Summary
Peripheral anterior inferior cerebellar artery (AICA) aneurysms are rare, accounting for less than 1% of all cerebral aneurysms. To our knowledge 34 flow-related cases including the present study have been reported in the literature.
Three patients harbouring four flow dependent aneurysms were referred to our institution. Two patients presented with subarachnoid hemorrhage, one presented with cerebellar manifestations. They were all treated by endovascular embolization of the aneurysm as well as the parent artery using liquid embolic material. Two cases were embolized using NBCA, Onyx was used in the third case.
No bleeding or rebleeding were encountered during the follow-up period which ranged from five to nine months.
One patient developed facial palsy, cerebellar symptoms and sensorineural hearing loss. The remaining two cases did not develop any post treatment neurological complications.
Endovascular management of flow-dependent AICA aneurysms by parent artery occlusion is feasible and efficient in terms of rebleeding prevention.
Post embolization neurological complications are unpredictable. This depends upon the adequacy of collaterals from other cerebellar arteries.
Key words: posterior fossa aneurysms, flow dependent aneurysms, AICA aneurysms
Introduction
Peripheral anterior inferior cerebellar artery (AICA) aneurysms are rare, accounting for less than 1% of all cerebral aneurysms 1. Patients with peripherally located AICA aneurysms may present with cerebellopontine angle mass effect or more commonly with subarachnoid haemorrhage. Flow dependent aneurysms are present in 2.8-9.3% of all cerebral arteriovenous malformations (AVMs) 2,3. Few cases of AICA flow-dependent aneurysms have been treated and were often described as case reports. The aim of this study was to evaluate the clinical presentation, outcome and endovascular technique of treatment by aneurysm embolization and parent artery occlusion using liquid embolic material in three cases harbouring four peripherally located AICA aneurysms. We also review the pertinent literature.
Anatomy of the AICA
The AICA is divided into four segments: the anterior pontine, the lateral pontine, the floculopeduncular and the cortical segments. The lateral pontine segment which begins at the anterolateral margin of the pons is subdivided into three sub-segments the pre-meatal, meatal and post-meatal according to the relation with the porus of the internal auditory meatus. The third segment is the floculopeduncular segment where it reaches the middle cerebellar peduncle and cerebello-pontine fissure. The cortical segment supplies the petrosal surface of the cerebellum 4.
Case 1
Presentation
A 48-year-old man patient presented with cerebellar manifestations and headache. CT and MRI showed RT cerebellar AVM with a hyperdense dilated venous channel seen at the left outer aspect of the pons (Figure 1C).
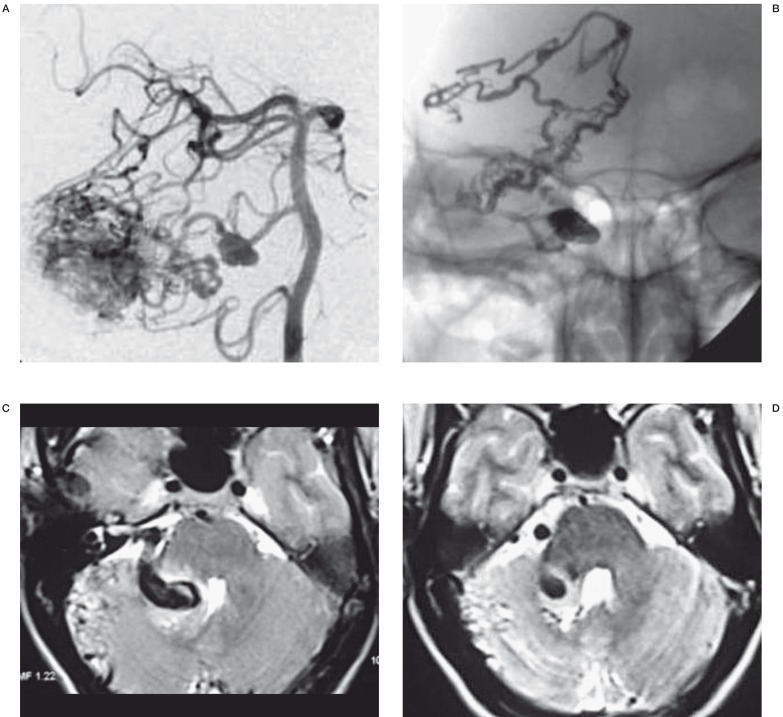
Figure 1.
