Abstract
Objective:
Attention bias modification training (ABMT) is a promising treatment. Nevertheless, few studies examine its effectiveness in anxious children. This study examined the efficacy of such an ABMT protocol in pediatric anxiety.
Method:
37 anxious children were randomly assigned to one of two ABMT conditions. In the attention-towards-positive (ATP) condition, children searched 3 × 3 matrices for a happy face amongst angry faces. In the attention-training-control (ATC) condition, they searched for a bird amongst flowers. Children completed 160 trials in each of four training sessions per week for three weeks at home (1920 total trials). Clinical and attention bias measures were assessed before and after ABMT.
Results:
Children randomized to ATP showed greater post-training attention bias towards happy faces than children randomized to ATC. ATP also produced significantly greater reductions in clinician-rated diagnostic severity and number of diagnoses, compared to ATC. In the ATP group, 50% of children who completed training did not meet criteria for their principal diagnosis, compared to 8% in the ATC group.
Conclusion:
Training anxious children to focus attention on positive features of their environment may be a promising treatment.
Keywords: Attention bias, Anxiety, Attention bias modification training, Cognitive behavioural therapy
1. Introduction
Pediatric anxiety disorders are common, debilitating conditions associated with concurrent and long-term burden (Bittner et al., 2007; Verduin & Kendall, 2007). Cognitive-behavioural therapy (CBT) and selective serotonin reuptake inhibitors (SSRIs) are first-line treatments (James et al., 2006; Walkup et al., 2008). However, approximately 30–40% of treated anxious children experience continued disability, and many receive either insufficient or no treatment at all (Essau et al., 2002; Walkup et al., 2008), highlighting the need for novel interventions.
The propensity to direct attention towards threat is a robust correlate of anxiety in both child and adult populations (Bar-Haim et al., 2007), and may play a causal or maintaining role in anxiety (MacLeod et al., 2002). Recent research using attention-bias-modification-training (ABMT), which trains attention away from threat to reduce anxiety, has shown promising results in anxious adults (Hakamata et al., 2010; Amir et al., 2008, 2009). Less research examines ABMT with children, with only one clinical, and one non-clinical, controlled trial, which trained anxious children to shift attention away from threat (Bar-Haim et al., 2011; Eldar et al., 2012). While results suggested some utility, they also raised key questions. Namely, biased attention towards threat only manifests in a subset of anxious children (Eldar et al., 2012). Training some anxious children to avoid threat, such as those who enter treatment with no bias, may not be beneficial and even could exacerbate anxiety (Eldar et al., 2012; Cowart and Ollendick, 2011). By contrast, unique benefits with fewer potential adverse consequences could result from training anxious children to preferentially focus attention on positive stimuli. Dandeneau and colleagues (2007) adopted a visual-search training paradigm in which adult participants in the positive-training condition searched matrices for one smiling face embedded amongst disapproving faces. In the control condition, participants searched for one particular flower embedded among other flowers. Participants in the positive-training condition experienced significant reductions in physiological and self-report stress responses, relative to participants in the control condition. Other findings suggest that attending to rewards might minimize anxiety or stress reactivity (Johnson, 2009; Taylor et al., 2011; Wadlinger and Isaacowitz, 2008).
Building on this work (i.e., Dandeneau et al., 2007), the present study examines effects of attention training towards positive stimuli on attention biases and anxiety symptoms in pediatric anxiety disorders. In the attention-towards-positive condition (ATP), children searched picture arrays for a happy face amongst angry faces. In the attention-training-control condition (ATC), children searched for a bird amongst flowers. It was hypothesized that ATP produces an attention bias towards positive stimuli (happy faces) and away from threat (angry faces), as well as reducing diagnostic and symptom measures of anxiety, compared with ATC.
2. Materials and methods
2.1. Participants
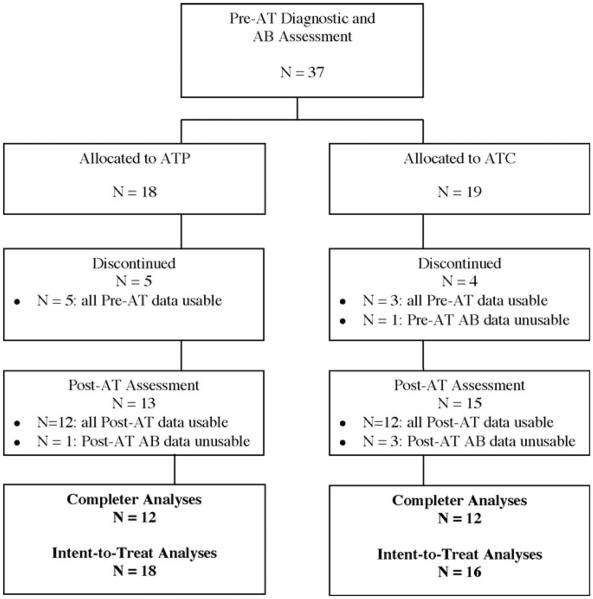
These were 37 clinically anxious children (aged 7–13 years) referred to the Griffith University Child Anxiety Research Program (see Table 1). Eighteen were randomly assigned to ATP and 19 to ATC. Intent-to-treat analyses were based on children with pre-attention training data: 18 and 16 children in the ATP and ATC groups, respectively. Completer analyses were based on children with usable data at pre- and post-attention training assessments: 12 children each in the ATP and ATC groups (see Fig. 1 for flow of participants through the study). Parents provided written informed consent for children’s participation. This study was approved by the Griffith University Human Research Ethics Committee.
