Abstract
Axon-glial interactions are critical for normal functioning of peripheral nerves, and their disruption leads to peripheral neuropathies. Fibroblast growth factors (FGF) are key players in peripheral nerve regeneration after injury. We investigated the role of FGF receptor (Fgfr) signaling in Schwann cells and the consequent regulation of normal Schwann cell-axon interactions. Fgfr1 and Fgfr2 were conditionally inactivated, either singly or in combination, in myelinating and non-myelinating Schwann cells (NMSC) of transgenic mice. The double mutant mice displayed significant loss of thermal sensitivity accompanied by marked neuropathy of unmyelinated nociceptive sensory axons terminating in the dorsal horn of spinal cords, the primary site for integrating pain and temperature inputs. Neuropathy, although to a lesser extent, was also observed in the nociceptive c-fibers in the Remak bundles of sciatic nerves; however, there was no loss of NMSC that ensheathe these axons. Further, axons wrapped by myelinating-Schwann cells and associated myelin sheaths appeared to be unaffected. Relative to the double mutants, axonal neuropathy developed much later in the Fgfr1 but not Fgfr2 single mutant, indicating a difference in signaling potential of the two receptors, with Fgfr1 being more robust than Fgfr2. These findings emphasize the importance of Fgfr1 and Fgfr2 signaling as potential mediators of axon-glial interaction in the peripheral sensory pain pathway primarily via influencing NMSC function, which in turn modulates the structure and function of unmyelinated sensory axons. This study provides a novel molecular mechanism for nociception with possible implications for pain sensitivity in peripheral sensory neuropathies.
Keywords: FGF, FGF receptors, axonal neuropathy, Receptor, Glia, Schwann Cell
INTRODUCTION
Schwann cell-axon interactions are critical for the normal development and functioning of peripheral nerves (Nave and Trapp, 2008). Myelinating Schwann cells wrap multi-lamellar membranes around large diameter axons to form myelin, while non-myelinating Schwann cells (NMSC) form Remak bundles that ensheathe several small diameter unmyelinated sensory axons (c-fibers). These c-fibers are primarily responsible for nociception, the sensory detection of noxious stimulus, including thermal stimuli (Shir and Seltzer, 1090). Several molecules, such as Neuregulin 1 (Chen et al., 2003; Michailov et al., 2004), L1 (Haney et al., 1999), integrins (Feltri et al., 2002), MAG (myelin-associated glycoprotein; Yin et al., 1998) and Po (Li et al., 2006), have been implicated in mediating interactions between peripheral axons and Schwann cells. However, the molecular mechanisms underlying Schwann cell-axon interactions and the involvement of other signaling molecules in this process remain to be further elucidated.
Fibroblast growth factor-2 (FGF2) is a key regulator of peripheral nerve regeneration following injury (reviewed in Grothe and Nikkhah, 2001). FGF2 and three of its receptors, Fgfr1, Fgfr2 and Fgfr3, are expressed by Schwann cells and dorsal root ganglion (DRG) neurons and are up-regulated following injury (Grothe and Nikkhah, 2001). FGF2 is a known mitogen for Schwann cells in culture (Davis and Stroobant, 1990), and its important role during regeneration of myelinated peripheral nerves has been well documented in FGF2-null and Fgfr3-null mice (Grothe et al., 2006). However, the role and mechanisms of FGF signaling via Fgfr1 and Fgfr2, particularly in NMSC for maintaining normal peripheral nerve structure and function, is poorly understood. Therefore, to elucidate the in vivo role of FGF signaling in the PNS, we generated conditional knock-out mice with disrupted Fgfr1 and Fgfr2 signaling in both myelinating Schwann cells and NMSC.
We found that a lack of Fgfr1 and Fgfr2 signaling in NMSC in the double mutant and to a lesser extent in the Fgfr1 single mutant resulted in neuropathy of unmyelinated c-fiber sensory axons and was accompanied by functional impairment of thermal sensitivity without loss of NMSC. These findings emphasize the importance of FGF signaling for normal functioning of NMSC in maintaining the integrity and pain sensitivity of the sensory axons.
MATERIAL AND METHODS
Generation of Fgfr1, Fgfr2 single and Fgfr1/Fgfr2 double conditional knock-out mice
The generation of floxed Fgfr1 flox/+ and Fgfr2 flox/+ (129SV/CD1 strains) and CNP cre/+ mice (2’,3’-cyclic nucleotide 3’-phosphohydrolase; C57Bl/6 strain) has been previously described (Pirvola et al., 2002; Lappe-Siefke et al., 2003; Kaga et al., 2006). Briefly, loxP sites in the Fgfr1 flox/+ mice flank regions encoding the transmembrane and tyrosine kinase domains and in the Fgfr2 flox/+ mice flank the ligand binding IgIII domain and the transmembrane domain of the receptors. Deletion of these regions renders these receptors inactive (Pirvola et al., 2002; Kaga et al., 2006).
