Abstract
Objective
Many injuries to children cannot be prevented without some degree of active behavior on the part of parents. A better understanding of social and cognitive determinants of parents’ injury prevention behavior and the identification of potential subgroups for targeted message delivery could advance the effectiveness of educational and behavioral interventions. This study assessed the degree to which parents’ injury prevention behavior is associated with theoretical determinants and examined whether this relation differs by age or birth order of child.
Design
Cross sectional observational study.
Setting
Three Midwestern pediatric clinics.
Subjects
594 parents of children ages 0–4 attending routine well child visits.
Measures
Injury prevention attitudes, beliefs, and practices.
Results
Overall, only modest relations were observed between injury beliefs and attitudes and injury prevention behaviors. However, these relations differed substantially by child age and birth order, with stronger associations observed for parents of older first born children. Outcome expectations and social norms were more strongly related to injury prevention behavior among parents of preschool children than among parents of infants and toddlers, while attitudes were more predictive for parents of first born children than parents of later born children.
Conclusions
These findings highlight the complexity of relations between theorized determinants and behavior, and suggest the potential utility of using audience segmentation strategies in behavioral interventions addressing injury prevention.
The goal of audience segmentation in health communication is to identify and describe population subgroups that are homogeneous in ways that are relevant to some desired behavior or outcome.1 When such groups are identified and well understood, different communication strategies can be developed to reach different subgroups.2 These group specific, or targeted, strategies should enhance the effectiveness of health communication by increasing its relevance to a given audience.3 As a step towards the development of targeted and more effective child injury prevention programs, this study seeks to determine whether parents of young children can be segmented into distinct subgroups that are homogeneous with respect to the most important injury prevention attitudes and beliefs to target.
Unintentional injuries are the leading cause of preventable death and a major cause of morbidity among children ages 1–5 years in the United States.4 5 Demographic risk factors for pediatric injury include age and sex of the child, socioeconomic status, and geographic location.6 The type and severity of injuries occurring during these years exhibit developmental patterns, reflecting changes both in exposure and developmental capabilities.6–9 While considerable progress has been made in reducing the burden of injury, it is estimated that approximately one third of childhood injury deaths are preventable.10
Some injury prevention strategies for children can be implemented solely through passive means (for example, legislation of flame retardant sleepwear); however, many require active behavior on the part of the parent or guardian to be effective (for example, complying with motor vehicle child restraint laws, using a stair gate, or supervising young children in the bathtub). Unfortunately, the effectiveness of educational strategies implemented to date has been less than optimal.11–16 To improve educational strategies, there is a need to better understand the determinants of injury prevention behavior and how they may vary among different groups of parents.16 Social cognitive theory17 as well as other influential cognitive theories18 19 would suggest that specific attitudes and beliefs, such as beliefs about the outcomes of performing the behavior, beliefs about one’s capability in performing the behavior, perceived social norms, and perceived environmental barriers would be important mediators to target in interventions designed to increase injury prevention behavior. Indeed, previous studies show an effect of outcome expectations,20–24 social norms,20 24 and barriers24–26 on the injury prevention behavior of parents. However, the magnitude of these relations is consistently small.
One explanation for these findings could be that the relation varies according to characteristics of the parent or child. Injury prevention behaviors are practiced across a developmental spectrum for any given child, and for most parents, across successive children. Injury prevention practices, then, may be influenced by previous parenting behavior. Previous studies indicate that age and birth order of the child are associated with injury prevention practices. Mothers of younger children have been found to have more accurate perceptions of safety prevention behaviors than parents of older children,27 28 and parents of children older than 2.5 years were less likely to use safety measures than parents of younger children.28 In another study, children born third or later in the birth order were at 5.7 times greater risk of sustaining an injury.29 Thus, parents may be influenced by their experiences with previous children or otherwise change their parenting practices over time, and thus be differentially influenced by cognitive or social factors such as norms or expectations.
The purpose of this study is to assess the degree to which injury prevention behavior is associated with theoretically driven determinants, including outcome expectations, barriers, attitudes, and social norms, and to determine whether this relation differs by age and/or birth order of child. It is hypothesized that these determinants will be related to injury prevention behaviors, but that the degree of association will vary by child age and birth order.
METHODS
Participants
Participants were 594 parents of children ages 0–4 attending a well child visit at one of three Midwestern pediatric clinics. The three clinics are part of the Southern Illinois Healthcare Foundation, with one clinic located in East Saint Louis, the second located in Centreville, and the third located in Bethalto. The patient population of the first two clinics is primarily low income African-American children and parents; the third serves primarily low to middle income white children and parents. Parents of children ages 0–4 years who were scheduled for a routine well child visit were invited to participate in the study (n = 872). Of these, 601 (69%) agreed to participate in the study. Seven participants did not complete the baseline assessment of injury prevention behaviors, and so were not included in this analysis; thus the resulting sample size was 594. The sample was primarily of lower socioeconomic status, with 59% of the participants having incomes less than $25,000; 35% between $25,000 and $49,999; and 6% greater than $50,000. Fifty six percent of the participants were African-American, 34% were white, and 10% were other races.
