Abstract
Objectives
This study examined early psychosocial precursors (internalizing behaviors and parent-child bonding) of adult tobacco use, alcohol, and other drug-related problems and later adverse health consequences.
Methods
A community-based sample of 502 participants were interviewed over a 22-year period (1983, 1985–1986, 1997, 2002, and 2005).
Results
There is a strong relationship between later adolescent internalizing behaviors and later adverse health consequences in adulthood. Later adolescent internalizing behaviors serves as a mediator between low parent-child bonding in earlier adolescence and later adverse health consequences. Tobacco use, alcohol, and other drug-related problems in the late 20s and early 30s are directly related to later adverse health consequences and indirectly as mediators between earlier psychosocial difficulties and later adverse health consequences.
Conclusions
Public health and clinical implications suggest the importance of creating policies and programs and providing treatment that target parent-child bonding and internalizing behaviors in order to reduce tobacco use, alcohol, and other drug-related problems, and ultimately, later health problems.
INTRODUCTION
Tobacco, alcohol, and drug use affect the health of United States adults. Marijuana is the most commonly used illicit drug.1–4 Smoking is the leading cause and alcohol use is the third leading cause of death in the nation.5, 6 Aside from mortality, smoking, marijuana, and alcohol use are associated with great morbidity, including respiratory diseases, cardiovascular diseases, and cancer.1–6 In addition to overall adverse health consequences, marijuana and alcohol use, specifically, also affect neurological health, such as the effects associated with impaired short-term memory and learning difficulties.1, 4 In Healthy People 2010, the federal government clearly prioritized tobacco use, alcohol and drug abuse, physical health, and mental health as national public health concerns, thereby establishing goals to be reached by the year 2010.7
There is evidence that health status and outcomes are affected by the quality of earlier personal relationships, particularly parent-child bonding.8–10 The literature also suggests that aspects of internalizing behaviors and tobacco use, alcohol, and other drug-related problems are associated with an increased risk for later health problems.11 The present study examines the pathway from parent-child bonding during adolescence to health in the mid-thirties. Our measures of health refer to three areas of health, namely, neurocognitive health, respiratory health, and general malaise. This study is unique in that it examines adolescent psychosocial factors as predictors of later adverse health consequences in the mid-thirties. The present investigation is also the first longitudinal study to examine the interrelationship of adolescent psychosocial factors, tobacco use, alcohol, and other drug-related problems in the late twenties and early thirties, and adverse health consequences during the mid-thirties.
Three types of early psychosocial antecedents related to later health outcomes were identified in this study; (a) parent-child bonding, which consisted of identification with parents, parent-child centeredness, and parental affection, (b) internalizing behaviors, which consisted of anxiety, depression, interpersonal difficulties, low ego-integration, and maladaptive coping with internal stressors, and (c) tobacco use, alcohol, and other drug-related problems. Based on the empirical literature and Family Interactional Theory (FIT), we hypothesized that in earlier adolescence low parent-child bonding, characterized by lack of affection or support from parents, predicts internalizing behaviors.12–15 In addition, only a few studies have explored the long-term relationships between internalizing behaviors in earlier adolescence and health in the fourth decade of life. Recent research based on the Terman Life-Cycle Study supports the general relationship between aspects of personality in childhood and health in adulthood.8–10, 16 Based on these studies, we further hypothesized that low parent-child bonding and internalizing behaviors are significantly associated with later adverse health consequences.
Besides the empirical literature, our hypotheses are derived from FIT. FIT emphasizes the importance of the early attachment between parent and child. Effective parent-child bonding is characterized by affection, child-centeredness, and minimal parent-child conflict. In addition, a strong attachment is characterized by the child identifying with parental values (e.g., conventional beliefs and values). Such a strong bond between the parent and child sets the stage for the development on the part of the child of two types of behavior that have been identified in the literature, namely, internalizing behaviors (e.g., depression and anxiety)11, 17 and externalizing behaviors expressed in nonconventional forms of behavior (e.g., illegal drug use).18, 19 Externalizing behaviors in the late twenties and early thirties, is a manifestation of externalizing behaviors at an earlier stage of development. _According to FIT, mutual parent-child bonding characterized by affection is associated with good intrapersonal functioning, which insulates the adolescent from smoking and abusing alcohol and drugs.17, 20, 21 There is a degree of developmental stability in these characteristics so that their influences extend into later years. In recent years, we have applied FIT conceptions to predicting tobacco use in adulthood. We have used FIT in analyses designed to assess the developmental pathways with regards to predictors of cigarette use and smoking cessation.22, 23 FIT has served as an organizing perspective for our results as we have reliable measures of parental bonding, internalizing and externalizing behaviors, and their developmental stability.
