Abstract
Mindfulness-based stress reduction (MBSR) and aerobic exercise training (AET) programs improve health and wellbeing. Exercise participation has been related to mindfulness and may be altered by MBSR training.
PURPOSE
Compare 8-weeks of MBSR, AET and no-treatment control during the fall season on objectively-measured physical activity in healthy adults.
METHODS
Participants (n=66) wore an Actigraph GT3X+ accelerometer for seven days pre-randomization, and following 8-week MBSR or AET interventions, or neither (control). Mean daily minutes (min) of moderate-to-vigorous physical activities (MVPA) were calculated along with weekly time spent in bouts of MVPA ≥10 min (MVPABouts) to assess physical activity sufficient to meet national guidelines. Groups were compared on pairwise changes in outcomes across time. Effect sizes were calculated using Cohen’s d.
RESULTS
Sufficient data (≥3 weekdays, ≥1 weekend day, ≥10 hours/day) were obtained from 49 participants (18 MBSR, 14 AET, 17 control). Daily MVPA decreased in all groups from pre-randomization to post-intervention (Aug-Nov); control decreased 17.9±25.7 min/day, MBSR decreased 5.7±7.5 min/day, and AET decreased 7.4±14.3 min/day (mean±SD), without significant differences among the groups (all p>0.05). MVPABouts decreased 77.3±106.6 min/week in control and 15.5±37.0 min/week in MBSR (between-group difference: p=0.08; d=0.86), while it increased by 5.7±64.1 min/week in AET (compared to control: p=0.029; d=0.97; compared to MBSR; p=0.564; d=0.29).
CONCLUSION
Data from participants in a randomized controlled trial showed that while AET increases moderate-to-vigorous physical activity bouts compared to no treatment, MBSR training may also mitigate the influence of shorter day length and cooler weather on participation in physical activities. Future research is needed to determine how MBSR affects exercise to inform interventions. Interventions combining MBSR and exercise may be particularly successful at increasing physical activity participation.
Keywords: Meditation, mindfulness, accelerometer, aerobic exercise, sedentary
Introduction
People who are regularly active or physically fit have better health in almost every measurable dimension when compared to inactive or less-fit individuals: psychological wellbeing, lower risk of cancer, cardiovascular disease, reduced all-cause mortality, longer life span, etc. (1–5). Yet, participation rates in exercise remain low, especially when measured objectively (6–8). Therefore, there is significant interest in optimizing interventions to increase participation in higher intensity activity, including regular ‘exercise’ (i.e., planned, structured and repetitive bouts where the goal is to improve or maintain physical fitness) (9) and through increasing non-structured time spent in moderate-to-vigorous physical activity (MVPA) across the day. Physical activity participation is typically affected by seasonal changes in weather and temperature patterns (10) which adds another barrier in areas with significant seasonal weather variation. Given the low adherence rates in spite of the benefits of exercise, creative ways are needed to increase participation in physical activity during times of the year when weather may limit physical activity participation.
Mindfulness-based stress reduction (MBSR) programs can improve both physical and psychological wellbeing in both healthy and clinical populations (11) with accrued benefits comparable to those achieved via exercise training programs (12, 13). However, because the focus is often on the meditative aspects, and thus the more sedentary aspects of the intervention, less attention has been given to whether MBSR may change participation in higher intensity physical activity. Moreover, high-quality research evaluating the benefits of structured MBSR training is still rare (for reviews and associated commentary, see (13–15)) pointing to a need for methodologically sound trials that include physical activity as an outcome. Indeed, there may be some similar psychological benefits of aerobic exercise training (AET) to MBSR, including the mindful focus during training and stress reduction post-exercise (16), making it a valid comparator. Adults with higher objectively-measured physical activity report greater psychological wellbeing and better mindfulness skills than their less active peers (17) and mindfulness can predict physical activity behavior among those with higher mindfulness (18). A recent meta-analysis found a small-to-moderate effect (d = .42) increase in self-reported physical activity following randomized controlled trials of mindfulness training in overweight or obese adults (19). Therefore, training in mindfulness may lead to greater participation in physical activity, although few studies have assessed changes in exercise or physical activity levels after MBSR training and none have done so with an objective method of physical activity assessment.
Potentially synergizing with low levels of moderate-to-vigorous physical activity, excessive time spent sedentary (or time spent sitting, reclining or in a lying posture while awake with low energy expenditure [<1.5 METs]) (20, 21) is also related to many poor health outcomes (22–24). Large amounts of prolonged sedentary time have been consistently related to negative mental health and wellbeing (25–29). Thus, it is also important for interventions designed to improve physical activity to assess their influence on sedentary time (30), particularly as sedentary time also appears to be impacted by seasonal weather changes with sedentary time increasing during the fall months (31). Programs that influence physical activity (i.e., MBSR and AET) may have secondary effects on sedentary time or changing sedentary patterns (e.g., decreasing the duration of prolonged sedentary bouts). It is possible that MBSR and AET may have different effects on sedentary behavior, although this question has yet to be explored.
A randomized, controlled trial (RCT), Mindfulness or Exercise to Prevent Acute Respiratory Infection (MEPARI-2), offered the unique opportunity to assess the relative influence of MBSR and AET on physical activity and sedentary time in generally healthy adults. The primary aim of the present analysis was to compare the effects of eight weeks of AET, MBSR training and no-treatment control on objectively-measured physical activity and sedentary behavior during the fall season. Specifically, two primary questions were addressed:
Do MBSR and AET programs differentially influence objectively-monitored daily physical activity and weekly exercise relative to a no-treatment control?
Do MBSR and AET programs alter sedentary behavior (total minutes or minutes of prolonged bouts lasting longer than 30 or 60 min)?