A) Oblique view angiography shows an AICA aneurysm proximal to a cerebellar AVM. B) The Onyx cast fills the aneurysm sac and part of the AVM. C) Pre-treatment MRI T2-weighted image shows the compressing effect of the venous channel over the fourth ventricle. D) MRI T2-weighted image 6 months post-embolization shows the relative improvement of the fourth ventricle compression.
Treatment
All procedures were done under general anaesthesia and systemic heparinisation with (ACT) monitoring targeting a range between 250-300 seconds. Low molecular weight heparin was continued for 24 hours at 40 mg every 12 hours. A 6 French Envoy catheter (Cordis, Miami, FL) was used as guiding catheter. Vertebral angiography showed a RT AICA aneurysm in the premeatal segment proximal to the cerebellar AVM (Figure 1A). A Marathon microcatheter (ev3 Neurovascular, Irvine, CA, USA) was used to catheterise the AICA. Multiple views were taken to identify the aneurysm segment, its size and the presence of an identifiable neck. The tip of the microcatheter was navigated to the aneurysm sac. One cc of Onyx (ev3 Neurovascular, Irvine, CA, USA) was injected achieving complete exclusion of the sac. A small part of the AVM nidus was embolized in this session. No neurological complications were encountered.
Case 2
Presentation
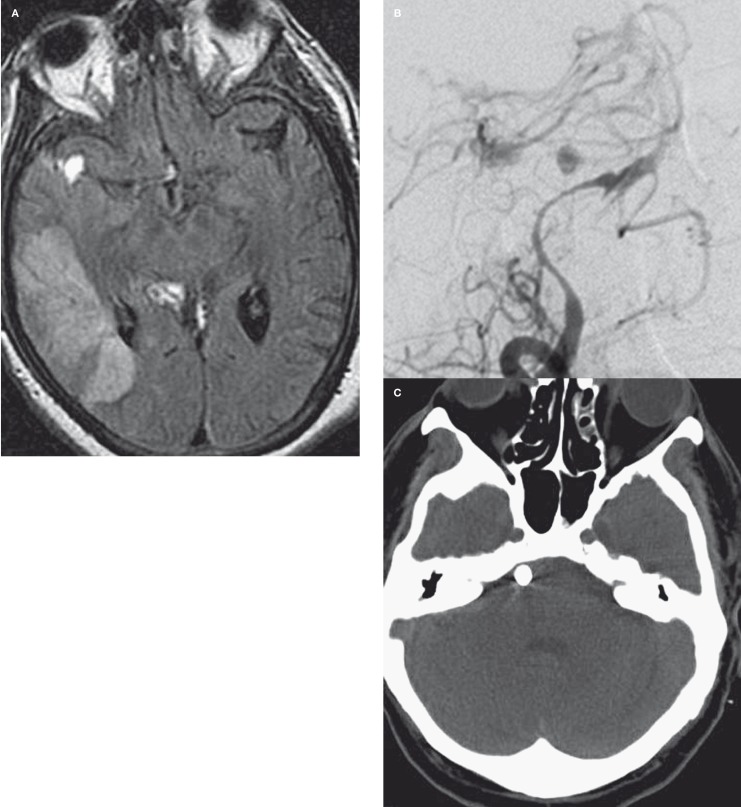
A 52-year-old man was referred to our institute with left side hemiplegia, dysphasia and disturbed level of consciousness a few days following a bout of severe headache. CT and MRI showed subarachnoid haemorrhage at the right cerebellopontine angle, right sylvian fissure with intra-ventricular extension. This was associated with a large right temporo-parieto-occipital infarction (Figure 2A).
Treatment
Vertebral angiography revealed a peripheral AICA aneurysm located at the pre-meatal segment measuring 6 mm in maximum diameter proximal to an associated AVM. Severe vasospasm was noted, indicating that probably he had bled few days before admission and presented when vasospasm and subsequent parieto-occipital infarction manifestations appeared (Figure 2B).
