). Participants were weighed and measured in street clothing and without shoes. Data were used to calculate BMI (kg/m2). Given that BMI increases with age as children mature, zBMI values were calculated for child participants using age- (to the nearest month) and sex-specific median, SD, and power of the Box–Cox transformation based on national norms from the CDC.16
Mealtime Family Interaction Coding System
The MICS is an observational coding system based on the McMaster Model of Family Functioning17,18 designed to assess family functioning during the unstructured, naturalistic situation of mealtimes. Family interactions are coded along six dimensions—task accomplishment, communication, roles, affective responsiveness, affective involvement, behavior control—and one separate scale of general functioning. Each dimension is scored on a 7-point scale ranging from 1 (very unhealthy) to 7 (very healthy). Each dimension has a clinical cutoff score, with ratings less than 5 considered in the unhealthy range and indicative of problematic functioning; scores of 5 and higher are considered in the healthy range and indicative of good/adequate functioning. Per measure parameters, coding of interactions began when the meal started, as indicated by the presence of food on the table and the initiation of eating by at least one family member, and coding stopped at the end of the meal or after 20 min, whichever occurred first.
Coders were postdoctoral fellows who attending a training workshop taught by the developers of the MICS and were trained to a reliability of 0.80 or greater. For this sample, intraclass correlations between coders were found to be acceptable19 for each dimension, based on reliability coding of one-third of the meals: Task Accomplishment = 0.83, Communication = 0.67, Affective Management = 0.91, Interpersonal Involvement = 0.92, Behavior Control = 0.83, Roles = 0.89, and Overall Family Functioning = 0.95. The reliability and validity of this assessment has been strongly supported in the literature.18
Mealtime Observation Form
The Mealtime Observation Form (Benson and Munoz, 2004, unpublished manual, Syracuse University) assessed structural characteristics of the meal environment. Variables assessed included how the meal was served, whether food was distributed safely, whether the television was on/off, type of beverage served, if dessert was served, complaints about food, refusal to eat, and instances of conflict. These data were coded by a trained research assistant in a separate viewing of the mealtime compared to MICS coding.
About Your Child’s Eating-R
About Your Child’s Eating-R (AYCE-R)20 is a 25-item measure that assesses caregiver beliefs and concerns about children’s eating and family mealtime interactions and is designed to target mealtime issues for families of children with medical conditions. Caregivers are asked to rate on a 5-point scale ranging from “never” to “nearly all the time” how often a variety of situations take place in their family around children’s eating. Factor analyses revealed three factors: Resistance to Eating, Positive Mealtime Interaction, and Child Aversion to Mealtime.21 For the purpose of the current study, a revised version of the Resistance to Eating scale, named “Mealtime Challenges,” was used because it omits items that are not salient to an obese population.2 This measure demonstrated adequate internal consistency21 for the current sample across Mealtime Challenges (α = 0.66), Positive Mealtime Interaction (α = 0.76), and Child Aversion to Mealtime (α = 0.60) subscales.
Mealtime Typicality Form
This is a 5-item measure that assesses how representative the videotaped meal was on a variety of dimensions. After completion of the meal, caregivers and children were asked to rate the typicality of the videotaped meal. Specifically, raters compared similarity of the child’s behavior, family interactions, and overall meal to their typical meals on a scale of 1 (not at all typical) to 5 (most typical possible). Only meals rated with an overall typical rating, per parent report, between 3 (typical) and 5 (most typical possible) were included. This procedure is consistent with similar observational research in pediatric populations.7,8
Statistical Analyses
On the basis of previous research,9 a total sample of size of 54 gave sufficient power (β = 0.74) to detect a large effect (d = 0.72 overall family functioning), using a two-tailed test and alpha level of 0.05. Descriptive statistics were calculated for variables of interest including demographic variables, meal characteristics, and MICS and AYCE-R scales. Student t-tests and chi-squared analyses were conducted to test for group differences on demographic variables and meal characteristics. Demographic variables that differed significantly between groups (i.e., SES) were entered as covariates in subsequent models. Analyses of covariance variance (ANCOVA) were used to determine differences between groups on the MICS and AYCE-R measures. Chi-squared analyses were conducted to assess for differences in the percentage of participants who met MICS clinical cutoff scores by group. Finally, Pearson correlations were calculated to determine relations between the MICS and AYCE-R scales.
