Abstract
Transient osteoporosis is a rare condition causing regional pain, immobility and functional compromise. The authors present the case of a pregnant lady with multiple sites of transient osteoporosis, including a stress fracture, successfully treated with intravenous pamidronate and a physical rehabilitation programme. The authors discuss the mechanisms for the syndrome and its overlap with complex regional pain syndrome type I; as well as the implications of bisphosphonate administration to a nursing mother. The authors also highlight the advantages of MRI over standard radiography when investigating unexplained foot pain.
Background
Transient osteoporosis is a rare condition and occurs most commonly in the hip, and also in the knee, foot, ankle and hand. It typically affects middle-aged men, and pregnant women usually in the third trimester, although it can occur in all age groups including children. This case reviews the current literature with regard to the treatment and difficulties in a pregnant lady. It also highlights the need for a full investigation of the ongoing pain in the view of normal radiographs and demonstrates the superiority of MRI over plain radiography. Although multiple sites may be affected, our case is unusual in that the condition occurred in four separate sites, of which one was associated with a stress fracture.
Case presentation
A 37-year-old nulliparous part-time secretary developed pain around the dorsum of her left foot at 26 weeks gestation. It worsened with exercise and was better when she rested. At 31 weeks gestation, after heavy exercise she felt severe pain poorly localised to her left foot that she rated 10/10 associated with clamminess, sweating and transient urinary incontinence. She felt that she had broken her foot although there had been no trauma. She received analgesics but her mobility deteriorated and she required two crutches. At 33 weeks gestation, she presented to the Royal London Hospital because of pain in her left foot having hit her right foot. She rated the pain 10/10, described that when the right foot was knocked she could feel pain in the left foot radiating up her leg to her groin. She described ‘pins and needles’ in the left foot.
Previously she had fractured ribs and her left wrist after falling. Bilateral ulnar neuropathies diagnosed without nerve conduction studies had resolved. She had gestational diabetes mellitus, cervical spondylosis, eczema, rosacea and ‘infected-bite syndrome’. She described herself as anxious and exercised regularly walking up to 6 miles. She took paracetamol 4 g and codeine 240 mg daily.
She was unable to mobilise. Her weight was 55 kg. Examination revealed soft tissue swelling around the left foot. Straight leg raise was to 60 ° on the right and 0 ° on the left. Neurological examination was abnormal with dysaesthesia described around the left foot in a non-dermatomal pattern. Sensation was altered in the distribution of L3, L4 and S1 on the left side. No systemic features or back tenderness were reported and examination of her internal organs was normal.
Investigations
Routine blood tests including C reactive protein (CRP), antinuclear antibody and rheumatoid factor were all normal or negative. Lumbar spine radiograph was normal (figure 1A). Her left hip demonstrated bone oedema in the femoral head and a joint effusion on MRI. The right hip demonstrated a small amount of bony oedema with no joint effusion (figure 1B). These changes are characteristic of transient osteoporosis. She received intramuscular pethidine 100 mg and co-codamol (30/500 mg, eight tablets daily) and physiotherapy. She received an epidural and delivered a healthy baby girl on 18 November 2007 via a lower segment Caesarean section.
Figure 1.


(A) Normal lumbar spine. (B) Widespread bony oedema and joint effusion affecting left hip with localised bony oedema affecting right hip.
Treatment
As she had sustained previous fractures and was in continuing severe pain, she also received an infusion of 30 mg pamidronate with 1000 mg calcium and 800 IU vitamin D daily on day 3 postpartum and was told to express and discard her milk for the following 24 h. She had a beneficial response within 24 h with evidence of pain relief and increased mobilisation. She relapsed, however, and received another infusion of 30 mg pamidronate at day 8. She made a rapid recovery and was discharged mobilising with one crutch at day 12 postpartum.
Outcome and follow-up
Two months later she was still tender around her left ankle and knee but had normal ranges of movement in both of her hips. An MRI of her left ankle demonstrated a tibiotalar joint effusion and an insufficiency fracture of her talar dome (figure 2A) despite the normal x-ray appearances (figure 2B). An MRI of her left knee demonstrated bony oedema in her tibia (figure 2C). She received a third dose of 30 mg pamidronate. Fifteen months after initial presentation she was walking uninterrupted for 2 miles. She had intermittent pain from her right hip and a feeling of ‘fuzziness’ in her left foot but had returned to almost all of her normal activities. Her child was growing normally and attaining developmental milestones appropriate for her age.
Figure 2.