One mg (5 cc) of nimodipine diluted over 15cc normal saline was injected slowly in the guiding catheter over ten minutes. Continuous infusion of 2 mg nimodipine diluted over 1liter of the guiding catheter flush system was maintained throughout the procedure. An Excelsior SL 10 (Boston Scientific, Fremont, CA, USA) was used to catheterize the AICA. The aneurysm sac, the parent artery and the AVM nidus were embolized using n-butyl-cyanoacrylate (NBCA) - Lipiodol (Guerbet, Aulnay-sous-Bois, France) mixture at a concentration of 33%. No procedure-related complications were encountered.
Figure 2.
A) MRI Flair image shows subarachnoid blood in the sylvian fissure with associated temporo-parieto-occipital infarction. B) Conventional angiography oblique view shows severe vasospasm in the whole posterior circulation. C) Post embolization CT shows the aneurysm sac filled with embolising cast.
Case 3
Presentation
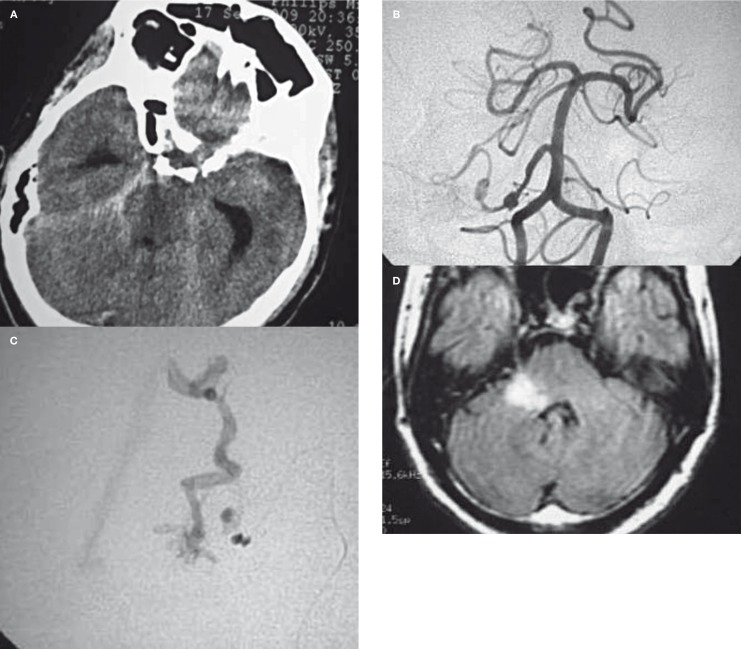
A 58-year-old man presented with disturbed loss of consciousness. CT scan revealed right cerebellar haematoma and subarachnoid haemorrhage. The following day, his consciousness level improved but was still confused. Two days later he became more confused and sleepy. CT scan confirmed subarachnoid re-bleeding with intra-ventricular extension. At this stage he was referred to our institute.
Treatment
Vertebral angiography revealed two AICA aneurysms located at the premeatal segment measuring 7 and 9 mm in maximum diameter proximal to a cerebellar AVM (Figure 3B,C). There was an associated right occipital AVM supplied by the left posterior cerebral artery. The RT AICA was catheterised using a Marathon microcatheter (ev3 Neurovascular, Irvine, CA, USA). The tip of the catheter was placed just proximal to the aneurysms, 33% of NBCA- lipiodol (Guerbet, Aulnay-sous-Bois, France) mixture was used to embolize both aneurysms and the parent artery. The AVM nidus was not embolized.
Complications
The patient recovered with sensorineural hearing loss, facial palsy and cerebellar symptoms.
Figure 3.
A) CT shows subarachnoid hemorrhage at the prepontine cistern. B) Early arterial phase angiography shows 2 AICA aneurysms. C) Selective microcatheter angiography shows the aneurysms proximal to the infratentorial AVM. D) MRI Flair image shows infarction at the brachium pontis.
Results
All four aneurysmal sacs were filled with embolizing material whether NBCA or Onyx. Control angiogram showed no more filling of any of the four treated aneurysms with delayed filling of the parent artery. All aneurysms were located in the pre-meatal segment. Follow-up angiogram was done in case 1 four months later and showed complete obliteration of the aneurysm.
