Abstract
Although recent declines in life expectancy among non-Hispanic Whites, coined “deaths of despair,” grabbed the headlines of most major media outlets, this is neither a recent problem nor is it confined to Whites. The decline in America’s health has been described in the public health literature for decades and has long been hypothesized to be attributable to an array of worsening psychosocial problems that are not specific to Whites.
To test some of the dominant hypotheses, we show how various measures of despair have been increasing in the United States since 1980 and how these trends relate to changes in health and longevity. We show that mortality increases among Whites caused by the opioid epidemic come on the heels of the crack and HIV syndemic among Blacks. Both occurred on top of already higher mortality rates among all Americans relative to people in other nations, and both occurred among declines in measures of well-being.
We believe that the attention given to Whites is distracting researchers and policymakers from much more serious, longer-term structural problems that affect all Americans. (Am J Public Health. Published online ahead of print September 25, 2018: e1–e6. doi:10.2105/AJPH. 2018.304585)
It is an axiom in demography and public health that life expectancy increases over time.1 In nations that are free of war, famine, and disease outbreaks, the increase in life expectancy over time has been described as “so extraordinarily linear that it may be the most remarkable regularity of mass endeavor ever observed.”1(p1029) However, in the 1990s, public health researchers began sounding an alarm about some disturbing changes observed in the United States. In particular, researchers observed 3 aberrant trends1: the self-rated health of Americans had leveled off and started to take a downward turn2–4; life expectancy growth in the United States was slowing relative to other nations, even for socioeconomically advantaged White subpopulations; and3 absolute survival rates were declining for socioeconomically disadvantaged White women.4–10
By the turn of the millennium, the United States had become a curious outlier among its peers. Health system costs per capita rose to twice that of the next highest country, but overall survival was barely budging and was falling year-on-year for segments of the White population and for Native Americans overall.5,9 As a result, the long-term relative decline in life expectancy culminated in a multiyear absolute decline in life expectancy in the United States in 2015 and 2016.11–14 One of the drivers of this absolute decline in life expectancy is an ongoing opioid-related mortality epidemic, which contributed to more than 60 000 lives lost in 2016.15 However, absolute declines in life expectancy were observed for some groups and localities starting at least as early as 1980—decades before the opioid epidemic began.12
In 2015, Princeton researchers Case and Deaton documented a recent spike in mortality rates among less-educated non-Hispanic Whites. Although mortality increases among those with declining socioeconomic mobility, particularly in Southern “stroke belt” counties and among White women, had been previously noted,14 Case and Deaton provided a narrative with media resonance. They termed this excess mortality “deaths of despair,” on the basis of their finding that mortality increases were largely driven by suicide, cirrhosis of the liver, and fatal opioid-related overdoses— causes that suggest victims are likely to be suffering from psychological distress16,17. Linking these trends to deaths that can be traced back to psychological despair allowed a clear story to be distilled from a mass of data. The identification of increasing mortality rates among middle-aged non-Hispanic Whites (generally referred to as “Whites” here for ease) was particularly shocking for the lay press. The hypothesis received headline coverage on the major networks and newspapers, with Bloomberg News labeling the term “deaths of despair” a “part of the American lexicon.”16
We believe that Case and Deaton observed an epidemic of opioid-related deaths super-imposed on longer-term trends toward worsening health and declining longevity in the United States. We argue that these deaths represent an uptick in a much broader trend and that declines in survival and life expectancy would not have been possible without the long-term malaise seen in the United States. This is important to highlight because the broader story of America’s decline has been told by many different research teams in many different ways but has not been given much of a powerful voice. Case and Deaton found that voice, but they may have overlooked the longer-term trends and the overall malaise described by sociologists, demographers, health services researchers, epidemiologists, and economists over the past 3 decades.
