Abstract
Accumulating lines of experimental evidence have revealed that hypoxia-inducible factors, HIF-1α and HIF-2α, are key regulators of the adaptation of cancer- and metastasis-initiating cells and their differentiated progenies to oxygen and nutrient deprivation during cancer progression under normoxic and hypoxic conditions. Particularly, the sustained stimulation of epidermal growth factor receptor (EGFR), insulin-like growth factor-1 receptor (IGF-1R), stem cell factor (SCF) receptor KIT, transforming growth factor-β receptors (TGF-βRs) and Notch and their downstream signalling elements such as phosphatidylinositol 3′-kinase (PI3K)/Akt/molecular target of rapamycin (mTOR) may lead to an enhanced activity of HIFs. Moreover, the up-regulation of HIFs in cancer cells may also occur in the hypoxic intratumoral regions formed within primary and secondary neoplasms as well as in leukaemic cells and metastatic prostate and breast cancer cells homing in the hypoxic endosteal niche of bone marrow. The activated HIFs may induce the expression of numerous gene products such as induced pluripotency-associated transcription factors (Oct-3/4, Nanog and Sox-2), glycolysis- and epithelial-mesenchymal transition (EMT) programme-associated molecules, including CXC chemokine receptor 4 (CXCR4), snail and twist, microRNAs and angiogenic factors such as vascular endothelial growth factor (VEGF). These gene products in turn can play critical roles for high self-renewal ability, survival, altered energy metabolism, invasion and metastases of cancer cells, angiogenic switch and treatment resistance. Consequently, the targeting of HIF signalling network and altered metabolic pathways represents new promising strategies to eradicate the total mass of cancer cells and improve the efficacy of current therapies against aggressive and metastatic cancers and prevent disease relapse.
Keywords: Hypoxia, Hypoxia-inducible factors, Metabolic pathways, Cancer progression, Metastases, Cancer stem/progenitor cells, Cancer-initiating cells, Metastasis-initiating cells, Targeted therapies
Introduction
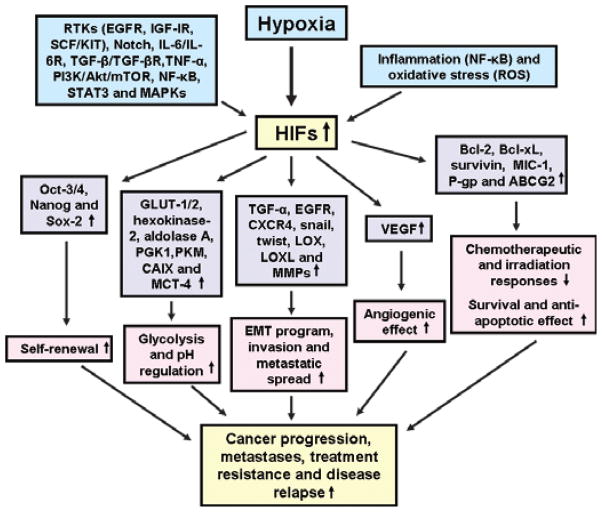
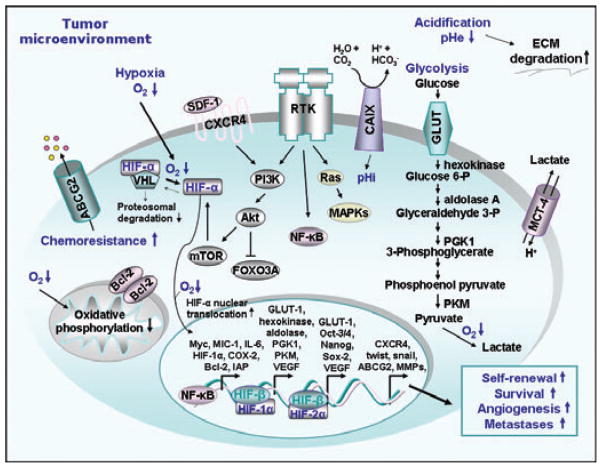
Recent advances in cancer research have indicated that the enhanced expression and activation of hypoxia-inducible factors (HIFs) frequently occur in cancer cells during cancer progression and is associated with their acquisition of a more malignant behaviour, treatment resistance and poor outcome of cancer patients (Fig. 1) [1–12]. Particularly, responses of cancer cells to environmental stress as observed for their normal counterparts generally implicate the induction of HIFs [1, 3–5, 9–16]. HIF transcription factors of the basic helix-loop-helix (bHLH)/PAS family include HIF-1α that is differently expressed in most tissues and HIF-2α which shows a more restricted tissue expression pattern in various locations, including kidneys, brain, lungs, liver, gastrointestinal tract, pancreas and heart [1, 2, 17, 18, 18–20]. The regulation of the cellular stability and activity of HIF-1α and HIF-2α in normal cells and cancer cells is highly dependent on oxygen supply (Figs 1–4) [3, 18, 21, 22]. In fact, oxygen-sensitive HIF-α proteins are generally hydroxylated by prolyl hydroxylase domain (PHD) proteins under normoxic conditions [21, 23]. This molecular event results in the interaction of HIF-α with Von Hippel-Lindau (VHL) tumour suppressor gene product, which is a component of the protein complex possessing a ubiquitin ligase E3 activity, that targets the HIF-α subunit for polyubiquitylation and subsequent proteasomal degradation (Fig. 3) [22, 23]. In contrast, the HIF-α subunit does not interact with the VHL protein in the presence of low oxygen levels and translocates to the nucleus where it forms a heterodimer with the constitutively expressed HIF-β partner subunit, also designated as aryl hydrocarbon receptor nuclear translocator (ARNT) that specifically binds to hypoxia-responsive elements (HREs) found in target gene promoters (Fig. 3) [3, 24].
Fig. 1.
Cellular events and signalling elements involved in the regulation of the stabilization and activation of hypoxia-inducible factors. The increase in the stability and activation of HIFs, HIF-1α and HIF-2α, in cancer cells including cancer stem/progenitor cells, which may be induced via different growth factor and cytokine pathways under normoxic and hypoxic conditions, hypoxic microenvironment and inflammation are illustrated. The potential cellular signalling elements modulated through the up-regulation of HIFs and which can contribute to high self-renewal, altered glycolytic metabolism, invasion, metastases, treatment resistance and disease relapse are also indicated. BCRP/ABCG2: breast cancer resistance protein; CAIX: carbonic anhydrase; EGFR: epidermal growth factor receptor; GLUT: glucose transporter; IL-6: interleukin-6; MAPK: mitogen-activated protein kinase; MCT-4: monocarboxylate transporter-4; MIC-1: macrophage inhibitory cytokine-1; MMPs: metalloproteinases; mTOR: molecular target of rapamycin; NF-κB: nuclear factor-κB; RTK: receptor tyrosine kinase; PI3K: phosphatidylinositol 3′-kinase; PGK1: phosphoglycerate kinase 1; PKM: pyruvate kinase M; P-gp: P-glycoprotein; ROS: reactive oxygen species; TGF-β: transforming growth factor-β; TNF-α: tumour necrosis factor-α; STAT3: signal transducer and activator of transcription 3; VEGF: vascular endothelial growth factor.
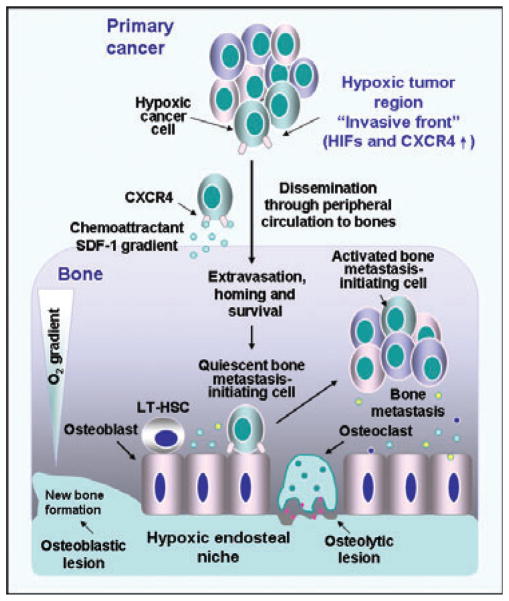
Fig. 4.
Proposed model of potential transforming events occurring in hypoxic cancer cells during epithelial cancer progression and bone metastasis. The up-regulated expression levels of stem cell-like phenotypes, HIFs, CXC chemokine receptor (CXCR4) and occurrence of the EMT programme in prostate or breast cancer cells within the hypoxic region at the invasive front of the primary tumour may lead to their invasion and dissemination through the peripheral circulation and homing at distant metastatic sites. More specifically, circulating prostate or breast cancer cells expressing high level of CXCR4 can preferentially disseminate and home to specific metastatic sites such as bones at least in part through the chemoattractant gradient formed by stromal cell-derived factor-1 (SDF-1) released by endothelial cells. The hypoxia-adapted prostate or breast cancer cells may compete with long-term haematopoietic stem cells (LT-HSCs) to occupy the hypoxic endosteal niche within BM and survive under a dormant state for a short or long period of time. The activation of dormant prostate or breast cancer cells may occur through the release of different growth factors and cytokines by cancer cells and stromal host cells under specific microenvironmental conditions. The activated prostate or breast cancer cells can give rise to the total tumour cell mass and skeletal metastasis formation. The bone metastases of prostate cancer cells are predominantly associated with the formation of osteoblastic lesions (bone formation), whereas bone metastases of breast cancer cells are generally related with the formation of osteolytic lesions (bone destruction).
Fig. 3.
Scheme showing the potential molecular events induced in cancer cells in the hypoxic tumour microenvironment. The intracellular consequences of decreased oxygen level (hypoxia) in cancer cells including the switch of mitochondrial oxidative phosphorylation to anaerobic glycolysis and enhanced nuclear translocation of HIF-α subunit are illustrated. The enhanced stabilization and activation of HIF-1α and HIF-2α and their formation of nuclear heterodimers with HIF-β receptor in cancer cells under hypoxia that in turn may result in the transcriptional activation of numerous gene products involved in anaerobic glycolysis, pH regulation, self-renewal, survival and induction of angiogenic switch and metastases are indicated. The enhanced cellular accumulation and activation of HIF-α protein subunit which may be induced through the stimulation of different receptor tyrosine kinases (RTKs) in cancer cells under normoxic and hypoxic conditions are also illustrated. Particularly, the stimulation of RTKs may lead to the sustained activation of phosphatidylinositol 3′-kinase (PI3K)/Akt/molecular target of rapamycin (mTOR) pathway that in turn may induce the translational machinery and HIF protein synthesis and/or enhanced stabilization of HIF-α subunit. Moreover, the activation of RTKs may result in the stimulation of nuclear factor-kappaB (NF-κB) that in turn can induce the transcriptional up-regulation of HIFs. ABCG2/BCRP: breast cancer resistance protein; CAIX: carbonic anhydrase IX; COX-2: clyooxygenase-2; ECM: extracellular matrix; FOXO3A: forehead 3A; GLUT: glucose transporter; HIFs: hypoxia-inducible factors; IAP: inhibitor of apoptosis protein; IL-6: interleukin-6; MAPK: mitogen-activated protein kinase; MCT: monocarboxylate transporter; MIC-1: macrophage inhibitory cytokine-1; MMPs: matrix metalloproteinases; pHe: extracellular pH; pHi: intracellular pH; PGK1: phosphoglycerate kinase 1; PKM: pyruvate kinase M; VEGF: vascular endothelial growth factor.
In addition to the up-regulation of HIF activity under low oxygen tension, the stability and activation of HIF-1α and HIF-2α in cancer cells may also be differently regulated through the sustained stimulation of different growth factor and cytokine pathways and oxidative stress under normoxic and hypoxic conditions (Figs 1 and 3) [25–33]. The growth factor signalling elements include different receptor tyrosine kinases (RTKs), such as epidermal growth factor receptor (EGFR/erbB1), HER2/erbB2/Neu, insulin-like growth factor-1 receptor (IGF-1R), stem cell factor (SCF)/KIT receptor, Notch, interleukin- 6/IL-6R receptor and transforming growth factor-β/TGF-βR receptors [25–39]. These tumourigenic pathways may cooperate to stimulate different downstream signalling elements, including phosphatidylinositol 3′-kinase (PI3K)/Akt/molecular target of rapamycin (mTOR), Ras/mitogen-activated kinase (MEK)/extracellular signal-regulated kinase (ERK), nuclear factor-kappaB (NF-κB) and signal transducer and activator of transcription 3 (STAT3) pathways that in turn up-regulate the expression and/or stability of HIF-α subunit [25–40]. Also, inactivation of tumour suppressor proteins such as pVHL, phosphatase tensin deleted on chromosome 10 (PTEN) and p53 in cancer cells may impair HIF degradation and/or enhanced PI3K/Akt activation and lead to HIF-α protein accumulation and increased expression of many HIF-regulated genes under normoxic and hypoxic conditions [1, 22, 28, 38, 41, 42]. Hence, HIF transcription factors can activate the transcription of numerous gene products that contribute to the malignant reprogramming of cancer cells during cancer progression and metastases and tumour angiogenic switch (Figs 1 and 3) [4, 25–33, 36, 37, 39, 41–44].
Importantly, recent findings have also indicated that HIF-1α and HIF-2α play critical roles for the gain of more malignant phenotypes by highly tumourigenic cancer stem/progenitor cells endowed with stem cell-like properties also designated as cancer-, tumour-, and metastasis-initiating cells that are able to generate the bulk mass of heterogeneous and differentiated cancer cells within tumours and which are involved in primary cancer progression, metastases, resistance to current cancer therapies and disease relapse [14, 45–53]. Thus, the complete eradication of the total mass of tumour cells, including hypoxic and normoxic cancer stem/progenitor cells and their differentiated progenies, by targeting the HIF signalling network might be crucial to improve current cancer therapies and prevent disease relapse. New therapeutic strategies such as guanine-rich oligodeoxynucleotides (G-rich ODNs), chemical compounds and chemotherapeutic drugs that target HIF-1α and/or HIF-2α proteins and repress the expression of their target genes in various cancer cells have been shown to counteract primary cancer progression and metastases at distant sites, and reverse treatment resistance under normoxic and hypoxic conditions (Tables 1 and 2) [11, 39, 44, 54–66]. In this matter, we review recent findings indicating pivotal roles of HIF-1α and HIF-2α in the modulation of stemness properties and altered metabolic pathways of cancer stem/progenitor cells and their differentiated progenies during the development of diverse aggressive and recurrent cancers. The emphasis is on the functions of HIFs during leukaemogenesis and the development of glioblastoma multiforme, melanoma and prostate, breast and pancreatic cancers and novel targeted therapies directed against HIFs and altered metabolic pathways, including glycolysis, lipogenesis and autophagy.
Table 1.
Potential therapeutic strategies targeting altered growth factor and intracellular elements in normoxic and hypoxic cancer- and metastasis-initiating cells and their differentiated progenies
| Molecular target | Name of inhibitory agent |
|---|---|
| Hypoxia-activated pro-drug | |
| Hypoxic cancer cells | TH-302 |
| Growth factor signalling elements | |
| EGFR (erbB1) | Anti-EGFR mAb (cetuximab or IMC-C225 (Erbitux®)*, panitumumab (Vectibix®)*, mAb-C225); TKI (gefitinib (Iressa®)*, erlotinib (Tarceva®)*, AG1478) |
| HER-2 (erbB2) | Anti-HER-2 mAb (trastuzumab (Herceptin®)*) |
| IGF-1R | Anti-IGF-1R mAb (robatumumab or R1507); TKI (NVP-AEW541, BMS-536924) |
| TGF-βRI | SD-208 |
| KIT | Imatinib mesylate (Gleevec®)*, dasatinib (Sprycel®)* nilotinib or AMN107 (Tasigna®)*, bafetinib (INNO-406) |
| Notch | γ-secretase inhibitor (DAPT, MK-0752, GSI-18) |
| Nodal/Cripto | Anti-Cripto mAb, LEFTY |
| Wnt/β-catenin | Anti-Wnt antibody, AV65, WIF-1 |
| CXCR4 | Anti-CXCR4 mAb, CXCR4 antagonist (plerixafor or AMD3100 (Mozobil®)*) |
| VEGF | Anti-VEGF mAb (bevacizumab (Avastin®)*) |
| VEGFR-2 | Anti-VEGFR-2 mAb (ramucirumab or IMC-1121B, DC101 or IMC-1C11) |
| VEGFR-2, EGFR, RET-TKI | MKI (Vandetanib or ZD6474) |
| VEGFRs, PDGFRs, KIT | MKI [Sunitinib (Sutent®)*, Axitinib or AG-013736 (Inlyta®)*] |
| VEGFR-2 and -3, PDGFRs, KIT, B-Raf, C-Raf | MKI (Sorafenib (Nexavar®)*) |
| VEGFRs, PDGFRs, FGFR-1, FGFR-3, KIT, Itk, Lck and c-Fms | MKI (Pazopanib (Votrient®)*) |
| Intracellular signalling elements | |
| HIFs | YC-1, P276-00, P3155, NSC-134754, PX-478, KCN1 G-rich ODNs (JG243 and JG244), anthracyclins, 2-methoxyestradiol, echinomycin, Rakicidin A |
| PI3K | LY294002, Wortmannin |
| mTOR | Everolimus or RAD001 (Afinitor, Zortress or Certican®)*, temsirolimus or CCI-779 (Torisel®)*, sirolimus or rapamycin (Rapamune®)* |
| PI3K/mTOR | PI-103, NVP-BEZ235 |
| Ras | S-trans trans-farnesylthiosalicylic acid |
| NF-κB | bortezomib (Velcade®)*, sulphasalazine (Azulfidine®)*, salinosporamides A (NPI-0052), parthenolide IkBα inhibitor (PS-341) |
| STAT3 | G-rich ODN (T40214) |
| COX-2 | Etodolax (Lodine SR or Eccoxolac®)*, NS-396 |
| Bcl-2 and/or Bcl-xL | AS (oblimersen sodium (Genasense®)*), ABT-263 |
| BCR-ABL | Imatinib mesylate (Gleevec®)*, dasatinib (Sprycel®)* nilotinib or AMN107 (Tasigna®)*, bafetinib (INNO-406) |
Trade name of Food and Drug Administration (FDA) approved drug for treating specific cancer(s) and/or other disorder(s).
c-Fms: transmembrane glycoprotein receptor tyrosine kinase; AS: antisense oligonucleotide; COX-2: clyooxygenase-2; CXCR4: CXC chemokine receptor 4; DAPT: N-(N-3,5-difluorophenacetyl)-L-alanyl]-S-phenylglycine t-butyl ester; EGFR: epidermal growth factor receptor; G-rich ODNs: guanine-rich oligodeoxynucleotides; FGFR: fibroblast growth factor receptor; IGF-RI: insulin-like growth factor-1 receptor; Itk: interleukin-2 receptor inducible T-cell kinase; KCN1: 3,4-dimeth-oxy-N-[(2,2-dimethyl-2H-chromen-6-yl)methyl]-N-phenylbenzenesulpfonamide; Lek: leucocyte-specific protein tyrosine kinase; mAb: monoclonal antibody; MKI: multi-targeted kinase inhibitor; NF-κB: nuclear factor-kappaB; PI3K: phosphatidylinositol 3′-kinase; STAT3: signal transducer and activator of transcription 3; TGF-βR: transforming growth factor-β receptor; TKI: tyrosine kinase inhibitor; VEGF: vascular growth factor; Wnt: Wingless ligand.
Table 2.
Potential therapeutic strategies targeting altered metabolic and pH regulatory signalling pathways in normoxic and hypoxic cancer- and metastasis-initiating cells and their differentiated progenies
| Molecular therapeutic target | Name of inhibitory agent |
|---|---|
| Altered metabolic signalling elements | |
| Glucose transporters | 2-deoxy-D-glucose |
| Hexokinase-2 | Lonidamine |
| Glyoxalase-1 | S-p-bromobenzylglutathione |
| FASN | Orlistat, cerulenin, C75, resveratrol |
| Monoacylglycerol lipase | JZL184 |
| Autophagy | Bafilomycin A1, 3-methyladenine, chloroquine (Aralen®)*, hydrochloroquine (Plaquenil®)* |
| pH regulatory signalling element | |
| CAIX | Anti-CAIX mAbs (M75 and G250), glycosyl coumarins (GC-204 and GC-205), sulphonamides (CAI17, ureido-sulphonamide, U-104) |
Trade name of Food and Drug Administration (FDA) approved drug. CAIX: carbonic anhydrase IX; FASN: fatty acid synthase.
Critical functions of HIFs in the acquisition of more malignant phenotypes and behaviour by cancer- and metastasis-initiating cells and their differentiated progenies
A growing body of experimental evidence has indicated that most human cancers may originate from the accumulation of different genetic and epigenetic alterations in tissue-resident adult stem cells and/or their early progenitors with stem cell-like properties during the lifespan resulting in their malignant transformation into cancer stem/progenitor cells [45, 47, 49, 52, 53, 67–73]. In support of this, cancer cells expressing stem cell-like markers and endowed with a high self-renewal ability and aberrant differentiation potential have been identified and isolated from primary neoplasms, peripheral circulation and metastatic tissue specimens [45, 53, 68, 71, 73–83]. Cancer types harbouring a cancer stem/progenitor cell subpopulation include leukaemias, brain tumours, melanomas and various epithelial cancers such as lung, liver, gastrointestinal, colorectal, pancreatic, breast, ovarian and prostate cancers [45, 47, 53, 68, 71, 73–77, 79, 80, 82–86]. It has been shown that cancer stem/progenitor cells can give rise to the total mass of heterogeneous and differentiated cancer cells within primary and secondary tumours and play key roles for invasion, metastases at regional and distant tissues as well as tumour angiogenesis [45, 47, 49, 52, 53, 68, 69, 71, 73–77, 79, 82, 83, 87–89]. New findings have also indicated that cancer- and metastasis-initiating cells with stem cell-like features typically display a higher resistance than the bulk mass of differentiated cancer cells to oxygen and nutrient deprivation and current anti-hormonal, radiation therapy and chemotherapy, and thereby they can be responsible for disease relapse [6, 12, 49, 51–53, 56, 73–77, 79, 82, 83, 88, 90–96].
