Abstract
Objective:
Patient expectations are related to treatment outcome across a broad variety of patient conditions. Here we sought to examine factors associated with the expectation of complete relief from treatment for spinal pain.
Design:
Secondary analysis of data pooled from two randomized controlled trials of conservative rehabilitation interventions.
Patients:
252 patients (103 men, 149 women) with neck (n=140) or back (n=112) pain.
Methods:
We used logistic regression model with backward elimination to test which patient clinical or demographic factors were most related to the expectation of complete relief.
Main Outcome Measures:
The expectation of complete recovery, which was collected at the baseline examination visit in the primary trials.
Results:
The final model examining the contributions of patient and clinical characteristics to the expectation of complete relief included two significant interactions. First, increasing disability was associated with increased odds of expecting complete recovery in women while there was very little change for men across levels of disability (OR 0.9 [95%CI 0.8, 0.9]). Second, patients with low fear and a sudden onset of pain had higher odds of expecting recovery than patients with a gradual onset of pain (OR 0.7 [95%CI 0.5, 0.97]). A main effect for education level of the patient was also significant with better odds for expecting complete recovery for college educated patients compared to those with graduate school education (OR 5.0 [95%CI 1.9, 13.4]).
Conclusion:
The results should assist physical therapists to recognize patients who may have lower expectations of recovery and plan pre-treatment education interventions.
INTRODUCTION
Successive studies have indicated that patient expectations play a role in the outcomes of many treatments. These findings have been demonstrated across a wide variety of conditions such as: diabetes (Hayes and Naegeli, 2010); overactive bladder (Marschall-Kehrel, Roberts, and Brubaker, 2006); HIV (Rhodes, Bernays, and Terzic, 2009); and spinal pain (Bishop, Bialosky, and Cleland, 2011; Bishop, Mintken, Bialosky, and Cleland, 2013). Of specific interest in this current paper is what Thompson and Sunol (1995) have defined as ‘predicted’ expectations, which relate to anticipated outcomes. Previously we examined the influence of such a predicted expectation after manual interventions for spinal disorders (Bishop, Bialosky, and Cleland, 2011; Bishop, Mintken, Bialosky, and Cleland, 2013). Findings from those studies suggested that if a patient expects complete relief of symptoms from treatment for spinal pain, that patient has better long-term outcomes from that treatment both in self-ratings of disability and global ratings of change (GROC).
These findings are similar to other studies of expectations and associations with outcomes in patients with spinal pain. For example, Palmlöf, Holm, Alfredsson, and Skillgate (2016) asked patients receiving manual therapy interventions for neck pain ‘How likely is it, according to your judgment, that you are completely recovered from your neck problems in 7 weeks’. Expectations were categorized as low, medium and high. These authors found that men and women with high expectations had an increased probability (compared to low expectations) of rating themselves to be improved at follow up. Similarly, Kongsted et al. (2014) asked patients seeking care for back pain from a general medical practitioner or chiropractic physician how likely he or she was to be recovered at 3-months. Again patients with higher expectations were more likely to perceive themselves to be improved. There were also associations between expectations and reported pain intensity at follow up in this study.
These results are supported by systematic reviews of the association between expectation of recovery and other outcomes in patients with low back pain. Iles, Davidson, Taylor, and O’Halloran (2009) reviewed 10 studies and reported that expectation of recovery was associated with activity-based outcome. These authors recommended that expectations for recovery be measured early in the treatment plan. Additionally, another systematic review indicated that negative expectations for recovery were associated with lower rates of return to work after treatment for low back pain (Iles, Davidson, and Taylor, 2008).
Therefore, expectation is an important, and potentially modifiable, moderator of outcome for individuals presenting with spinal pain. Expectations are unique to the individual and context of treatment, and are developed by both past personal experiences and the experiences of family members and acquaintances (Thompson and Sunol, 1995). Patient expectations are also influenced by a range of individual characteristics: 1) demographic factors (sex) (Gepstein, Arinzon, Adunsky, and Folman, 2006; Goldstein, Morgenstern, Hurwitz, and Yu, 2002; Ozegovic, Carroll, and David, 2009); (education level) (Gepstein, Arinzon, Adunsky, and Folman, 2006; Ozegovic, Carroll, and David, 2009); (age) (Gepstein, Arinzon, Adunsky, and Folman, 2006; Goldstein, Morgenstern, Hurwitz, and Yu, 2002); and (race) (Goldstein, Morgenstern, Hurwitz, and Yu, 2002); and 2) psychological factors (fear) (Goossens et al, 2005); and depression (Goossens et al, 2005; Ozegovic, Carroll, and David, 2009).
Our purpose was to examine patient related factors to determine the extent to which these factors influenced the expectations for benefit from interventions provided by a physical therapist. Specifically we examined the expectation of complete relief that was identified in our previous studies as a strong determinant of long-term outcome after treatment. Understanding factors that influence patient expectations is important and likely to be an integral part of developing meaningful treatment plans that include the patient in the decision making process.