Table 1.
Socio-demographic and pre-treatment diagnosis information, and satisfaction and learning ratings.
| Intent-to-treat |
Completer |
|||
|---|---|---|---|---|
| ATP (n = 18) | ATC (n = 16) | ATP (n = 12) | ATC (n = 12) | |
| Gender | ||||
| Number of females/males | 13/5 | 9/7 | 8/4 | 7/5 |
| Child’s age (in years) | 9.3 (1.20) | 9.9 (1.40) | 9.3 (1.21) | 9.7 (1.47) |
| Parental occupational status | ||||
| Mother | 4.74 (1.12) | 4.28 (1.28) | 4.69 (1.18) | 4.16 (1.19) |
| Father* | 4.61 (.80) | 3.41 (.82) | 4.69 (.82) | 3.31 (.89) |
| Marital status of parents | ||||
| % married | 77 | 75 | 92 | 83 |
| Child’s country of birth | ||||
| % Australia | 100 | 100 | 100 | 100 |
| Principal anxiety diagnosis (%) | ||||
| Generalised Anxiety Disorder | 50 | 25 | 50 | 25 |
| Separation Anxiety Disorder | 16 | 12 | 16 | 8 |
| Social Phobia | 22 | 31 | 16 | 33 |
| Specific Phobia | 11 | 31 | 16 | 33 |
| Children with more than one anxiety diagnosis (%) | 88 | 100 | 92 | 100 |
| Satisfaction ratings | ||||
| Parent | 1.40 (.96) | 1.89 (1.56) | ||
| Child | 2.00 (1.49) | 2.00 (1.05) | ||
| Learning ratings | ||||
| Parent | 1.56 (.94) | 1.00 (1.66) | ||
| Child | 2.60 (1.51) | 1.90 (1.72) | ||
Note: Standard deviations in parentheses. Parental occupational status determined by the Daniel Prestige Scale (Daniel, 1983); scores range from 1 (high) to 7 (low).
Indicates significant differences. For satisfaction and learning ratings: scale ranged from 0 (not at all) to 4 (very much), and n was 10 and 9 in ATP and ATC groups, respectively.
Satisfaction and Learning ratings were based on n = 10 for the ATP group and n = 9 forthe ATC group.
Fig. 1.
Flow diagram demonstrating the progress of participants (AB = attention bias).
2.2. Measures
2.2.1. Diagnostic assessment
Diagnostic interviews used the parent-schedule of the Anxiety Disorders Interview Schedule: Child/Parent Versions (ADIS-C-IV-C/P) (Silverman and Albano, 1996). Only children with an ADIS-C-IV-C/P clinical severity rating (CSR) of four or higher for their principal anxiety diagnosis were included. Telephone administration of the ADISC-IV-C/P was used for determining diagnostic status at all time-points to reduce the burden on families visiting the University for assessments. The ADIS-C-IV-C/P possesses good inter-rater reliability, high agreement with face-to-face administration, sound psychometric properties (Lyneham and Rapee, 2006; Silverman et al., 2001) and is commonly relied upon in treatment outcomes trials for pediatric anxiety disorders (e.g., Cobham et al., 2010; Lyneham and Rapee, 2006; Spence et al., 2006). Pre-attention training ADIS-C-IV-C/P interviews were conducted by the second author, and subsequent interviews were conducted by eight clinical psychology postgraduate students trained in the interview protocol. Inter-rater reliability was examined across 20% of the audio-taped ADIS-C-IV-C/P interviews by an independent rater, which indicated excellent reliability (principal diagnosis κ = .89; second diagnosis κ = .81; third diagnosis κ = .84).
2.2.2. Parent and child ratings
The parent- and child-report formats of the Spence Children’s Anxiety Scale (SCAS-P, SCAS-C) (Spence, 1998; Nauta et al., 2004) were utilised to assess anxiety symptoms at all time-points. Both formats contain 4-point response scales (0 = never true to 3 = always true), yielding total scores and possessing sound psychometric properties (Spence, 1998; Nauta et al., 2004). Mean SCAS-P and SCAS-C total scores of 31.8 and 32.2, respectively, have been reported for clinically anxious children (Spence, 1998; Nauta et al., 2004).
The Centre for Epidemiologic Studies Depression Scale for Children (CES-DC) is a 20-item self-report screening inventory with adequate psychometric properties; scores over 15 indicate significant depressive symptoms (Weissman et al., 1980).