Results
Demographic Characteristics
As expected, no significant differences were identified between groups on child age (t(52) = 0.43, p = 0.67), gender (χ2(l, N = 54) = 0.08, p = 0.78), or race (χ2(l, N = 53) = 0.50, p = 0.58). There were expected differences in child BMI (t(52) = 12.17, p < 0.001) and BMI z-score (t(52) = 10.92, p < 0.001) by group. Significant group differences were also noted for mother’s BMI (t(51) = 5.25, p < 0.001) and family SES (t(51) = −2.32, p < 0.05), with mothers of children who are obese being significantly heavier and within families of lower SES than families of comparisons. No differences were found for father BMI (t(25) = 1.44, p = 0.16). Demographic characteristics for each group and the total sample are presented in Table 1.
Table 1.
Demographic Characteristics of Participants
| Obese | Comparison | Total Sample | |
|---|---|---|---|
|
| |||
| Child age | 9.65 (2.1) yr | 9.41 (2.1) yr | 9.53 (2.1) yr |
|
| |||
| Child gender | |||
| Male | 37% | 33% | 35% |
| Female | 63% | 67% | 65% |
|
| |||
| Child race | |||
| White | 37% | 45% | 42% |
| Black | 48% | 48% | 47% |
| Other | 15% | 4% | 11% |
|
| |||
| Child BMI/zBMI** | 32.2 (5.7)/ 2.5 (0.3) | 17.5 (2.7)/ 0.17 (0.2) | 24.8 (8.7)/1.4 (1.4) |
|
| |||
| Child BMI percentile | 98.9 (0.7) | 57.6 (25.8) | 78.2 (29.1) |
|
| |||
| Primary caregiver | |||
| Mother/stepmother | 78% | 92% | 83% |
| Father/stepfather | 7% | 4% | 6% |
| Other | 15% | 4% | 11% |
|
| |||
| Mother BMI* | 37.9 (6.9) | 28.2 (6.6) | 33.0 (8.3) |
|
| |||
| Father BMI | 34.2 (7.9) | 30.4 (5.6) | 32.1 (6.8) |
|
| |||
| Family Duncan** | 51.39 (23.4) | 66.4 (21.5) | 58.8 (23.1) |
|
| |||
| Mother marital statusa | |||
| Single | 59% | 39% | 49% |
| Married | 41% | 61% | 51% |
p < 0.01.
p < 0.05.
Single = Divorced/separated/widowed/single; Married = Married/remarried.
Observed Meal Characteristics
The characteristics of the meal, including overall typicality and the number of children and adults present during the meal, were similar for both groups (see Table 2). However, the length of the meal was significantly longer for the comparison group (t(52) = 0.43, p = 0.05), Both groups were similar on structural characteristics of the meal environment (Mealtime Observation Form; see Table 3). Specifically, the obese and nonobese groups were observed to have comparable rates of children complaining about the food (11%–15%), refusing to eat (11–15%), and being provided a second helping (63%–66%). The obese group was noted to have the television on for 37% of families (22% TV on in same room; 11% TV on in adjoining room), whereas the comparison group had the television on in 22% of families (11% for each in the same room and adjoining room). Finally, 15% of the obese sample was provided soda with the meal compared to only 4% of the comparison group. It is important to note that we did not statistically test how the meal was served because a large percentage was uncodable for who served the meal due to the meal being served off-camera or in another room.
Table 2.
Characteristics of Meal
| Obese M (SD) | Comparison M (SD) | Total Sample M (SD) | |
|---|---|---|---|
|
| |||
| Meal length | 18.0(6.3) | 21.5 (6.5) | 19.8 (8.7) |
|
| |||
| Total people present at meal | |||
| Total adults | 1.5(0.6) | 1.8(0.8) | 1.7 (0.7) |
| Total children | 2.0 (0.8) | 2.6(1.1) | 2.3 (1.0) |
|
| |||
| Typicality ratings | |||
| People present at meal | 4.7 (0.6) | 4.5 (0.7) | 4.6 (0.7) |
| Discussion/interactions | 4.7 (0.5) | 4.7 (0.5) | 4.7(0.4) |
| Type of food | 4.5 (0.9) | 4.5 (0.9) | 4.5(0.9) |
| Amount of food | 4.3 (0.8) | 4.5 (0.7) | 4.4(0.8) |
| Overall | 4.6 (0.6) | 4.6 (0.7) | 4.6(0.6) |
p = 0.05.
