Abstract
Transient lateral patellar dislocation (TLPD) is a common lesion in young adults. Vascular injury as a complication of TLPD has not been previously described. We report a case of descending genicular artery (DGA) injury after TLPD. Immediate angiography demonstrated rupture of DGA. Embolization was performed with sudden interruption of bleeding. DGA injury should be considered as a complication after TLPD and prompt diagnosis and intervention are required. We propose selective embolization as a safe and effective procedure to stop bleeding.
Keywords: Lateral patellar dislocation, Descending genicular artery, Medial patellofemoral ligament, Arterial injury, Angiographic embolization
1. Introduction
Transient lateral patellar dislocation (TLPD) is common in young and active patients as a consequence of low-energy traumas in sports and physical activity and may be complicated by patellofemoral chondral lesions as well as damage to the medial patellar stabilizers.1, 2
Injuries of vessels supplying medial capsular ligamentous structures of the knee have been rarely described following knee surgical procedures 3, 4, 5, 6, 7, 8 and trauma.9 We report a case of descending genicular artery (DGA) injury after a TLPD requiring an urgent angiographic coil embolization. To our knowledge, this occurrence has not previously been described. The diagnostic strategy and treatment are discussed.
2. Case report
A 27-year-old male patient was admitted to the Emergency Department because of a right knee haematoma after a TLPD which occurred during tennis activity two hours before. The patient felt lateral patellar dislocation after a sudden change of direction, subsiding after a few moments. He experienced a similar episode to the left knee one year before.
Physical examination revealed a large swelling in the medial side of the right knee with no signs of patellar dislocation or subluxation; the range of motion (ROM) was limited by severe pain. No collateral or cruciate ligament instability was detected.
The lower limb was warm and the peripheral pulses were strong and symmetrical. No acute peripheral nervous deficiency was observed. A complete blood count showed normal values. Knee x-rays ruled out fractures or dislocation. A color doppler ultrasound exam revealed an extensive haematoma, especially located in the medial aspect of the knee, with no pulsatile masses. One hour later, knee swelling increased, and an urgent contrast-enhanced CT showed a 10 cm haematoma supplied by active bleeding from a thin distal branch of the DGA (Fig. 1A, B). Immediate angiography of the left common femoral artery demonstrated contrast medium extravasation from distal branch of the DGA (Fig. 2A). Embolization was successfully performed using micro metal coils and Spongostan (Fig. 2B), and no further extravasation was noted. Two days later, the patient was discharged with a knee brace locked at 30°, and weight-bearing was delayed for 20 days. A 30-day deep vein thrombosis prophylaxis (Enoxaparin 4000 U.I. SC once a day; Clexane, Sanofi Aventis, France) and a 7-day antibiotic prophylaxis course (Amoxicillin-Clavulanic Acid, 875 + 125 mg orally 3 times a day; Augmentin, Glaxo Smith Kline, UK) were administered.
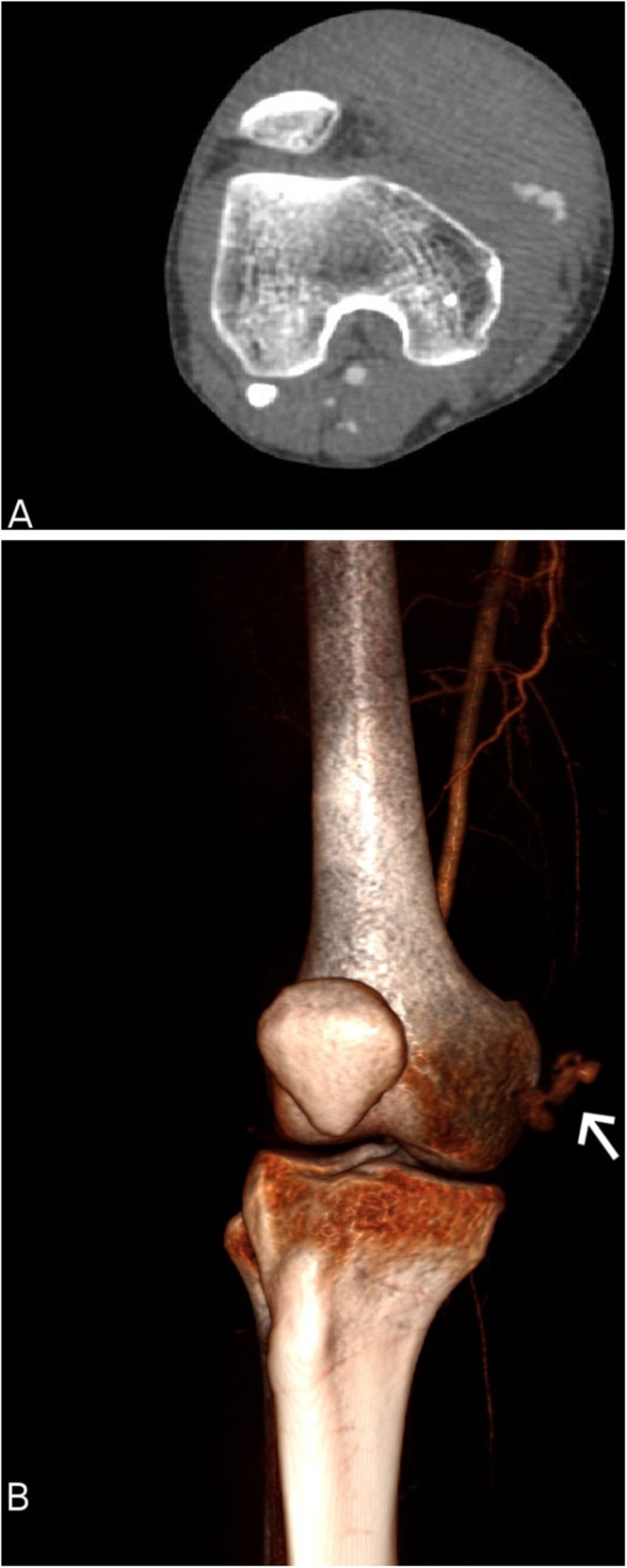
Fig. 1.
Knee contrast-enhanced computed tomography (CT). Axial view (A) showing a large haematoma in the medial side of the knee. 3D CT reconstruction (B) revealingactive bleeding (arrow) from the descending genicular artery (DGA).
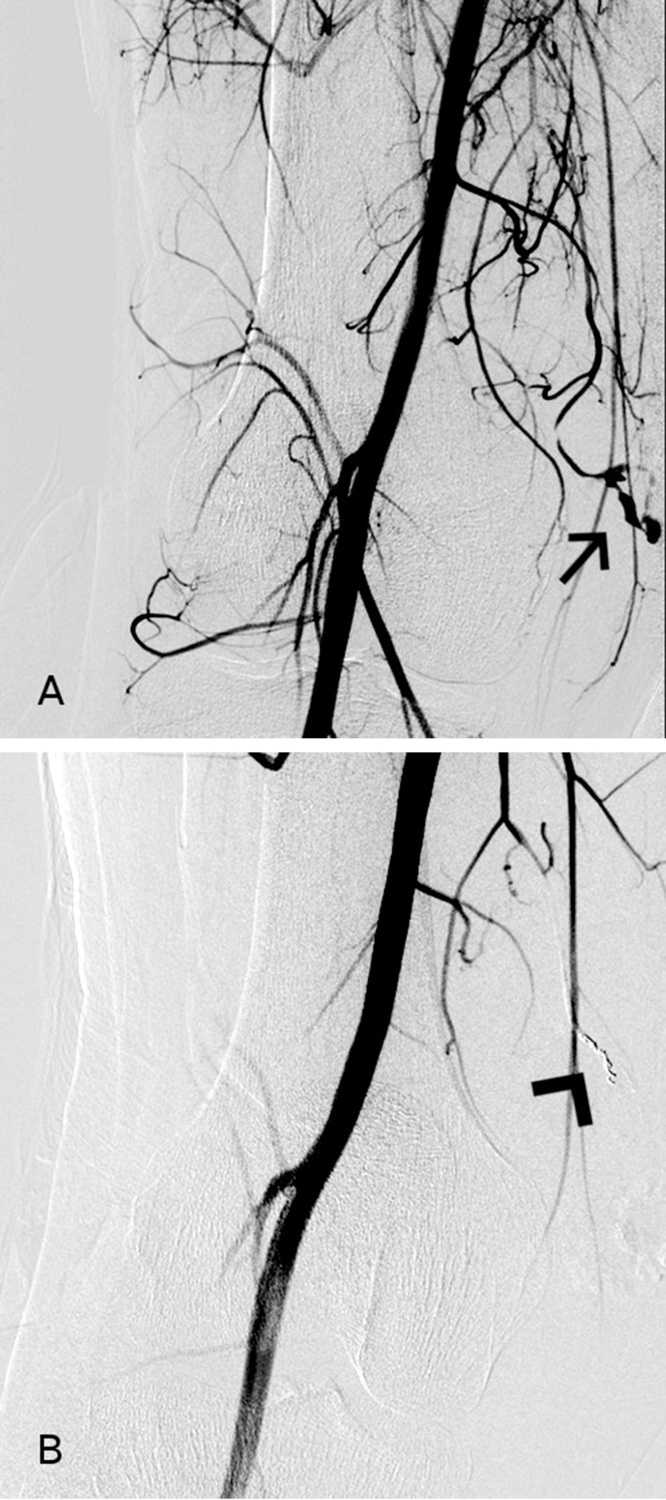
Fig. 2.
Selective angiography. Pre-embolization angiography (A) showing contrast medium extravasation from a distal branch of the DGA (arrow). Post-embolization angiography (B) demonstrating no residual bleeding from the injured vessel (arrowhead).
At 3-month follow-up, knee magnetic resonance imaging (MRI) detected abnormalities of medial patellofemoral ligament (MPFL) at the femoral attachment and vastus medialis obliquus (VMO) fibers as a result of muscle strain (Fig. 3A, B). Knee MRI also revealed several predisposing factors for patellar instability, such as trochlear dysplasia (trochlear facet asymmetry ratio of 0.3, trochlear inclination of 10.5°, and trochlear depth of 4 mm) (Fig. 4), and patella alta (Insall-Salvati index of 1.5) (Fig. 5). Lateralization of the tibial tuberosity (the distance between Tibial Tuberosity and Tibial Groove) was found to be pathological on CT scan (2.4 cm) (Fig. 6).
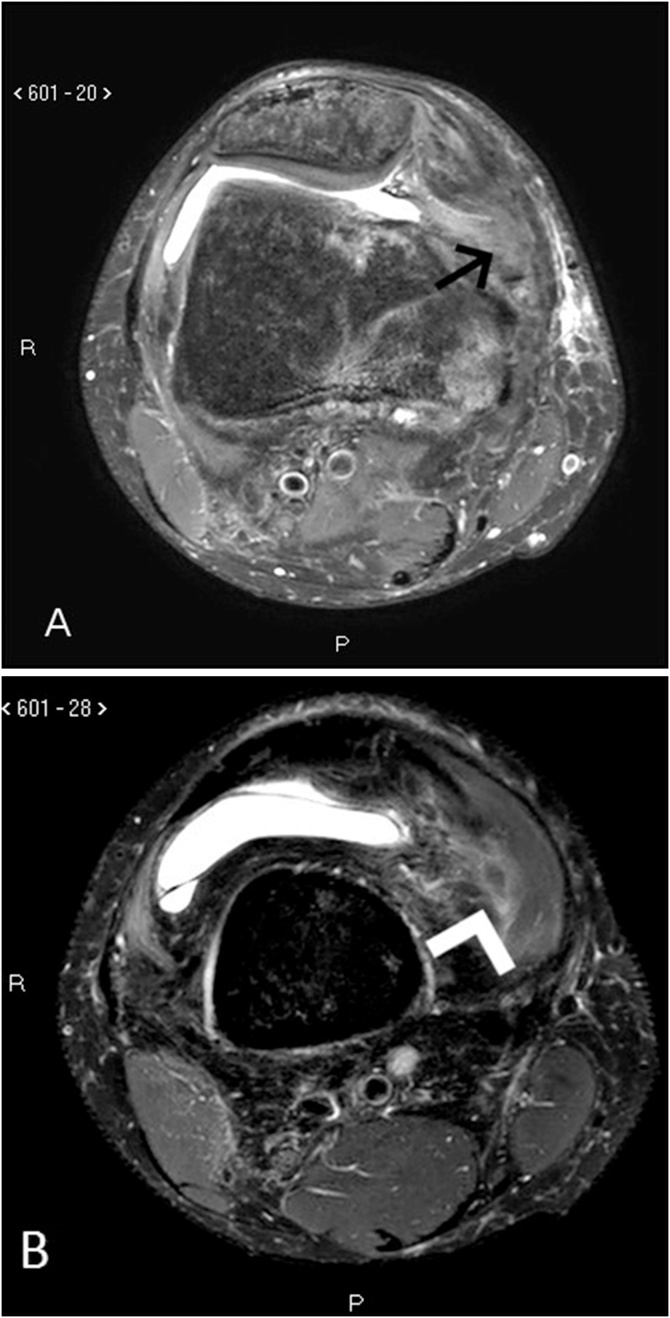
Fig. 3.
