Abstract
Rationale
Although evidence supporting use of non-invasive ventilation (NIV) during acute exacerbations of chronic obstructive pulmonary disease (COPD) is strong, evidence varies widely for other causes of acute respiratory failure.
Objectives
To compare utilization trends and outcomes associated with NIV in patients with and without COPD.
Methods
We identified 11,659,668 cases of acute respiratory failure from the Nationwide Inpatient Sample during years 2000-2009 and compared NIV utilization trends and failure rates for cases with or without a diagnosis of COPD.
Results and Measurements
The proportion of patients with COPD who received NIV increased from 3.5% in 2000 to 12.3% in 2009 (250% increase) and the proportion of patients without COPD who received NIV increased from 1.2% in 2000 compared with 6.0% in 2009 (400% increase). The rate of increase in the use of NIV was significantly greater for patients without COPD (18.1% annual change) as compared to patients with COPD (14.3% annual change), p=0.02. Patients without COPD were more likely to have failure of NIV requiring endotracheal intubation [adjusted odds ratio: 1.19 (95% CI 1.15-1.22, p<0.0001)]. Patients in whom NIV failed had higher hospital mortality than patients receiving mechanical ventilation without a preceding trial of NIV [adjusted odds ratio: 1.14 (95% CI 1.11-1.17), p<0.0001.
Conclusion
Utilization of NIV during acute respiratory failure has increased at a similar rate for all diagnoses, regardless of supporting evidence. However, NIV is more likely to fail in patients without COPD and NIV failure is associated with increased mortality.
Keywords: respiratory insufficiency, non-Invasive Ventilation, Positive-Pressure, Research, health services, outcome study
Introduction
Physicians report wide use of non-invasive ventilation (NIV) for a variety of clinical indications.(1-4) NIV may be particularly attractive to clinicians as it potentially offers an “easier,” less invasive form of respiratory support for patients with acute respiratory failure than traditional mechanical ventilation implemented through an endotracheal tube (MV). However, the ease of use of NIV may not translate into improved clinical outcomes. Indeed, the strength of evidence supporting use of NIV for acute respiratory failure varies according to the etiology of respiratory failure. Randomized trials consistently support improvements in mortality and reduction in endotracheal intubation rates with use of NIV during acute exacerbations of chronic obstructive pulmonary disease (COPD).(5) Findings supporting NIV for acute cardiogenic pulmonary edema are mixed,(6) though the weight of evidence favors a reduction in mortality and endotracheal intubation.(7) Little evidence supports the use of NIV for other causes of acute respiratory failure such as asthma(8) or pneumonia.(9, 10).
Clinical practice guidelines recommend use of NIV in patients with acute exacerbations of COPD and cardiogenic pulmonary edema, but generally do not recommend NIV for other causes of acute respiratory failure.(11-14) In accordance with clinical practice guidelines, utilization of NIV for acute exacerbations of COPD increased 4-fold from 1998-2008 in the United States, with concomitant decreased endotracheal intubation and hospital mortality.(15) Utilization patterns and outcomes associated with NIV use for other causes of acute respiratory failure outside of clinical trials remain unclear.
Given the enthusiasm reported by physicians for NIV in a variety of clinical presentations, (1-4) we hypothesized that, despite little supporting evidence, utilization of NIV in non-COPD causes of acute respiratory failure has increased at a similar rate to the use of NIV in COPD. Thus, we compared utilization trends and patient outcomes associated with NIV over the last decade in a nationwide, population-based sample of patients with acute respiratory failure associated with COPD and non-COPD diagnoses. Some of the results of this study have been previously reported in the form of an abstract.(16).
Methods
Data Source
We examined hospitalizations for adults (age ≥18 years) using year 2000-2009 discharge data from the Nationwide Inpatient Sample (NIS), Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality.(17) The NIS is an approximate 20% stratified probability sample of all non-Federal acute care hospitals and contains de-identified information from approximately 5-8 million hospital discharges yearly. NIS sampling strata are based on hospital characteristics such as ownership/control, teaching status, urban/rural location, US region and bed size. The 2000 NIS contained data from 994 hospitals in 28 states and the 2009 NIS included data from 1050 hospitals in 44 states. Abstracted NIS elements include demographics, admission and discharge status, length of stay, International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes, and hospital characteristics (geographic region, bed size, teaching status, urban/rural location). Although 25 ICD-9-CM codes were available in 2009, in order to avoid potential bias from an increased number of available diagnoses in 2009, only the first 15 diagnoses were abstracted for all years. Study procedures were deemed exempt by the Boston University Medical Campus Institutional Review Board.
