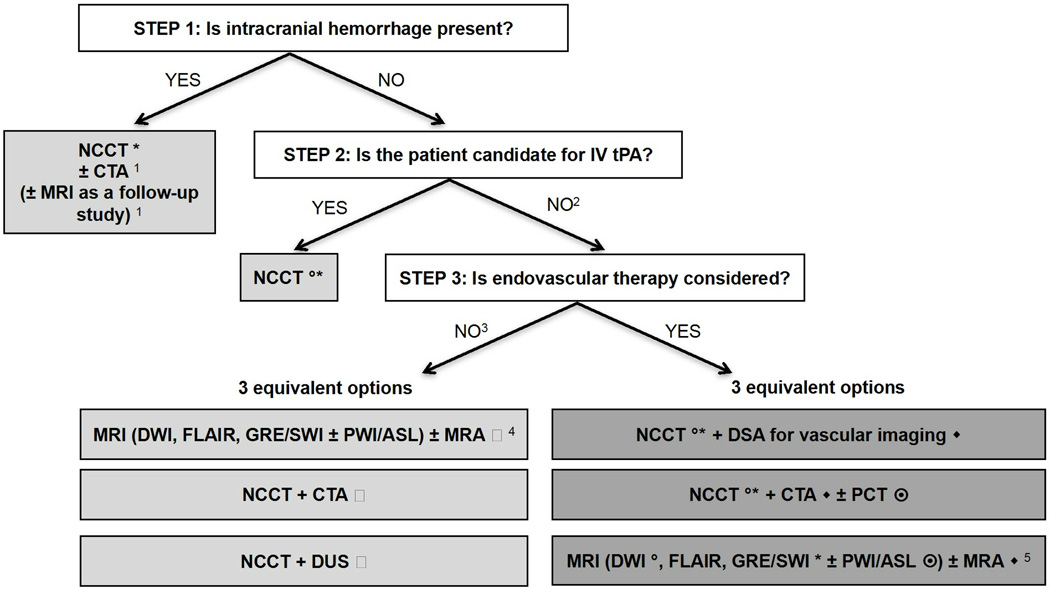
Figure 1. Suggested imaging protocols for patients presenting with acute stroke symptoms based on the clinical scenario and the therapeutic options considered and available.
Each of the gray boxes represents one imaging strategy. In order not to delay treatment, a standardized imaging approach should be used: one imaging strategy (gray box) should be selected and all imaging studies belonging to this strategy should be performed upfront in as few sessions as possible.
1 To assess the etiology of the intracranial hemorrhage (CTA for vascular pathologies, such as aneurysms, arteriovenous malformations, vasculopathies; MRI for vascular malformations, neoplastic and other pathologies associated with hemorrhage)
2 Also if the patient is not a candidate for IV tPA (contraindication to tPA, outside time window for tPA) or if IV tPA failed or it is thought that it may fail.
3 For patients who are outside the time window for acute reperfusion therapies (> 4.5 hours at sites where only IV tPA is being considered; > 8 hours at sites where endovascular therapy is considered), and for patients with TIAs, emphasis is on secondary prevention, and their imaging work-up should be focused on vascular imaging (CTA, MRA of DUS) to assess carotid arteries as a possible cause of the ischemic stroke, with secondary prevention in mind. If MRA is obtained, it makes sense to concurrently obtain MRI with DWI, FLAIR and GRE/SWI. Echocardiography should also be obtained to assess for cardiac sources.
4 If available, MRI/MRA is the preferred imaging modality for TIA patients.
5 At institutions where MRI is available 24/7 and can be performed within a short time after admission.
* to assess for intracranial hemorrhage
◦ to assess the extent of ischemic core
◆ to assess the location and extent of the intravascular clot
to assess carotid atherosclerotic disease
to assess the extent of viable tissue