THE TRUE DEATHS OF DESPAIR
We argue that “despair,” which we define broadly as a decline in measures of psychosocial well-being over time, is a core public health problem in the United States. However, we believe that despair plays only 1 role in the opioid epidemic. Moreover, we posit that increases in despair over time have produced a broad effect among all groups in the United States, not just less-educated Whites. In fact, declines in the relative life expectancy of Americans relative to other nations has occurred across most groups since at least 1980.5
The Effects of Epidemics Are Time Limited
When looking at longer-term trends, a fuller picture of American health emerges. Since publication of the original Case and Deaton report, efforts have been made to specify how the patterns observed vary across race, age, and gender.18,19 When one looks at the big picture—with data spanning decades—we see that suicide rates are barely higher than they were in 1980 (Figure 1). We also see that deaths from alcoholic cirrhosis have increased only mildly since then. However, we do see that there is a shorter-term opioid epidemic that is predominantly affecting Whites.19
FIGURE 1—
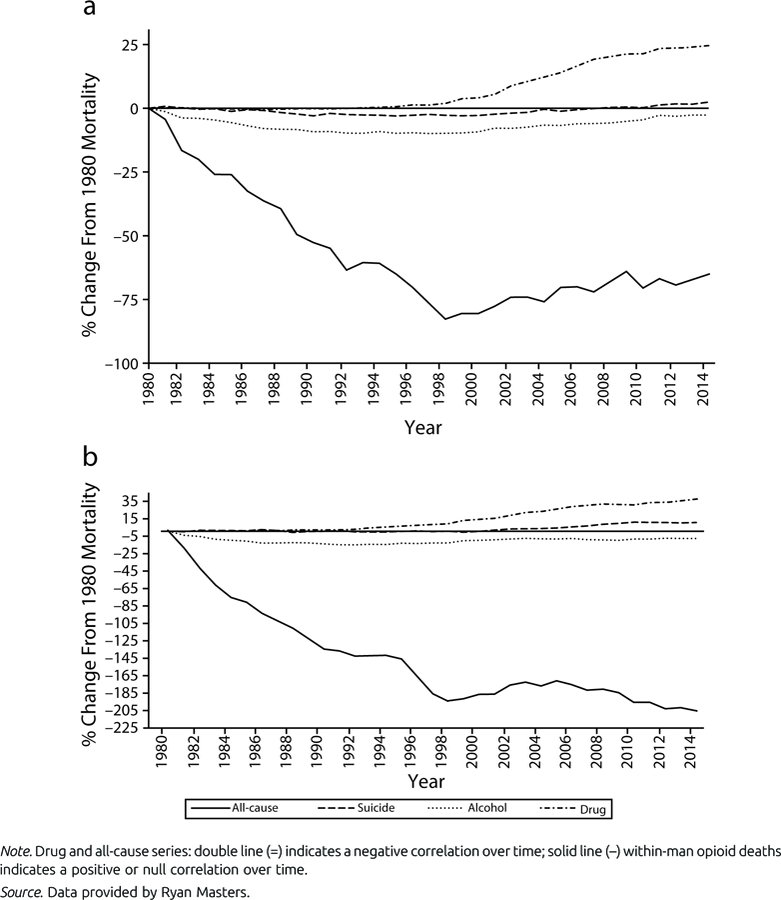
All-Cause and Cause-Specific Percentage Changes in Mortality Rates Attributable to Drugs, Suicides, or Alcohol Among White 45- to 54-Year-Old (a) Women and (b) Men: United States, 1980–2013
This opioid epidemic, although extremely severe and alarming, has been relatively recent and has predominantly affected men.16,20 The absolute increases in mortality among Whites that grabbed the attention of public health officials are seen only among women (Figure 1). Rather than driving the decline in life expectancy among White women, opioid-associated deaths have merely accelerated the manifestation of a trend that was already well under way.5 This trend toward an increase in mortality among White women began at least as early as 1980.
In Figure 2, we see that Black–White disparities in mortality were generally parallel or converging through the early 1980s. This convergence was interrupted in the mid-1980s through the mid-1990s by the HIV/AIDS and crack epidemics, which predominantly affected Blacks.21,22 In this figure, we see that health disparities by race increased greatly during the epidemics. However, once the epidemics ended, reductions in mortality rates for Blacks relative to Whites resumed. Although the proximate cause of such epidemics is relatively straightforward, factors such as despair are plausible contributors.