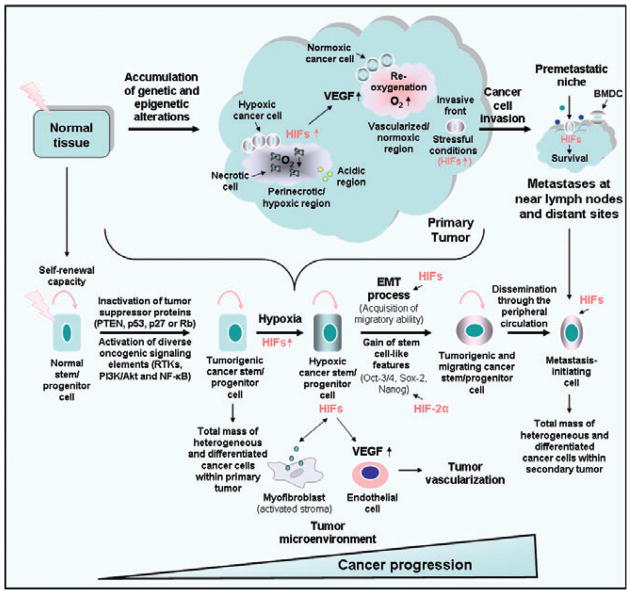
Recently, the cancer stem cell hypothesis has also been reviewed to consider the complexity of molecular transforming events that may occur in these immature cancer cells and their differentiated progenies as well as their local microenvironment under normoxic and hypoxic conditions during cancer development [6, 47, 49, 82, 83]. Based on the cancer stem cell concept, cancer heterogeneity may be attributed to the differences between tissue-resident stem/progenitor cell types at the origin of particular cancer subtypes as well as progressive changes in the number and phenotypes of these immature cancer cells and their differentiated progenies and their local microenvironment during disease progression and after treatment initiation (Fig. 2) [7, 47, 82, 83, 97]. In this regard, rapidly growing tumours are typically characterized by disorganized vasculature with an abnormal leaky and tortuous structure [5–7, 98–100]. These rapidly growing tumours also exhibit hypoxic intratumoral regions that did not supply sufficient oxygen and nutrients to cells and require a high adaptation of cancer cells for their survival [5–7, 98–100]. It has been shown that changes in the local microenvironment of cancer stem/progenitor cells and their progenies, including the induction of hypoxic intratumoral regions within poorly vascularized tumours, may result in alterations of different gene products that contribute to their acquisition of more aggressive phenotypes and survival advantages [1, 7, 14, 46, 48, 50, 51, 66, 89, 98–104]. More specifically, it has been observed that hypoxia and enhanced expression and activity of HIF-1α and HIF-2α in cancer stem/progenitor cells and their progenies frequently occur during disease progression and metastases and may result in the up-regulation of different stemness gene products and survival signalling elements [6, 14, 48, 50, 90, 94, 99, 102, 104, 105]. The altered gene products modulated by HIFs comprise the regulators of induced pluripotency (octamer-binding transcription factor Oct-3/4, Sox-2 and Nanog), epithelial-mesenchymal transition (EMT) programme (EGFR, CXCR4, snail and twist), glucose transporters (GLUT-1/2) involved in the glucose uptake, altered metabolic pathways such as glycolytic enzymes, microRNAs (miRNAs) and drug resistance- associated molecules (ABCB2, Bcl-2, Bcl-xL, survivin and macrophage inhibitory cytokine-1 ‘MIC-1’; Figs 1–3) [4, 14, 22, 25, 51, 99, 100, 106–110]. These HIF-induced signalling elements may provide critical functions for high self-renewal capacity, energy supply through enhanced aerobic and anaerobic glycolysis, invasion, metastases and treatment resistance of cancer- and metastasis-initiating cells and their differentiated progenies [4, 14, 22, 25, 99, 100, 106–112].
Fig. 2.
Proposed model of malignant transforming events associated with cancer progression and metastases driving hypoxia and enhanced expression of HIFs in cancer stem/progenitor cells. Genetic and epigenetic alterations occurring in tissue-resident adult stem/progenitor cells during intense injury, oxidative stress, inflammation and/or ageing may result in their malignant transformation into tumourigenic cancer stem/progenitor cells also designated cancer-initiating cells that are able to generate the bulk mass of heterogeneous and differentiated cancer cells within tumour. The scheme also shows the potential localization of clusters of cancer stem/progenitor cells expressing HIFs at the hypoxic region near a necrotic areas and invasive front of the primary tumour. The enhanced expression of HIFs in highly tumourigenic cancer stem/progenitor cells and their differentiated progenies, which may be induced under hypoxia or sustained activation of growth factor pathways and PI3K/Akt/mTOR under normoxic and hypoxic conditions, may promote the EMT programme, altered metabolic pathways and re-expression of stem cell-like markers such as Oct-3/4, Sox-2 and Nanog and pro-angiogenic factor VEGF. These molecular transforming events in turn may contribute to the acquisition of a more malignant behaviour and migratory ability by cancer cells and tumour neovascularization. Moreover, bi-directional cross-talks between cancer cells and stromal myofibroblasts found within their local tumour microenvironment also may promote their gain of more aggressive phenotypes. Hence, highly tumourigenic and migratory cancer stem/progenitor cells with stem cell-like properties that survive under stressful conditions, including low oxygen tension and nutrient deprivation, during primary cancer progression and reach the invasive front of primary tumour can be involved in dissemination and metastatic spread at near lymph nodes and distant tissues. The disseminated cancer stem/progenitor cells that are able to survive in their novel microenvironment prevalent at metastatic sites can give rise to the total mass of differentiated cancer cells forming secondary tumours. The preferential migration of cancer cells to pre-metastatic niches induced by different soluble factors released from primary tumour and bone marrow-derived cells (BMDCs) at distant sites is also illustrated.
In addition, among other important gene products modulated by HIF-1α, monocarboxylate transporter-4 (MCT-4) and carbonic anhydrase IX (CAIX) are often overexpressed in several cancer types as compared with normal tissues and involved in the pH regulatory system of hypoxic cancer cells characterized by a high rate of glycolytic metabolism and production of acidic metabolites such as lactic and carbonic acids (Fig. 3) [113–116]. More specifically, MCT-4 can contribute to the export of lactate into extracellular space of cancer cells [115, 116]. Furthermore, CAIX is a dimeric transmembrane metalloenzyme that catalyses the rapid interconversion of carbon dioxide (CO2) molecules to bicarbonate (HCO3−) and protons (H+) in the extracellular space of hypoxic cancer cells [113–115]. Hence, bicarbonate generated by CAIX may be subsequently transported by different bicarbonate transporters such as sodium bicarbonate co-transporters into cancer cells, and thereby plays key roles for the maintenance of intracellular pH (pHi) necessary for the survival and growth of cancer cells [113–115]. Also, the generation of protons through the hydration of carbon dioxide by CAIX and accumulation of acidic metabolites in the local microenvironment of cancer cells may contribute to the acidification of extracellular pH (pHe) that favours the normal cell death, degradation of extracellular matrix (ECM), stromal invasion and metastases of cancer cells (Fig. 3) [113–115]. In addition, the induction of tumour angiogenesis by HIFs through the up-regulated expression of pro-angiogenic factors such as vascular endothelial growth factor (VEGF) in cancer stem/progenitor cells and their differentiated progenies may also promote the tumour growth and formation of invasive and metastatic cancers (Figs 1–3) [25, 35, 39, 106, 117–119].
Although a highly structural homology exists between HIF-1α and HIF-2α, these transcription factors may also be differently regulated and transactivate common and unique targeted gene products in a cancer cell-dependent manner under normoxic and hypoxic conditions (Fig. 3) [16, 20, 24, 89, 106, 107, 117, 120–125]. Particularly, the differences between the tissue expression pattern and transactivation domains of HIF-1α and HIF-2α proteins and their recruitment of different transcriptional factors acting co-activator or co-repressor may lead to their activation of specific gene subsets in normal and cancer cells [20, 23, 24, 106, 122, 123]. The transcription factors that can cooperate with HIFs include different histone acetyl transferase (HAT) co-activators such as CREB-binding protein (CBP)/adenovirus E1A-binding protein p300 (p300) and proteins in steroid receptor co-activators (SRCs)/p160 family such as SRC-1 [20, 23, 24, 106, 122, 123]. In general, HIF-1α may specifically induce the enhanced expression of CAIX, lysyl oxidase (LOX) and glycolytic enzymes such as hexokinase-2, aldolase A, phosphoglycerate kinase 1 (PGK1) and pyruvate kinase M (PKM), whereas HIF-2α appears to preferentially up-regulate the gene products including TGF-α, Myc, cyclin D1 and embryonic stem cell-like markers such as Oct-3/4, Sox-2 and/or Nanog in cancer cells under normoxic and hypoxic conditions (Figs 1 and 3) [16, 106, 107, 117, 120, 121, 124–127]. In this regard, we review the molecular mechanisms controlling the expression levels and specific functions of HIF-1α and HIF-2α and their downstream signalling elements during initiation and progression of leukaemias, glioblastoma multiforme, melanoma and epithelial cancers such as prostate, breast and pancreatic cancers.
Functions of HIF-1α in leukaemic stem/progenitor cells and their differentiated progenies and novel targeted therapies
Numerous investigations have revealed that leukaemias may originate from the accumulation of genetic and/or epigenetic alterations occurring in haematopoietic stem cells (HSCs), precancerous-LSCs (pre-LSCs) or more committed myeloid progenitor cells endowed with a high self-renewal ability and aberrant differentiation potential [45, 68, 69, 71, 87]. Importantly, recent lines of experimental evidence have also indicated that LSCs and their early progenitors may occupy the endosteal and perivascular niches of normal haematopoietic stem/progenitor cells (HSCs and HPCs) [45, 55, 72, 87, 128, 129]. More particularly, the homing of primitive LSCs in the hypoxic microenvironment in BM endosteum, which may lead to an up-regulation of HIF-1α and metabolic adaptation of these immature leukaemic cells to low oxygen supply and glucose availability as observed for their normal counterpart, long-term HSCs (LT-HSCs), may contribute to their survival and treatment resistance [6, 55, 56, 69, 90, 128–130]. In fact, the homing of LSCs under a quiescent state in the more hypoxic endosteal region of BM may allow these immature leukaemic cells to exist in a low cycling state that protects them from oxidative stress, DNA damages and cell death stimuli induced by cytotoxic agents [45, 87, 90, 94, 129].
More particularly, chronic myeloid leukaemia (CML) is a clonal disorder which is often accompanied by a chromosomal translocation resulting in a shortened chromosome 22, designated the Philadelphia (Ph+) chromosome in HSCs [68–70]. This molecular event generates a chimeric BCR-ABL fusion oncoprotein endowed with a constitutive tyrosine kinase activity in LSCs in the initial chronic phase of CML [68 –70]. Typically, this initial chronic phase of CML progresses to an accelerated phase mediated through the occurrence of further oncogenic events in LSCs, that ultimately leads to the terminal phase of CML, designated as blast-crisis (Bc)-CML [68–70, 131]. Also, an increase in the β-catenin level may occur in the granulocyte-macrophage progenitors when patients reach a later stage of Bc-CML and result in their acquisition of an enhanced self-renewal capacity and leukaemic potential [68, 130]. In this matter, it has been shown that tyrosine kinase inhibitors (TKIs) such as imatinib mesylate (IM) or the second generation of drugs, including dasatinib, nilotinib and bafetinib (INNO-406), targeting the BCR-ABL fusion protein in proliferative leukaemic cells are highly effective for treating patients with chronic phase CMLs and Ph-positive acute lymphoid leukaemias (ALLs) [6, 56, 91–93, 130, 132]. Unfortunately, CML cells can exhibit BCR-ABL kinase-dependent and -independent mechanisms of resistance to these TKIs [6, 56, 91–93, 130]. Moreover, these TKIs did not appear to eradicate the total mass of leukaemic cells including primitive and quiescent BCR-ABL LSCs with a high self-renewal potential [6, 56, 91–93, 130]. Consequently, the persistence of LSCs in the hypoxic endosteal niche of BM after cessation of TKI therapy may result in disease relapse and require a long-life treatment with TKIs for the survival of CML patients [6, 56, 91–93, 130]. Importantly, it has been observed that human BCR-ABL+ CML-LSCs engrafted in the BM of immunodeficient mice and survived under severe hypoxia (<1.3% oxygen) along the endosteum [90]. It has also been shown that BCR-ABL fusion oncoprotein can up-regulated the expression levels of HIF-1α and its target genes via the stimulation of PI3K/Akt/mTOR pathway in the murine BCR-ABL+ Ba/F3 leukaemic cell line and contribute to their survival [55]. Moreover, hypoxia and HIF-1α in turn can promote the selection of LSCs in CML that are refractory to IM and bortezomib [90, 94, 133]. More specifically, it has been reported that hypoxia-adapted BCR-ABL+ leukaemic cell lines obtained after long-term culture under 1% oxygen level exhibited stem cell-like properties, a great number of leukaemic cells in the side population (SP) and under a dormant state, high resistance to TKIs including IM, INNO-406 or dasatinib, enhanced expression level of β-catenin and glyoxalase-1 activity and transplantation efficacy [90]. Hence, these data suggest that BCR-ABL induced–enhanced expression of HIF-1α in CML cells, including CML-LSCs, may contribute to their quiescence and survival in the hypoxic endosteal niche of HSCs in BM after treatment initiation and disease relapse.
Of therapeutic interest, the deletion of HIF-1α in a mouse model of human CML has been observed to inhibit the cell cycle progression and induce the apoptosis via an induction of p16INK4A and p19ARF tumour suppressor proteins in LSCs [55]. Moreover, it has been shown that a natural product of Micromonospora strain designated as Rakicidin A, which acts as a hypoxia-selective cytotoxin, was effective at inducing the apoptotic death of TKI-resistant and hypoxia-adapted BCR-ABL+ CML cells endowed with stem cell-like properties maintained in suspension under low-oxygen conditions for more than 6 months [56]. The combined use of Rakicidin A plus IM or dasatinib also resulted in synergistic cytotoxic effects on hypoxia-adapted BCR-ABL + CML cells [56]. In the same way, it has also been observed that the down-regulation of HIF-1α by small hairpin RNA (shRNA) or using a HIF-1α inhibitor, echinomycin eradicated mouse lymphoma-initiating cells and human acute myeloid leukaemia (AML)-LSCs in both in vitro colony formation assays and in vivo mouse models, whereas normal HSCs were 100-fold less sensitive to echinomycin than lymphoma CSCs in vitro [134].
On the other hand, other molecular mechanisms that may contribute to the resistance of LSCs or their early progenitors also include the elevated expression of β-catenin and enhanced glycolytic metabolism and autophagy under normoxic and hypoxic conditions [90, 130, 135]. Importantly, a novel Wnt/β-catenin signalling inhibitor, AV65, has been reported to reduce the β-catenin expression and inhibit the proliferation of IM-resistant and hypoxia-adapted CML cells [130]. It has also been noted that a combination of AV65 plus IM induced synergistic anti-proliferative effects on CML cells [130]. Moreover, the targeting of glyoxalase-1, which catalyses the detoxification of a highly cytotoxic by-product of glycolysis termed methylglyoxal, using a specific inhibitor termed S-p-bromobenzylglutathione cyclopentyl diester was also more effective at inducing the apoptotic effects on TKI-resistant, quiescent and hypoxia-adapted BCR-ABL leukaemic cells with acquired stem cell-like features than on parental leukaemic cell lines in vitro and in vivo [90]. In the same way, the inhibition of autophagy by using pharmacological agent such as bafilomycin A1 or 3-methyladenine as well as chloroquine which can act as an inhibitor of late-stage autophagy has been observed to potentiate the cytotoxic effects induced by TKIs such as IM or dasatinib on CML cells, including more primitive CML-LSCs, in vitro and in vivo [135].
Overall, these recent studies have underlined the critical role of hypoxia and H1F-1α, altered metabolic pathways and autophagy for the survival and treatment resistance of LSCs in the hypoxic microenvironment of BM, including in the insensitivity of BCR-ABL+ CML-LSCs to TKIs that target the bulk mass of proliferative leukaemic cells. Thus, the combined inhibition of H1F-1α, glycolysis and autophagy constitutes promising approaches to kill the LSC subpopulation in the hypoxic endosteal niche of BM that may be responsible for treatment resistance and disease relapse, and thereby improve the efficacy of current therapies against aggressive and recurrent leukaemias.
Functions of hypoxia and HIFs in the development of glioblastoma multiforme and targeted therapies
Glioblastomas are among the most frequent, aggressive and lethal brain tumours because their rapid progression to locally invasive disease states and development of different molecular mechanisms of resistance by tumour cells to current radiation therapies and chemotherapies with DNA-alkylating agents such as temozolomide, nitrosoureas and/or cisplatin [82, 136–138]. In this regard, recent accumulating lines of evidence have revealed that a subpopulation of glioma stem cells (GSCs), also designated as glioma-initiating cells, expressing stem cell-like markers such as CD133, nestin, CD44, Oligo- 2, Oct-3/4, Sox-2, Nanog, Musashi and/or Bmi-1 and endowed with high self-renewal and tumourigenic capacities may be responsible for driving glioblastoma multiforme (GBM) development, local invasion, resistance to current therapeutic treatment and disease recurrence [82, 126, 127, 139–141].
Glioblastoma multiforme is a heterogeneous disease and encompasses distinct molecular subtypes characterized by specific gene signatures [82, 142–144]. In general, GBMs are highly vascularized tumours and exhibit intratumoral heterogeneity, including in phenotypic features of tumour cells found within normoxic and hypoxic regions [1, 82, 127]. Particularly, GBM pathogenesis typically implicates an increased expression of many growth factors, cytokines and chemokines and their cognate receptors in tumour cells that cooperate to their malignant transformation and acquisition of more aggressive phenotypes and tumour neoangiogenesis during progression to locally invasive GBMs [82]. The changes within local tumour microenvironment of GBM cells, including hypoxia also may induce the enhanced expression of HIF-1α, HIF-2α and stem cell-like markers such as pluripotency-associated gene products Oct-3/4, Sox-2, Nanog and Myc that promote their stem cell-like properties and gain of a more aggressive behaviour [126, 127, 145, 146]. Importantly, immunohistochemical analyses have indicated that HIF-1α and HIF-2α and their target genes, including glycolytic enzymes and VEGF are frequently overexpressed in tumour cells in hypoxic zones closest to areas of necrosis, which demarcate surrounding regions of tumour angiogenesis, during GBM development [1, 2, 127]. Moreover, it has been noticed that an enhanced expression of HIF-1α and HIF-2α in tumour cells was strongly correlated with tumour grade and vascularity of GBM tissue specimens [1]. These data suggest that HIF-1α and HIF-2α can contribute to the rapid re-oxygenation of hypoxic zones of GBMs that may be mediated in part through the enhanced expression of pro-angiogenic factors such as VEGF (Fig. 2). In this regard, it has also been observed that GSCs are enriched in a region, designated as vascular niche around tumour vessels as well as in a hypoxic niche localized near necrotic areas associated with restricted oxygen and nutrients [82, 139–141]. It has also been shown that HIF-2α can play key roles in GSCs found within perinecrotic/hypoxic niche by inducing enhanced expression of specific tumour stem cell signature genes, including mastermind-like protein 3 (Notch pathway), nuclear factor of activated T cells 2 (calcineurin pathway) and aspartate β-hydroxylase domain-containing protein 2 that are associated with a poor prognosis of GBM patients [147]. In the same way, the enhanced expression of HIF-1α in CD133+ GSCs from human glioma specimens propagated under hypoxia (1% oxygen) also promoted their self-renewal capacity, inhibited their differentiation and led to the expansion of GSCs expressing CXCR4, CD44low and A2B5 surface markers [148].
Interestingly, it have also been observed that GSCs expressing stem cell-like markers CD133, Oligo-2, Oct-3/4, Sox-2, Nanog, Musashi and Bmi-1 from human glioblastoma biopsy specimens xenografted into brains of immunocompromised mice secreted high levels of VEGF, which were promoted under hypoxia, and generated highly vascularized tumours with areas of necrosis and haemorrhage [149]. In contrast, CD133− tumour cells only formed a few secondary tumours that were poorly vascularized [149]. In the same way, the data of immunohistochemical analyses have indicated that HIF-2α was co-expressed with CD133 stem cell-like marker in GBM tissue specimens, and associated with a poor survival of glioma patients [127]. It has also been noted that HIF-2α and its target genes, including Oct-3/4, SerpinB9, GLUT-1 and VEGF were preferentially expressed in CD133+ GSCs from glioblastoma surgical biopsy specimens or xenografts derived from brain tumour specimens as compared with CD133− tumour cells under hypoxic conditions [127].