Diagnosis and procedure classification
We selected our analysis cohort from hospitalizations with an ICD-9-CM code representing acute respiratory failure (518.81, 518.82, 518.84, 786.09, 799.1).(15) Patients with COPD were identified via ICD-9-CM codes for chronic bronchitis and emphysema (490-492, 495, 496). (15) We also performed a sensitivity analysis using an alternative definition of COPD that included the above codes as well as ICD-9-CM 493.22 (acute exacerbation of chronic obstructive asthma).(18) Patients without a COPD-associated ICD-9-CM code were classified as ‘non-COPD’ patients. As an exploratory analysis, we sub-classified non-COPD patients via a mutually exclusive algorithm according to the presence of a diagnosis of heart failure or cardiogenic pulmonary edema, asthma, pneumonia, sepsis, acute neurological disease, or other/unspecified etiology associated with acute respiratory failure (Table E1, online data supplement). In our algorithm, patients were assigned a diagnosis of COPD if any COPD diagnosis code was present; if no COPD code was found, then diagnosis codes were searched for a heart failure diagnosis, if no heart failure diagnosis was present, then an asthma diagnosis was searched, etc. Our algorithm was conservative in that patients were first assessed for diagnoses with a higher level of evidence for NIV prior to moving on to an alternative diagnosis with a lower level of NIV evidence. We selected comorbid conditions through enhanced Charlson and Elixhauser ICD-9-CM codes(19) for myocardial infarction, obesity, hypertension, diabetes mellitus, dementia, human immunodeficiency virus infection, paralysis, chronic liver disease, chronic kidney disease, neutropenia, and metastatic or hematologic malignancy. Acute factors were assessed through ICD-9-CM codes for type of acute organ dysfunction diagnoses,(20, 21) electrolyte abnormalities, critical care procedures (arterial catheterization, central venous catheterization, dialysis), and hospital strata characteristics (Table E1). Patients receiving NIV were identified with ICD-9-CM procedure code 93.90, and mechanical ventilation (MV) via endotracheal route was identified with a procedure code for mechanical ventilation (96.7) or endotracheal intubation (96.04).(15) Prior studies have shown that ICD-9-CM codes for MV (kappa 0.9)(22) and NIV (sensitivity 78%, specificity 100%)(23) are reliable. In patients with both NIV and MV procedure codes, patients were defined as having “NIV failure” if the NIV procedure day preceded or matched the procedure day of MV. In the NIS, procedures codes are identified by the hospital day on which they were performed, whereas diagnosis codes lack temporal markers.
Statistical analyses
We derived population estimates from the NIS using hospital weights with SAS version 9.1.3 (Cary, NC) surveyfreq, surveymeans and surveylogistic procedures. We used the glimmix procedure to calculate yearly age-adjusted rates of NIV use in patients with COPD and patients without COPD. We then used Joinpoint version 3.5.2 (Statistical Research and Applications Branch, National Cancer Institute, Bethesda, Maryland) to calculate the relative annual percent change (APC) in ventilator utilization and to test for differences in NIV utilization trends between COPD- and non-COPD- associated acute respiratory failure hospitalizations. Our primary outcome measure was the relative change in NIV utilization. Because of the evidence in support of NIV for cardiogenic pulmonary edema, we performed a sensitivity analysis comparing NIV utilization trends in patients with COPD or cardiogenic pulmonary edema to those without one of these diagnoses. We used logistic regression models (adjusted for patient demographics, comorbid conditions, acute organ failures, procedures, hospital characteristics, and year) to calculate odds ratios (OR) for NIV failure based upon COPD status. We used similar multivariable-adjusted logistic regression models (including above covariates, as well as the potential etiology of acute respiratory failure) to assess the association between NIV failure and hospital mortality. Because patients with sleep apnea may receive NIV for an indication other than acute respiratory failure, we performed an additional sensitivity analysis excluding patients with a sleep apnea diagnosis (ICD-9-CM 372.2 or 780.57). A two-sided alpha level of 0.05 was selected for statistical significance.
Results
Trends in acute respiratory failure
Of about 78 million (346 million population-weighted) discharges included in the NIS during years 2000-2009, we identified 2,380,632 [(3%); 11,659,668 million population-weighted] hospitalizations with an acute respiratory failure claim. Characteristics of patients with acute respiratory failure claims in years 2000 and 2009 are shown in Table 1. COPD was present in 900,750 [(37%); 4.4 million population-weighted] cases with an acute respiratory failure code (Figure E1, online data supplement). From years 2000-2009 the incidence of acute respiratory failure-coded hospitalizations/increased from 165 to 257/100,000 US residents (56% increase) for patients with COPD and increased from 238 to 463/100,000 (95% increase) in patients without COPD. (Figure E2, online data supplement).