As described previously (Kaga et al., 2006), to generate single or double conditional knock-out mice, Fgfr1 flox/+, Fgfr2 flox/+ or Fgfr1 flox/flox; Fgfr2 flox/flox transgenic mice were suitably crossed with CNP cre/+ mice to produce progeny in which Fgfr1 and/or Fgfr2 are disrupted in CNP-expressing myelinating and non-myelinating Schwann cells and oligodendrocytes.
The efficiency and specificity of Fgfr1 and Fgfr2 recombination was assessed by PCR, immunoblotting and in situ hybridization (Supplementary Fig.1; Kaga et al., 2006). CNPCre/+ mice were also mated with reporter mice, Rosa26-YFP (yellow fluorescent protein), for assessment of Cre-mediated recombination in the sciatic nerve and spinal cord (Supplementary Fig. 1).
Behavior Tests
Hot Plate Test
The hot plate test was performed as described (Crawley, 2007) using analgesia meter (myNeuroLab, MO, USA) maintained at 52 or 55 ± 0.2 °C. Mice of three age groups (1-2, 6-9, 12-15 months) were placed on the hot plate and the time taken to begin licking their hind paws, shaking or jumping (latency) was recorded. In order to minimize damage to the tissue a cut-off times of 60 s or 30 s were set. Test was performed blindly with respect to the genotypes of the mice by three investigators.
Von Frey Test
Mechanical sensitivity of mice was evaluated by this test as described (Chen et al., 2003; Crawley, 2007 and Supplementary Fig. 3).
Motor Function Tests
Rotarod and Hanging-Wire tests were performed as described (Crawley, 2007 and Supplementary Fig. 3).
Histology and Immunohistochemistry
Mice were perfused with 4% paraformaldehyde/PBS. Sciatic nerves, sural nerves, DRGs and spinal cords were cryoprotected, embedded and cryostat cross-sections (15 μm) were prepared. Sections were incubated overnight (4°C) in anti-Calcitonin-gene-related-protein (CGRP; 1:200; Bachem, CA), anti- p75 (1:200, Promega, WI), anti-β-amyloid Precursor Protein (β-APP; 1:500; Zymed Lab., CA) or biotinylated griffonia-simplicifolla-lectin-I-isolectin-B4 (IB4; 1:100; Vector Lab., CA). For β-APP, sections were pretreated with 0.1% H2O2 and heated (5min, 0.1 M citrate buffer, pH6). Sections were incubated (1hr) with secondary antibodies conjugated to Alexa 488 or 594 (1:500, Molecular Probes, CA), Cy3 (1:600, Jackson Immuno Research Lab., PA) or with avidin-biotin peroxidase (ABC-Kit; Vector Lab., CA). Nuclei were counterstained with Hoechst 33342. For fluoro-Jade® B labeling, the sections were dehydrated, rehydrated, treated with 0.06% potassium permanganate (10 min) and incubated in 0.0004% fluoro-Jade® B solution in 0.1% acetic acid (20 min).
Electron microscopy
Electron Microscopy on spinal cords and sciatic nerves was performed as described (Marcus et al. 2008). Sections (1 μm) were stained with toluidine blue for light microscopy.
In situ hybridization, Immunoblotting, PCR
These procedures were performed as described (Kaga et al., 2006 and Supplementary Figs. 1,2).
RESULTS
Floxed Fgfr1 and Fgfr2 transgenic mice were crossed with CNP cre/+ mice to produce progeny with single or double Fgfr null mutations in CNP-expressing cells. In the peripheral nervous system, CNP is expressed by myelinating-Schwann cells and NMSC, but not by neurons (Toma et al., 2007). CNP-Cre-mediated recombination was specifically achieved in the Fgfr mutant mice (Supplementary Fig.1; Materials and Methods).
The ultrastructure of Fgfr1-/-;Fgfr2-/- sciatic nerves was analyzed by electron microscopy and semi-thin sections. We found that the loss of these receptors did not adversely affect the structure or numbers of myelinated axons and that the myelin appeared to be well compacted, with no reduction in thickness or in P0 protein expression (Supplementary Fig. 2). In contrast, some sensory axons in the Remak bundles of Fgfr1-/-;Fgfr2-/- sciatic nerves contained electron-dense structures (Fig.1A) suggestive of axonal degeneration (Yamano et al., 1982). Such structures were never found in littermate controls. Since a few Remak bundles in Fgfr1-/-;Fgfr2-/- sciatic nerves clearly had degenerating axons, we asked whether a widespread defect in sensory axon integrity was more apparent by measuring nociception in Fgfr1-/-;Fgfr2-/- mice. We therefore performed the ‘hot plate’ test to examine the response of thermal nociception conveyed primarily by unmyelinated c-fibers found in Remak bundles (Fig.1B). Fgfr1-/-;Fgfr2-/- mice, tested using 3 different age groups (1-2, 6-9, 12-15 months), exhibited significantly longer (~1.6-fold) paw withdrawal latencies than littermate control mice at 55°C. The same test, performed at 52.5°C, yielded similar results (data not shown). These findings suggest that Fgfr1-/-;Fgfr2-/- mice have significantly impaired thermosensory functions in unmyelinated axons.