Methods
Participants and Procedures
This is a secondary analysis from a RCT evaluating the effects of MBSR and AET on reducing the incidence, duration and severity of acute respiratory infection (MEPARI2). The trial is described on clinicaltrials.gov (NLM identifier: NCT01654289) and is partially reported elsewhere (32). The results reported here are from an add-on assessment offered to the fourth and final cohort of the MEPARI2 trial.
MEPARI2 enrolled community-dwelling healthy adults (ages 30–69 years) from the Madison, WI area through local advertisements. After a successful phone screening, prospective participants were invited to enroll in a two-week run-in phase to assess inclusion/exclusion criteria and likelihood of compliance. Potential study participants who reported being inactive at baseline (as defined by self-reporting not regularly exercising vigorously twice per week or moderately three times per week) and susceptible to colds (i.e., self-report ≥1 cold annually) were invited to participate. Following successful completion of this phase, participants provided informed consent for the main trial and were randomly assigned to one of three conditions: MBSR, AET, or to serve as observational controls. The MBSR and AET interventions involved 8 weeks of group classes (2.5 hr sessions weekly) and included instructions to participate in the designated activity (exercise or meditation) outside of the weekly classes. The MBSR and AET interventions were delivered in group therapy settings and matched in terms of class location (healthcare facility), similar class size (~15 participants per class), and in-class time (2.5 hours/week). There were also similar instructions for 20–45 min of daily practice at-home during the 8-week training period as well as a 6-hr weekend retreat around the 7th week of the intervention. Run-in and randomization occurred in July and August (summer months) with classes being held in September and October (fall months), and post-intervention assessments scheduled in November (end of fall).
MBSR training
Training in MBSR was accomplished through a standardized 8-week behavioral training routine in mindfulness meditation (33), which consisted of one session each week lasting 2.5 hr with encouragement for participants to perform 20 to 45 min of at-home practice each day. The MBSR program, used across the U.S., begins by guiding participants in body sensation awareness (body scan), sitting meditation, and mind-body imagery. Participants were then introduced to mindful stretching and walking (mindful movement) and breathing exercises, and encouraged to incorporate mindfulness in their daily activities. Instruction included information and training in practices promoting an adaptive, mindful response to physical, emotional, cognitive and interpersonal stressors. Instructors for the MBSR group had completed the Mindfulness-Based Stress Reduction Mind-Body Medicine Professional Training and the Teacher Practicum Intensive in Mindfulness Based Stress Reduction, both with the Center for Mindfulness at the University of Massachusetts Medical School.
Aerobic Exercise training (AET)
AET focused on participating in aerobic activities, such as walking or jogging, which would be easy to perform without the need for specialized equipment. In accordance with the 2008 guidelines, the goal for participants was sustained moderate intensity physical activity for 20 to 45 minutes each day, aiming for at least 150 min per week in bouts of at least 10 min (34). Exercise intensity was monitored via self-assessment using Borg’s Rating of Perceived Exertion (RPE) with a target RPE during each exercise bout of 12 to 16 (moderate to hard) (35). Each weekly 2.5 hr session included 1.5 hr of classroom-based instruction and 1 hr of group activity in a fitness center, with the remainder of the 150 min weekly goal to be accomplished through at-home practice using RPE to monitor intensity. The classroom portion began with a review of the previous week’s activities before proceeding to a brief presentation on various exercise techniques and effects, a discussion of strategies and principles of behavior change, and ended by a discussion of activity goals for the upcoming week. The physical activity retreat lasted a half-day and included didactics, group discussion and activities, and time for individual physical activity practice. Instructors in the AET group were clinical exercise physiologists (MS or higher).
Weekly practice logs
Each week, participants entered daily practice minutes via computerized self-report of moderate and vigorous physical activity in the AET group only or daily practice minutes of informal and formal meditative practice in the MBSR group only. Intensity levels of exercise practice were defined as: “A moderate level of physical activity noticeably increases your heart rate and breathing rate. You may sweat, but you are still able to carry on a conversation. With vigorous activity, you are breathing rapidly and are only able to speak in short phrases. Your heart rate is substantially increased and you are likely to be sweating.” Mindfulness practice types were defined as: “Formal practice is when you schedule specific time to just do that particular activity. For example, scheduling 15 minutes to sit and focus on your breath is formal meditation practice. Taking a moment to notice your breath during your work day is informal practice. Scheduling time to take a walk for the purpose of practicing meditation is formal practice. Walking mindfully from your kitchen to the living room is informal practice.” Participants were asked to prospectively record practice minutes each day on paper, and then to enter data once weekly.
ABC sub-study
Every participant who provided informed consent for the MEPARI2 study for the final wave of recruitment in 2015 was offered the opportunity to participate in the ABC (Accelerometry and Breath-Counting) sub-study. The ABC sub-study participants were asked to wear an accelerometer for 7 days during the run-in phase of the study (prior to randomization; baseline – end of summer) and for another 7 days following the 8-week interventions (post-intervention – end of fall). The University of Wisconsin-Madison Institutional Review Board approved both the main trial and the sub-study. Written informed consent was obtained from all participants.
Accelerometry
The Actigraph GT3X+ accelerometer was used in the present study to objectively monitor physical activity across the intervention. This accelerometer has been shown to reliably measure free-living activity in healthy adults (36). Participants were instructed to wear the accelerometer on a belt on their waistline for 7 full days during all of their waking hours (except while participating in water-based activities). Participants were asked to put on the accelerometer before getting out of bed in the morning and to take it off as they were getting into bed to go to sleep each night with participants keeping a log of on/off time. Data were collected continuously in 1-sec epochs. After at least 7 full days, participants returned their accelerometers to study staff.