SD, Standard deviation.
Table 3.
Comparison of Characteristics of Meal Environment between Obese and Comparison Groups
| Obese | Comparison | ||
|---|---|---|---|
| How meal served | Parent only | 33.3% | 40.7% |
| Family style | 14.8% | 14.8% | |
| Child directed | 3.5% | 25.9% | |
| Undeterminable | 48.1% | 18.5% | |
| Food prepared and distributed safely | Yes | 96.3% | 100.0% |
| TV on in room dinner eaten | Yes | 22.2% | 11.1% |
| TV on in adjoining room | Yes | 14.8% | 11.1% |
| Child refuses to eat | Yes | 11.1% | 14.8% |
| Child complains doesn’t like food | Yes | 14.8% | 11.1% |
| Child given second helping | Yes | 63.0% | 66.7% |
| Child requested second helping | Yes | 44.4% | 59.3% |
| Drink child served | Water | 14.8% | 14.8% |
| Milk | 14.8%__ | 18.5% | |
| Soda | 14.8% | 3.7% | |
| Other | 22.2% | 22.2% | |
| Family discussion of food/nutrition | Yes | 11.1% | 7.4% |
| Dessert served | Yes | 3.7% | 22.2% |
| Child satiated at end of meal | Yes | 96.3% | 100.0% |
Percentages may not add to 100% due to missing data for some families.
Differences in Family Functioning and Mealtime Climate between Groups
Family socioeconomic status was used as a covariate in subsequent analysis of variance (ANOVA) models examining differences in MICS and AYCE-R scores. No significant mean group differences were found on MICS dimensions (Table 4). In contrast, significant mean group differences were detected on two scales of the AYCE-R; families of children who are obese reported greater mealtime challenges (F(l,50) = 10.48, p < 0.01) and a less positive meal environment (F(l,50) = 5.25, p < 0.05) compared to families with nonobese children.
Table 4.
Functioning across Obese and Comparison Groups Controlling for Family SES
| Obese M (SD) | Comparison M (SD) | F (df) | Effect size (r) | ||
|---|---|---|---|---|---|
| MICS | Task accomplishment | 5.22 (0.97) | 5.54 (1.24) | 0.26 (50) | −.14 |
| Communication | 4.92 (0.69) | 5.46 (1.21) | 1.60 (49) | −.26 | |
| Affect management | 4.70 (1.17) | 5.27 (1.34) | 1.48 (50) | −.22 | |
| Interpersonal involvement | 5.07 (1.21) | 5.42 (1.27) | 0.24 (50) | −.14 | |
| Behavior control | 4.93 (1.01) | 5.42 (1.53) | 0.71(50) | −.19 | |
| Roles | 5.26 (1.06) | 5.62 (1.17) | 0.43(50) | −.16 | |
| Overall functioning | 5.07 (1.04) | 5.46 (1.30) | 0.39 (52) | −.16 | |
| AYCE-R | Child Mealtime challenges | 21.78 (3.85) | 17.65 (5.23) | 10.86(50)* | −.41 |
| Positive meal environment | 18.89 (3.07) | 21.00 (2.37) | 5.25(50)** | −.36 | |
| Parent aversion to mealtime | 6.11 (2.38) | 5.08 (1.26) | 1.89(50) | .26 |
p<0.01 level.
p < 0.05 level.
SES, Socioeconomic status; SD, standard deviation; MICS, Mealtime Interaction Coding System; AYCE-R, About Your Child’s Eating-R.