Fig. 1. Fgfr1-/-;Fgfr2-/- mice show neuropathy of unmyelinated sensory axon in sciatic nerve and have impaired responses to noxious thermal stimuli.
A. Electron microscopy analysis of sciatic nerve from 10 month old control and Fgfr1-/-;Fgfr2-/- littermates show abnormal electron dense structures in some axons of the Remak bundles of the mutant mice. Scale bars, 1μm. B. Paw withdrawal latency in seconds (s), was examined by hot plate test at 55°C in a total of 27 control (CT) and 27 mutant (KO) mice (divided into three age groups of 1-2, 6-9, 12-15 months). Note that the increased latency time is indicative of reduced heat sensitivity of the mutant mice. ** P<0.01, * P<0.05 analyzed by Mann-Whitney U-test. Error bars, SEM, n=12 CT, 10 KO (1-2 months), 7 CT, 6 KO (6-9 months), 8 CT, 11 KO (12-15 months). Out of 27, 19 KOs were littermates with controls.
We also performed the von Frey, Rotarod, and Hanging-Wire tests using these mice to evaluate their mechanosensory and motor functions, which are driven primarily by myelinated axons (Shir and Seltzer, 1990). No impairment of these functions was observed, consistent with the normal structure of peripheral myelinated axons in these mutants (Supplementary Fig. 2,3).
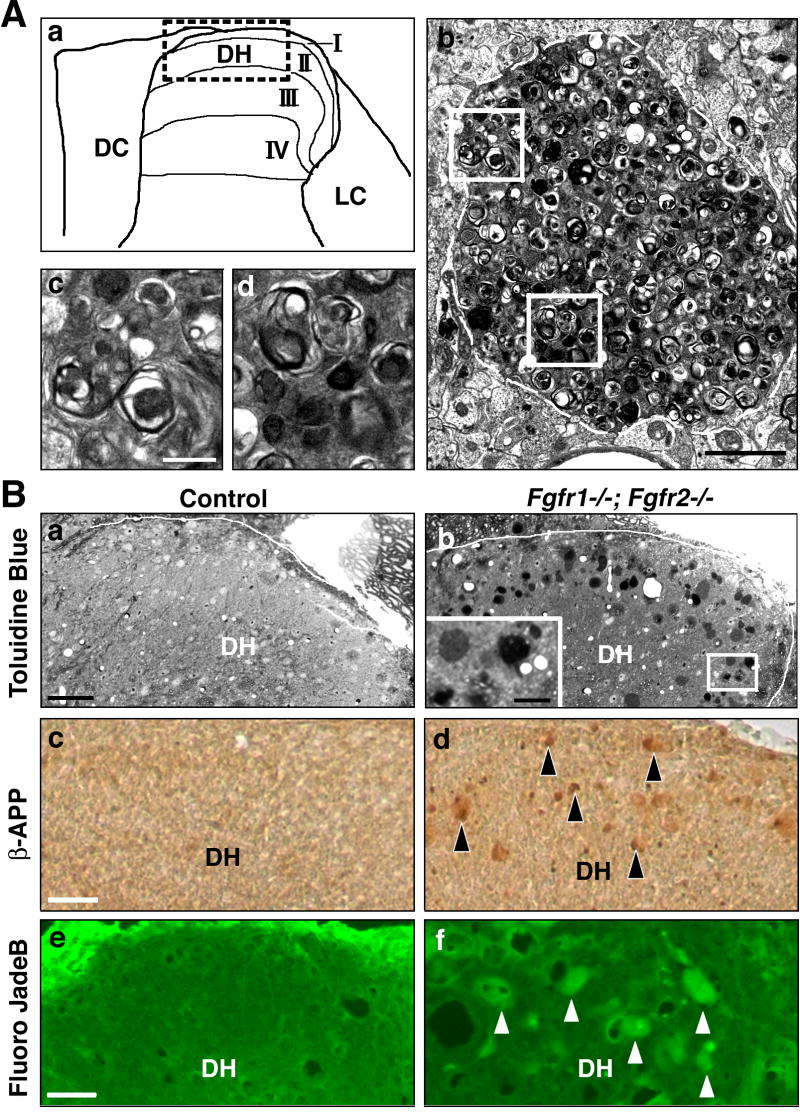
How do such profound physiological changes occur in the absence of dramatic axonal loss in the Remak bundles? Since lamina I and II of the dorsal horn of the spinal cord (Fig. 2Aa) is the predominant site that receives the unmyelinatined nociceptive c-fiber afferents and is a primary site for integrating pain and temperature sensation information, one explanation might be that there are disrupted connections in this region (Hunt and Mantyh, 2001). Toluidine blue staining of Fgfr1-/-;Fgfr2-/- spinal cords revealed numerous large round structures (spheroids) restricted to the lamina I and II of the dorsal horn (Fig. 2Ba,b). These abnormalities were seen in both the cervical and lumbar regions of Fgfr1-/-;Fgfr2-/- mice spinal cords. Electron microscopy analysis (Fig. 2Ab-d) revealed large (10-20μm) axonal spheroids that correspond to the dense spheroids seen in the toludine blue stained semi-thin sections (Fig. 2B). These spheroids are membrane-bound structures containing large collections of dense bodies and vesicles with membrane whorls and amorphous substances of varying densities. These materials selectively accumulated in the spheroids but not in the cytoplasm of neighboring cells. The spheroidal structures were never observed in control littermate mice, even at 14 months of age. Immunostaining with anti-beta-amyloid precursor protein (β-APP) and Fluoro JadeB, two common markers of degenerating axons (Coleman, 2005; Schmued et al., 1997; Fig. 2Bc-f) showed labeling of spheroids by these markers in lamina I and II of Fgfr1-/-;Fgfr2-/- dorsal horns, but not in control mice. Thus, the spheroids of mutant spinal cords are degenerating nociceptive c-fiber axons, and their disruption is consistent with impaired nociceptive signaling.