Table 1. Characteristics of patients with acute respiratory failure by year.
| Weighted N (%) unless otherwise specified | 2000 Unweighted n=172,629 Weighted n=841,817 | 2009 Unweighted n=331,573 Weighted n=1,673,631 |
|---|---|---|
| Age, years, mean (95% CI) | 67.2 (67.2-67.4) | 66.1 (66.0-66.1) |
| Sex, female | 443,664 (52.7) | 862,026 (51.5) |
| Race/ethnicity | ||
| White | 501,047 (59.5) | 1,029,353 (61.5) |
| Black | 83,558 (9.9) | 178,961 (10.7) |
| Hispanic | 44,103 (5.2) | 108,623 (6.5) |
| Asian or Pacific Islander | 11,103 (1.3) | 30,284 (1.8) |
| Native American | 1350 (0.2) | 8179 (0.5) |
| Other or missing | 200,656 (23.8) | 318,232 (19.0) |
| Comorbidities | ||
| Total number of comorbidities, mean, (95% CI) | 0.94 (0.93-0.94) | 1.38 (1.37-1.38) |
| Hypertension | 293,339 (34.8) | 853,575 (51.0) |
| Diabetes mellitus | 176,759 (21.0) | 451,823 (27.0) |
| Chronic kidney disease | 81,609 (9.7) | 330,300 (19.7) |
| Dementia | 48,630 (5.8) | 131,816 (7.9) |
| Metastatic or hematologic malignancy | 58,182 (6.9) | 121,099 (7.2) |
| Chronic liver disease | 19,490 (2.3) | 50,907 (3.0) |
| Obesity | 40,786 (4.8) | 155,666 (9.3) |
| Myocardial infarction | 29,470 (3.5) | 68,455 (4.1) |
| Paralysis/plegia | 18,672 (2.2) | 53,832 (3.2) |
| Neutropenia | 14,668 (1.7) | 75,641 (4.5) |
| Human immunodeficiency virus | 8281 (1.0) | 12,958 (0.77) |
| Acute non-respiratory organ failures | ||
| Total # of acute organ failures, mean (95% CI) | 0.38 (0.38-0.38) | 0.72 (0.72-0.72) |
| Renal failure | 98,412 (11.7) | 462,110 (27.6) |
| Circulatory failure | 92,283 (11.0) | 323,539 (19.3) |
| Hematologic failure | 48,796 (5.8) | 126,588 (7.6) |
| Metabolic failure (acidosis) | 66,598 (7.9) | 235,601 (14.0) |
| Hepatic failure | 12,471 (1.5) | 57,306 (3.4) |
| Electrolyte abnormality | 279,547 (33.2) | 745,286 (44.5) |
| Procedures | ||
| Dialysis | 38,667 (4.6) | 114,711 (6.9) |
| Peripheral arterial catheter | 33,106 (3.9) | 85,063 (5.1) |
| Central venous catheter | 139,065 (16.5) | 446,933 (26.7) |
| Acute respiratory failure-associated diagnosis | ||
| COPD | 344,707 (40.9) | 597,022 (35.7) |
| Cardiogenic pulmonary edema | 155,396 (18.5) | 293,862 (17.6) |
| Asthma | 12,067 (1.4) | 54,877 (3.3) |
| Pneumonia | 121,682 (14.5) | 314,339 (18.8) |
| Sepsis | 24,763 (2.9) | 79,744 (4.8) |
| Neurological condition | 35,463 (4.3) | 91,995 (5.5) |
| Other/unknown | 146,777 (17.4) | 241,634 (14.4) |
| US Geographic Region | ||
| Northeast | 169,616 (20.1) | 277,172 (16.6) |
| Midwest | 174,886 (20.8) | 394,585 (23.6) |
| South | 354,270 (42.1) | 704,122 (42.1) |
| West | 143,082 (17.0) | 297,758 (17.8) |
| Hospital Bed size | ||
| Small | 89,164 (10.6) | 189,115 (11.5) |
| Medium | 239,147 (28.5) | 383,392 (23.3) |
| Large | 512,071 (60.9) | 1,070,949 (64.2) |
| Hospital Location - Urban | 716,130 (85.2) | 1,452,340 (88.4) |
| Teaching Hospital | 325,444 (38.7) | 704,711 (42.9) |
| Payer | ||
| Medicare | 540,255 (64.4) | 1053827 (63.1) |
| Medicaid | 76,487 (9.1) | 173,509 (10.4) |
| Private Insurance | 176,422 (21.0) | 324,163 (19.4) |
| Self-pay | 27,118 (3.2) | 71,970 (4.3) |
| Other | 18,262 (2.2) | 46,858 (2.8) |
Trends in NIV and MV
Population-based utilization of NIV during a hospitalization with an acute respiratory failure claim increased in patients with COPD from 8.6 to 39/100,000 US residents (360% increase) and NIV utilization in patients without COPD increased from 6 to 39 patients/100,000 US residents during years 2000-2009 (560% increase); use of MV increased by 73% for patients without COPD but remained relatively stable among patients with COPD (7% increase), (Figure 1).
Figure 1.
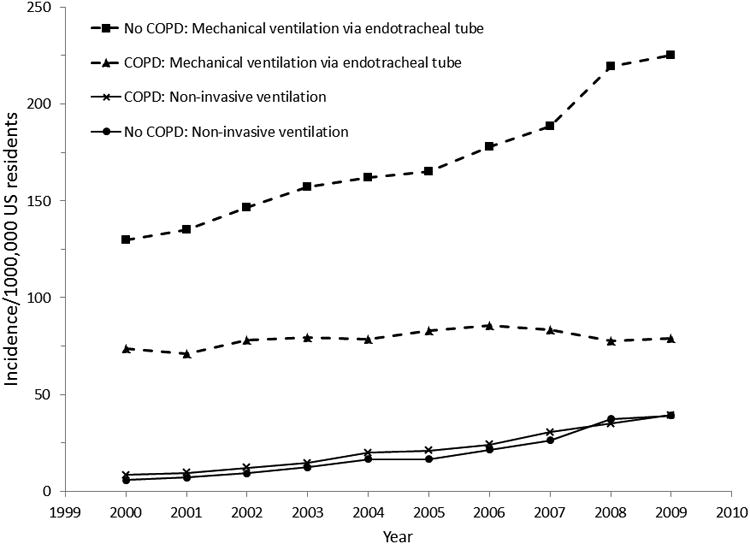
Population incidence of mechanical ventilation and non-invasive ventilation utilization among patients with an acute respiratory failure diagnosis in the United States, 2000-2009.
Among patients with acute respiratory failure codes, practice patterns involving the choice of initial ventilator interface changed similarly for patients with COPD (Figure 2A) and patients without COPD (Figure 2B) from 2000-2009. The proportion of patients with a COPD diagnosis who received NIV increased from 3.5% in 2000 to 12.3% in 2009 (250% increase) whereas 1.2% of patients without COPD received NIV in 2000 compared with 6.0% in 2009 (400% increase). These results represent a 14.3% APC (95% CI 12.1, 16.8%) in NIV among patients with COPD and a 18.1% APC (95% CI 15.9, 20.7%) among patients without COPD, p=0.02 (Figure E3, online data supplement). Results did not change substantially in a sensitivity analysis using an alternative definition of COPD (COPD: 260% increase in NIV, No COPD: 360% increase in NIV) or in a sensitivity analysis where patients with COPD or cardiogenic pulmonary edema (300% increase in NIV) were compared to patients without COPD or cardiogenic pulmonary edema (340% increase in NIV). The proportion of patients with COPD (Figure 2A) and without COPD (Figure 2B) who received MV showed a relative decline from 2000-2009 [COPD: −4.1% APC (95% CI −2.4, −5.8%); No COPD: −1.4% APC (95% CI −0.8, −2.0%)].