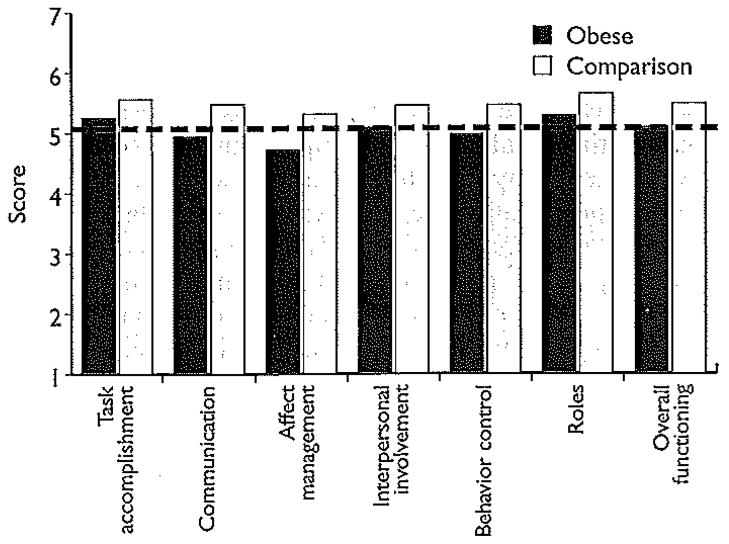
Figure 1 displays the group means compared to the clinical cutoff for each MICS domain. The obese group was below the clinical cutoff (i.e., less healthy functioning) on several MICS domains: Communication, affect management, and behavior control. In contrast, the comparison group was above the clinical cutoff on all domains. Chi-squared analyses indicated no significant differences between groups regarding the proportion of children who were in the healthy versus unhealthy range of Overall Family Functioning (χ2(l, N = 54) = 1.2, p = 0.47).
Figure 1.
Group means relative to clinical cutoff (Mealtime Interaction Coding System [MICS] dimensions). Dark grey bars, obese; light grey bars, comparison.
Relationship Between Family Functioning and Mealtime Climate Across Groups
No significant relations were found between MICS and AYCE-R scales (rs = 00–.20, p = not significant [N.S.]).
Discussion
The present study builds upon prior research suggesting family dysfunction and mealtime stress for obese treatment-seeking youth.2,3 Surprisingly, families of treatment-seeking obese children appeared remarkably similar to nonobese children on a rigorous observational measure (i.e., MICS) of mealtime family functioning, as well as most general mealtime characteristics (e.g., child refusing to eat, complaining of food, given second helping). These findings are in contrast to previous studies using the MICS,10,11 although direct comparisons across studies is challenging. Jacobs and Fiese11 reported greater impairment in family functioning in obese children seeking treatment for asthma (e.g., nondietary intervention), not obesity. Moens et al.,10 while characterizing a similar sample (e.g., waitlist group of overweight/obese youth seeking weight management treatment), made study-specific alterations to the MICS scoring domains and employed a racially homogeneous sample (i.e., Caucasian). However, consistent with prior work,2 caregivers of obese children self-reported greater mealtime challenges and a less positive meal environment at the time of treatment initiation than comparison caregivers. As discussed by Faith et al.,22 these differences may reflect that observational methods are focused on one meal whereas caregiver report is a more global rating of mealtime functioning. Taken together, the present findings suggest family functioning at the dinner meal may not appear different between families with or without an obese child, but nonetheless, the female caregiver perceives there to be a negative mealtime environment. Study strengths include a controlled and multimethod design, with findings leading to important treatment implications and directions for future research.
Clinical Implications
A caregiver’s perceptions of mealtime challenges at the time of treatment initiation is an important target of intervention. For example, clinicians might use mealtime-related stress as an initial discussion point with families with obese children. Discussion of mealtime challenges may provide an opening for clinicians (e.g., pediatricians, nurses, other health care professionals) to describe the potential benefit that obesity intervention programs, such as behavioral treatments, may have for families. Motivational interviewing techniques may be useful in the context of these conversations to encourage families to consider behavior change.23 Additionally, based on clinical cutoffs within this sample, the areas of communication, affect management, and behavior control at mealtimes were in the unhealthy range for the obese group. These areas are likely important for practitioners working with these families to assess and monitor, as further intervention may be warranted as well as impact family’s success at weight loss intervention. An empirically supported clinical intervention such as Wysocki and colleagues24 Behavioral Family Systems Therapy (BFST) could be effectively adapted for this population. Furthermore, interventions that actively address decreasing mealtime challenges and improving the overall meal environment may help to improve a family’s treatment success and maintain their motivation to maintain healthy lifestyle behaviors over time. Given the results of the current study, future research could examine the relationship between caregiver perceptions of behaviors and family functioning related to weight management, caregivers’ abilities to implement treatment recommendations, and treatment outcomes.