FIGURE 2—
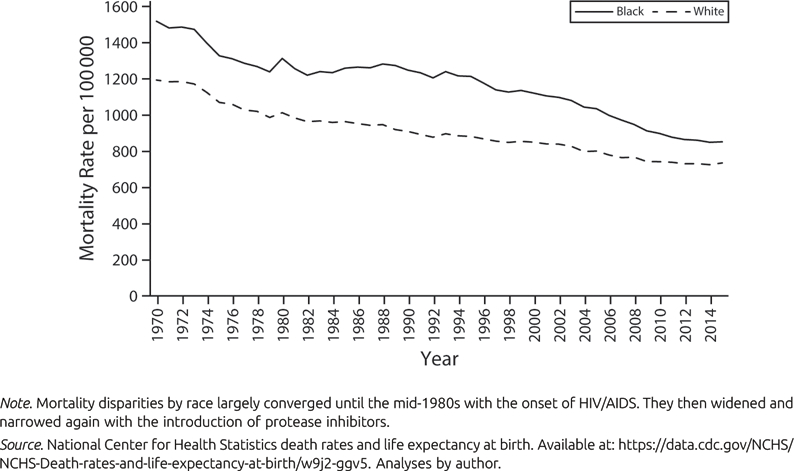
Black and White Mortality Rates per 100 000 Standard Population: United States, 1970–2015
Despair Has Been Rising for a Long Time
Sociologists have observed the decline in various measures of psychosocial well-being in the United States for some time. Alarming declines in measures such as trust have been documented for decades.23 But is the United States different from other nations? Australia serves as an apt comparator nation because it has seen some of the most rapid declines in mortality rates in the world over the past 40 years and because it has a colonial history and a population composition similar to those of the United States.5 Some semblance of historical and demographic similarity is important because survey responses are patterned by these factors as well as by cultural orientations. Australians consume goods and services from the United States, including its media.
Using the General Social Survey, we plotted trends in self-reported happiness and self-reported trust in others from a survey that is administered in both the United States and Australia (Figure 3). Self-reported happiness serves as a generic but powerful measure of psychological well-being. Self-reported trust is a widely used measure of social capital. In both instances, the United States is declining relative to Australia. In Figure 3, we have also included a number of other measures that were available only for the United States. (Comparable measures were not available for Australia.) Over time, Americans are less likely to see others as fair, to believe their standard of living was as good as their parents, and to have recreational sex.
FIGURE 3—
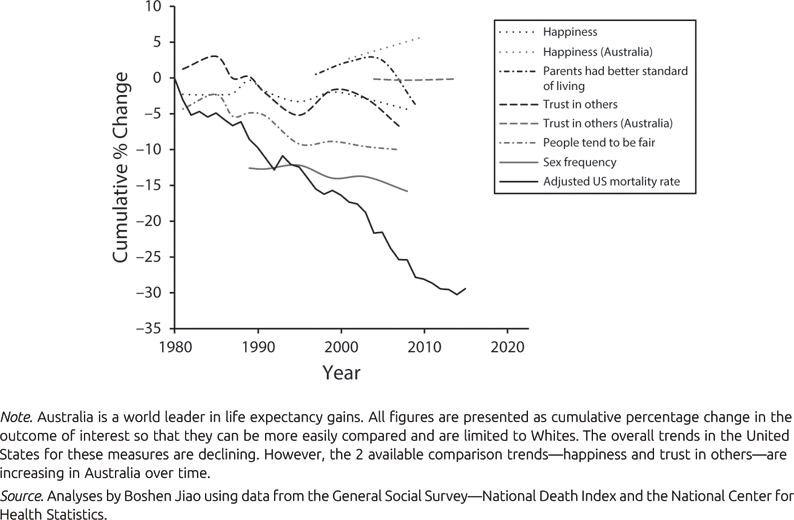
Long-Term Trends in Selected Measures of Well-Being in the United States and Australia: 1983–2012.
When one steps outside the sociological literature and examines the health literature, a similar picture of despair emerges. In the Behavioral Risk Factor Surveillance Survey, respondents are asked, “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” A similar question is asked about physical health. On both measures of physical and mental health, declines are evident in the United States.3 Although these questions are not meant to measure rates of clinical disease, such as depression, they have been extensively validated (including among low-income subgroups)24 for general reliability and validity. Unfortunately, data on objective measures of depression prevalence in the US population or elsewhere are thin.25 Over the relatively near term, clinical depression is worsening in the United States, albeit mostly among younger people.