Procedures
Data used in these analyses were collected as the baseline assessment for a randomized trial evaluating injury prevention communication provided in a clinical setting. Parents were recruited to the study when they arrived at the pediatric clinic for a well child visit. Parents were eligible for the study if they had a child age 4 years or younger who was receiving a well child visit, and could read/speak English. If parents had two children in the target age range, they were asked to complete the assessment regarding the younger one. Written consent was obtained from each participating parent, and parents were assured of the confidentiality of their responses. Participants completed the baseline assessment using a computer kiosk located in the clinic waiting room. Questions were presented one at a time on the computer screen, and participants selected their responses using a mouse. The kiosk was placed away from the main waiting area, so that participant responses would not be observed by others in the waiting room. Research staff explained how to use the computer and were available to participants should they request assistance, but remained at a distance to provide privacy during completion of the assessment. The study was approved by both the National Institute of Child Health and Human Development Institutional Review Board (IRB) and the Saint Louis University IRB.
Measures
Measures included an assessment of participants’ current injury prevention and injury risk behaviors, hypothesized determinants of injury prevention behaviors derived from theories of health behavior change,17 19 and relevant demographic items. These measures are defined below. Scaled scores were computed by calculating the mean responses to items in the scale and treating them as continuous variables; Cronbach’s alpha is included in parentheses as a measure of the internal consistency of the scale, where applicable.
Injury prevention behaviors
Injury prevention behaviors were measured by items assessing specific behaviors relevant to each of six child injury risk areas—motor vehicle injuries, burns, falls, poisoning, airway obstruction, and drowning. Behaviors were selected for inclusion in the assessment based on current recommendations of the American Academy of Pediatrics. Programmed skip patterns were used so that parents answered only questions relevant to their child’s age (for example, sleep position assessed only for infants; use of a stair gate and a walker assessed for children ages 7–23 months, and so on). Individual injury prevention behaviors were weighted on a four point scale (low, moderate, high, or very high risk) based on the frequency and severity of injuries associated with that behavior (so that behavior representing high risk would contribute more strongly to the overall score than behavior representing lower risk). An overall injury prevention score was calculated for each participant as the weighted percent of age appropriate injury prevention behaviors reported by the parent. Possible scores range from 0–100% and indicate the weighted percent of age appropriate injury prevention behaviors reported by the parent.
Outcome expectations (α = 0.96)
Participants rated the perceived risk of 18 injury related risk behaviors and the perceived effectiveness of five injury prevention devices on 1–10 scales of “no risk” to “extremely high risk” (for risk behaviors) and “no protection” to “perfect protection” (for protective devices).
Attitudes (α = 0.70)
Participants rated the extent to which they agreed or disagreed with six items reflecting different reasons for not using injury prevention measures (perceived lack of control over injury, using supervision rather than injury prevention measures, teaching the child to obey rather than using injury prevention measures, and the perceived normalcy of minor injuries).
Social norms (α = 0.88)
On a 1–10 scale ranging from “not important” to “extremely important”, participants completed five items rating the importance of injury prevention measures to their spouse or partner, parents, other relatives, friends, and other parents they know.
Barriers (α = 0.95)
On a 1–10 scale ranging from “not a problem at all” to “very much a problem”, participants rated the extent to which each of six common barriers was a problem for them. Barriers included lack of resources, fatigue, hassles, lack of knowledge, demands on time and attention, and constraints in the home environment.
Demographics
Participants provided relevant demographic information on personal, child, and household characteristics including child’s sex, birth order, race, parent’s age, education, household income, and homeowner status.
Analysis
Descriptive analyses were conducted to determine the prevalence of injury risk and prevention behaviors. The four explanatory variables were evaluated for normality, linearity, homoscedasticity, independence of residuals, and outliers. To reduce skewness and improve normality, inverse transformations were applied to outcome expectations, attitudes, and social norms; square root transformation was used for barriers. To test the relation of each explanatory variable with injury prevention score, and to determine whether these relations differ by age and birth order, hierarchical multiple regression analyses were conducted. Injury prevention score was regressed on each explanatory variable, along with age, race, and birth order; interaction terms were then added to each model. Only those variables demonstrating significant main effects or interactions were retained in the models. Significant interactions were graphed, with age dichotomized into 0–23 months versus 2–4 years. To further analyze the predictive utility of these constructs regression equations were generated for each of four subgroups by age and birth order, with injury prevention score regressed on those explanatory variables showing significant correlations with injury prevention score for each subgroup.