In sum, based on FIT and the empirical literature cited above, we hypothesized that (a) difficulty in parent-child bonding during earlier adolescence is related to internalizing problems in later adolescence, and that, in turn, (b) both difficult parent-child bonding and internalizing behaviors are linked to tobacco use, alcohol, and other drug-related problems in the late 20s and early 30s, and that finally, (c) tobacco use, alcohol, and other drug-related problems in the late 20s and early 30s are related to adverse health consequences in the mid 30s. In addition, we hypothesized that internalizing behaviors has a direct adverse effect on health. This study has the methodological advantage of having data collected from participants at different developmental periods (earlier and later adolescence, late twenties, and early and mid-thirties).
METHODS
Participants and Procedure
Participant data were based on a randomly selected cohort first studied in 1975 and then prospectively from 1983 to 2005. The families in this study were generally representative of the population of families in the Northeast in 1975 when the initial wave of the data was collected. Data was collected in Albany and Saratoga, two upstate New York counties; families in both locations were similar to the data collected nationally by the 1980s United States Census Bureau with respect to gender, education, family income, and family structure. For example, 75% of the children lived with married parents, and 19% lived with a mother who was not currently married; the 1980 census figures were 79% and 17%, respectively. Follow-up data were collected in the participants’ homes in 1983 (N=756; earlier adolescence), 1985–1986 (N=739; later adolescence), 1997 (N=749; late twenties), 2002 (N=673; early thirties), and 2005 (N=502; mid-thirties). The mean ages (SDs) of the participants at the follow-up interviews were: 14.05 (2.80), 16.26 (2.81), 26.99 (2.80), 32.00 (2.84), and 35.08 (2.99), respectively.
Extensively trained and supervised lay interviewers administered the interviews in private. Written informed consent was obtained from the participants and their mothers in 1983 and 1985–1986, and from the participants only in 1997, 2002, and 2005. Approval for the use of human subjects was given by the Institutional Review Board of the New York University School of Medicine. For more details about the sampling procedures and the original sample, see Cohen and Cohen24 and Brook, Brook, Whiteman, Gordon, and Cohen.15
The sample of 502 participants during their mid-thirties represents a random sample of the 673 participants who took part in the study during their early thirties. There were no significant age differences on the psychosocial measures between those who participated during their early thirties and remained in the study during their mid-thirties and those who were not included during their mid-thirties (t = 0.78, p >0.05). But there were differences for gender and parental education (t = 2.57, p < 0.05; t = −2.80, p < 0.05, respectively). We controlled for gender, age, and parental education in our analysis. Five hundred participants were included in our analyses (two cases were excluded because of missing health variables during their mid-thirties). There were 435 (87%) participants who had complete data. Less than 5% of the participants had missing values on one or more of the independent variables. For those participants with missing data, we used the full information maximum likelihood (FIML) approach which allows parameter estimation in the presence of missing data.25
Ninety-five percent of the sample was White and 56% were female. Sixty-two percent of these adults were married, 95% had at least a high school education, 46.3% had a job as a manager, administrator, or professional with/without a doctoral degree, and the median annual income in 2005_before tax was $25,000–$34,999.
Measures
Low Parent-Child Bonding During Earlier Adolescence
We hypothesized a latent variable of parent-child bonding at mean age 14, which consisted of three manifest variables, i.e., identification with parents, parental affection, and parental child-centeredness. Identification with parents was created by combining measures of identification with mother and father [alpha = .92; 28 items; e.g., “I admire my mother in her role as a parent in every way.”26]. Parental affection was a combined measure of maternal and paternal affection [alpha = .72; 10 items; e.g., “She frequently shows her love for me.”27]. Parental child-centeredness was a combined measure of maternal and paternal child-centeredness [alpha =. 80; 10 items; e.g., “She likes to talk with me and be with me much of the time.”24]. Higher scores on parent-child bonding represents closer bonding while lower scores represents more distance in the parent-child bonding.
