Abstract
Effect of T1 signal on FSL voxel-based morphometry (VBM) modulated gray matter density (mGM) and Freesurfer cortical thickness (CT) is explored. The techniques rely on different analyses but are both commonly used to detect spatial changes in gray matter. Standard pipelines show FSL-VBM is sensitive to T1 signal alterations within a physiologic range and results can appear discordant between FSL-VBM and Freesurfer-CT. Care should be taken in extrapolating results to effect on brain volume.
Introduction
Cortical segmentation methodologies vary and are used throughout neuroimaging research as well as, increasingly, in clinical care. Two commonly used methods to study cortical gray matter (GM) are FSL voxel-based morphometry (VBM)1 and Freesurfer cortical thickness (CT)2: FSL-VBM outputs a 3D map of modulated gray matter density (mGM) and Freesurfer-CT analysis outputs one-dimensional measurements around the cortical ribbon. Both are commonly interpreted as informing cortical volume though there are instances where volume was increased based on one technique and decreased based on the other,3-4 suggesting factors beyond brain volume contribute to results.
Gray and white matter contrast, naturally contributes to successful segmentation; however, extent to which changes in cortical T1 signal affect mGM and CT are not known. Understanding this relationship is critical for appropriate interpretation. This study explores the effect of subtle T1 signal alterations within a physiologic range on FSL-VBM1 and Freesurfer-CT2 using standard processing pipelines. We also illustrate discordance between techniques using individual clinical examples.
Methods
The study is in compliance with our IRB. MPRAGE was performed at 3T (Skyra; Siemens Medical Solutions, Erlangen, Germany) (FOV=256×256mm2, resolution=1×1×1mm3, matrix=256×256, slices=192, TR/TE/TI=2100/3.19/900ms, bandwidth=260Hz/pixel, FA=8°).
Signal Intensity Simulation
MPRAGE images from a 25-year-old healthy male were used to generate simulated signal changes within the frontal operculum (Fig.1). 40% of voxels within the ROI were randomly selected for signal intensity alteration of up to ±20% (5% increments), covering a physiologic T1 range of GM. Pearson correlation coefficient was measured (5% significance level).
Figure 1.
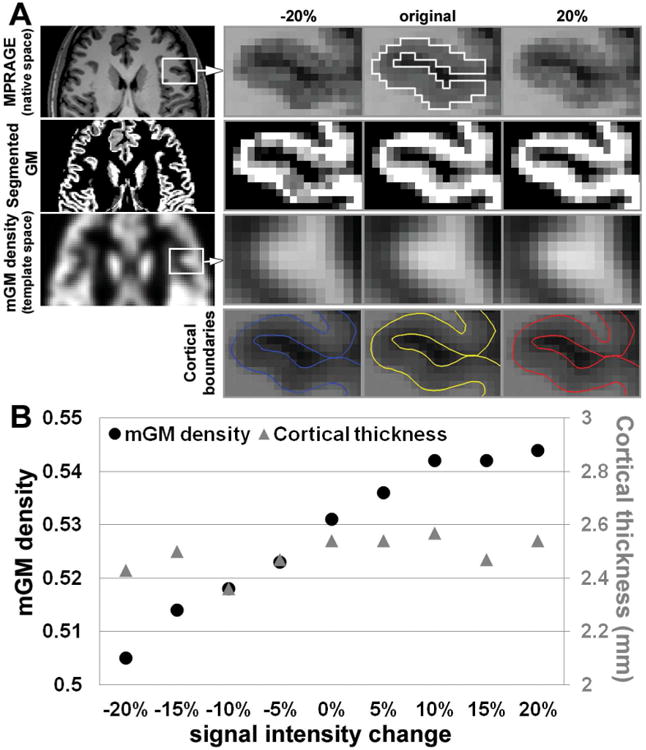
Simulated cortical signal change. (A) (1st row, left-right) Representative MPRAGE in a healthy control individual (25 year-old male). Forty percent of voxels through 7 slices within the ROI were randomly selected and used to simulate changes in T1 signal intensity via decreasing and increasing voxel intensity up to 20% in increments of 5%. Selected ROI from the frontal operculum for simulating signal change is shown in the original image (white solid line). (2nd row) Corresponding segmented GM maps in the native space. (3rd row) mGM density maps in the template space and (4th row) corresponding cortical boundaries from Freesurfer. (B) High correlation between signal intensity and mGM density is observed (black dots; (R=0.964, p<0.001), but no relationship between signal intensity and cortical thickness (gray triangles).