METHODS
In this study we performed a secondary analysis of data combined from two randomized controlled clinical trials comparing interventions for patients with: 1) neck pain (NCT00504686) (Cleland et al, 2010); and 2) interventions for patients with low back pain (NCT00257998) (Cleland et al, 2009). Combining these studies was appropriate for this current analysis as both studies used the same data collection forms and procedures. Patients in both trials who consented to participate completed a series of surveys at the initial visit, and prior to randomization to interventions, including demographic data, measures of pain, disability and mood. In addition, patients completed a survey regarding general expectations for benefit from participating in treatment by a physical therapist. These measures are outlined below.
Participants
The study of interventions for neck pain enrolled 140 patients with a primary report of neck pain seen in 1 of 5 physical therapy clinics located in 4 different states across the United States (New Hampshire, Wisconsin, Colorado, Massachusetts). Patients were eligible to participate in the primary study if they were between 18 and 60 years of age, had a primary report of neck pain with or without unilateral upper-extremity symptoms, and had a Neck Disability Index (NDI) score of at least 20%. Patients were excluded if they had any of the following: serious pathologies; diagnosis of cervical spinal stenosis; bilateral upper-extremity symptoms; evidence of central nervous system involvement; neurologic signs consistent with nerve root compression; or inability to adhere to the treatment and follow-up schedule. Interventions studied in this trial were a thoracic spine focused manipulation and range of motion exercises.
In the second trial, 112 patients seeking care for LBP (with or without lower extremity symptoms) were recruited from outpatient physical therapy clinics affiliated with Concord Hospital, Concord, NH; Intermountain Healthcare, Salt Lake City, UT; and the University of Southern California, Los Angeles, CA. For patients to be eligible, they had to have a modified Oswestry Disability Questionnaire (ODQ) (Fritz and Irrgang, 2001) score of >25%, be between 18 and 60 years of age, and to be positive for the validated spinal manipulation clinical prediction rule (CPR) using the originally published criteria (Childs et al, 2004). Exclusion criteria included the presence of any red flags (i.e. tumor, metabolic diseases, RA, osteoporosis, and prolonged history of steroid use), signs consistent with nerve root compression. Other exclusion criteria included prior surgery to the lumbar spine and current pregnancy. Interventions in this study were lumbar spine focused joint manipulation or lumbar spine focused joint mobilization techniques. All patients provided informed consent prior to their enrollment in either of the studies and the primary pain and disability outcomes are reported elsewhere (Cleland et al, 2009; Cleland et al, 2010).
Demographic Characteristics
All patients completed demographic surveys including sex, age, marital status, educational background. In addition, current work status, and any workers compensation or ligation currently underway was collected (Table 1).
Table 1.
Characteristics of patients in the sample
| Median (Range) | |
|---|---|
| Pain Intensity | 5 (1, 8) |
| Duration (days) | 251 (2, 310) |
| Disability | 30 (20, 62) |
| Number of patients (%) | |
| Gender (female) | 118 (47) |
| Region of pain | |
| Cervical | 140 (55) |
| Lumbar | 112 (45) |
| Location of pain | |
| Spine only | 168 (67) |
| Proximal segment | 47 (19) |
| Distal segment | 33 (13) |
| Mode of onset | |
| Gradual | 122 (49) |
| Sudden | 90 (36) |
| Traumatic | 35 (14) |
| Prior treatments for spine pain | |
| None | 146 (58) |
| Surgery | 0 (0) |
| PT | 6 (2) |
| Medication | 79 (32) |
| Chiropractic | 5 (2) |
| Massage therapy | 5 (2) |
| Not indicated | 10 (4) |
| Level of education | |
| Less than High school | 6 (2) |
| High school | 35 (14) |
| Some college | 54 (22) |
| Completed college | 49 (20) |
| Some graduate school | 55 (22) |
| Completed graduate school | 47 (19) |
| Not indicated | 5 (2) |
| Workers compensation | |
| Yes | 19 (8) |
Clinical Characteristics
Pain Experience
Both studies used an 11-point numeric rating scale (NRS) to quantify pain intensity at baseline. The scale is anchored on the left (score of 0) with the phrase “no pain” and on the right (score of 10) with the phrase “worst imaginable pain.” Participants were asked to rate the intensity of their current level of pain, as well as their worst and least amount of pain in the previous 24 hours. The average of the 3 ratings was used to represent the patient’s level of pain.
Information about the current pain experience was also collected. The location of symptoms was categorized into spinal pain only or spinal pain with radiation into the limb. Any concomitant peripheral weakness was noted during the physical examination at the initial examination. Mechanism of injury was categorized as onset related to trauma, sudden onset without trauma or gradual onset. The duration of the current episode of pain problem was recorded in days. Patients were asked about other treatment (i.e. use and types of medication) for the current episode of pain.
Self-Reported Disability
Patients in this study completed one of two region-specific self-reported disability questionnaires. The Oswestry Disability Questionnaire (ODQ) is a condition-specific disability scale for patients with back pain that consists of 10 items including questions about pain and function, each scored from 0 to 5, with a maximum score of 50 points. The score is commonly reported as a percentage with higher scores indicating greater perceived disability (Fritz and Irrgang, 2001).