Data Processing and Analysis
All statistical analyses were performed in R 3.4.1 (Single Candle; R Foundation for Statistical Computing, Vienna, Austria). Accelerometer data were initially downloaded by ActiLife Version 6.12.0 (Actigraph, LLC, Pensacola, FL) and then processed via the Sojourns 3-axis method (37). Non-wear time was defined as 60 consecutive min of zero values on all three axes and was removed from analysis. Type I error rate was held at 0.05 for each statistical test and pairwise comparison. Pre-intervention sedentary time and physical activity levels were assessed via pairwise comparisons among the three groups. Means and standard deviations are used to describe the self-reported amount of exercise and meditation practice across the intervention periods. To estimate the magnitude of differences, Cohen’s d effect sizes were calculated where appropriate (38).
Accelerometer Processing
Participants were included in the analysis if they provided at least 10 hr/day of valid wear time for at least 3 weekdays and 1 weekend day both before and after the interventions. The sojourn-3 axis method (37) provides robust measurement of physical activity intensity and was used for processing the accelerometer data. Briefly, this method uses a neural network to identify transitions in the movement pattern across all three axes and breaks the data into sojourns, or bouts, of activity where each sojourn appears to be a distinct activity. Each sojourn is assigned a MET value based upon the count distribution across the three axes, and, based upon the MET value, each sojourn was classified as sedentary (0–1.5), light (1.5–3), moderate (3–6) or vigorous (6+) intensity activity. Time spent participating in each category of physical activity and sedentary behavior is expressed as the average daily minutes engaged in each type of activity. Time spent in bouts of physical activity of either moderate or vigorous intensity (or a combination) lasting longer than 10 min were summed to provide weekly minutes toward meeting physical activity guidelines (34). Similarly, for prolonged or extended sedentary time, minutes spent in bouts of sedentary time that lasted longer than 30 min or longer than 60 min were averaged to determine the mean time each participant spent engaged in prolonged sedentary activities.
Specific Aim 1
Means and standard deviations were calculated for average daily minutes of physical activity in each category (light, moderate or vigorous) for each group at baseline and post-intervention. Minutes in moderate-to-vigorous physical activity (MVPA) are reported to evaluate minutes of potentially exercise-related behavior. Weekly minutes of MVPA in bouts lasting longer than 10 min were compared across the groups to assess minutes of exercise of sufficient duration to meet physical activity guidelines of 150 minutes of MVPA in bouts lasting longer than 10 min (34). Changes in physical activity were compared across the groups using pairwise comparisons of the change scores (post-pre) between each pairing of the three groups (i.e. MBSR vs. AET, MBSR vs. control and AET vs. control).
Specific Aim 2
Average minutes spent in sedentary activities were calculated across the week of activity monitoring by taking each participant’s mean number of minutes spent sedentary on valid days of wear time. Changes in minutes spent in sedentary activities (total, bouts 30+ and bouts 60+) were compared across the groups using a 3 (group; MBSR, AET, control) X 2 (time; baseline, post-intervention) ANOVA with pairwise comparisons of the change scores (post-pre) between each pairing of the three groups.
Results
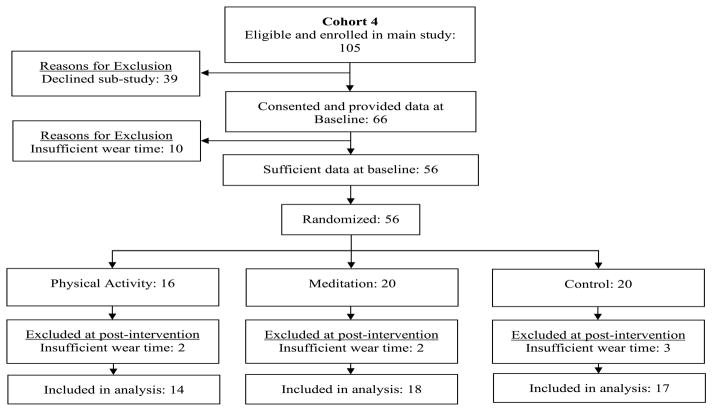
Out of the 105 participants who enrolled in the run-in trial in the fourth cohort of MEPARI2, 66 provided consent for the sub-study and were fitted with an accelerometer at run-in (Figure 1). Of those, 10 provided insufficient data or did not progress beyond run-in, leaving 56 to be randomized. Participants who did not provide sufficient data or did not progress beyond the run-in period were not significantly different than those who did in terms of age, gender, BMI, race or education (t-tests [age and BMI] and chi-square tests [gender, race and education], all p > 0.05). Of the 56 who were randomized, twenty were assigned to the control group, 16 to AET, and 20 to MBSR. At post-intervention, 7 participants did not return the accelerometer with sufficient data, including 2 in the MBSR group, 2 in the AET group, and 3 in the control group. For this completers-only set of analyses, the final sample included 18 in the MBSR group, 14 in the AET group, and 17 in the control group. Participants were predominantly female (82%), in middle adulthood (age: 51.9 ± 11.1 years), generally overweight (BMI: 31.3 ± 7.8), identified as white or Caucasian (90%) and well educated with 98% having at least some college education (Table 1). Participants provided 6.6 mean days of valid wear time pre-intervention and 6.5 mean days at post-intervention with mean daily wear time of 14.7 hr/day and 14.3 hr/day, respectively.
Figure 1.
CONSORT diagram showing the flow through the sub-study. If accelerometers did not contain at least 10 hours of valid data on ≥3 weekdays and ≥1 weekend days then they were not included in the analysis.
Table 1.
