Abstract
Background
Impairments in psychosocial status and cognition relate to poor clinical outcomes in patients with atrial fibrillation (AF). However, how often these conditions co-occur and associations between burden of psychosocial and cognitive impairment and quality of life (QoL) have not been systematically examined in patients with AF.
Methods
218 patients with symptomatic AF were enrolled in a prospective study of AF and psychosocial factors between 5/2013 – 10/2014 at the University of Massachusetts Medical Center. Cognitive function, depression and anxiety were assessed at baseline and AF-specific QoL was assessed 6 months after enrollment using validated instruments. Demographic and clinical information were obtained from a structured interview and medical record review.
Results
The mean age of the study participants was 63.5 ± 10.2 years, 35% were male, and 81% had paroxysmal AF. Prevalence of impairment in 1, 2, or 3 psychosocial/cognitive domains (e.g., depression, anxiety, or cognition) was 75 (34.4%), 51 (23.4%), and 16 (7.3%), respectively. Patients with co-occurring psychosocial/cognitive impairments (e.g., >1 domain) were older, more likely to smoke, had less education, and were more likely to have heart failure (all p<0.05). Compared to participants with no psychosocial/cognitive impairments, AF-specific QoL at six months was significantly poorer among participants with baseline impairment in two (B=−13.6, 95%CI −21.7, −5.4) or three (B=−15.1, 95%CI −28.0, −2.2) psychosocial/cognitive domains.
Conclusion
Depression, anxiety, and impaired cognition were common in our cohort of patients with symptomatic AF and often co-occurred. Higher burden of psychosocial/cognitive impairment was associated with poorer AF-specific QoL.
Keywords: Atrial fibrillation, psychosocial impairment, cognitive impairment, multimorbidity, quality of life
Introduction
Atrial fibrillation (AF) is the most common sustained heart rhythm abnormality, affecting approximately 3–6 million U.S. adults, including almost 1 in 20 people over age 60.1,2 Owing to the aging of the U.S. population, the number of people diagnosed with AF is expected to more than double by the year 2050.1,3 The increasing prevalence of AF has significant personal, clinical, and socioeconomic implications,4 in part due to the fact that patients with AF often also have anxiety, depression, and cognitive impairment or dementia, even in the absence of ischemic stroke.5,6
Impairments in mood or cognition exert powerful and negative impacts on the prognosis of AF patients.6–9 Specifically, depression and anxiety are associated with poorer AF outcomes, including higher AF recurrence rates, higher mortality rates, worse symptom severity, and greater healthcare utilization.6–9 Patients with AF who are affected by cognitive impairment have poorer anticoagulation adherence, more frequent adverse cardiovascular events, and show greater functional impairment compared to non-impaired AF patients.10
Although individually harmful, psychosocial and/or cognitive impairments may in fact confer even poorer outcomes when they occur together, and evidence suggests that these impairments frequently cluster.11 For example, anxiety and depression often co-occur in the general population,11 and their combined presence negatively impacts important health outcomes, including somatic symptomatology, treatment response, and suicidality.11,12 Studies also show that patients with even mild cognitive impairment are vulnerable to mood disorders, including depression.13 Data also show that psychosocial and cognitive impairments cluster in patients with coronary artery disease, in whom anxiety and depression occur together commonly,14–16 and in whom the combination of anxiety and depression confers a higher risk for worse cardiovascular outcomes than either anxiety or depression alone.15,16
Despite work highlighting the profound impact of either depression, anxiety, or cognitive impairment individually on the long-term prognosis of patients with AF and data showing clustering of psychosocial and cognitive comorbidities in patients with other forms of cardiovascular disease,6–9,14,16 we know little about patterns of co-occurrence in AF patients, their joint influence on AF-related quality of life (QoL), or patient factors associated with a greater burden of psychosocial and cognitive impairments. To address these knowledge gaps, we conducted the present analysis using data from InRhythm, a prospective study of psychosocial and cognitive factors in AF.