He has been treated by a second session dedicated for AVM embolization using onyx and has been referred later on for radiosurgery. MRA examination was done for case 3 one month later showing no filling of aneurysms with occlusion of the AICA near its origin. He has been referred for radiosurgery as well. No angiographic control was done for case 2. None of the aneurysms bled after treatment during the follow-up period which was nine months in case 1 and five months in cases 2 and 3.
The third case developed facial palsy and sensorineural hearing loss proved by audiometry. The patient also complained of vertigo and cerebellar ataxia. MRI examination revealed right side cerebellar infarction at the petrous surface, brachium pontis and cerebellopontine angle region (Figure 3D).
The cerebellar symptoms markedly improved during the follow-up period yet the facial palsy and hearing loss persisted. The first two cases did not develop any neurological consequences post endovascular treatment. To demonstrate total exclusion of the AVM in case 2, control angiogram was proposed, however the patient refused.
Discussion
Aneurysms of the posterior fossa account for 8-12% of all cerebral aneurysms 5,6. The AICA is the least of the cerebellar arteries that may develop an aneurysm 7.
The aetiology of flow-dependent aneurysms is thought to be directly related to the presence of a high flow AVM distally exerting hemodynamic stress on the arterial wall.
Redekop et al. classified aneurysms associated with AVMs into intranidal, flow-related and unrelated aneurysms. They raised the point whether intranidal aneurysms and flow-related aneurysms are true aneurysms or just pseudo aneurysms that develop after bleeding from a fragile arterial wall 8. Lacking an identifiable neck, selective treatment of this aneurysm group with preservation of the parent artery is not always possible. Also coiling of such aneurysm whose nature is not properly understood may increase the perforation risk.
Most peripherally located AICA aneurysms often present with subarachnoid haemorrhage and hence urgent intervention is needed 9. The aim of our treatment was to secure the aneurysm (s) bothy in the ruptured or the non ruptured cases by filling the aneurysm sac with liquid embolic material then trying to embolize part or the whole AVM nidus in the same injection whenever possible. This technique succeeded in embolizing all aneurysms which appeared full of embolizing cast in the control CT scan. In case 3 the striking fact was the presence of two AVMs in the left cerebellar region supplied by the AICA and the left occipital region supplied by the left posterior cerebral artery (PCA). This was probably part of Rendu Osler Weber disease as the patient gave a history of recurrent epistaxis. We think that continuous angiographic follow-up will not be of value in assessing treatment stability as aneurysm re-canalisation after filling of the sac with liquid embolic agent and parent artery occlusion is unlikely to occur.
From 144 aneurysms we found reported in the English literature located in the AICA 37 aneurysms in 34 patients (including ours) were associated with vascular lesions (25%) (Table 1). There were 32 cases associated with AVM, one with dural fistula and one with hemangioblastoma. The initial presentation was identified in 33/34 cases. SAH was the main presentation, from 30 cases that presented with bleeding (91%), 28 presented with SAH (85%). The remainder presented with cerebellar symptoms, headache and tinnitus.
Table 1.
Reported cases of AICA aneurysms associated with vascular lesions.