The Neck Disability Index (NDI) is a condition-specific disability scale for patients with neck pain that based on the ODQ and, therefore, scored and reported similarly. The NDI has been reported to be a reliable and valid outcome measure for patients with neck pain (Cleland, Childs, and Whitman, 2008; Cleland, Fritz, Whitman, and Palmer, 2006).
Fear Avoidance Beliefs Questionnaire
The FABQ was used to quantify a subject’s fear-avoidance beliefs about physical activity as well as the fear about work due to back pain (Waddell et al, 1993). The FABQ consists of work (FABQW, range: 0 to 42) and physical activity (FABQPA, FABQ-PA, range: 0 to 24) subscales, each of which has been shown to exhibit a high level of test-retest reliability (Jacob, Baras, Zeev, and Epstein, 2001).
Expectations
We were specifically interested in the general expectations for the effectiveness of a treatment plan provided by a physical therapist. Participants were not asked to consider any particular intervention but rather treatment by a physical therapist in general. These data were collected at the initial visit in both studies before specific intervention plans were developed. All patients were given a form with the question “What results do you expect from your treatment?” Of interest in this current study were responses to the item: ‘Complete relief from symptoms (pain, stiffness, swelling, numbness, weakness). Possible responses were ‘definitely yes’, ‘yes’, ‘not sure’, ‘no’ and ‘definitely no’ with ‘not sure’ the mid-point response. This questionnaire was developed specifically for the primary studies. Consequently, the psychometric properties of the question are unknown at this time.
Analysis
First, the patient responses regarding expectation were reduced to create a dichotomous variable with categories ‘definitely yes’ and ‘yes’ combined and ‘no’ and ‘definitely no’ combined. Those patients who responded ‘unsure’ were excluded from the tests of association. Next, we determined the univariate associations among the demographic and clinical characteristics and the expectation of the participants using independent t-tests and chi-squared analyses. Variables with associations (p < 0.1) were then used to build regression models to determine the strongest associations with expectation using logistic binary regression methods. Any continuous variables were checked for co-linearity. Continuous predictor variables were assessed for normalcy using histograms. Models were built using the generalized linear model function in IBM SPSS Statistics for Windows (Version 21.0. Armonk, NY: IBM Corp) by adding all main effects first. All possible two-way interactions were added in the next step. Non-significant interactions and main effects were removed in a backwards step-wise manner (p > 0.05 to remove) to build a parsimonious final model. Model fit was determined using area under the receiver operator curve calculated from the parsimonious model.
RESULTS
Description of Patients
The total sample consisted of 252 patients (103 men, 149 women) with neck (n = 140) or back (n = 112) pain. A summary of pertinent characteristics of these patients is shown in Table 1. Briefly, patients had experience pain for a median of 251 days and the pain intensity (average of current, best and worst) at the initial examination was 5 (out of 10 using the 11-point NRS). Self-reported disability at baseline across the sample was 31.9% (SD = 8.4). The majority of patients had pain localized to the spine with approximately 12% reporting radiation of symptoms in to the distal extremity (forearm or shank), and more people reported a gradual onset of symptoms. If patients had sought prior treatment for spine pain, the most common treatment was the prescription of medication (31%). The sample included in the analysis was 208 patients; 44 patients were excluded from the analysis because they stated they were ‘not sure’ about their expectation for treatment.
Demographic Relationships to Expectation
Univariate associations with the expectation of complete relief were identified for region of pain, mode of onset, gender, education level and the presence of peripheral weakness. See Table 2 for the associations between these variables and holding the expectation for complete relief. Patient age, self-reported disability and fear avoidance beliefs related to physical activity were associated with the expectation of complete relief. These associations are shown in Table 3. Fear and disability were significantly but modestly correlated with each other (r = 0.293, p < 0.001). Both of these continuous variables were included in the regression model.
Table 2.
Associations between. categorical variables for patients expecting complete recovery (yes) and those who do not (no).
| Yes | No | Chi-square | p-value | |
|---|---|---|---|---|
| Gender | 5.18 | 0.023 | ||
| Male | 80 (88) | 11 (12) | ||
| Female | 89 (75) | 29 (25) | ||
| Zone | 16.25 | <0.0001 | ||
| Cervical | 79 (71) | 33 (29) | ||
| Lumbar | 90 (93) | 7 (7) | ||
| Mode of onset | 14.19 | 0.001 | ||
| Gradual | 68 (72) | 27 (28) | ||
| Sudden | 75 (94) | 5 (6) | ||
| Traumatic | 25 (78) | 7 (22) | ||
| Limb weakness | 5.17 | 0.023 | ||
| Present | 40 (93) | 3 (7) | ||
| Absent | 129 (78) | 37 (22) | ||
| Education | 18.48 | <0.0001 | ||
| High School | 32 (94) | 2 (6) | ||
| College | 80 (89) | 10 (11) | ||
| Graduate School | 56 (67) | 28 (33) | ||
| Prior history | 0.08 | 0.781 | ||
| No | 81 (83) | 17 (17) | ||
| Yes | 88 (79) | 23 (21) |
Table 3.