It is difficult to make statements about despair trends with any certainty because of the lack of a validated despair measure or systematic meta-analyses of analogous concepts. Nevertheless, both our exploratory analyses and the broader literature portend worsening mistrust, loneliness, mental health, and health across all ages, races, ethnicities, and quartiles of socioeconomic status where measured.26,27 The literature previously cited and in Case and Deaton’s report does suggest that there is period- and cohort-based deterioration in many measures of well-being over time in the United States. Likewise, the public health literature we cited suggests a deterioration in health and longevity over the same period.
We provide an overview of disturbing trends toward both increasing despair and declining health observed among a broad array of groups in the United States. We also note that there have been other deadly drug epidemics among different groups over time, most notably among Blacks in the mid-1980s. Emotional pain can logically lead one to use and become addicted to drugs. But can we say that these epidemics were driven by despair?
Opioid Death Causes Are Fairly Well Understood
Numerous accounts have chronicled the machinations of a pharmaceutical industry capitalizing on a well-intended surgeon general who regarded pain as undertreated in the United States.15,16 Prescriptions for opioids have increased 4-fold since 1995. Deaths have increased steadily since, mainly among Whites in lower-income communities.15,28
It is hardly a mystery that less-educated Whites are disproportionately affected by the opioid crisis.20 The opioid crisis is believed to have some roots in prescription opiates. Whites have better access to health care—and, thus, prescription pain medications—than do Hispanics or Blacks. Even among those who do access care, Whites are much more likely to be treated for pain with opioids than are Blacks or Hispanics.29 Older, blue-collar Whites have high levels of disability relative to their better-off peers, so their need for pain relief is higher.15,30 Another factor implicated in increasing opioid overdose deaths is that powerful synthetic opioids (e.g., fentanyl) are cheap to smuggle into the United States in smaller quantities than are traditional heroin and, even when consumed in small quantities, increase the likelihood of drug overdoses compared with heroin, leading to higher mortality rates.
Finally, deaths attributable to opioid use shifted from baby boomers to millennial men, a group that is healthier and, by definition, younger than are most Americans.11 Together, this suggests that White mortality and the deaths of despair are actually a spike in opioid-related deaths that are occurring in addition to long-term trends in declining health and well-being in the United States.
ALTERNATIVE STORIES
If longer-term trends toward social malaise, declining health, and increases in mortality preceded the opioid epidemic, we must explore other explanations for America’s relative fall in health and global life expectancy rankings. The relative decline is likely to have many proximal and distal causes and cannot be explained by a single hypothesis. Moreover, the possibilities are nearly infinite and each upstream risk could lead to a cascade of downstream risks. These could include the increases in industrial chemicals in the environment, screen time, reliance on private automobiles, and mechanization of human tasks and worsening of the quality of the food supply chain. Virtually any social trend that might correlate over time with changes in health curves is a candidate. For the purposes of illustration, we describe some of the more popular or plausible explanations on the basis of our reading of the published research and feedback from scholars active in this area.
-
(1)
Failure of democratic institutions and regulations might be making life more hazardous, particularly for Whites in red states.31,32 Welfare programs are stronger in blue states. Blue states also tend to have stronger governance, stricter gun laws, safer roads, and more stringent environmental protections. Certainly, some of the regulatory standards from blue states spill over to red states (e.g., automobile standards and trans fat bans) because it is more expensive for companies to make different products for different markets. But many, such as Medicaid expansion, do not.33
Such variation in public investment also exists across countries. The United States is falling behind other nations with respect to educational performance, income equality, environmental protection, transportation, waste management, the rule of law, and private gun ownership regulations.34 Many of the institutions that have long protected low-income Whites from abject poverty are now disappearing, particularly in those states and counties with the highest increases in mortality rates. There is some experimental evidence that welfare policies influence long-term health, but there is considerably more work that needs to be done to ascertain which policies work and for whom.35–38
-
(2)
Economic stagnation since the 1980s for moderate-income households of all races/ethnicities could have adverse health implications apart from despair. As characterized by the John Henryism and weathering hypotheses and related empirical literature, the roles of chronic stressors and the tenacious coping needed to survive or overcome them have cumulative adverse health effects.39,40 These are reflected in the early onset of life-threatening chronic diseases and in generally increased health vulnerability as body systems become dysregulated or exhausted by prolonged stress-mediated wear and tear.41
-
(3)
Changing demographics may be inflating longevity losses in the United States by race, by county, or for the country as a whole. Some of the declining health and longevity in the United States has long been masked by immigration. Foreign-born Americans are generally much healthier than are native-born Americans of similar socioeconomic position.42 It is possible that when immigration to the United States leveled off, immigrants stopped contributing to life expectancy gains and that this drove recent declines in overall life expectancy in the United States.14 The migration story is supported by a relatively strong correlation between mortality and in-migration trends and the fact that areas without major urban centers that attract healthy international migrants have experienced a leveling off in life expectancy over the past decade.43
Internal migration may also play a role. This problem is best illustrated by a comparison between survival patterns in widely divergent labor markets. The “stroke belt,” where employment opportunity has been contracting for some time, suffers from absolute increases in mortality, whereas urban innovation centers such as San Francisco, California; Portland, Oregon; and New York City show drops in mortality.12 If healthy people leave poorer counties to seek job opportunities in larger, coastal, urban areas, this would create a statistical reduction in health quality and an increase in mortality in poorer geographic areas attributable purely to compositional, rather than intraindividual, change.