In addition, the maintenance of GSCs and their differentiated progenies in normoxic and hypoxic regions within tumours also requires the interplay of different intrinsic and extrinsic factors that govern the embryonic brain tumour development [41, 82, 127, 150, 151]. Particularly, the sustained activation of different growth factor cascades, including EGFR, constitutively activated EGFRvIII mutant and IGF-1/IGF-1R may stimulate PI3K/Akt/mTOR signalling elements that in turn induce the stabilization and/or translation of HIF-1α and HIF-2α proteins in GSCs and their progenies and angiogenic switch [82, 137, 152]. Moreover, GBM development is typically characterized by a high incidence of PTEN mutation in late stage of tumorigenesis [41, 82, 137, 153]. PTEN inactivation may promote the sustained activation of PI3K/Akt pathway that in turn can induce HIF-1α stabilization and transcriptional expression of its target genes, and thereby contribute to the survival of GBM cells under normoxic and hypoxic conditions [41, 82, 137, 153]. For instance, it has been observed that the ectopic overexpression of wild-type PTEN in the human U373 glioblastoma-derived cell line lacking functional PTEN reduced IGF-1- and hypoxia-induced Akt activation and consequently the HIF-1α stabilization and expression of its target gene products, including glycolytic enzymes, PGK-1 and PFK, COX-1 and VEGF [41].
Of therapeutic interest, numerous studies have also indicated the benefit to target HIF signalling network, including growth factors implicated in the regulation of HIF activity, altered metabolic pathways and angiogenic factors to kill GSCs and their differentiated progenies under normoxic and hypoxic conditions, and thereby prevent GBM progression to locally invasive disease state [108, 127, 148, 154, 155]. For instance, it has been observed that the targeting of HIF-1α or HIF-2α by shRNA in CD133+ GSCs from a patient’s glioblastoma specimen inhibited their neurosphere-forming ability and proliferation, induced the caspase-dependent apoptotic effect in vitro and attenuated their tumour-initiating potential in vivo [127, 148]. Moreover, the down-regulation of histone methyltransferase mixed-lineage leukaemia 1 (MLL1) by shRNA in GBM cells, which is induced under hypoxic condition, was also effective at reducing the expression of HIF-2α protein and its target genes, including VEGF and inhibiting the self-renewal, growth and tumourigenicity of GSCs [108]. The targeting of VEGF using neutralizing mAb, bevacizumab was also effective at inhibiting tumour growth of xenografts derived from CD133+ glioma-initiating cells or U87 glioma cells by decreasing the number of self-renewing and vessel-associated CD133+/nestin+ tumour cells [141, 149].
In addition, the down-regulation of key regulators of autophagy such as DNA-damage regulated autophagy modulator protein 1 (DRAM1) or p62 encoded by sequestosome 1 (SQSTM1) by shRNA in GSCs has also been shown to impair autophagy, reduce metabolic energy, including ATP and lactate levels, and inhibit the migration and invasion of GSCs [154]. Moreover, the data from a randomized and double-blind, placebo-controlled trial carried out with 30 patients with surgically confirmed GBMs have also indicated that the autophagy inhibitor, chloroquine improved the anticarcinogenic efficacy induced by conventional radiotherapy and chemotherapy and median survival of GBM patients [156].
Collectively, these observations suggest that HIF-induced–enhanced glycolysis and VEGF expression as well as altered autophagy in GSCs may represent selective adaptations that are necessary for their survival under stressful conditions, including in a hypoxic microenvironment and nutrient deprivation, rapid tumour neovascularization and re-oxygenation and progression to locally invasive disease states. The development of new combination therapies consisting to target HIF signalling network and altered metabolic pathways in GSCs and their progenies as well as the components of their vascular and hypoxic niches represents new therapeutic strategies to improve the efficacy of current therapies and counteract the progression to highly invasive and lethal GBMs.
Functions of hypoxia and HIFs in the development of melanoma and targeted therapies
Malignant cutaneous melanoma is the most aggressive and lethal form of skin cancer with a poor prognosis for patients with advanced disease [157–160]. Although surgical tumour excision of early melanocytic lesions is associated with high cure rates, the rapid progression to locally invasive and metastatic melanomas that are resistant to current radiotherapies and chemotherapies usually led to disease relapse and the death of melanoma patients [157–160]. A growing body of evidence has indicated that intertumoral and intratumoral heterogeneity of melanomas may be due in part to the differences between melanoma stem/progenitor cells at the origin of a particular melanoma subtype as well as the changes in their number and phenotypic and functional features during melanoma progression and after treatment initiation. In support with this, a subset of melanoma stem/progenitor cells expressing stem cell-like markers such as CD133, nestin, neural crest nerve growth factor receptor CD271, Oct-3/4, Nanog, multi-drug resistance protein-1 (MDR1), ABCG2 and/or ABCB5 has been isolated from human primary and metastatic melanoma specimens or melanoma cell lines [83, 161–165]. Tumourigenic melanoma stem/progenitor cells with high self-renewal capacity and aberrant differentiation potential were able to generate melanomas when transplanted into human skin or bone or animal models with histopathological features resembling human melanomas [161–164].
Importantly, high expression levels of HIF-1α, HIF-2α and their target genes such as VEGF, have also been detected in melanoma cells in up to 80% cases of primary and metastatic melanoma specimens from patients, and more particularly at the margin of necrotic areas of tumours, and associated with melanoma progression as well as a poor prognosis of patients [1, 166–169]. Moreover, a nuclear staining for pluripotency-associated transcription factor Oct-3/4 was also seen in a small subset of melanoma cells, and particularly in hypoxic cancer cells near necrotic areas within primary melanomas in vertical growth phase or metastatic melanoma tissue specimens [112]. It has also been shown that the exposure of melanoma cell lines to hypoxia up-regulated expression levels of HIF-1α and HIF-2α and their target genes including Oct-3/4, Nanog, Nodal, connective tissue growth factor (CTGF), snail-1 and VEGF that in turn promoted their self-renewal ability, tumourigenicity, metastatic potential and resistance to current chemotherapeutic drugs such as temozolomide and cisplatin as well as angiogenic switch [112, 170–172]. The ectopic overexpression of Oct-3/4 in melanoma cell lines was also effective to enhance their expression of stem cell-like markers such as CD271, MDR1, ABCG2, ABCB5, Kruppel-like factor 4 (KLF4) and Nanog and self-renewal capacity [112].
In addition to hypoxia, enhanced expression and/or stability of HIFs in melanoma cells may also be induced by stress signals such as heat shock and reactive oxygen species (ROS), microphthalmia-associated transcription factor (MITF) and stimulation of oncogenic growth factor cascades under normoxic and hypoxic conditions [173 –180]. The tumourigenic signalling elements involved in the modulation of HIF activity include Notch, endothelins (ETs)/ETB receptor and constitutively activated B-Raf or N-Raf mutant that may contribute to the sustained activation of PI3K/Akt, MAPKs and/or NF-κB [173–180]. Particularly, it has been shown that B-RafV600E mutant may induce an increase in HIF-1α expression under normoxic and hypoxic conditions [177]. It has also been noticed that the expression of a HIF-1α785 isoform lacking a part of the oxygen regulation domain and which is more stable than full-length HIF-1α under high oxygen tension, was also induced by 12V-H-Ras, hyperthermia, serum, EGF, phorbol 12-myristate 13-acetate (PMA), heat and oxidative stresses in melanoma cell lines under normoxic conditions [178, 181]. Moreover, tumour hypoxia has also been associated with enhanced expression of HIFs, lactate dehydrogenase 5 and autophagy-related proteins, including beclin-1 and light chain 3A (LC3A), in hypoxic melanoma cells that may promote anaerobic glycolysis and extensive autophagy activity and contribute to their survival under oxygen and nutrient deprivation [169]. On the other hand, high level of HIF-1α has also been detected in melanoma cells expressing melanoma antigen recognized by T cells-1 MART-1+ found in perivascular regions within tumour as well as MART-1− non-haematopoietic melanoma- associated stromal cells, including CD146+ pericytes associated with CD31+ endothelial cells and Sca-1+ stromal cells in a mouse model of melanoma [182]. This suggests that stromal cells and melanoma cells, which can form functional vessel-like structures by vasculogenic mimicry, can cooperate for tumour vascularization supporting the interest to co-target these cells to counteract melanoma development.
Novel therapeutic strategies against aggressive and metastatic melanomas have also been investigated that consist to the molecular targeting of HIFs and/or their target gene products including proangiogenic factors such as VEGF, EMT programme- and altered metabolism-associated molecules in melanoma stem/progenitor cells and their progenies to counteract melanoma progression and metastases and reversing treatment resistance [23, 33, 172, 176, 179, 180, 183–188]. For instance, the ETBR blockage using a pharmacological antagonist, A-192621 resulted in a decrease in HIF-1α and HIF-2α stability concomitant with an increase in prolyl hydroxylase domain protein 2 level that was accompanied by an inhibition of tumour growth and angiogenesis of human M10 melanoma cell-derived xenografts in nude mice [176]. It has also been shown that the treatment of human A2058 melanoma cells with a small-molecule STAT3 inhibitor, CPA-7 was effective at inhibiting the expression of HIF-1α and VEGF in vitro and tumour growth and angiogenesis of human A2058 melanoma tumours in vivo [33].
Together these studies have indicated that the enhanced expression of HIFs and their target gene products and altered metabolism in melanoma cells during disease progression may promote their malignant reprogramming, including their acquisition of stem cell-like properties and more aggressive and metastatic phenotypes and angiogenic switch. The targeting of HIF signalling elements that are involved in the survival of melanoma-initiating cells under hypoxic and stressful conditions represents new promising strategies to prevent melanoma development and treatment resistance.
Functions of hypoxia and HIFs in the development of prostate cancer and metastases
Prostate cancer (PC) is among the most common malignancies in men [160, 189, 190]. Metastatic PCs still represent the second leading cause of cancer-related death [160, 189, 190]. Although important advances have led to an earlier diagnosis and effective therapeutic intervention by prostatectomy and/or radiation therapy for patients with localized PCs, the disease progression to locally invasive and metastatic castration-resistant prostate cancers (CRPCs) is generally associated with treatment resistance and disease relapse [160, 189, 190]. Moreover, current anti-hormonal treatments and first-line docetaxel-based chemotherapies against metastatic CRPCs are only palliative and culminate in the death of most patients after about 12–19 months [160, 189, 190]. Importantly, accumulating lines of experimental evidence have indicated that PC- and metastasis-initiating cells expressing stem cell-like markers such as CD133+, CD44high, ALDHhigh, ABCG2+ and/or CXCR4high and endowed with a high self-renewal ability can play critical functions for PC progression, metastases and resistance to current clinical therapies [45, 53, 95, 97, 191–194].
Recent studies have also revealed that an increase in expression levels and transcriptional activity of HIF-1α and HIF-2α frequently occur in PC cells during primary PC progression and bone metastases and is associated with treatment resistance and a poor outcome of patients [1, 4, 9, 13, 101, 195–200]. More specifically, the sustained activation of EGF and TGF-α/EGFR and TGF-β/TGF-βR cascades as well as the down-regulation or loss of PTEN and enhanced levels of inflammatory cytokines such as TNF-α during PC progression and after treatment initiation may result in the stimulation of PI3K/Akt/mTOR, NF-κB and/or MAPK signalling elements in PC cells [28, 34, 35, 42, 119, 201]. These tumourigenic pathways in turn may induce the expression, stabilization and nuclear translocation of HIF-1α and/or HIF-2α in PC cells under normoxic and hypoxic conditions and contribute to their gain of a more malignant behaviour [28, 34, 35, 42, 119, 201–203]. Moreover, it has been observed that the changes in the tumour microenvironment of PC cells, including the prevalence of hypoxic zones in primary PCs, and more particularly at the invasive front, may induce HIF-1α and HIF-2α and the reprogramming of PC cells to re-express high levels of some stemness gene products such as CD44, Oct-3/4 and Nanog (Figs 2 and 3) [4]. The maintenance of PC cell lines under hypoxic conditions has also been observed to result in their acquisition of more aggressive phenotypes and enrichment of hypoxic cancer cells with stem cell-like features and expressing high levels of drug resistance-associated molecules, such as multi-drug transporter, ABCG2 and anti-apoptotic factor, Bcl-xL [8, 14, 48, 57, 111, 204]. For instance, it has been observed that the culture of human androgen-independent (AI) and metastatic PC3 and DU145 prostatic cancer cells under low oxygen level (7% or 1% O2) was accompanied by up-regulation of HIF-1α and HIF-2α expression and enhanced colony formation efficacy of these hypoxic PC cells as compared with normoxic conditions (20% O2) [14]. Moreover, the number of SP cells and PC3 and DU145 cells expressing stem cell-like markers such as CD44high, ABCG2high, Oct-3/4 and Nanog and endowed with high prostasphere-forming ability detected in PC3 and DU145 cell lines was also increased under hypoxia [14]. On the other hand, the conditioned medium from PC-associated fibroblasts activated by TGF-β1 or IL-6 has also been observed to promote in a paracrine manner the induction of EMT programme in PC3 cells and their gain of stem cell-like features, including high prostasphere-forming capacity and migratory ability by inducing inflammatory factors such as cycloxygenase-2 (COX-2), NF-κB and HIF-1α [205, 206].
In addition, some studies have also indicated that the metastases of PC cells at distant sites, including bones, may occur early during disease progression, and the persistence of dormant PC cells homing at bones, may represent a determinant factor associated with the bone tumour formation and disease relapse after treatment initiation (Fig. 4) [53, 207–209]. Some similarities between the molecular mechanisms that govern the specific engraftment and homing of HSCs to bones are also observed for PC cells that preferentially migrate and adhere to bones. More specifically, the chemoattractant gradient formed by SDF-1 molecules released from BM-resident endothelial cells and stromal cells appears to provide critical functions for the specific dissemination, engraftment, migration through matrix and homing of CXCR4+ PC cells to BM as observed for LT-HSCs (Fig. 4) [53, 208, 210–214]. Moreover, it has been shown that metastatic PC cells homing at BM can compete with resident HSCs to occupy the most hypoxic endosteal niche formed by osteoblasts [208, 211]. In this regard, numerous growth factors and cytokines, including SDF-1, EGF, sonic hedgehog (SHH), TGF-β1, bone morphogenic proteins (BMPs) and MIC-1 released by metastatic PC cells, stromal fibroblasts, osteoblasts, osteoclasts and HSC/HPCs in BM microenvironment may contribute to the regulation of dormancy phenomenon of PC cells in hypoxic endosteal niche and promote their re-activation and formation of macrometastases and osteoblastic and/or osteolytic lesions under specific microenvironmental conditions [53, 194, 209, 215–217]. More particularly, it has been shown that BMP-7 secreted by BM-resident stromal cells may activate BMP receptor 2-induced p38/N-myc downstream-regulated gene 1 axis and cause a reversible senescence state in PC stem cell-like cells suggesting that BMP-7 can play a critical role in the regulation of their dormancy and hibernation at bones [216]. Moreover, it has also been observed that CXCR4 was highly up-regulated in both metastatic and AI PC3 and DU145 cells grown under prostasphere-forming conditions compared with monolayer growth conditions as well as in the CD133+/CD44+ PC stem/progenitor cell subpopulation from these PC cell lines relative to the CD133−/CD44− PC fraction [194]. The isolated CXCR4+ or CD133+/CD44+/CXCR4+ PC3 and DU145 stem/progenitor cell subpopulation also displayed higher prostasphere- and colony-forming abilities in vitro and tumourigenicity in vivo than CXCR4− or CD133−/CD44− PC cells [194]. It has also been observed that the stimulation of PC3 and DU145 cells with exogenous SDF-1 activated PI3K/Akt-induced inhibition of forkhead (FOXO3A) transcription factor pathway and led to an enrichment of CD133+/CD44+ PC cell number (Fig. 3) [194]. These data suggest that the stimulation of CD133+/CD44+/CXCR4+ PC stem/progenitor cells by SDF-1 can induce the PI3K/Akt cascade that in turn plays critical functions for their high self-renewal and skeletal metastases. Future investigations are, however, necessary to further establish the functions of the hypoxic microenvironment in the BM endosteal niche and HIFs in controlling the dormancy phenomenon, self-renewal, survival and formation of well-established metastases by metastasis-initiating PC cells as well as their interactive cross-talks with other growth factor pathways including SDF-1/CXCR4 axis and TGF-β family members.
Novel therapies by targeting HIFs and altered metabolic pathways in PC stem/progenitor cells and their differentiated progenies
Numerous studies have been carried out to establish the therapeutic benefit to down-regulate expression levels, stability and/or transcriptional activity of HIF-1α and/or HIF-2α by RNA interference or using pharmacological inhibitors of HIFs to eradicate PC cells [8, 54, 57–61, 202, 206, 218–222]. Among the pharmacological agents targeting HIF signalling network, there are specific inhibitors of HIFs (YC-1, P276-00, P3155, JG243, JG244 and NSC-134754), zinc, cyclin-dependent kinase inhibitor (P276-00), histone deacetylases (panobinostat) and mTOR complex 1 (everolimus) (Table 1) [8, 54, 57–61, 206, 218–222]. The results have indicated that the targeting of HIF pathway with these inhibitory agents induced the anti-proliferative, anti-invasive, anti-metastatic and/or apoptotic effects on PC cells under normoxic and hypoxic conditions and improved the cytotoxic and anti-angiogenic effects induced by irradiation and chemotherapy in vitro and in vivo [8, 54, 57–61, 202, 206, 218, 219, 221, 222]. For instance, it has been reported that the prostasphere-forming capacity of PC3 cells stimulated by the conditioned medium from activated fibroblasts as well as their tumour growth and metastatic spread in nude mice were significantly inhibited by shRNA targeting the proinflammatory signature including COX-2, NF-κB or HIF-1α [206]. New G-rich ODNs termed JG243 and JG244, which form an intramolecular parallel G-quartet structure, have also been observed to selectively interact with HIF-1α and HIF-2α proteins and induce their proteasomal degradation [54]. JG243 or JG244 mixed with a solution of polyethylenimine (PEI) was also effective at inhibiting the expression of HIF-regulated proteins such as VEGF, Bcl-2 and Bcl-xL and dramatically suppressing the growth of human PC3 tumour xenografts in nude mice [54]. Moreover, a combination of JG244/PEI plus a G-rich ODN directed against the phosphorylated STAT-3 protein termed T40214/PEI also inhibited the growth and induced the apoptotic effect on human DU145 prostate tumours and transgenic adenocarcinoma of mouse prostate (TRAMP)-C2 model in vivo as compared with drugs alone [218]. Interestingly, it has also been observed that the treatment of PC3 cells with anthracyclines, doxorubicin or daunorubicin was effective at suppressing the HIF-1α transcriptional activity and its target genes, GLUT-1 and VEGF [58]. Also, treatment of severe combined immunodeficient (SCID) mice bearing PC3 cell-derived tumour xenografts with doxorubicin or daunorubicin significantly reduced the tumour growth, recruitment of BM-derived cells and angiogenesis as compared with untreated mice [58]. Another study using doxorubicin encapsulated in pegylated liposomes has also indicated that this liposomal formulation Caelyx® was effective at improving the cytotoxic effects induced by radiation treatment on hypoxic tumours derived from androgen-sensitive CWR22 cells [201]. These data suggest that anthracyclines could be used, either alone or in combination therapy with current chemotherapeutic drug docetaxel, to inhibit the HIF-1α activity and induce the anti-angiogenic effects in hypoxic prostate tumours.
In considering the fact that the major cause of disease relapse of PC patients is caused by a rapid spread of PC cells to distant sites, including bones, and their homing under a dormant state, the targeting of metastasis-initiating PC cells is highly necessary to improve the efficacy of current cancer treatments and prevent severe and intractable pain associated with osteoblastic and osteolytic bone lesions (Fig. 4). Importantly, it has been observed that the enhanced expression of CXCR4 in PC cells, which may be induced under hypoxic conditions, was associated with a high risk of metastases at distant sites including bones and poor outcome of cancer patients [223]. Of therapeutic interest, it has also been reported that the targeting of CXCR4 using antagonist AMD3100 or anti-CXCR4 antibody was effective at decreasing the CD133+/CD44+ PC subpopulation, but did not significantly affect the CD133−/CD44− PC fraction within the total mass of PC3 or DU145 cells [194]. An opposed effect, however, was seen with docetaxel or 5-fluorouracil treatment which induced an enrichment of CD133+/CD44+ PC subpopulation [194]. Importantly, a combination of CXCR4 antagonist AMD3100 or Akt inhibitor NVP-BEZ235, which targets CD133+/CD44+/CXCR4+ DU145 stem/progenitor cells plus docetaxel was also more effective at inducing the tumour growth inhibitory effect on DU145 cell xenografts in non-obese diabetic (NOD)/SCID mice and preventing the tumour re-growth after treatment cessation as compared with individual drugs [194]. Moreover, the inhibition of SDF-1/CXCR-4 axis in metastatic PC3 cells using anti-CXCR4 monoclonal antibody (mAb) or CXCR4 antagonist, AMD3011 has been observed to impair their homing at the hypoxic endosteal niche in BM and inhibit bone tumour formation [208, 211, 224]. These results underline great interest to target CXCR4 and Akt in PC- and metastasis-initiating cells for improving current therapies and preventing disease relapse.