| Author | Age | Sex | Symptoms and signs | Location | Max diameter in mm |
Number | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| Gacs 1 9 | 59 | F | SAH, slight cerebellar signs | Meatal | 3 | 1 | Aneurysm resection | Good, mild residual symptoms |
| Gacs 2 9 | 28 | F | Diplopia for one year, SAH, cerebellar and medullary signs |
Meatal | 4 | 1 | Aneurysm and AVM resection |
Satisfactory, significant symptoms improvement |
| Kikuchi 10 | 45 | M | Left facial pain, history of SAH 15 years ago |
Meatal | 4 | 1 | Surgery | Uneventful |
| Menovsky 1 11 | 52 | F | SAH | Pre-meatal | 15 | 1 | Wrapping | Uneventful, re-bleeding 5 years later |
| Menovsky 2 11 | 17 | F | Right side cerebellar & IVH | Meatal | 20 | 1 | Aneurysm clipping & AVM resection |
No neurological deficit |
| Nishi 12 | 45 | M | SAH | Pre-meatal | 7 | 1 | Parent artery occlusion | Death 2 weeks after AVM rupture. No deficits |
| Akyuz 13 | 52 | M | SAH, cerebellar symptoms | 2 pre-meatal 1 meatal | 4,5,6 | 3 | Trial for clipping | Persistent dizziness |
| Peluso 1 14 | 44 | F | SAH & IVH, facial palsy and hearing loss |
Pre-meatal | NA | 1 | Coil occlusion of the aneurysm Gamma Knife later on for the AVM |
Infarction of the brachium pontis, persistent facial palsy and hearing loss |
| Peluso 2 11 | 57 | M | SAH & IVH | Pre-meatal | NA | 1 | Coil occlusion of the aneurysm and Gamma Knife later for the AVM |
No infarction on MRI independent |
| Gonzales 1 1 | 54 | M | SAH and IPH | Meatal or cortical (Distal segment) |
NA | 1 | Clipping & AVM resection | Unchanged GOS 2 |
| Gonzales 2 1 | 46 | F | SAH &IVH | Pre-meatal | NA | 1 | Clipping & AVM resection | Unchanged GOS 3 |
| Gonzales 3 1 | 24 | F | SAH | Pre-meatal | NA | 1 | Clipping & AVM resection | Unchanged GOS 3 |
| Gonzales 4 1 | 72 | F | SAH | (Meatal or cortical Distal segment |
NA | 1 | Clipping & AVM resection | Unchanged GOS 3 |
| Lubicz 15 | 62 | F | SAH | NA | NA | 1 | Parent artery occlusion | Facial nerve palsy |
| Seung Hwan Lee 16 |
47 | M | SAH, RT cerebellar hematoma |
Cortical | 7 | 1 | Clipping and AVM resection | Uneventful |
| Kan 17 | 27 | M | Tinnitus Headache, meningismus, bilateral six nerve palsy |
Cortical | 3 | 1 | Surgical resection of the fistula |
Uneventful |
| Saito 18 | 31 | F | SAH | Cortical | 5 | 1 | Clipping of the aneurysm and AVM resection |
Uneventful |
| Drake 1 19 | NA | NA | SAH | NA | NA | NA | Clipping and AVM removal |
Poor |
| Drake 2 19 | NA | NA | SAH | NA | NA | NA | Clipping and AVM removal |
Good |
| Drake 3 19 | NA | NA | SAH | NA | NA | NA | Inoperable AVM, aneurysm clipping |
Post-operative bleeding and hemiparesis |
| Drake 4 19 | NA | NA | SAH | NA | NA | NA | Inoperable AVM, aneurysm clipping |
Post-operative bleeding and death |
| Binggeli 20 | 58 | M | SAH | Rostral AICA duplicate |
4 | 1 | Inoperable AVM, aneurysm clipping |
Good |
| Mourier 21 | 50 | M | SAH | NA | NA | NA | Aneurysm clipping |
Good |
| Deruty 22 | 39 | M | Cerebellar bleeding | Meatal | NA | NA | AVM embolization and aneurysm clipping |
Good |
| Kaech 23 | 44 | M | SAH and cerebellar hematoma |
Meatal | 10 | 1 | Aneurysm clipping and AVM partial embolization |
Good |
| Lee 24 | 55 | M | SAH | Meatal | 2.5 | 1 | Surgical trapping of the meatal loop |
Uneventful |
| Li 25 | 35 | M | SAH, IPH | Post-meatal | 12 | 1 | Clipping of the artery, dissection of the aneurysm and the AVM |
No post operative neurologic complication |
| Suh 26 | 41 | M | Incidental | Pre-meatal | 9 | 1 | Coiling with artery preservation |
Good, mRS 1 |
| Vincentelli 27 | 35 | F | SAH | 1 | Aneurysm clipping and AVM resection |
Uneventful | ||
| DeAguiar 28 | 58 | M | SAH, IVH | Pre- meatal | 4 | 1 | Endovascular treatment (non specified) for the aneurysm, AVM resection |
Uneventful |
| Redekop 29 | NA | NA | NA | NA | NA | 1 | NA | NA |
| Mahmoud 1 | 48 | M | Cerebellar ataxia and headache |
Pre-meatal | 14 | 1 | Endovascular Parent artery occlusion |
Uneventful |
| Mahmoud 2 | 52 | M | SAH & IV hemorrhage | Pre-meatal | 6 | 1 | Endovascular Parent artery occlusion |
Uneventful |
| Mahmoud 3 | 58 | M | SAH, cerebellar hematoma & IV extension |
Pre-meatal, Pre-meatal |
7, 9 |
2 | Endovascular Parent artery occlusion |
Cerebellar infarction, VII & VIII cranial nerve palsy |
Patients' demographics, presentation, aneurysm size, location, treatment and outcome are summarised in Table 1.