Differences between patients expecting complete recovery (yes) and those who do not (no).
| Yes | No | p-value | |
|---|---|---|---|
| Disability* | 33.±8.2 | 28.9±8.7 | 0.006 |
| Fear Avoidance Beliefs, Physical Activity | 12.3±5.3 | 10.7±4.8 | 0.080 |
| Fear Avoidance Beliefs, Work | 11.3±7.7 | 12.7±7.6 | 0.318 |
| Pain Intensity | 4.8±1.4 | 4.5±1.4 | 0.329 |
| Days since onset | 56.8±48.9 | 59.1±55.3 | 0.814 |
| Age (years) | 39.8±10.9 | 43.8±12.2 | 0.068 |
Oswestry Disability Index or Neck Disability Index
Consequently, the full model started with region of pain, gender, educational level, peripheral weakness and mode of onset entered as categorical factors and fear, age and disability as continuous factors. Two-way interactions were built for each combination of variables and entered in to the model at the first step. Subsequent models were inspected and terms with p > 0.1 were removed from the model unless to do so would invalidate an interaction term.
The final parsimonious logistic model examining the contributions of patient and clinical characteristics to the expectation of complete relief is shown in Table 4. This model included two significant interactions. There was an interaction between gender and disability such that the probability of expecting completely recovery was greater for women than men at low levels of disability and was higher for men as disability increased. Figure 1 shows the graphs of the odds curves for men and women across levels of disability. For men, there was a very slight increase in odds as disability increased. For women the odds were low at low levels of disability and increased to be greater than those of women at levels of disability greater than 50%. Further decomposition indicated a modest but significant difference between men and women in average disability at baseline (men>women, mean difference 3.1, p = 0.004). Future studies are needed to further examine this hypothesis.
Table 4.
Odds ratios and confidence intervals for each level of variable predicting ‘high’ expectations.
| Odds ratio | 95% Confidence level | Sig. | |||
|---|---|---|---|---|---|
| Educational background | High School | 5.41 | 0.92 | 31.81 | .062 |
| College | 5.07 | 1.92 | 13.36 | .001 | |
| Graduate school | ref | ||||
| Mode of onset | Traumatic | 2.91 | 0.21 | 39.91 | .426 |
| Sudden | 360.80 | 6.30 | 20674.02 | .004 | |
| Gradual | ref | ||||
| Gender | Male | 225.89 | 5.74 | 8890.51 | .004 |
| Female | ref | ||||
| FABQ-PA | 1.09 | 0.96 | 1.54 | .102 | |
| Disability | 1.11 | 1.03 | 1.21 | .009 | |
| Traumatic onset * FABQ-PA | 0.89 | 0.69 | 1.14 | .350 | |
| Sudden onset * FABQ-PA | 0.67 | 0.46 | 0.97 | .018 | |
| Gradual onset * FABQ-PA | ref | ||||
| Male * Disability | 0.9 | 0.8 | 0.9 | .013 | |
| Female * Disability | ref | ||||
Ref: Reference category
FABQ-PA: Fear avoidance beliefs, physical activity
Figure 1.

Gender by Disability interaction expressed in odds.
A second interaction was significant between fear avoidance beliefs about physical activity and the mechanism of onset. In this interaction is shown in Figure 2. While the interaction terms indicate that this interaction generally reduced the odds of expecting complete recovery, those with sudden onset of pain had higher odds of expecting complete recovery at low levels of fear, which gradually decreased with increasing fear. The categorical main effects in both interaction terms had large estimates and confidence intervals suggesting instability in these estimates for higher values of the continuous predictors.
Figure 2.
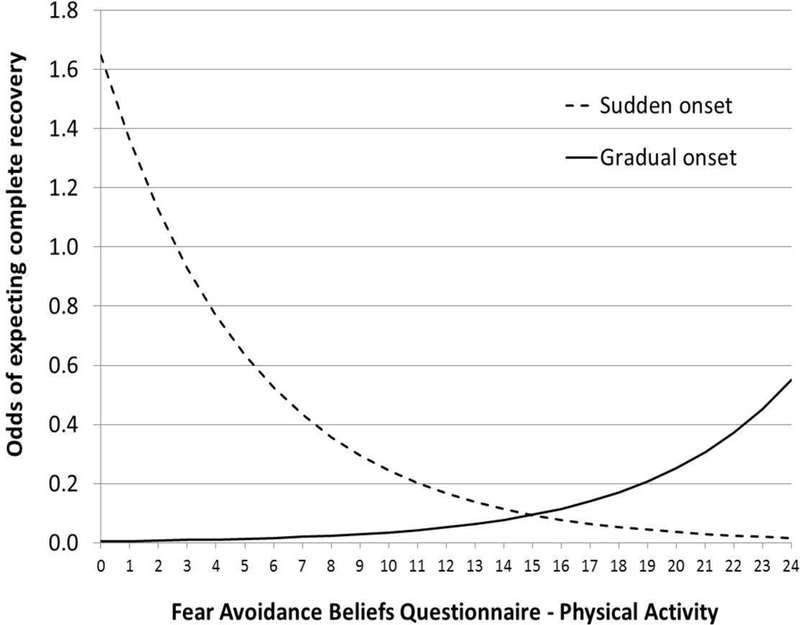
Interaction between the mode of onset of spinal pain and fear avoidance beliefs about physical activity expressed in odds.