Clinical Examples
Several clinical cases were selected to illustrate concordant and discordant results: 1) acute and chronic infarcts; 2) 19-year-old and 50-year-old healthy subjects; and 3) 28-year-old male with mild traumatic brain injury (mTBI) and an age and sex-matched control.
Image Analysis
All images underwent de-noising.5 Standard FSL-VBM processing steps (v1.1; http://fsl.fmrib.ox.ac.uk/fsl/fslwiki/FSLVBM/) included brain extraction, manual editing, automated tissue type segmentation, nonlinear registration to GM template, modulation, smoothing with isotropic Gaussian kernel (σ=3mm). FreeSurfer was performed to estimate regional CT (v5.3.0; http://freesurfer.net/fswiki).
ROIs were drawn around areas of acute and chronic infarct in the native space and compared with contralateral normal appearing analogous brain. For the control and mTBI subjects, a precuneal ROI from the Harvard-Oxford atlas was interrogated as previous studies report age-associated6 and TBI-associated7 morphometry changes in this region. ROIs drawn in native space were warped to target space by using transform matrices created by FSL-VBM and Freesurfer-CT, respectively.
Results
Simulation results show a strong correlation between signal intensity and mGM (R=0.964, p<0.001). No correlation is present between signal intensity and CT (Fig.1B).
Concordant and discordant results are illustrated in Figures 2,3. The acute infarct showed 23% higher mGM and 52% higher CT compared with contralateral analogous brain. The older healthy subject showed 30% lower mGM and 8% lower CT in the precuneus compared with the younger control. Discordant results included area of chronic infarct, demonstrating 26% higher mGM and 43% lower CT compared with contralateral normal-appearing analogous brain. In the mTBI patient, mGM density was 12% lower and CT was 2% higher in a precuneal ROI compared with a matched control.
Figure 2.
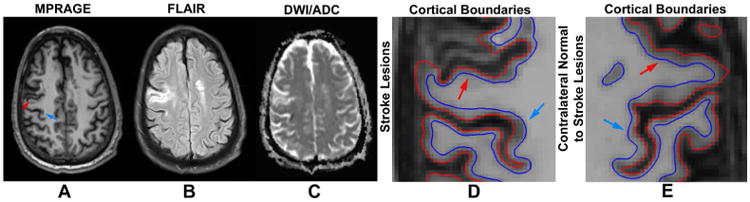
Seventy-one-year-old man with acute onset weakness of the left upper extremity presents with an area of acute infarction (blue arrow) along the deep posterior cortex of the right precentral gyrus involving the hand motor region with relative (A) hypointensity on MPRAGE, (B) hyperintensity on FLAIR and (C) restricted diffusion on ADC map. The patient also has an area of chronic infarction more anteriorly (red arrow) showing relative (A) hypointensity on MPRAGE, (B) hyperintensity on FLAIR and (C) T2 shine-through on ADC map. (D) ROIs in the affected areas show higher and lower cortical thickness, respectively, compared with (E) contralateral analogous brain; however, mGM density as a marker of cortical volume was higher in the acute infarct, as expected, but also higher in the chronic infarct.
Figure 3.
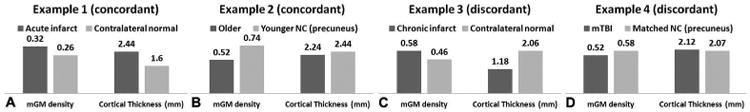
In vivo examples illustrate concordant results between FSL-VBM and Freesurfer cortical thickness in ROIs of (A) acute infarct as well as (B) when comparing younger and older healthy controls, and discordant cortical morphometry results in ROIs of (C) chronic infarct and (D) in the precuneus in an mTBI patient compared with a matched control subject. Of note, prior work reports morphometric changes to the precuneus in aging and traumatic brain injury. The mean values within the ROIs were reported.