Axial knee magnetic resonance imaging (MRI) in T2 SPAIR sequence: abnormalities of MPFL (A) at the femoral attachment (arrow), and signs of vastus medialis oblique (VMO) fibers strain (B) (arrowhead).
Fig. 4.
Axial knee MRI image in sax cartilage sequences revealing trochlear displasia: trochlear facet asymmetry ratio (A) of 0.3, trochlear inclination (B) of 10.5°.
Fig. 5.
Sagittal knee MRI image in T1 sequence demonstrating patella alta (Insall-Salvati index of 1.5).
Fig. 6.
Overlapping axial CT images through the tibial tuberosity (TT) and mid-trochlear groove (TG) for calculation of the TT–TG distance reveals lateralization of TT (value of 2.4 cm).
Six-month clinical evaluation showed complete articular ROM and no patellar instability. The patient returned to previous work and recreational activities.
3. Discussion
TLPD usually occurs in young athletes, as a result of a low-energy trauma, by two possible mechanisms. The most common is due to femoral internal rotation with a flexed knee and the tibia extrarotated. A direct trauma to the medial aspect of the patella is more rarely involved. The direction of dislocation is usually medial to lateral, and knee extension restores joint congruity.1
The main predisposing factors for patellar dislocation can be easily measured with MRI or CT, and include trochlear dysplasia, patella alta, and lateralization of the tibial tuberosity. In our patient, a lateral trochlear inclination of 10.5° and a ratio of 0.3 between the two trochlear facets demonstrated trochlear dysplasia. Insall-Salvati ratio of 1.5 was consistent with patella alta. Finally, an increased lateralization of the tibial tuberosity was found (2.4 cm).1 The association between these anatomical factors and a low-energy trauma (femoral internal rotation with flexed knee) was sufficient to explain the TLPD.
Patellofemoral osteochondral lesions, MPFL and medial retinaculum injuries, and edema or strain of the distal VMO fibers are well known complications of patellar dislocation,2 but to our knowledge, vascular complications have not been described previously. The medial region of the patella and the medial and proximal capsular ligaments of the knee are vascularized by the articular branches of the DGA and the medial-superior genicular artery.9 DGA is the distal branch of the superficial femoral artery which usually originates about 13 cm proximal to the knee joint line. The artery splits into the saphenous, muscular and articular branches, supplying the skin of the medial aspect of the knee, the VMO's distal fibers and the medial capsular ligamentous structures, respectively. Furthermore, the articular branch descends distally and divides before the adductor tubercle into its terminal branches: the superficial capsular branches, laying on top of the MPFL, and the deep articular branches, passing underneath the ligament.10 DGA injuries have been rarely reported as a result of knee surgical procedures, such as hamstring anterior cruciate ligament reconstruction,3 replacement surgery,4 arthroscopy,5 and arthrotomy with synovectomy.6, 7 Arthroscopic portals,4, 6 placement of active drains,5, 7 and direct lesion during operative exposures 8 are the main iatrogenic causes of DGA lesion. The MPFL originates from the adductor tubercle and inserts on the superomedial patellar surface. It takes connection with two branches of the DGA: the superficial capsular branch, passing superficial to the ligament, and the deep articular branch, which runs deep to the ligament.9 In our patient, muscular and articular branches of DGA are likely to have been damaged during trauma, as well as MPFL and VMO fibers, as showed in the knee MRI. Furthermore, ligamentous, muscular, and vascular structures could have been injured through a distracting mechanism caused by the sudden lateralization of the patella.