Only one main effect was included in the model without an interaction term. This was level of education. Analysis of the effect suggested that patients with college education were more likely to have expectations of complete relief than patients who completed graduate school when all other factors in the model were kept constant.
To test model fit, we calculated area under the receiver operator curve. Results indicate an area of 0.827 (p < 0.001). The model identified 95% of the participants who expected complete recovery correctly and 28% of the participants without expectations of complete recovery (Table 5 and Figure 3).
Table 5.
Predicted values based on the parsimonious model versus responses of patients expecting complete recovery (yes) and those who do not (no).
| Predicted responses | ||
|---|---|---|
| Observed responses | Yes | No |
| Yes | 160 | 8 |
| No | 28 | 11 |
| Percentage correct | 85.1% | 57.9% |
Figure 3.

Receiver operator curve of the parsimonious model accuracy. Area under the curve equal is to 0.827.
DISCUSSION
The expectation for complete relief from symptoms has been showed to be a strong predictor of long term self-reported outcomes of conservative manual interventions for patients with spinal pain. Patient expectations take many forms. Thompson and Sunol (1995) described a model consisting of four categories of expectation: 1) predicted expectations or what the individual believes will occur; 2) ideal expectations or what the individual wants to occur; 3) normative expectations or what the individual believes should occur; and 4) unformed expectation or the lack of a preconceived notion regarding a situation or intervention. In this study we focused on predicted expectations.
Expectation is a key element of the placebo components that comprise part of every intervention. Placebos result in robust analgesia when individuals expect relief of symptoms. Traditionally, placebos are considered inert agents, devoid of a treatment effect; however, placebos are suprapinally mediated neurophysiological mechanisms of pain relief dependent upon expectation and conditioning (Bialosky et al, 2009). Despite this knowledge, identifying individuals likely to demonstrate a placebo response is elusive and placebo responses differ within individuals when differently labeled placebos are studied (Branthwaite and Cooper, 1981; Faasse et al, 2016). Placebo mechanisms are inherent to all interventions for pain and accounting for their magnitude as a mechanism of MT could result in the more effective provision of MT by taking advantage of factors known to maximize this particular mechanism such as maximizing expectation for the intervention or enhanced patient/ provider interaction (Benedetti, 2013) during the application of MT. Consequently, understanding factors influencing expectation will likely improve our understanding of factors influencing placebo and therefore pain relief mechanisms.
In this paper we sought to determine what patient factors were related to holding an expectation of complete recovery. We had no specific hypothesis regarding potential interactions in this exploratory study; however, the results of our analysis indicate interactions between gender and self-reported disability and levels of fear and the mode of the onset of pain, as well as an effects related to the education of the patient.
The nature of the interactions identified in our analyses suggests that simply using the level of a patient’s fear, or disability as an indicator for an intervention maybe insufficient for making prognostic judgments. These measures, fear and disability, are well-established prognostic factors predicting poorer outcomes in the management of patients with spinal pain; however, our findings show that the influence of these factors may act differently among patients to shape expectations of symptom relief and, potentially, result in worse or better outcomes through this mechanism. Our data show that the impact of fear avoidance beliefs about activity on expectations is different for patients that have a sudden onset of their pain compared to patients with a gradual onset of pain. Patients with a sudden onset of pain with low fear avoidance beliefs had better odds of expecting complete recovery than patients with gradual onset of pain at low levels of fear. This scenario can be illustrated by considering two patients with low fear avoidance beliefs; one wakes with pain, the other has had a long slow onset of pain. In this example, there are better odds that the patient who woke with pain will expect complete recovery. In contrast our model suggests that a patient with high fear and a sudden onset of pain has worse odds than a patient with a gradual onset and high fear. Here, we consider a patient with high fear avoidance beliefs. The fearful patient who wakes one morning with pain is likely to have lower odds of expecting complete recovery than the patient who is fearful but has had the pain gradually come on. It should be noted; however, that the for the most part, the odds of expecting complete recovery were below one for both patterns of pain onset except at low levels of fear.
The other interaction was between disability and gender where increases in disability had a larger effect for women than on men in this sample of patients. The effect for men resulted in an odds ratio close to 1 (which would indicate no change in odds) suggesting that the odds of men expecting complete recovery were very stable and consistent across all levels of disability while, in contrast, women had lower odds of expecting complete recovery at low levels of disability than men and higher odds at higher levels of disability. The underpinning cause of why there would be higher odds of a woman expecting complete recovery than a man at the same level of high disability is unclear. However, there is evidence from other work that women are more likely to seek healthcare than men (Eriksen, Sjogren, Ekholm, and Rasmussen, 2004; Shalev, Chodick, Heymann, and Kokia, 2005). This finding suggests some underpinning expectation in women more so than men that healthcare providers can impact the health condition. Alternatively, the result could be driven by the fact that more men in our study had: 1) higher expectations for recovery than women (in the univariate analysis); and 2) higher disability scores. This could explain the fairly stable level of expectations across the levels of disability in men; that is, potential range restriction in the variability of both the outcome (expectation) and part of the interaction term (disability). Additionally, estimates became very large once disability increased above 65%. However, this may have been a spurious finding as the findings could have possibly been exaggerated by the few individuals of both genders in our sample having levels of disability this high.