Demographic Information
| Entire cohort(n = 49) | Control (n = 17) | Meditation(n = 18) | Exercise(n = 14) | |
|---|---|---|---|---|
| Age (years), mean (SD) | 51.9 (11.1) | 49.6 (11.2) | 50.9 (12.5) | 55.9 (8.3) |
| BMI, mean (SD) | 31.3 (7.8) | 29.3 (6.6) | 32.1 (9.2) | 32.9 (7.2) |
| Male, sex, n (%) | 9 (18%) | 2 (11%) | 4 (22%) | 3 (21%) |
| Race, n (%) | ||||
| Black/African American | 3 (6%) | 0 (0%) | 2 (11%) | 1 (7%) |
| White/Caucasian | 44 (90%) | 15 (88%) | 16 (89%) | 13 (93%) |
| Asian | 1 (2%) | 1 (6%) | 0 (0%) | 0 (0%) |
| Other | 1 (2%) | 1 (6%) | 0 (0%) | 0 (0%) |
| Education, n (%) | ||||
| Some high school | 1 (2%) | 0 (1%) | 1 (6%) | 0 (0%) |
| Some college/tech school | 10 (20%) | 4 (24%) | 3 (17%) | 3 (21%) |
| College grad (bachelor’s) | 14 (29%) | 6 (35%) | 3 (17%) | 5 (36%) |
| College post grad (master’s, doctoral) | 24 (49%) | 7 (41%) | 11 (61%) | 6 (43%) |
Across the study period, participants averaged around 11.5 hr/day of sedentary time, just over 2 hr/day of light intensity activity, slightly under 1 hr/day of moderate and around 10 min/day of vigorous intensity activity (Table 2). Minutes spent in each of the activity categories decreased from August (pre-intervention) to November (post-intervention), while sedentary minutes increased slightly. There were no significant pre-intervention pairwise differences pre-intervention between any of the groups for time spent engaged in either physical activity or sedentary behavior (all p < 0.05; Table 2).
Table 2.
Time spent in intensity categories across groups and time
| Pre-Intervention | Post-Intervention | |||||
|---|---|---|---|---|---|---|
| Control (n=17) | Exercise (n=14) | MBSR (n=18) | Control (n=17) | Exercise (n=14) | MBSR (n=18) | |
| Sedentary Time | ||||||
| Total | 669 (85) | 685 (82) | 663 (107) | 664 (106) | 695 (77) | 668 (103) |
| Bouts of 30+ min | 354 (103) | 337 (92) | 322 (124) | 380 (87) | 378 (80) | 351 (112) |
| Bouts of 60+ min | 192 (104) | 155 (79) | 161 (114) | 218 (81) | 183 (61) | 191 (90) |
| Physical Activity | ||||||
| Light | 133 (44) | 142 (41) | 140 (54) | 113 (35) | 127 (30) | 124 (42) |
| Moderate | 61 (32) | 62 (17) | 63 (29) | 44 (13) | 52 (16) | 61 (33) |
| Vigorous | 13 (8) | 9 (4) | 12 (10) | 11 (9) | 12 (7) | 8 (6) |
| MVPA | 73 (38) | 72 (19) | 74 (37) | 55 (19) | 64 (20) | 69 (37) |
| Bouts of 10+ min MVPA | 155 (161) | 112 (63) | 111 (117) | 77 (90) * | 118 (102) * | 95 (118) |
Data are expressed as mean minutes/day of each variable (except ‘Bouts of 10+ min MVPA’ which is expressed in min/week) within each group (mean SD). No significant differences existed between sessions at baseline (all p >0.05).
indicates a significant difference (p < 0.05) for the pairwise comparison between change scores pre to post intervention between the exercise and control groups.
Abbreviations: MBSR: mindfulness-based stress reduction, MVPA = moderate-or-vigorous physical activity.
During the interventions, participants in the MBSR group reported 344 total minutes of meditation practice on average each week (73 informal and 271 formal), while participants in the exercise group reported 316 total minutes of MVPA on average each week (232 moderate and 84 vigorous; Table 3).
Table 3.
Self-reported average weekly practice minutes in the intervention groups
| Meditation (n = 18) | Exercise (n = 14) | |
|---|---|---|
| Informal meditation or moderate exercise | 73 (50) | 232 (97) |
| Formal meditation or vigorous exercise | 271 (71) | 84 (79) |
| Total (informal + formal OR moderate + vigorous) | 344 (99) | 316 (102) |
Data represent weekly means (SD) of minutes/week across the eight intervention weeks. Meditation group participants self-reported minutes spent practicing informal and formal meditation; exercise group participants self-reported minutes spent practicing moderate or vigorous intensity exercise.