RESULTS
Overall injury prevention scores ranged from 0.03 to 1.00, with a mean of 0.83 (SD 0.11), indicating an 83% mean weighted adherence to injury prevention recommendations (see http://www.injuryprevention.com/Supplemental for table 1). No significant differences in injury prevention score were observed by the child’s sex or birth order; parent’s age or education; or household income or homeowner status. However, there were significant differences in injury prevention scores by race, with white parents reporting higher injury prevention scores.
Table 1.
Sample characteristics
| Sample, n | % | Injury prevention score* | |
|---|---|---|---|
| Child characteristics | |||
| Sex | NS | ||
| Male | 321 | 54.0% | 0.83 |
| Female | 273 | 46.0% | 0.84 |
| Birth order | NS | ||
| First born | 227 | 38.2% | 0.83 |
| Later born | 367 | 61.8% | 0.83 |
| Race | (F = 8.2; p < 0.001) | ||
| White | 202 | 34.2% | 0.86a |
| African-American | 329 | 55.7% | 0.82b |
| Other | 60 | 10.2% | 0.80b |
| Participant characteristics | |||
| Participant age (years) | NS | ||
| ≥20 | 138 | 23.4% | 0.81 |
| 21–25 | 224 | 37.9% | 0.84 |
| 26–30 | 108 | 18.3% | 0.84 |
| 31–35 | 54 | 9.1% | 0.86 |
| >35 | 67 | 11.3% | 0.83 |
| Participant education | NS | ||
| <High school diploma | 89 | 14.8% | 0.82 |
| High school diploma/GED | 278 | 46.7% | 0.84 |
| Some college | 175 | 29.2% | 0.83 |
| College graduate | 39 | 6.5% | 0.83 |
| Postgraduate | 10 | 1.7% | 0.76 |
| Household characteristics | |||
| Household income | NS | ||
| <$10,000 | 227 | 38.8% | 0.83 |
| $10,000–$14,999 | 123 | 20.0% | 0.83 |
| $15,000–$24,999 | 113 | 19.3% | 0.84 |
| $25,000–$49,999 | 89 | 15.2% | 0.84 |
| $50,000–$74,999 | 25 | 4.3% | 0.87 |
| ≥$75,000 | 8 | 1.4% | 0.78 |
| Homeowner status | NS | ||
| Rent home | 446 | 75.3% | 0.83 |
| Own home | 146 | 24.7% | 0.84 |
Significant difference in injury prevention score by demographic characteristic is indicated in parentheses.
Groups with different superscript letters are significantly different in post hoc analyses.
NS, not significant.
Adherence to different injury prevention behaviors ranged from 39% to 98% (table 2). Adherence rates for prevention behaviors related to motor vehicle safety were high: 90% of parents report always using a car seat, 92% never take the child out of the seat while the car is moving, and 98% place the car seat in the back of the car. Adherence rates were lower for many other behaviors. Only 39% of parents reported having a crib free of choking risk items, 43% of parents reported ensuring that their hot water heater was set at a temperature of 120° or less, only half of those with stairs in the home reported using stair gates consistently, and half of the parents reported using a walker.
Table 2.
Prevalence of injury prevention behaviors
| Injury prevention behavior | %* |
|---|---|
| Burn/fire risk | |
| Smoke detector in home | 96.8 |
| Checked or changed battery in past 6 months (if has a smoke detector) | 79.4 |
| Child not held while cooking or holding a hot liquid | 86.8 |
| Child not in kitchen when cooking | 72.6 |
| Pot handles away from edge of stove (if child in kitchen) | 94.5 |
| Child kept away from stove or oven (if child in kitchen) | 98.1 |
| Hot dishes away from edge of counter (if child in kitchen) | 96.4 |
| Outlet covers or plugs in unused outlets | 60.5 |
| Hot water temperature 120° or less | 42.5 |
| Fall risk | |
| Child always strapped into high chair, swing, or stroller | 97.7 |
| Child not allowed to play on balconies or high porches | 96.9 |
| Child not left alone on bed | 86.2 |
| Child cannot access open windows in home | 75.5 |
| Walker not used | 53.8 |
| Stair gate always used | 53.7 |
| Airway obstruction risk | |
| Cords on drapes or window blinds non-accessible, cut, or anchored | 90.3 |
| Infant placed on back or side for sleeping | 89.7 |
| Toys checked to avoid small pieces | 89.0 |
| Crib free of choking risk items | 38.7 |
| Choking risk foods avoided | 38.7 |
| Poisoning risk | |
| Reads instructions or talks with provider before giving over-the-counter medication | 98.8 |
| Medications locked or inaccessible | 89.3 |
| Childproof caps on medications | 88.6 |
| Knows how to contact poison control center | 83.6 |
| Visitor’s purses/bags not accessible to child | 80.4 |
| Poison control center number posted in home | 79.6 |
| Household cleaners locked or inaccessible | 78.9 |
| Car injury risk | |
| Car seat placed in back seat | 98.3 |
| Child never taken out of car seat while car is moving | 92.2 |
| Car seat always used | 90.4 |
| Car seat appropriate for age and weight | 75.9 |
| Drowning risk | |
| Water not left standing in tub, bucket, or kiddie pool | 94.8 |
| Child not left alone by pool (if home has a pool) | 92.6 |
| Child not left alone in tub | 91.0 |
| Fence around pool (if home has a pool) | 55.6 |
Each injury prevention behavior was only assessed if it was applicable based on the child’s age—thus the denominator for this percent varies.