Contrast-enhanced CT is the gold standard for better evaluating the presence and the site of active bleeding. Successful treatments of hematomas around the knee by angiographic embolization or surgical ligation of the feeding artery have been reported. We consider the treatment used in our case both effective and safe: angiography is crucial to confirm the origin of hemorrhage and to perform vessel embolization with the benefits of a minimally invasive procedure.11
In conclusion, DGA injury should be considered as a vascular complication following TLPD. An accurate patient history is an important tool to identify this unusual complication, as spontaneous patellar relocation is common. Therefore, in the presence of any clinical evidence of vascular damage, contrast-enhanced CT and angiographic embolization as a minimally invasive treatment to solve this complication should be considered.
Conflict of interest
The authors have none to declare.
Funding
This case report did not receive any specific grant from funding agencies in the public, commercial, or not-for profit sectors.
References
- 1.Earhart C., Patel D.B., White E.A., Gottsegen C.J., Forrester D.M., Matcuk G.R., Jr. Transient lateral patellar dislocation: review of imaging findings, patellofemoral anatomy, and treatment options. Emerg Radiol. 2013;20(1):11–23. doi: 10.1007/s10140-012-1073-9. [DOI] [PubMed] [Google Scholar]
- 2.Elias D.A., White L.M., Fithian D.C. Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology. 2002;225(3):736–743. doi: 10.1148/radiol.2253011578. [DOI] [PubMed] [Google Scholar]
- 3.Tsubosaka M., Matsushita T., Kuroda R., Matsumoto T., Kurosaka M. Pseudoaneurysm of the articular branch of the descending genicular artery following double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2721–2724. doi: 10.1007/s00167-015-3639-z. [DOI] [PubMed] [Google Scholar]
- 4.Shaw A., Stephen A., Lund J., Bungay P., Denunzio M. Geniculate arterial pseudoaneurysm formation following trauma and elective orthopaedic surgery to the knee: 2 case reports and a review of the literature. J Radiol Case Rep. 2009;3(3):12–16. doi: 10.3941/jrcr.v3i3.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tozzi A., Ferri E., Serrao E., Colonna M., De Marco P., Mangialardi N. Pseudoaneurysm of the descending genicular artery after arthroscopic meniscectomy: report of a case. J Trauma. 1996;41(2):340–341. doi: 10.1097/00005373-199608000-00024. [DOI] [PubMed] [Google Scholar]
- 6.Scoles P.V., King D. Traumatic aneurysm of the descending geniculate artery: a complication of suction drainage in synovectomy for hemophilic arthropathy. Clin Orthop Relat Res. 1980;150:245–246. [PubMed] [Google Scholar]
- 7.Rifaat M.A., Massould A.F., Shafie M.B. Post-operative aneurysm of the descending genicular artery presenting as a pulsating haemarthrosis of the knee. J Bone Joint Surg Br. 1969;51(3):506–507. [PubMed] [Google Scholar]
- 8.Denoncourt P.M., O'Connell F.D. False aneurysm of the medial superior genicular artery complicating a closed knee injury. Clin Orthop Relat Res. 1985;194:291–292. [PubMed] [Google Scholar]
- 9.Baldwin J.L. The anatomy of the medial patellofemoral ligament. Am J Sports Med. 2009;37(12):2355–2361. doi: 10.1177/0363546509339909. [DOI] [PubMed] [Google Scholar]
- 10.García-Pumarino R., Franco J.M. Anatomical variability of descending genicular artery. Ann Plast Surg. 2014;73(5):607–611. doi: 10.1097/SAP.0b013e318276d964. [DOI] [PubMed] [Google Scholar]
- 11.Saad N.E., Saad W.E., Davies M.G., Waldman D.L., Fultz P.J., Rubens D.J. Pseudoaneurysms and the role of minimally invasive techniques in their management. Radiographics. 2005;25(Suppl. 1):S173–89. doi: 10.1148/rg.25si055503. [DOI] [PubMed] [Google Scholar]