Fig. 2. Fgfr1-/-;Fgfr2-/- mice show degeneration of unmyelinated sensory axons in spinal cord dorsal horn lamina I and II.
A. (a) Diagram of lamina I-IV of dorsal horn (DH); boxed area is shown in other panels. (b) Electron micrograph of dorsal horn from 10 months Fgfr1-/-;Fgfr2-/- mice shows a neuropathic axonal spheroid; (c-d) higher magnifications of boxed areas shows electron dense structures within the spheroid. B. Toluidine blue stained large axonal spheroids are absent from control (a) but present in lamina I/II of Fgfr1-/-;Fgfr2-/- littermates (b). Spinal cord sections from 8 month old control (c,e) and Fgfr1-/-;Fgfr2-/- littermates (d,f) stained for beta-amyloid precursor protein (β-APP) and Fluoro JadeB detected degenerated axons (examples shown by arrowheads). Three controls and mutants were examined for each analysis. Representative images are shown. Scale bars, Ab, 2μm; Ac,d, 0.5μm; Ba,b, 100μm; Bb insert, 25μm; Bc-f, 50μm. DH: Dorsal-Horn. DC: Dorsal-Column. LC: Lateral-Column.
C-fibers are divided into two mostly non-overlapping groups: 1) IB4-lectin binding fibers that express receptors for glial-cell-derived neurotrophic factor (GDNF) terminating almost exclusively within the inner lamina II, and 2) fibers containing calcitonin- gene-related peptide (CGRP), substance P and TrkA receptor, terminating primarily in lamina I and outer lamina II (Hunt and Mantyh, 2001). Although both c-fiber types are nociceptive and respond to similar stimuli, their differential axonal receptor expression profiles suggest that their response to growth factors may also differ. Therefore, we labeled spinal cord sections for IB4 and CGRP to confirm that the spheroids correspond to nociceptive c-fibers and to determine their subtype (Fig. 3A). The large spheroidal structures were found to be strongly labeled by IB4 (in lamina II) and CGRP (in lamina I/II) in Fgfr1-/-;Fgfr2-/- mice. These structures were not co-labeled with the Hoechst nuclear stain, confirming that these were axonal structures and not cell bodies. These data strongly suggest that both subgroups of sensory c-fibers in Fgfr1-/-;Fgfr2-/- mice undergo neuropathological changes.
Fig. 3. Degeneration of both IB4+ and CGRP+ subgroups of unmyelinated sensory axon in Fgfr1-/-; Fgfr2-/- mice without loss of non-myelinating Schwann cells.
A. Spinal cord cross sections show IB4+ and CGRP+ spheroids in lamina I/II of dorsal horn (DH) in Fgfr1-/-;Fgfr2-/- but not in littermate controls at 8 months (M). B. IB4 staining of postnatal day 15 (P15), 1M and 2M spinal cords show onset of spheroid formation at P15, which progressively increase in size and numbers reaching a plateau around 2M. Boxed areas magnified in inserts. Three controls and mutants were examined for each analysis. Representative images are shown. C. Cross sections of sural nerve from 2M control (a) and Fgfr1-/-;Fgfr2-/- littermates (b) stained with anti-p75 show equal numbers of p75+ NMSC (c). N=3. Scale bars, A,B, 100μm; C, 50μm; inserts, 50μm.