Associations of injury prevention scores and theoretical constructs
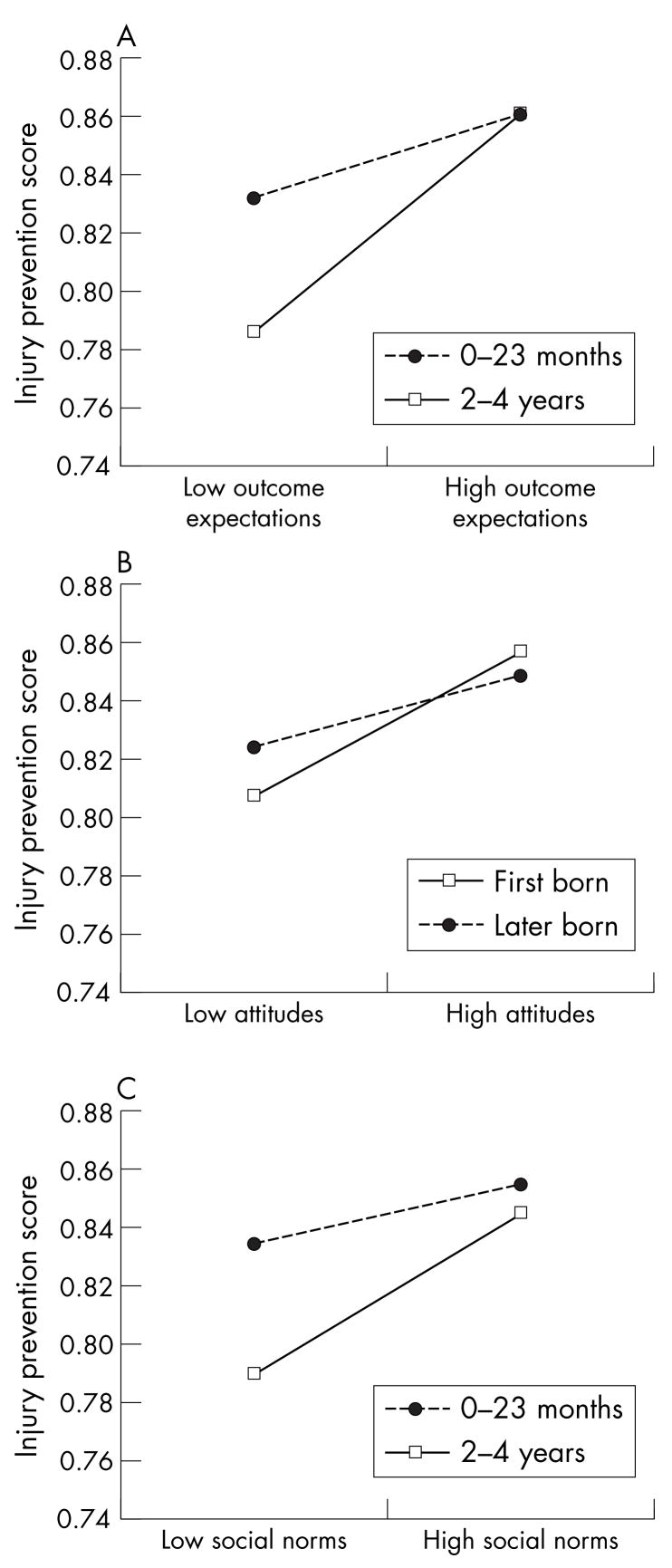
Each hypothesized determinant of injury prevention behavior was modestly predictive of injury prevention score (table 3). Significant interactions were observed for three of the four hypothesized determinants. Both outcome expectations and social norms interacted with child age to predict injury prevention score; attitudes interacted with child birth order. Outcome expectations and social norms were more strongly predictive of injury prevention behavior among parents of older than younger children (fig 1). Attitudes were more strongly predictive of injury prevention behavior among parents of first born than later born children. Barriers were somewhat predictive of injury prevention behavior, but did not interact with age or birth order.
Table 3.