Methods
Study Sample
The InRhythm study is a prospective study of AF and its relationship to psychosocial and cognitive impairment. Participants with symptomatic AF were recruited and followed at one of three ambulatory clinics associated with the University of Massachusetts Medical Center (UMMC) AF Treatment Clinic (Heywood Hospital, Marlborough Hospital, and the UMMC University Campus). The present analysis includes 218 InRhythm participants with symptomatic AF and available clinical, psychosocial, cognitive and quality of life data. All participants gave informed consent, and all InRhythm protocols were approved by the University of Massachusetts Medical School Review Board.
Data abstraction
All InRhythm study participants underwent a history, physical examination, and laboratory evaluation as part of their routine clinical evaluation for AF. The demographic, clinical, and treatment characteristics of InRhythm participants were abstracted from the electronic medical record by trained study staff. Information abstracted from the medical record included information about participant’s age, sex, race, type of AF, cardiovascular comorbidities (e.g., myocardial infarction, diabetes, hypertension, and heart failure), non-cardiovascular comorbidities (e.g., anemia, renal failure), and prior antiarrhythmic drug exposure status. Participants were classified as having AF if the arrhythmia was present on a 12-lead electrocardiogram obtained during an AF Treatment Center clinic visit or an encounter with an outside health care provider, on a Holter or cardiac event monitor, or if AF was noted in any hospital record.
Cognitive function
Global cognitive function was assessed using the Montreal Cognitive Assessment Battery (MoCA).17 The MoCA is a 10-minute, 30-item screening tool that was designed to assist physicians in detecting mild cognitive impairment (CI). The MoCA is the currently recommended screening test for CI in patients with cardiovascular disease by the National Institute for Neurologic Disorders and Stroke and the Canadian Stroke Institute.18 A cutoff score of 27 (range 0–30) has been shown to have a high sensitivity (0.90) and specificity (0.87) for detecting mild CI, and was used as a cutoff to define cognitive impairment (scores of 26 and below were ‘impaired’).17
Depression
Depression was assessed using the 9-item version of the Patient Health Questionnaire (PHQ-9).19 Using a cut-point range of ≥10 (range = 0–27), the PHQ-9 has high sensitivity (0.88) and specificity (0.88) for detecting major depression.20
Anxiety
Anxiety was assessed using the Generalized Anxiety Disorder-7 scale (GAD-7), a revised version of the anxiety module from the Patient Health Questionnaire which consists of DSM-IV criteria for generalized anxiety disorder over the past 2 weeks.19 The GAD-7 score ranges from 0–27 with a score ≥10 having high sensitivity (0.89) and specificity (0.82) for psychiatrist-diagnosed anxiety disorder.21
Atrial Fibrillation Related Quality of Life
Disease specific QoL was measured during a clinic visit using the Atrial Fibrillation Effect on QualiTy-of-Life (AFEQT) Questionnaire, which includes sub-scales for symptom severity, global well-being, AF burden, and impact on healthcare utilization.22 The AFEQT questionnaire consists of 20 questions separated into 4 domains: symptoms, treatment concerns, daily activities, and treatment satisfaction. Each question is graded on a 1–7 point scale, and the total raw score is transformed to a 0–100 scale, with 100 points indicating the best possible AF-related QoL and 0 points indicating the poorest possible AF-related QoL. AFEQT scores correlate to severity of physical symptoms from AF22 and health-care utilization.23
Statistical analyses
We compared the characteristics of InRhythm participants according to number of psychosocial and cognitive comorbidities (count of anxiety, depression and cognitive impairment; range = 0–3) and compared baseline patient characteristics by number of comorbidities using ANOVA for continuous variables and the χ2-test for categorical variables. We used a linear regression model to examine associations between baseline burden of psychosocial/cognitive comorbidity and AF-specific QoL score at 6-months, adjusting for all factors associated with psychosocial/cognitive comorbidity (p ≤ 0.2) in univariate analyses. Covariates included in multivariable models included: age, sex, white race, education, smoking status, heart failure, prior stroke, anemia, renal failure, and total number of cardiac comorbidities.