Specific aim 1
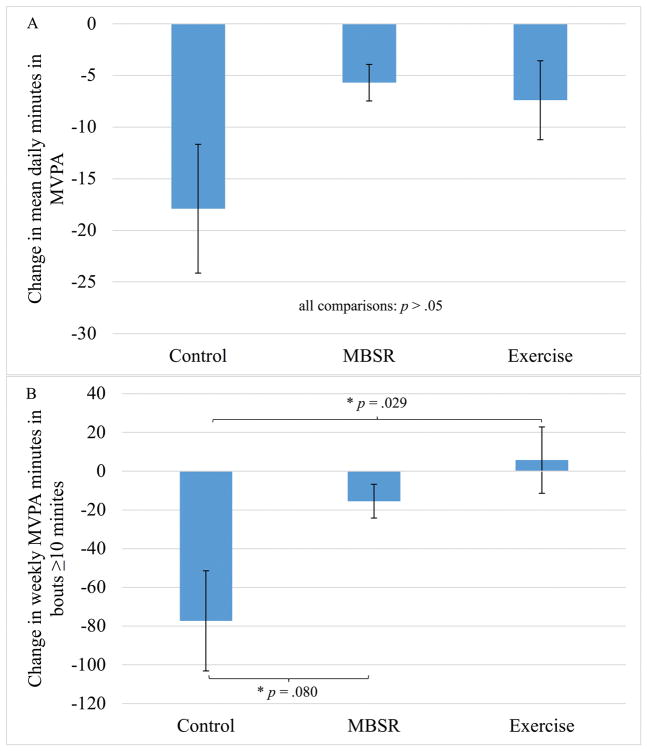
Daily MVPA decreased in all groups from pre-enrollment to post-intervention (Aug-Nov); the MBSR group decreased 5.7±7.5 min/day, the AET group decreased 7.4±14.3 min/day, and the control group decreased 17.9±25.7 min/day (mean±SD), without significant differences among the groups (all p>0.05, see Figure 2A). MVPA bouts lasting at least 10 minutes decreased 15.5±37.0 min/week in the MBSR group, increased 5.7±64.1 min/week in the AET group, and decreased 77.3±106.6 min/week in the control group. However, for exercise-related behavior, pairwise comparisons revealed no significant difference between changes in MVPA in bouts lasting longer than 10 minutes between the MBSR and AET groups (p = 0.564, d= 0.29). There was a nonsignificant difference favoring MBSR in the comparison between MBSR and control (p = 0.080, d = 0.86), and a significant difference between the AET and control groups (p = 0.029; d = 0.97; Figure 2B).
Figure 2.
Mean changes across the 8-week interventions by group for overall daily moderate-to-vigorous physical activity (MVPA) [A] or weekly minutes in MVPA in bouts of at least 10 minutes [B] (error bars represent the standard error of the mean). P-values indicate pairwise comparisons of change scores across the intervention between groups. * indicates p < 0.05.
Specific aim 2
For total daily sedentary time, there was not a differential effect of group by time; the interaction term was not significant (F2,92 = 0.042, p = 0.959) with no main effect of group (F2,92 = 0.598, p = 0.552) or time (F1,92 = 0.034, p = 0.855). When categorizing total sedentary time into bouts lasting longer than 30 min, there was not a differential effect of group by time; the interaction term was nonsignificant (F2,92 = 0.049, p = 0.952) with no main effect of group (F2,92 = 0.812, p = 0.447) or time (F1,92 = 2.243, p = 0.138). For daily sedentary time in bouts longer than 60 min, there was again not a differential effect of group by time; the interaction term was nonsignificant (F2,92 = 0.015, p = 0.986) with no main effect of group (F2,92 = 1.442, p = 0.242) or time (F1,92 = 3.817, p = 0.054). There were no significant pairwise comparisons among the groups for total daily sedentary time, sedentary time in 30+ or 60+ min bouts (all p > 0.05).
Discussion
Our analyses indicated a significant difference between the changes in physical activity accumulated in 10+ min bouts (i.e., exercise of intensity and duration sufficient to count toward meeting physical activity guidelines) between the AET and control groups across the 8-week interventions. This effect demonstrates a positive benefit of AET on objectively-monitored exercise participation (Figure 2). Unexpectedly, AET and MBSR had similar effects across the interventions in terms of total daily MVPA and weekly MVPA in 10+ min bouts indicating that MBSR and aerobic exercise training may have similar effects on overall physical activity behavior. These results are particularly noteworthy given the much larger decreases in daily physical activity (−17.9 min/day) and weekly exercise (−77.3 min/week) that were seen in the control group. The decline in MVPA across time was potentially the result of the seasonal scheduling of our training intervention and subsequent data collection (i.e., end of summer to end of fall). The results suggest that MBSR training may convey positive effects on physical activity behavior of a similar magnitude to those achieved by structured exercise training. Future work is now needed to clarify the effects of MBSR on physical activity and formal exercise and to determine if specific aspects of the MBSR training influence participation in physical activity. There may be unique aspects of MBSR, such as stress reduction or being mindful in the present moment, that will prove useful to incorporate into interventions that are designed to optimize participation in physical activity.
Neither AET nor MBSR prevented the increase in time spent sedentary that was also prominent in the control group. There were negligible between-group differences for total time spent sedentary and the shift in time spent sedentary towards longer bouts across the intervention (Table 2). This shift to longer bouts was not unexpected as the intervention occurred during the fall and previous research has noted a seasonal shift in sedentary patterns incorporating more time and longer bouts during winter months (31). The present findings suggest that sedentary behavior may not appear to be influenced by MBSR or AET programs. It is possible that future interventions may need to intentionally target a reduction in sedentary behavior as a goal, or address specific correlates of sedentary behavior, in order for meaningful reductions to occur (for reviews and further analysis of changing sedentary behavior, see (39–41)).
Accelerometry is regularly employed in physical activity assessment trials but has yet to be adopted as routine practice in trials evaluating the health benefits of training in mindfulness, making our report of MBSR training relatively unique. Following a combined exercise and meditation intervention (via a mindfulness CD), Rabin and colleagues (42) found that young adult cancer survivors increased their physical activity by self-report but not when assessed via 3-days of objective measurement. Grossman and colleagues (43) assessed a single day of physical activity following 8-weeks of MBSR training via accelerometry and did not see a difference in activity patterns in fibromyalgia patients. Although not assessing objective physical activity, Martin and colleagues (44) combined a mindfulness intervention with a fitness walking program and found improvements in 1-mile walking test time and cardiorespiratory fitness (VO2max); however, there were no control groups to determine the specific effect of the mindfulness training. Fulwiler and colleagues reported that interventions are beginning to combine mindfulness practices with exercise to enhance their intervention programs (45), yet objective monitoring of physical activity changes is still rare in mindfulness research. The present analysis, which was based on objective monitoring within a RCT, supports the conclusions from previous research with self-reported physical activity. It indicates that MBSR can positively impact PA participation (19), an effect that warrants further study.