Figure 2.
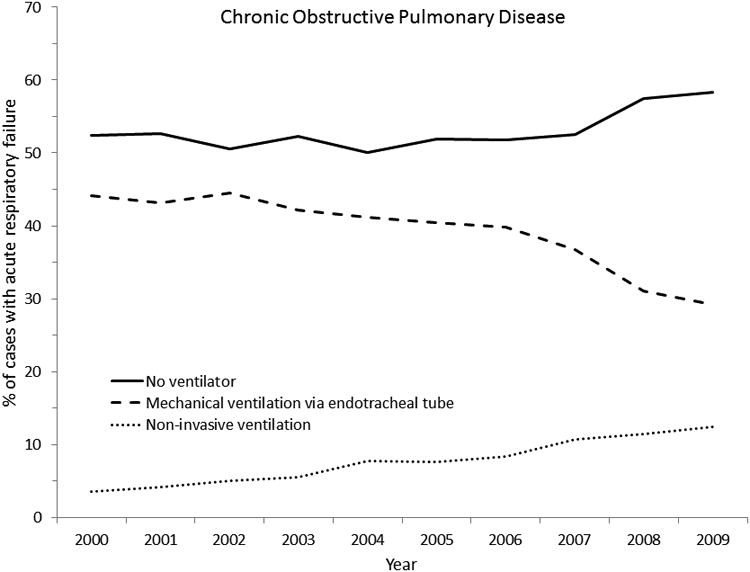

2A: United States trends in ventilator practice patterns during acute respiratory failure hospitalizations among patients with chronic obstructive pulmonary disease, 2000-2009.
2B: United States trends in ventilator practice patterns during acute respiratory failure hospitalizations among patients without a diagnosis of chronic obstructive pulmonary disease, 2000-2009.
The proportion of patients who received neither MV nor NIV increased among patients with COPD [1.3% APC (0.3, 2.4)] but did not significantly change among patients without COPD [0.4% APC (−0.1, 1.0%)]. When patients with and without COPD were combined, the proportion of patients who did not receive MV or NIV did not change from 2000-2009 (p=0.09).
Trends in NIV-Associated Diagnoses
Although COPD represented the most common diagnosis associated with use of NIV (52.6% of NIV utilization), among patients receiving NIV the proportion with a COPD diagnosis declined during the period from 2000-2009 (Figure 3).
Figure 3.
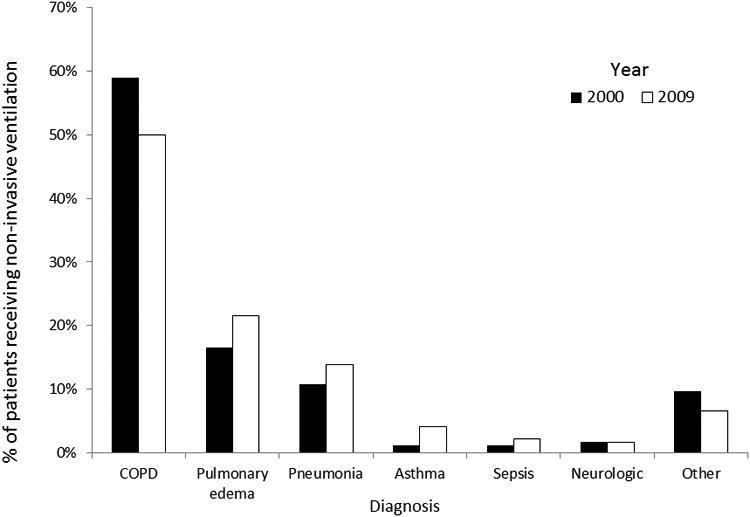
Changing etiologies of acute respiratory failure among patients receiving non-invasive ventilation, 2000 vs. 2009.
NIV Failure
A greater percentage of patients without a COPD diagnosis who received NIV subsequently required MV (i.e., failed NIV) [69,374/335717 (20.7%)] as compared to patients with COPD who received NIV [54,911/409,062 (13.4%)], multivariable-adjusted OR 1.19 (95% confidence intervals (CI) 1.15-1.22, p<0.0001). Table 2 demonstrates the other potential etiologies of acute respiratory failure that were associated with a greater risk of NIV failure than COPD. Among patients who received MV, those that experienced NIV failure prior to MV had greater hospital mortality, multivariable-adjusted OR 1.14 (95% CI 1.11-1.17), p<0.0001. Results did not appreciably differ in a sensitivity analysis using an alternative definition of COPD: the risk of NIV failure was greater in patients without COPD [OR 1.19 (95% CI 1.15-1.22)] and patients with NIV failure had greater hospital mortality [OR 1.13 (95% CI 1.10-1.16)].
