Abstract
Objectives:
To explore trajectories of physical and psychosocial health, and their interrelationship, among women completing fistula repair in Uganda for one-year post-surgery.
Methods:
We recruited a 60-woman longitudinal cohort at surgical hospitalization from Mulago Hospital in Kampala Uganda (Dec 2014-June 2015) and followed them for one year. We collected survey data on physical and psychosocial health at surgery and at 3, 6, 9, and 12 months via mobile phone. Fistula characteristics were abstracted from medical records. All participants provided written informed consent. We present univariate analysis and linear regression results.
Results:
Across post-surgical follow-up, most women reported improvements in physical and psychosocial health, largely within the first six months. By 12 months, urinary incontinence had declined from 98% to 33%, and general weakness from 33% to 17%, while excellent to good general health rose from 0% to 60%. Reintegration, self-esteem, and quality of life all increased through six months and remained stable thereafter. Reported stigma reduced, yet some negative self-perception remained at twelve months (mean 17.8). Psychosocial health was significantly impacted by report of physical symptoms; at 12 months, physical symptoms were associated with a 21.9 lower mean reintegration score (95% CI −30.1, −12.4)
Conclusions:
Our longitudinal cohort experienced dramatic improvements in physical and psychosocial health after surgery. Continuing fistula-related symptoms and the substantial differences in psychosocial health by physical symptoms supports additional intervention to support women’s recovery or more targeted psychosocial support and reintegration services to ensure that those coping with physical or psychosocial challenges are appropriately supported.
Keywords: Vesicovaginal Fistula, Rectovaginal Fistula, Obstetric Labor Complications, Urinary Incontinence, Social Stigma, Quality of Life
Introduction
Prolonged obstructed labour combined with delays in accessing comprehensive emergency obstetric care results in multifaceted physical trauma, often involving multiple organ systems, termed obstructed labour injury complex(1). Although all the conditions associated with obstructed labour injury complex represent significant maternal morbidity, obstetric fistula has been the primary focus of public health programing due to its severe physical, psychological, and social sequelae(2–6). Women with fistula experience constant leakage of urine and/or faeces, are subjected to stigma that frequently results in familial and community isolation(7, 8), and report high rates of depression (6, 9–12). Accurately estimating the burden of obstetric fistula is a challenge; estimates suggest that as many as 2 million women globally may be affected, with thousands of annual incident cases(13–15).
Fistula closure rates at hospital discharge range from 65% to 90%(16–18). Due to the array of physical and psychosocial correlates of fistula, longitudinal studies that follow women beyond the period of short-term clinical outcomes are of significant interest(3, 19, 20). Studies assessing patient-focused outcomes of surgery have identified significant short-term improvements including enhanced overall quality of life(21), psychological status(22), social functioning(23, 24), and economic status(25). However, they also report significant long-term challenges, including persistent residual incontinence(20, 26, 27), pain and weakness(21, 28), and sexual and fertility complications(5, 21, 29–31). Lingering physical problems such as these reduce women’s ability to resume social roles, making them less likely to consider themselves to have recovered,(3, 21, 25, 32) and placing them at greater risk of continued poor mental health(28, 33, 34).
Most longitudinal studies of fistula recovery are limited to a single, short-term, post-surgical follow-up, precluding our ability to understand the process of longer-term physical and psychosocial recovery. Given the significant physical and psychosocial morbidities experienced by women with fistula, and the lengthy period of time that many women live with fistula prior to accessing treatment, physical and psychosocial recovery is likely a lengthier and more complex process than can be captured at one time point. This study explores women’s trajectories of physical recovery and their relationship to psychosocial health following surgical repair of obstetric fistula in Uganda, assessed at four time points over 12 months post-surgery.
Methods
We recruited a longitudinal cohort of women accessing fistula surgery at Mulago National Referral and Teaching Hospital in Kampala, Uganda from December 2014 to June 2015(35). Fistula repair within the urogynaecology division is an ongoing surgical service supplemented by several annual fistula repair camps.
Women with obstetric or childbirth-related iatrogenic fistula were eligible for participation upon completion of initial examination and clearance for surgery if they spoke Luganda or English, resided in a community with cellular telephone coverage, and were capable of providing informed consent. Patients scheduled for surgery were approached and screened for eligibility by research staff, who obtained written informed consent or thumbprint confirmation. Where eligible participants were unable to be approached prior to surgery, they were asked to participate post-operatively, following sufficient recovery.
Non-enrolled eligible women included one woman whose fistula resolved through urinary catheterization and another who refused surgery. Data were captured from the participants prior to surgery (baseline), and 3-, 6-, 9-, and 12-months post-surgery, and abstracted from medical records. Our baseline questionnaire was administered in person by local research staff in the participant’s preferred language and included questions on socio-demographic characteristics, obstetric history, and physical and psychosocial health measures (Supplemental Table 1). Etiology of fistula was inconsistently captured in medical records; we classified fistula etiology into obstetric versus likely childbirth-related iatrogenic using criteria proposed by Raasen et al. (36). Subsequent surveys included questions on changeable socio-demographic characteristics, and physical and psychosocial health measures. All four post-discharge follow-up surveys were administered over mobile telephone; telephones and airtime were provided to participants. Physical health assessment measures included the Stanford Self-Rated Health measure for general health(37), the International Consultation on Incontinence Questionnaire Short Form (ICIQ-SF)(38), self-reported experience of other fistula-related symptoms (i.e., faecal incontinence, general body weakness, general pain, pain with urination, vaginal pain, skin irritation, vaginal discharge, and difficulty walking), and menstrual irregularity. Psychosocial health assessment included a post-surgical reintegration success instrument, operationalized as global functioning status specific to women affected by fistula(39), the Hopkins Symptom Checklist (HSC) for depression(40, 41), the WHO Quality of Life (QOL) BREF for quality of life(42, 43), the Rosenberg self-esteem scale(44), a fistula-related stigma assessment modified from a scale used to measure HIV-related stigma(45), the Primary Care Post Traumatic Stress Disorder (PTSD) Screen for trauma (46), and the multidimensional scale of perceived social support (47, 48). We considered a mean HSC score of >1.75 as positive for depressive symptomatology(49, 50). The QOL BREF and PTSD screen were not administered at 3 or 9 months to reduce participant response burden. We defined depressive symptomatology using mean HSC score of 1.75 or above, based on commonly-used criteria(51, 52). Each interview lasted between 30-60 minutes. Medical record abstraction captured fistula characteristics and surgical outcomes.