2.2.3. Attention bias
The visual probe task is a well-validated method of assessing attention biases (Bar-Haim et al., 2007); the version used here is suitable for clinically anxious children (for task details see Waters et al., 2008a). Stimuli were grey-scale photographs of face-pairs from 64 actors (half female) forming 32 angry–neutral, 32 happy–neutral and 16 neutral–neutral face pairs. Each trial began with a 500 ms central fixation-cross, followed by a pair of faces (side-by-side) for 500 ms, which was replaced with an asterisk (probe) for 1100 ms in the spatial location previously occupied by one of the faces. Participants pressed one of two keys as quickly and accurately as possible, to indicate whether the asterisk appeared on the left or right. Intertrial interval varied randomly (750–1250 ms). After 10 practice trials, one block of 80 trials was presented. On critical trials with angry–neutral or happy–neutral face-pairs, the probe appeared in the same (congruent) or opposite (incongruent) location as the emotional face with equal frequency. This task was used at each assessment time-point, with a new random trial-order for each child and assessment.
2.2.4. Attention bias modification training
The ATP and ATC tasks were based on Dandeneau et al. (2007) and programmed in Java. For ATP, stimuli were colour-pictures of 16 angry and 16 happy faces (half female) from the NimStim set (Tottenham et al., 2009). Each happy face was presented 10 times, and each angry face presented 80 times across trials, balanced across the different positions in the 3 × 3 matrix. This yielded 160 training trials (two blocks of 80 trials). Children had to mouse-click on the happy face within the 3 × 3 matrix of angry faces as quickly and as accurately as possible. The matrix disappeared after the child mouse-clicked on the correct face and the next trial began. For ATC, stimuli were 20 colour-pictures of individual birds and flowers used in prior visual-search tasks with children (Waters and Lipp, 2008). Children mouse-clicked on the bird presented amongst flowers as quickly and accurately as possible. Other task parameters were similar to the ATP task (i.e., 160 training trials). No performance feedback was given in either condition. Participants completed the assigned attention-training task four times a week for three weeks (i.e. twelve sessions), yielding 1920 trials.
2.2.5. Satisfaction and learning ratings
Children and parents rated how much they learnt and were satisfied with attention training using response scales (0 = not at all to 4 = very much).
2.3. Procedure
An initial telephone screening interview addressing inclusion/exclusion criteria was conducted with parents of referred children. Parents were informed that the study involved two sequentially administered treatment phases: (1) an initial, at-home computer-based treatment over 3 weeks designed to help children control their attention, which was followed by (2) group-based cognitive-behavioural therapy (CBT) over 10 weeks. Parents (usually mothers) of eligible children then completed the ADIS-C-IV-C/P by telephone with the second author. The parent and child then attended an assessment session at the university where they parents signed consent forms, children completed the visual-probe task, and both parents and children completed questionnaires.
Children were then randomly assigned to ATP or ATC. Both children and parents were blind to group assignment. Between 5 and 10 children (across both training groups) started attention training at the same time, transitioning through all stages of the study at a similar rate. This design enabled enrolment into group-based treatment, following training. Families were mailed a CD with the relevant training task, with follow-up by telephone to ensure it was working correctly. Participants emailed the output files generated by the task at the end of each week and a follow-up call was made if files were not received the following week. Children completed a minimum of 10/12 training sessions.
Within two weeks after completing attention training, parents completed the ADIS-C-IV-C/P by telephone with a clinical psychology postgraduate student blind to the child’s pre-training diagnoses and assigned group. Families returned to the university to complete the post-attention training questionnaires and visual-probe task. All assessments were completed within 2–4 weeks after attention training which did not differ between groups.
All children were subsequently offered group CBT (e.g., Waters et al., 2008b, 2009) following attention training to ensure all children received first-line treatment. However, analyses of treatment outcomes post-CBT as a function of attention training group were not adequately powered due to attrition by the post-CBT assessment.
2.4. Data screening, response definitions and data analysis
2.4.1. Attention bias
Response times (RTs) from trials with incorrect responses and outliers (<200 ms or >3 SDs above each participant’s mean) were excluded. Attention bias scores were calculated separately for each assessment and face type; e.g., happy bias scores were calculated from data from trials with happy–neutral face pairs, by subtracting the average RT on happy-congruent trials (probe replaced happy face) from that on happy-incongruent trials (probe replaced neutral face of happy–neutral pair). Bias scores were similarly calculated for angry faces. Positive scores indicate attention towards happy (or angry) relative to neutral faces.
2.4.2. Data analysis
Completer analyses were based on children who completed assessments at pre- and post-attention training, defined as completing at least 10/12 attention training sessions and had diagnostic, symptom and attention bias measures available at pre- and post-attention training (i.e., n = 12 each in the ATP and ATC group). For intent-to-treat analyses, the last-point-carried-forward method was used to deal with missing data at the next assessment time-point (see Fig. 1) (Lyneham and Rapee, 2006). Therefore, pre-attention training assessment data was carried forward for participants who discontinued treatment but had diagnostic, symptom and attention bias data available at the pre-attention training assessment. Analyses used Fisher exact tests, independent samples t-tests and mixed factorial analyses of variance (ANOVA). Post hoc comparisons used Bonferroni adjustments and is reported for effect sizes.