The present trial provides preliminary evidence of a preservation of physical activity following a standardized 8-week MBSR training program that is comparable to the effect of an AET program. These results highlight a potential unintended health-related benefit of MBSR (i.e., increasing physical activity or preventing physical activity declines). They also highlight a need for future trials to monitor physical activity to replicate the effect of MBSR on this outcome. In situations where physical activity participation is expected to decline or aerobic exercise training may not be feasible (e.g., after surgery, during chemotherapy, etc.), MBSR training could be a useful tool for maintaining physical activity participation.
Physical activity guidelines indicate that exercise should be accumulated in bouts of at least 10 minutes for the health-enhancing effects to occur (34). However, physical activity that is sustained for shorter bouts may also be relevant for health promotion and disease prevention. In the present study, all three groups decreased MVPA when there was no bout threshold (i.e., every minute of MVPA across the day); although the AET group had a blunted decrease compared to the controls (moderate effect size; d=0.53) with greater mitigation in the MBSR group (d=0.73) and little difference between the intervention groups (d=0.15; <2 min; Figure 2). The seasonal decline in the present study in all groups is in accordance with data from a sample of 1,166 adults, where middle-aged adults showed a change in objectively-measured MVPA of −10.7 minutes from summer to winter (46). Therefore, the +10 min difference in the change across the intervention in AET compared to controls and +11 min in MBSR compared to controls suggest a large influence on preventing seasonal declines in physical activity.
In terms of MVPA accumulated in bouts of sufficient duration to meet national recommendations (i.e., 10+ min at a time), the control group had a large seasonal-decrease in their MVPA while the AET group increased their weekly activity slightly (moderate effect size difference; d = 0.71, +83 min compared with control change), and the MBSR group slightly decreased their weekly activity with a moderate difference from the controls (d = 0.64, +62 min) and, again, little difference between the intervention groups (d = 0.29; 21 min). Compared to changes in the control group, participants in the intervention groups were better off by roughly half of the weekly 150 min of MVPA recommendation across the intervention. Moving from sedentary adults to those who accumulate roughly half of the physical activity guidelines results in myriad benefits, such as extending life expectancy by 1.8 years (47). In our participants who had self-identified as inactive prior to inclusion in the study, the roughly 75-minute improvement in activity compared to the Controls is encouraging given that the largest benefit of participation in physical activity is seen in people moving from being inactive to even a small amount of physical activity (34, 48). The present findings suggest that, whether physical activity behavior is evaluated via daily minutes of MVPA or weekly minutes in 10+ min bouts, MBSR and AET had similar effects on blunting the expected seasonal decline (10) with moderate-to-large effects in this previously inactive sample. Given that MBSR training does not specifically promote exercise participation, it is surprising to find a similar effect to a more traditional exercise training program on physical activity and exercise participation.
Limitations
This was a secondary data analysis of a subset of participants in a trial designed to evaluate the influence of the mindfulness and exercise interventions on acute respiratory infections. Thus, future research with directed hypotheses is now needed to confirm the effects of mindfulness training on physical activity reported here. We also acknowledge the relatively small group sizes, which limit statistical power, as well as the exploratory, hypothesis-generating nature of this report. Although accelerometers can provide nuanced information regarding movement, they do not provide other contextual information that may be particularly relevant in understanding the adverse health effects of sedentary time (e.g., being alone vs. with others, TV viewing vs. reading, etc.). The seasonal nature of the MEPARI2 trial (end of summer to end of fall) also meant that participants had a natural tendency to decrease their physical activity. Although the MBSR and AET groups showed a substantial mitigation of this seasonal shift toward less activity as compared to Control. It would now be of interest to determine if either MBSR or AET programs would yield even larger incremental gains during a time of year with longer day-length when it is more conducive to engage in outside activity. Finally, selection of accelerometer type (Actigraph GT3X+) and data analytic techniques for accelerometers can influence results and their interpretation (49). Our data were processed with the Sojourns 3-axis method (37), which has been shown to perform particularly well for differentiating both low intensity activities (e.g., sedentary time) and for higher intensity activities (e.g., exercise).
Conclusions
These results from 49 participants in a RCT showed that while AET increases MVPA in bouts lasting longer than 10 min as compared to no treatment, training in MBSR may also lessen seasonal declines in physical activity. However, in this study, neither AET nor MBSR significantly influenced the amount of time spent sedentary. For reductions in sedentary time to occur, this behavior may need to be a specific target of the intervention. Future research is needed to determine how MBSR affects physical activity to inform future exercise promotion interventions. Combining MBSR and exercise training, or sequentially providing the two interventions, may be more successful at influencing physical activity than current approaches.
Acknowledgments
Funding for the MEPARI2 trial came from National Institutes of Health, National Center for Complementary and Integrative Health (NCCIH; R01AT006970). JM was supported by the Health Resources and Services Administration (HRSA; T32HP10010) during his time on this project while MG was supported by NCCIH (T32AT006956). Bruce Barrett was supported by a mid-career research and mentoring grant from NCCIH (K24AT006543). AEZ’s work was supported by the K23AA017508 award from the National Institutes of Health National Institute on Alcohol Abuse and Alcoholism. ET was supported by the University of Wisconsin-Madison Office of the Vice Chancellor for Research and Graduate Education Fall Competition Award, the UW Institute for Clinical and Translation Research (ICTR) Scholars Program, and the Clinical and Translational Science Award program through the NIH National Center for Advancing Translational Sciences (UL1TR000427 & KL2TR000428, PI: Drezner). The trial was registered at ClinicalTrials.gov before the first participant was enrolled (NCT01654289). The authors would like to acknowledge the significant work performed by members of the study team including Shari Barlow, Mary Checovich, Supriya Hayer, Jodi Barnet, Amber Schemmel, Eric Anderson and Jaylene Thompson, and the participants for their time and effort.