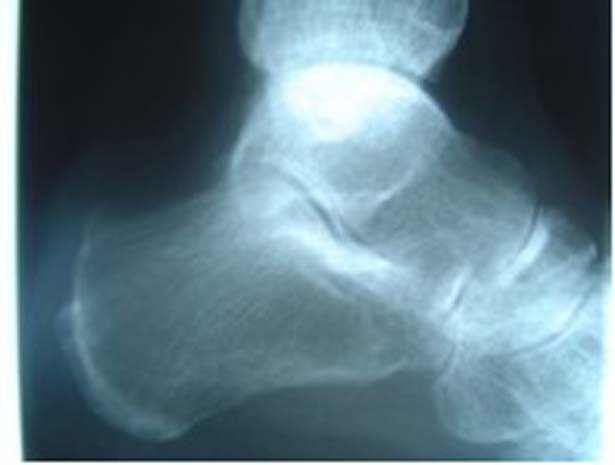

(A) MRI demonstrating stress fracture of talar dome. (B) Normal ankle x-ray taken at a similar time. (C) Bony oedema affecting tibial plateau.
Discussion
Transient osteoporosis was first described in three pregnant ladies by Curtiss and Kincaid in 1959.1 The condition is rare and occurs most commonly in the hip, but also in the knee, foot, ankle and hand. Middle-aged men and pregnant women, usually in the third trimester are seen most frequently, although transient osteoporosis affects all age groups including children. The disease probably occurs more frequently as the natural course is self-limiting with symptoms typically improving over 6–12 months.
Patients present with regional pain, immobility and functional impairment and can often identify the exact time of the onset of their symptoms. Demineralisation is radiographically evident about 1 month from the symptom onset and MRI changes have been reported within 48 h.2 Fractures, including the femoral neck, are rarely recognised to happen. Usually one joint is affected although multiple sites are recognised. Our case is unusual in having the condition identified in four separate sites, one of which was associated with a stress fracture.
Differential diagnosis includes avascular necrosis (AVN), stress fracture, neoplasm, infection, inflammatory arthritis and bone bruise. There are no specific serological tests but biochemical markers of bone turnover are increased including urinary hydroxyproline, N-telopeptide cross-linking region of type I collagen and fluoride.3 4 There is usually osteopaenic evidence on standard radiography and MRI demonstrates bone oedema with high-intensity signal seen on T2 weighted images. Radionuclide bone scans are hot around the area affected and can be used to distinguish between transient osteoporosis and AVN as the uptake is more pronounced and widespread in transient osteoporosis and is not associated with a ‘cold spot’ often seen in AVN around the anterosuperior femoral head.2 An ultrasound can demonstrate an effusion although this is less commonly present.
Standard treatment necessitates non-weight bearing activities, non-steroidal anti-inflammatory drugs, analgesics including strong opioids and gentle mobilisation of the affected limb including hydrotherapy. Other treatments have included sympathectomy, casting and corticosteroids.5 Salmon calcitonin has been used to good effect.2 Core decompression has also been used.6
Ibandronate, clodronate, pamidronate, neridronate, alendronate have all been used successfully in conjunction with calcium and vitamin D supplements in patients with transient osteoporosis.7–10 The use of bisphosphonates during pregnancy is controversial. Although bisphosphonates are known to cross the placental barrier and may have an effect on foetal serum calcium levels and growth there have been no reports of congenital abnormalities associated with use of bisphosphonates in animal teratology studies.11 Pamidronate has a plasma half-life of less than 3 h and there are no known metabolites. Pamidronate is also known to be undetectable in breast milk of nursing mothers in the first 48 h after a 30 mg infusion4 and is poorly absorbed via the oral route. Any pamidronate excreted in the breast milk is therefore unlikely to be absorbed by the baby. Our case demonstrated a good clinical response to pamidronate with no adverse effects to the child after 1 year of follow-up.
The pathogenesis of transient osteoporosis is unknown. MRI and radionuclide bone scans demonstrate the hyperaemia state and oedematous changes. Mechanisms that might predispose pregnant women to develop bone pathology include physiological hypercalciuria and oestrogen deficiency but this does not account for the imaging findings. Other mechanisms pertinent to hip demineralisation during pregnancy include compression of the pelvic sympathetic nerves, pudendal nerve and inferior vena cava as well as hypertriglyceridaemia and the carrying of extra weight.12 Interestingly more reported cases seem to involve the left hip than the right, although this needs further study. Histology of the acute phase has come from core decompression procedures where a raised intramedullary pressure evidenced by dilated medullary sinuses is found. Rarely there was necrotic marrow and no vascular occlusions were identified.13 A review of the histological changes noted that there was invariably evidence of changes in both bone and marrow in sites that corresponded to MRI changes with some areas of necrosis as well as reparative processes. Special stains demonstrated viable osteocytes as well as evidence of bone death. There is no evidence of an increase in osteoclastic activity to account for bisphosphonates’ therapeutic effects.2
Lequesne first suggested that transient osteoporosis is a reflex sympathetic dystrophy and more recently the hypothesis was revisited.14 15 However, in the absence of distal sympathetic nervous system dysregulation, vasomotor instability or trophic changes, the diagnosis of complex regional pain syndrome (CRPS) type I (formerly reflex sympathetic dystrophy) is difficult to make. Our case presented initially with some of these features in her left leg and this is enough for the diagnosis of CRPS in the absence of an alternative diagnosis.16
Finally, even though her radiograph was normal the MRI demonstrated a stress fracture in her talar dome. Persistent pain should be investigated appropriately.