Is the observed c-fiber neuropathology a consequence of disrupted signaling during development or a loss of signals required for maintenance of axonal integrity? To answer this question we analyzed spinal cords from control and Fgfr1-/-;Fgfr2-/- mice as a function of age (Fig. 3A,B). No spheroids (IB4+ or CGRP+) were observed at P9 (data not shown), and only small spheroids could be occasionally observed at P15 in the mutants. Their size and number, however, increased progressively with age becoming quite prominent by one-two months (Fig. 3A,B). A similar conclusion was obtained by analyzing β-APP and semi-thin sections (data not shown).
Why does elimination of Fgfr1/Fgfr2 in NMSC cause c-fiber axonal neuropathy? Loss of FGF signaling in the NMSC might adversely affect their viability, resulting in axon degeneration similar to mice with disrupted NRG1-ErbB signaling (Chen et al., 2003). To investigate this possibility, we immunostained sciatic nerves and c-fiber rich sural nerve sections with anti-p75, a marker of NMSC, and counted the total number of positive cells (Fig. 3C). No differences were found between control and Fgfr1-/-;Fgfr2-/- mice, suggesting sensory axon degeneration is not due to a loss of NMSC.
Is the axonal degeneration in the Fgfr1-/-;Fgfr2-/- double mutant due to a loss of signaling via Fgfr1 or Fgfr2 or both? To address this question we analyzed Fgfr1-/- and Fgfr2-/- single mutants as a function of age. Examination of the dorsal horn by immunolabelling for IB4, CGRP and β-APP or by toluidine blue stained semi-thin section and EM showed that in contrast to double mutants there was no axonal degeneration in either of the single mutants up to 7 months. By eight months, however, Fgfr1-/- but not Fgfr2-/- mice developed numerous axonal spheroids in lamina I/II (Fig. 4; Supplementary Fig. 4), suggesting involvement of both receptors, with Fgfr1 playing a more prominent role than Fgfr2.
Fig. 4. Unmyelinated sensory axon degenerate in Fgfr1-/- but not in Fgfr2-/- mice.
Spinal cord cross sections showing dorsal horn (DH) of control and Fgfr1-/- or Fgfr2-/- mice stained for IB4, CGRP or β-APP at 8 months (M) (boxed areas magnified in inserts) and with toluidine blue (semi-thin sections) at 10M. No spheroids were seen in either of the single mutants untill 7M (Supplementary Fig. 4). By 8M they appeared in the Fgfr1-/- but never in Fgfr2-/- mice. Three controls and mutants were examined for each analysis. Representative images are shown. Scale bars, IB4 and CGRP, 100μm; β-APP, Toluidine Blue and insert, 50μm.
DISCUSSION
Pathology of myelinated axons is a common feature in several hereditary peripheral neuropathies in which myelinating Schwann cells bear the primary mutation, suggesting an important modulatory influence of myelinating Schwann cells on axons (Sahenk, 1999; Wrabetz et al., 2004; Nave and Trapp, 2008). Here, we report that disruption of Fgfr1 and Fgfr2 signaling in non-myelinating Schwann cells (NMSC) resulted in neuropathy of non-myelinated peripheral sensory axons, accompanied by significant insensitivity to noxious thermal stimuli. In contrast, no abnormalities were observed in the structure or functions of myelinated axons from disrupted Fgfr signaling.
The large spheroidal structures observed in lamina I and II of the spinal cord dorsal horn in the Fgfr1-/-; Fgfr2-/- mice may represent degenerating presynaptic axonal terminal or distal region of c-fibers sensory axons. Similar spheroids, reminiscent of proliferative lysosomal structures have been observed in various lysosomal storage disorders (Fujisawa, 1988), including Niemann-Pick type C disease, where they were observed in the dorsal horn and described as “dystrophic presynaptic axonal terminals” (Ohara et al., 2004). Similar structures were also reported in Alzheimer disease (Nixon, 2007). It should be noted that although dramatic neuropathy of axonal terminals was observed in the dorsal horn of Fgfr mutant mice, no loss of neuronal cell bodies was seen in the DRG by electron microscopy (data not shown). This raises the possibility that spheroid formation may represent a form of distal axonopathy in which the terminal portion of axons and presynaptic axon terminals are preferentially affected. It has been shown that axons degenerate earlier than the cell body in Niemann-Pick type C mouse brain (Ohara et al., 2004) and after transaction of the sciatic nerve (Tandrup et al., 2000). Furthermore, in certain conditions, neuronal cell bodies remain viable even while the axons are degenerating (Sagot et al., 1995), dissociating neuronal and axonal functions. Axonal spheroids in the rat gracile nuclei can also develop as a consequence of normal aging (Fujisawa, 1988). However in the Fgfr1-/-;Fgfr2-/- mutants these structures first appear in young adults, suggesting that this defect differs from that seen in normal aging animals. C-fiber-evoked activity in the dorsal horn begins to develop gradually only over the postnatal period into adulthood (Fitzgerald, 2005); similarly, the manifestation of the c-fiber defect in our mutant mice also developed over approximately a parallel time frame. Therefore, it is possible that the defect may be somehow correlated with the functional maturity of the c-fibers.