On the other hand, numerous studies have also revealed the possibility to inhibit lipogenesis, glycolysis and/or autophagy to restraint the energy supply required for a high proliferation rate and survival of metastatic and hypoxic PC cells including PC stem/progenitor cells [48, 95, 225–234]. Particularly, the data from global transcriptional profiling have revealed that the activity of monoacylglycerol lipase (MAGL), which plays a major role in lipogenesis in metastatic PC cells by converting monoglycerides to free fatty acids, was higher in AI and metastatic PC3 and DU145 cells relative to androgen-dependent LNCaP cells and associated with a gene signature that correlated with the EMT programme and stem cell-like properties of PC cells [234]. Also, the treatment of PC3 and DU145 cells with a selective inhibitor JZL184 of MAGL activity was effective at reducing their migration, invasion and survival in vitro and inhibiting the tumour growth of PC3 cell xenografts in SCID mice [234]. In addition, the results from a phase I trial have also indicated that the administration of a synthetic glucose analogue, 2-deoxy-D-glucose (2-DG) to PC patients had no major secondary effects and five of eight patients assessed with fluorodeoxyglucose (18F)-positron emission tomography (FDG-PET) scanning exhibited a decreased FDG uptake by day two of therapy [228]. It has however been noted that a treatment with 2-DG may be associated with enhanced autophagy in PC cells which may contribute to their 2-DG resistance [228]. Of therapeutic interest, the combination of 2-DG with an anti-diabetic compound including pioglitazone or metformin, which acts at least in part as an inhibitor of 2-DG-induced autophagy, has been observed to be more effective at inducing the apoptotic effects on metastatic LNCaP, PC3 and DU145 cells than drugs alone [229, 232].
Collectively, these recent studies have revealed that the adaptation of AI and metastatic PC stem/progenitor cells and their differentiated progenies to hypoxia and nutrient deprivation through the induction of HIFs, glycolytic pathways and autophagy may result in their enhanced expression of pluripotency-associated molecules and acquisition of a more aggressive behaviour during PC progression and bone metastases. Novel inhibitors of HIF-1α and/or HIF-2α and altered energy metabolism have been shown to be effective at inducing cytotoxic effects on hypoxic PC cells. Thus, these observations support therapeutic interest to further investigate these pharmacological agents for eradicating hypoxic PC- and metastasis-initiating cells endowed with stem cell-like properties and reversing the resistance to current anti-hormonal treatments, radiation therapy and docetaxel-based chemotherapies.
Functions of hypoxia and HIFs in the development of breast cancer and metastases
Breast cancer encompasses a heterogenous group of disease characterized by an accumulation of different genetic and epigenetic alterations occurring in the basal and/or luminal breast epithelial cells in the mammary gland [235, 236]. Although breast tumour resection may lead to a high survival rate for breast cancer patients diagnosed at early stages, locally advanced and highly invasive and metastatic breast cancer subtypes are generally refractory to current anti-hormonal treatments, targeted therapies against erbB2/HER2, irradiation and chemotherapies [160, 237, 238]. The heterogeneous nature of breast cancers may be due in part to the implication of different subpopulations of breast cancer stem cells (BCSCs) and their early progenitors that are responsible for tumour development and metastases at distant sites [73–80, 88, 239]. More specifically, highly tumourigenic BCSCs and their early progenitors endowed with a high self-renewal potential and which can express different stem cell-like markers such as CD44+, CD24−/low, epithelial-specific antigen (ESA+), CD133+, ALDH1high, Oct-3/4, Nanog, Kruppel-like factor (KLF-4) and/or CXCR4high have been detected and isolated from breast tumour specimens from patients and breast cancer cell lines [73–80, 88, 239]. Moreover, gene expression profiling and gene set enrichment analyses have revealed that CD44+/CD24−/low BCSC subpopulation showed increased expression of genes involved in TGF-β, TNF-α, interferon and NF-κB pathways that can contribute to the induction of the EMT programme in BCSCs and promote their mammosphere-forming ability and tumourigenicity [239–245]. Importantly, BCSCs expressing high levels of multi-drug transporters such as brain cancer resistance protein (BCRP)/ABCG2high, DNA repair enzymes and free radical scavengers and which can survive under oxygen and nutrient deprivation have been shown to be involved in the resistance to anti-hormonal and anti-angiogenic treatments, radiation and chemotherapies [45, 74, 79, 96, 241, 246–250].
Recent lines of experimental evidence have also indicated that enhanced expression levels of HIFs in BCSCs and their differentiated progenies in hypoxic intratumoral regions within poorly vascularized tumours and hypoxic BM microenvironment as well as the induction of the EMT programme may result in their acquisition of stem cell-like features, a high rate of glycolytic metabolism and more aggressive and invasive phenotypes as well as enhanced tumour angiogenesis during breast cancer progression [4, 15, 16, 50, 74, 75, 77, 79, 88, 251]. In support of this, a direct relationship between the co-expression of HIF-1α and the CD44+/CD24−/low phenotype has been observed by immunohistochemical analyses of 253 samples of breast ductal carcinoma from patients, and associated with a worse prognosis of breast cancer patients [50]. Moreover, it has been observed that the expression levels of Jagged2 and nuclear Notch intracellular domain were up-regulated in hypoxic regions at the invasive front of breast tumour tissues, and the enhanced expression of Jagged2 in breast cancer cells cultured under hypoxia led to the activation of Notch pathway and induction of the EMT programme [15]. An enhanced activity of HIF-1α under hypoxia has also been observed to result in the up-regulated expression of TGF-β superfamily member, Nodal through the activated Notch pathway in breast cancer cells that in turn contributed to their invasion and metastatic spread [16]. Importantly, CD44+/CD24−/low BCSCs expressing high levels of HIF-1α and mesenchymal markers such as N-cadherin and vimentin, but low level of E-cadherin, activated Wnt/β-catenin, and PI3K/Akt cascades also displayed higher clonogenic and mammosphere-forming abilities and tumourigenicity under normoxic and hypoxic conditions than their differentiated progenies [16, 74, 88]. Interestingly, an exposure of non-adherent human metastatic MDA-MB-231 and BCM2 breast cancer cells to three cycles of hypoxia and re-oxygenation has also been observed to be accompanied by an enrichment of the CD44+/CD24−/low/ESA+ BCSC fraction [79]. The CD44+/CD24−/low/ESA+ BCSC subpopulation from MDA-MB-231 and BCM2 cells also expressed the EMT markers such as vimentin and snail and decreased expression of E-cadherin and displayed higher mammosphere- forming capacity, tumourigenicity and metastatic potential to lungs as compared with parental breast cancer cell lines [79]. In addition, it has also been observed that activated breast cancer-associated stromal myofibroblasts may promote the mammosphere formation and tumourigenicity of breast cancer cells through the release of SDF-1 that in turn stimulates CD44+/CD24−/low BCSCs expressing their cognate receptor CXCR4 and angiogenesis [252].
Although the molecular mechanisms that control the high propensity of breast cancer cells to preferentially metastasize to specific tissues and organs, such as lungs and bones remain not precisely established, it has been shown that hypoxic breast cancer cells within primary and secondary breast tumours can play critical roles in the formation of pre-metastatic niches and metastases within the hypoxic bone microenvironment (Fig. 4) [15, 239, 253–256]. In this matter, an increased expression level of HIF-1α in primary breast tumour and metastases has been associated with enhanced rates of metastases at distant sites and decreased survival of breast cancer patients [1, 10]. More specifically, it has been shown that HIF-1α may induce an enhanced expression of lysyl oxidase (LOX), lysyl oxidase-like 2 (LOXL2) and LOXL4 in hypoxic breast cancer cells within primary breast tumour [125, 257]. LOX and LOXLs secreted from hypoxic breast cancer cells in turn can contribute to the formation of pre-metastatic niches at distant tissues such as lungs by inducing the remodelling of the extracellular matrix (ECM) through cross-link collagens and elastins and promoting the recruitment of CD11b+ bone marrow-derived cells (BMDCs) [125, 257]. Moreover, the enhanced expression of CXCR4 in breast cancer cells can also play critical roles for their preferential metastatic spread to distant sites, including bones and lungs, which secrete high levels of SDF-1 ligand molecules that act as a chemoattractant gradient (Fig. 4) [256].
In addition, it has also been shown that BCSCs can be involved in bone metastases within hypoxic bone microenvironment [15, 253–255]. Particularly, different growth factors and cytokines released by stromal cells and breast cancer cells, including SDF-1, TGF-β1 and BMPs as well as the up-regulation of HIF-1α, NF-κB, vascular cell adhesion molecule-1 (VCAM-1) and Notch in breast cancer cells typically control their dormancy, survival and self-renewal ability and formation of osteolytic bone metastasis [1, 15, 239, 251, 254, 258–261]. More specifically, a novel animal model of breast cancer metastasizing to bone has been investigated which consisted of injecting human CD44+/CD24−/low BCSCs subpopulation from MDA-MB-231 cells in mice previously implanted with human bone in the right or left dorsal flanks [253]. It has been observed that BCSCs displayed higher incidence of human bone metastasis relative to the parental breast cancer cell line, and metastatic bone tissues strongly stained for CD44, CXCR4 and osteopontin [253]. Moreover, it has also been noted that the enhanced activity of HIF-1α and TGF-β signalling elements promoted the EMT programme and up-regulated the expression levels of CXCR4 and VEGF in breast cancer cells, and thereby cooperated for their invasion, metastatic spread to bones and skeletal metastases [239]. In contrast, BMP-2/7 heterodimer, which acts as a powerful antagonist of TGF-β signalling pathway-induced EMT programme and invasiveness of breast cancer cells, strongly reduced the number of ALDHhigh/CD44high/CD24−/low BCSCs and bone metastases [262]. Furthermore, the co-culture of CD44+/CD24−/low/ESA+ BCSCs from MDA231BoM cell line endowed with a strong propensity to metastasize to bones with immortalized human BM stromal cells HS5 expressing Jagged2 under hypoxia also resulted in the activation of Notch pathway in BCSCs that promoted their self-renewal potential [15]. These data suggest that the interactions between stromal cells and BCSCs in hypoxic BM microenvironment can play important functions for the regulation of their dormant state, self-renewal ability, bone metastases and treatment resistance. Hence, this underlines great interest to target hypoxic BCSCs and their supporting host cells in the hypoxic endosteal niche of BM to prevent skeletal metastases and disease relapse.
Molecular targeting of HIFs and altered metabolic pathways in BCSCs and their differentiated progenies
In view of the fact that BCSCs appear to be principal cancer cells responsible for breast tumour development and metastases in the hypoxic bone microenvironment and are typically more resistant than their differentiated progenies to anti-hormonal and herceptin treatment, chemotherapy and radiotherapy, their molecular targeting is of major importance to prevent disease recurrence. In this regard, numerous studies have indicated that the targeting of HIF and altered metabolic pathways may eradicate hypoxic breast cancer- and bone metastasis-initiating cells, reduce tumour angiogenesis and improve the efficacy of current cancer therapies (Tables 1 and 2) [75, 78, 96, 115, 239, 247, 249, 257, 263–267]. For instance, it has been observed that the down-regulation of HIF-1α by shRNA or pharmacological inhibition with 2-methoxyestradiol inhibited the angiogenesis, reduced the tumour development in bone derived from MDA-MB-231 breast cancer cells intracardially injected in nude mice and increased the mouse survival [239]. Moreover, the systemic administration of a combination of specific inhibitors of HIF-1α and TGF-βRI signalling elements, 2-methoxyestradiol plus SD-208, respectively, that target breast tumour cells and bone microenvironment, was also more effective at decreasing bone metastases of MDA-MB-231 breast cancer cells and osteoclastic bone resorption and stimulating the formation of bone mass than individual drugs [239]. On the other hand, the targeting of CAIX, which is induced by HIF-1α in breast tumour cells under hypoxia and involved in the pHi regulation also constitutes a promising therapeutic strategy. It has been observed that inhibition of CAIX by shRNA or using pharmacological agents such as sulphonamide compounds (CAI17, ureido-sulphonamide, U-104) or glycosyl coumarins (GC-204 and GC-205) induced the apoptosis and reduced the primary tumour growth and lung metastases of hypoxic breast cancer cells [115]. Moreover, the inhibition of LOX, which is induced by HIF-1α in hypoxic breast cancer cells at primary tumours by shRNA, was also effective at preventing the CD11b+ BMDC recruitment, pre-metastatic niche formation and metastatic growth of MDA-MB-231 breast cancer cells at lungs in a mouse model [257].
Other therapeutic strategies to eradicate BCSCs and their progenies may also include the targeting of signalling elements such as hexokinase-2, AMP-activated protein kinase (AMPK), Akt/mTORC1 and/or fatty acid synthase (FASN) that are involved in the regulation of glycolysis, lipogenesis and/or autophagy induced under hypoxia and nutrient deprivation (Fig. 3 and Tables 1 and 2) [75, 78, 96, 247, 249, 263–269]. For instance, the treatment of orthotopic tumours established from hypoxic pre-conditioned MDA-MB-231 cells with EGFR-targeted nanoparticles (NPs) loaded with paclitaxel and lonidamine, which is an inhibitor of hexokinase-2 that catalyses the phosphorylation of glucose to yield glucose 6-phosphate during the glycolysis, has been observed to reduce the tumour growth relative to NPs loaded with single agent [75]. The anticarcinogenic effects of NPs were mediated in part through the down-regulation of the expression levels of HIF-1α, EGFR, P-glycoprotein (P-gp) and SCF [75]. Moreover, a potent and orally bioavailable AMPK activator designated as OSU-53 has also been observed to reduce the viability and clonogenic growth of triple-negative MDA-MB-231 and MDA-MB-468 breast cancer cells in vitro and in vivo through the inhibition of mTOR pathway, lipogenesis and HIF-1α-induced EMT programme [263]. It has however been noted that OSU-53 induced protective autophagy in breast cancer cells which could be attenuated by a co-treatment with an autophagy inhibitor, chloroquine that promoted the in vivo tumour-suppressive activity of OSU-53 [263]. Also, the inhibition of FASN activity, which is up-regulated in hypoxic regions of breast cancer tumours via the activation of Akt and HIF-1α-induced sterol regulatory element binding protein-1, using cerulenin or PI3K inhibitor LY294002, has also been observed to reverse the resistance of breast cancer cells to cyclophosphamide under hypoxic conditions [265]. In the same way, the CD44 knockdown using shRNA lentivirus particles in BCSCs also induced their differentiation and down-regulated the expression levels of FASN and different stem cell-like markers, oncogenes and anti-apoptotic factors such as lymphoid enhancer-binding factor-1 (LEF-1), Myc, EGFR, mucin-1 and Bcl-2 and thereby sensitized these immature cancer cells to the anti-tumoral effect induced by doxorubicin [249, 267]. Of particular interest, it has also been shown that anti-diabetic drug metformin inhibited different metabolic pathways, selectively eradicated BCSCs and acted in synergy with chemotherapeutic drugs such as doxorubicin and irradiation treatment to kill the total mass of breast cancer cells and thereby counteract tumour re-growth and disease recurrence [78, 96, 247, 250, 264, 269].
Altogether, these findings have indicated that the enhanced expression and activity of HIFs and altered metabolism in breast cancer cells can promote their malignant reprogramming and gain of stem cell-like features and thereby contribute to their high self-renewal ability, survival, tumourigenicity, invasiveness and treatment resistance under stressful conditions. Hence, novel multi-targeted therapies directed against HIFs and signalling elements involved in glycolysis, lipogenesis and autophagy, alone or in combination with current cancer therapies, constitute new promising approaches to eradicate total mass of breast cancer cells, including BCSCs, and thereby prevent their metastatic spread and disease relapse.
Functions of hypoxia and HIFs in the development of pancreatic cancer and metastases
Pancreatic ductal adenocarcinomas (PDACs) are extremely aggressive solid tumours, with a poor 5-year survival rate of less than 6% [160, 270, 271]. The late stage detection and surgical resection of primary pancreatic tumours result in the disease relapse in most cases [160, 270, 271]. Moreover, the radiation therapy and first-line gemcitabine-based chemotherapeutic treatments of patients with locally advanced and metastatic PDACs are only palliative and lead to a modest improvement in survival rates [160, 270, 271]. The inefficacy of current treatments and the poor outcome of PDAC patients are because of a rapid progression to metastatic disease states and the development of diverse mechanisms of resistance by pancreatic cancer cells to conventional therapies [271–276]. Particularly, it has been shown that pancreatic cancer stem/progenitor cells expressing stem cell-like markers such as CD133, CD44 and ABCG2 multi-drug transporter may be more resistant to oxygen and nutrient deprivation, irradiation and gemcitabine treatment than the bulk mass of differentiated pancreatic cancer cells [12, 51, 52, 63, 275].
Pancreatic ductal adenocarcinomas are among the most hypoxic of all solid tumours, and are typically characterized by a dense stromal fibrosis also known as desmoplasia and a poor tumour vascularization that may contribute to restraint procedures of drug delivery and promote altered metabolic pathways and treatment resistance [11, 12, 274, 277–279]. In this regard, HIF-1α is up-regulated in PDACs and can play critical roles for the adaptation of pancreatic cancer cells and stromal cells to the hypoxic desmoplastic microenvironment during disease progression, treatment resistance and a poor outcome for PDAC patients [1, 11, 25, 118, 279–282]. Specifically, a nuclear HIF-1α staining was seen in about 88% of pancreatic ductal adenocarcinoma specimens from patients and 43% adjacent stroma, but in only 16% of the normal pancreatic tissues [11]. Moreover, the co-expression of HIF-1α and other important oncogenic products and drug resistance-associated molecules such as K-Ras mutant, which is detected in up to 75–90% of PDAC cases, hedgehog signalling elements, CXCR4, toll-like receptor 4 (TLR4), NF-κB p65, survivin, proliferating cell nuclear antigen and VEGF has also been detected in PDAC tissue specimens from patients and pancreatic cancer cell lines [118, 280, 282–288]. The expression levels of sonic hedgehog (SHH) signalling elements, which play critical functions in the desmoplasic lesion formation were also induced in pancreatic cancer cells under hypoxic conditions, and the tumour and stromal HIF-1α staining positively correlated with SHH ligand expression in pancreatic cancer tumour samples [285]. On the other hand, it has also been shown that the activation of IGF-1/IGF-1R and SCF/KIT axes in pancreatic cancer cells may contribute to the induction of HIF-1α through the stimulation of PI3K/Akt and/or Ras/MEK/ERK pathways and tumour angiogenesis under normoxic conditions [25, 26].
In addition, the data from immunohistochemical analyses have indicated that the markers associated with hypoxia (CAIX), pancreatic cancer stem/progenitor cells (CD44 and CD24) and autophagy (beclin- 1 and microtubule-associated protein light chain 3 ‘LC3’) were co-expressed in PDAC tissue specimens from patients [51]. It has also been observed that the exposure of human MIA-PaCa-2 pancreatic cancer cells expressing high levels of CD44 and CD24 stem cell-like markers to hypoxia and nutrient starvation induced the EMT programme and the expression of HIF-1α and autophagy-related genes [51]. The hypoxia also enhanced the clonogenic capacity, survival, migration of MIA-PaCa-2 cells and formation of autophagic and acidic vesicles [51]. In contrast, BxPC-3 pancreatic cancer cells expressing low levels of stem cell-like markers did not survive under hypoxic and starvation conditions [51]. In the same way, the expression levels of CD133, CXCR4 and HIF-1α were also enhanced in the pancreatic cancer cell lines under hypoxia as compared with normoxic conditions and associated with an enhanced invasiveness of CD133+ pancreatic cancer cells [46, 51]. Importantly, the characterization of a series of early passage xenografts from 16 patients undergoing surgery for PDACs and orthotopically grown in nude mice has also revealed that the presence of hypoxic intratumoral regions was highly correlated with a rapid tumour growth and spontaneous metastasis formation [289]. Moreover, the analyses of the HIF-1α expression level in 48 pancreatic cancer tissues from patients who received adjuvant gemcitabine treatment after pancreatectomy have indicated that HIF-1α expression was associated with an enhanced neo-microvascularity in the hypoxic tumour environment and gemcitabine resistance [12]. It has also been noted that the patients with pancreatic tumours expressing a strong HIF-1α level had a shorter period until disease recurrence as compared with those with a weak HIF-1α expression underlining the importance of also targeting the HIF signalling network to kill hypoxic pancreatic cancer cells [12].
Novel therapies by targeting HIFs and altered metabolic pathways in pancreatic stem/progenitor cells and their differentiated progenies
New therapeutic strategies by targeting hypoxia and HIF-1α pathways using RNA interference or specific inhibitory agents in pancreatic cancer- and metastasis-initiating cells and their differentiated progenies for improving current therapies have recently been investigated under normoxic and hypoxic conditions (Tables 1 and 2) [11, 62–65, 290]. For instance, it has been observed that a hypoxia-activated pro-drug designated as TH-302, which selectively targets hypoxic regions of solid tumours in combination with conventional chemotherapeutic drugs such as gemcitabine-induced greater anti-tumoral effects on diverse human tumour xenograft models including pancreatic cancer xenografts than individual drugs without major toxicity [64, 291]. Moreover, it has been reported that a novel fusicoccin derivative (ISIR-042) was more effective at inducing the growth inhibitory and cytotoxic effects on hypoxic pancreatic cancer cells than on normoxic pancreatic cancer cells in vitro and in vivo through a reduction in HIF-1α and Akt activation [63]. Also, ISIR-042 preferentially induced the cytotoxic effects on gemcitabine-resistant CD24+/CD44+ pancreatic cancer stem/progenitor cells from pancreatic cancer cell lines [63]. In the same way, the inhibition of HIF-1α by a novel selective inhibitor PX-478 was also effective at potentiating the cytotoxic effects induced by fractioned radiation treatment, with or without combined treatment with gemcitabine, on in vitro and in vivo human PANC-1, CFPAC-1 or SU.86.86 pancreatic cancer models at least in part by reversing radiation resistance of these hypoxic tumour cells and inhibiting the pro-angiogenic effect of HIF-1α [11].