Regression models for each of the four explanatory variables predicting injury prevention behaviors
| Main effects
|
Main effects and interactions
|
|||||||
|---|---|---|---|---|---|---|---|---|
| b | 95% CI | β | p Value | B | 95% CI | β | P Value | |
| Race | 0.05 | 0.03 to 0.06 | 0.22 | <0.001 | 0.05 | 0.03 to 0.06 | 0.22 | <0.001 |
| Age | −0.01 | −0.01 to −0.00 | −0.17 | <0.001 | −0.02 | −0.03 to −0.01 | −0.37 | <0.001 |
| Outcome expectations | 0.11 | 0.08 to 0.14 | 0.31 | <0.001 | 0.06 | 0.00 to 0.03 | 0.16 | 0.05 |
| Outcome expectations × age | 0.02 | 0.00 to 0.03 | 0.27 | 0.03 | ||||
| Adj r2 = 0.145; F = 31.15** | Adj r2 = 0.151; F change = 4.86* | |||||||
| Race | 0.03 | 0.02 to 0.5 | 0.15 | <0.001 | 0.03 | 0.02 to 0.05 | 0.15 | <0.001 |
| Age | −0.01 | −0.01 to −0.01 | −0.17 | <0.001 | −0.01 | −0.01 to −0.01 | −0.17 | <0.001 |
| Attitudes | 0.11 | 0.07 to 0.15 | 0.20 | <0.001 | 20.03 | 20.16 to 0.09 | 20.06 | 0.60 |
| Birth order | 0.01 | 0.01 to 0.03 | 0.01 | 0.31 | 0.08 | 0.02 to 0.15 | 0.39 | 0.01 |
| Attitudes × birth order | 0.10 | 0.02 to 0.19 | 0.46 | 0.02 | ||||
| Adj r2 = 0.086; F = 14.61** | Adj r2 = 0.093; F change = 5.56* | |||||||
| Race | 0.04 | 0.02 to 0.05 | 0.18 | <0.001 | 0.04 | 0.02 to 0.05 | 0.18 | <0.001 |
| Age | −0.01 | −0.05 to −0.02 | −0.17 | <0.001 | −0.02 | −0.03 to −0.01 | −0.45 | <0.001 |
| Social norms | 0.06 | 0.03 to 0.08 | 0.17 | <0.001 | 20.00 | 20.05 to 0.05 | 20.01 | 0.94 |
| Social norms × age | 0.02 | 0.00 to 0.03 | 0.35 | 0.01 | ||||
| Adj r2 = 0.081; F = 16.63** | Adj r2 = 0.090; F change = 6.17* | |||||||
| Race | 0.04 | 0.02 to 0.05 | 0.17 | <0.001 | ||||
| Age | −0.01 | −0.05 to −0.02 | −0.17 | <0.001 | ||||
| Barriers | −0.01 | −0.02 to −0.00 | −0.13 | 0.002 | ||||
| Adj r2 = 0.070; F = 14.21** | ||||||||
p < 0.05;
p < 0.001; b, unstandardized beta; β, standardized beta.
Figure 1.
Interactions among explanatory variables and demographic characteristics: (A) outcome expectations by age; (B) attitudes by birth order; (C) social norms by age.
Predictive models of injury prevention scores
As shown in the linear regression models (table 4), the hypothesized determinants were moderately predictive of injury prevention behaviors for younger children (both first and later born) and older later born children, but strongly predictive for older first born children. Among parents of children ages 0–23 months, attitudes and social norms were predictive of injury prevention behaviors for parents of first born children, while outcome expectations and barriers were predictive of injury prevention behaviors for parents of a later born child. For parents of older later born children, the only significant predictor was outcome expectations. However, none of the hypothesized determinants was highly predictive. Among parents of older first born children, outcome expectations and attitudes were significant predictors of injury prevention scores. For this subgroup, the set of hypothesized determinants was substantially predictive, accounting for 50% of the variance in injury prevention scores (r2 = 0.50, adjusted r2 = 0.46).
Table 4.