Parent artery occlusion was performed in eight patients: five by injecting embolizing material and two by coils. One patient has been treated by coiling and artery preservation.
Four complications (including ours) were reported after parent artery occlusion. One death occurred after AVM rupture this was linked to hemodynamic disturbance occurring post embolization with EVAL mixture 10. One patient had facial palsy, two had facial palsy and sensorineural hearing loss.
Surgery for distal AICA aneurysms is challenging as cranial nerve affection may follow surgery despite anatomical preservation due to vascular injury 11.
According to Bambakidis et al., location near to the skull base and proximity to multiple cranial nerves are the main difficulties in AICA surgery 12. Nader et al. believed that the risks and morbidity associated with AICA surgery make microsurgical clipping a less favourable option than endovascular intervention 13.
Occlusion of the AICA is unpredictable and may result in neurological manifestations including vertigo, nystagmus, cerebellar symptoms, nausea and vomiting. Other neurological manifestations may include ipsilateral loss of pain and temperature sensation on the face and corneal hypoesthesia, Horner syndrome, cerebellar ataxia, asynergia and incomplete loss of pain and temperature sensation on the contralateral half of the body. These manifestations are inversely proportional to the adequacy of the collateral circulation supplied by the posterior inferior cerebellar artery (PICA) and the superior cerebellar artery (SCA) 4. Ophthalmoplegia, quadriplegia, coma and death may also follow AICA occlusion according to Bambakidis et al. 13.
Vestibulocochlear nerve affection is the result of internal auditory artery occlusion so occlusion of the AICA proximal to the internal auditory meatus level will probably increase the risk of facial palsy and sensorineural hearing loss. We are aware that the technique described is not new but to our knowledge this is the first article gathering all aneurysms of this entity and summarizing the methods of treatment, aneurysm demographics and procedure-related complications.
Conclusion
Endovascular management of flow-dependent AICA aneurysms by parent artery occlusion is feasible and efficient in terms of re-bleeding prevention. Post-embolization neurological complications are unpredictable and depend on the site of occlusion and the adequacy of collaterals from other cerebellar arteries.
References
- 1.Gonzales LF, Alexander MJ, McDougall CG, et al. Anterior inferior cerebellar artery aneurysms surgical approaches and outcomes a review of 34 cases. Neurosurgery. 2004;55:1025–1035. doi: 10.1227/01.neu.0000141083.00866.82. [DOI] [PubMed] [Google Scholar]
- 2.Cronqvist S, Troupp H. Intracranial arteriovenous malformation and arterial aneurysm in the same patient. Acta Neurol Scand. 1966;2:307–316. doi: 10.1111/j.1600-0404.1966.tb01185.x. [DOI] [PubMed] [Google Scholar]
- 3.Rohde V, Spangenberg P, Mayfrank L, et al. Advanced neuronavigation in skull base tumors and vascular lesions. Minim Invasive Neurosurg. 2005;43:13–18. doi: 10.1055/s-2004-830179. [DOI] [PubMed] [Google Scholar]
- 4.Rhoton AL Jr. The posterior cranial fossa: microsurgical anatomy and surgical approaches. Neurosurgery. 2000;47:S5–S6. doi: 10.1097/00006123-200105000-00064. [DOI] [PubMed] [Google Scholar]
- 5.Duvoisin RC, Yahr MD. Posterior fossa aneurysms. Neurology. 1965;15:231–241. doi: 10.1212/wnl.15.3.231. [DOI] [PubMed] [Google Scholar]