The effect of level of education on expectation was not expected. The findings from our analysis suggested that the odds of patients with college education expecting complete relief were higher than patients who completed graduate school. Other studies of expectations of benefit of treatment suggest that higher levels of education were associated with increased expectations of treatment. For example, Lurie et al, identified that patients who had not completed education beyond high school education expected less total benefit from care for back pain compared to those with more than high school education (Lurie et al, 2008). Additionally, Gepstein, Arinzon, Adunsky, and Folman (2005) found similar results with higher levels of education associated with positive expectations of benefit from surgery for spinal stenosis. Our study did differ from Gepstein, Arinzon, Adunsky, and Folman (2005) in that surgical interventions were not considered; however, patients in the study by Lurie were asked to consider surgical and non-surgical interventions. One explanation is that those other studies created dichotomous variables for education (i.e. less than high school or more than high school) and found the groups ‘more than high school’ to have higher expectations. Our data differed by adding the category for graduate education. Adding a category while increasing precision may decrease power of the comparison between highest and lowest categories of education. Alternatively, if our finding is a ‘true’ finding, the effects of the other studies may have been driven by the ‘college’ education category.
Our results are also different from other studies that identify demographic characteristics associated with predicted expectations. For example, Kongsted et al. (2014) identified duration of pain and number of previous episodes of LBP as having significant associations with the expectation of complete recovery. This was not the case in our study although our sample (patients who volunteered for our studies) and modeling (i.e including interactions in our models) was different. Recent evidence has begun to demonstrate that patient expectations are directly correlated with reductions in pain and improvements in function (Bishop, Bialosky, and Cleland, 2011; Bishop, Mintken, Bialosky, and Cleland, 2013; Palmlöf, Holm, Alfredsson, and Skillgate, 2016). The results of the current study provide clinicians with the availability to potentially identify individuals with a low expectation of treatment benefits. In these circumstances it may be essential for clinicians to educate the patient about potential interventions perhaps enhancing their expectation for the benefits a particular treatment approach.
Limitations
It is important to note that this was an explorative study. We tested all available interactions without specific hypotheses, testing all possible interactions. As such our findings may reflect chance findings among the data. Additionally, we analyzed previously collected data and, therefore, were not able to make any power or sample size calculations prior to beginning our analysis. This may have influenced the purposeful model building as potentially important associations might have not been identified in our sample, and interactions among predictors that were included might have been missed.
We also chose to create a binary outcome variable and pursue a logistic approach to improve interpretability of our modeling. The expectation for complete symptom relief was a five-level ordered variable and there is the potential that we lost some precision in our estimates. Therefore, we are unable to comment, based on this analysis, if there are meaningful predictors of what differentiates between ‘definitely yes’ and ‘yes’ levels of expecting complete symptom relief or ‘unsure’ and ‘no’ responses. Additionally, the measure of expectation we used has not been subjected to extensive testing. Consequently, we cannot be certain of the reliability of the simple question that was used to assess the general expectation of recovery. Nor has face validity of the question been established. Despite this limitation, this method of assessing predicted expectations has been previously used in the literature (Palmlöf, Holm, Alfredsson, and Skillgate, 2016). There is a need for universal recommendations to assess each primary category of expectations (e.g. normative and predictive) to allow improved comparison of results across settings and patient populations. Potential examples of these might include recommendations for the use of a visual analogue scale versus a categorical scale for ratings, time frames over which expectations might be established, and framing of expectations for specific interventions versus the general expectations of participating in care.
The majority of participants in this study had generally high expectations for recovery. This is likely related to at least two inter-related factors. First, these are patients who agreed to enroll in this study potentially indicating a selection bias toward patients who had even higher expectations than normally expected enrolling in our study. There was no method for determining if any differences existed between those patients who enrolled in our study and those who did not. Such a measure would useful to collect in future studies of conservative interventions. Second, patients seeking interventions for musculoskeletal dysfunction likely have high expectations of care; that is, they seek care precisely because they expect improvement. For example, patients seeking care for a musculoskeletal disorder from a physical therapist expect an 80% reduction in pain, and a 100% reduction in interference to their daily activities (Zeppieri et al, 2012). We propose, not unlike other forms of screening, that there is an opportunity for physical therapists to build positive, but realistic, expectations of recovery for patients.
