Abstract
This study was carried out to monitor current iodization and its impact on iodine excess. The results show medians values increasing gradually from 62 ug/L to 283 μg/L then dropping to 169 μg/L for acceptable significance to above toxicity significant values of 300 μg/L as from 2006, exaggerated in 2018 at 1145 μg/L. Salt iodine contents, compared to the 20 – 40 ppm range recommended by WHO, show coarse grain as lowest with average 26.9 ppm while fine grain for human consumption average was 57.3 ppm. The extra fine grain variety has the highest iodine content at 248.8 ppm. Imported cerebos salt from France contained iodine at an average of 45.5 ppm while the Senegal salt contained iodine at an average of 182.2 ppm. The F-ratio (62.9) indicates great variation in iodine content of the salt involved while the p-value (p = 0.0002) indicates significant differences in iodine content of the salt of different refineries. By implication, there are still lapses on iodization.
Keywords: Endocrinology, Food analysis, Food safety, Nutrition, Public health
1. Introduction
It has been diagnosed that approximately two billion individuals worldwide have insufficient iodine intake, with those in south Asia and sub-Saharan Africa particularly affected (WHO, 2007). To salvage the situation, World Health Organization (WHO) and United Nations Children's Fund (UNICEF) recommended universal salt iodization (USI) as the main strategy to achieve elimination of iodine-deficiency disorders (IDD) (WHO/NHD/01.1, 2001). Universal salt iodization (USI) has been adopted in nearly all countries and has become the best strategy to control iodine deficiency as one of the most cost-effective ways to contribute to economic and social development (WHO/NHD/01.1, 2001). Iodine is an essential component of the thyroid hormones, thyroxine (T4) and triiodothyronine (T3), necessary for normal growth, development, and metabolism during pregnancy, infancy and throughout life (Hetzel, 1991). When the physiological requirements for iodine are not met, a series of functional and developmental abnormalities occur, including thyroid function abnormalities termed IDD (Hetzel, 1991).
In the light of these facts, production, supply and use of iodized salt for humans and animals should become the behavioural norm. Monitoring the process of salt iodization and its impact on the iodine nutrition is of major importance to ensure the efficiency and efficacy of USI in any given population (Aburto et al., 2014). Since production and importation of only iodized edible salt obviously are the main pillars of USI efforts, monitoring at production and importation should be more regular. It is much easier to do this since production plants and importer warehouses are not always many, and they usually serve wide regional consumer populations. In reviewing the data of monitoring at production from several countries WHO/UNICEF/ICCIDD Consultation of 1996 (WHO/NHD/01.1, 2001) revised the norms (of 100 ppm) for iodized salt production and recommended 20–40 ppm of iodine or 34–66 ppm of Potassium Iodate. Also, urinary iodine survey and iodized salt consumption need careful monitoring because both iodine deficiency and iodine excess have adverse effects on health. While lack of iodine results to IDD, iodine excess brings about hyperthyroidism (an overactive thyroid gland), a condition in which excess thyroid hormone is produced. Patients with hyperthyroidism have increased risks of various cardiovascular problems, such as atrial fibrillation, hypertension, coronary artery disease, stroke and heart failure (Ertek and Cicero, 2013). Treatment of hyperthyroidism with either antithyroid medications or radioactive iodine is known to decrease these risks, but the risks are still higher than average when compared to a person without hyperthyroidism (Martin et al., 2007). The aim of this study is to advocate prevention through control.
The two commonly used indicators for assessing excess iodine are the iodine content and household coverage of iodized salt and the median urinary iodine concentration (UIC) value for the sampled population (Fereia et al., 2018; Lantum, 2011). Lantum (Lantum, 1990–1995 and Lantum, 1999) deployed a lot of efforts towards effective elimination of IDD in Cameroon through baseline survey, advocacy, sensitization and ensuring iodization, but consistent control for sustainability is necessary.
In view of the above this study was carried out to monitor: the effectiveness of refinery iodization, the iodine content of salt at the port (importation level), household level consumption of iodized salt and UIC of Cameroon population.
Study hypothesis: Median UIC increases tremendously because of excess iodization.
2. Material and methods
The study was designed firstly to visit the production and importation chains of the Douala port regularly, twice a year (starting from 2002), in January–February and August for five years consecutively for evaluation and education. Subsequently to evaluate, in 2017 and 2018, the impact of the previous visits. Household salt iodine content and UIC for all the years involved were concomitantly determined.
In all visits at the port and production chains, salt samples were collected from each target point that included the importers’ warehouses and from each producer (crude and iodized salt at the sacking points). Where a refinery was producing both coarse grain salt, fine table salt, and extra-fine powder, samples of all the three types were taken. To assure that the iodine content at each level was not accidental, at least four samples were taken from each level in order to eventually use the mean - values to determine the iodization trends. All samples were analyzed at the International Reference Laboratory (IRLI) for Iodine in Yaounde by iodimetric titration (World Health Organization, 2001).