Internalizing Behaviors During Later Adolescence
We hypothesized a latent variable of adolescent internalizing behaviors at mean age 16, which was assessed by the use of 5 items assessing depression [alpha = .75; e.g., “Over the last few years, how much were you bothered by feeling low in energy or slowed down?”28], 4 items assessing anxiety [alpha = .65; e.g., “Over the last few years, how much were you bothered by feeling fearful?”28], 6 items assessing interpersonal difficulties [alpha = .74; e.g., “Over the last few years, how much were you bothered by feeling easily annoyed or irritated with other people?”28], 7 items assessing ego-integration [alpha = .62; e.g., “I generally rely on careful reasoning in making up my mind.”15], and 4 items assessing coping [alpha = .52; e.g., “What happens to me in the future mostly depends on me.”29]. These five measures then served as manifest variables for the latent construct titled internalizing behaviors.
Tobacco Use, Alcohol, and Other Drug-Related Problems During the Late Twenties and the Early Thirties
A latent variable consisting of eight manifest variables was hypothesized (four at the late twenties: adult tobacco use, alcohol, marijuana, and other illicit drug-related problems and four were assessed in the early thirties: adult tobacco use, alcohol, marijuana, and other illicit drug-related problems). We assessed the participants’ smoking cigarettes during the past five years in the late twenties and in the early thirties. The tobacco measure at each point in time had a scale coded as none (1), less than daily (2), 1–5 cigarettes a day (3), about half a pack a day (4), about a pack a day (5), and about 1.5 packs a day or more (6). Three nine-item scales (27 items) were used to assess problems related to marijuana, alcohol, and other illicit drugs (alpha range for the four manifest variables .80–.98; e.g., “My use of marijuana caused me to behave in ways that I later regretted.”).26 Each item had a response option of no (0) or yes (1).
Measurement of Health Problems During the Mid-Thirties
A latent variable of health problems was measured by assessing physical symptoms in three areas of health. Participants were asked how long a particular health problem bothered him/her during the past year. Each item had a response option of not in the past year (0), 1–4 weeks (1), 1–3 months (2), and more than three months (3). Participants were asked 14 questions in order to derive three groups of symptoms.
A. Neurocognitive symptoms (α = .71): (a) headaches; (b) trouble remembering things; (c) difficulty thinking and concentrating; and (d) trouble learning new things.26
B. Respiratory symptoms (α = .75): (a) asthma; (b) bronchitis or pneumonia; (c) coughing spells; (d) chest colds; (e) shortness of breath when not exercising; and (f) wheezing and gasping.26
C. General malaise (α = .64): (a) appetite loss; (b) trouble getting started in the morning; (c) trouble sleeping; and (d) staying home most or all of the day because of not feeling well.26
Data Analysis
A latent variable structural equation model (SEM) was used to examine the empirical validity of the hypothesized pathways. SEM is a multivariate statistical method that evaluates both the measurement quality of a set of variables used to assess a latent construct (the measurement model) and the relationships among the latent constructs (the structural model). We attempted to account for the influences of the youths’ gender, age, and parental educational level on the measurement and structural models. To do this, we used partial covariance matrices as the input matrices, which were created by statistically partialing out the effects of these demographic factors on each of the original manifest variables. This should afford us a more generalizeable model. This strategy allows us to statistically control for the effects of demographic variables without hypothesizing exactly where they influence the model. _We then employed maximum likelihood methods to estimate the models by using LISREL VIII.
To account for the non-normal distribution of the model variables, we used the Satorra-Bentler30 scaled statistic or the S-B χ2 as the test statistic for model evaluation, as recommended by Hu, Bentler & Kano.31 We chose several fit indices to assess the fit of the models: (a) the LISREL goodness of fit index, or GFI32; (b) the root mean square error of approximation (RMSEA); and (c) Bentler’s comparative fit index (CFI).30 For the GFI and CFI, values between .90 and 1.0 indicate that the model provides a good fit to the data, whereas RMSEA should be below .10.33 Total (direct plus indirect) effects of each earlier latent variable estimated in the analysis of adverse health consequences during the mid-thirties was computed in order to help in the interpretation of the structural coefficients.