Future Directions
Several study limitations provide consequent directions for future research. First, our sample size was modest. Although power analyses indicated adequate power to detect expected effect sizes for overall family functioning, use of the MICS with a larger sample may reveal specific areas in family functioning (e.g., task accomplishment, communication) that may warrant intervention. Second, MICS methodology recommends observation for which only the first 20 min are coded. Clearly, dinner is only one part of families’ daily interactions related to food. Furthermore, the dinner meal was observed to be significantly longer for families with nonobese children. It may be informative to observe family interactions at all meals/snacks and include the entire event to better understand whether there may be unique differences between obese and nonobese families. Certainly the caregiver self-report measure detected group differences when defining mealtimes more broadly. Third, data were collected at the time of treatment initiation, but prior to intervention. Future studies should consider additional comparisons to families of obese children who are not seeking weight management treatment or obese children who are active in or completed treatment. It may be that, for example, the use of videotaped observations is beneficial and provides more insight when children and families are actively engaged in weight-loss efforts. It also remains to be seen how observed or reported family functioning changes over the course of weight management interventions.
Conclusion
This study highlights the importance of considering family factors when attempting to understand the functioning of children and their families presenting for weight loss treatment. Given that many pediatric weight loss interventions rely on caregivers to implement dietary and lifestyle changes,25,26 the influence of mealtime climate and family interactions during meals on weight management outcomes, as well as the role of caregiver distress about mealtimes, will be important factors to consider within interventions and in future research.
Acknowledgments
This work was supported by a National Institutes of Health (NIH) T32 grant (T32 DK63929) to C.P.W. and A.C.M. and a K23 grant (DK60031) to M.H.Z. The authors thank all of the children and their families who participated in this study. We would also like to acknowledge the research assistants and summer students who were instrumental in recruiting participants, and collecting or coding data, including Julie Koumoutsos, Sarah Valentine, Christina Ramey, Lindsay Wilson, Neha Godiwala, Matthew Flanigan, and Demaree Bruck. In addition, we appreciate the support from the staff at HealthWorks!, Pediatric Primary Care Center, and Clinical Trials Database Office at Cincinnati Children’s Hospital Medical Center.
Footnotes
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Raynor H. Evidenced-based treatments for childhood obesity. In: Jelalian E, Stelte RG, editors. Handbook of Childhood and Adolescent Obesity. Springer; New York: 2008. pp. 201–220. [Google Scholar]
- 2.Zeller MH, Reiter-Purtill J, Modi AC, et al. Controlled study of critical parent and family factors in the obesigenic environment. Obesity (Silver Spring) 2007;15:126–136. doi: 10.1038/oby.2007.517. [DOI] [PubMed] [Google Scholar]
- 3.Zeller MH, Boles RE, Reiter-Purtill J. The additive and interactive effects of parenting style and temperament in obese youth seeking treatment. Int J Obes. 2008;32:1474–1480. doi: 10.1038/ijo.2008.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Drotar D. Relating parent and family functioning to the psychological adjustment of children with chronic health conditions: What have we learned? What do we need to know? J Pediatr Psychol. 1997;22:149–165. doi: 10.1093/jpepsy/22.2.149. [DOI] [PubMed] [Google Scholar]
- 5.Alderfer MA, Fiese BH, Gold JI, et al. Evidence-based assessment in pediatric psychology: Family measures. J Pediatr Psychol. 2008;33:1046. doi: 10.1093/jpepsy/jsm083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dickstein S, Hayden LC, Schiller M, et al. Unpublished manual. Providence, RI: 1994. Providence family study mealtime interaction coding system. [Google Scholar]
- 7.Janicke DM, Mitchell MJ, Stark LJ. Family functioning in school-age children with cystic fibrosis: an observational assessment of family interactions in the mealtime environment. J Pediatr Psychol. 2005;30:179–186. doi: 10.1093/jpepsy/jsi005. [DOI] [PubMed] [Google Scholar]