Socio-demographic and obstetric characteristics were described using univariate analyses: means and standard deviations (SD) or medians and interquartile ranges (IQR) for continuous variables and proportions across categorical variables. Physical and psychosocial health measures were standardized to range 0-100 for comparability, and are presented similarly. Analyses of psychosocial health separately evaluated domains comprising the WHO QOL-BREF (domains: overall, physical, environment, social relationships, and psychological) and the fistula-related stigma assessment (domains: negative self-perception, social isolation, verbal abuse, and fear of contagion). We estimated separate linear regression models to understand the relationship between any persistent physical symptoms over time (urinary incontinence, faecal incontinence, general body weakness, pain, pain with urination, vaginal pain, skin irritation, vaginal discharge, and difficulty walking) and our psychosocial health measures of reintegration, self-esteem, depression, quality of life, and stigma. All analyses were performed with Stata v14 software (StataCorp, College Station, TX). Differences were considered statistically significant at p<0.05.
The study protocol was approved by the Makerere University College of Health Sciences, School of Medicine Research and Ethics Committee, the Uganda National Council for Science and Technology, and the University of California, San Francisco Human Research Protection Program, Committee on Human Research.
Results
Sociodemographic and Obstetric Characteristics of Study Participants
Research staff screened a total of 79 individuals; 62 were eligible, and 60 were enrolled. Retention was 97% at 12 months post-surgery. Median age at study entry was 28 years (IQR 21-36) (Table 1). Educational attainment varied, but most women had not completed primary school (67%), nor did they work outside the home (58%). Primary sources of financial support were self (30%), husbands (35%) or other individuals (35%), primarily relatives. Household assets varied, with most participants reporting having a radio (58%) and a mobile phone (65%) in the household. Two-thirds of study participants had living children (65%).
Table 1.
Socio-demographic and obstetric characteristics of study participants at baseline (n=60).
| Characteristic | n | % |
|---|---|---|
| Current Age in years (median, IQR) | 28 (21-36) | |
| Living Situation | ||
| Aloneb | 13 | 31.6 |
| Husbandb | 24 | 40.0 |
| Parentsb | 8 | 13.3 |
| Otherb | 15 | 25.1 |
| Any Living Children | 39 | 65 |
| Educational Attainment | ||
| None | 10 | 16.7 |
| Some Primary | 24 | 40.0 |
| Completed Primary | 17 | 28.3 |
| Any Secondary | 9 | 15 |
| Occupation | ||
| None | 35 | 58.3 |
| Vendor/Shopkeeper | 5 | 8.3 |
| Farmer | 15 | 25.0 |
| Other | 5 | 8.3 |
| Primary Source of Financial Support | ||
| Self | 18 | 30 |
| Husband | 21 | 35 |
| Other | 21 | 35 |
| Household Assets | ||
| Piped Water | 9 | 15.0 |
| Flush/pour flush toilet | 4 | 6.7 |
| Electricity | 26 | 43.3 |
| Radio | 35 | 58.3 |
| Television | 17 | 28.3 |
| Mobile phone | 39 | 65 |
| Refrigerator | 26 | 43.3 |
| Age at First Birtha | 18 (16.5-20) | |
| Pregnancies Before Fistulaa | 1 (0-3) | |
| Live Births Before Fistulaa | 1 (0-3) | |
| Any Births Since Fistulaa | 7 | 11.7 |
| Age at Fistulaa | 22.5 (18-31) | |
| Duration Living with Fistula | ||
| < 1 Mo | 8 | 13.3 |
| 1-3 Mo | 19 | 31.7 |
| 3-12 Mo | 9 | 13.3 |
| 1-2 Years | 3 | 5 |
| 3-5 Years | 5 | 8.3 |
| >5 Years | 17 | 28.3 |
| Any ANC for Pregnancy Resulting in Fistula | 56 | 93.3 |
| Health Facility Delivery for Pregnancy Resulting in Fistula | 58 | 96.7 |
| Infant Survived Delivery for Pregnancy Resulting in Fistula | 17 | 28.3 |
| Likely Etiology of Fistula | ||
| Obstetric | 53 | 88.3 |
| Childbirth-related iatrogenic | 7 | 11.7 |
Notes.
maximum 2 participants per each ‘other’ district;
with or without young children; iqr =interquartile range.
Median age at first birth was 18 years (IQR 17-20). Most women had vesicovaginal fistula only (95%), two women had both vesicovaginal and rectovaginal fistula (3%), and one woman had rectovaginal fistula only (2%). Forty percent of our participants had developed fistula at their first delivery (40%), with 52% reporting a prior live birth. Seven women (12%) had delivered since fistula development. Time between fistula development and surgery ranged from two weeks to thirty-one years: 13% accessed surgery within one month, and 32% between one to three months; however, 28% lived with fistula for more than five years. Most women delivered at a health facility (97%), and only 28% of infants survived. Nearly one-third of fistula were classified as likely childbirth-related iatrogenic (31.7%).
Physical Health across Study Follow-Up
Most women reported fistula-related symptoms at baseline (Figure 1; Table 2). Self-report of general health status was poor (82%) or fair (18%). Most women reported urinary incontinence (98%), with 75% reporting it all of the time, and 20% reporting it several times per day. Three women reported faecal incontinence (5%). Nearly half of women reported vaginal pain (45%) and 37% reported general pain. Approximately one-third reported weakness (33%), difficulty walking (33%), vaginal discharge (32%), or skin irritation (28%). At hospital discharge leaking was resolved among 37 of 59 women with VVF (63%) and two of three women with RVF. Of the 22 leaking urine at hospital discharge, 9 had repair breakdown only, 10 had post-repair urethral incontinence only, and one had both repair breakdown and post-repair urethral incontinence. The origin of leakage for two participants was not available in their medical record.
Figure 1.