-
(4)
Rising medical costs may be compromising Americans ability to satisfy basic needs. If there is anything to which one can point that makes the United States an outlier in global rankings of health measures, it is medical costs. In the early 1970s, medical costs in the United States were in line with those in other nations. They have since substantially outpaced increases in other nations and are now more than twice as high as the next biggest spender, Switzerland.5 Out-of-pocket payments for insured people are rising sharply over time.44 These costs are eating into middle-class American’s disposable income. Whites are likely to be uniquely affected because they have historically been more likely to receive employer-based health insurance, which has seen rising copayments and deductibles. Those receiving Medicaid, on the other hand, have been somewhat shielded from these market-driven increases. Medicaid has, over time, become a benefit for low-income Americans in more diverse blue states.
-
(5)
Earlier smoking among White women could be producing lagged mortality effects that are surfacing in middle and older ages. Wang and Preston find that the prevalence of smoking in the United States was much higher than in other nations, particularly among White women, and that the full effects of smoking on population health do not materialize for decades. Research has shown that smoking rates among White women did not peak until the 1960s and that they subsequently declined very slowly among low socioeconomic status White women relative to both high socioeconomic status women and men.45 Additionally, smoking rates declined much faster in blue states with higher cigarette taxation. Because of the coincidence of smoking and drug use, it is quite possible that the contemporary effects of cigarette smoking overlap with the effects of the opioid epidemic.
These and other hypotheses warrant consideration alongside wage-driven White despair. In all likelihood, the answer rests in some combination of factors that include, but are not limited to, stagnating wages.9 Any such analyses should factor in the weakening of democratic institutions and regulations, increased stress exposure and the high-effort coping it entails, rising medical costs, migration of healthy people, and gendered smoking patterns.
CONCLUSIONS
We undertook a critical cross-examination of the deaths of despair hypothesis. The United States has experienced what amounts to a social crisis that dates back to at least the 1980s. This crisis is reflected not only in various measures of worsening despair but also in declining relative life expectancy. It is a problem that has recently received a good deal of attention because Whites were identified as the primary victims. But it is a problem that is more extensive and more enduring than the White despair narrative can fully explain. As 1 example, the earlier crack and HIV/AIDS epidemic, neglected in the recent narratives about despair in the United States, also produced a decline in life expectancy in the United States. It is logical that groups with higher levels of disadvantage would be struck by declines in health first.41
However, the relative increase in various measures of despair recorded in the sociological literature and the relative decline in health and well-being in the public health literature also preceded this epidemic among Blacks. The epidemic of opioid-related deaths has brought renewed attention to this downturn. But middle-aged non-Hispanic Whites are not the core protagonists in the story, nor are opioids. Rather, it seems that the opioid epidemic is sitting on top of a much longer, and more poorly understood, decline in well-being in the United States.
ACKNOWLEDGMENTS
This work was supported in part by a re-search grant from the US National Institute on Drug Abuse, National Institutes of Health (grant T32DA031099).
We would like to thank Boshen Jiao, Ryan Masters, Sam Preston, Steve Woolf, Katherine Keyes, Sherry Glied, Dana Glei, Andrew Gelman, Jonathan Aeurbach, and Jennifer Karas-Montez for their insightful comments, data, and analyses.