Table 2. Failure of non-invasive ventilation among patients without COPD compared to patients with COPD.
| Acute respiratory failure etiology Weighted N | Adjusted odds ratio (95% CI) for failure of Non-invasive ventilation |
|---|---|
| COPD N=409,062 | Reference |
| Sepsis N=12,962 | 1.07 (0.97-1.19) |
| Heart failure N=153,489 | 1.08 (1.04-1.13) |
| Asthma N=24,438 | 1.18 (1.09-1.28) |
| Pneumonia N=78,162 | 1.56 (1.48-1.63) |
| Neurological diagnosis N=9075 | 1.70 (1.51-1.93) |
| Other/unknown diagnosis N=55,59 | 0.95 (0.89-1.01) |
Sensitivity analysis excluding sleep apnea
We identified 645,953 (5.5%) patients with acute respiratory failure who also had a sleep apnea diagnosis. A greater proportion of patients receiving NIV had sleep apnea [122,054/916,235 (13.3%)] than patients who did not receive NIV [523,899/10,219,350 (4.9%)]. After excluding patients with sleep apnea, we found little change in our results. The proportion of patients with COPD who received NIV again increased from 3.2% in 2000 to 11.4% in 2009 and the proportion of patients without COPD receiving NIV increased from 1.1% in 2000 to 5.5% in 2009. The multivariable-associated risk of NIV failure was similarly higher in patients without a COPD diagnosis as compared to with a COPD diagnosis [OR 1.20 (95% CI 1.16-1.24)]. Hospital mortality remained greater in patients who failed NIV than those that did not receive NIV prior to MV, multivariable-adjusted OR 1.16 (95% CI 1.13-1.19).
Discussion
We investigated population-based trends in the use of NIV among patients with an acute respiratory failure diagnosis code in the United States. Despite substantial differences in the evidence base supporting use of NIV to treat acute respiratory failure from COPD or cardiogenic pulmonary edema as compared to other etiologies, NIV utilization increased at similar relative rates regardless of the potential etiology of respiratory failure. When NIV was used in situations with weaker supporting evidence, such as patients without a COPD diagnosis, NIV was more likely to fail. Importantly, patients who required MV after NIV failure were more likely to die in the hospital than patients who received MV via endotracheal tube without a preceding trial of NIV.
Our results expand upon two prior studies investigating NIV utilization trends.(15, 24) Esteban et al. compared NIV utilization in 1998 with utilization in 2004 among critically ill patients who received MV through either an endotracheal tube or via NIV for at least 12 hours. Use of NIV was observed more frequently in 2004 [186/4968 ventilated patients (3.7%)] than in 1998 [61/5183 ventilated patients (1.1%)], with use increasing among both patients with COPD (17% in 1998 vs. 44% in 2004) and patients with acute respiratory failure from other etiologies (4% in 1998 vs. 10% in 2004). Chandra et al. investigated NIV trends in patients hospitalized with COPD and found a 4-fold increase in NIV and a decrease in use of MV from 1998-2008. Although the proportion of patients with COPD who received NIV was approximately 3 times greater in our study - most likely because our cohort was required to have an acute respiratory failure diagnosis code in addition to a COPD diagnosis - we observed similar NIV and MV trends among patients with COPD as Chandra et al.
Our findings of higher rates of NIV failure among patients without COPD are supported by findings of previous randomized trials (25, 26) and single center observational studies(27, 28) A systemic review of randomized trials comparing NIV to standard care for acute hypoxemic respiratory failure showed marked heterogeneity in outcomes; no mortality benefit was observed in patients without COPD or cardiogenic pulmonary edema.(29) Our results are also supported by previous studies that show an increase risk of death in patients with acute respiratory failure (28) or acute exacerbations of COPD (15) who fail NIV. The strength of our findings regarding utilization and outcomes associated with NIV during acute respiratory lies in the ‘real world’ population-based data, in which management was not controlled by clinical trial protocols or limited to a single center's experience.
We recognize that our study has limitations, most of which relate to our reliance on administrative data prepared for purposes of billing rather than clinical care or research. The ICD-9-CM codes used for our analyses depend on reliable healthcare provider identification and documentation of disease. Most ICD-9-CM validation studies(18, 23, 30, 31) demonstrate that claims data generally has lower sensitivity to identify diagnoses of interest, but high specificity, thus underestimating disease prevalence or incidence. Documentation in administrative data may reflect true trends in disease epidemiology or alternatively, may represent evolving documentation in response to changing reimbursement algorithms.(32) For example, over recent years hospitals may be increasingly likely to code “acute respiratory failure” when patients meet minimum criteria, in order to garner the higher reimbursement associated with codes assigned a higher disease severity level. Such “upcoding” may explain our finding of a decreasing proportion of patients with acute respiratory failure codes receiving invasive mechanical ventilation in later study years. However, two observations argue against this: 1) disease severity (as measured by number of organ failures) of patients with acute respiratory failure actually rose over time, suggesting a sicker population; 2) the proportion of patients with acute respiratory failure that received neither invasive nor non-invasive ventilation did not change over time, suggesting that the decreasing proportion of acute respiratory failure patients treated with invasive mechanical ventilation represents an increasing tendency to substitute NIV for treatment of respiratory failure. Using ICD-9-CM diagnosis codes, we could not ascertain with certainty the cause of acute respiratory failure, the indication for ventilatory support, disease severity, mitigating circumstances to clinical decision making (e.g., do not resuscitate status) or the temporality of diagnoses. In addition we could not ascertain the location of care or setting in which NIV was implemented. Although some evidence supports use of NIV in severely immunocompromised patients with hypoxemic respiratory failure,(33) assessment of immunocompromised status was limited with administrative data alone; thus we could not assess utilization or outcomes in the immunocompromised. Given the observational study design, we could not establish a causal relationship between NIV failure or acute respiratory failure etiology and outcomes such as mortality.