3. Results
3.1. Comparisons of children who dropped-out versus completed treatment
Analyses comparing demographic, diagnostic, symptom and attention bias measures among the 9 children who did not, and the 24 children who did, complete treatment revealed one significant difference; children who dropped out had fewer anxiety diagnoses on average (M = 2.5; SD = .88) than completers (M = 3.9; SD = 1.7), t(31) = 5.31, p = .025. Non-completers tended to be more likely to have unmarried parents (44%) compared to completers (13%), p = .068 (Fisher’s exact test, two-tailed). Of those who dropped out, there was no significant difference in number allocated to ATP (n = 5) or ATC (n = 4) groups, p = 1.00 (Fisher’s exact test, two-tailed).
3.2. Pre-treatment group comparisons
For intent-to-treat and completer analyses, initial pre-treatment comparisons of ATP and ATC groups showed no significant group differences in demographic or clinical measures (ts < 1.31), with one exception. Treatment groups unexpectedly differed in fathers’ occupational status (intent-to-treat: t(32) = 4.91, p < .001; completer: t(22) = 3.83, p < .001), but not mothers’ occupational status (both t < 1.12). Fathers of children in the ATC group had lower status than in the ATP group (Table 1). However, analyses conducted with father’s occupational status used as a covariate revealed no significant effects from the covariate on outcomes and are not reported further.
3.3. Attention bias
For intent-to-treat and completer analyses, the 2 (Time) × 2 (Face-Valence) × 2 (Attention-Training Group) mixed factorial ANOVA of bias scores revealed significant Time × Face-Valence × Group interactions, F(1, 32) = 4.09, p = .05, and F(1, 22) = 4.39, p = .048, respectively (Fig. 2), indicating that ATP increased attention to happy faces. The groups did not differ in pre-training attention biases for angry or happy faces (ps > .5). However, the ATP group showed significantly larger attention bias towards happy faces post-training compared not only with pre-training, but also with post-training happy-face biases of the ATC group (all ps < .05). In completer analyses, the ATP group’s post-training bias towards happy faces was significantly larger than their post-training bias for angry faces (p = .011).
Fig. 2.
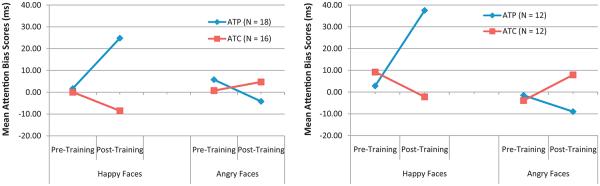
Mean attention bias scores for happy and angry faces from pre- to post-attention training for intent-to-treat analyses (left panel) and completer analyses (right panel).
3.4. Clinical outcome measures
3.4.1. Diagnostic assessment
The completer analyses of principal diagnosis severity ratings (ADIS-C-IV-C/P CSRs) showed significant main effects of Time (F(1, 22) = 14.55, p < .001, ), and Group (F(1, 22) = 4.98, p = .036, ), which were qualified by a significant Time × Group interaction (F(1, 22) = 11.85, p = .002, ) (Table 2). This reflected significant reduction in CSRs from pre- to post-training in the ATP group (p = .001) but not the ATC group (p = .80). Furthermore, post-training CSRs were significantly lower in the ATP than ATC group (p = .004). Effects were the same in intent-to-treat analyses: significant Time main effect (F(1, 32) = 9.60, p = .004, ), Group main effect (F(1, 32) = 5.10, p = .03, ) and Time × Group interaction (F(1, 32) = 7.62, p = .009, ).
Table 2.
Diagnostic and symptom measures as a function of group at pre- and post-attention training (AT).
| Measure | Pre-AT |
Post-AT |
Pre-AT |
Post-AT |
||||
|---|---|---|---|---|---|---|---|---|
| Intent-to-treat |
Completer |
|||||||
| ATP (n = 18) | ATC (n = 16) | ATP (n = 18) | ATC (n = 16) | ATP (n = 12) | ATC (n = 12) | ATP (n = 12) | ATC (n = 12) | |
| Diagnostic severity | ||||||||
| M | 6.22 | 6.19 | 4.06 | 6.06 | 6.42 | 6.08 | 3.17 | 5.12 |
| SD | .88 | 1.37 | 2.41 | 1.57 | .79 | 1.50 | 2.44 | .73 |
| Number diagnoses | ||||||||
| M | 3.77 | 3.75 | 2.05 | 3.12 | 4.5 | 3.66 | 1.91 | 2.83 |
| SD | 1.76 | 1.65 | 1.47 | 1.66 | 1.67 | 1.55 | 1.72 | 1.46 |
| SCAS-P total | ||||||||
| M | 30.72 | 31.25 | 28.78 | 26.75 | 32.25 | 30.08 | 39.33 | 24.08 |
| SD | 12.35 | 9.76 | 11.97 | 8.89 | 11.47 | 9.40 | 11.14 | 6.42 |
| SCAS-C total | ||||||||
| M | 41.94 | 38.94 | 29.66 | 37.33 | 43.42 | 38.25 | 25.88 | 36.50 |
| SD | 19.23 | 15.02 | 13.24 | 20.10 | 18.31 | 14.09 | 8.35 | 19.81 |
| CES-DC total | ||||||||
| M | 19.00 | 18.31 | 18.11 | 12.81 | 20.08 | 18.50 | 18.75 | 11.17 |
| SD | 11.21 | 9.44 | 12.32 | 6.77 | 8.82 | 10.50 | 10.97 | 6.29 |
Note: Diagnostic severity = ADIS-C-IV-P clinical severity rating 0 (low)–8 (high); SCAS-P; SCAS-C = Spence Children’s Anxiety Scale, Parent; Child; CES-DC = Centre for Epidemiological Studies – Depression Scale for Children; Satisfaction-P; -C; Learning-P; -C ratings = 0 (not at all) – 4 (very much).