Results
218 adults with symptomatic AF who were willing to complete a study assessment of psychosocial factors and cognition comprised our study sample. The cohort was comprised mostly of middle-aged and older adults with a modest burden of cardiovascular and non-cardiovascular risk factors. The cohort was predominantly female (64.9%) and white (93.9%) with an average age of 64 years. The majority of participants had paroxysmal AF (81%) and 68% had a college degree. Most patients carried a diagnosis of hypertension (77%) and the majority were taking an anti-arrhythmic medication for rhythm control (82%). Just over one-half of participants used an antiplatelet agent (56%) and 3 out of 4 were prescribed an oral anticoagulation (56% on warfarin, 24% on a target-specific oral anticoagulant).
Burden of psychosocial and cognitive comorbidities
Depression was the most commonly observed psychosocial or cognitive impairment among InRhythm participants, noted in almost half of patients (45%). Nearly one-third (30%) of participants were cognitively impaired and 29% were noted to have anxiety (Figure 1). Only 35% of participants were free from any psychosocial or cognitive impairment. Psychosocial and cognitive comorbidities clustered frequently. Approximately one-third (34%) of the participants had a single psychosocial or cognitive impairment, one-quarter (23%) had two impairments, and 7% were affected by all three impairments (Figure 1).
Figure 1.
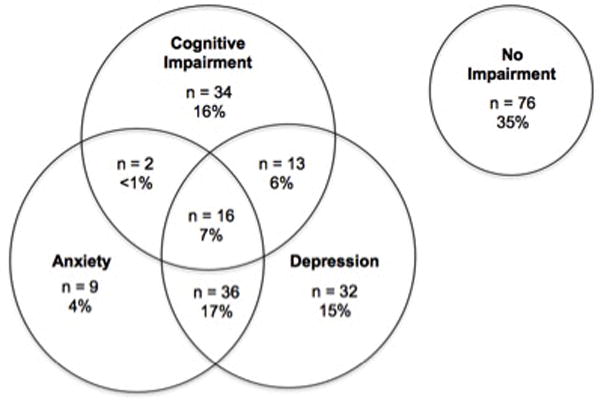
InRhythm participants categorized by impairment in psychosocial and cognitive domains. Percentage values refer to the percent of the total study population (n = 218).
Certain groupings of psychosocial/cognitive comorbidities were more common than others (Figure 1). For example, almost one-fifth (17%) of all participants experienced both depression and anxiety. Anxiety more often co-occurred with depression and/or cognitive impairment rather than in isolation. Cognitive impairment was most likely to occur on its own, but nevertheless almost half of participants with cognitive impairment also had impairment in another domain (48%). Seven percent of participants were impaired in all 3 domains.
Patient characteristics associated with increased burden of impairment
Participants with 1 or more psychosocial or cognitive impairments were older (p<0.001), had less formal education (p<0.001) and were more likely to be current smokers (p=0.01). With the exception of heart failure, which was more prevalent among patients with multiple psychosocial and cognitive impairments (p=0.03), the prevalence of comorbidities such as hypertension, diabetes, stroke, etc., did not vary by level of psychosocial comorbidity (Table 1). Women were less likely than men to have multiple impairments (p=0.02).
Table 1.
Characteristics of Participants by Burden of Psychosocial (Depression, Anxiety) or Cognitive Impairments.