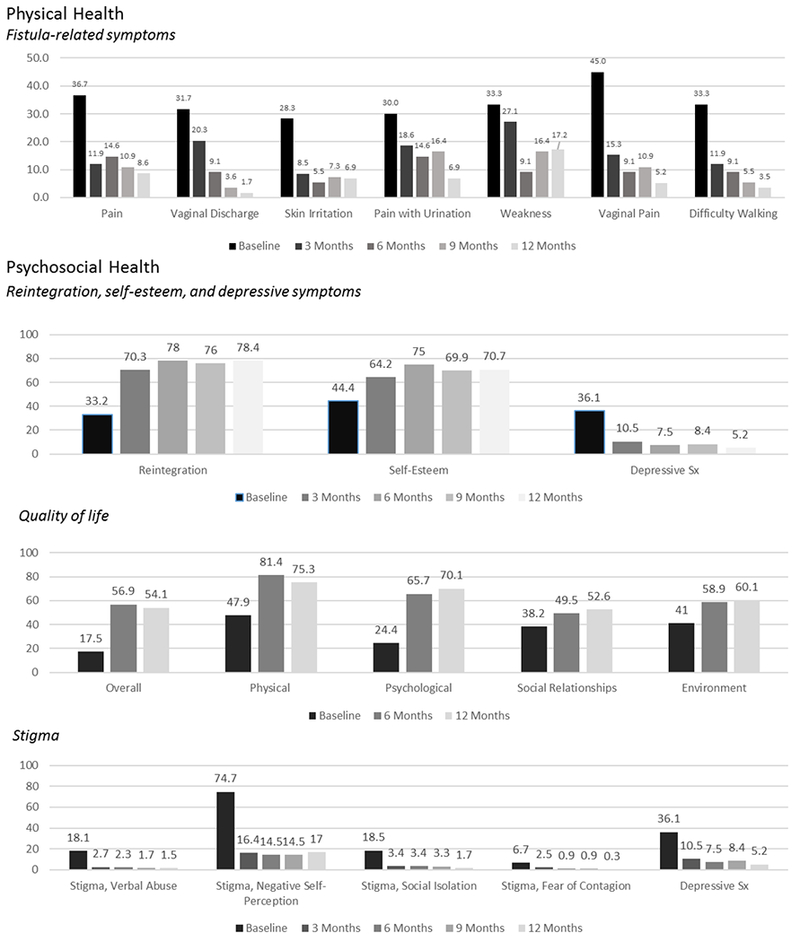
Trajectories of fistula-related physical symptoms and psychosocial health indicators across twelve-month study follow-up
Table 2.
Physical and psychological health across twelve-month study follow-up.
| Baseline | 3 Months | 6 Months | 9 Months | 12 Months | |
|---|---|---|---|---|---|
| n=60 | n=59 | n=55 | n=55 | n=58 | |
| Physical Health | |||||
| General Health | |||||
| Excellent | 0 (0) | 2 (3.4) | 2 (3.6) | 0 (0) | 0 (0) |
| Very good | 0 (0) | 18 (31.5) | 30 (54.6) | 24 (43.6) | 24 (41.4) |
| Good | 0 (0) | 15 (25.4) | 7 (12.7) | 9 (16.4) | 16 (27.6) |
| Fair | 11 (18.3) | 17 (28.8) | 12 (21.8) | 18 (32.7) | 17 (29.3) |
| Poor | 49 (81.7) | 7 (11.9) | 4 (7.3) | 4 (7.3) | 1 (1.7) |
| Urinary Incontinence | 59 (98.3) | 23 (38.9) | 18 (32.7) | 20 (36.4) | 19 (32.8) |
| Frequency of Urinary Incontinence | |||||
| Never | 1 (1.7) | 36 (61) | 37 (67.3) | 35 (63.6) | 39 (67.2) |
| Once per week or less | 0 (0) | 1 (1.7) | 1 (1.8) | 3 (5.5) | 5 (8.6) |
| Two or three times per week | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Once per day | 2 (3.3) | 4 (6.7) | 1 (1.8) | 2 (3.6) | 4 (6.9) |
| Several times per day | 12 (20) | 7 (11.9) | 6 (10.9) | 7 (12.7) | 4 (6.9) |
| All the time | 45 (75) | 11 (18.6) | 10 (18.2) | 8 (14.6) | 6 (10.3) |
| Faecal Incontinence | 3 (5) | 1 (1.7) | 0 (0) | 0 (0) | 0 (0) |
| Menstrual Cycle* | n=55 | n=54 | n=50 | n=50 | n=53 |
| Regular | 18 (32.7) | 29 (53.7) | 35 (70) | 33 (66.6) | 32 (60.4) |
| Irregular | 2 (3.6) | 2 (3.7) | 1 (2) | 3 (6) | 5 (9.4) |
| Amenorrheic | 35 (63.6) | 23 (42.6) | 14 (28) | 14 (28) | 16 (30.2) |
| Psychosocial Health | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) |
| Reintegration | 33.2 (20.4) | 70.4 (27.1) | 78.0 (23.7) | 75.9 (25.7) | 78.4 (19.2) |
| Self-Esteem | 44.4 (15.4) | 64.2 (19.0) | 72.4 (24.0) | 69.9 (20.3) | 70.7 (19.8) |
| Depressive symptoms | 36.1 (16.9) | 10.5 (13.2) | 7.5 (9.6) | 8.4 (11.8) | 5.2 (7.7) |
| Quality of Life | |||||
| Overall | 17.5 (10.7) | 56.9 (16.5) | 54.2 (16.5) | ||
| Physical | 47.9 (24.2) | 81.4 (16.5) | 75.3 (13.4) | ||
| Environment | 41.0 (15.1) | 58.9 (11.9) | 60.2 (11.2) | ||
| Social Relationships | 38.2 (22.2) | 49.5 (22.7) | 52.6 (15.9) | ||
| Psychological | 24.4 (15.1) | 65.7 (21.6) | 69.0 (17.4) | ||
| PTSD Screen Positive N (%) | 10 (16.7) | 1 (1.8) | 0 (0) | ||
| Stigma | |||||
| Negative Self-Perception | 74.7 (36.2) | 16.4 (32.5) | 14.5 (29.4) | 14.5 (32.9) | 17.8 (33.6) |
| Social Isolation | 18.5 (27.2) | 3.4 (10.1) | 3.4 (13.3) | 3.3 (10.3) | 1.4 (6.1) |
| Verbal Abuse | 18.1 (26.5) | 2.7 (7.8) | 2.3 (7.2) | 1.7 (6.4) | 1.2 (3.8) |
| Fear of Contagion | 6.7 (18.4) | 2.5 (8.7) | 0.9 (5.0) | 0.9 (5.0) | 0 (0) |
| Social Support | 42.7 (10.0) | 45.6 (12.3) | 56.1 (20.5) | 44.4 (11.6) | 55.7 (19.4) |
Note:
among age<45 only. Notes: Mean (SD). Improvement is represented by increases in value for reintegration, self-esteem, and quality of life and decreases in depressive symptoms and stigma. Psychosocial measures are standardized to range 0-100.