RESULTS
Table 1 presents the duration of the participant’s neurocognitive health symptoms, respiratory symptoms, and general malaise. As noted in Table 1 and the Analysis Section, the health symptoms (e.g., respiratory symptoms) were somewhat skewed. As a result, we used the Bentler Procedure.30,31
Table 1.
Duration During the Past Year of Neurocognitive, Respiratory, and General Malaise Symptoms Reported by Participants During Their Mid-Thirties (N=500)
| Symptoms | Duration * | |||
|---|---|---|---|---|
| Not in the Past Year |
1–4 Weeks |
1–3 Months |
More Than 3 Months |
|
| % | % | % | % | |
| Neurocognitive Symptoms | ||||
| Headache | 43.2 | 39.7 | 9.0 | 8.1 |
| Difficulty Thinking or Concentrating | 75.7 | 16.8 | 4.1 | 3.4 |
| Trouble Remembering Things | 80.6 | 11.3 | 3.0 | 5.1 |
| Trouble Learning New Things | 93.7 | 2.8 | 1.1 | 2.4 |
| Respiratory Symptoms | ||||
| Chest Colds | 53.6 | 42.6 | 3.8 | 0.0 |
| Coughing Spells | 75.3 | 21.3 | 2.8 | 0.6 |
| Shortness of Breath When Not Exercising | 87.0 | 9.8 | 2.4 | 0.8 |
| Bronchitis or Pneumonia | 90.2 | 8.6 | 0.2 | 1.0 |
| Asthma | 91.2 | 5.2 | 0.8 | 2.8 |
| General Malaise | ||||
| Trouble Sleeping | 56.0 | 26.6 | 8.8 | 8.6 |
| Staying Home Most or All of the Day Because of Not | 56.1 | 39.9 | 2.2 | 2.2 |
| Feeling Well | ||||
| Trouble Getting Started in the Morning | 63.7 | 23.9 | 6.0 | 6.4 |
| Appetite Loss | 85.7 | 11.7 | 1.6 | 1.0 |
Note: How often during the past year did the following bother you?
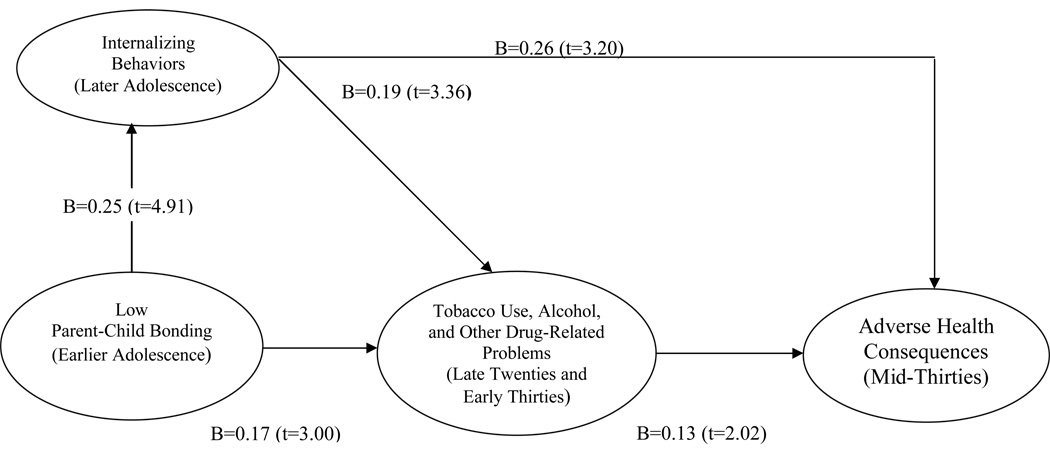
Using LISREL VIII,32 we tested the measurement model as well as the structural model, controlling for the youths’ age and gender and parental educational level. All factor loadings were significant (p<0.001). These findings show that the indicator variables were satisfactory measures of the latent constructs. The partial covariance matrices and the information about the factor loadings from the measurement model are available from the authors upon request. The Satorra-Bentler chi-square (S-B χ2) was 336.23. The following fit indices were also obtained: GFI=0.93; RMSEA=0.051, and Bentler’s CFI=0.95. These results reflect a satisfactory model fit (as previously noted). The obtained path diagram along with the standardized regression weights are depicted in Figure 1. As noted in Figure 1, low parent-child bonding during earlier adolescence was associated with later adolescent internalizing behaviors and tobacco use, alcohol, and other drug-related problems in the late 20s and early 30s (B = 0.25; t = 4.91 and B = 0.17; t = 3.00, respectively). Later adolescent internalizing behaviors was associated with tobacco use, alcohol, and other drug-related problems in the late 20s and early 30s (B = 0.19; t = 3.36), which, in turn, were directly associated with adverse health consequences in the middle 30s (B = 0.13; t = 2.02). In addition, there was a direct association between later adolescent internalizing behaviors and adverse health consequences in the middle 30s (B = 0.26; t = 3.20).