Since study site was Cameroon, the national baseline data obtained by authors (Lantum, 1991), was exploited to conveniently choose study areas from amongst 20 endemic areas previously selected as sentinel sites for specific studies. Exceptions were 1999 and 2002 where surveys were comprehensive and national. An additional area like Yaounde was included in order to observe the reality of iodine consumption in the country. In all cases, local primary schools were visited for a study population of 5–12 years to evaluate the influence of transport (from refinery) on salt iodine content and household consumption of iodized salt. Children were served sachets and asked to bring about 25 g (two spoonsful) of salt from their mother's kitchen the next day and urine samples (25–50 ml) were collected from them for UIC determination.
Whether sampling involved sentinel sites at household level or the entire territory, urine and salt sample sizes were determined according to the goitre prevalence rate (at 95% confidence level) after the method of Stokes and Tom (2004), used in epidemiological studies. This team of researchers didn't carry out any survey in 2002 but data from randomly selected clusters obtained by the ministry of Public Health in that year was exploited for median value of UIC (Ministère de Santé Publique, 2002).
Ethical clearance was not recommended, but the authorizations required for the study were obtained from Divisional and Regional Delegations of Public Health.
The iodine content of the urine samples was determined in the various samples collected by alkaline dry ash method as described (Karmarkar et al., 1986). Urine was mixed with K2CO3 (1.25M) and dried in an oven at 100 °C (3hours) then transferred to a muffle furnace regulated at 600 °C (≥2 h); content regenerated with sodium meta-arsenite for Sandell-Kolthoff reaction.
The Centre for Research on Food and Nutrition participates in EQUIP (Ensuring the Quality of Urinary Iodine Procedure) external quality control assurance programme.
Advantage of this External Quality Assessment was exploited by introducing in each run EQUIP samples of known iodine concentrations so as to ensure accurate results. This technique helped to ensure scientific validity of the results as well as the reliability of all operations.
2.1. Statistical analyses
Raw data obtained were analyzed in a statistical package of Statgraphic 5.0, in one-way Analysis of Variance (ANOVA) according to the procedure of Steel and Torrie (1980). Significantly different means or averages were separated using the methods of Duncan (1955). The values obtained were presented as Least Significance Differences (LSD) of means at (p < 0.05) compared to those which did not differ significantly (p > 0.05) from the value of Duncan. Sigmaplots11.0 was used for plotting of graphs.
3. Results and discussions
3.1. Median urinary iodine values and implications
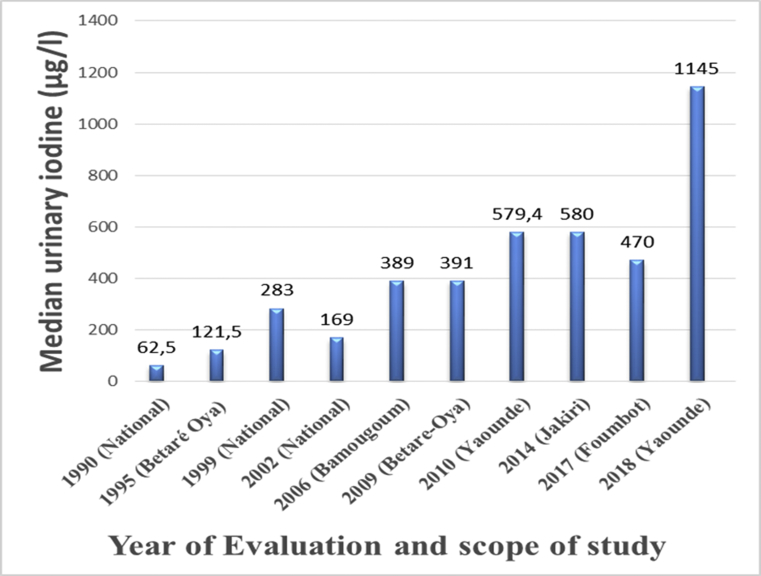
Iodine levels in contrast vary with iodine intake and cannot be reliably measured at individual levels (Rasmussen et al., 1999), but median urinary iodine concentrations (UIC) are recommended and have been widely used as a biomarker of population iodine intake. Levels >300 μg/l are considered excessive in children and adults while levels >500 μg/l are considered excessive in pregnant women (WHO/UNICEF/ICCIDD, 2007). From the baseline value of 62.5 μg/L (Fig. 1), the median values are observed to increase gradually to 283 μg/L in 1999, dropping to 169 μg/L for acceptable significance to above the toxicity significant values as from 2006, being exaggerated in 2018 at 1145 μg/L.