Linear regression analyses predicting injury prevention score
| b | 95% CI | β | p Value | |
|---|---|---|---|---|
| Age 0–23 months; first born (n = 161; 27% of total sample) Adjusted r2 = 0.08 | ||||
| Attitudes | 0.08 | 0.04 to 0.13 | 0.17 | <0.001 |
| Social norms | 0.05 | 0.02 to 0.07 | 0.15 | <0.001 |
| Race | 0.04 | 0.02 to 0.05 | 0.18 | <0.001 |
| Age 0–23 months; later born (n = 237; 40% of total sample) Adjusted r2 = 0.12 | ||||
| Outcome expectations | 0.09 | 0.03 to 0.14 | 0.22 | <0.01 |
| Barriers | −0.02 | −0.03 to −0.01 | −0.16 | 0.02 |
| Race | 0.06 | 0.08 to 0.03 | 0.26 | <0.001 |
| Age 2–4 years; first born (n = 66; 11% of total sample) Adjusted r2 = 0.46 | ||||
| Outcome expectations | 0.18 | 0.10 to 0.26 | 0.48 | <0.001 |
| Attitudes | 0.17 | 0.06 to 0.28 | 0.31 | <0.01 |
| Social norms | 0.15 | −0.02 to 0.12 | 0.14 | 0.19 |
| Race | 0.05 | 0.10 to 0.09 | 0.24 | 0.02 |
| Age 2–4 years; later born (n = 130; 22% of total sample) Adjusted r2 = 0.13 | ||||
| Outcome expectations | 0.09 | 0.03 to 0.16 | 0.30 | <0.01 |
| Social norms | 0.04 | −0.01 to 0.10 | 0.14 | 0.15 |
| Race | 0.03 | 0.01 to 0.06 | 0.14 | 0.12 |
b, unstandardized beta; β, standardized beta.
DISCUSSION
Overall, parents’ injury prevention score was only modestly related to theoretical determinants of behavior; however, the magnitude of these relations differed significantly by age of the child and birth order. Both outcome expectations and social norms were more strongly related to injury prevention behavior among parents of preschool children (ages 2–4) than among parents of infants and toddlers. It may be that parenting experiences during the child’s early years shape the development of outcome expectations and social norms, and these constructs gain influence based on experiences. Attitudes, however, were more predictive for parents of first born children than parents of later born children. It is possible that parenting experience diminishes the influence of attitudes, as behavior becomes more influenced by experience and expected outcomes. Overall, then, the potential determinants were most strongly associated with injury prevention behavior among parents of first born preschool children.
The findings of this study suggest the utility of an audience segmentation strategy for child injury prevention that distinguishes first time parents from parents of multiple children, and also considers children’s age. A good segmentation strategy has at least four key characteristics. First, it will identify distinct subgroups that are truly different with respect to the outcomes of interest. Second, these subgroups will be large enough in size or population proportion to justify allocation of resources to reach its members. Third, in order to assure that these groups can be reached with targeted communication, methods of identifying members of different audience segments should exist, be fast and easy to use, and reliable. Finally, the unique characteristics of each audience segment should provide clear opportunities and directions for targeting health information content and/or delivery channels. The proposed strategy meets all four criteria.
Although audience segmentation is recognized as a best practice in health communication, its application in many public health and injury prevention efforts has been relatively unsophisticated.30 Historically, public health educators have relied on risk status and/or demographic characteristics in defining target audiences. For example, potential target audiences for car injury prevention among infants and toddlers might vary by parent risk behavior,31 previous injury,32 33 or demographics, such as parent age34 or socioeconomic status.35 For obvious reasons, parents are identified most often as the target audience for health communication about child injury prevention. However, assuming homogeneity within such a broadly defined category (that is, parents) may not be justified. If subgroups of parents differ in systematic ways with respect to injury prevention beliefs and behaviors, different intervention approaches may be indicated.
Findings from this study suggest intervention strategies based on a social cognitive approach may be most effective with parents of first born children. Early work with these parents should emphasize the development of social norms and attitudes that are supportive of injury prevention behavior, including messages that establish injury prevention measures as an integral part of parenting; provide a sense of control over the occurrence of injuries; and promote supervision and training as necessary, but not sufficient for injury prevention. Establishing parents’ injury prevention behavior patterns during a child’s infancy and as the child becomes a toddler may facilitate the development of positive outcome expectations for injury prevention behavior as the child develops. It is possible that outcome expectations develop primarily out of parenting experience; if so, intervening to influence early behavior patterns is especially important. During the early childhood years, fostering parents’ positive outcome expectations appears to be a promising approach, as does assisting parents to identify and manage barriers to injury prevention behavior that they encounter.
Intervention approaches for experienced parents may be especially challenging, as social cognitive determinants were less associated with behavior for these parents, regardless of child age. Findings would suggest some utility in building positive outcome expectations, reducing barriers (primarily for parents of younger children), and promoting protective social norms (primarily for parents of older children). However, these measures may not be sufficient to affect behavior change. In working with these parents, it may be important to first assess injury prevention practices with previous children; then promote maintenance of previous preventive behavior, determine receptivity to changes from any previous risk behavior, and assess factors inhibiting these changes.