In conclusion, we have presented a lady with transient osteoporosis of pregnancy in four separate sites and features of CRPS. We treated her successfully with intravenous pamidronate although she sustained a stress fracture during her recovery. Transient osteoporosis has been discussed with particular reference to the use of pamidronate in pregnancy and nursing mothers.
Learning points.
-
▶
Transient osteoporosis of pregnancy is a rare but important condition that can cause significant impairment.
-
▶
Treatment with bisphosphonate may be difficult in pregnancy.
-
▶
Persistent pain should be investigated appropriately: although radiographs were normal, MRI showed a stress fracture in this lady.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Curtiss PH, Jr, Kincaid WE. Transitory demineralization of the hip in pregnancy. A report of three cases. J Bone Joint Surg Am 1959;41-A:1327–33 [PubMed] [Google Scholar]
- 2.Arayssi TK, Tawbi HA, Usta IM, et al. Calcitonin in the treatment of transient osteoporosis of the hip. Semin Arthritis Rheum 2003;32:388–97 [DOI] [PubMed] [Google Scholar]
- 3.Berger CE, Kröner AH, Minai-Pour MB, et al. Biochemical markers of bone metabolism in bone marrow edema syndrome of the hip. Bone 2003;33:346–51 [DOI] [PubMed] [Google Scholar]
- 4.Siminoski K, Fitzgerald AA, Flesch G, et al. Intravenous pamidronate for treatment of reflex sympathetic dystrophy during breast feeding. J Bone Miner Res 2000;15:2052–5 [DOI] [PubMed] [Google Scholar]
- 5.Carmona-Ortells L, Carvajal-Méndez I, García-Vadillo JA, et al. Transient osteoporosis of the hip: successful response to deflazacort. Clin Exp Rheumatol 1995;13:653–5 [PubMed] [Google Scholar]
- 6.Berger CE, Kröner AH, Kristen KH, et al. Transient bone marrow edema syndrome of the knee: clinical and magnetic resonance imaging results at 5 years after core decompression. Arthroscopy 2006;22:866–71 [DOI] [PubMed] [Google Scholar]
- 7.Varenna M, Sinigaglia L, Binelli L, et al. Transient osteoporosis of the hip: a densitometric study. Clin Rheumatol 1996;15:169–73 [DOI] [PubMed] [Google Scholar]
- 8.Ringe JD, Dorst A, Faber H. Effective and rapid treatment of painful localized transient osteoporosis (bone marrow edema) with intravenous ibandronate. Osteoporos Int 2005;16:2063–8 [DOI] [PubMed] [Google Scholar]
- 9.Samdani A, Lachmann E, Nagler W. Transient osteoporosis of the hip during pregnancy: a case report. Am J Phys Med Rehabil 1998;77:153–6 [PubMed] [Google Scholar]
- 10.La Montagna G, Malesci D, Tirri R, et al. Successful neridronate therapy in transient osteoporosis of the hip. Clin Rheumatol 2005;24:67–9 [DOI] [PubMed] [Google Scholar]
- 11.French AE, Kaplan N, Lishner M, et al. Taking bisphosphonates during pregnancy. Can Fam Physician 2003;49:1281–2 [PMC free article] [PubMed] [Google Scholar]
- 12.Dieme C, Dansokho A, Sane A. Transient osteoporosis of the hip in pregnancy complicated by spontaneous bilateral femoral neck fracture. J Orthopaedics 2006;3:e14 [Google Scholar]
- 13.Plenk H, Jr, Hofmann S, Eschberger J, et al. Histomorphology and bone morphometry of the bone marrow edema syndrome of the hip. Clin Orthop Relat Res 1997;73–84 [PubMed] [Google Scholar]
- 14.Lequesne M. Transient osteoporosis of the hip. A nontraumatic variety of Südeck's atrophy. Ann Rheum Dis 1968;27:463–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mailis A, Inman R, Pham D. Transient migratory osteoporosis: a variant of reflex sympathetic dystrophy? Report of 3 cases and literature review. J Rheumatol 1992;19:758–64 [PubMed] [Google Scholar]
- 16.Stanton-Hicks M, Jänig W, Hassenbusch S, et al. Reflex sympathetic dystrophy: changing concepts and taxonomy. Pain 1995;63:127–33 [DOI] [PubMed] [Google Scholar]