Other potential strategies for eradicating pancreatic cancer stem/progenitor cells and their progenies and reversing treatment resistance, may consist of targeting Ras mutant, EGFR, IGF-1R, PI3K/pAkt and EMT process-associated molecules, altered metabolic pathways and autophagy under normoxic or hypoxic conditions [29, 30, 51, 63, 284, 292–296]. For instance, it has been reported that the pharmacological inhibition of NF-κB activity, which is activated in response to the enhanced expression and activity of HIF-1α under hypoxia, was effective at attenuating the induction of the EMT programme and reversing highly invasive and drug-resistant phenotypes of pancreatic cancer cells [296]. It has also been noted that the sensitivity of PANC-1 cells to gemcitabine was reduced under hypoxic conditions and the targeting of PI3K/Akt pathway using LY294002 plus human checkpoint kinase 1 (Chk1) inhibitor designated as 7-hydroxystaurosporine (UCN-01) partially reversed the gemcitabine resistance [274]. Of particular interest, the functional inhibition of active Ras by S-trans, trans-farnesylthiosalicylic acid was also effective at reducing HIF-1α expression and promoting anti-proliferative and apoptotic effects induced by the glycolytic inhibitor 2-DG on pancreatic cancer cells both in vitro and in vivo [284]. Importantly, the inhibition of autophagy using 3-methyladenine or monensin also reduced the clonogenicity, spheroid formation, expression of stem cell-like markers and tumourigenicity of pancreatic cancer cells and induced the apoptotic effect on pancreatic cancer cells with stem cell-like properties under hypoxic and starvation conditions [51]. Moreover, the anti-diabetic metformin, alone or in combination with difluorinated curcumin analogue (CDF), was also effective at inhibiting the cell survival, clonogenicity and pancreatosphere-forming ability of pancreatic cancer cells [276]. Metformin, alone or combined with CDF, also promoted the pancreatosphere disintegration in both gemcitabine-sensitive and gemcitabine-resistant pancreatic cancer cells [276].
Altogether, these observations suggest that the up-regulation of HIF-1α activity, glycolytic metabolism and autophagy may represent important adaptive processes for the survival of pancreatic cancer stem/progenitor cells and their progenies under tumour microenvironmental conditions such as hypoxia and nutrient deficiency. Consequently, the co-targeting of HIF-1α and altered metabolic pathways in pancreatic cancer- and metastasis-initiating cells and their differentiated progenies represent potential therapeutic strategies to counteract rapid PDAC progression, metastatic spread at distant sites, treatment resistance and disease relapse of this very aggressive and lethal disease.
Conclusions and perspectives
Taken together, these recent investigations have revealed that the malignant reprogramming of cancer- and metastasis-initiating cells and their differentiated progenies may occur within hypoxic intratumoral regions at primary neoplasms and hypoxic niches at distant metastatic sites, including BM, and play critical roles for their acquisition of aggressive phenotypes and treatment resistance (Fig. 2). HIF-1α and HIF-2α appear to act as master regulators of adaptation of cancer stem/progenitor cells and their differentiated progenies to oxygen and nutrient deprivation by modulating their stem cell-like properties and metabolic and survival pathways and by activating tumour-associated stromal cells. Future investigations are, however, required to more precisely establish the molecular mechanisms at the basis of specific functions of HIF-1α and HIF-2α, common and unique gene patterns modulated through these transcription factors and their cooperative interactions with other growth factors in various human cancers during disease progression under normoxic and hypoxic conditions.
The results from some pre-clinical studies have also underlined great importance of targeting HIFs and altered energy metabolism in cancer- and metastasis-initiating cells and their progenies as well as their supporting host cells to overcome the treatment resistance and thereby prevent disease relapse and the death of cancer patients. Data from clinical trials have revealed that some anti-angiogenic drugs may reduce tumour tissue oxygenation and consequently promote the aggressive behaviour of cancer cells and treatment resistance. Therefore, the targeting of HIFs represents an attractive adjuvant cancer therapy to simultaneously eradicate cancer cells and induce anti-angiogenic effects in highly hypoxic tumours.
We can now envision the possibility of performing expression analyses of distinct molecular biomarkers associated with hypoxia and altered metabolic pathways in addition to the current diagnostic tests to select cancer patients who are likely to respond to cancer therapies targeting hypoxia including inhibitors of HIF signalling network, glycolysis, lipogenesis and autophagy. These multi-targeted approaches should be more effective, alone or in combination with current anti-hormonal treatments, radiotherapy and/or chemotherapy, against aggressive, metastatic and hypoxic tumours to eradicate total mass of cancer cells and cure cancer patients.
Acknowledgments
The authors of this work are supported, in part, by the National Institutes of Health [R01CA138791, TMEN U54 CA163120, SPORE P50 CA127297, EDRN UO1 CA111294] and Department of Defense (PC074289, BC074639).
Footnotes
This is an open access article under the terms of the Creative Commons Attribution License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
Conflicts of interest
The authors confirm that there are no conflicts of interest.
References
- 1.Zhong H, De Marzo AM, Laughner E, et al. Overexpression of hypoxia-inducible factor 1 alpha in common human cancers and their metastases. Cancer Res. 1999;59:5830–5. [PubMed] [Google Scholar]
- 2.Cangul H, Salnikow K, Yee HZ, et al. Enhanced overexpression of an HIF-1/hypoxia-related protein in cancer cells. Environ Health Perspect. 2002;110:783–8. doi: 10.1289/ehp.02110s5783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wenger RH. Cellular adaptation to hypoxia: O2-sensing protein hydroxylases, hypoxia-inducible transcription factors, and O2-regulated gene expression. FASEB J. 2002;16:1151–62. doi: 10.1096/fj.01-0944rev. [DOI] [PubMed] [Google Scholar]
- 4.Mathieu J, Zhang Z, Zhou W, et al. HIF induces human embryonic stem cell markers in cancer cells. Cancer Res. 2011;71:4640–52. doi: 10.1158/0008-5472.CAN-10-3320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jubb AM, Buffa FM, Harris AL. Assessment of tumour hypoxia for prediction of response to therapy and cancer prognosis. J Cell Mol Med. 2010;14:18–29. doi: 10.1111/j.1582-4934.2009.00944.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giuntoli S, Tanturli M, Di Gesualdo F, et al. Glucose availability in hypoxia regulates the selection of chronic myeloid leukemia progenitor subsets with different resistance to imatinib-mesylate. Haematologica. 2011;96:204–12. doi: 10.3324/haematol.2010.029082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blazek ER, Foutch JL, Maki G. Daoy medulloblastoma cells that express CD133 are radioresistant relative to CD133- cells, and the CD133+ sector is enlarged by hypoxia. Int J Radiat Oncol Biol Phys. 2007;67:1–5. doi: 10.1016/j.ijrobp.2006.09.037. [DOI] [PubMed] [Google Scholar]
- 8.Dai Y, Bae K, Siemann DW. Impact of hypoxia on the metastatic potential of human prostate cancer cells. Int J Radiat Oncol Biol Phys. 2011;81:521–8. doi: 10.1016/j.ijrobp.2011.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Milosevic M, Warde P, Menard C, et al. Tumor hypoxia predicts biochemical failure following radiotherapy for clinically localized prostate cancer. Clin Cancer Res. 2012;18:2108–14. doi: 10.1158/1078-0432.CCR-11-2711. [DOI] [PubMed] [Google Scholar]
- 10.Bos R, van der Groep P, Greijer AE, et al. Levels of hypoxia-inducible factor-1 alpha independently predict prognosis in patients with lymph node negative breast carcinoma. Cancer. 2003;97:1573–81. doi: 10.1002/cncr.11246. [DOI] [PubMed] [Google Scholar]
- 11.Schwartz DL, Bankson JA, Lemos R, Jr, et al. Radiosensitization and stromal imaging response correlates for the HIF-1 inhibitor PX-478 given with or without chemotherapy in pancreatic cancer. Mol Cancer Ther. 2010;9:2057–67. doi: 10.1158/1535-7163.MCT-09-0768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kasuya K, Tsuchida A, Nagakawa Y, et al. Hypoxia-inducible factor-1 alpha expression and gemcitabine chemotherapy for pancreatic cancer. Oncol Rep. 2011;26:1399–406. doi: 10.3892/or.2011.1457. [DOI] [PubMed] [Google Scholar]
- 13.Johansson A, Rudolfsson SH, Kilter S, et al. Targeting castration-induced tumour hypoxia enhances the acute effects of castration therapy in a rat prostate cancer model. BJU Int. 2011;107:1818–24. doi: 10.1111/j.1464-410X.2010.09690.x. [DOI] [PubMed] [Google Scholar]
- 14.Ma Y, Liang D, Liu J, et al. Prostate cancer cell lines under hypoxia exhibit greater stem-like properties. PLoS ONE. 2011;6:e29170. doi: 10.1371/journal.pone.0029170. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 15.Xing F, Okuda H, Watabe M, et al. Hypoxia-induced Jagged2 promotes breast cancer metastasis and self-renewal of cancer stem-like cells. Oncogene. 2011;30:4075–86. doi: 10.1038/onc.2011.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Quail DF, Taylor MJ, Walsh LA, et al. Low oxygen levels induce the expression of the embryonic morphogen Nodal. Mol Biol Cell. 2011;22:4809–21. doi: 10.1091/mbc.E11-03-0263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Semenza GL. Targeting HIF-1 for cancer therapy. Nat Rev Cancer. 2003;3:721–32. doi: 10.1038/nrc1187. [DOI] [PubMed] [Google Scholar]
- 18.Wiesener MS, Jurgensen JS, Rosenberger C, et al. Widespread hypoxia-inducible expression of HIF-2 alpha in distinct cell populations of different organs. FASEB J. 2003;17:271–3. doi: 10.1096/fj.02-0445fje. [DOI] [PubMed] [Google Scholar]
- 19.Kewley RJ, Whitelaw ML, Chapman-Smith A. The mammalian basic helix-loop-helix/PAS family of transcriptional regulators. Int J Biochem Cell Biol. 2004;36:189–204. doi: 10.1016/s1357-2725(03)00211-5. [DOI] [PubMed] [Google Scholar]
- 20.Partch CL, Gardner KH. Coactivator recruitment: a new role for PAS domains in transcriptional regulation by the bHLH-PAS family. J Cell Physiol. 2010;223:553–7. doi: 10.1002/jcp.22067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fong GH, Takeda K. Role and regulation of prolyl hydroxylase domain proteins. Cell Death Differ. 2008;15:635–41. doi: 10.1038/cdd.2008.10. [DOI] [PubMed] [Google Scholar]
- 22.Kaelin WG., Jr The von Hippel-Lindau tumor suppressor gene and kidney cancer. Clin Cancer Res. 2004;10:6290S–5S. doi: 10.1158/1078-0432.CCR-sup-040025. [DOI] [PubMed] [Google Scholar]
- 23.D’Alterio C, Barbieri A, Portella L, et al. Inhibition of stromal CXCR4 impairs development of lung metastases. Cancer Immunol Immunother. 2012;61:1713–20. doi: 10.1007/s00262-012-1223-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Partch CL, Gardner KH. Coactivators necessary for transcriptional output of the hypoxia inducible factor, HIF, are directly recruited by ARNT PAS-B. Proc Natl Acad Sci USA. 2011;108:7739–44. doi: 10.1073/pnas.1101357108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stoeltzing O, Liu W, Reinmuth N, et al. Regulation of hypoxia-inducible factor-1 alpha, vascular endothelial growth factor, and angiogenesis by an insulin-like growth factor-I receptor autocrine loop in human pancreatic cancer. Am J Pathol. 2003;163:1001–11. doi: 10.1016/s0002-9440(10)63460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhang M, Ma Q, Hu H, et al. Stem cell factor/c-kit signalling enhances invasion of pancreatic cancer cells via HIF-1 alpha under normoxic condition. Cancer Lett. 2011;303:108–17. doi: 10.1016/j.canlet.2011.01.017. [DOI] [PubMed] [Google Scholar]
- 27.Nilsson CL, Dillon R, Devakumar A, et al. Quantitative phosphoproteomic analysis of the STAT3/IL-6/HIF1alpha signalling network: an initial study in GSC11 glioblastoma stem cells. J Proteome Res. 2010;9:430–43. doi: 10.1021/pr9007927. [DOI] [PubMed] [Google Scholar]
- 28.Zhong H, Chiles K, Feldser D, et al. Modulation of hypoxia-inducible factor 1 alpha expression by the epidermal growth factor/phosphatidylinositol 3-kinase/PTEN/AKT/FRAP pathway in human prostate cancer cells: implications for tumor angiogenesis and therapeutics. Cancer Res. 2000;60:1541–5. [PubMed] [Google Scholar]
- 29.Tonra JR, Corcoran E, Deevi DS, et al. Prioritization of EGFR/IGF-IR/VEGFR2 combination targeted therapies utilizing cancer models. Anticancer Res. 2009;29:1999–2007. [PubMed] [Google Scholar]
- 30.Azzariti A, Porcelli L, Gatti G, et al. Synergic antiproliferative and antiangiogenic effects of EGFR and mTor inhibitors on pancreatic cancer cells. Biochem Pharmacol. 2008;75:1035–44. doi: 10.1016/j.bcp.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 31.Peng XH, Karna P, Cao Z, et al. Cross-talk between epidermal growth factor receptor and hypoxia-inducible factor-1alpha signal pathways increases resistance to apoptosis by up-regulating survivin gene expression. J Biol Chem. 2006;281:25903–14. doi: 10.1074/jbc.M603414200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Phillips RJ, Mestas J, Gharaee-Kermani M, et al. Epidermal growth factor and hypoxia-induced expression of CXC chemokine receptor 4 on non-small cell lung cancer cells is regulated by the phosphatidylinositol 3-kinase/PTEN/AKT/mammalian target of rapamycin signalling pathway and activation of hypoxia inducible factor-1 alpha. J Biol Chem. 2005;280:22473–81. doi: 10.1074/jbc.M500963200. [DOI] [PubMed] [Google Scholar]
- 33.Xu Q, Briggs J, Park S, et al. Targeting Stat3 blocks both HIF-1 and VEGF expression induced by multiple oncogenic growth signalling pathways. Oncogene. 2005;24:5552–60. doi: 10.1038/sj.onc.1208719. [DOI] [PubMed] [Google Scholar]
- 34.Schoolmeesters A, Brown DD, Fedorov Y. Kinome-wide functional genomics screen reveals a novel mechanism of TNF alpha-induced nuclear accumulation of the HIF-1 alpha transcription factor in cancer cells. PLoS ONE. 2012;7:e31270. doi: 10.1371/journal.pone.0031270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chae KS, Kang MJ, Lee JH, et al. Opposite functions of HIF-alpha isoforms in VEGF induction by TGF-beta1 under non-hypoxic conditions. Oncogene. 2011;30:1213–28. doi: 10.1038/onc.2010.498. [DOI] [PubMed] [Google Scholar]
- 36.Harada H, Itasaka S, Kizaka-Kondoh S, et al. The Akt/mTOR pathway assures the synthesis of HIF-1 alpha protein in a glucose- and reoxygenation-dependent manner in irradiated tumors. J Biol Chem. 2009;284:5332–42. doi: 10.1074/jbc.M806653200. [DOI] [PubMed] [Google Scholar]
- 37.Fukuda R, Kelly B, Semenza GL. Vascular endothelial growth factor gene expression in colon cancer cells exposed to prostaglandin E2 is mediated by hypoxia-inducible factor 1. Cancer Res. 2003;63:2330–4. [PubMed] [Google Scholar]
- 38.Laughner E, Taghavi P, Chiles K, et al. HER2 (neu) signalling increases the rate of hypoxia-inducible factor 1 alpha (HIF-1 alpha) synthesis: novel mechanism for HIF-1-mediated vascular endothelial growth factor expression. Mol Cell Biol. 2001;21:3995–4004. doi: 10.1128/MCB.21.12.3995-4004.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Qayum N, Muschel RJ, Im JH, et al. Tumor vascular changes mediated by inhibition of oncogenic signalling. Cancer Res. 2009;69:6347–54. doi: 10.1158/0008-5472.CAN-09-0657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fukuda R, Hirota K, Fan F, et al. Insulin-like growth factor 1 induces hypoxia-inducible factor 1-mediated vascular endothelial growth factor expression, which is dependent on MAP kinase and phosphatidylinositol 3-kinase signalling in colon cancer cells. J Biol Chem. 2002;277:38205–11. doi: 10.1074/jbc.M203781200. [DOI] [PubMed] [Google Scholar]
- 41.Zundel W, Schindler C, Haas-Kogan D, et al. Loss of PTEN facilitates HIF-1-mediated gene expression. Genes Dev. 2000;14:391–6. [PMC free article] [PubMed] [Google Scholar]
- 42.Hudson CC, Liu M, Chiang GG, et al. Regulation of hypoxia-inducible factor 1 alpha expression and function by the mammalian target of rapamycin. Mol Cell Biol. 2002;22:7004–14. doi: 10.1128/MCB.22.20.7004-7014.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hu HT, Ma QY, Zhang D, et al. HIF-1 alpha links beta-adrenoceptor agonists and pancreatic cancer cells under normoxic condition. Acta Pharmacol Sin. 2010;31:102–10. doi: 10.1038/aps.2009.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moeller BJ, Cao Y, Li CY, et al. Radiation activates HIF-1 to regulate vascular radio-sensitivity in tumors: role of reoxygenation, free radicals, and stress granules. Cancer Cell. 2004;5:429–41. doi: 10.1016/s1535-6108(04)00115-1. [DOI] [PubMed] [Google Scholar]
- 45.Mimeault M, Hauke R, Mehta PP, et al. Recent advances on cancer stem/progenitor cell research: therapeutic implications for overcoming resistance to the most aggressive cancers. J Cell Mol Med. 2007;11:981–1011. doi: 10.1111/j.1582-4934.2007.00088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hashimoto O, Shimizu K, Semba S, et al. Hypoxia induces tumor aggressiveness and the expansion of CD133-positive cells in a hypoxia-inducible factor-1 alpha-dependent manner in pancreatic cancer cells. Pathobiology. 2011;78:181–92. doi: 10.1159/000325538. [DOI] [PubMed] [Google Scholar]
- 47.Mimeault M, Batra SK. New advances on critical implications of tumor- and metastasis- initiating cells in cancer progression, treatment resistance and disease recurrence. Histol Histopathol. 2010;25:1057–73. doi: 10.14670/hh-25.1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Anderson KM, Guinan P, Rubenstein M. The effect of normoxia and hypoxia on a prostate (PC-3) CD44/CD41 cell side fraction. Anticancer Res. 2011;31:487–94. [PubMed] [Google Scholar]
- 49.Mimeault M, Batra SK. New promising drug targets in cancer- and metastasis-initiating cells. Drug Discov Today. 2010;15:354–64. doi: 10.1016/j.drudis.2010.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Oliveira-Costa JP, Zanetti JS, Silveira GG, et al. Differential expression of HIF-1 alpha in CD44+CD24−/low breast ductal carcinomas. Diagn Pathol. 2011;6:73. doi: 10.1186/1746-1596-6-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rausch V, Liu L, Apel A, et al. Autophagy mediates survival of pancreatic tumour-initiating cells in a hypoxic microenvironment. J Pathol. 2012;227:325–35. doi: 10.1002/path.3994. [DOI] [PubMed] [Google Scholar]
- 52.Mimeault M, Batra SK. Novel therapies against aggressive and recurrent epithelial cancers by molecular targeting tumor- and metastasis-initiating cells and their progenies. Anticancer Agents Med Chem. 2010;10:137–51. doi: 10.2174/187152010790909353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mimeault M, Johansson SL, Batra SK. Pathobiological implications of the expression of EGFR, pAkt, NF-kB and MIC-1 in prostate cancer stem cells and their progenies. PLoS ONE. 2012;7:e31919. doi: 10.1371/journal.pone.0031919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Guan Y, Reddy KR, Zhu Q, et al. G-rich oligonucleotides inhibit HIF-1 alpha and HIF-2 alpha and block tumor growth. Mol Ther. 2010;18:188–97. doi: 10.1038/mt.2009.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhang H, Li H, Xi HS, et al. HIF1 alpha is required for survival maintenance of chronic myeloid leukemia stem cells. Blood. 2012;119:2595–607. doi: 10.1182/blood-2011-10-387381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Takeuchi M, Ashihara E, Yamazaki Y, et al. Rakicidin A effectively induces apoptosis in hypoxia adapted Bcr-Abl positive leukemic cells. Cancer Sci. 2011;102:591–6. doi: 10.1111/j.1349-7006.2010.01813.x. [DOI] [PubMed] [Google Scholar]