Completer analyses of the average number of diagnoses for which children met criteria revealed a significant main effect of Time, F(1, 22) = 47.29, p < .001, , and significant Time × Group interaction, F(1, 22) = 12.41, p = .002, . Although both groups experienced a reduction in mean number of diagnoses at post- compared to pre-training (both p < .027), the ATP group had significantly fewer diagnoses at post-training than the ATC group (p = .042). Similar effects were observed in intent-to-treat analyses: significant Time main effect (F(1, 32) = 24.33, p < .001, ) and Time x Group interaction (F(1, 32) = 5.32, p = .028, ) (Table 2).
Furthermore, more children in the ATP group no longer met diagnostic criteria for their principal anxiety diagnosis at post-attention-training, compared with the ATC group (completer analyses: 50% in ATP group versus 8% in ATC group, p = .034, Fisher’s exact test, one-tailed; intent-to-treat analyses: 33% versus 6%, respectively, p = .045, Fisher’s exact test, one-tailed).
3.4.2. Parent and child ratings
Anxiety scores reduced significantly in both groups from pre- to post-training; i.e., significant main effects of Time on SCAS-P and SCAS-C in completer analyses: (F(1, 22) = 6.18, p < .02, ) and (F(1, 22) = 15.73, p < .001, ) respectively; and intent-to-treat analyses: (F(1, 32) = 6.11, p < .019, ) and (F(1, 32) = 13.84, p < .001, ). Similarly, reduction in CES-DC scores from preto post-training was significant in the intent-to-treat analyses (F(1, 32) = 4.05, p < .05, ) and marginal in completer analyses (F(1, 22) = 3.06, p < .06, ). However, unlike for clinician ratings, treatment did not impact parent or child ratings (Group main effects and Time x Group interactions, all F < 2.54, ns).
3.4.3. Associations between symptom measures and attention bias
Zero-order correlations based on the whole sample (ATP and ATC groups combined) using completer analyses showed that lower post-training ADIS-C-IV-C/P CSRs (i.e. better treatment outcomes) were significantly associated with lower post-training attention bias towards angry faces (r = .47, p = .02), and marginally with greater post-training attention bias towards happy faces (r = −.37, p = .07). The intent-to-treat analyses found the same marginal association between post-training CSRs and attention biases towards happy faces (r = −.31, p = .07), but no significant effects for angry faces (r = .27, p = .12). Correlations in each group separately were not significant.
3.4.4. Moderated-mediation analyses
Results are presented in Table 3. There were significant main effects on change in principal diagnosis CSRs due to change in attention bias scores for happy faces (p = .01), and angry faces (p = .05) and due to attention training group (p = .002). Other results from these supplementary analyses were not significant; e.g., no evidence of interactions between attention training group and change in attention bias scores for happy and angry faces in predicting change in principal diagnosis CSRs (see Table 3). However, it should be noted that statistical power is limited on these analyses due to the small sample size, particularly for tests of interactions.
Table 3.
Predicting change in principal diagnosis CSRs after attention training using attention training group and change in attention bias scores for angry and happy faces as predictors. Coefficients (standard errors) and t-values are reported. ATG-ΔAB: Relation between attention training condition and change in attention bias score; ΔAB-ΔCSR: Relation between change in attention bias score and change in ADIS-C-IV-P CSRs; ATG-ΔCSR: effect of attention training condition on change in ADIS-C-IV-P CSRs; ATG × ΔAB-ΔCSR: interaction of attention training condition and change in attention bias scores on change in ADIS-C-IV-P CSRs.
| ATG-ΔAB |
ΔAB-ΔCSR |
ATG-ΔCSR |
ATG × ΔAB-ΔCSR |
|||||
|---|---|---|---|---|---|---|---|---|
| β (SE) | t | β (SE) | t | β (SE) | t | β (SE) | t | |
| Angry faces | −.45 (.41) | −1.11 | .41 (.20) | 2.08* | 1.16 (.34) | 3.44** | −.19 (.35) | −.56 |
| Happy faces | −.80 (.39) | −1.92+ | −.50 (.18) | −2.74** | 1.16 (.34) | 3.44** | .93 (.34) | −1.24 |
p = .05.
p < .05.
p = .06.