Although Schwann cells and DRG neurons both express Fgfr1 and Fgfr2 (Grothe and Nikkhah, 2001), these receptors should be eliminated in principle only from CNP-expressing Schwann cells of Fgfr1 and Fgfr2 conditional knock-out mice. Nevertheless, the possibility exists that Fgfrs may have also been eliminated from DRG neurons as a result of a Cre-mediated recombination that occurred earlier in embryonic development if CNP promoter activity were present in neural precursors. Further, dysfunction of sensory neurons can potentially occur due to deletion of Fgfrs from the peripheral (skin) or central (spinal cord neurons) targets of unmyelinated axons, resulting in impairment of trophic support from these targets. In situ hybridization analysis of the mutant mice, using a probe against the deleted sequence of Fgfr1, failed to demonstrate loss of Fgfr1 from either DRG and spinal cord neurons or from regions of the skin that are innervated by c-fibers, thus ruling out these possibilities (Supplementary Fig.1). We therefore favor the model in which the neuropathy of sensory neurons in mutant mice is caused by the elimination of Fgfr1 and Fgfr2 in NMSCs, which then indirectly modulate neuronal function, leading to neuropathy.
The phenotypic difference that was observed between Fgfr1 and Fgfr2 single mutants suggests that these Fgfrs have distinct signaling potentials, thresholds, or specificities in NMSCs, as has been observed in oligodendrocytes (Fortin et al., 2005). Although Fgfr1 signaling is more robust than Fgfr2, the phenotype of Fgfr1-/-; Fgfr2-/- double mutants is more severe than the Fgfr1-/- single mutant, suggesting that Fgfr2 is involved as well. Thus, the phenotype of the double mutant potentially emerges from cooperative signaling by both receptors.
Degeneration and loss of sensory axons resulting from loss of NMSC bearing the ErbB receptor mutation has been reported (Chen et al., 2003); however, unlike the ErbB mutant, the axonal degeneration in the Fgfr1-/-; Fgfr2-/- mice was not coupled to the death of NMSC. Therefore NMSC mortality may not be necessary, and simply perturbing NMSC receptor function may be sufficient to adversely modulate axonal function. Nevertheless, in both cases it is clear that disruption of axon-glia signaling resulted in neuropathology.
Exactly how Fgfr1/2 signaling in NMSC influences axonal function remains to be determined. A model can be proposed in which Fgfr signaling in NMSC regulates the production or delivery of certain trophic factors or regulates the expression of cell surface ligands that are essential for normal function or survival of axons, the disruption of which in the mutant would then result in axonal neuropathy and degeneration. For example, FGF signaling is known to upregulate GDNF and NGF mRNA in cells expressing Fgfr1 and Fgfr2 (Ferhat et al., 1997; Suter-Crazzolara and Unsicker, 1996). These growth factors, produced by Schwann cells (Bandtlow et al., 1987; Hammarberg et al., 1996), provide essential trophic support to sensory neurons expressing receptors of these growth factors (Chen et al., 2003). Disruption of Fgfr1/2 signaling in non-myelinating Schwann cells may also affect the expression of modulatory molecules (like MAG is for myelinating Schwann cells; Yin et al., 1998) that function as ligands to help stabilize the axonal cytoskeleton and transport. Impairment of axonal transport may in turn lead to the accumulation of molecules, organelles, and disorganized cytoskeletal elements in local enlargements of distal axons or axon terminals, thereby giving rise to spheroidal structures. The accumulation of β-APP in these spheroids, as seen in the mutants, is consistent with a failure in efficient axonal transport, which is considered as an early event in the process of axonal degeneration (Coleman, 2005).
In summary, the selective loss of Fgfr1/2 signaling in NMSC results in marked neuropathy of sensory c-fibers accompanied by significant insensitivity to thermal stimuli. We propose that neuron-derived FGFs activate glial Fgfrs, which then transduce signals for production of trophic factors or adhesion molecules that are essential for maintenance of sensory functions like axonal transport or survival. Dysfunction of NMSC and Fgfr signaling may therefore be implicated in the modulation of pain sensitivity in peripheral sensory neuropathies.
Supplementary Material
Acknowledgments
We would like to thank Dr. D. M. Ornitz (Washington University School of Medicine, St. Louis, MO) for providing us with floxed Fgfr1 and Fgfr2 transgenic mice, Dr. K. Nave (Max Planck Institute of Experimental Medicine, Goettingen, Germany) for CNP-Cre mice, Dr. M. N. Rasband (Baylor College of Medicine, Houston, TX) for review of the manuscript, Drs. S. Patel (V. A. Conn.) and N. K. Dwyer (Lipid Cell Biology, NIH) for their comments on the electron micrograph of axonal spheroids. Supported by grant from NIH NS38878 (R.B).