| Characteristic | Number of Factors Impaired | P-value | |||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | ||
| N= 76 | N=75 | N=51 | N=16 | ||
| Age, years, mean (SD) | 65 (13) | 70 (13) | 75 (12) | 77 (11) | <0.001 |
| Age, years, N (%) | |||||
| <65 | 31 (41) | 26 (35) | 9 (18) | 2 (12) | |
| 65–74 | 23 (30) | 16 (22) | 12 (24) | 3 (19) | |
| 75–84 | 17 (22) | 23 (30) | 19 (37) | 7 (44) | |
| ≥85 | 5 (7) | 10 (13) | 11 (21) | 4 (25) | <0.001 |
| Female, N (%) | 41 (54) | 34 (46) | 22 (44) | 6 (35) | 0.02 |
| White race, N (%) | 66 (87) | 68 (91) | 45 (88) | 13 (82) | 0.11 |
| Education, N (%) | |||||
| < High school | 7 (9) | 12 (16) | 17 (33) | 7 (43) | |
| High school/some college | 24 (32) | 33 (44) | 19 (37) | 6 (38) | |
| ≥ College graduate | 46 (60) | 30 (40) | 15 (30) | 3 (19) | <0.001 |
| Current smoker, N (%) | 8 (11) | 13 (17) | 4 (7) | 2 (11) | 0.01 |
| Medical History, N (%) | |||||
| Heart failure | 50 (66) | 53 (70) | 36 (71) | 13 (81) | 0.03 |
| Coronary artery disease | 27 (36) | 23 (30) | 16 (32) | 5 (30) | 0.61 |
| Peripheral vascular disease | 13 (17) | 16 (21) | 9 (17) | 3 (21) | 0.49 |
| Hypertension | 60 (79) | 58 (77) | 42 (83) | 13 (79) | 0.44 |
| Diabetes | 27 (36) | 24 (32) | 18 (36) | 6 (38) | 0.61 |
| Stroke | 6 (8) | 8 (10) | 8 (16) | 3 (19) | 0.15 |
| Alcohol abuse/dependency | 5 (7) | 2 (3) | 3 (6) | 1 (8) | 0.69 |
| Anemia | 14 (18) | 14 (18) | 13 (25) | 3 (19) | 0.18 |
| Asthma/COPD | 17 (23) | 27 (36) | 14 (28) | 5 (31) | 0.06 |
| Renal failure | 21 (27) | 26 (34) | 19 (38) | 6 (39) | 0.11 |
| Implantable cardiac device | 10 (13) | 6 (8) | 6 (12) | 2 (15) | 0.25 |
| Total cardiac comorbid conditions, mean (SD)* | 3.4 (1.5) | 3.4 (1.6) | 3.6 (1.5) | 3.7 (1.6) | 0.06 |
Cardiac comorbidities include: heart failure, coronary artery disease, hypertension, diabetes, stroke, and peripheral vascular disease. COPD = chronic obstructive pulmonary disease.
Baseline burden of psychosocial and cognitive impairment in relation to AF-specific quality of life
Out of the 218 patients who completed baseline interviews, 180 (82.5%) completed the AFEQT questionnaire 6 months after enrolment. Based on their responses, greater burden of psychosocial and cognitive impairment at baseline was associated with poorer AF-specific QoL at 6 months. In multivariable models adjusting for potential confounders (referent group = 0 impairments), there was a dose-response relationship between number of impairments and QoL score (Table 2). Impairment in 1 domain was associated with a 5-point (p=0.236) lower score on the 100-point AFEQT, impairment in 2 domains with a 14-point (p<0.001) lower score, and impairment in 3 domains was associated with a 15-point lower AFEQT score (p=0.02).
Table 2.
Linear regression of AFEQT score compared to psychosocial or cognitive burden reported as adjusted B-coefficient.†
| Number of Impairments | Adjusted B Coefficient (95% CI) | P-Value |
|---|---|---|
| 0 (Ref) | -- | -- |
| 1 | −4.6 (−12.5, 3.4) | 0.257 |
| 2 | −13.6 (−21.7, −5.4) | 0.001 |
| 3 | −15.1 (−28.0, −2.2) | 0.022 |
B adjusted for age, sex, white race, education, smoking status, heart failure, prior stroke, anemia, renal failure, and total number of cardiac comorbidities.
Discussion
In our study of 218 middle-aged and older adults with symptomatic AF, we observed that anxiety, depression, and cognitive impairment were common comorbid illnesses and frequently co-occurred. Certain patterns of psychosocial and cognitive comorbidity were noted, with anxiety and depression frequently being observed together. Finally, we showed that impairment in 2 or more cognitive or psychosocial domains was associated with lower AF-specific QoL at 6 months in adjusted regression models.