Figure 1.
Obtained Model: Adolescence/Young Adult Psychosocial Factors and Tobacco Use, Alcohol, and Other Drug-Related Problems as Related to Adult Adverse Health Consequences (N=500).
- GFI = 0.93; RMSEA=0.051; CFI=0.95;
- Parental education, age, and gender were statistically controlled;
- B=standardized path coefficient; t=t statistic;
- All Bs are significant at p < 0.05 (two-tailed tests).
Table 2 shows the following standardized total effects (STE) _based on a two-tailed test: tobacco use, alcohol, and other drug-related problems in the late 20s and early 30s (STE = 0.13; t = 2.02; p < .05); later adolescent internalizing behaviors (STE = 0.28; t = 3.44; p < .001); and earlier adolescent low parent-child bonding (STE = 0.09; t = 3.47; p < .001). Thus, each earlier latent variable had a significant total effect on adverse health consequences in the middle 30s.
Table 2.
Standardized Total Effects of Adolescent/Young Adult Psychosocial Factors and Tobacco Use, Alcohol, and Drug-Related Problems on Adult Adverse Health Consequences (N = 500)
| Adverse Health Consequences During Mid-Thirties STE (t) | |
|---|---|
| Tobacco Use, Alcohol, and Other Drug-Related Problems (Late Twenties and Early Thirties) | 0.13 (2.02)* |
| Internalizing Behaviors (Later Adolescence) | 0.28 (3.44)** |
| Low Parent-Child Bonding (Earlier Adolescence) | 0.09 (3.47)** |
1.*p<.05; ** p<0.001 (two-tailed tests);
2. STE refers to Standardized Total Effects.
DISCUSSION
This is the first longitudinal study to examine adolescent psychosocial antecedents as predictors of adverse health consequences in the mid-thirties, using SEM. Our hypotheses regarding the pathways to adverse health consequences were supported. First, there was a strong direct relationship between internalizing behaviors and later adverse health consequences. Indeed, the relationship between internalizing behaviors and health consequences was as strong, or stronger, than the effects of tobacco use, alcohol, and other drug-related problems on health. Second, the results indicated that internalizing behaviors serve as partial mediators between low parent-child bonding and later adverse health consequences. Internalizing behaviors also mediate the relationship of low parent-child bonding and tobacco use, alcohol, and other drug-related problems. Third, earlier tobacco use, alcohol, and other drug-related problems were related to later adverse health consequences and also served as mediators between earlier psychosocial difficulties and later adverse health consequences. Fourth, low parent-child bonding has long-term consequences on health, given the fact that the participants’ relationships were assessed 22 years prior to the assessment of adverse health consequences.
FIT postulates that the effects of adolescent personality and parent-child bonding on adult health outcomes are mediated in part by risk behaviors (problems resulting from tobacco use, alcohol, and other drugs).34 The influence of adolescent psychosocial difficulties on later adverse health consequences (neurocognitive health, respiratory health, and general malaise) was partially mediated by tobacco use, alcohol, and other drug-related problems, as noted above. These results provide support for FIT and point to the possible mechanisms that operate between adolescent psychosocial attributes and adult health outcomes. Furthermore, we found both direct and indirect effects of later adolescent internalizing behaviors on later health. The indirect effect of internalizing behaviors on adverse health consequences emerged over two decades despite the fact that there were many chances for other biological and psychosocial factors to influence health outcomes.