Another consideration is that very large estimates were calculated with broad confidence intervals for two of the main effects in the model; specifically the odds ratios of males compared to females and of sudden onset compared to gradual onset. This effect occurs from inadequate membership within a specific cell and limited ranges in the data. Inspection of the cells suggests this potentially the case for sudden onset neck pain but not for males. Often when modelling using logistic regression, the effects with large estimates and confidence intervals are considered unstable and not suitable for further calculations based on the model. However, when interaction effects based on these main effects are significant, they supersede the main effects in interpretation of the model. Given that our estimates provided for the interaction terms were significant and appear stable and appropriate, the main effects were retained within the model and presented in our results.
Additionally, all patients were seeking care from a physical therapist and determinants of expectation for complete relief may differ for other types of healthcare providers and we only measured expectation at baseline. Expectations may change over time so it may be important to consider expectations at differing time points and whether the predictors remain the same as expectations evolve. We also did not have access to information regarding patient disposition at the intake examination. Evidence indicates that positive disposition is related to holding higher expectations of benefit and successful outcome (Morton, Watson, El-Deredy, and Jones, 2009). Last, we cannot be certain of the framework that patients used and while questions emphasized predictive expectations for treatment, we cannot rule out that a patient may have indicated his or her ‘desire’ or ‘hope’ for treatment in response to that questions. In general desired outcomes are for lower pain and better function than predicted outcomes (Zeppieri et al, 2012).
CONCLUSIONS
Our primary objective was to examine factors associated with a patient holding an expectation of complete recovery. Our findings show that interactions exist among previously described factors know to impact outcome in patients with spinal pain. An interaction between gender and disability suggested that the odds of expecting complete recovery remained relatively stable over differing levels of disability for men, while the odds of expecting completely recovery increased as disability increased for women (OR 0.9 [95%CI 0.8, 0.9]). Second, the level of fear avoidance beliefs about physical activity affected the odds of expecting recovery differently for patients with a sudden onset of pain (higher odds) compared to patients with gradual onset of pain but only at very low levels of fear (OR 0.7 [95%CI 0.5, 0.97]). The education level of the patient was also associated with better odds for expecting complete recovery for college-educated patients compared to those with graduate school education (OR 5.0 [95%CI 1.9, 13.4]). This was an explorative study without specific hypotheses and the results could have been influenced by error related to multiple hypothesis testing.
ACKNOWLEDGMENTS
The original trials on which this current work was based were directly supported by the Foundation for Physical Therapy, the Orthopaedic Section of the American Physical Therapy Association and an American Academy of Orthopaedic Manual Physical Therapists Cardon Rehabilitation Products Grant. MDB and JEB received support from the National Center of Complementary and Integrative Health (AT006334).
Footnotes
Declaration of Interest
The authors indicate no conflict of interest.
REFERENCES
- Benedetti F 2013. Placebo and the new physiology of the doctor-patient relationship. Physiological Reviews 93: 1207–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ 2009. The mechanisms of manual therapy in the treatment of musculoskeletal pain: A comprehensive model. Manual Therapy 14: 531–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop MD, Bialosky JE, Cleland JA 2011. Patient expectations of benefit from common interventions for low back pain and effects on outcome: Secondary analysis of a clinical trial of manual therapy interventions. Journal of Manual and Manipulative Therapy 19: 20–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop MD, Mintken PE, Bialosky JE, Cleland JA 2013. Patient expectations of benefit from interventions for neck pain and resulting influence on outcomes. Journal of Orthopaedic and Sports Physical Therapy 43: 457–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Branthwaite A, Cooper P 1981. Analgesic effects of branding in treatment of headaches. British Medical Journal 282(6276): 1576–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Childs JD, Fritz JM, Flynn TW, Irrgang JJ, Johnson KK, Majkowski GR, Delitto A 2004. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: A validation study. Annals of Internal Medicine 141: 920–928. [DOI] [PubMed] [Google Scholar]
- Cleland JA, Childs JD, Whitman JM 2008. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Archives of Physical Medicine and Rehabilitation 89: 69–74. [DOI] [PubMed] [Google Scholar]
- Cleland JA, Fritz JM, Kulig K, Davenport TE, Eberhart S, Magel J, Childs JD 2009. Comparison of the effectiveness of three manual physical therapy techniques in a subgroup of patients with low back pain who satisfy a clinical prediction rule: A randomized clinical trial. Spine 34: 2720–2729. [DOI] [PubMed] [Google Scholar]
