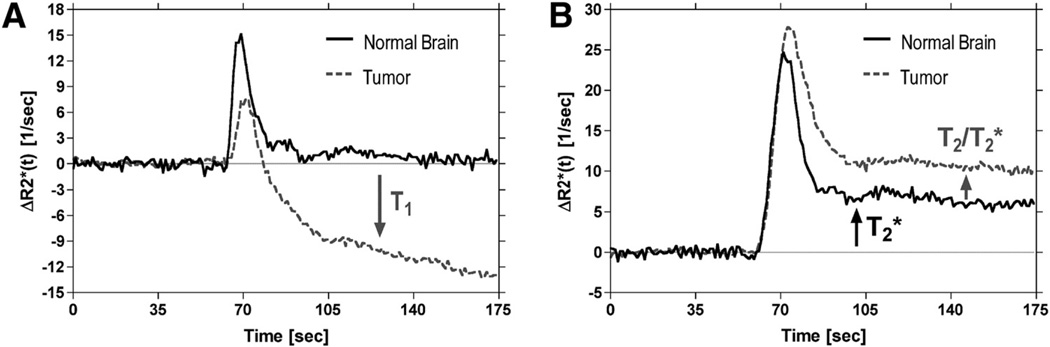
Figure 1.
Illustration of confounding leakage and recirculation effects on dynamic susceptibility contrast (DSC)-magnetic resonance imaging (MRI) concentration–time curves for representative voxels in normal brain and brain tumor. Representative concentration–time curves are shown for voxels in normal brain and brain tumor after serial primary (1°), 0.1 mmol/kg) (A) and secondary (2°, 0.2 mmol/kg) (B) injections of Gd contrast agent in the same patient with glioma. Acquisitions were performed at 1.5 T using a gradient echo-echo planar imaging (GRE-EPI) pulse sequence with flip angle = 90°, TE = 30 milliseconds, and repetition time (TR) = 1000 milliseconds. In regions of normal brain with an intact BBB, a concentrated bolus of Gd contrast agent will remain compartmentalized to the vasculature, resulting in transient signal changes, that ultimately return to the prebolus baseline value (A). However, in regions of tumor with a disrupted blood–brain barrier (BBB), a fraction of the contrast agent will leak out of the vasculature into the extravascular extracellular space (EES), resulting in T1 shortening effects that contaminate tumor concentration–time curves. After secondary injection, the postbolus portions of both normal brain and the tumor concentration–time curves are elevated above their prebolus baseline values (B). The fact that this occurs in normal brain, with a presumably intact BBB, suggests that this is not a leakage effect, but instead may be attributable to a residual susceptibility effect caused by recirculation of an increased steady-state concentration of the contrast agent. However, the additional elevated endline in the tumor concentration–time curve suggests a dipolar T2 leakage effect or additional susceptibility effect. These curves show that both dipolar T1 and T2 and/or residual susceptibility effects may confound perfusion estimates derived by DSC-MRI.