Despite these limitations, use of administrative data has a number of unique strengths. We were able to ascertain temporality between NIV and MV and procedure codes occurring on different hospital days; procedure codes for MV and NIV have previously been shown to be reliable.(22, 23) In addition, Lagu et al. demonstrated that mortality risk-adjustment using administrative data in critically ill patients with sepsis may be a “viable alternative” to severity of illness scores obtained from direct chart review (ie, APACHE II and SAPS II).(34) Of note, the NIS data used for the present study does not reliably contain two data elements that were present in Lagu et al. (ie.,early use of intensive care and vasopressors), thus risk-adjustment using NIS is currently uncertain. Most importantly, we were able to observe trends in use of invasive and non-invasive ventilation over a decade among millions of patients with acute respiratory failure from a nationally representative sample of U.S. hospitals. Use of a national database such as the NIS provides a ‘real world’ view of provider practice patterns that are unlikely affected by potential ‘Hawthorne effects’ and are more generalizable than limited patient or medical center characteristics of prospective cohorts, providing valuable information that allow for benchmarking of clinical practice and estimates of clinical effectiveness.
Our findings are consistent with prior surveys in which physicians expressed enthusiasm for use of NIV in clinical indications with little supporting evidence (e.g., asthma, pneumonia). (1-4) This type of “spill-over” of medical technology from an indication with proven efficacy to other indications has occurred in other areas as well. As healthcare providers become more comfortable with a medical technology and witness “success stories” associated with its use, we may seek to find broader application for the technology for untested indications. One recent example of this phenomenon is the use of drug-eluting coronary artery stents. During the first three years after FDA approval of drug-eluting stents, approximately 50% of patients received a drug eluting stent for an ‘off-label’ or ‘untested’ indication.(35, 36) ‘Off-label’ use of drug eluting stents was associated with worse outcomes than ‘on-label’ use,(35, 36) a finding that led an FDA advisory panel(37, 38) and revised societal guidelines(37) to recommend greater caution when considering ‘off-label’ or ‘untested’ use of drug eluting stents. After release of the FDA advisory panel recommendations, ‘off-label’ use of drug-eluting stents declined by approximately 66%.(39) Our findings of increasing utilization and worse outcomes associated with NIV use ‘outside of the evidence’ are similar to those of drug-eluting stents. Unless further trial data emerge, we recommend similar caution and increased vigilance when selecting NIV for indications without strong supporting evidence.
Supplementary Material
At a Glance Commentary.
Scientific Knowledge on the Subject: Utilization of non-invasive ventilation during exacerbations of chronic obstructive pulmonary disease has increased in association with strong evidence demonstrating clinical outcome benefits. Population-based utilization and outcomes of non-invasive ventilation for indications with weaker supporting evidence are unclear.
What This Study Adds to the Field: Utilization of non-invasive ventilation during acute respiratory failure has increased similarly for patients with and without chronic obstructive lung disease. Patients without chronic obstructive pulmonary disease are more likely to experience failure of non-invasive ventilation, and those who fail NIV experience higher in-hospital mortality.
Acknowledgments
Support: R21HL112672 (AJW) K07 CA138772 (RSW) and the Department of Veterans Affairs (RSW). No funding organization had a role in the design or conduct of the study.
Abbreviations
- APC
annual percent change
- CI
Confidence Interval
- COPD
Chronic obstructive pulmonary disease
- ICD-9-CM
International Classification of Disease, 9th Revision, Clinical Modification
- MV
Mechanical ventilation through endotracheal tube
- NIV
Non-invasive ventilation
- NIS
Nationwide Inpatient Sample
- OR
odds ratio
Footnotes
Contributions: concept, design, data analysis, interpretation, drafting of manuscript
Contributor Information
Allan J. Walkey, The Pulmonary Center, Division of Pulmonary and Critical Care Medicine, Department of Medicine, Boston University School of Medicine, Boston, MA, USA.
Renda Soylemez Wiener, The Pulmonary Center, Division of Pulmonary and Critical Care Medicine, Boston University School of Medicine, Boston, MA USA. Center for Health Quality, Outcomes, & Economic Research, Edith Nourse Rogers Memorial VA Hospital, Bedford, MA, USA.
References
- 1.Hess DR, Pang JM, Camargo CA., Jr A survey of the use of noninvasive ventilation in academic emergency departments in the United States. Respir Care. 2009;54:1306–1312. [PubMed] [Google Scholar]
- 2.Burns KE, Sinuff T, Adhikari NK, Meade MO, Heels-Ansdell D, Martin CM, Cook DJ. Bilevel noninvasive positive pressure ventilation for acute respiratory failure: survey of Ontario practice. Crit Care Med. 2005;33:1477–1483. doi: 10.1097/01.ccm.0000168042.59035.d8. [DOI] [PubMed] [Google Scholar]
- 3.Crimi C, Noto A, Princi P, Esquinas A, Nava S. A European survey of noninvasive ventilation practices. Eur Respir J. 2010;36:362–369. doi: 10.1183/09031936.00123509. [DOI] [PubMed] [Google Scholar]