- 57.Huang Y, Yu J, Yan C, et al. Effect of small interfering RNA targeting hypoxia-inducible factor-1 alpha on radiosensitivity of PC3 cell line. Urology. 2012;79:744.e17–24. doi: 10.1016/j.urology.2011.10.024. [DOI] [PubMed] [Google Scholar]
- 58.Lee K, Qian DZ, Rey S, et al. Anthracycline chemotherapy inhibits HIF-1 transcriptional activity and tumor-induced mobilization of circulating angiogenic cells. Proc Natl Acad Sci USA. 2009;106:2353–8. doi: 10.1073/pnas.0812801106. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 59.Manohar SM, Padgaonkar AA, Jalota-Badhwar A, et al. Cyclin-dependent kinase inhibitor, P276–00, inhibits HIF-1alpha and induces G2/M arrest under hypoxia in prostate cancer cells. Prostate Cancer Prostatic Dis. 2012;15:15–27. doi: 10.1038/pcan.2011.51. [DOI] [PubMed] [Google Scholar]
- 60.Baker LC, Boult JK, Walker-Samuel S, et al. The HIF-pathway inhibitor NSC-134754 induces metabolic changes and anti-tumour activity while maintaining vascular function. Br J Cancer. 2012;106:1638–47. doi: 10.1038/bjc.2012.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Manohar SM, Padgaonkar AA, Jalota-Badhwar A, et al. A novel inhibitor of hypoxia-inducible factor-1 alpha P3155 also modulates PI3K pathway and inhibits growth of prostate cancer cells. BMC Cancer. 2011;11:338. doi: 10.1186/1471-2407-11-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mizuno T, Nagao M, Yamada Y, et al. Small interfering RNA expression vector targeting hypoxia-inducible factor 1 alpha inhibits tumor growth in hepatobiliary and pancreatic cancers. Cancer Gene Ther. 2006;13:131–40. doi: 10.1038/sj.cgt.7700871. [DOI] [PubMed] [Google Scholar]
- 63.Kawakami K, Hattori M, Inoue T, et al. A novel fusicoccin derivative preferentially targets hypoxic tumor cells and inhibits tumor growth in xenografts. Anticancer Agents Med Chem. 2012;12:791–800. doi: 10.2174/187152012802650264. [DOI] [PubMed] [Google Scholar]
- 64.Liu Q, Sun JD, Wang J, et al. TH-302, a hypoxia-activated prodrug with broad in vivo preclinical combination therapy efficacy: optimization of dosing regimens and schedules. Cancer Chemother Pharmacol. 2012;69:1487–98. doi: 10.1007/s00280-012-1852-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Boreddy SR, Sahu RP, Srivastava SK. Benzyl isothiocyanate suppresses pancreatic tumor angiogenesis and invasion by inhibiting HIF-alpha/VEGF/Rho-GTPases: pivotal role of STAT-3. PLoS ONE. 2011;6:e25799. doi: 10.1371/journal.pone.0025799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Staab A, Fleischer M, Loeffler J, et al. Small interfering RNA targeting HIF-1 alpha reduces hypoxia-dependent transcription and radiosensitizes hypoxic HT 1080 human fibrosarcoma cells in vitro. Strahlenther Onkol. 2011;187:252–9. doi: 10.1007/s00066-011-2167-0. [DOI] [PubMed] [Google Scholar]
- 67.Mimeault M, Batra SK. Recent advances on skin-resident stem/progenitor cell functions in skin regeneration, aging and cancers and novel anti-aging and cancer therapies. J Cell Mol Med. 2010;14:116–34. doi: 10.1111/j.1582-4934.2009.00885.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jamieson CH, Ailles LE, Dylla SJ, et al. Granulocyte-macrophage progenitors as candidate leukemic stem cells in blast-crisis CML. N Engl J Med. 2004;351:657–67. doi: 10.1056/NEJMoa040258. [DOI] [PubMed] [Google Scholar]
- 69.Hu Y, Swerdlow S, Duffy TM, et al. Targeting multiple kinase pathways in leukemic progenitors and stem cells is essential for improved treatment of Ph+ leukemia in mice. Proc Natl Acad Sci USA. 2006;103:16870–5. doi: 10.1073/pnas.0606509103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Melo JV, Barnes DJ. Chronic myeloid leukaemia as a model of disease evolution in human cancer. Nat Rev Cancer. 2007;7:441–53. doi: 10.1038/nrc2147. [DOI] [PubMed] [Google Scholar]
- 71.Miyamoto T, Weissman IL, Akashi K. AML1/ETO-expressing nonleukemic stem cells in acute myelogenous leukemia with 8;21 chromosomal translocation. Proc Natl Acad Sci USA. 2000;97:7521–6. doi: 10.1073/pnas.97.13.7521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Colmone A, Amorim M, Pontier AL, et al. Leukemic cells create bone marrow niches that disrupt the behavior of normal hematopoietic progenitor cells. Science. 2008;322:1861–5. doi: 10.1126/science.1164390. [DOI] [PubMed] [Google Scholar]
- 73.Hwang-Verslues WW, Kuo WH, Chang PH, et al. Multiple lineages of human breast cancer stem/progenitor cells identified by profiling with stem cell markers. PLoS ONE. 2009;4:e8377. doi: 10.1371/journal.pone.0008377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Conley SJ, Gheordunescu E, Kakarala P, et al. Antiangiogenic agents increase breast cancer stem cells via the generation of tumor hypoxia. Proc Natl Acad Sci USA. 2012;109:2784–9. doi: 10.1073/pnas.1018866109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Milane L, Duan Z, Amiji M. Therapeutic efficacy and safety of paclitaxel/lonidamine loaded EGFR-targeted nanoparticles for the treatment of multi-drug resistant cancer. PLoS ONE. 2011;6:e24075. doi: 10.1371/journal.pone.0024075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Al-Hajj M, Wicha MS, Ito-Hernandez A, et al. Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci USA. 2003;100:3983–8. doi: 10.1073/pnas.0530291100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wang Z, Shi Q, Wang Z, et al. Clinicopathologic correlation of cancer stem cell markers CD44, CD24, VEGF and HIF-1 alpha in ductal carcinoma in situ and invasive ductal carcinoma of breast: an immunohistochemistry- based pilot study. Pathol Res Pract. 2011;207:505–13. doi: 10.1016/j.prp.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 78.Jung JW, Park SB, Lee SJ, et al. Metformin represses self-renewal of the human breast carcinoma stem cells via inhibition of estrogen receptor-mediated OCT4 expression. PLoS ONE. 2011;6:e28068. doi: 10.1371/journal.pone.0028068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Louie E, Nik S, Chen JS, et al. Identification of a stem-like cell population by exposing metastatic breast cancer cell lines to repetitive cycles of hypoxia and reoxygenation. Breast Cancer Res. 2010;12:R94. doi: 10.1186/bcr2773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Krohn A, Song YH, Muehlberg F, et al. CXCR4 receptor positive spheroid forming cells are responsible for tumor invasion in vitro. Cancer Lett. 2009;280:65–71. doi: 10.1016/j.canlet.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 81.Mimeault M, Johansson SL, Henichart JP, et al. Cytotoxic effects induced by docetaxel, gefitinib, and cyclopamine on side population and non-side population cell fractions from human invasive prostate cancer cells. Mol Cancer Ther. 2010;9:617–30. doi: 10.1158/1535-7163.MCT-09-1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mimeault M, Batra SK. Complex oncogenic signalling networks regulate brain tumor-initiating cells and their progenies: pivotal roles of wild-type EGFR, EGFRvIII mutant and hedgehog cascades and novel multitargeted therapies. Brain Pathol. 2011;21:479–500. doi: 10.1111/j.1750-3639.2011.00505.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mimeault M, Batra SK. Novel biomarkers and therapeutic targets for optimizing the therapeutic management of melanomas. World J Clin Oncol. 2012;3:32–42. doi: 10.5306/wjco.v3.i3.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Frankfurt O, Tallman MS. Growth factors in leukemia. J Natl Compr Canc Netw. 2007;5:203–15. doi: 10.6004/jnccn.2007.0020. [DOI] [PubMed] [Google Scholar]
- 85.Zhao C, Chen A, Jamieson CH, et al. Hedgehog signalling is essential for maintenance of cancer stem cells in myeloid leukaemia. Nature. 2009;458:776–9. doi: 10.1038/nature07737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Lessard J, Sauvageau G. Bmi-1 determines the proliferative capacity of normal and leukaemic stem cells. Nature. 2003;423:255–60. doi: 10.1038/nature01572. [DOI] [PubMed] [Google Scholar]
- 87.Mimeault M, Hauke R, Batra SK. Stem cells – A revolution in therapeutics–Recent advances on the stem cell biology and their therapeutic applications in regenerative medicine and cancer therapies. Clin Pharmacol Ther. 2007;82:252–64. doi: 10.1038/sj.clpt.6100301. [DOI] [PubMed] [Google Scholar]
- 88.Han M, Wang Y, Liu M, et al. MiR-21 regulates epithelial-mesenchymal transition phenotype and hypoxia-inducible factor-1 alpha expression in third-sphere forming breast cancer stem cell-like cells. Cancer Sci. 2012;103:1058–64. doi: 10.1111/j.1349-7006.2012.02281.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Barbieri A, Palma G, Rosati A, et al. Role of endothelial nitric oxide synthase (eNOS) in chronic stress-promoted tumour growth. J Cell Mol Med. 2012;16:920–6. doi: 10.1111/j.1582-4934.2011.01375.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Takeuchi M, Kimura S, Kuroda J, et al. Glyoxalase-I is a novel target against Bcr-Abl+ leukemic cells acquiring stem-like characteristics in a hypoxic environment. Cell Death Differ. 2010;17:1211–20. doi: 10.1038/cdd.2010.6. [DOI] [PubMed] [Google Scholar]
- 91.Druker BJ, Sawyers CL, Kantarjian H, et al. Activity of a specific inhibitor of the BCR-ABL tyrosine kinase in the blast crisis of chronic myeloid leukemia and acute lymphoblastic leukemia with the Philadelphia chromosome. N Engl J Med. 2001;344:1038–42. doi: 10.1056/NEJM200104053441402. [DOI] [PubMed] [Google Scholar]
- 92.Graham SM, Jorgensen HG, Allan E, et al. Primitive, quiescent, Philadelphia-positive stem cells from patients with chronic myeloid leukemia are insensitive to STI571 in vitro. Blood. 2002;99:319–25. doi: 10.1182/blood.v99.1.319. [DOI] [PubMed] [Google Scholar]
- 93.Hamilton A, Helgason GV, Schemionek M, et al. Chronic myeloid leukemia stem cells are not dependent on Bcr-Abl kinase activity for their survival. Blood. 2012;119:1501–10. doi: 10.1182/blood-2010-12-326843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tanturli M, Giuntoli S, Barbetti V, et al. Hypoxia selects bortezomib-resistant stem cells of chronic myeloid leukemia. PLoS ONE. 2011;6:e17008. doi: 10.1371/journal.pone.0017008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ibanez E, Agliano A, Prior C, et al. The quinoline imidoselenocarbamate EI201 blocks AKT/mTOR pathway and targets cancer stem cells leading to a strong antitumor activity. Curr Med Chem. 2012;19:3031–43. doi: 10.2174/092986712800672076. [DOI] [PubMed] [Google Scholar]
- 96.Vazquez-Martin A, Oliveras-Ferraros C, Del Barco S, et al. The anti-diabetic drug metformin suppresses self-renewal and proliferation of trastuzumab-resistant tumor-initiating breast cancer stem cells. Breast Cancer Res Treat. 2011;126:355–64. doi: 10.1007/s10549-010-0924-x. [DOI] [PubMed] [Google Scholar]
- 97.Mimeault M, Batra SK. Frequent deregulations in the hedgehog signalling network and cross-talks with the epidermal growth factor receptor pathway involved in cancer progression and targeted therapies. Pharmacol Rev. 2010;62:497–524. doi: 10.1124/pr.109.002329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Annabi B, Rojas-Sutterlin S, Laflamme C, et al. Tumor environment dictates medulloblastoma cancer stem cell expression and invasive phenotype. Mol Cancer Res. 2008;6:907–16. doi: 10.1158/1541-7786.MCR-07-2184. [DOI] [PubMed] [Google Scholar]
- 99.Yang MH, Wu MZ, Chiou SH, et al. Direct regulation of TWIST by HIF-1 alpha promotes metastasis. Nat Cell Biol. 2008;10:295–305. doi: 10.1038/ncb1691. [DOI] [PubMed] [Google Scholar]
- 100.Jing SW, Wang YD, Chen LQ, et al. Hypoxia suppresses E-cadherin and enhances matrix metalloproteinase-2 expression favoring esophageal carcinoma migration and invasion via hypoxia inducible factor-1 alpha activation. Dis Esophagus. 2012 doi: 10.1111/j.1442-2050.2011.01321.x. in press. [DOI] [PubMed] [Google Scholar]
- 101.Gravdal K, Halvorsen OJ, Haukaas SA, et al. Proliferation of immature tumor vessels is a novel marker of clinical progression in prostate cancer. Cancer Res. 2009;69:4708–15. doi: 10.1158/0008-5472.CAN-08-4417. [DOI] [PubMed] [Google Scholar]
- 102.Zhang L, Hill RP. Hypoxia enhances metastatic efficiency in HT1080 fibrosarcoma cells by increasing cell survival in lungs, not cell adhesion and invasion. Cancer Res. 2007;67:7789–97. doi: 10.1158/0008-5472.CAN-06-4221. [DOI] [PubMed] [Google Scholar]
- 103.Karlsson H, Fryknas M, Larsson R, et al. Loss of cancer drug activity in colon cancer HCT-116 cells during spheroid formation in a new 3-D spheroid cell culture system. Exp Cell Res. 2012;318:1577–85. doi: 10.1016/j.yexcr.2012.03.026. [DOI] [PubMed] [Google Scholar]
- 104.Saigusa S, Tanaka K, Toiyama Y, et al. Clinical significance of CD133 and hypoxia inducible factor-1 alpha gene expression in rectal cancer after preoperative chemoradiotherapy. Clin Oncol. 2011;23:323–32. doi: 10.1016/j.clon.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 105.Das B, Tsuchida R, Malkin D, et al. Hypoxia enhances tumor stemness by increasing the invasive and tumorigenic side population fraction. Stem Cells. 2008;26:1818–30. doi: 10.1634/stemcells.2007-0724. [DOI] [PubMed] [Google Scholar]
- 106.Holmquist-Mengelbier L, Fredlund E, Lofstedt T, et al. Recruitment of HIF-1 alpha and HIF-2 alpha to common target genes is differentially regulated in neuroblastoma: HIF-2 alpha promotes an aggressive phenotype. Cancer Cell. 2006;10:413–23. doi: 10.1016/j.ccr.2006.08.026. [DOI] [PubMed] [Google Scholar]
- 107.Chen B, Yuping S, Ni J. Rapamycin decreases survivin expression to induce NSCLC cell apoptosis under hypoxia through inhibiting HIF-1 alpha induction. Mol Biol Rep. 2012;39:185–91. doi: 10.1007/s11033-011-0724-3. [DOI] [PubMed] [Google Scholar]
- 108.Heddleston JM, Wu Q, Rivera M, et al. Hypoxia-induced mixed-lineage leukemia 1 regulates glioma stem cell tumorigenic potential. Cell Death Differ. 2012;19:428–39. doi: 10.1038/cdd.2011.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Krieg AJ, Rankin EB, Chan D, et al. Regulation of the histone demethylase JMJD1A by hypoxia-inducible factor 1 alpha enhances hypoxic gene expression and tumor growth. Mol Cell Biol. 2010;30:344–53. doi: 10.1128/MCB.00444-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Elvidge GP, Glenny L, Appelhoff RJ, et al. Concordant regulation of gene expression by hypoxia and 2-oxoglutarate-dependent dioxygenase inhibition: the role of HIF-1 alpha, HIF-2 alpha, and other pathways. J Biol Chem. 2006;281:15215–26. doi: 10.1074/jbc.M511408200. [DOI] [PubMed] [Google Scholar]
- 111.Chen N, Chen X, Huang R, et al. BCL-xL is a target gene regulated by hypoxia-inducible factor-1 alpha. J Biol Chem. 2009;284:10004–12. doi: 10.1074/jbc.M805997200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kumar SM, Liu S, Lu H, et al. Acquired cancer stem cell phenotypes through Oct4-mediated dedifferentiation. Oncogene. 2012;31:4898–911. doi: 10.1038/onc.2011.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Chiche J, Brahimi-Horn MC, Pouyssegur J. Tumour hypoxia induces a metabolic shift causing acidosis: a common feature in cancer. J Cell Mol Med. 2010;14:771–94. doi: 10.1111/j.1582-4934.2009.00994.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Svastova E, Witarski W, Csaderova L, et al. Carbonic anhydrase IX interacts with bicarbonate transporters in lamellipodia and increases cell migration via its catalytic domain. J Biol Chem. 2012;287:3392–402. doi: 10.1074/jbc.M111.286062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lou Y, McDonald PC, Oloumi A, et al. Targeting tumor hypoxia: suppression of breast tumor growth and metastasis by novel carbonic anhydrase IX inhibitors. Cancer Res. 2011;71:3364–76. doi: 10.1158/0008-5472.CAN-10-4261. [DOI] [PubMed] [Google Scholar]
- 116.Ullah MS, Davies AJ, Halestrap AP. The plasma membrane lactate transporter MCT4, but not MCT1, is up-regulated by hypoxia through a HIF-1 alpha-dependent mechanism. J Biol Chem. 2006;281:9030–7. doi: 10.1074/jbc.M511397200. [DOI] [PubMed] [Google Scholar]
- 117.Shinojima T, Oya M, Takayanagi A, et al. Renal cancer cells lacking hypoxia inducible factor (HIF)-1 alpha expression maintain vascular endothelial growth factor expression through HIF-2 alpha. Carcinogenesis. 2007;28:529–36. doi: 10.1093/carcin/bgl143. [DOI] [PubMed] [Google Scholar]
- 118.Shibaji T, Nagao M, Ikeda N, et al. Prognostic significance of HIF-1 alpha overexpression in human pancreatic cancer. Anticancer Res. 2003;23:4721–7. [PubMed] [Google Scholar]
- 119.Fang J, Ding M, Yang L, et al. PI3K/PTEN/AKT signalling regulates prostate tumor angiogenesis. Cell Signal. 2007;19:2487–97. doi: 10.1016/j.cellsig.2007.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Gordan JD, Bertout JA, Hu CJ, et al. HIF-2 alpha promotes hypoxic cell proliferation by enhancing c-myc transcriptional activity. Cancer Cell. 2007;11:335–47. doi: 10.1016/j.ccr.2007.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Covello KL, Kehler J, Yu H, et al. HIF-2 alpha regulates Oct-4: effects of hypoxia on stem cell function, embryonic development, and tumor growth. Genes Dev. 2006;20:557–70. doi: 10.1101/gad.1399906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Carrero P, Okamoto K, Coumailleau P, et al. Redox-regulated recruitment of the transcriptional coactivators CREB-binding protein and SRC-1 to hypoxia-inducible factor 1 alpha. Mol Cell Biol. 2000;20:402–15. doi: 10.1128/mcb.20.1.402-415.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ruas JL, Berchner-Pfannschmidt U, Malik S, et al. Complex regulation of the transactivation function of hypoxia-inducible factor- 1 alpha by direct interaction with two distinct domains of the CREB-binding protein/p300. J Biol Chem. 2010;285:2601–9. doi: 10.1074/jbc.M109.021824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hasmim M, Noman MZ, Lauriol J, et al. Hypoxia-dependent inhibition of tumor cell susceptibility to CTL-mediated lysis involves NANOG induction in target cells. J Immunol. 2011;187:4031–9. doi: 10.4049/jimmunol.1101011. [DOI] [PubMed] [Google Scholar]
- 125.Wong CC, Gilkes DM, Zhang H, et al. Hypoxia-inducible factor 1 is a master regulator of breast cancer metastatic niche formation. Proc Natl Acad Sci USA. 2011;108:16369–74. doi: 10.1073/pnas.1113483108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Heddleston JM, Li Z, McLendon RE, et al. The hypoxic microenvironment maintains glioblastoma stem cells and promotes reprogramming towards a cancer stem cell phenotype. Cell Cycle. 2009;8:3274–84. doi: 10.4161/cc.8.20.9701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Li Z, Bao S, Wu Q, et al. Hypoxia-inducible factors regulate tumorigenic capacity of glioma stem cells. Cancer Cell. 2009;15:501–13. doi: 10.1016/j.ccr.2009.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Gibbs BF, Yasinska IM, Oniku AE, et al. Effects of stem cell factor on hypoxia-inducible factor 1 alpha accumulation in human acute myeloid leukaemia and LAD2 mast cells. PLoS ONE. 2011;6:e22502. doi: 10.1371/journal.pone.0022502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Rizo A, Vellenga E, de Haan G, et al. Signalling pathways in self-renewing hematopoietic and leukemic stem cells: do all stem cells need a niche? Hum Mol Genet. 2006;15:R210–9. doi: 10.1093/hmg/ddl175. [DOI] [PubMed] [Google Scholar]
- 130.Nagao R, Ashihara E, Kimura S, et al. Growth inhibition of imatinib-resistant CML cells with the T315I mutation and hypoxia-adaptation by AV65–a novel Wnt/beta-catenin signalling inhibitor. Cancer Lett. 2011;312:91–100. doi: 10.1016/j.canlet.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 131.Sengupta A, Banerjee D, Chandra S, et al. B Deregulation and cross talk among Sonic hedgehog, Wnt, Hox and Notch signalling in chronic myeloid leukemia progression. Leukemia. 2007;21:949–55. doi: 10.1038/sj.leu.2404657. [DOI] [PubMed] [Google Scholar]
- 132.Talpaz M, Shah NP, Kantarjian H, et al. Dasatinib in imatinib-resistant Philadelphia chromosome-positive leukemias. N Engl J Med. 2006;354:2531–41. doi: 10.1056/NEJMoa055229. [DOI] [PubMed] [Google Scholar]