Several limitations to the study should be noted. The sample was predominantly of lower socioeconomic status from a limited geographical area, and so findings may not generalize to other populations. Data are cross sectional; thus we could not assess longitudinal or reciprocal relations between attitudes/beliefs and behavior. It should also be noted that subgroup analyses increase the chance of Type I error, and therefore the results have been interpreted cautiously to account for the possibility of such error. Injury prevention behavior was assessed by self report, and may be prone to social desirability bias. However, survey administration was conducted via computer kiosk, providing privacy to encourage honest responding. In addition, many of the safety behaviors assessed, such as consistency of car seat use or avoidance of choking risk foods, could not be assessed through single observations. Thus, self report remains the most practical method for assessing a broad spectrum of injury prevention behaviors.
Key points
Theorized social cognitive determinants of behavior were related to parent report of injury prevention practices, but degree of association ranged from modest to substantial within subgroups based on age and birth order of the child.
Outcome expectations and social norms were more strongly related to injury prevention behavior among parents of preschool children than among parents of infants and toddlers, while attitudes were more predictive for parents of first born children than parents of later born children.
An audience segmentation strategy for child injury prevention that distinguishes first time parents from parents of multiple children, and also considers the children’s age, may enhance effectiveness of injury prevention efforts.
Prevention approaches with experienced parents may be particularly challenging.
Findings from this study provide guidance for the development of programs targeting different groups of parents and their use of injury prevention practices. They also speak to the difficulties faced in the design of such programs. Typically, the most effective behavioral intervention efforts are those that modify key theoretical determinants of behavior. However, in this study, these determinants were only modestly associated with injury prevention behaviors for some subgroups. Considering that previous studies addressing potential determinants of injury prevention behavior have also found relatively weak relations,22 25 28 36 further work to elucidate the determinants of injury prevention behavior is needed. Currently, modifiable attitudes and beliefs that most effectively influence parents’ injury behavior are not sufficiently understood to optimally design effective prevention programs. Continued work using theory driven research and preventive intervention, with refinement and advancement of health communication strategies, is needed to realize the full benefit of active injury prevention strategies.
Footnotes
Competing interests: none.
References
- 1.Slater MD. Theory and method in health audience segmentation. J Health Commun. 1996;1:267–83. doi: 10.1080/108107396128059. [DOI] [PubMed] [Google Scholar]
- 2.Slater M. Choosing audience segmentation strategies and methods for health communication. In: Maibach E, Parrott R, editors. Designing health messages: approaches from communication theory and public health practice. Thousand Oaks, CA: Sage Publications; 1995. pp. 186–98. [Google Scholar]
- 3.Kreuter MW, Wray RJ. Tailored and targeted health communication: strategies for enhancing information relevance. Am J Health Behav. 2003;27(Suppl 3):S227–S232. doi: 10.5993/ajhb.27.1.s3.6. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System. Atlanta, Georgia: National Center for Injury Prevention and Control; 2002. [Google Scholar]
- 5.Centers for Disease Control and Prevention. Childhood Injury Fact Sheet. Atlanta, Georgia: National Center for Injury Prevention and Control; 2004. [Google Scholar]
- 6.Dowd MD, Keenan HT, Bratton SL. Epidemiology and prevention of childhood injuries. Crit Care Med. 2002;30:S385–S391. doi: 10.1097/00003246-200211001-00002. [DOI] [PubMed] [Google Scholar]
- 7.Mazurek A. Pediatric injury patterns. Int Anesthesiology Clin. 1994;32:11–25. [PubMed] [Google Scholar]
- 8.Pickett W, Streight S, Simpson D, et al. Injuries experienced by infant children: a population-based epidemiological analysis. Pediatrics. 2003;111:365–70. doi: 10.1542/peds.111.4.e365. [DOI] [PubMed] [Google Scholar]
- 9.Scheidt P, Harel Y, Trumble A, et al. The epidemiology of nonfatal injuries among US children and youth. Am J Public Health. 1995;85:932–8. doi: 10.2105/ajph.85.7.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Philippakis A, Hemenway D, Alexe DM, et al. A quantification of preventable unintentional childhood injury mortality in the United States. Inj Prev. 2004;10:79–82. doi: 10.1136/ip.2003.004119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Damashek A, Peterson L. Unintentional injury prevention efforts for young children: levels, methods, types, and targets. J Dev Behav Pediatr. 2002;23:443–55. doi: 10.1097/00004703-200212000-00010. [DOI] [PubMed] [Google Scholar]