Consistent with previous findings,16 our results showed a direct link between adolescent internalizing behaviors and adverse health consequences in the mid-thirties. It may be that these measures of internalizing psychological symptoms were markers for more generalized stressful experiences predisposing to health problems.35–38
Using a community sample, our findings shed light on components of a developmental sequence over 22 years, which so far have only been examined in the literature in segments. In contrast to past studies, this study combines several psychosocial influences into a single model spanning several developmental stages. In past studies, researchers examined the separate associations between tobacco use, alcohol, and other drug-related problems and a) parent-child bonding,13, 17, 20 b) internalizing behaviors,17 and c) health.11 Our study therefore is unique in that we examined antecedents and consequences of tobacco use, alcohol, and other drug-related problems in a comprehensive SEM across several developmental stages.
Limitations
We can only present the temporal relationships among the sets of variables in our model, but cannot prove causality. For example, we examined the effects of parent-child bonding on internalizing behaviors. However, internalizing behaviors could potentially affect parent-child bonding. Internalizing behaviors might be considered a temperamental characteristic of a child, which is at least partially if not substantially under genetic influence. Some interplay between parent-child bonding and internalizing behaviors may have occurred prior to the child reaching adolescence. Future research using in-depth studies should examine the interplay of internalizing behaviors and parent-child bonding over time. In addition, future research should study earlier manifestations of externalizing behaviors, such as aggression. Future analyses with these data will include more in-depth examinations of possible gender differences in the pathways to adult health which might better illuminate the relationships between internalizing, externalizing, and drug-using behaviors and later health outcomes. It is important to take into account that not all parents are pro-social influences. In very high-risk samples, the relationships confirmed here might have to be modified.
Conclusions and Implications
The results of this investigation provide new evidence regarding the important role that tobacco use, alcohol, and other drug-related problems play in mediating the relationship between earlier adolescent psychosocial factors and later adverse health consequences. Interventions during the late twenties and early thirties should focus on tobacco use, alcohol, and other drug-related problems. Interventions during adolescence should focus on parent-child bonding and internalizing behaviors. From both public health and clinical perspectives, creating policies and programs directed at improving parent-child bonding and reducing internalizing behaviors may be instrumental in reducing tobacco use, alcohol, and other drug-related problems, and therefore, may prevent and/or reduce later adverse health consequences.
There is a long and rich history of family-focused interventions which have demonstrated the importance of bonding to effective parents during this period. The current_research provides support for family-based prevention programs39 to continue emphasizing parent-child bonding. In addition, this research gives credence to focusing on internalizing behaviors in prevention programs by Liddle39 and Szapocznik.39 School and community prevention programs might benefit by expanding their curriculum to incorporate parent-child bonding and attachment components (e.g., family or parenting workshops), in order to prevent later tobacco use, alcohol and other drug-related problems and adverse health. The Coping Power Program by Dr. John Lochman and Project STAR (Student Taught Awareness and Resistance) by Dr. Mary Anne Pentz are examples of school and community prevention programs that include parent-child bonding and attachment components to prevent substance abuse.39
In sum, this research provides support for the critical need of prevention programs for tobacco use, alcohol, and other drug-related problems, and the specific need to focus on enhancing parent-child bonding, thereby minimizing internalizing behaviors, and subsequent tobacco use, alcohol, and other drug-related problems and adverse health consequences.
ACKNOWLEDGEMENTS
This study was supported by the following NIH grants from the National Institute on Drug Abuse and the National Cancer Institiute: Research Scientist Award K05 DA00244, R01 DA003188-26, and CA 094845-06.
CONTRIBUTORS
Judith S. Brook conceived the study and supervised all aspects of its implementation. Naomi S. Katten reviewed the literature and wrote drafts of the introduction and discussion, and contributed to the writing of the manuscript. Chenshu Zhang did the statistical analysis, wrote the data analysis and result sections, and contributed to the discussion section. David W. Brook developed the theoretical framework, contributed to the design of the study, and approved the final version to be published.
HUMAN PARTICIPANT PROTECTION
The study was approved by New York University’s Institutional Review Board, protocol numbers 11462 (K05 DA00244), 11430 (R01 DA003188-26), and 11456 (CA 094845-06).