Depression or anxiety have been shown to affect up to one-half of patients with AF,6 and patients with AF are at a 2-fold higher risk of cognitive impairment than same-aged patients without AF.24 Thus the rates of anxiety, depression, and cognitive impairment observed in our study were high, but remarkably similar to those reported in prior, albeit smaller studies of patients with AF.6,25 The current study validates these findings in a larger sample of well-characterized ambulatory patients with symptomatic AF and extends current knowledge by illustrating that these psychosocial and/or cognitive impairments frequently co-occurred in individual patients (Figure 1). Furthermore, impairment in multiple domains was associated with poorer AF-specific QoL at 6 months.
Importantly, we observed that psychosocial and cognitive multimorbidity exerts a powerful and negative effect on AF-specific QoL. Differences in QoL scores between participants with multiple impairments as compared to participants with cognitive impairment, anxiety, and depression alone was clinically meaningful26 as well as statistically significant. Our finding that AF patients with an increasing burden of psychosocial or cognitive comorbidities also reported lower QoL scores reflects greater symptom severity and likely relates to the fact that depressed and anxious AF patients utilize health resources at higher rates than do patients free from these mood disorders (e.g., greater number of clinic and emergency room visits).6,9 Indeed, several previous studies have examined the negative impact of individual psychosocial impairments on QoL in patients with AF.6,9,27 However, only one of these prior studies assessed AF-specific QoL 9, and none examined how the co-occurrence of multiple impairments collectively affected AF-specific QoL.
As mentioned above, depression, anxiety, and CI are common in patients with AF;6,24 they are also common in other chronic cardiovascular pathologies. As illustrated by the 2008 statement of the American Heart Association’s Council on Clinical Cardiology, mood and cognition are becoming increasingly recognized for their role in the risk, management, and prognosis of cardiovascular disease, including in the context of stable coronary artery disease, heart failure, AF, and myocardial infarction.28–32 Impairments in mood and cognition have myriad adverse effects, including higher rates of morbidity, symptom severity, health care utilization, and even mortality 30.
Although there is a growing appreciation for the importance of mood and cognitive impairments in the natural history of AF, no prior studies have examined their co-occurrence in AF patients. Especially in light of the fact that anxiety and depression so frequently co-occur in individuals with other chronic medical conditions,33 and given their negative effects on cognitive performance,13 it is not surprising, but nonetheless significant, that we observed a high rate of multi-morbidity across distinct psychosocial and cognitive domains in patients with symptomatic AF. Our findings point to the profound impact of disease clusters on symptom severity, suggesting that assessments of mood and cognition should be performed in concert in order to best characterize AF patients at the greatest risk for complications.
Despite the increasing recognition of the importance of cognitive and psychosocial characteristics as determinants of response to cardiovascular treatments, including rhythm control for AF, contemporary AF Treatment Guidelines do not recommend routine assessment for cognitive impairment, depression, or anxiety.34 Our findings would suggest that such assessments might be useful in patients with symptomatic AF given their close relations with AF-specific QoL, symptom burden, and rehospitalization, which are major targets for contemporary rhythm control therapies, especially catheter ablation.35
Strengths and Limitations
The strengths of the present investigation include its prospective design, the enrollment of AF patients recruited from 3 different academic and community ambulatory clinics, the in-depth characterization of participants’ AF history, as well as the use of validated instruments to characterize each participant’s psychosocial status, cognitive function, and QoL. Our study has several limitations, however, that should be considered when interpreting our results. First, all InRhythm study participants had symptomatic AF and were identified from cardiology clinics, so our findings may not be generalizable to older asymptomatic AF patients1 who are evaluated in other settings. Also, the InRhythm cohort was comprised mostly of white individuals of European descent and those with paroxysmal AF, thereby limiting generalizability of our primary findings to other racial and ethnic groups or those with different types of AF. Finally, we did not adjust for factors that may have confounded or mediated relations between psychosocial and cognitive predictors and AF-specific QoL (e.g., adherence to medications, cardioversions, emergency department visits, or baseline symptom severity).