Across the twelve-month study, most women reported improvements in physical health (Table 2). The largest improvement in general health status was observed from baseline to three months where report of general health as excellent, very good or good increased from 0% to 60%. Continued improvement was observed through six months (71%). Urinary incontinence, reported by 98% at baseline, was the most prevalent continuing physical symptom. The greatest improvement in urinary incontinence was between baseline and three months (39%). Continued reduction in urinary incontinence was reported through six months (33%). Among the 19 women reporting persistent incontinence at twelve months, 53% reported it at least once to several or more times per day, and 26% reported it once per week or less. Among those with faecal incontinence at baseline (n=3), the one post-surgical persistent case resolved by six months. Among women age <45y, 64% reported amenorrhea at baseline, which dropped to 43% at three months, and to 28% at six months.
Other fistula-related physical symptoms also declined over follow-up (Figure 1). Large declines were observed from baseline through three months in vaginal pain (45%−15%), general pain (37%−12%), difficulty walking (33%−12%), and skin irritation (28%−9%). Continued but less pronounced reductions were observed for vaginal pain, general pain, and difficulty walking. By 12 months after surgery, 9% reported general pain, 7% skin irritation, 5% reported vaginal pain and 4% difficulty walking. Declines in vaginal discharge were less steep than the other symptoms, dropping from 32% to 20% in the first three months following surgery, with only 2% reporting vaginal discharge by 12 months. Pain with urination dropped rapidly between baseline and 3 months (30% to 19%), plateaued at 6 through 9 months (15%) and further decreased by 12 months (7%). General weakness changed minimally from baseline to three months (33% to 27%) and declined more steeply through six months (9%), but this gain was not maintained; general weakness at nine and twelve months was 16% and 17%, respectively. After urinary incontinence, weakness was the second most prevalent fistula-related symptom at twelve months post-surgery.
Reintegration and Psychosocial Health across Study Follow-Up
Similarly, improvement was observed across study follow-up in all psychosocial health indicators of reintegration, self-esteem, depressive symptoms, quality of life, PTSD, stigma, and social support (Figure 1; Table 2). Psychosocial indicators were standardized to range 0-100. Mean reintegration score at baseline was 33.2, increased substantially to 70.4 at three months post-surgery, gained an additional eight percentage points to 78.0 at six months and maintained through the end of the study. Self-esteem at baseline was mean 44.4, increased to 64.2 at 3 months and 72.4 at 6 months, and remained stable thereafter. Mean depressive symptoms also saw the greatest improvement from baseline to three months, (36.1 to 10.5), followed by a small decrease to 5.2 at 12 months. Over the twelve months, depressive symptomatology decreased from 85% to 7% (not shown).
We observed considerable elevations across all quality of life domains from baseline through 6 months post-surgery, but no further change through 12 months. The greatest mean increases from baseline to 6 months were for overall QOL (17.5 to 56.9) and the psychological health domain (24.4 to 65.7). Smaller increases, but still substantial, were observed for social relationships (38.2 to 49.5) and environment (41.0 to 58.9) domains. Ten participants (17%) screened positive for PTSD symptoms at baseline, reduced to one (2%) at 6 months, and none at 12 months.
At baseline, the highest mean fistula-related stigma score was observed for the negative self-perception domain at 74.7 followed by the social isolation and verbal abuse domains (18.5 and 18.1, respectively). Mean score for fear of contagion was the lowest, at 6.7. Substantial declines were observed across all stigma domains during follow-up, with the largest improvements between baseline and three months. Mean stigma score improved by approximately 80% between baseline and three months for the domains of verbal abuse, social isolation, and negative self-perception. Continued decline occurred through 12 months for verbal abuse (mean 1.2), and social isolation (mean 1.4). For negative self-perception, the decline continued through 6 months post-surgery, but a small uptick occurred at 12 months (mean 17.8).
Psychosocial Health among Women with Fistula-Related Physical Symptoms
We assessed the relationship between urinary incontinence or other fistula-related physical symptoms and indicators of women’s psychosocial health (Table 3). Across study follow-up, self-report of physical symptoms largely correlated with significantly lower psychosocial health. Mean reintegration score differed by about 20 points at each time point comparing women reporting physical symptoms to those reporting no symptoms. At twelve months, women reporting physical symptoms had a mean reintegration score 21.9 points lower than women reporting no physical symptoms (95% CI: −30.2, −13.5). Self-esteem among women reporting physical symptoms was also significantly lower: this difference ranged in magnitude from mean 19.3 points lower at three months (95% CI −29.3, −9.4) to 21.2 points lower at 12 months (95% CI −30.1, −12.4). Women reporting physical symptoms had significantly higher mean depression at 3, 9, and 12 months by about eight points. At twelve months, women reporting physical symptoms scored on average 7.8 points higher (95% CI 4.3, 11.3) on the standardized depression measure compared to those with no symptoms. Physical symptoms were associated with substantial differences in quality of life domains as well. At twelve months, we observed an approximately twenty-point lower value in overall quality of life (−22.5, 95% CI −28.9, −16.1) and in the physical (−17.1, 95% CI −22.5, −11.7), and psychological domains (−19.1, 95% CI −26.8, −11.4) for women reporting physical symptoms compared to those reporting no symptoms. Slightly lower differences were observed for quality of life domains of social relationships (−13.1, 95% CI −20.7, −5.4) and environment (−13.2, 95% CI −18.0, −8.4). Differences in stigma by report of physical symptoms were less consistent. Across all time points, large and statistically significant differences in the stigma domain of negative-self-perception were observed, with a mean 22.5 at baseline (95% CI 4.2-40.8) and rising to 34.0 (95% CI 18.8-49.1) at 12 months. Smaller and largely non-significant differences were identified across symptom categories for the stigma domains social isolation, verbal abuse, and fear of contagion. The reduction in difference for social isolation by twelve months was less than that observed for the other domains.
Table 3.
