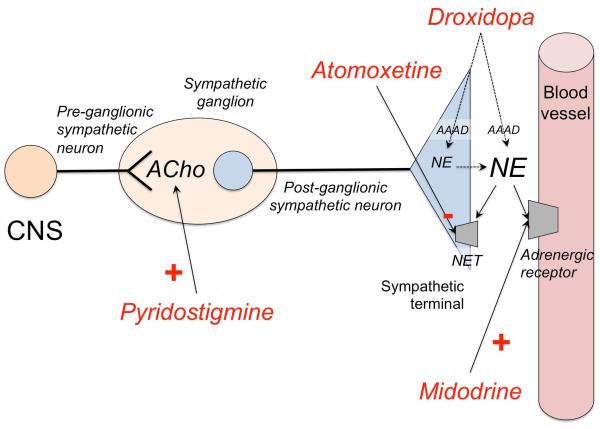
Figure 4. Mechanism of action of drugs for neurogenic orthostatic hypotension.
Commonly used short-acting vasoconstrictor agents include midodrine, an alpha-1-adrenergic receptor agonist; and droxidopa, an artificial aminoacid, which is converted to norepinephrine (NE) by the enzyme aromatic aminoacid decarboxylase (AAAD) in the postganglionic sympathetic terminal, but also extra-neurally in other organs (e.g., kidney). Less commonly used, pyridostigmine, an acetylcholinesterase inhibitor, enhances cholinergic (ACho) transmission in the pre to postganglionic synapse of the sympathetic pathways, but its pressor effect is less consistent. Atomoxetine is a norepinephrine transporter (NET) inhibitor that increases norepinephrine levels; clinical trials are underway to ascertain if chronic treatment with atomoxetine exerts a significant pressor effect in patients with nOH. Fludrocortisone (not shown) is a mineralocorticoid that retains sodium and water therefore increasing intravascular volume. CNS: Central nervous system.