Discussion
FSL-VBM is sensitive to T1 signal variations within a clinically relevant range, not found to be true for Freesurfer-CT. Although mGM and CT are completely different measures, both are commonly used to assess GM volume. Discordant results between FSL-VBM and Freesurfer-CT analyses may result from T1 effects on mGM. This observation is of clinical and research importance as there are a myriad of conditions that affect T1 signal. Careful interpretation of FSL-VBM is warranted particularly in the setting of discordant findings.
Several FSL-VBM methodologic steps are worth comment: 1) bias correction may alter T1 signal, and 2) tissue type segmentation can affect output mGM. All images underwent identical bias correction prior to both analyses and we demonstrate the effect of T1 signal change on mGM and CT by applying standard pipelines to recreate commonly used approaches that have widespread availability. Future optimization is warranted to achieve accurate detection of pathology.
Other methods of cortical segmentation are not specifically addressed here. Whether a similar dependence on T1 signal is present in VBM approaches such as SPM12 is not known. The cases provided as part of this report are not meant as generalizable results regarding specific pathologies described but instead serve as in vivo examples of the phenomenon of discordance in terms of interpreting FSL-VBM and Freesurfer-CT. Future studies with larger cohorts would be useful to study specific conditions; these results from single subjects demonstrate discordance may be present not only at a groupwise statistical level, but on an individual basis.
In summary, we demonstrate the dependence of mGM on T1 signal. Care should be taken in interpreting mGM results as volume change alone. Used in concert, FSL-VBM and Freesurfer-CT analyses may be complementary.
Acknowledgments
This research is supported by NIH/NINDS R01 NS039135.
Abbreviations
- VBM
voxel-based morphometry
- mGM
modulated GM density
- CT
cortical thickness
- mTBI
mild traumatic brain injury
References
- 1.Good CD, Johnsrude IS, Ashburner J, Henson RN, Friston KJ, Frackowiak RS. A voxel-based morphometric study of ageing in 465 normal adult human brains. Neuroimage. 2001 Jul;14:21–36. doi: 10.1006/nimg.2001.0786. [DOI] [PubMed] [Google Scholar]
- 2.Dale AM, Fischl B, Sereno MI. Cortical surface-based analysis-I. Segmentation and surface reconstruction. Neuroimage. 1999 Feb;9(2):179–194. doi: 10.1006/nimg.1998.0395. [DOI] [PubMed] [Google Scholar]
- 3.Hutton C, Draganski B, Ashburner J, Weiskopf N. A comparison between voxel-based cortical thickness and voxel-based morphometry in normal aging. Neuroimage. 2009 Nov;48(2):371–380. doi: 10.1016/j.neuroimage.2009.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Winkler AM, Kochunov P, Blangero J, et al. Cortical thickness or grey matter volume? The importance of selecting the phenotype for imaging genetics studies. Neuroimage. 2010 Nov;53(3):1135–1146. doi: 10.1016/j.neuroimage.2009.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith SM, Brady JM. SUSAN-A new approach to low level image processing. Int J Comput Vision. 1997 May;23(1):45–78. [Google Scholar]
- 6.Gaetz W, Roberts TP, Singh KD, Muthukumaraswamy SD. Functional and structural correlates of the aging brain: relating visual cortex (V1) gamma band responses to age-related structural change. Hum Brain MappSep. 2012 Sep;33(9):2035–2046. doi: 10.1002/hbm.21339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou Y, Kierans A, Kenul D, et al. Mild traumatic brain injury: longitudinal regional brain volume changes. Radiology. 2013 Jun;267(3):880–890. doi: 10.1148/radiol.13122542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eriksson SH, Free SL, Thom M, et al. Quantitative grey matter histological measures do not correlate with grey matter probability values from in vivo MRI in the temporal lobe. J Neurosci Methods. 2009 Jun;181(1):111–118. doi: 10.1016/j.jneumeth.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