REFERENCES
- 1.Office of National Drug Control Policy. [Accessed 6/28/07];Drug Facts: Marijuana. Available at http://www.whitehousedrugpolicy.gov/drugfact/marijuana/index.html.
- 2.Jones RT. Cardiovascular system effects of marijuana. J Clin Pharmacol. 2002;42:58S–63S. doi: 10.1002/j.1552-4604.2002.tb06004.x. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control. [Accessed 12/28/07];Quick Stats: General Information on Alcohol Use and Health. Available at http://www.cdc.gov/print.do?url= http://www.cdc.gov/alcohol/quickstats/general_info.htm.
- 4.Mokdad A, Marks J, Stroup D, Gerberding J. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control. [Accessed 6/28/07];Smoking & Tobacco Use: Fact Sheet: Health Effects of Cigarette Smoking. Available at www.cdc.gov/tobacco/data_statistics/Factsheets/health_effects.htm.
- 6.Centers for Disease Control. [Accessed 6/28/07];Smoking & Tobacco Use. Available at www.cdc.gov/tobacco/basic_information/FastFacts.htm.
- 7.Healthy People 2010. [Accessed 6/28/07];What Are the Leading Health Indicators? Available at www.healthypeople.gov/LHI/lhiwhat.htm.
- 8.De Benedittis G, Lorenzetti A, Pieri A. The role of stressful life events on the onset of chronic primary headache. Pain. 1990;40:65–75. doi: 10.1016/0304-3959(90)91052-K. [DOI] [PubMed] [Google Scholar]
- 9.Friedman HS, Booth-Kewley S. The "Disease-prone personality" A meta-analytic view of the construct. Am Psychol. 1987;42(6):539–555. doi: 10.1037//0003-066x.42.6.539. [DOI] [PubMed] [Google Scholar]
- 10.Friedman HS, Tucker JS, Tomlinson-Keasey C, Schwartz JE, Wingard DL, Criqui MH. Does childhood personality predict longevity? J Pers Soc Psychol. 1993;65(1):176–185. doi: 10.1037//0022-3514.65.1.176. [DOI] [PubMed] [Google Scholar]
- 11.Conwell LS, O'Callaghan MJ, Andersen MJ, Bor W, Najman JM, Williams GM. Early adolescent smoking and a web of personal and social disadvantage. J Pediatr Child Health. 2003;39:580–585. doi: 10.1046/j.1440-1754.2003.00240.x. [DOI] [PubMed] [Google Scholar]
- 12.Allen JP, Moore C, Kuperminc G, Bell K. Attachment and adolescent psychosocial functioning. Child Dev. 1998;69:1406–1419. [PMC free article] [PubMed] [Google Scholar]
- 13.Buist KL, Dekovic M, Meeus W, van Aken MAG. The reciprocal relationship between early adolescent attachment and internalizing and externalizing problem behavior. J Adolesc. 2004;27:251–266. doi: 10.1016/j.adolescence.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 14.Dekovic M. Risk and protective factors in the development of problem behavior during adolescence. Journal of Youth and Adolescence. 1999;28:667–685. [Google Scholar]
- 15.Brook JS, Brook DW, Gordon AS, Whiteman M, Cohen P. The psychological etiology of adolescent drug use: A family interactional approach. Genet Soc Gen Psychol Monogr. 1990;116:111–267. (entire monograph) [PubMed] [Google Scholar]
- 16.Friedman HS, Tucker JS, Schwartz JE, Martin LR, Tomlinson-Keasey C, Wingard DL, et al. Childhood conscientiousness and longevity: Health behaviors and cause of death. J Pers Soc Psychol. 1995;68(4):696–703. doi: 10.1037//0022-3514.68.4.696. [DOI] [PubMed] [Google Scholar]
- 17.Fleming CB, Kim H, Harachi TW, Catalano RF. Family processes for children in early elementary school as predictors of smoking initiation. J Adolesc Health. 2002 30;:184–189. doi: 10.1016/s1054-139x(01)00327-5. [DOI] [PubMed] [Google Scholar]
- 18.Brook JS, Brook DW, De La Rosa M, Whiteman M, Johnson E, Montoya I. Adolescent illegal drug use: The impact of personality, family, and enviornmental factors. J Behav Med. 2000;24:183–203. doi: 10.1023/a:1010714715534. [DOI] [PubMed] [Google Scholar]