- 133.Giuffrida D, Rogers IM. Targeting cancer stem cell lines as a new treatment of human cancer. Recent Pat Anticancer Drug Discov. 2010;5:205–18. doi: 10.2174/157489210791760535. [DOI] [PubMed] [Google Scholar]
- 134.Wang Y, Liu Y, Malek SN, et al. Targeting HIF1 alpha eliminates cancer stem cells in hematological malignancies. Cell Stem Cell. 2011;8:399–411. doi: 10.1016/j.stem.2011.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Calabretta B, Salomoni P. Suppression of autophagy by BCR/ABL. Front Biosci. 2012;4:453–60. doi: 10.2741/278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Stupp R, Mason WP, van den Bent MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 2005;352:987–96. doi: 10.1056/NEJMoa043330. [DOI] [PubMed] [Google Scholar]
- 137.Furnari FB, Fenton T, Bachoo RM, et al. Malignant astrocytic glioma: genetics, biology, and paths to treatment. Genes Dev. 2007;21:2683–710. doi: 10.1101/gad.1596707. [DOI] [PubMed] [Google Scholar]
- 138.Karpel-Massler G, Schmidt U, Unterberg A, et al. Therapeutic inhibition of the epidermal growth factor receptor in high-grade gliomas: where do we stand? Mol Cancer Res. 2009;7:1000–12. doi: 10.1158/1541-7786.MCR-08-0479. [DOI] [PubMed] [Google Scholar]
- 139.Bao S, Wu Q, McLendon RE, et al. Glioma stem cells promote radioresistance by preferential activation of the DNA damage response. Nature. 2006;444:756–60. doi: 10.1038/nature05236. [DOI] [PubMed] [Google Scholar]
- 140.Eramo A, Ricci-Vitiani L, Zeuner A, et al. Chemotherapy resistance of glioblastoma stem cells. Cell Death Differ. 2006;13:1238–41. doi: 10.1038/sj.cdd.4401872. [DOI] [PubMed] [Google Scholar]
- 141.Calabrese C, Poppleton H, Kocak M, et al. A perivascular niche for brain tumor stem cells. Cancer Cell. 2007;11:69–82. doi: 10.1016/j.ccr.2006.11.020. [DOI] [PubMed] [Google Scholar]
- 142.Li A, Walling J, Ahn S, et al. Unsupervised analysis of transcriptomic profiles reveals six glioma subtypes. Cancer Res. 2009;69:2091–9. doi: 10.1158/0008-5472.CAN-08-2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Verhaak RG, Hoadley KA, Purdom E, et al. Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell. 2010;17:98–110. doi: 10.1016/j.ccr.2009.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Brennan C, Momota H, Hambardzumyan D, et al. Glioblastoma subclasses can be defined by activity among signal transduction pathways and associated genomic alterations. PLoS ONE. 2009;4:e7752. doi: 10.1371/journal.pone.0007752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Platet N, Liu SY, Atifi ME, et al. Influence of oxygen tension on CD133 phenotype in human glioma cell cultures. Cancer Lett. 2007;258:286–90. doi: 10.1016/j.canlet.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 146.Hjelmeland AB, Wu Q, Heddleston JM, et al. Acidic stress promotes a glioma stem cell phenotype. Cell Death Differ. 2011;18:829–40. doi: 10.1038/cdd.2010.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Seidel S, Garvalov BK, Wirta V, et al. A hypoxic niche regulates glioblastoma stem cells through hypoxia inducible factor 2 alpha. Brain. 2010;133:983–95. doi: 10.1093/brain/awq042. [DOI] [PubMed] [Google Scholar]
- 148.Soeda A, Park M, Lee D, et al. Hypoxia promotes expansion of the CD133-positive glioma stem cells through activation of HIF-1 alpha. Oncogene. 2009;28:3949–59. doi: 10.1038/onc.2009.252. [DOI] [PubMed] [Google Scholar]
- 149.Bao S, Wu Q, Sathornsumetee S, et al. Stem cell-like glioma cells promote tumor angiogenesis through vascular endothelial growth factor. Cancer Res. 2006;66:7843–8. doi: 10.1158/0008-5472.CAN-06-1010. [DOI] [PubMed] [Google Scholar]
- 150.Wang J, Wang H, Li Z, et al. c-Myc is required for maintenance of glioma cancer stem cells. PLoS ONE. 2008;3:e3769. doi: 10.1371/journal.pone.0003769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Bao S, Wu Q, Li Z, et al. Targeting cancer stem cells through L1CAM suppresses glioma growth. Cancer Res. 2008;68:6043–8. doi: 10.1158/0008-5472.CAN-08-1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Andersson U, Schwartzbaum J, Wiklund F, et al. A comprehensive study of the association between the EGFR and ERBB2 genes and glioma risk. Acta Oncol. 2010;49:767–75. doi: 10.3109/0284186X.2010.480980. [DOI] [PubMed] [Google Scholar]
- 153.Cloughesy TF, Yoshimoto K, Nghiemphu P, et al. Antitumor activity of rapamycin in a Phase I trial for patients with recurrent PTEN-deficient glioblastoma. PLoS Med. 2008;5:e8. doi: 10.1371/journal.pmed.0050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Galavotti S, Bartesaghi S, Faccenda D, et al. The autophagy-associated factors DRAM1 and p62 regulate cell migration and invasion in glioblastoma stem cells. Oncogene. 2012 doi: 10.1038/onc.2012.111. in press. [DOI] [PubMed] [Google Scholar]
- 155.Yin S, Kaluz S, Devi NS, et al. Arylsulfonamide KCN1 inhibits in vivo glioma growth and interferes with HIF signalling by disrupting HIF-1 alpha interaction with co-factors p300/CBP. Clin Cancer Res. 2012 doi: 10.1158/1078-0432.CCR-12-0861. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Sotelo J, Briceno E, Lopez-Gonzalez MA, et al. Adding chloroquine to conventional treatment for glioblastoma multiforme: a randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2006;144:337–43. doi: 10.7326/0003-4819-144-5-200603070-00008. [DOI] [PubMed] [Google Scholar]
- 157.Tsao H, Atkins MB, Sober AJ, et al. Management of cutaneous melanoma. N Engl J Med. 2004;351:998–1012. doi: 10.1056/NEJMra041245. [DOI] [PubMed] [Google Scholar]
- 158.Gray-Schopfer V, Wellbrock C, Marais R. Melanoma biology and new targeted therapy. Nature. 2007;445:851–7. doi: 10.1038/nature05661. [DOI] [PubMed] [Google Scholar]
- 159.Garbe C, Leiter U. Melanoma epidemiology and trends. Clin Dermatol. 2009;27:3–9. doi: 10.1016/j.clindermatol.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 160.Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 161.Fang D, Nguyen TK, Leishear K, et al. A tumorigenic subpopulation with stem cell properties in melanomas. Cancer Res. 2005;65:9328–37. doi: 10.1158/0008-5472.CAN-05-1343. [DOI] [PubMed] [Google Scholar]
- 162.Monzani E, Facchetti F, Galmozzi E, et al. Melanoma contains CD133 and ABCG2 positive cells with enhanced tumourigenic potential. Eur J Cancer. 2007;43:935–46. doi: 10.1016/j.ejca.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 163.Schatton T, Murphy GF, Frank NY, et al. Identification of cells initiating human melanomas. Nature. 2008;451:345–9. doi: 10.1038/nature06489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Boiko AD, Razorenova OV, van de Rijn M, et al. Human melanoma-initiating cells express neural crest nerve growth factor receptor CD271. Nature. 2010;466:133–7. doi: 10.1038/nature09161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Strizzi L, Abbott DE, Salomon DS, et al. Potential for cripto-1 in defining stem cell-like characteristics in human malignant melanoma. Cell Cycle. 2008;7:1931–5. doi: 10.4161/cc.7.13.6236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Giatromanolaki A, Sivridis E, Kouskoukis C, et al. Hypoxia-inducible factors 1 alpha and 2 alpha are related to vascular endothelial growth factor expression and a poorer prognosis in nodular malignant melanomas of the skin. Melanoma Res. 2003;13:493–501. doi: 10.1097/00008390-200310000-00008. [DOI] [PubMed] [Google Scholar]
- 167.Valencak J, Kittler H, Schmid K, et al. Prognostic relevance of hypoxia inducible factor-1 alpha expression in patients with melanoma. Clin Exp Dermatol. 2009;34:e962–4. doi: 10.1111/j.1365-2230.2009.03706.x. [DOI] [PubMed] [Google Scholar]
- 168.Konstantina A, Lazaris AC, Ioannidis E, et al. Immunohistochemical expression of VEGF, HIF1-a, and PlGF in malignant melanomas and dysplastic nevi. Melanoma Res. 2011;21:389–94. doi: 10.1097/CMR.0b013e328347ee33. [DOI] [PubMed] [Google Scholar]
- 169.Sivridis E, Koukourakis MI, Mendrinos SE, et al. Beclin-1 and LC3A expression in cutaneous malignant melanomas: a biphasic survival pattern for beclin-1. Melanoma Res. 2011;21:188–95. doi: 10.1097/CMR.0b013e328346612c. [DOI] [PubMed] [Google Scholar]
- 170.Strizzi L, Bianco C, Normanno N, et al. Cripto-1: a multifunctional modulator during embryogenesis and oncogenesis. Oncogene. 2005;24:5731–41. doi: 10.1038/sj.onc.1208918. [DOI] [PubMed] [Google Scholar]
- 171.Rofstad EK, Danielsen T. Hypoxia-induced metastasis of human melanoma cells: involvement of vascular endothelial growth factor-mediated angiogenesis. Br J Cancer. 1999;80:1697–707. doi: 10.1038/sj.bjc.6690586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Braig S, Wallner S, Junglas B, et al. CTGF is overexpressed in malignant melanoma and promotes cell invasion and migration. Br J Cancer. 2011;105:231–8. doi: 10.1038/bjc.2011.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Omholt K, Platz A, Kanter L, et al. NRAS and BRAF mutations arise early during melanoma pathogenesis and are preserved throughout tumor progression. Clin Cancer Res. 2003;9:6483–8. [PubMed] [Google Scholar]
- 174.Bertolotto C, Lesueur F, Giuliano S, et al. A SUMOylation-defective MITF germline mutation predisposes to melanoma and renal carcinoma. Nature. 2011;480:94–8. doi: 10.1038/nature10539. [DOI] [PubMed] [Google Scholar]
- 175.Busca R, Berra E, Gaggioli C, et al. Hypoxia-inducible factor 1{alpha} is a new target of microphthalmia-associated transcription factor (MITF) in melanoma cells. J Cell Biol. 2005;170:49–59. doi: 10.1083/jcb.200501067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Spinella F, Rosano L, Del Duca M, et al. Endothelin-1 inhibits prolyl hydroxylase domain 2 to activate hypoxia-inducible factor- 1 alpha in melanoma cells. PLoS ONE. 2010;5:e11241. doi: 10.1371/journal.pone.0011241. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 177.Kumar SM, Yu H, Edwards R, et al. Mutant V600E BRAF increases hypoxia inducible factor-1 alpha expression in melanoma. Cancer Res. 2007;67:3177–84. doi: 10.1158/0008-5472.CAN-06-3312. [DOI] [PubMed] [Google Scholar]
- 178.Mills CN, Joshi SS, Niles RM. Expression and function of hypoxia inducible factor-1 alpha in human melanoma under non-hypoxic conditions. Mol Cancer. 2009;8:104. doi: 10.1186/1476-4598-8-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Comito G, Calvani M, Giannoni E, et al. HIF-1alpha stabilization by mitochondrial ROS promotes Met-dependent invasive growth and vasculogenic mimicry in melanoma cells. Free Radic Biol Med. 2011;51:893–904. doi: 10.1016/j.freeradbiomed.2011.05.042. [DOI] [PubMed] [Google Scholar]
- 180.Kuphal S, Winklmeier A, Warnecke C, et al. Constitutive HIF-1 activity in malignant melanoma. Eur J Cancer. 2010;46:1159–69. doi: 10.1016/j.ejca.2010.01.031. [DOI] [PubMed] [Google Scholar]
- 181.Chun YS, Lee KH, Choi E, et al. Phorbol ester stimulates the nonhypoxic induction of a novel hypoxia-inducible factor 1 alpha isoform: implications for tumor promotion. Cancer Res. 2003;63:8700–7. [PubMed] [Google Scholar]
- 182.Trevino-Villarreal JH, Cotanche DA, Sepulveda R, et al. Host-derived pericytes and Sca-1+ cells predominate in the MART-1- stroma fraction of experimentally induced melanoma. J Histochem Cytochem. 2011;59:1060–75. doi: 10.1369/0022155411428078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Frank NY, Schatton T, Kim S, et al. VEG-FR-1 expressed by malignant melanoma-initiating cells is required for tumor growth. Cancer Res. 2011;71:1474–85. doi: 10.1158/0008-5472.CAN-10-1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Levy C, Khaled M, Fisher DE. MITF: master regulator of melanocyte development and melanoma oncogene. Trends Mol Med. 2006;12:406–14. doi: 10.1016/j.molmed.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 185.Hamsa TP, Kuttan G. Antiangiogenic activity of berberine is mediated through the downregulation of hypoxia-inducible factor- 1, VEGF, and proinflammatory mediators. Drug Chem Toxicol. 2012;35:57–70. doi: 10.3109/01480545.2011.589437. [DOI] [PubMed] [Google Scholar]
- 186.Trapp V, Parmakhtiar B, Papazian V, et al. Anti-angiogenic effects of resveratrol mediated by decreased VEGF and increased TSP1 expression in melanoma-endothelial cell co-culture. Angiogenesis. 2010;13:305–15. doi: 10.1007/s10456-010-9187-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Yang XC, Tu CX, Luo PH, et al. Antimetastatic activity of MONCPT in preclinical melanoma mice model. Invest New Drugs. 2010;28:800–11. doi: 10.1007/s10637-009-9323-8. [DOI] [PubMed] [Google Scholar]
- 188.Franco R, Cantile M, Scala S, et al. Histomorphologic parameters and CXCR4 mRNA and protein expression in sentinel node melanoma metastasis are correlated to clinical outcome. Cancer Biol Ther. 2010;9:423–9. doi: 10.4161/cbt.9.6.10996. [DOI] [PubMed] [Google Scholar]
- 189.Petrylak DP, Tangen CM, Hussain MH, et al. Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med. 2004;351:1513–20. doi: 10.1056/NEJMoa041318. [DOI] [PubMed] [Google Scholar]
- 190.Tannock IF, de Wit R, Berry WR, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004;351:1502–12. doi: 10.1056/NEJMoa040720. [DOI] [PubMed] [Google Scholar]
- 191.Mimeault M, Batra SK. Animal models of prostate carcinogenesis underlining the critical implication of prostatic stem progenitor cells. Biochim Biophys Acta. 2011;1816:25–37. doi: 10.1016/j.bbcan.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Tu SM, Lin SH. Prostate cancer stem cells. Clin Genitourin Cancer. 2012;10:69–76. doi: 10.1016/j.clgc.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Jeter CR, Liu B, Liu X, et al. NANOG promotes cancer stem cell characteristics and prostate cancer resistance to androgen deprivation. Oncogene. 2011;30:3833–45. doi: 10.1038/onc.2011.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Dubrovska A, Elliott J, Salamone RJ, et al. CXCR4 expression in prostate cancer progenitor cells. PLoS ONE. 2012;7:e31226. doi: 10.1371/journal.pone.0031226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Nanni S, Benvenuti V, Grasselli A, et al. Endothelial NOS, estrogen receptor beta, and HIFs cooperate in the activation of a prognostic transcriptional pattern in aggressive human prostate cancer. J Clin Invest. 2009;119:1093–108. doi: 10.1172/JCI35079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Shaida N, Chan P, Turley H, et al. Nuclear localization of factor inhibitor hypoxia-inducible factor in prostate cancer is associated with poor prognosis. J Urol. 2011;185:1513–8. doi: 10.1016/j.juro.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 197.Al-Ubaidi FL, Schultz N, Egevad L, et al. Castration therapy of prostate cancer results in downregulation of HIF-1 alpha levels. Int J Radiat Oncol Biol Phys. 2012;82:1243–8. doi: 10.1016/j.ijrobp.2011.10.038. [DOI] [PubMed] [Google Scholar]
- 198.Hennessey D, Martin LM, Atzberger A, et al. Exposure to hypoxia following irradiation increases radioresistance in prostate cancer cells. Urol Oncol. 2011 doi: 10.1016/j.urolonc.2011.10.008. in press. [DOI] [PubMed] [Google Scholar]
- 199.Mitani T, Yamaji R, Higashimura Y, et al. Hypoxia enhances transcriptional activity of androgen receptor through hypoxia-inducible factor-1 alpha in a low androgen environment. J Steroid Biochem Mol Biol. 2011;123:58–64. doi: 10.1016/j.jsbmb.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 200.Mishra A, Wang J, Shiozawa Y, et al. Hypoxia stabilizes GAS6/AXl signalling in metastatic prostate cancer. Mol Cancer Res. 2012;10:703–12. doi: 10.1158/1541-7786.MCR-11-0569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Hagtvet E, Roe K, Olsen DR. Liposomal doxorubicin improves radiotherapy response in hypoxic prostate cancer xenografts. Radiat Oncol. 2011;6:135. doi: 10.1186/1748-717X-6-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Cho SY, Lee HJ, Jeong SJ, et al. Sphingosine kinase 1 pathway is involved in melatonin- induced HIF-1 alpha inactivation in hypoxic PC-3 prostate cancer cells. J Pineal Res. 2011;51:87–93. doi: 10.1111/j.1600-079X.2011.00865.x. [DOI] [PubMed] [Google Scholar]
- 203.Branco-Price C, Zhang N, Schnelle M, et al. Endothelial cell HIF-1 alpha and HIF-2 alpha differentially regulate metastatic success. Cancer Cell. 2012;21:52–65. doi: 10.1016/j.ccr.2011.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Yamasaki M, Nomura T, Sato F, et al. Chronic hypoxia induces androgen-independent and invasive behavior in LNCaP human prostate cancer cells. Urol Oncol. 2012 doi: 10.1016/j.urolonc.2011.12.007. in press. [DOI] [PubMed] [Google Scholar]
- 205.Giannoni E, Bianchini F, Masieri L, et al. Reciprocal activation of prostate cancer cells and cancer-associated fibroblasts stimulates epithelial-mesenchymal transition and cancer stemness. Cancer Res. 2010;70:6945–56. doi: 10.1158/0008-5472.CAN-10-0785. [DOI] [PubMed] [Google Scholar]
- 206.Giannoni E, Bianchini F, Calorini L, et al. Cancer associated fibroblasts exploit reactive oxygen species through a pro-inflammatory signature leading to EMT and stemness. Antioxid Redox Signal. 2011;14:2361–71. doi: 10.1089/ars.2010.3727. [DOI] [PubMed] [Google Scholar]
- 207.Melchior SW, Corey E, Ellis WJ, et al. Early tumor cell dissemination in patients with clinically localized carcinoma of the prostate. Clin Cancer Res. 1997;3:249–56. [PubMed] [Google Scholar]
- 208.Shiozawa Y, Pedersen EA, Havens AM, et al. Human prostate cancer metastases target the hematopoietic stem cell niche to establish footholds in mouse bone marrow. J Clin Invest. 2011;121:1298–312. doi: 10.1172/JCI43414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Selander KS, Brown DA, Sequeiros GB, et al. Serum macrophage inhibitory cytokine- 1 concentrations correlate with the presence of prostate cancer bone metastases. Cancer Epidemiol Biomarkers Prev. 2007;16:532–7. doi: 10.1158/1055-9965.EPI-06-0841. [DOI] [PubMed] [Google Scholar]
- 210.Burger JA, Kipps TJ. CXCR4: a key receptor in the crosstalk between tumor cells and their microenvironment. Blood. 2006;107:1761–7. doi: 10.1182/blood-2005-08-3182. [DOI] [PubMed] [Google Scholar]
- 211.Shiozawa Y, Pienta KJ, Taichman RS. Hematopoietic stem cell niche is a potential therapeutic target for bone metastatic tumors. Clin Cancer Res. 2011;17:5553–8. doi: 10.1158/1078-0432.CCR-10-2505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Mohyeldin A, Garzon-Muvdi T, Quinones-Hinojosa A. Oxygen in stem cell biology: a critical component of the stem cell niche. Cell Stem Cell. 2010;7:150–61. doi: 10.1016/j.stem.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 213.Chinni SR, Sivalogan S, Dong Z, et al. FCXCL12/CXCR4 signalling activates Akt-1 and MMP-9 expression in prostate cancer cells: the role of bone microenvironmentassociated CXCL12. Prostate. 2006;66:32–48. doi: 10.1002/pros.20318. [DOI] [PubMed] [Google Scholar]
- 214.Chinni SR, Yamamoto H, Dong Z, et al. CXCL12/CXCR4 transactivates HER2 in lipid rafts of prostate cancer cells and promotes growth of metastatic deposits in bone. Mol Cancer Res. 2008;6:446–57. doi: 10.1158/1541-7786.MCR-07-0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Joseph J, Shiozawa Y, Jung Y, et al. Disseminated prostate cancer cells can instruct hematopoietic stem and progenitor cells to regulate bone phenotype. Mol Cancer Res. 2012;10:282–92. doi: 10.1158/1541-7786.MCR-11-0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Kobayashi A, Okuda H, Xing F, et al. PBone morphogenetic protein 7 in dormancy and metastasis of prostate cancer stem-like cells in bone. J Exp Med. 2011;208:2641–55. doi: 10.1084/jem.20110840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Mimeault M, Batra SK. Frequent gene products and molecular pathways altered in prostate cancer- and metastasis-initiating cells and novel promising multitargeted therapies. Mol Med. 2011;17:649–64. doi: 10.2119/molmed.2011.00115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Reddy KR, Guan Y, Qin G, et al. Combined treatment targeting HIF-1 alpha and Stat3 is a potent strategy for prostate cancer therapy. Prostate. 2011;71:1796–809. doi: 10.1002/pros.21397. [DOI] [PubMed] [Google Scholar]