References
- Bandtlow CE, Heumann R, Schwab ME, Thoenen H. Cellular localization of nerve growth factor synthesis by in situ hybridization. EMBO J. 1987;6:891–899. doi: 10.1002/j.1460-2075.1987.tb04835.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S, Rio C, Ji RR, Dikkes P, Coggeshall RE, Woolf C, Corfas G. Disruption of ErbB receptor signaling in adult non-myelinating Schwann cells causes progressive sensory loss. Nat Neurosci. 2003;6:1186–1193. doi: 10.1038/nn1139. [DOI] [PubMed] [Google Scholar]
- Coleman C. Axon degeneration mechanisms; commonality amid diversity. Nat Rev Neurosci. 2005;6:889–898. doi: 10.1038/nrn1788. [DOI] [PubMed] [Google Scholar]
- Crawley JN. In: What’s wrong with my mouse? Behavioral phenotype of transgenic and knockout mice. Crawley JN, editor. New York: Wiley; 2007. pp. 62–109. [Google Scholar]
- Davis JB, Stroobant P. Platelet-derived growth factors and fibroblast growth factors are mitogens for rat Schwann cells. J Cell Biol. 1990;110:1353–1360. doi: 10.1083/jcb.110.4.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feltri ML, Graus Porta D, Previtali SC, Nodari A, Migliavacca B, Cassetti A, Littlewood-Evans A, Reichardt LF, Messing A, Quattrini A, Mueller U, Wrabetz L. Conditional disruption of beta 1 integrin in Schwann cells impedes interactions with axons. J Cell Biol. 2002;156:199–209. doi: 10.1083/jcb.200109021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferhat L, Represa A, Zouaoui-Aggoun D, Ferhat W, Ben-Ari Y, Khrestchatisky M. FGF-2 induces nerve growth factor expression in cultured rat hippocampal neurons. Eur J Neurosci. 1997;9:1282–1289. doi: 10.1111/j.1460-9568.1997.tb01483.x. [DOI] [PubMed] [Google Scholar]
- Fitzgerald M. The development of nociceptive circuits. Nat Rev Neurosci. 2005;6:507–520. doi: 10.1038/nrn1701. [DOI] [PubMed] [Google Scholar]
- Fortin D, Rom E, Sun H, Yayon A, Bansal R. Distinct fibroblast growth factor (FGF)/FGF receptor signaling pairs initiate diverse cellular responses in the oligodendrocyte lineage. J Neurosci. 2005;25:7470–7479. doi: 10.1523/JNEUROSCI.2120-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujisawa K. Study of axonal dystrophy. Posterior funiculus and posterior column of ageing and old rats. Acta Neuropathol. 1988;76:115–127. doi: 10.1007/BF00688095. [DOI] [PubMed] [Google Scholar]
- Grothe C, Haastert K, Jungnickel J. Physiological function and putative therapeutic impact of the FGF-2 system in peripheral nerve regeneration—Lessons from in vivo studies in mice and rats. Brain Res Rev. 2006;51:293–299. doi: 10.1016/j.brainresrev.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Grothe C, Nikkhah G. The role of basic fibroblast growth factor in peripheral nerve regeneration. Anat Embryol. 2001;204:171–177. doi: 10.1007/s004290100205. [DOI] [PubMed] [Google Scholar]
- Hammarberg H, Piehl F, Cullheim S, Fiell J, Hökfelt T, Fried K. GDNF mRNA in Schwann cells and DRG satellite cells after chronic sciatic nerve injury. Neuroreport. 1996;7:857–860. doi: 10.1097/00001756-199603220-00004. [DOI] [PubMed] [Google Scholar]
- Haney CA, Sahenk Z, Li C, Lemmon VP, Roder J, Trapp BD. Heterophilic binding of L1 on unmyelinated sensory axons mediates Schwann cell adhesion and is required for axonal survival. J Cell Biol. 1999;146:1173–1183. doi: 10.1083/jcb.146.5.1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt SP, Mantyh PW. The molecular dynamics of pain control. Nat Rev Neurosci. 2001;2:83–91. doi: 10.1038/35053509. [DOI] [PubMed] [Google Scholar]
- Kaga Y, Shoemaker WJ, Furusho M, Bryant M, Rosenbluth J, Pfeiffer SE, Oh L, Rasband M, Lappe-Siefke C, Yu K, Ornitz DM, Nave KA, Bansal R. Mice with conditional inactivation of fibroblast growth factor receptor-2 signaling in oligodendrocytes have normal myelin but display dramatic hyperactivity when combined with Cnp1 inactivation. J Neurosci. 2006;26:12339–12350. doi: 10.1523/JNEUROSCI.3573-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Bai Y, Ianakova E, Grandis M, Uchwat F, Trostinskaia A, Krajewski KM, Garbern J, Kupsky WJ, Shy ME. Major myelin protein gene (P0) mutation causes a novel form of axonal degeneration. J Comp Neurol. 2006;498:252–265. doi: 10.1002/cne.21051. [DOI] [PubMed] [Google Scholar]