- Cleland JA, Fritz JM, Whitman JM, Palmer JA 2006. The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy. Spine 31: 598–602. [DOI] [PubMed] [Google Scholar]
- Cleland JA, Mintken PE, Carpenter K, Fritz JM, Glynn P, Whitman J, Childs JD 2010. Examination of a clinical prediction rule to identify patients with neck pain likely to benefit from thoracic spine thrust manipulation and a general cervical range of motion exercise: Multi-center randomized clinical trial. Physical Therapy 90: 1239–1250. [DOI] [PubMed] [Google Scholar]
- Eriksen J, Sjogren P, Ekholm O, Rasmussen NK 2004. Health care utilisation among individuals reporting long-term pain: An epidemiological study based on Danish National Health Surveys. European Journal of Pain 8: 517–523. [DOI] [PubMed] [Google Scholar]
- Faasse K, Martin LR, Grey A, Gamble G, Petrie KJ 2016. Impact of brand or generic labeling on medication effectiveness and side effects. Health Psychology 35: 187–190. [DOI] [PubMed] [Google Scholar]
- Fritz JM, Irrgang JJ 2001. A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Physical Therapy 81: 776–788. [DOI] [PubMed] [Google Scholar]
- Gepstein R, Arinzon Z, Adunsky A, Folman Y 2005. Decompression surgery for lumbar spinal stenosis in the elderly: Preoperative expectations and postoperative satisfaction. Spinal Cord 44: 427–431. [DOI] [PubMed] [Google Scholar]
- Goldstein MS, Morgenstern H, Hurwitz EL, Yu F 2002. The impact of treatment confidence on pain and related disability among patients with low-back pain: Results from the University of California, Los Angeles, low-back pain study. Spine Journal 2: 391–399. [DOI] [PubMed] [Google Scholar]
- Goossens ME, Vlaeyen JW, Hidding A, Kole-Snijders A, Evers SM 2005. Treatment expectancy affects the outcome of cognitive-behavioral interventions in chronic pain. Clinical Journal of Pain 21: 18–26. [DOI] [PubMed] [Google Scholar]
- Hayes RP, Naegeli AN 2010. The contribution of pretreatment expectations and expectation perception difference to change in treatment satisfaction and end point treatment satisfaction in the context of initiation of inhaled insulin therapy in patients with type 2 diabetes. Diabetes Technology and Therapeutics 12: 447–453. [DOI] [PubMed] [Google Scholar]
- Iles RA, Davidson M, Taylor NF 2008. Psychosocial predictors of failure to return to work in non-chronic non-specific low back pain: A systematic review. Occupational and Environmental Medicine 65: 507–517. [DOI] [PubMed] [Google Scholar]
- Iles RA, Davidson M, Taylor NF, O’Halloran P 2009. Systematic review of the ability of recovery expectations to predict outcomes in non-chronic non-specific low back pain. European Spine Journal 19: 25–40. [DOI] [PubMed] [Google Scholar]
- Jacob T, Baras M, Zeev A, Epstein L 2001. Low back pain: Reliability of a set of pain measurement tools. Archives of Physical Medicine and Rehabilitation 82: 735–742. [DOI] [PubMed] [Google Scholar]
- Kongsted A, Vach W, Axo M, Bech RN, Hestbaek L 2014. Expectation of recovery from low back pain: A longitudinal cohort study investigating patient characteristics related to expectations and the association between expectations and 3-month outcome. Spine 39: 81–90. [DOI] [PubMed] [Google Scholar]
- Lurie JD, Berven SH, Gibson-Chambers J, Tosteson T, Tosteson A, Hu SS, Weinstein JN 2008. Patient preferences and expectations for care determinants in patients with lumbar intervertebral disc herniation. Spine 34: 2663–2668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marschall-Kehrel D, Roberts RG, Brubaker L 2006. Patient-reported outcomes in overactive bladder: The influence of perception of condition and expectation for treatment benefit. Urology 68 (2 Suppl): 29–37. [DOI] [PubMed] [Google Scholar]
- Morton DL, Watson A, El-Deredy W, Jones AK 2009. Reproducibility of placebo analgesia: Effect of dispositional optimism. Pain 146: 194–198. [DOI] [PubMed] [Google Scholar]
- Ozegovic D, Carroll LJ, David CJ 2009. Does expecting mean achieving? The association between expecting to return to work and recovery in whiplash associated disorders: A population-based prospective cohort study. European Spine Journal 18: 893–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmlöf L, Holm LW, Alfredsson L, Skillgate E 2016. Expectations of recovery: A prognostic factor in patients with neck pain undergoing manual therapy treatment. European Journal of Pain 20: 1384–1391. [DOI] [PubMed] [Google Scholar]
- Rhodes T, Bernays S, Terzic KJ 2009. Medical promise and the recalibration of expectation: hope and HIV treatment engagement in a transitional setting. Social Science and Medicine 68: 1050–1059. [DOI] [PubMed] [Google Scholar]
- Shalev V, Chodick G, Heymann AD, Kokia E 2005. Gender differences in healthcare utilization and medical indicators among patients with diabetes. Public Health 119: 45–49. [DOI] [PubMed] [Google Scholar]
- Thompson AG, Sunol R 1995. Expectations as determinants of patient satisfaction: Concepts, theory and evidence. International Journal of Quality Health Care 7: 127–141. [DOI] [PubMed] [Google Scholar]
- Waddell G, Newton M, Henderson I, Somerville D, Main CJ 1993. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear- avoidance beliefs in chronic low back pain and disability. Pain 52: 157–168. [DOI] [PubMed] [Google Scholar]
- Zeppieri G Jr, Lentz TA, Atchison JW, Indelicato PA, Moser MW, Vincent KR, George SZ 2012. Preliminary results of patient-defined success criteria for individuals with musculoskeletal pain in outpatient physical therapy settings. Archives of Physical Medicine and Rehabilitation 93: 434–440. [DOI] [PubMed] [Google Scholar]