Contributor Information
Peter A. Muennig, Department of Health Policy and Management, Mailman School of Public Health, Columbia University, New York, NY..
Megan Reynolds, Department of Sociology, University of Utah, Salt Lake City..
David S. Fink, Department of Epidemiology, Mailman School of Public Health..
Zafar Zafari, Global Research Analytics for Population Health Center, Mailman School of Public Health..
Arline T. Geronimus, Health Behavior and Health Education, School of Public Health and the Population Studies Center, Institute for Social Research, University of Michigan, Ann Arbor..
REFERENCES
- 1.Oeppen J, Vaupel JW. Broken limits to life expectancy. Science 2002;296(5570): 1029–1031. [DOI] [PubMed] [Google Scholar]
- 2.Salomon JA, Nordhagen S, Oza S, Murray CJ. Are Americans feeling less healthy? The puzzle of trends in self-rated health. Am J Epidemiol 2009;170(3):351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zack MM, Moriarty DG, Stroup DF, Ford ES, Mokdad AH. Worsening trends in adult health-related quality of life and self-rated health—United States, 1993–2001. Public Health Rep 2004;119(5):493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crimmins EM, Saito Y. Trends in healthy life expectancy in the United States, 1970–1990: gender, racial, and educational differences. Soc Sci Med 2001; 52(11):1629–1641. [DOI] [PubMed] [Google Scholar]
- 5.Muennig PA, Glied SA. What changes in survival rates tell us about US health care. Health Aff (Millwood) 2010;29(11): 2105–2113. [DOI] [PubMed] [Google Scholar]
- 6.Meara ER, Richards S, Cutler DM. The gap gets bigger: changes in mortality and life expectancy, by education, 1981– 2000. Health Aff (Millwood) 2008;27(2): –360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bound J, Geronimus AT, Rodriguez JM, Waidmann TA. Measuring recent apparent declines in longevity: the role of increasing educational attainment. Health Aff (Millwood) 2015;34(12):2167–2173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh GK, Siahpush M. All-cause and cause-specific mortality of immigrants and native born in the United States. Am J Public Health 2001;91(3):392–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Woolf SH, Aron L. US Health in International Perspective: Shorter Lives, Poorer Health Washington, DC: National Academies Press; 2013. [PubMed] [Google Scholar]
- 10.Montez JK, Zajacova A. Why is life expectancy declining among low-educated women in the United States? Am Public Health 2014;104(10):e5–e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Mortality in the United States, 2016. Available at: https://www.cdc.gov/nchs/products/databriefs/db293.htm. Accessed December 22, 2017.
- 12.Murray CJ, Kulkarni SC, Michaud C, et al. Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Med 2006;3(9):e260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Espey DK, Jim MA, Cobb N, et al. Leading causes of death and all-cause mortality in American Indians and Alaska Natives. Am J Public Health 2014;104-(suppl 3):S303–S311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, et al. Inequalities in life expectancy among US counties, 1980 to 2014: temporal trends and key drivers. JAMA Intern Med 2017;177(7):1003– 1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dowell D, Noonan RK, Houry D. Underlying factors in drug overdose deaths JAMA 2017;318(23):2295–2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fox J Which came first, the opioids or the despair? 2017. Available at: www.bloomberg.com/view/articles/2017-09-11/which-came-first-the-opioids-or-the-despair. Accessed October 8, 2017.