- 4.Bierer GB, Soo Hoo GW. Noninvasive ventilation for acute respiratory failure: a national survey of Veterans Affairs hospitals. Respir Care. 2009;54:1313–1320. [PubMed] [Google Scholar]
- 5.Ram FS, Picot J, Lightowler J, Wedzicha JA. Non-invasive positive pressure ventilation for treatment of respiratory failure due to exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2004;(3):CD004104. doi: 10.1002/14651858.CD004104.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Gray A, Goodacre S, Newby DE, Masson M, Sampson F, Nicholl J 3CPO Trialists. Noninvasive ventilation in acute cardiogenic pulmonary edema. N Engl J Med. 2008;359:142–151. doi: 10.1056/NEJMoa0707992. [DOI] [PubMed] [Google Scholar]
- 7.Weng CL, Zhao YT, Liu QH, Fu CJ, Sun F, Ma YL, Chen YW, He QY. Meta-analysis: Noninvasive ventilation in acute cardiogenic pulmonary edema. Ann Intern Med. 2010;152:590–600. doi: 10.7326/0003-4819-152-9-201005040-00009. [DOI] [PubMed] [Google Scholar]
- 8.Ram FS, Wellington S, Rowe BH, Wedzicha JA. Non-invasive positive pressure ventilation for treatment of respiratory failure due to severe acute exacerbations of asthma. Cochrane Database Syst Rev. 2005;(1):CD004360. doi: 10.1002/14651858.CD004360.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Wysocki M, Tric L, Wolff MA, Millet H, Herman B. Noninvasive pressure support ventilation in patients with acute respiratory failure. A randomized comparison with conventional therapy. Chest. 1995;107:761–768. doi: 10.1378/chest.107.3.761. [DOI] [PubMed] [Google Scholar]
- 10.Confalonieri M, Potena A, Carbone G, Porta RD, Tolley EA, Umberto Meduri G. Acute respiratory failure in patients with severe community-acquired pneumonia. A prospective randomized evaluation of noninvasive ventilation. Am J Respir Crit Care Med. 1999;160:1585–1591. doi: 10.1164/ajrccm.160.5.9903015. [DOI] [PubMed] [Google Scholar]
- 11.British Thoracic Society Standards of Care Committee. Non-invasive ventilation in acute respiratory failure. Thorax. 2002;57:192–211. doi: 10.1136/thorax.57.3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Organized jointly by the American Thoracic Society, the European Respiratory Society, the European Society of Intensive Care Medicine, and the Societe de Reanimation de Langue Francaise, and approved by ATS Board of Directors, December 2000. International Consensus Conferences in Intensive Care Medicine: noninvasive positive pressure ventilation in acute Respiratory failure. Am J Respir Crit Care Med. 2001;(163):283–291. [Google Scholar]
- 13.Keenan SP, Sinuff T, Burns KE, Muscedere J, Kutsogiannis J, Mehta S, Cook DJ, Ayas N, Adhikari NK, Hand L, Scales DC, Pagnotta R, Lazosky L, Rocker G, Dial S, Laupland K, Sanders K, Dodek P Canadian Critical Care Trials Group/Canadian Critical Care Society Noninvasive Ventilation Guidelines Group. Clinical practice guidelines for the use of noninvasive positive-pressure ventilation and noninvasive continuous positive airway pressure in the acute care setting. CMAJ. 2011;183:E195–214. doi: 10.1503/cmaj.100071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schonhofer B, Kuhlen R, Neumann P, Westhoff M, Berndt C, Sitter H. Clinical practice guideline: non-invasive mechanical ventilation as treatment of acute respiratory failure. Dtsch Arztebl Int. 2008;105:424–433. doi: 10.3238/arztebl.2008.0424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chandra D, Stamm JA, Taylor B, Ramos RM, Satterwhite L, Krishnan JA, Mannino D, Sciurba FC, Holguin F. Outcomes of noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease in the United States, 1998-2008. Am J Respir Crit Care Med. 2012;185:152–159. doi: 10.1164/rccm.201106-1094OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walkey AJ, Wiener RS. Utilization Of Non-Invasive Ventilation In Patients With Acute Respiratory Failure From 2000-2009: A Population-Based Study [abstract] Am J Respir Crit Care Med. 2012;185:A6488. [Google Scholar]
- 17.HCUP Nationwide Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality. Rockville, MD: 1998-2009. [Google Scholar]
- 18.Stein BD, Bautista A, Schumock GT, Lee TA, Charbeneau JT, Lauderdale DS, Naureckas ET, Meltzer DO, Krishnan JA. The validity of International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis codes for identifying patients hospitalized for COPD exacerbations. Chest. 2012;141:87–93. doi: 10.1378/chest.11-0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 20.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 21.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Quan H, Parsons GA, Ghali WA. Validity of procedure codes in International Classification of Diseases, 9th revision, clinical modification administrative data. Med Care. 2004;42:801–809. doi: 10.1097/01.mlr.0000132391.59713.0d. [DOI] [PubMed] [Google Scholar]
- 23.Chio A, Ciccone G, Calvo A, Vercellino M, Di Vito N, Ghiglione P, Mutani R Piemonte and Valle d'Aosta Register for ALS. Validity of hospital morbidity records for amyotrophic lateral sclerosis. A population-based study J Clin Epidemiol. 2002;55:723–727. doi: 10.1016/s0895-4356(02)00409-2. [DOI] [PubMed] [Google Scholar]
- 24.Esteban A, Ferguson ND, Meade MO, Frutos-Vivar F, Apezteguia C, Brochard L, Raymondos K, Nin N, Hurtado J, Tomicic V, Gonzalez M, Elizalde J, Nightingale P, Abroug F, Pelosi P, Arabi Y, Moreno R, Jibaja M, D'Empaire G, Sandi F, Matamis D, Montanez AM, Anzueto A. Evolution of mechanical ventilation in response to clinical research. Am J Respir Crit Care Med. 2008;177:170–7. doi: 10.1164/rccm.200706-893OC. [DOI] [PubMed] [Google Scholar]