Footnotes
Conflicts of Interest: The authors report no conflicts of interest. The results of the present study do not constitute endorsement by ACSM. The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
References
- 1.Wen CP, Wai JPM, Tsai MK, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. The Lancet. 2011;378(9798):1244–53. doi: 10.1016/S0140-6736(11)60749-6. [DOI] [PubMed] [Google Scholar]
- 2.Lee IM. Physical activity and cancer prevention--data from epidemiologic studies. Med Sci Sports Exerc. 2003;35(11):1823–7. doi: 10.1249/01.MSS.0000093620.27893.23. [DOI] [PubMed] [Google Scholar]
- 3.Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301(19):2024–35. doi: 10.1001/jama.2009.681. [DOI] [PubMed] [Google Scholar]
- 4.Scully D, Kremer J, Meade MM, Graham R, Dudgeon K. Physical exercise and psychological well being: a critical review. Br J Sports Med. 1998;32(2):111–20. doi: 10.1136/bjsm.32.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Myers J. Exercise and Cardiovascular Health. Circulation. 2003;107(1):e2–5. doi: 10.1161/01.cir.0000048890.59383.8d. [DOI] [PubMed] [Google Scholar]
- 6.Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71(sup2):1–14. doi: 10.1080/02701367.2000.11082780. [DOI] [PubMed] [Google Scholar]
- 7.Ham SA, Kruger J, Tudor-Locke C. Participation by US adults in sports, exercise, and recreational physical activities. J Phys Act Health. 2009;6(1):6–14. doi: 10.1123/jpah.6.1.6. [DOI] [PubMed] [Google Scholar]
- 8.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 9.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–31. [PMC free article] [PubMed] [Google Scholar]
- 10.Tucker P, Gilliland J. The effect of season and weather on physical activity: a systematic review. Public Health. 2007;121(12):909–22. doi: 10.1016/j.puhe.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 11.Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. J Psychosom Res. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 12.Creswell JD. Mindfulness interventions. Annu Rev Psychol. 2017;68(1):491–516. doi: 10.1146/annurev-psych-042716-051139. [DOI] [PubMed] [Google Scholar]
- 13.Goyal M, Singh S, Sibinga EMS, et al. Meditation Programs for Psychological Stress and Well-being: A Systematic Review and Meta-analysis. JAMA Intern Med. 2014;174(3):357–68. doi: 10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Van Dam NT, van Vugt MK, Vago DR, et al. Mind the Hype: A Critical Evaluation and Prescriptive Agenda for Research on Mindfulness and Meditation. Perspect Psychol Sci J Assoc Psychol Sci. 2018;13(1):36–61. doi: 10.1177/1745691617709589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davidson RJ, Dahl CJ. Outstanding Challenges in Scientific Research on Mindfulness and Meditation. Perspect Psychol Sci J Assoc Psychol Sci. 2018;13(1):62–5. doi: 10.1177/1745691617718358. [DOI] [PubMed] [Google Scholar]
- 16.Ulmer CS, Stetson BA, Salmon PG. Mindfulness and acceptance are associated with exercise maintenance in YMCA exercisers. Behav Res Ther. 2010;48(8):805–9. doi: 10.1016/j.brat.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 17.Kangasniemi A, Lappalainen R, Kankaanpää A, Tammelin T. Mindfulness skills, psychological flexibility, and psychological symptoms among physically less active and active adults. Ment Health Phys Act. 2014;7(3):121–7. [Google Scholar]
- 18.Chatzisarantis NLD, Hagger MS. Mindfulness and the Intention-Behavior Relationship Within the Theory of Planned Behavior. Pers Soc Psychol Bull. 2007;33(5):663–76. doi: 10.1177/0146167206297401. [DOI] [PubMed] [Google Scholar]
- 19.Ruffault A, Czernichow S, Hagger MS, et al. The effects of mindfulness training on weight-loss and health-related behaviours in adults with overweight and obesity: A systematic review and meta-analysis. Obes Res Clin Pract. 2017;11(5S1):90–111. doi: 10.1016/j.orcp.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 20.Tremblay MS, Aubert S, Barnes JD, et al. Sedentary Behavior Research Network (SBRN) – Terminology Consensus Project process and outcome. Int J Behav Nutr Phys Act. 2017;14:75. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sedentary Behaviour Research Network. Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab. 2012;37(3):540–2. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 22.Benatti FB, Ried-Larsen M. The effects of breaking up prolonged sitting time: a review of experimental studies. Med Sci Sports Exerc. 2015;47(10):2053–61. doi: 10.1249/MSS.0000000000000654. [DOI] [PubMed] [Google Scholar]
- 23.Dunstan DW, Howard B, Healy GN, Owen N. Too much sitting – A health hazard. Diabetes Res Clin Pract. 2012;97(3):368–76. doi: 10.1016/j.diabres.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 24.Healy GN, Matthews CE, Dunstan DW, Winkler EAH, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J. 2011;32(5):590–7. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Teychenne M, Ball K, Salmon J. Physical activity and likelihood of depression in adults: A review. Prev Med. 2008;46(5):397–411. doi: 10.1016/j.ypmed.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 26.Teychenne M, Costigan SA, Parker K. The association between sedentary behaviour and risk of anxiety: a systematic review. BMC Public Health. 2015;15(1):513. doi: 10.1186/s12889-015-1843-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hamer M, Stamatakis E. Prospective study of sedentary behavior, risk of depression, and cognitive impairment. Med Sci Sports Exerc. 