- 17.Case A, Deaton A. Mortality and morbidity in the 21st century Available at: https://www.brookings.edu/wp-content/uploads/2017/08/casetextsp17bpea.pdf. Accessed January 5, 2018. [DOI] [PMC free article] [PubMed]
- 18.Gelman A, Auerbach J. Age-aggregation bias in mortality trends. Proc Natl Acad Sci U S A 2016;113(7):E816–E817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Masters RK, Tilstra AM, Simon DH. Explaining recent mortality trends among younger and middle-aged White Ameri-cans. Int J Epidemiol 2018;47(1):81–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription opioid use, misuse, and use disorders in US adults: 2015 National Survey on Drug Use and Health. Ann Intern Med 2017;167(5): 293–301. [DOI] [PubMed] [Google Scholar]
- 21.Edlin BR, Irwin KL, Faruque S, et al. Intersecting epidemics—crack cocaine use and HIV infection among inner-city young adults. N Engl J Med 1994;331(21): 1422–1427. [DOI] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Deaths: final data for 2014. Nat Vital Stat Rep 2016;65(4):1–122. [PubMed] [Google Scholar]
- 23.Putnam RD. Tuning in, tuning out: the strange disappearance of social capital in America. PS Political Sci Politics 1995; 28(4):664–683. [Google Scholar]
- 24.Moriarty DG, Zack MM, Kobau R. The Centers for Disease Control and Prevention’s Healthy Days Measures— population tracking of perceived physical and mental health over time. Health Qual Life Outcomes 2003;1:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weinberger A, Gbedemah M, Martinez A, Nash D, Galea S, Goodwin R. Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychol Med 2018;48(8):1308–1315. [DOI] [PubMed] [Google Scholar]
- 26.Baker D All the Lonely People: Loneliness in Australia, 2001–2009 Manuka, Australia: Australia Institute; 2012. [Google Scholar]
- 27.Putnam RD. Bowling Alone New York, NY: Simon & Schuster; 2001. [Google Scholar]
- 28.Monnat SM, Brown DL. More than a rural revolt: landscapes of despair and the 2016 presidential election. J Rural Stud 2017;55:227–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. JAMA 1993;269(12):1537–1539. [PubMed] [Google Scholar]
- 30.Caban-Martinez AJ, Lee DJ, Fleming LE, et al. Arthritis, occupational class, and the aging US workforce. Am J Public Health 2011;101(9):1729–1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bor J Diverging life expectancies and voting patterns in the 2016 US presidential election. Am J Public Health 2017;107(10): 1560–1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bilal U, Knapp EA, Cooper RS. Swing voting in the 2016 presidential election in counties where midlife mortality has been rising in White non-Hispanic Americans. Soc Sci Med 2018; 197:33–38. [DOI] [PubMed] [Google Scholar]
- 33.Bhatt CB, Beck-Sagué CM. Medicaid expansion and infant mortality in the United States. Am J Public Health 2018; 108(4):e1–e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Organization for Economic Co-operation and Development. Level of GDP per capita and productivity Avail-able at: http://stats.oecd.org. Accessed October 16, 2017.
- 35.Kawachi I, Adler NE, Dow WH. Money, schooling, and health: mechanisms and causal evidence. Ann Y Acad Sci 2010;1186(1):56–68. [DOI] [PubMed] [Google Scholar]
- 36.Muennig PA, Mohit B, Wu J, Jia H, Rosen Z. Cost effectiveness of the earned income tax credit as a health policy in-vestment. Am J Prev Med 2016;51(6): –881. [DOI] [PubMed] [Google Scholar]
- 37.Ludwig J, Duncan GJ, Gennetian LA, et al. Neighborhood effects on the long-term well-being of low-income adults. Science 2012;337(6101):1505–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Muennig P Can universal pre-kindergarten programs improve population health and longevity? Mechanisms, evidence, and policy implications. Soc Sci Med 2015;127:116–123. [DOI] [PubMed] [Google Scholar]
- 39.Booth JM, Jonassaint CR. The role of disadvantaged neighborhood environments in the association of John Henryism with hypertension and obesity. Psychosom Med 2016;78(5):552–561. [DOI] [PubMed] [Google Scholar]
- 40.Geronimus AT, Pearson JA, Linnen-bringer E, et al. Race–ethnicity, poverty, urban stressors, and telomere length in a Detroit community-based sample. J Health Soc Behav 2015;56(2):199–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Geronimus AT. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethn Dis 1992;2(3): –221. [PubMed] [Google Scholar]
- 42.Singh GK, Miller BA. Health, life expectancy, and mortality patterns among immigrant populations in the United States. Can J Public Health 2004;95(3): I14–I21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gibson CJ, Lennon E. Historical Census Statistics on the Foreign-Born Population of the United States: 1850–1990 Washington, DC: US Bureau of the Census; 1999. [Google Scholar]
- 44.Polsky D, Grande D. The burden of health care costs for working families— implications for reform. N Engl J Med 2009;361(5):437–439. [DOI] [PubMed] [Google Scholar]
- 45.Wang H, Preston S. Forecasting United States mortality using cohort smoking histories. Proc Natl Acad Sci U S A 2009;106(2):393–398. [DOI] [PMC free article] [PubMed] [Google Scholar]