3.5. Satisfaction and learning
There were no group differences on parent- or child-reported satisfaction and learning following treatment, all t < .97, ns (Table 1).
4. Discussion
This study examined the efficacy of attention bias modification treatment in pediatric anxiety. Anxious children were trained to attend to positive stimuli. Completer and intent-to-treat analyses confirmed that this training induced an attention bias towards positive stimuli, relative to neutral stimuli, and also impacted clinical status. Specifically, ATP produced significant clinical improvement, as indicated by independent clinician-ratings of diagnoses: i.e., there were significantly greater reductions in diagnostic severity ratings and number of diagnoses in the ATP than ATC group; with 50% of children receiving ATP no longer met criteria for their principal diagnosis at post-training, compared to 8% in the ATC group. These rates are similar to those in the only other ABMT study of pediatric anxiety disorders (Eldar et al., 2012). That earlier study, unlike the current one, pre-selected children with attention bias towards threat and trained them to avoid threat. This may have minimized any potential adverse effect of training children, who do not have a pre-existing threat bias, to avoid threats.
The present study demonstrated that the anxiety-reducing effects of attention training towards positive stimuli were not due to general training in attention control regardless of valence (Eldar et al., 2012; Dandeneau et al., 2007); as clinical benefits were not observed in the ATC group. This control group required the same search strategy as the ATP group but for a non-affective target (i.e., a bird amongst flowers). Rather, searching for a happy face amongst angry expressions produced a valence-specific attention bias towards happy faces, that was demonstrated with a different set of happy (relative to neutral) faces in a visual-probe task, suggesting generalisation of training effects to different stimulus contexts and attention demands.
This study provides some evidence of therapeutic efficacy of ATP. However, the study did not generate clear insights on the mechanism by which ATP changes clinical symptoms or attention towards happy faces amongst angry distracters. ABMT is usually credited with reducing anxiety by redirecting attention from threat to non-threat cues (Hakamata et al., 2010). Indeed, Dandeneau et al. (2007) found that improved self-esteem was associated with reduced attention bias for disapproving/rejection faces which served as distracter stimuli during visual search training for smiling target faces. The different findings in the current study, in Dandeneau et al. (2007) and in prior studies using threat-related training could arise from the many differences among these studies. These include differences both in methodology (e.g., angry vs. disapproving distracter faces) and/or sample characteristics (self-esteem vs. anxiety; adults vs. children). Nevertheless, the present study showed improved attention bias towards happy faces across different stimuli and task demands. This could suggest that improved control of attention on positive stimuli contributed to the observed clinical benefits of ATP as a direct effect of inducing a positive attention bias, and possibly through effects on attention to threats. Although the moderated-mediation analyses did not show an interaction effect of attention training group and change in attention biases on change in symptom severity, statistical power on these analyses is limited by the small sample size. Given that threat attention biases may not be uniformly observed in anxious children (e.g., Eldar et al., 2012), training that encourages anxious children to preferentially attend to positive information in their environment may have distinct clinical benefits over other training procedures aimed at removing threat-related biases. Additional studies are needed to elucidate the underlying mechanisms of attention training towards positive stimuli.
Despite expected reductions in clinician-derived indices of anxiety, there was no ATP effect on parent- or child-report measures. Similar effects were observed in Eldar et al. (2012), where efficacy manifest only on clinician-rated but not parent or child-rated anxiety. Null results should be interpreted cautiously given small sample sizes. Nevertheless, one possibility is that clinicians possess unique expertise, relative to children and parents, when recognising signs of clinical improvement. The primacy of clinician-ratings in prior treatment trials of pediatric anxiety recognizes this possibility (Walkup et al., 2008). Such superiority could arise if parent and self-report measures were more vulnerable to expectancy or other aspects of control treatment (Eldar et al., 2012). This may be relevant here, because all families knew CBT, a treatment known to be effective, would follow attention training. Also, because ADIS-C-IV-C/P clinician-severity ratings take into account improvements in functional interference (Silverman and Albano, 1996), they may be more sensitive than the symptom measures to improvements which may have been associated with ATP, such as engagement in activities that previously caused distress. Further studies with larger sample sizes are required to clarify these alternative explanations.
Satisfaction and learning ratings were low to average and did not differ between groups. Other studies report high ABMT acceptance rates by youths and parents (Cowart and Ollendick, 2011; Rozenman et al., 2011). In the present study, attention training was conducted at home with no therapist contact; whereas in prior studies, between 25 and 100% of attention training was conducted in-session with a therapist, with emphasis on general rapport-building and treatment progress (Eldar et al., 2012; Cowart and Ollendick, 2011; Rozenman et al., 2011). Acceptability of the current approach could be improved through therapist-initiated phone contact during home-based training, which studies of rural children found enhanced outcomes (Lyneham and Rapee, 2006). Moreover, that all families were awaiting CBT after attention training could have influenced these ratings.