2014;46(4):718–23. doi: 10.1249/MSS.0000000000000156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vallance JK, Winkler EAH, Gardiner PA, Healy GN, Lynch BM, Owen N. Associations of objectively-assessed physical activity and sedentary time with depression: NHANES (2005–2006) Prev Med. 2011;53(4–5):284–8. doi: 10.1016/j.ypmed.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 29.Endrighi R, Steptoe A, Hamer M. The effect of experimentally induced sedentariness on mood and psychobiological responses to mental stress. Br J Psychiatry. 2015 doi: 10.1192/bjp.bp.114.150755. bjp.bp.114.150755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Henson J, Dunstan DW, Davies MJ, Yates T. Sedentary behaviour as a new behavioural target in the prevention and treatment of type 2 diabetes. Diabetes Metab Res Rev. 2016;32:213–20. doi: 10.1002/dmrr.2759. [DOI] [PubMed] [Google Scholar]
- 31.Diaz KM, Howard VJ, Hutto B, et al. Patterns of sedentary behavior in US middle-age and older adults: the REGARDS study. Med Sci Sports Exerc. 2016;48(3):430–8. doi: 10.1249/MSS.0000000000000792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maxwell L, Barrett B, Chase J, Brown R, Ewers T. Self-reported mental health predicts acute respiratory infection. WMJ Off Publ State Med Soc Wis. 2015;114(3):100–4. [PMC free article] [PubMed] [Google Scholar]
- 33.Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clin Psychol Sci Pract. 2003;10(2):144–56. [Google Scholar]
- 34.Office of Disease Prevention and Health Promotion, U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans. 2008 [date unknown]; [cited 2016 Jun 9 ] Available from: https://health.gov/paguidelines/guidelines/
- 35.Borg G. Borg’s perceived exertion and pain scales. Champaign, IL, US: Human Kinetics; 1998. p. 104. [Google Scholar]
- 36.Aadland E, Ylvisåker E. Reliability of the Actigraph GT3X+ accelerometer in adults under free-living conditions [Internet] PLoS ONE. 2015;10(8) doi: 10.1371/journal.pone.0134606. available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4537282/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lyden K, Keadle SK, Staudenmayer J, Freedson PS. A method to estimate free-living active and sedentary behavior from an accelerometer. Med Sci Sports Exerc. 2014;46(2):386–97. doi: 10.1249/MSS.0b013e3182a42a2d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Routledge Academic; 1988. p. 490. [Google Scholar]
- 39.Owen N, Sugiyama T, Eakin EE, Gardiner PA, Tremblay MS, Sallis JF. Adults’ sedentary behavior. Am J Prev Med. 2011;41(2):189–96. doi: 10.1016/j.amepre.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 40.Thraen-Borowski KM, Ellingson LD, Meyer JD, Cadmus-Bertram L. Nonworksite interventions to reduce sedentary behavior among adults: a systematic review. Transl J Am Coll Sports Med. 2017;2(12):68–78. doi: 10.1249/TJX.0000000000000036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Manini TM, Carr LJ, King AC, Marshall S, Robinson TN, Rejeski WJ. Interventions to Reduce Sedentary Behavior. Med Sci Sports Exerc. 2015;47(6):1306–10. doi: 10.1249/MSS.0000000000000519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rabin C, Pinto B, Fava J. Randomized trial of a physical activity and meditation intervention for young adult cancer survivors. J Adolesc Young Adult Oncol. 2015;5(1):41–7. doi: 10.1089/jayao.2015.0033. [DOI] [PubMed] [Google Scholar]
- 43.Grossman P, Deuring G, Walach H, Schwarzer B, Schmidt S. Mindfulness-based intervention does not influence cardiac autonomic control or pattern of physical activity in fibromyalgia during daily life: an ambulatory, multi-measure randomized controlled trial. Clin J Pain. 2017;33(5):385–94. doi: 10.1097/AJP.0000000000000420. [DOI] [PubMed] [Google Scholar]
- 44.Martin EC, Galloway-Williams N, Cox MG, Winett RA. Pilot testing of a mindfulness- and acceptance-based intervention for increasing cardiorespiratory fitness in sedentary adults: A feasibility study. J Context Behav Sci. 2015;4(4):237–45. doi: 10.1016/j.jcbs.2015.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fulwiler C, Brewer JA, Sinnott S, Loucks EB. Mindfulness-based interventions for weight loss and CVD risk management. Curr Cardiovasc Risk Rep. 2015;9(10):46. doi: 10.1007/s12170-015-0474-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cepeda Gil M, Koolhaas C, Franco O, Schoufour J. Seasonality of physical activity, sedentary behavior and nighttime sleep duration in middle aged and elderly population of the Rotterdam Study. Maturitas. 2017;103:94. doi: 10.1016/j.maturitas.2018.01.016. [DOI] [PubMed] [Google Scholar]
- 47.Moore SC, Patel AV, Matthews CE, et al. Leisure Time Physical Activity of Moderate to Vigorous Intensity and Mortality: A Large Pooled Cohort Analysis. PLOS Med. 2012;9(11):e1001335. doi: 10.1371/journal.pmed.1001335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Warburton DER, Nicol CW, Bredin SSD. Health benefits of physical activity: the evidence. CMAJ Can Med Assoc J. 2006;174(6):801–9. doi: 10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Powell C, Herring MP, Dowd KP, Donnelly AE, Carson BP. The cross-sectional associations between objectively measured sedentary time and cardiometabolic health markers in adults - a systematic review with meta-analysis component. Obes Rev Off J Int Assoc Study Obes. 2018;19(3):381–95. doi: 10.1111/obr.12642. [DOI] [PubMed] [Google Scholar]