Conclusions
Our findings suggest that cognitive and psychosocial impairments are common among patients with symptomatic AF and often co-occur, imparting risk for poorer AF-specific QoL. Knowledge of psychosocial and cognitive impairments may help guide patients, families, and physicians in appropriate screening and making informed AF treatment decisions.
Acknowledgments
Funding: This work was supported by U01HL105268, 1R01HL126911-01A1 (JSS & DDM), KL2RR031981 (DDM), K01AG33643 (JSS), T32AG1934 (AH) from the National Heart, Lung and Blood Institute and the National Institute on Aging of the National Institutes of Health, and the Division of Intramural Research, National Heart, Lung, and Blood Institute of the National Institutes of Health, Bethesda, MA.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- 1.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA J Am Med Assoc. 2001;285(18):2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 2.Steinberg JS. Atrial fibrillation: an emerging epidemic? Heart. 2004;90(3):239–240. doi: 10.1136/hrt.2003.014720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naccarelli GV, Varker H, Lin J, Schulman KL. Increasing prevalence of atrial fibrillation and flutter in the United States. Am J Cardiol. 2009;104(11):1534–1539. doi: 10.1016/j.amjcard.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 4.Kim MH, Johnston SS, Chu B-C, Dalal MR, Schulman KL. Estimation of Total Incremental Health Care Costs in Patients With Atrial Fibrillation in the United States. Circ Cardiovasc Qual Outcomes. 2011;4(3):313–320. doi: 10.1161/CIRCOUTCOMES.110.958165. [DOI] [PubMed] [Google Scholar]
- 5.Knecht S, Oelschlager C, Duning T, Lohmann H, Albers J, Stehling C, Heindel W, Breithardt G, Berger K, Ringelstein EB, Kirchhof P, Wersching H. Atrial fibrillation in stroke-free patients is associated with memory impairment and hippocampal atrophy. Eur Heart J. 2008;29(17):2125–2132. doi: 10.1093/eurheartj/ehn341. [DOI] [PubMed] [Google Scholar]
- 6.Thrall G, Lip GYH, Carroll D, Lane D. Depression, Anxiety, and Quality of Life in Patients With Atrial Fibrillation. Chest. 2007;132(4):1259–1264. doi: 10.1378/chest.07-0036. [DOI] [PubMed] [Google Scholar]
- 7.Frasure-Smith N, Lespérance F, Habra M, Talajic M, Khairy P, Dorian P, Roy D. Elevated depression symptoms predict long-term cardiovascular mortality in patients with atrial fibrillation and heart failure. Circulation. 2009;120(2):134–40. doi: 10.1161/CIRCULATIONAHA.109.851675. 3p following 140. [DOI] [PubMed] [Google Scholar]
- 8.Lange HW, Herrmann-Lingen C. Depressive symptoms predict recurrence of atrial fibrillation after cardioversion. J Psychosom Res. 2007;63(5):509–513. doi: 10.1016/j.jpsychores.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 9.Gehi AK, Sears S, Goli N, Walker TJ, Chung E, Schwartz J, Wood KA, Guise K, Mounsey JP. Psychopathology and symptoms of atrial fibrillation: implications for therapy. J Cardiovasc Electrophysiol. 2012;23(5):473–478. doi: 10.1111/j.1540-8167.2011.02264.x. [DOI] [PubMed] [Google Scholar]
- 10.Flaker GC, Pogue J, Yusuf S, Pfeffer MA, Goldhaber SZ, Granger CB, Anand IS, Hart R, Connolly SJ. Cognitive function and anticoagulation control in patients with atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2010;3(3):277–283. doi: 10.1161/CIRCOUTCOMES.109.884171. [DOI] [PubMed] [Google Scholar]