- 219.Jeong CW, Yoon CY, Jeong SJ, et al. The role of hypoxia-inducible factor-1 alpha and -2 alpha in androgen insensitive prostate cancer cells. Urol Oncol. 2012 doi: 10.1016/j.urolonc.2012.03.022. in press. [DOI] [PubMed] [Google Scholar]
- 220.Ellis L, Lehet K, Ramakrishnan S, et al. Concurrent HDAC and mTORC1 inhibition attenuate androgen receptor and hypoxia signalling associated with alterations in microRNA expression. PLoS ONE. 2011;6:e27178. doi: 10.1371/journal.pone.0027178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Befani CD, Vlachostergios PJ, Hatzidaki E, et al. Bortezomib represses HIF-1alpha protein expression and nuclear accumulation by inhibiting both PI3K/Akt/TOR and MAPK pathways in prostate cancer cells. J Mol Med. 2012;90:45–54. doi: 10.1007/s00109-011-0805-8. [DOI] [PubMed] [Google Scholar]
- 222.Sinha I, Null K, Wolter W, et al. Methylseleninic acid downregulates hypoxia-inducible factor-1 alpha in invasive prostate cancer. Int J Cancer. 2012;130:1430–9. doi: 10.1002/ijc.26141. [DOI] [PubMed] [Google Scholar]
- 223.Jung SJ, Kim CI, Park CH, et al. Correlation between chemokine receptor CXCR4 expression and prognostic factors in patients with prostate cancer. Korean J Urol. 2011;52:607–11. doi: 10.4111/kju.2011.52.9.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Sun YX, Schneider A, Jung Y, et al. Skeletal localization and neutralization of the SDF-1(CXCL12)/CXCR4 axis blocks prostate cancer metastasis and growth in osseous sites in vivo. J Bone Miner Res. 2005;20:318–29. doi: 10.1359/JBMR.041109. [DOI] [PubMed] [Google Scholar]
- 225.Baron A, Migita T, Tang D, et al. Fatty acid synthase: a metabolic oncogene in prostate cancer? J Cell Biochem. 2004;91:47–53. doi: 10.1002/jcb.10708. [DOI] [PubMed] [Google Scholar]
- 226.Yamaguchi R, Janssen E, Perkins G, et al. Efficient elimination of cancer cells by deoxyglucose- ABT-263/737 combination therapy. PLoS ONE. 2011;6:e24102. doi: 10.1371/journal.pone.0024102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Moon JS, Jin WJ, Kwak JH, et al. Androgen stimulates glycolysis for de novo lipid synthesis by increasing the activities of hexokinase 2 and 6-phosphofructo-2-kinase/fructose-2,6-bisphosphatase 2 in prostate cancer cells. Biochem J. 2011;433:225–33. doi: 10.1042/BJ20101104. [DOI] [PubMed] [Google Scholar]
- 228.Stein M, Lin H, Jeyamohan C, et al. Targeting tumor metabolism with 2-deoxy-glucose in patients with castrate-resistant prostate cancer and advanced malignancies. Prostate. 2010;70:1388–94. doi: 10.1002/pros.21172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Gottfried E, Rogenhofer S, Waibel H, et al. Pioglitazone modulates tumor cell metabolism and proliferation in multicellular tumor spheroids. Cancer Chemother Pharmacol. 2011;67:117–26. doi: 10.1007/s00280-010-1294-0. [DOI] [PubMed] [Google Scholar]
- 230.Sotgia F, Martinez-Outschoorn UE, Howell A, et al. Caveolin-1 and cancer metabolism in the tumor microenvironment: markers, models, and mechanisms. Annu Rev Pathol. 2012;7:423–67. doi: 10.1146/annurev-pathol-011811-120856. [DOI] [PubMed] [Google Scholar]
- 231.Hu H, Chai Y, Wang L, et al. Pentagalloyl-glucose induces autophagy and caspase-independent programmed deaths in human PC-3 and mouse TRAMP-C2 prostate cancer cells. Mol Cancer Ther. 2009;8:2833–43. doi: 10.1158/1535-7163.MCT-09-0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Ben Sahra I, Laurent K, Giuliano S, et al. Targeting cancer cell metabolism: the combination of metformin and 2-deoxyglucose induces p53-dependent apoptosis in prostate cancer cells. Cancer Res. 2010;70:2465–75. doi: 10.1158/0008-5472.CAN-09-2782. [DOI] [PubMed] [Google Scholar]
- 233.Chhipa RR, Wu Y, Ip C. AMPK-mediated autophagy is a survival mechanism in androgen-dependent prostate cancer cells subjected to androgen deprivation and hypoxia. Cell Signal. 2011;23:1466–72. doi: 10.1016/j.cellsig.2011.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Nomura DK, Lombardi DP, Chang JW, et al. Monoacylglycerol lipase exerts dual control over endocannabinoid and fatty acid pathways to support prostate cancer. Chem Biol. 2011;18:846–56. doi: 10.1016/j.chembiol.2011.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Sorlie T, Wang Y, Xiao C, et al. Distinct molecular mechanisms underlying clinically relevant subtypes of breast cancer: gene expression analyses across three different platforms. BMC Genomics. 2006;7:127. doi: 10.1186/1471-2164-7-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Guedj M, Marisa L, de Reynies A, et al. A refined molecular taxonomy of breast cancer. Oncogene. 2011;31:1196–206. doi: 10.1038/onc.2011.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Punglia RS, Morrow M, Winer EP, et al. Local therapy and survival in breast cancer. N Engl J Med. 2007;356:2399–405. doi: 10.1056/NEJMra065241. [DOI] [PubMed] [Google Scholar]
- 238.Arteaga CL, Sliwkowski MX, Osborne CK, et al. Treatment of HER2-positive breast cancer: current status and future perspectives. Nat Rev Clin Oncol. 2012;9:16–32. doi: 10.1038/nrclinonc.2011.177. [DOI] [PubMed] [Google Scholar]
- 239.Dunn LK, Mohammad KS, Fournier PG, et al. Hypoxia and TGF-beta drive breast cancer bone metastases through parallel signalling pathways in tumor cells and the bone microenvironment. PLoS ONE. 2009;4:e6896. doi: 10.1371/journal.pone.0006896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Shipitsin M, Campbell LL, Argani P, et al. Molecular definition of breast tumor heterogeneity. Cancer Cell. 2007;11:259–73. doi: 10.1016/j.ccr.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 241.Bandyopadhyay A, Wang L, Agyin J, et al. Doxorubicin in combination with a small TGFbeta inhibitor: a potential novel therapy for metastatic breast cancer in mouse models. PLoS ONE. 2010;5:e10365. doi: 10.1371/journal.pone.0010365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Yin X, Wolford CC, Chang YS, et al. ATF3, an adaptive-response gene, enhances TGF {beta} signalling and cancer-initiating cell features in breast cancer cells. J Cell Sci. 2010;123:3558–65. doi: 10.1242/jcs.064915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Wang Y, Yu Y, Tsuyada A, et al. Transforming growth factor-beta regulates the sphere-initiating stem cell-like feature in breast cancer through miRNA-181 and ATM. Oncogene. 2011;30:1470–80. doi: 10.1038/onc.2010.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Oliveras-Ferraros C, Cufi S, Vazquez-Martin A, et al. Micro(mi)RNA expression profile of breast cancer epithelial cells treated with the anti-diabetic drug metformin: induction of the tumor suppressor miRNA let-7a and suppression of the TGFbeta-induced oncomiR miRNA-181a. Cell Cycle. 2011;10:1144–51. doi: 10.4161/cc.10.7.15210. [DOI] [PubMed] [Google Scholar]
- 245.Asiedu MK, Ingle JN, Behrens MD, et al. TGFbeta/TNF(alpha)-mediated epithelial-mesenchymal transition generates breast cancer stem cells with a claudin-low phenotype. Cancer Res. 2011;71:4707–19. doi: 10.1158/0008-5472.CAN-10-4554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Natarajan K, Xie Y, Baer MR, et al. Role of breast cancer resistance protein (BCRP/ABCG2) in cancer drug resistance. Biochem Pharmacol. 2012;83:1084–103. doi: 10.1016/j.bcp.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Hirsch HA, Iliopoulos D, Tsichlis PN, et al. Metformin selectively targets cancer stem cells, and acts together with chemotherapy to block tumor growth and prolong remission. Cancer Res. 2009;69:7507–11. doi: 10.1158/0008-5472.CAN-09-2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Dubrovska A, Hartung A, Bouchez LC, et al. CXCR4 activation maintains a stem cell population in tamoxifen-resistant breast cancer cells through AhR signalling. Br J Cancer. 2012;107:43–52. doi: 10.1038/bjc.2012.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Van Phuc P, Nhan PL, Nhung TH, et al. TDownregulation of CD44 reduces doxorubicin resistance of CD44CD24 breast cancer cells. Onco Targets Ther. 2011;4:71–8. doi: 10.2147/OTT.S21431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Song CW, Lee H, Dings RP, et al. Metformin kills and radiosensitizes cancer cells and preferentially kills cancer stem cells. Sci Rep. 2012;2:362. doi: 10.1038/srep00362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Bendinelli P, Matteucci E, Maroni P, et al. NF-kappaB activation, dependent on acetylation/deacetylation, contributes to HIF-1 activity and migration of bone metastatic breast carcinoma cells. Mol Cancer Res. 2009;7:1328–41. doi: 10.1158/1541-7786.MCR-08-0548. [DOI] [PubMed] [Google Scholar]
- 252.Huang M, Li Y, Zhang H, et al. Breast cancer stromal fibroblasts promote the generation of CD44+CD24− cells through SDF-1/CXCR4 interaction. J Exp Clin Cancer Res. 2010;29:80. doi: 10.1186/1756-9966-29-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Ling LJ, Wang S, Liu XA, et al. A novel mouse model of human breast cancer stem-like cells with high CD44+CD24−/lower phenotype metastasis to human bone. Chin Med J. 2008;121:1980–6. [PubMed] [Google Scholar]
- 254.Liang Z, Wu T, Lou H, et al. Inhibition of breast cancer metastasis by selective synthetic polypeptide against CXCR4. Cancer Res. 2004;64:4302–8. doi: 10.1158/0008-5472.CAN-03-3958. [DOI] [PubMed] [Google Scholar]
- 255.Okuda H, Kobayashi A, Xia B, et al. Hyaluronan synthase HAS2 promotes tumor progression in bone by stimulating the interaction of breast cancer stem-like cells with macrophages and stromal cells. Cancer Res. 2012;72:537–47. doi: 10.1158/0008-5472.CAN-11-1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Muller A, Homey B, Soto H, et al. Involvement of chemokine receptors in breast cancer metastasis. Nature. 2001;410:50–6. doi: 10.1038/35065016. [DOI] [PubMed] [Google Scholar]
- 257.Erler JT, Bennewith KL, Cox TR, et al. Hypoxia-induced lysyl oxidase is a critical mediator of bone marrow cell recruitment to form the premetastatic niche. Cancer Cell. 2009;15:35–44. doi: 10.1016/j.ccr.2008.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Ibrahim T, Sacanna E, Gaudio M, et al. Role of RANK, RANKL, OPG, and CXCR4 tissue markers in predicting bone metastases in breast cancer patients. Clin Breast Cancer. 2011;11:369–75. doi: 10.1016/j.clbc.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 259.Lu X, Mu E, Wei Y, et al. VCAM-1 promotes osteolytic expansion of indolent bone micrometastasis of breast cancer by engaging alpha4beta1-positive osteoclast progenitors. Cancer Cell. 2011;20:701–14. doi: 10.1016/j.ccr.2011.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Suva LJ, Griffin RJ, Makhoul I. Mechanisms of bone metastases of breast cancer. Endocr Relat Cancer. 2009;16:703–13. doi: 10.1677/ERC-09-0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Buijs JT, Henriquez NV, van Overveld PG, et al. vTGF-beta and BMP7 interactions in tumour progression and bone metastasis. Clin Exp Metastasis. 2007;24:609–17. doi: 10.1007/s10585-007-9118-2. [DOI] [PubMed] [Google Scholar]
- 262.Buijs JT, van der Horst G, van den Hoogen C, et al. The BMP2/7 heterodimer inhibits the human breast cancer stem cell subpopulation and bone metastases formation. Oncogene. 2012;31:2164–74. doi: 10.1038/onc.2011.400. [DOI] [PubMed] [Google Scholar]
- 263.Lee KH, Hsu EC, Guh JH, et al. Targeting energy metabolic and oncogenic signalling pathways in triple-negative breast cancer by a novel adenosine monophosphate-activated protein kinase (AMPK) activator. J Biol Chem. 2011;286:39247–58. doi: 10.1074/jbc.M111.264598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Iliopoulos D, Hirsch HA, Struhl K. Metformin decreases the dose of chemotherapy for prolonging tumor remission in mouse xenografts involving multiple cancer cell types. Cancer Res. 2011;71:3196–201. doi: 10.1158/0008-5472.CAN-10-3471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Furuta E, Pai SK, Zhan R, et al. Fatty acid synthase gene is up-regulated by hypoxia via activation of Akt and sterol regulatory element binding protein-1. Cancer Res. 2008;68:1003–11. doi: 10.1158/0008-5472.CAN-07-2489. [DOI] [PubMed] [Google Scholar]
- 266.Pandey PR, Okuda H, Watabe M, et al. Resveratrol suppresses growth of cancer stem-like cells by inhibiting fatty acid synthase. Breast Cancer Res Treat. 2011;130:387–98. doi: 10.1007/s10549-010-1300-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Pham PV, Phan NL, Nguyen NT, et al. Differentiation of breast cancer stem cells by knockdown of CD44: promising differentiation therapy. J Transl Med. 2011;9:209. doi: 10.1186/1479-5876-9-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Zakikhani M, Dowling R, Fantus IG, et al. Metformin is an AMP kinase-dependent growth inhibitor for breast cancer cells. Cancer Res. 2006;66:10269–73. doi: 10.1158/0008-5472.CAN-06-1500. [DOI] [PubMed] [Google Scholar]
- 269.Del Barco S, Vazquez-Martin A, Cufi S, et al. Metformin: multi-faceted protection against cancer. Oncotarget. 2011;2:896–917. doi: 10.18632/oncotarget.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Brand RE, Lerch MM, Rubinstein WS, et al. Advances in counselling and surveillance of patients at risk for pancreatic cancer. Gut. 2007;56:1460–9. doi: 10.1136/gut.2006.108456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Hidalgo M. Pancreatic cancer. N Engl J Med. 2010;362:1605–17. doi: 10.1056/NEJMra0901557. [DOI] [PubMed] [Google Scholar]
- 272.Di Marco M, Di Cicilia R, Macchini M, et al. Metastatic pancreatic cancer: is gemcitabine still the best standard treatment? Oncol Rep. 2010;23:1183–92. doi: 10.3892/or_00000749. [DOI] [PubMed] [Google Scholar]
- 273.Mimeault M, Brand RE, Sasson AA, et al. Recent advances on the molecular mechanisms involved in pancreatic cancer progression and therapies. Pancreas. 2005;31:301–16. doi: 10.1097/01.mpa.0000175893.04660.1b. [DOI] [PubMed] [Google Scholar]
- 274.Onozuka H, Tsuchihara K, Esumi H. Hypoglycemic/hypoxic condition in vitro mimicking the tumor microenvironment markedly reduced the efficacy of anticancer drugs. Cancer Sci. 2011;102:975–82. doi: 10.1111/j.1349-7006.2011.01880.x. [DOI] [PubMed] [Google Scholar]
- 275.Mimeault M, Batra SK. Recent progress on normal and malignant pancreatic stem/progenitor cell research: therapeutic implications for the treatment of type 1 or 2 diabetes mellitus and aggressive pancreatic cancer. Gut. 2008;57:1456–68. doi: 10.1136/gut.2008.150052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Bao B, Wang Z, Ali S, et al. Metformin inhibits cell proliferation, migration and invasion by attenuating CSC function mediated by deregulating miRNAs in pancreatic cancer cells. Cancer Prev Res. 2012;5:355–64. doi: 10.1158/1940-6207.CAPR-11-0299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Chaika NV, Yu F, Purohit V, et al. Differential expression of metabolic genes in tumor and stromal components of primary and metastatic loci in pancreatic adenocarcinoma. PLoS ONE. 2012;7:e32996. doi: 10.1371/journal.pone.0032996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Kim EJ, Simeone DM. Advances in pancreatic cancer. Curr Opin Gastroenterol. 2011;27:460–6. doi: 10.1097/MOG.0b013e328349e31f. [DOI] [PubMed] [Google Scholar]
- 279.Akakura N, Kobayashi M, Horiuchi I, et al. Constitutive expression of hypoxia-inducible factor-1 alpha renders pancreatic cancer cells resistant to apoptosis induced by hypoxia and nutrient deprivation. Cancer Res. 2001;61:6548–54. [PubMed] [Google Scholar]
- 280.Wei H, Wang C, Chen L. Proliferating cell nuclear antigen, survivin, and CD34 expressions in pancreatic cancer and their correlation with hypoxia-inducible factor 1 alpha. Pancreas. 2006;32:159–63. doi: 10.1097/01.mpa.0000202961.71600.9b. [DOI] [PubMed] [Google Scholar]
- 281.Cheng BQ, Segersvard R, Permert J, et al. Pancreatic cancer cells expressing hypoxia-inducible factor-1 alpha tend to be adjacent to intratumoral blood vessels. Eur Surg Res. 2010;45:134–7. doi: 10.1159/000319876. [DOI] [PubMed] [Google Scholar]
- 282.Zhang JJ, Wu HS, Wang L, et al. Expression and significance of TLR4 and HIF-1 alpha in pancreatic ductal adenocarcinoma. World J Gastroenterol. 2010;16:2881–8. doi: 10.3748/wjg.v16.i23.2881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Ying H, Kimmelman AC, Lyssiotis CA, et al. Oncogenic Kras maintains pancreatic tumors through regulation of anabolic glucose metabolism. Cell. 2012;149:656–70. doi: 10.1016/j.cell.2012.01.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Goldberg L, Israeli R, Kloog Y. FTS and 2-DG induce pancreatic cancer cell death and tumor shrinkage in mice. Cell Death Dis. 2012;3:e284. doi: 10.1038/cddis.2012.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Taly S-K, Galen H, Daniel VH, et al. Hedgehog signaling and desmoplasia are regulated by hypoxia in pancreatic cancer. Fourth AACR International Conference on Molecular Diagnostics in Cancer Therapeutic Development; Sep 27–30, 2010; Denver, CO. [Google Scholar]
- 286.Marechal R, Demetter P, Nagy N, et al. High expression of CXCR4 may predict poor survival in resected pancreatic adenocarcinoma. Br J Cancer. 2009;100:1444– 51. doi: 10.1038/sj.bjc.6605020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Onishi H, Kai M, Odate S, et al. Hypoxia activates the hedgehog signalling pathway in a ligand-independent manner by upregulation of Smo transcription in pancreatic cancer. Cancer Sci. 2011;102:1144–50. doi: 10.1111/j.1349-7006.2011.01912.x. [DOI] [PubMed] [Google Scholar]
- 288.Onishi H, Morifuji Y, Kai M, et al. Hedgehog inhibitor decreases chemosensitivity to 5-FU and gemcitabine under hypoxic conditions in pancreatic cancer. Cancer Sci. 2012 doi: 10.1111/j.1349-7006.2012.02297.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Chang Q, Jurisica I, Do T, et al. Hypoxia predicts aggressive growth and spontaneous metastasis formation from orthotopically grown primary xenografts of human pancreatic cancer. Cancer Res. 2011;71:3110–20. doi: 10.1158/0008-5472.CAN-10-4049. [DOI] [PubMed] [Google Scholar]
- 290.Melstrom LG, Salabat MR, Ding XZ, et al. Apigenin down-regulates the hypoxia response genes: HIF-1 alpha, GLUT-1, and VEGF in human pancreatic cancer cells. J Surg Res. 2011;167:173–81. doi: 10.1016/j.jss.2010.10.041. [DOI] [PubMed] [Google Scholar]
- 291.Sun JD, Liu Q, Wang J, et al. Selective tumor hypoxia targeting by hypoxia-activated prodrug TH-302 inhibits tumor growth in preclinical models of cancer. Clin Cancer Res. 2012;18:758–70. doi: 10.1158/1078-0432.CCR-11-1980. [DOI] [PubMed] [Google Scholar]
- 292.Yang S, Kimmelman AC. A critical role for autophagy in pancreatic cancer. Autophagy. 2011;7:912–3. doi: 10.4161/auto.7.8.15762. [DOI] [PubMed] [Google Scholar]
- 293.Xi H, Kurtoglu M, Liu H, et al. 2-Deoxy-D-glucose activates autophagy via endoplasmic reticulum stress rather than ATP depletion. Cancer Chemother Pharmacol. 2011;67:899–910. doi: 10.1007/s00280-010-1391-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Bhardwaj V, Rizvi N, Lai MB, et al. Glycolytic enzyme inhibitors affect pancreatic cancer survival by modulating its signalling and energetics. Anticancer Res. 2010;30:743–9. [PubMed] [Google Scholar]
- 295.Cao X, Bloomston M, Zhang T, et al. Synergistic antipancreatic tumor effect by simultaneously targeting hypoxic cancer cells with HSP90 inhibitor and glycolysis inhibitor. Clin Cancer Res. 2008;14:1831–9. doi: 10.1158/1078-0432.CCR-07-1607. [DOI] [PubMed] [Google Scholar]
- 296.Cheng ZX, Sun B, Wang SJ, et al. Nuclear factor-kappaB-dependent epithelial to mesenchymal transition induced by HIF-1 alpha activation in pancreatic cancer cells under hypoxic conditions. PLoS ONE. 2011;6:e23752. doi: 10.1371/journal.pone.0023752. [DOI] [PMC free article] [PubMed] [Google Scholar]