- 6.Weibel J, Fields WS, Campos RJ. Aneurysms of the posterior cervicocranial circulation: clinical and angiographic considerations. J Neurosurg. 1967;26:223–234. doi: 10.3171/jns.1967.26.2.0223. [DOI] [PubMed] [Google Scholar]
- 7.Mizushima H, Kobayashi N, Yoshiharu S, et al. Aneurysm of the distal anterior inferior cerebellar artery at the medial branch: a case report and review of the literature. Surg Neurol. 1999;52:137–142. doi: 10.1016/s0090-3019(99)00042-7. [DOI] [PubMed] [Google Scholar]
- 8.Redekop G, TerBrugge K, Montanera W, et al. Arterial aneurysms associated with cerebral arteriovenous malformations: classification, incidence, and risk of hemorrhage. J Neurosurg. 1998;89:539–546. doi: 10.3171/jns.1998.89.4.0539. [DOI] [PubMed] [Google Scholar]
- 9.Yamakawa H, Hattori T, Tanigawara T, et al. Intracanalicular aneurysm at the meatal loop of the distal anterior inferior cerebellar artery: a case report and review of the literature. Surg Neurol. 2004;61:82–88. doi: 10.1016/s0090-3019(03)00270-2. [DOI] [PubMed] [Google Scholar]
- 10.Nishi S, Taki W, Nakahara I, et al. Embolization of cerebral aneurysms with a liquid embolus, EVAL mixture: Report of three cases. Acta Neurochirur (Wein) 1996;138:294–300. doi: 10.1007/BF01411740. [DOI] [PubMed] [Google Scholar]
- 11.Andaluz N, Pensak ML, Zuccarello M. Multiple, peripheral aneurysms of the anterior inferior cerebellar artery. Acta Neurochir (Wien) 2005;147:419–422. doi: 10.1007/s00701-004-0453-7. [DOI] [PubMed] [Google Scholar]
- 12.Bambakidis NC, Manjila S, Dashti S, et al. Management of anterior inferior cerebellar artery aneurysms: an illustrative case and review of literature. Neurosurg Focus. 2009;26:E6. doi: 10.3171/2009.1.FOCUS0915. [DOI] [PubMed] [Google Scholar]
- 13.Nader S, Phiroz T, Albert CL, et al. The current role of microsurgery for posterior circulation aneurysms: a selective approach in the endovascular era. Neurosurgery. 2008;62:1236–1253. doi: 10.1227/01.neu.0000333295.59738.de. [DOI] [PubMed] [Google Scholar]
- 14.Gacs G, Viñuela F, Fox AJ, et al. Peripheral aneurysm of the cerebellar arteries. Review of 16 cases. J Neurosurg. 1983;58:63–68. doi: 10.3171/jns.1983.58.1.0063. [DOI] [PubMed] [Google Scholar]
- 15.Kikuchi K, Kamisato N, Sasanuma J, et al. Trigeminal neuralgia associated with posterior fossa arterio-venous malformation and aneurysm fed by the same artery. Case report. Neurol Med Chir (Tokyo) 1990;30:918–921. doi: 10.2176/nmc.30.918. [DOI] [PubMed] [Google Scholar]
- 16.Menovsky T, Grotenhuis AJ, Bartels RH. Aneurysm of the anterior inferior cerebellar artery (AICA) associated with high-flow lesion: report of two cases and review of the literature. J Clin Neurosci. 2002;9:207–211. doi: 10.1054/jocn.2001.0945. [DOI] [PubMed] [Google Scholar]
- 17.Akyuz M, Tuncer R. Multiple anterior inferior cerebellar artery aneurysms associated with an arterio-venous malformation case report. Surg Neurol. 2005;64:S106–S108. doi: 10.1016/j.surneu.2005.07.037. [DOI] [PubMed] [Google Scholar]
- 18.Peluso PP, van Rooij WJ, Sluzewski M, et al. Distal aneurysms of cerebellar arteries: incidence, clinical presentation, and outcome of endovascular parent vessel occlusion. Am J Neuroradiol. 2007;28:1573–1578. doi: 10.3174/ajnr.A0607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lubicz B, Leclerc X, Gauvrit JY, et al. Endovascular treatment of peripheral cerebellar artery aneurysms. . Am J Neuroradiol. 2003;24:1208–1213. [PMC free article] [PubMed] [Google Scholar]