- 19.Brook JS, Pahl K. Predictors of drug use among South African adolescents. J Adolesc Health. 2006;38:26–34. doi: 10.1016/j.jadohealth.2004.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hill KG, Hawkins JD, Catalano RF, Abbott RD, Guo J. Family influences on the risk of daily smoking initiation. J Adolesc Health. 2005;37 doi: 10.1016/j.jadohealth.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 21.Tucker JS, Ellickson PL, Klein DJ. Predictors of the transition to regular smoking during adolescence and young adulthood. J Adolesc Health. 2003;32(4):314–324. doi: 10.1016/s1054-139x(02)00709-7. [DOI] [PubMed] [Google Scholar]
- 22.Marcus SE, Pahl K, Ning Y, Brook JS. Pathways to smoking cessation among African American and Puerto Rican young adults. AJPH. 2007;97:1444–1448. doi: 10.2105/AJPH.2006.101212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brook JS, Morojele NK, Brook DW, Rosen Z. Predictors of cigarette use among South African adolescents. Int J Behav Med. 2005;12:207–217. doi: 10.1207/s15327558ijbm1204_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cohen P, Cohen J. Life Values and Adolescent Mental Health. Mahwah, NJ: Lawrence Erlbaum Associates, Publishers; 1996. [Google Scholar]
- 25.Schaefer J, Graham J. Missing data: our view of the state of the art. Psychological methods. 2002;7:147–177. [PubMed] [Google Scholar]
- 26.Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use, 1975–2006 Volume I Secondary school students (NIH Publication No. 07-6205) Bethesda, MD: National Institute on Drug Abuse; 2007. [Google Scholar]
- 27.Schaefer E. Children's reports of parental behavior: An inventory. Child Dev. 1965;36(2):413–424. [PubMed] [Google Scholar]
- 28.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist 90-R (HSCL): A self-report symptom inventory. Behavioral Science. 1974;19:1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- 29.Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The Stress Process. Journal of Health and Social Behavior. 1981;22:337–356. [PubMed] [Google Scholar]
- 30.Satorra A, Bentler PM. American Statistical Association 1988 Proceedings of the Business and Economic Sections. Alexandria, VA: American Statistical Association; 1988. Scaling corrections for chi-square statistics in covariance structure analysis; pp. 308–313. [Google Scholar]
- 31.Hu L, Bentler PM, Kano Y. Can test statistics in covariance structure analysis be trusted? Psychol Bull. 1992;112:351–362. doi: 10.1037/0033-2909.112.2.351. [DOI] [PubMed] [Google Scholar]
- 32.Jöreskog KG, Sörbon D. LISREL 8 User's reference guide. Chicago: Scientific Software International; 1992. [Google Scholar]
- 33.Kelloway EK. Using LISREL for Structual Equation Modeling. Thousand Oaks, CA: SAGE Publications; 1998. [Google Scholar]
- 34.Brook JS, Balka EB, Fei K, Whiteman M. The effects of parental tobacco and marijuana use and personality attributes on child rearing in African-American and Puerto Rican young adults. Journal of Child and Family Studies. 2006;15:153–164. doi: 10.1007/s10826-005-9010-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burrows GD. Editorial: It is now the time to further help the professionals and the public understand the nature, role and implications of stress for ill-health. Stress and Health. 2006;22:139–141. [Google Scholar]
- 36.Kiecolt-Glaser JK, Preacher KJ, MacCallum RC, Atkinson C, Malarkey WB, Glaser R. Chronic stress and age-related increases in the proinflammatory cytokine IL-6. Proc Natl Acad Sci U S A. 2003;100(15):9090–9095. doi: 10.1073/pnas.1531903100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tian J, Wang X. An epidemiological survey of job stress and health in four occupational populations in Fuzhou city of China. Stress and Health. 2005;21(2):107–112. [Google Scholar]
- 38.Weekes NY, MacLean J, Berger DE. Sex, stress, and health: Does stress predict health symptoms differently in the two sexes? Stress and Health. 2005;21(3):147–156. [Google Scholar]
- 39.Sloboda Z, Bukowski WJ. Handbook of Drug Abuse Prevention: Theory, Science, and Practice. New York: Springer Publishing Company; 2003. [Google Scholar]