- 12.DiGuiseppi C, Roberts IG. Individual-level injury prevention strategies in the clinical setting. Future Child. 2000;10:53–82. [PubMed] [Google Scholar]
- 13.Scheidt PC. Behavioral research toward prevention of childhood injury. Am J Dis Child. 1988;142:612–17. doi: 10.1001/archpedi.1988.02150060046027. [DOI] [PubMed] [Google Scholar]
- 14.Pless IB, Arsenault L. The role of health education in the prevention of injuries to children. J Soc Issues. 1987;43:87–103. [Google Scholar]
- 15.Towner E. The role of health education in childhood injury prevention. Inj Prev. 1995;1:53–8. doi: 10.1136/ip.1.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wortel E, de Geus GH, Kok G, et al. Injury control in pre-school children: a review of parental safety measures and the behavioral determinants. Health Education Research. 1994;9:201–13. [Google Scholar]
- 17.Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 18.Ajzen I, Fishbein M. Attitudinal and normative variables as predictors of specific behaviors. J Pers Soc Psychol. 1973;27:41–57. [Google Scholar]
- 19.Ajzen I. Attitudes, personality, and behavior. Chicago: The Dorsey Press; 1988. [Google Scholar]
- 20.Gielen AC, Eriksen MP, Daltroy LH, et al. Factors associated with the use of child restraint devices. Health Educ Q. 1984;11:195–206. doi: 10.1177/109019818401100210. [DOI] [PubMed] [Google Scholar]
- 21.Inder T, Geddis DC. Factors influencing the use of infant car restraints. Accid Anal Prev. 1990;22:297–300. doi: 10.1016/0001-4575(90)90021-c. [DOI] [PubMed] [Google Scholar]
- 22.Peterson L, Farmer J, Kashani J. Parental injury prevention endeavors: a function of health beliefs? Health Psychol. 1990;9:177–91. doi: 10.1037//0278-6133.9.2.177. [DOI] [PubMed] [Google Scholar]
- 23.Peterson L, Farmer J, Kashani JH. The role of beliefs in parental injury prevention efforts. In: Johnson JH, Johnson SB, editors. Advances in child health psychology. Gainesville: University of Florida Press; 1991. pp. 115–26. [Google Scholar]
- 24.Sellstrom E, Bremberg S, Garling A, et al. Risk of childhood injury: predictors of mothers’ perceptions. Scand J Public Health. 2000;28:188–93. [PubMed] [Google Scholar]
- 25.Gielen AC, Wilson MEH, Fader RR, et al. In-home injury prevention practices for infants and toddlers: the role of parental beliefs, barriers, and housing quality. Health Educ Q. 1995;22:85–95. doi: 10.1177/109019819502200108. [DOI] [PubMed] [Google Scholar]
- 26.Russell KM, Champion VL. Health beliefs and social influence in home safety practices of mothers with preschool children. IMAGE: Journal of Nursing Scholarship. 1996;28:59–64. doi: 10.1111/j.1547-5069.1996.tb01180.x. [DOI] [PubMed] [Google Scholar]
- 27.Eichelberger MR, Gotschall CS, Feely HB, et al. Parental attitudes and knowledge of child safety. Child Safety. 1990;144:714–20. doi: 10.1001/archpedi.1990.02150300112029. [DOI] [PubMed] [Google Scholar]
- 28.Greaves P, Glik DC, Kronenfeld JJ, et al. Determinants of controllable in-home child safety hazards. Health Educ Res. 1994;9:307–15. [Google Scholar]
- 29.Bourguet CC, McArtor RE. Unintentional injuries: risk factors in preschool children. Am J Dis Child. 1989;143:556–9. [PubMed] [Google Scholar]
- 30.Maibach E, Maxfield A, Ladin K, et al. Translating health psychology into effective health communication: The American Healthstyles Audience Segmentation Project. J Health Psychol. 1996;15:261–77. doi: 10.1177/135910539600100302. [DOI] [PubMed] [Google Scholar]
- 31.Tertinger DA, Greene BF, Lutzker JR. Home safety: development and validation of one component of an ecobehavioral treatment program for abused and neglected children. J Appl Behav Anal. 1984;17:159–74. doi: 10.1901/jaba.1984.17-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cushman R, Down J, MacMillan N, et al. Helmen promotion in the emergency room following a bicycle injury: a randomized trial. Pediatrics. 1991;88:43–7. [PubMed] [Google Scholar]
- 33.Jenkins HML, Blank V, Miller K, et al. A randomized single-blind evaluation of a discharge teaching book for pediatric patients with burns. J Burn Care Rehabil. 1996;17:49–61. [PubMed] [Google Scholar]
- 34.Jordan EA, Duggan AK, Hardy JB. Injuries in children of adolescent mothers: home safety education associated with decreased injury risk. Pediatrics. 1993;91:481–7. [PubMed] [Google Scholar]
- 35.Hardy JB, Street R. Family support and parenting education in the home: an effective extension of clinic-based preventive health care services for poor children. J Pediatr. 1989;115:927–31. doi: 10.1016/s0022-3476(89)80744-9. [DOI] [PubMed] [Google Scholar]
- 36.Glik DC, Greaves PE, Kronenfeld JJ, et al. Safety hazards in households with young children. J Pediatr Psychol. 1993;18:115–31. doi: 10.1093/jpepsy/18.1.115. [DOI] [PubMed] [Google Scholar]