Unadjusted Linear Regression Models of Relationships between Urinary Incontinence or Other Fistula-Related Physical Symptom and Psychosocial Health across Study Follow-Up
| Three Months | Six Months | Nine Months | Twelve Months | |||||
|---|---|---|---|---|---|---|---|---|
| B (95% CI) | P | B (95% CI) | P | B (95% CI) | P | B (95% CI) | P | |
| Reintegration Measure | −24.1 (−38.8,−9.4) | 0.0018 | −18.2 (−30.2,−6.2) | 0.0038 | −22.6 (−35.6,−9.5) | 0.001 | −21.9 (−30.2,−13.5) | <0.0001 |
| Self-Esteem | −19.3 (−29.3,−9.4) | 0.0003 | −9.1 (−19.8,1.6) | 0.095 | −17.9 (−28.2,−7.6) | 0.001 | −21.2 (−30.1,−12.4) | <0.0001 |
| Depression | 10.7 (3.4,18) | 0.0047 | 2.7 (−2.5,7.9) | 0.3071 | 8.3 (2.1,14.5) | 0.0098 | 7.8 (4.3,11.3) | <0.0001 |
| Quality of Life | ||||||||
| Overall | −15.8 (−23.8,−7.8) | 0.0002 | −22.5 (−28.9,−16.1) | <0.0001 | ||||
| Physical | −17.6 (−25.3,−9.9) | <0.0001 | −17.1 (−22.5,−11.7) | <0.0001 | ||||
| Psychological | −17.9 (−28.7,−7.1) | 0.0016 | −19.1 (−26.8,−11.4) | <0.0001 | ||||
| Social Relationships | −13.1 (−25.1,−1.2) | 0.0321 | −13.1 (−20.7,−5.4) | 0.0012 | ||||
| Environment | −3.8 (−10.3,2.7) | 0.2443 | −13.2 (−18,−8.4) | <0.0001 | ||||
| Stigma | ||||||||
| Verbal Abuse | 3.7 (−0.8,8.2) | 0.106 | 0.3 (−3.6,4.3) | 0.8649 | 2.2 (−1.4,5.7) | 0.2236 | 2.3 (0.1,4.5) | 0.0415 |
| Negative Self-Perception | 22.5 (4.2,40.8) | 0.0169 | 22.1 (7.1,37.1) | 0.0046 | 23.5 (6.2,40.8) | 0.0086 | 34 (18.8,49.1) | <0.0001 |
| Social Isolation | 4.9 (−1,10.8) | 0.0989 | 2.4 (−4.9,9.7) | 0.5122 | 5.4 (−0.2,10.9) | 0.0568 | 4.2 (−0.7,9.1) | 0.091 |
| Fear of Contagion | 3.5 (−1.5,8.5) | 0.1706 | −0.9 (−3.6,1.9) | 0.5352 | 1.5 (−1.3,4.2) | 0.2923 | 0.6 (−0.6,1.7) | 0.3048 |
Improvement is represented by increases in value for reintegration, self-esteem, and quality of life and decreases in depressive symptoms and stigma. At each time point the values presented reflect the difference between those currently reporting symptoms versus those reporting no symptoms. Psychosocial measures are standardized to range 0-100.
Discussion
Our study is the first to prospectively assess trajectories of physical and psychosocial recovery in the first year following surgery for obstetric fistula. In this longitudinal cohort of women in Uganda, women experienced dramatic improvements in physical and psychosocial health following surgery. The most substantial gains were typically observed by 3 months with continued improvement through 6 months, after which little change was observed. Further, we quantified the large disparity in psychosocial health between women with persistent physical symptoms compared to those without, identifying significant differences across most indicators.
The most common persistent physical symptoms at 12 months post-surgery were urinary incontinence (32.8%) and weakness (17.2%). While the 12-month values represent a substantial reduction from baseline, the proportion of women with persistent symptoms is nonetheless concerning. Our findings on urinary incontinence were on the higher end of those reported in other studies reporting persistent incontinence rates of in 16-35% (13, 18, 32, 53–55). Our identification of non-incontinence-related persistent symptoms is also not unique; in a qualitative study of women repaired for fistula in Ethiopia, Donnelley et al reported that 40% of women reported physical health problems following surgery irrespective of their repair status(28). The substantial and significant differences in level of reintegration comparing women with persistent physical symptoms and those without supports additional intervention to resolve physical symptoms in order to support women’s recovery or more targeted psychosocial support and reintegration services to ensure that those coping with physical or psychosocial challenges are appropriately supported.
Our findings demonstrating dramatic improvement in quality of life following surgery are consistent with other reports,20,24,31 although several interesting differences in mean value and changes over time across setting are notable in two studies in India and Nigeria also using the WHO QOL BREF that followed women through six months (Nigeria) and median 26 months (India) after surgery(56, 57). The lowest pre-operative QOL score for all domains except social relationships and the largest improvements from the pre-to the post-operative period were in India. In India and Nigeria, significant improvements were noted in the physical, psychosocial, and social domains but no change was observed for the environment domain. The largest improvements in Uganda and India were observed in the physical domain. Further comparison with population-based samples of healthy women of reproductive age would help to place these data into context. Additional research on the contextual factors responsible for the differences identified in overall experience and change across time could help inform efforts to improve recovery trajectories across various cultural contexts.
We found substantial reductions across the dimensions of fistula-related stigma for the 12-month period, with the steepest declines observed from baseline through three months. In this cohort, negative self-perception was the most severe type of stigma experienced across all time points. Compared to negative self-perception, the relatively lower report of stigma domains representing enacted stigma (verbal abuse, social isolation, and fear of contagion) may be partially explained by nearly half of our cohort achieving surgery within 3 months of fistula development. Our finding of persistent stigma is consistent with one qualitative study of Ethiopian women’s post-surgical quality of life, where persistent internalized and enacted stigma were reported at mean 1.5 years following surgery irrespective of surgical outcome(28). Literature from other stigmatized conditions describes a complex relationship between perceived community stigma and internalized stigma(58), and supports a strong relationship between internalized stigma and depression and other poor health outcomes(59–61), highlighting the need for psychosocial intervention at multiple levels to reduce stigma experiences and associated consequences (62, 63).
The substantial differences observed in psychosocial outcomes comparing women with physical symptoms to those without highlights the need for identification of strategies to treat or better manage post-surgical fistula-related symptoms. Our results suggest that the greatest overall physical health benefits occur during the first six months following surgery, with concurrent psychosocial health improvement. Our findings that improvements in physical and psychosocial health indicators stagnated at about six months are consistent with qualitative work conducted in Kenya by Khisa et al(64). Khisa describes a ‘miracle phase’ in the immediate post-surgical period among women with successful repair. While some of the stagnation in trend may be due to floor and ceiling effects, our results may be also be influenced by individual experiences not explored here including fistula-related characteristics or experiences, sexual relationships, concerns around achieving or preventing pregnancy, and exposure to violence. Other factors such as poverty, lack of empowerment, and lack of social support, may also structure health status, and thus our findings may represent physical and psychosocial health status comparable to similar women of reproductive age in this setting who did not develop fistula. Subsequent work should explore the contributions of other factors, and development of interventions to improve recovery will benefit from the inclusion of theory-based conceptual models for recovery from mental health diagnoses suggest areas for counselling foci that are particularly salient for women recovering from fistula, based on our findings here and other literature (65).