- 20.Lee SH, Koh SJ, Bang JS, et al. Case of ruptured peripheral aneurysm of the anterior inferior cerebellar artery associated with an arteriovenous malformation: a less invasive image-guided transcortical approach. J Korean Neurosurg Soc. 2009;46:577–580. doi: 10.3340/jkns.2009.46.6.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kan P, Stevens EA, Warner J, et al. Resolution of an anterior inferior cerebellar artery feeding aneurysm with the treatment of a transverse-sigmoid dural fistula. Skull Base. 2007;17:205–210. doi: 10.1055/s-2007-970559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saito A, Nishino A, Suzuki I, et al. Subarachnoid hemorrhage caused by rupture of a distal anterior inferior cerebellar artery aneurysm: three case reports. Neurol Med Chir (Tokyo) 2008;48:506–511. doi: 10.2176/nmc.48.506. [DOI] [PubMed] [Google Scholar]
- 23.Drake CG, Friedman AH, Peerless SJ. Posterior fossa arterio-venous malformations. J Neurosurg. 1986;64:1–10. doi: 10.3171/jns.1986.64.1.0001. [DOI] [PubMed] [Google Scholar]
- 24.Binggeli RS, Schroth G, Steiger H-J. Distal aneurysm of the rostral duplicate anterior inferior cerebellar artery feeding an associated dural arteriovenous malformation: case report and review of the literature. J Clin Neurosci. 1998;5:237–244. doi: 10.1016/s0967-5868(98)90049-2. [DOI] [PubMed] [Google Scholar]
- 25.Mourier KL, Gelbert F, Assouline E, et al. MRI in multiple vascular lesions: identification of the ruptured malformation. Acta Neurochir (Wien) 1991;112:83–87. doi: 10.1007/BF01405131. [DOI] [PubMed] [Google Scholar]
- 26.Deruty R, Mottolese C, Soustiel JF, et al. Association of cerebral arteriovenous malformation and cerebral aneurysm. Diagnosis and management. Acta Neurochir (Wien) 1990;107:133–139. doi: 10.1007/BF01405792. [DOI] [PubMed] [Google Scholar]
- 27.Kaech D, de Tribolet N, Lasjaunias P. Anterior inferiorcerebellar artery aneurysm, carotid bifurcation aneurysm, and dural arterio-venous malformation of the tentorium in the same patient. Neurosurgery. 1987;21:575–582. doi: 10.1227/00006123-198710000-00027. [DOI] [PubMed] [Google Scholar]
- 28.Lee SJ, Koh JS, Ryu CW, et al. Ruptured intrameatal aneurysm of the anterior inferior cerebellar artery accompanying an arteriovenous malformation: a case report. Cerebellum. 2012 Jan 5; doi: 10.1007/s12311-011-0349-z. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 29.Li X, Zhang D, Zhao J. Anterior inferior cerebellar artery aneurysms: six cases and a review of the literature. Neurosurg Rev. 2012;35:111–119. doi: 10.1007/s10143-011-0338-1. [DOI] [PubMed] [Google Scholar]
- 30.Suh SH, Kim DJ, Kim DI, et al. Management of anterior inferior cerebellar artery aneurysms: endovascular treatment and clinical outcome. Am J Neuroradiol. 2011;32:159–164. doi: 10.3174/ajnr.A2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vincentelli F, Caruso G, Licastro G, et al. Association between an aneurysm of the anterior inferior cerebral artery and an arteriovenous malformation fed by the same artery. J Neurosurg Sci. 1998;42:41–45. [PubMed] [Google Scholar]
- 32.De Aguiar GB, Veiga JCE, Feres FJO, et al. Association between a ruptured distal anterior inferior cerebral artery aneurysm and arteriovenous malformation fed by the same artery. Arq Neuropsiquiatr. 2011;69:989–990. doi: 10.1590/s0004-282x2011000700027. [DOI] [PubMed] [Google Scholar]