- 11.Lenze EJ, Mulsant BH, Shear MK, Schulberg HC, Dew MA, Begley AE, Pollock BG, Reynolds CF. Comorbid anxiety disorders in depressed elderly patients. Am J Psychiatry. 2000;157(5):722–728. doi: 10.1176/appi.ajp.157.5.722. [DOI] [PubMed] [Google Scholar]
- 12.Moffitt TE, Harrington H, Caspi A, Kim-Cohen J, Goldberg D, Gregory AM, Poulton R. Depression and Generalized Anxiety Disorder. Arch Gen Psychiatry. 2007;64(6):651. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- 13.Lyketsos CG, Lopez O, Jones B, Fitzpatrick AL, Breitner J, DeKosky S. Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: results from the cardiovascular health study. JAMA. 2002;288(12):1475–1483. doi: 10.1001/jama.288.12.1475. [DOI] [PubMed] [Google Scholar]
- 14.Denollet J, Strik JJ, Lousberg R, Honig A. Recognizing increased risk of depressive comorbidity after myocardial infarction: looking for 4 symptoms of anxiety-depression. Psychother Psychosom. 2006;75(6):346–352. doi: 10.1159/000095440. [DOI] [PubMed] [Google Scholar]
- 15.Watkins LL, Blumenthal JA, Davidson JRT, Babyak MA, McCants CB, Sketch MH. Phobic anxiety, depression, and risk of ventricular arrhythmias in patients with coronary heart disease. Psychosom Med. 2006;68(5):651–656. doi: 10.1097/01.psy.0000228342.53606.b3. [DOI] [PubMed] [Google Scholar]
- 16.Doering LV, Moser DK, Riegel B, McKinley S, Davidson P, Baker H, Meischke H, Dracup K. Persistent comorbid symptoms of depression and anxiety predict mortality in heart disease. Int J Cardiol. 2010;145(2):188–192. doi: 10.1016/j.ijcard.2009.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, Chertkow H. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 18.Hachinski V, Iadecola C, Petersen RC, Breteler MM, Nyenhuis DL, Black SE, Powers WJ, DeCarli C, Merino JG, Kalaria RN, Vinters HV, Holtzman DM, Rosenberg Ga, Dichgans M, Marler JR, Leblanc GG. National Institute of Neurological Disorders and Stroke-Canadian Stroke Network vascular cognitive impairment harmonization standards. Stroke. 2006;37(9):2220–2241. doi: 10.1161/01.STR.0000237236.88823.47. [DOI] [PubMed] [Google Scholar]
- 19.Spitzer RL. Validation and Utility of a Self-report Version of PRIME-MD: The PHQ Primary Care Study. JAMA. 1999;282(18):1737. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 22.Spertus J, Dorian P, Bubien R, Lewis S, Godejohn D, Reynolds MR, Lakkireddy DR, Wimmer AP, Bhandari A, Burk C. Development and Validation of the Atrial Fibrillation Effect on QualiTy-of-Life (AFEQT) Questionnaire in Patients With Atrial Fibrillation. Circ Arrhythmia Electrophysiol. 2011;4(1):15–25. doi: 10.1161/CIRCEP.110.958033. [DOI] [PubMed] [Google Scholar]
- 23.Freeman JV, Simon DN, Go AS, Spertus J, Fonarow GC, Gersh BJ, Hylek EM, Kowey PR, Mahaffey KW, Thomas LE, Chang P, Peterson ED, Piccini JP. Association Between Atrial Fibrillation Symptoms, Quality of Life, and Patient Outcomes. Circ Cardiovasc Qual Outcomes. 2015;8(4):393–402. doi: 10.1161/CIRCOUTCOMES.114.001303. [DOI] [PubMed] [Google Scholar]
- 24.Kwok CS, Loke YK, Hale R, Potter JF, Myint PK. Atrial fibrillation and incidence of dementia: A systematic review and meta-analysis. Neurology. 2011;76(10):914–922. doi: 10.1212/WNL.0b013e31820f2e38. [DOI] [PubMed] [Google Scholar]
- 25.Ball J, Carrington MJ, Stewart S. Mild cognitive impairment in high-risk patients with chronic atrial fibrillation: a forgotten component of clinical management? Heart. 2013;99(8):542–547. doi: 10.1136/heartjnl-2012-303182. [DOI] [PubMed] [Google Scholar]