We recognize several limitations to this study. Our sample size was based on feasibility; thus our results should be validated in larger samples. Despite our small sample, our rates of participation were high, and our cohort was representative of women accessing fistula repair at Mulago Hospital during the recruitment period. Both similarities and important differences in women’s experiences of fistula and recovery are observed in the literature, thus a nuanced assessment of the contextual factors contributing to these differences across countries will help establish the generalizability of our results. In particular, many women in our cohort rapidly accessed surgery and nearly thirty percent of infants survived the labour resulting in the fistula, suggesting improved care access for this cohort compared to some other studies. Our sample included participants with childbirth-related fistula due to pressure necrosis from obstructed labor and iatrogenic etiologies; however, designation of likely iatrogenic among this sample was retrospectively assigned using medical record criteria(36). Our findings can be considered generally representative of women with obstetric fistula, but further research exploring differences in recovery trajectories by etiology is of interest, particularly as iatrogenic female genital fistula appears to be increasing(66). Our study is both strengthened and limited by the length of follow-up; our focus on the twelve months following surgery expands the length of follow-up conducted in many other studies, yet may be inadequate to understand the rates and consequences of fistula recurrence and adverse perinatal outcome over a woman’s reproductive life, both of which have been found to be high among women receiving surgical repair for obstetric fistula(67).
Reducing the impact of fistula-related maternal morbidity on the health of women requires their engagement in the full continuum of fistula-related management. Prevention is key and improving women’s timely access to surgical repair of fistula is critical. Yet limiting attention to women recovering from fistula in the immediate post-surgical period is inadequate. Intervention programming to support the spectrum of women’s physical and psychosocial needs during their recovery from fistula may result in improved outcomes after repair. Efforts must also be made to maintain women’s engagement with health systems and to improve the responsiveness of health systems to women’s needs following surgery to protect maternal health and well-being.
Supplementary Material
Supplemental Table 1. Description of Physical and Psychosocial Health Measures
Supplemental Table 2. Psychosocial health indicators across study twelve-month study follow-up, Unstandardized
Acknowledgments
Declarations
Acknowledgements: The authors would like to recognize our study participants for their commitment to this study, and thank Erin Mielke and Mary Ellen Stanton for their comments and Amy J. Markowitz, JD, for her editorial support. Luganda translations for WHO QOL-BREF and the Hopkins Symptom Checklist were created by The School of International Development, University of East Anglia, UK; and The Social Science Programme, Medical Research Council/UVRI Uganda Research Unit on AIDS, Entebbe, Uganda. Funding for open source publication was provided by the Fistula Care Plus Project, administered by EngenderHealth (cooperative agreement AID-OAA-A14-00013), and the opinions expressed herein are those of the authors and do not necessarily reflect the views of USAID, or the United States Government.
Ethics Approval: The study protocol was approved by the Makerere University College of Health Sciences, School of Medicine Research and Ethics Committee (#2014-052, Apr 2014), the Uganda National Council for Science and Technology (#154/212/01, June 2015), and the University of California, San Francisco Human Research Protection Program, Committee on Human Research (#12-09573, Oct 2012).
Funding: The study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the United States National Institutes of Health (NICHD; Project number R21HD075008), the Fistula Foundation and from the United States Agency for International Development (USAID) via the Fistula Care Plus Project, administered by EngenderHealth (cooperative agreement AID-OAA-A14-00013). The opinions expressed are those of the authors and do not necessarily reflect the views of USAID, or the United States Government. Continuing analytical work was funded by NICHD (Project number K99HD086232).
References
- 1.Arrowsmith S, Hamlin EC, Wall LL. Obstructed labor injury complex: obstetric fistula formation and the multifaceted morbidity of maternal birth trauma in the developing world. Obstet Gynecol Surv. 1996;51(9):568–74. [DOI] [PubMed] [Google Scholar]
- 2.Ahmed S, Holtz SA. Social and economic consequences of obstetric fistula: life changed forever? Int J Gynaecol Obstet. 2007;99 Suppl 1:S10–5. [DOI] [PubMed] [Google Scholar]
- 3.Browning A, Menber B. Women with obstetric fistula in Ethiopia: a 6-month follow-up after surgical treatment. BJOG. 2008;115:1564–9. [DOI] [PubMed] [Google Scholar]
- 4.Roush KM. Social implications of obstetric fistula: an integrative review. J Midwifery Womens Health. 2009;54(2):e21–33. [DOI] [PubMed] [Google Scholar]
- 5.Turan JM, Johnson K, Polan ML. Experiences of women seeking medical care for obstetric fistula in Eritrea: implications for prevention, treatment, and social reintegration. Glob Public Health. 2007;2(1):64–77. [DOI] [PubMed] [Google Scholar]
- 6.Siddle K, Mwambingu S, Malinga T, Fiander A. Psychosocial impact of obstetric fistula in women presenting for surgical care in Tanzania. Int Urogynecol J. 2013;24(7):1215–20. [DOI] [PubMed] [Google Scholar]
- 7.Ashford L Obstetric Fistula: Cause of Stigma and Disability in Less Developed Countries. Population Reference Bureau; 2002. retrieved 9/2003. [Google Scholar]
- 8.Bangser M Obstetric fistula and stigma. Lancet. 2006;367(9509):535–6. [DOI] [PubMed] [Google Scholar]
- 9.Gebresilase YT. A qualitative study of the experience of obstetric fistula survivors in Addis Ababa, Ethiopia. International journal of women’s health. 2014;6:1033–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ojengbede OA, Baba Y, Morhason-Bello IO, Armah M, Dimiti A, Buwa D, et al. Group psychological therapy in obstetric fistula care: a complementary recipe for the accompanying mental ill health morbidities? Afr J Reprod Health. 2014;18(1):155–9. [PubMed] [Google Scholar]