- Marcus J, Honigbaum S, Shroff S, Honke K, Rosenbluth J, Dupree JL. Sulfatide is essential for the maintenance of CNS myelin and axon structure. Glia. 2006;53:372–381. doi: 10.1002/glia.20292. [DOI] [PubMed] [Google Scholar]
- Michailov GV, Sereda MW, Brinkmann BG, Fischer TM, Haug B, Birchmeier C, Role L, Lai C, Schwab MH, Nave KA. Axonal neureglin-1 regulates myelin sheath thickness. Science. 2004;304:700–703. doi: 10.1126/science.1095862. [DOI] [PubMed] [Google Scholar]
- Nave KA, Trapp BD. Axon-glial signaling and the glial support of axon function. Ann Rev Neurosci. 2008;31:535–561. doi: 10.1146/annurev.neuro.30.051606.094309. [DOI] [PubMed] [Google Scholar]
- Nixon RA. Autophagy, amyloidgenesis and Alzheimer disease. J Cell Sci. 2007;120:4081–4091. doi: 10.1242/jcs.019265. [DOI] [PubMed] [Google Scholar]
- Ohara S, Ukita Y, Ninomiya H, Ohno K. Axonal dystrophy of dorsal root ganglion sensory neurons in a mouse model of Niemann–Pick disease type C. Exp Neurol. 2004;187:289–298. doi: 10.1016/j.expneurol.2004.03.002. [DOI] [PubMed] [Google Scholar]
- Pirvola U, Ylikoski J, Trokovic R, Hébert JM, McConnell SK, Patanen J. FGFR1 is required for the development of the auditory sensory epithelium. Neuron. 2002;35:671–680. doi: 10.1016/s0896-6273(02)00824-3. [DOI] [PubMed] [Google Scholar]
- Sagot Y, Dubois-Dauphin M, Tan SA, de Bilbao F, Aebischer P, Martinou JC, Kato AC. Bcl-2 overexpression prevents motoneuron cell body loss but not axonal degeneration in a mouse model of a neurodegenerative disease. J Neurosci. 1995;15:7727–7733. doi: 10.1523/JNEUROSCI.15-11-07727.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahenk Z. Abnormal Schwann cell-axon interaction in CMT neuropathies – the effects of mutant Schwann cells on the axonal cytoskeleton and regeneration-associated myelination. Ann NY AcadSci. 1999;833:415–426. [PubMed] [Google Scholar]
- Schmued LC, Albertson C, Slikker W., Jr Fluoro-Jade: a novel fluorochrome for the sensitive and reliable histochemical localization of neuronal degeneration. Brain Res. 1997;751:37–46. doi: 10.1016/s0006-8993(96)01387-x. [DOI] [PubMed] [Google Scholar]
- Shir Y, Seltzer Z. A-fibers mediate mechanical hyperesthesia and allodynia and C-fibers mediate thermal hyperalgesia in a new model of causalgiform pain disorders in rats. Neurosci Lett. 1990;115:62–67. doi: 10.1016/0304-3940(90)90518-e. [DOI] [PubMed] [Google Scholar]
- Suter-Crazzolara C, Unsicker K. GDNF mRNA levels are induced by FGF-2 in rat C6 glioblastoma cells. Mol Brain Res. 1996;41:175–182. doi: 10.1016/0169-328x(96)00089-7. [DOI] [PubMed] [Google Scholar]
- Tandrup T, Woolf CJ, Coggeshall RE. Delayed loss of small dorsal root ganglion cells after transection of the rat sciatic nerve. J Comp Neurol. 2000;422:172–180. doi: 10.1002/(sici)1096-9861(20000626)422:2<172::aid-cne2>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- Toma JS, McPhail LT, Ramer MS. Differential RIP antigen (CNPase) expression in peripheral ensheathing glia. Brain Res. 2007;117:1–10. doi: 10.1016/j.brainres.2006.12.053. [DOI] [PubMed] [Google Scholar]
- Wrabetz L, Feltri ML, Kleopa KA, Scherer SS. Inherited neuropathies: clinical, genetic, and biological features. In: Lazzarini RA, editor. Myelin biology and disorders. Elsevier Academic Press; 2004. pp. 905–951. [Google Scholar]
- Yamano T, Shimada M, Okada S, Yutaka T, Kato T, Yabuuchi H. Ultrastructural study of biopsy specimens of Rectal Mucosa. Its use in neuronal storage diseases. Arch Pathol LabMed. 1982;106:673–677. [PubMed] [Google Scholar]
- Yin X, Crawford TO, Griffin JW, Tu P, Lee VM, Li C, Roder J, Trapp BD. Myelin-associated glycoprotein is a myelin signal that modulates the caliber of myelinated axons. J Neurosci. 1998;18:1953–1962. doi: 10.1523/JNEUROSCI.18-06-01953.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.