- 26.Dorian P, Burk C, Mullin CM, Bubien R, Godejohn D, Reynolds MR, Lakkireddy DR, Wimmer AP, Bhandari A, Spertus J. Interpreting changes in quality of life in atrial fibrillation: How much change is meaningful? Am Heart J. 2013;166(2):381–387. e8. doi: 10.1016/j.ahj.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 27.Suzuki SI, Kasanuki H. The influences of psychosocial aspects and anxiety symptoms on quality of life of patients with arrhythmia: Investigation in paroxysmal atrial fibrillation. Int J Behav Med. 2004;11(2):104–109. doi: 10.1207/s15327558ijbm1102_6. [DOI] [PubMed] [Google Scholar]
- 28.Lichtman JH, Bigger JT, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lespérance F, Mark DB, Sheps DS, Taylor CB, Froelicher ES. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on. Circulation. 2008;118(17):1768–1775. doi: 10.1161/CIRCULATIONAHA.108.190769. [DOI] [PubMed] [Google Scholar]
- 29.Ruo B, Rumsfeld JS, Hlatky Ma, Liu H, Browner WS, Whooley Ma. Depressive symptoms and health-related quality of life: the Heart and Soul Study. JAMA. 2003;290(2):215–221. doi: 10.1001/jama.290.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rutledge T, Reis SE, Olson M, Owens J, Kelsey SF, Pepine CJ, Mankad S, Rogers WJ, Sopko G, Cornell CE, Sharaf B, Merz CNB. Depression Is Associated With Cardiac Symptoms, Mortality Risk, and Hospitalization Among Women With Suspected Coronary Disease: The NHLBI-Sponsored WISE Study. Psychosom Med. 2006;68(2):217–223. doi: 10.1097/01.psy.0000195751.94998.e3. [DOI] [PubMed] [Google Scholar]
- 31.Cacciatore F, Abete P, Ferrara N, Calabrese C, Napoli C, Maggi S, Varricchio M, Rengo F. Congestive heart failure and cognitive impairment in an older population. Osservatorio Geriatrico Campano Study Group. J Am Geriatr Soc. 1998;46(11):1343–1348. doi: 10.1111/j.1532-5415.1998.tb05999.x. [DOI] [PubMed] [Google Scholar]
- 32.Lane D, Carroll D, Ring C, Beevers DG, Lip GYH. The prevalence and persistence of depression and anxiety following myocardial infarction. Br J Health Psychol. 2002;7(1):11–21. doi: 10.1348/135910702169321. [DOI] [PubMed] [Google Scholar]
- 33.Katon W, Lin EHB, Kroenke K. The association of depression and anxiety with medical symptom burden in patients with chronic medical illness. Gen Hosp Psychiatry. 2007;29(2):147–155. doi: 10.1016/j.genhosppsych.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 34.Fuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Le Heuzey J-Y, Kay GN, Lowe JE, Olsson SB, Prystowsky EN, Tamargo JL, Wann S, Smith SC, Jacobs AK, Adams CD, Anderson JL, Antman EM, Hunt SA, Nishimura R, Ornato JP, Page RL, Riegel B, Priori SG, Blanc J-J, Budaj A, Camm AJ, Dean V, Deckers JW, Despres C, Dickstein K, Lekakis J, McGregor K, Metra M, Morais J, Osterspey A, Zamorano JL. ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Comm. J Am Coll Cardiol. 2006;48(4):854–906. doi: 10.1016/j.jacc.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 35.Goldberg A, Menen M, Mickelsen S, MacIndoe C, Binder M, Nawman R, West G, Kusumoto FM. Atrial fibrillation ablation leads to long-term improvement of quality of life and reduced utilization of healthcare resources. J Interv Card Electrophysiol. 2003;8(1):59–64. doi: 10.1023/a:1022348216072. [DOI] [PubMed] [Google Scholar]