- 11.Zeleke BM, Ayele TA, Woldetsadik MA, Bisetegn TA, Adane AA. Depression among women with obstetric fistula, and pelvic organ prolapse in northwest Ethiopia. BMC psychiatry. 2013;13:236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weston K, Mutiso S, Mwangi JW, Qureshi Z, Beard J, Venkat P. Depression among women with obstetric fistula in Kenya. Int J Gynaecol Obstet. 2011;115(1):31–3. [DOI] [PubMed] [Google Scholar]
- 13.Wall LL. Obstetric vesicovaginal fistula as an international public-health problem. Lancet. 2006;368(9542):1201–9. [DOI] [PubMed] [Google Scholar]
- 14.WHO. Obstetric Fistula: Guiding Principles for Clinical Management and Programme Development. 2006. [DOI] [PubMed] [Google Scholar]
- 15.Adler AJ, Ronsmans C, Calvert C, Filippi V. Estimating the prevalence of obstetric fistula: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2013;13:246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kayondo M, Wasswa S, Kabakyenga J, Mukiibi N, Senkungu J, Stenson A, et al. Predictors and outcome of surgical repair of obstetric fistula at a regional referral hospital, Mbarara, western Uganda. BMC Urology. 2011;11(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Bernis L Obstetric fistula: guiding principles for clinical management and programme development, a new WHO guideline. Int J Gynaecol Obstet. 2007;99 Suppl 1:S117–21. [DOI] [PubMed] [Google Scholar]
- 18.Delamou A, Diallo M, Beavogui AH, Delvaux T, Millimono S, Kourouma M, et al. Good clinical outcomes from a 7-year holistic programme of fistula repair in Guinea. Trop Med Int Health. 2015;20(6):813–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arrowsmith SD, Ruminjo J & Landry EG. Current Practices in Treatment of Female Genital Fistula: A Cross Sectional Study. BMC Pregnancy & Childbirth. 2010;10(73). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Browning A Risk factors for developing residual urinary incontinence after obstetric fistula repair. British Journal of Obstetrics and Gynaecology. 2006;113:482–85. [DOI] [PubMed] [Google Scholar]
- 21.Pope R, Bangser M, Requejo JH. Restoring dignity: social reintegration after obstetric fistula repair in Ukerewe, Tanzania. Glob Public Health. 2011;6(8):859–73. [DOI] [PubMed] [Google Scholar]
- 22.Wilson SM, Sikkema KJ, Watt MH, Masenga GG, Mosha MV. Psychological Symptoms and Social Functioning Following Repair of Obstetric Fistula in a Low-Income Setting. Matern Child Health J. 2016;20(5):941–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Browning AM B Women with Obstetric Fistula in Ethiopia: A 6 Month Follow Up After Surgical Treatment. British Journal of Obstetrics and Gynaecology. 2008;115:1564–9. [DOI] [PubMed] [Google Scholar]
- 24.Wilson SM, Sikkema KJ, Watt MH, Masenga GG. Psychological Symptoms Among Obstetric Fistula Patients Compared to Gynecology Outpatients in Tanzania. International journal of behavioral medicine. 2015;22(5):605–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Landry E, Frajzyngier V, Ruminjo J, Asiimwe F, Barry TH, Bello A, et al. Profiles and experiences of women undergoing genital fistula repair: Findings from five countries. Glob Public Health. 2013;8(8):926–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Women’s Dignity Project, EngenderHealth. Sharing the Burden: Ugandan Women Speak about Obstetric Fistula. Dat es Salaam, Tanzania: Women’s Dignity Project and EngenderHealth; 2007. [Google Scholar]
- 27.Bangser M Strengthening public health priority-setting through research on fistula, maternal health, and health inequities. Int J Gynaecol Obstet. 2007;99 Suppl 1:S16–20. [DOI] [PubMed] [Google Scholar]
- 28.Donnelly K, Oliveras E, Tilahun Y, Belachew M, Asnake M. Quality of life of Ethiopian women after fistula repair: implications on rehabilitation and social reintegration policy and programming. Culture, health & sexuality. 2015;17(2):150–64. [DOI] [PubMed] [Google Scholar]
- 29.Anzaku SA, Lengmang SJ, Mikah S, Shephard SN, Edem BE. Sexual activity among Nigerian women following successful obstetric fistula repair. Int J Gynaecol Obstet. 2017;137(1):67–71. [DOI] [PubMed] [Google Scholar]
- 30.Khisa AM, Nyamongo IK. Still living with fistula: an exploratory study of the experience of women with obstetric fistula following corrective surgery in West Pokot, Kenya. Reprod Health Matters. 2012;20(40):59–66. [DOI] [PubMed] [Google Scholar]
- 31.El-Gazzaz G, Hull TL, Mignanelli E, Hammel J, Gurland B, Zutshi M. Obstetric and cryptoglandular rectovaginal fistulas: long-term surgical outcome; quality of life; and sexual function. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2010;14(11):1758–63. [DOI] [PubMed] [Google Scholar]
- 32.Nielsen HS, Lindberg L, Nygaard U, Aytenfisu H, Johnston OL, Sorensen B, et al. A community-based long-term follow up of women undergoing obstetric fistula repair in rural Ethiopia. Bjog. 2009;116(9):1258–64. [DOI] [PubMed] [Google Scholar]
- 33.Wall LL, Arrowsmith SD, Briggs ND, Lassey A. Urinary Incontinence in the Developing World: The Obstetric Fistula In: Abrams P, Cardozo L, Khoury S, Wein A, Incontinence. Plymouth, U.K.: Health Publication Ltd; 2002. [Google Scholar]
- 34.Wall LL. Dead mothers and injured wives: the social context of maternal morbidity and mortality among the Hausa of northern Nigeria. Stud Fam Plann. 1998;29(4):341–59. [PubMed] [Google Scholar]
- 35.Byamugisha J, El Ayadi A, Obore S, Mwanje H, Kakaire O, Barageine J, et al. Beyond repair - family and community reintegration after obstetric fistula surgery: study protocol. Reprod Health. 2015;12:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Raassen TJ, Ngongo CJ, Mahendeka MM. Iatrogenic genitourinary fistula: an 18-year retrospective review of 805 injuries. Int Urogynecol J. 2014;25(12):1699–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lorig K, Steward A, Ritter P, Gonzalez V, Laurent D, Lynch J. Outcome Measures for Health Education and Other Health Care Interventions. Thousand Oaks, CA: Sage Publications; 1996. [Google Scholar]
- 38.Klovning A, Avery K, Sandvik H, Hunskaar S. Comparison of two questionnaires for assessing the severity of urinary incontinence: The ICIQ-UI SF versus the incontinence severity index. Neurourol Urodyn. 2009;28(5):411–5. [DOI] [PubMed] [Google Scholar]
- 39.El Ayadi A, Byamugisha J, Obore S, Mwanje H, Kakaire O, Barageine J, et al. Development and preliminary validation of a post-fistula repair reintegration instrument among Ugandan women. Reproductive Health Journal. 2017;14(1):109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bolton P, Wilk CM, Ndogoni L. Assessment of depression prevalence in rural Uganda using symptom and function criteria. Social psychiatry and psychiatric epidemiology. 2004;39(6):442–7. [DOI] [PubMed] [Google Scholar]