This study had limitations, most notably, the small sample size, which limits generalisability and requires replication of findings. The study employed face stimuli rather than tailoring training stimuli to children’s concerns (Hakamata et al., 2010), which could have attenuated outcomes and limited generalisability to other affective stimuli. Also, different classes of stimuli were used in the ATP and ATC conditions (i.e., human faces vs. plants and animals). While the use of such stimuli is comparable with prior research using visual search attention training paradigms (e.g., Dandeneau et al., 2007, used faces and flowers in active training and control conditions, respectively), it may raise questions of whether the findings could be explained by an artefact related to non-affective differences between the stimuli (e.g. searching for a human vs. animal target, or for a face vs. full-bodied creature target; or to a difference in the distracting effect of background human faces vs. plants). While these questions cannot be resolved by the present data, it should be noted that there are no strong theoretical grounds for predicting that such non-affective differences in stimuli would explain the observed reduction in clinical anxiety, or the increased attention bias to happy faces (whereas there are strong theoretical grounds for predicting that such changes are due to the affective content of the training stimuli) This study also included children with mixed anxiety diagnoses. Although this is current practice due to high rates of comorbidity (Rapee et al., 2009), it prevented examination of disorder-specific effects. Finally, other studies have found promising effects with between 1 and 4 sessions (Amir et al., 2008; Eldar et al., 2012). Fewer training sessions would have eased the burden on families.
Nevertheless, this study applied a novel treatment with anxious children by training them to direct attention to positive stimuli. This was conducted solely in the home with minimal therapist contact. This form of attention training produced an attention bias towards happy faces and enhanced remission rates relative to a control condition. Future research is needed to replicate these findings and to elucidate the mechanisms underlying this form of attention training.
Acknowledgement
The Australian Research Council Grant DP1095536 supported this research.
Footnotes
Conflict of interest
The authors declare no financial interests or conflicts of interest.
References
- Amir N, Weber G, Beard C, Bomyea J, Taylor CT. The effect of a single-session attention modification program on response to a public-speaking challenge in socially anxious individuals. Journal of Abnormal Psychology. 2008;117:860–868. doi: 10.1037/a0013445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir N, Beard C, Burns M, Bomyea J. Attention modification program in individuals with generalized anxiety disorder. Journal of Abnormal Psychology. 2009;118:28–33. doi: 10.1037/a0012589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, van Ijzendoorn MH. Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychological Bulletin. 2007;133:1–24. doi: 10.1037/0033-2909.133.1.1. [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y, Morag I, Glickman S. Training anxious children to disengage attention from threat: a randomized controlled trial. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2011;52:861–869. doi: 10.1111/j.1469-7610.2011.02368.x. [DOI] [PubMed] [Google Scholar]
- Bittner A, Egger HL, Erkanli A, Costello E, Foley DL, Angold A. What do childhood anxiety disorders predict? Journal of Child Psychology and Psychiatry and Allied Disciplines. 2007;48:1174–1183. doi: 10.1111/j.1469-7610.2007.01812.x. [DOI] [PubMed] [Google Scholar]
- Cobham VE, Dadds MR, Spence SH, McDermott B. Parental anxiety in the treatment of childhood anxiety: a different story three years later. Journal of Clinical Child and Adolescent Psychology. 2010;39(3):410–420. doi: 10.1080/15374411003691719. [DOI] [PubMed] [Google Scholar]
- Cowart MJW, Ollendick TH. Attention training in socially anxious children: a multiple baseline design analysis. Journal of Anxiety Disorders. 2011;25:972–977. doi: 10.1016/j.janxdis.2011.06.005. [DOI] [PubMed] [Google Scholar]
- Dandeneau SD, Baldwin MW, Baccus JR, Sakellaropoulo M, Pruessner JC. Cutting stress off at the pass: reducing vigilance and responsiveness to social threat by manipulating attention. Journal of Personality and Social Psychology. 2007;93:651–666. doi: 10.1037/0022-3514.93.4.651. [DOI] [PubMed] [Google Scholar]
- Daniel AE. Power, Privilege and Prestige. Longman Cheshire; Melbourne, Australia: 1983. [Google Scholar]
- Eldar S, Apter A, Lotan D, Perez-Edgar K, Naim R, Fox NA, Pine DS, Bar-Haim Y. Attention bias modification treatment for pediatric anxiety disorders: a randomized control trial. American Journal of Psychiatry. 2012;169:213–230. doi: 10.1176/appi.ajp.2011.11060886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essau CA, Conradt J, Petermann F. Course and outcome of anxiety disorders in adolescents. Journal of Anxiety Disorders. 2002;16:67–81. doi: 10.1016/s0887-6185(01)00091-3. [DOI] [PubMed] [Google Scholar]