- 25.Delclaux C, L'Her E, Alberti C, Mancebo J, Abroug F, Conti G, Guerin C, Schortgen F, Lefort Y, Antonelli M, Lepage E, Lemaire F, Brochard L. Treatment of acute hypoxemic nonhypercapnic respiratory insufficiency with continuous positive airway pressure delivered by a face mask: A randomized controlled trial. JAMA. 2000;284:2352–2360. doi: 10.1001/jama.284.18.2352. [DOI] [PubMed] [Google Scholar]
- 26.Kramer N, Meyer TJ, Meharg J, Cece RD, Hill NS. Randomized, prospective trial of noninvasive positive pressure ventilation in acute respiratory failure. Am J Respir Crit Care Med. 1995;151:1799–1806. doi: 10.1164/ajrccm.151.6.7767523. [DOI] [PubMed] [Google Scholar]
- 27.Phua J, Kong K, Lee KH, Shen L, Lim TK. Noninvasive ventilation in hypercapnic acute respiratory failure due to chronic obstructive pulmonary disease vs. other conditions: effectiveness and predictors of failure. Intensive Care Med. 2005;31:533–539. doi: 10.1007/s00134-005-2582-8. [DOI] [PubMed] [Google Scholar]
- 28.Carrillo A, Gonzalez-Diaz G, Ferrer M, Martinez-Quintana ME, Lopez-Martinez A, Llamas N, Alcazar M, Torres A. Non-invasive ventilation in community-acquired pneumonia and severe acute respiratory failure. Intensive Care Med. 2012;38:458–466. doi: 10.1007/s00134-012-2475-6. [DOI] [PubMed] [Google Scholar]
- 29.Keenan SP, Sinuff T, Cook DJ, Hill NS. Does noninvasive positive pressure ventilation improve outcome in acute hypoxemic respiratory failure? A systematic review. Crit Care Med. 2004;32:2516–2523. doi: 10.1097/01.ccm.0000148011.51681.e2. [DOI] [PubMed] [Google Scholar]
- 30.Birman-Deych E, Waterman AD, Yan Y, Nilasena DS, Radford MJ, Gage BF. Accuracy of ICD-9-CM codes for identifying cardiovascular and stroke risk factors. Med Care. 2005;43:480–485. doi: 10.1097/01.mlr.0000160417.39497.a9. [DOI] [PubMed] [Google Scholar]
- 31.Walkey AJ, Wiener RS, Ghobrial JM, Curtis LH, Benjamin EJ. Incident stroke and mortality associated with new-onset atrial fibrillation in patients hospitalized with severe sepsis. JAMA. 2011;306:2248–2254. doi: 10.1001/jama.2011.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lindenauer PK, Lagu T, Shieh M, Pekow PS, Rothberg MB. Association of Diagnostic Coding With Trends in Hospitalizations and Mortality of Patients With Pneumonia, 2003-2009. JAMA: The Journal of the American Medical Association. 2012;307:1405–1413. doi: 10.1001/jama.2012.384. [DOI] [PubMed] [Google Scholar]
- 33.Hilbert G, Gruson D, Vargas F, Valentino R, Gbikpi-Benissan G, Dupon M, Reiffers J, Cardinaud JP. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N Engl J Med. 2001;344:481–487. doi: 10.1056/NEJM200102153440703. [DOI] [PubMed] [Google Scholar]
- 34.Lagu T, Lindenauer PK, Rothberg MB, Nathanson BH, Pekow PS, Steingrub JS, Higgins TL. Development and validation of a model that uses enhanced administrative data to predict mortality in patients with sepsis. Crit Care Med. 2011;39:2425–2430. doi: 10.1097/CCM.0b013e31822572e3. [DOI] [PubMed] [Google Scholar]
- 35.Beohar N, Davidson CJ, Kip KE, Goodreau L, Vlachos HA, Meyers SN, Benzuly KH, Flaherty JD, Ricciardi MJ, Bennett CL, Williams DO. Outcomes and complications associated with off-label and untested use of drug-eluting stents. JAMA. 2007;297:1992–2000. doi: 10.1001/jama.297.18.1992. [DOI] [PubMed] [Google Scholar]
- 36.Win HK, Caldera AE, Maresh K, Lopez J, Rihal CS, Parikh MA, Granada JF, Marulkar S, Nassif D, Cohen DJ, Kleiman NS EVENT Registry Investigators. Clinical outcomes and stent thrombosis following off-label use of drug-eluting stents. JAMA. 2007;297:2001–2009. doi: 10.1001/jama.297.18.2001. [DOI] [PubMed] [Google Scholar]
- 37.King SB, 3rd, Smith SC, Jr, Hirshfeld JW, Jr, Jacobs AK, Morrison DA, Williams DO, 2005 WRITING COMMITTEE MEMBERS. Feldman TE, Kern MJ, O'Neill WW, Schaff HV, Whitlow PL, Adams CD, Anderson JL, Buller CE, Creager MA, Ettinger SM, Halperin JL, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura R, Page RL, Riegel B, Tarkington LG, Yancy CW. 2007 Focused Update of the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: 2007 Writing Group to Review New Evidence and Update the ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention, Writing on Behalf of the 2005 Writing Committee. Circulation. 2008;117:261–295. doi: 10.1161/CIRCULATIONAHA.107.188208. [DOI] [PubMed] [Google Scholar]
- 38.Farb A, Boam AB. Stent thrombosis redux--the FDA perspective. N Engl J Med. 2007;356:984–987. doi: 10.1056/NEJMp068304. [DOI] [PubMed] [Google Scholar]
- 39.Roe MT, Chen AY, Cannon CP, Rao S, Rumsfeld J, Magid DJ, Brindis R, Klein LW, Gibler WB, Ohman EM, Peterson ED CRUSADE and ACTION-GWTG Registry Participants. Temporal changes in the use of drug-eluting stents for patients with non-ST-Segment-elevation myocardial infarction undergoing percutaneous coronary intervention from 2006 to 2008: results from the can rapid risk stratification of unstable angina patients supress ADverse outcomes with early implementation of the ACC/AHA guidelines (CRUSADE) and acute coronary treatment and intervention outcomes network-get with the guidelines (ACTION-GWTG) registries. Circ Cardiovasc Qual Outcomes. 2009;2:414–420. doi: 10.1161/CIRCOUTCOMES.109.850248. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