- 8.Mitchell MJ, Powers SW, Byars KC, et al. Family functioning in young children with cystic fibrosis: observations of interactions at mealtime. J Dev Behav Pediatr. 2004;25:335–346. doi: 10.1097/00004703-200410000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Piazza-Waggoner C, Modi AC, Powers SW, et al. Observational assessment of family functioning in families with children who have type 1 diabetes mellitus. J Dev Behav Pediatr. 2008;29:101–105. doi: 10.1097/DBP.0b013e31815f24ce. [DOI] [PubMed] [Google Scholar]
- 10.Moens E, Braet C, Soetens B. Observation of family functioning at mealtime: A comparison between families of children with and without overweight. J Pediatr Psychol. 2006;32:52. doi: 10.1093/jpepsy/jsl011. [DOI] [PubMed] [Google Scholar]
- 11.Jacobs MP, Fiese BH. Family mealtime interactions and overweight children with asthma: Potential for compounded risks? J Pediatr Psychol. 2006;32:64. doi: 10.1093./jpepsy/jsl026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patton SR, Dolan LM, Powers SW. Differences in family mealtime interactions between young children with Type 1 diabetes and controls: Implications for behavioral intervention. J Pediatr Psychol. 2008;33:885–893. doi: 10.1093/jpepsy/jsn026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Powers SW, Mitchell MJ, Patton SR, et al. Mealtime behaviors in families of infants and toddlers with cystic fibrosis. J Cysl Fibros. 2005;4:175–182. doi: 10.1016/j.jcf.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 14.Stark LJ, Powers SW. Behavioral aspects of nutrition in children with cystic fibrosis. Curr Opm Pulm Med. 2005;11:539–542. doi: 10.1097/01.mcp.0000183051.18611.e4. [DOI] [PubMed] [Google Scholar]
- 15.Stevens G, Featherman DL. A revised socioeconomic index of occupational status. Soc Sci Med. 1981;10:364–395. [Google Scholar]
- 16.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM. Advanced Data from Vital and Health Statistics, no 314. National Center for Health Statistics; Hyattsville, MD: 2000. CDC Growth Charts: United States. [Google Scholar]
- 17.Hayden LC, Schiller M, Dickstein S, et al. Levels of family assessment I: Family, marital, and parent-child interaction. J Fam Psychol. 1998;12:7–22. [Google Scholar]
- 18.Dickstein S, Seifer R, Hayden LC, et al. Levels of family assessment II: Impact of maternal psychopathology on family functioning. J Fam Psychol. 1998;12:23–40. [Google Scholar]
- 19.Shrout PE. Measurement reliability and agreement in psychiatry. Stat Methods Med Res. 1998;7:301. doi: 10.1177/096228029800700306. [DOI] [PubMed] [Google Scholar]
- 20.Davies WH, Ackerman LK, Davies CM, et al. About your child’s eating: Factor structure and psychometric properties of a feeding relationship measure. Eat Behav. 2007;8:457–463. doi: 10.1016/j.eatbeh.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 21.Ware JE, Brook RH, Davies AR, et al. Conceptualization and Measurement of Health for Adults in the Health Insurance Study: Model of Health and Methodology. Rand; 1980. [Google Scholar]
- 22.Faith MS, Scanlon KS, Birch LL, et al. Parent-child feeding strategies and their relationships to child eating and weight status. Obesity Res. 2004;12:1711–1722. doi: 10.1038/oby.2004.212. [DOI] [PubMed] [Google Scholar]
- 23.Schwartz RP, Hamre R, Dietz WH, et al. Office-based motivational interviewing to prevent childhood obesity: A feasibility study. Arch Pediatr Adolesc Med. 2007;161:495–501. doi: 10.1001/archpedi.161.5.495. [DOI] [PubMed] [Google Scholar]
- 24.Wysocki T, Harris MA, Buckloh LM, et al. Randomized, controlled trial of Behavioral Family Systems Therapy for Diabetes: Maintenance and generalization of effect on parent-adolescent communication. Behav Ther. 2008;39:33–46. doi: 10.1016/j.beth.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 25.Wadden TA, Stunkard AJ, Rich L, et al. Obesity in black adolescent girls: A controlled clinical trial of treatment by diet, behavior modification, and parental support. Pediatrics. 1990;85:345. [PubMed] [Google Scholar]
- 26.Epstein LH, Klein KR, Wisniewski L. Child and parent factors that influence psychological problems in obese children. Int J Eat Disord. 1994;15:151–158. doi: 10.1002/1098-108x(199403)15:2<151::aid-eat2260150206>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]