- Hakamata Y, Lissek S, Bar-Haim Y, Britton JC, Fox N, Leibenluft E, Ernst M, Pine DS. Attention bias modification treatment: a meta-analysis towards the establishment of novel treatment for anxiety. Biological Psychiatry. 2010;68:982–990. doi: 10.1016/j.biopsych.2010.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James A, Soler A, Weatherall R. Cognitive behavioural therapy for anxiety disorders in children and adolescents. The Cochrane Library. 2006;1:1–25. doi: 10.1002/14651858.CD004690.pub2. [DOI] [PubMed] [Google Scholar]
- Johnson DR. Goal-directed attentional deployment to emotional faces and individual differences in emotion regulation. Journal of Research in Personality. 2009;43:8–13. [Google Scholar]
- Lyneham HJ, Rapee RM. Evaluation of therapist-supported parent-implemented CBT for anxiety disorders in rural children. Behaviour Research and Therapy. 2006;44:1287–1300. doi: 10.1016/j.brat.2005.09.009. [DOI] [PubMed] [Google Scholar]
- MacLeod C, Rutherford E, Campbell L, Ebsworthy G, Holker L. Selective attention and emotional vulnerability: assessing the causal basis of their association through the experimental manipulation of attentional bias. Journal of Abnormal Psychology. 2002;111:107–123. [PubMed] [Google Scholar]
- Nauta MH, Scholing A, Rapee R, Abbott M, Spence SH, Waters AM. Parent-report measure of children’s anxiety: psychometric properties and comparison with child-report in clinical and normal samples. Behaviour Research and Therapy. 2004;42:413–439. doi: 10.1016/S0005-7967(03)00200-6. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Schniering C, Hudson JL. Anxiety disorders during childhood and adolescents: origins and treatment. Annual Review of Clinical Psychology. 2009;5:311–341. doi: 10.1146/annurev.clinpsy.032408.153628. [DOI] [PubMed] [Google Scholar]
- Rozenman M, Weersing R, Amir N. A case series of attention modification in clinically anxious youths. Behaviour Research and Therapy. 2011;49:324–330. doi: 10.1016/j.brat.2011.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Versions. The Psychological Corporation; San Antonio, USA: 1996. [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with the Anxiety Disorders Interview Schedule for DSM-IV: child and parent versions. Journal of the American Academy of Child Psychiatry. 2001;40:937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Spence SH. A measure of anxiety symptoms among children. Behaviour Research and Therapy. 1998;36:545–566. doi: 10.1016/s0005-7967(98)00034-5. [DOI] [PubMed] [Google Scholar]
- Spence SH, Holmes JM, March S, Lipp OV. The feasibility and outcome of clinic plus internet delivery of cognitive-behavior therapy for childhood anxiety. Journal of Consulting and Clinical Psychology. 2006;74:614–621. doi: 10.1037/0022-006X.74.3.614. [DOI] [PubMed] [Google Scholar]
- Taylor CT, Bomyea J, Amir N. Malleability of attentional bias for positive emotional information and anxiety vulnerability. Emotion. 2011;11:127–138. doi: 10.1037/a0021301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tottenham N, Tanaka J, Leon AC, McCarry T, Nurse M, Hare TA, Marcus DJ, Westerlund A, Casey BJ, Nelson C. The NimStim set of facial expressions: judgments from untrained research participants. Psychiatry Research. 2009;168:242L 9. doi: 10.1016/j.psychres.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verduin TL, Kendall P. Peer perceptions and liking of children with anxiety disorders. Journal of Abnormal Child Psychology. 2007;36:459–469. doi: 10.1007/s10802-007-9192-6. [DOI] [PubMed] [Google Scholar]
- Wadlinger HA, Isaacowitz DM. Looking happy: the experimental manipulation of a positive visual attention bias. Emotion. 2008;8:121–126. doi: 10.1037/1528-3542.8.1.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. New England Journal of Medicine. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters AM, Lipp OV. The influence of animal fear on attentional capture by fear-relevant animal stimuli in children. Behaviour Research and Therapy. 2008;46:114–121. doi: 10.1016/j.brat.2007.11.002. [DOI] [PubMed] [Google Scholar]
- Waters AM, Mogg K, Bradley BP, Pine DS. Attentional bias for emotional faces in children with generalized anxiety disorder. Journal of the American Academy of Child Psychiatry. 2008a;47:435–442. doi: 10.1097/CHI.0b013e3181642992. [DOI] [PubMed] [Google Scholar]
- Waters AM, Wharton TA, Zimmer-Gembeck MJ, Craske MG. Threat-based cognitive biases in anxious children: comparison with non-anxious children before and after cognitive-behavioural treatment. Behaviour Research and Therapy. 2008b;46(3):358–374. doi: 10.1016/j.brat.2008.01.002. [DOI] [PubMed] [Google Scholar]
- Waters AM, Ford LA, Wharton TA, Cobham VE. Cognitive behavioural therapy for young children with anxiety disorders: comparison of group-based child + parent versus parent only focused treatment. Behaviour Research and Therapy. 2009;47:654–662. doi: 10.1016/j.brat.2009.04.008. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Orvaschel H, Padian N. Children’s symptom and social functioning self-report scales: comparison of mothers’ and children’s reports. Journal of Nervous and Mental Disease. 1980;168:736–740. doi: 10.1097/00005053-198012000-00005. [DOI] [PubMed] [Google Scholar]