- 41.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behavioral Science. 1974;19(1):1–15. [DOI] [PubMed] [Google Scholar]
- 42.Martin F, Russell S, Seeley J. The WHOQOL BREF questionnaire in Luganda: Validation with a sample including people living with HIV in Uganda. Working Paper 46. Norwich, United Kingdom: School of International Development, University of East Anglia; 2013. [Google Scholar]
- 43.Webster J, Nicholas C, Velacott C, Cridland N, Fawcett L. Validation of the WHOQOL-BREF among women following childbirth. Aust N Z J Obstet Gynaecol. 2010;50(2):132–7. [DOI] [PubMed] [Google Scholar]
- 44.Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 45.Holzemer WL, Uys LR, Chirwa ML, Greeff M, Makoae LN, Kohi TW, et al. Validation of the HIV/AIDS Stigma Instrument - PLWA (HASI-P). AIDS Care. 2007;19(8):1002–12. [DOI] [PubMed] [Google Scholar]
- 46.Prins A, Ouimette P, Kimerling R, Cameron RP, Hugelshofer DS, Shwaw-Hegwer J, et al. The primary care PTSD screen (PC_PTSD): development and operating characteristics. Primary Care Psychiatry. 2003;9:9–14. [Google Scholar]
- 47.Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. Journal of personality assessment. 1990;55(3-4):610–7. [DOI] [PubMed] [Google Scholar]
- 48.Nakigudde J, Musisi S, Ehnvall A, Airaksinen E, Agren H. Adaptation of the multidimensional scale of perceived social support in a Ugandan setting. Afr Health Sci. 2009;9 Suppl 1:S35–41. [PMC free article] [PubMed] [Google Scholar]
- 49.Bolton P, Bass J, Neugebauer R, Verdeli H, Clougherty KF, Wickramaratne P, et al. Group interpersonal psychotherapy for depression in rural Uganda: a randomized controlled trial. JAMA. 2003;289(23):3117–24. [DOI] [PubMed] [Google Scholar]
- 50.Kaida A, Matthews LT, Ashaba S, Tsai AC, Kanters S, Robak M, et al. Depression during pregnancy and the postpartum among HIV-infected women on antiretroviral therapy in Uganda. J Acquir Immune Defic Syndr. 2014;67 Suppl 4:S179–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Psaros C, Haberer JE, Boum Y 2nd, Tsai AC, Martin JN, Hunt PW, et al. The factor structure and presentation of depression among HIV-positive adults in Uganda. AIDS and behavior. 2015;19(1):27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ashaba S, Kakuhikire B, Vorechovska D, Perkins JM, Cooper-Vince CE, Maling S, et al. Reliability, Validity, and Factor Structure of the Hopkins Symptom Checklist-25: Population-Based Study of Persons Living with HIV in Rural Uganda. AIDS and behavior. 2018;22(5):1467–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Semere L, Nour NM. Obstetric fistula: living with incontinence and shame. Reviews in obstetrics and gynecology. 2008;1(4):193–7. [PMC free article] [PubMed] [Google Scholar]
- 54.Lewis A, Kaufman MR, Wolter CE, Phillips SE, Maggi D, Condry L, et al. Genitourinary fistula experience in Sierra Leone: review of 505 cases. The Journal of urology. 2009;181(4):1725–31. [DOI] [PubMed] [Google Scholar]
- 55.Nardos R, Browning A, Chen CC. Risk factors that predict failure after vaginal repair of obstetric vesicovaginal fistulae. Am J Obstet Gynecol. 2009;200(5):578, e1–4. [DOI] [PubMed] [Google Scholar]
- 56.Singh V, Jhanwar A, Mehrotra S, Paul S, Sinha RJ. A comparison of quality of life before and after successful repair of genitourinary fistula: Is there improvement across all the domains of WHOQOL-BREF questionnaire? African Journal of Urology. 2015;21(4):230–4. [Google Scholar]
- 57.Umoiyoho AJ, Inyang-Etoh EC, Abah GM, Abasiattai AM, Akaiso OE. Quality of life following successful repair of vesicovaginal fistula in Nigeria. Rural Remote Health. 2011;11(3):1734. [PubMed] [Google Scholar]
- 58.Turan B, Budhwani H, Fazeli PL, Browning WR, Raper JL, Mugavero MJ, et al. How Does Stigma Affect People Living with HIV? The Mediating Roles of Internalized and Anticipated HIV Stigma in the Effects of Perceived Community Stigma on Health and Psychosocial Outcomes. AIDS and behavior. 2017;21(1):283–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, Turan JM. Framing Mechanisms Linking HIV-Related Stigma, Adherence to Treatment, and Health Outcomes. Am J Public Health. 2017;107(6):863–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Turan B, Smith W, Cohen MH, Wilson TE, Adimora AA, Merenstein D, et al. Mechanisms for the Negative Effects of Internalized HIV-Related Stigma on Antiretroviral Therapy Adherence in Women: The Mediating Roles of Social Isolation and Depression. J Acquir Immune Defic Syndr. 2016;72(2):198–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sweeney SM, Vanable PA. The Association of HIV-Related Stigma to HIV Medication Adherence: A Systematic Review and Synthesis of the Literature. AIDS and behavior. 2016;20(1):29–50. [DOI] [PubMed] [Google Scholar]
- 62.Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? Journal of the International AIDS Society. 2013;16(3 Suppl 2):18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Takada S, Weiser SD, Kumbakumba E, Muzoora C, Martin JN, Hunt PW, et al. The dynamic relationship between social support and HIV-related stigma in rural Uganda. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 2014;48(1):26–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Khisa W, Wakasiaka S, McGowan L, Campbell M, Lavender T. Understanding the lived experience of women before and after fistula repair: a qualitative study in Kenya. BJOG. 2017;124(3):503–10. [DOI] [PubMed] [Google Scholar]
- 65.Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. The British journal of psychiatry : the journal of mental science. 2011;199(6):445–52. [DOI] [PubMed] [Google Scholar]
- 66.Wright J, Ayenachew F, Ballard KD. The changing face of obstetric fistula surgery in Ethiopia. International journal of women’s health. 2016;8:243–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Delamou A, Delvaux T, El Ayadi AM, Tripathi V, Camara BS, Beavogui AH, et al. Fistula recurrence, pregnancy, and childbirth following successful closure of female genital fistula in Guinea: a longitudinal study. The Lancet Global health. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1. Description of Physical and Psychosocial Health Measures
Supplemental Table 2. Psychosocial health indicators across study twelve-month study follow-up, Unstandardized