Fig. 1.
Evaluation year against median urinary iodine values.
An auto-regulatory phenomenon in which excess uptake of iodine by the thyroid inhibits thyroid hormone synthesis is called Wolff-Chaikoff effect (Kirstie and Symonds, 2017). This might have happened in Yaounde where iodine intake is very high. This phenomenon that occurs in some susceptible patients, with excess iodine furnishing rich ingredients for increased production of thyroid hormones might be transient or permanent (DeGroot, 2016). This iodine-induced hyperthyroidism that is also called the Jod–Basedow phenomenon was first described in the early 1800s in patients with endemic goiter treated with iodine supplementation (Coindet, 1821). Though this situation is generally well-tolerated in most people, nobody has researched to confirm or infirm a similar scenario in Cameroon, especially in a major city with high iodine intake like Yaounde. Also, infants with congenital heart disease exposed to excess iodine are more susceptible to thyroid disorders and impaired renal function (Thaker et al., 2017). These precarious situations have either been occurring and merit further investigations or may soon start happening in Cameroon, due to high median values as seen in Fig. 1. Similar situations occurred in Poland, Greece, Australia, Sweden etc (Angela and Lewis, 2014) but were mitigated with adequate intervention measures.
3.2. Results on iodized salt and its implication
The salt producers studied were: Société de Transformation du Sel (SOTRASEL), Société de Purification du Sel (SOCAPURSEL), African Salt Company (Société de Raffinage du Sel) producing AIGLE-brand, and Sel du CAMEROUN (SELCAM). The fifth dealer was a major importer (SOREPCO Sarl) of the brand Sel de Sine Saloum (SSS), and the sixth dealer was an importer marketing CEREBOS which is table salt from France.
Table 1 shows that in the crude imported for refining, there is some natural iodine, if it is marine salt; with an average iodine content of 2.9 ppm, range 1.1–8.5 ppm. Cattle or coarse grain has an average of 26.9 ppm with range 0–70.9 ppm and it is the most widely marketed while fine grain for human consumption has an average of 57.3 ppm with a range of 12.7–157.5 ppm. Refineries received orders to produce extra-fine (industrial salt) needed by the milk industry (NESTLE), Chocolate factory (CHOCOCAM) and bakeries. The extra fine grain variety has the highest iodine content at 248.8 ppm with range 31.7–751.5 ppm. The F-ratio (62.9) indicates great variation in iodine content of all salt varieties involved while the p-value (p = 0.0002) indicates significant differences in the salt of different refineries.
Table 1.
Means, averages and ranges of iodine in salt refineries varieties.
| Salt variety | Refinery | Count | Mean iodine (ppm) | Average (ppm) | Range |
|---|---|---|---|---|---|
| Crude | SELCAM | 8 | 1.4 ± 23.2a | 2.9a | 1.1–8.5 |
| SOTRASEL | 18 | 4.7 ± 15.5a | |||
| SOCAPURSEL | 24 | 2.4 ± 13.4a | |||
| EAGLE | 8 | 2.3 ± 23.3a | |||
| Cattle or Coarse grain | SELCAM | 4 | 22.6 ± 32.9ab | 26.9ab | 0.0–70.9 |
| SOTRASEL | 18 | 36.8 ± 15.5ab | |||
| SOCAPURSEL | 13 | 11.2 ± 18.3ab | |||
| EAGLE | 8 | 32.5 ± 23.3ab | |||
| Fine grain | SOCAPURSEL | 17 | 62.6 ± 16b | 57.3b | 12.7–157.5 |
| EAGLE | 8 | 49.6 ± 23.3ab | |||
| Extra fine grain | SOTRASEL | 12 | 356.4 ± 19.0d | 248.8c | 31.7–751.5 |
| SOCAPURSEL | 13 | 149.5 ± 18.3c | |||
| P value | 0.0002 | ||||
| F ratio | 62.9 | ||||
Values in the same column having the same superscripts are not significantly different from each other (p > 0.05).
From Table 1, there was the tendency for most salt producers to iodize fine and extra fine varieties more than the recommended range of 20–40 ppm iodine by (ICCIDD/UNICEF/WHO, 1996). However, apart from SOCAPURSEL that iodized coarse grain at 11.2 ppm most refineries tended to respect this recommendation for the cattle or coarse grain variety according to 26.9 ppm iodine value obtained. This coarse-grain or cattle salt is marketed in standard 18 kg sacks and is effectively largely used for animal consumption. This is by far the commonest variety in the popular markets of the countries of the Central African Sub-region, as it is also consumed by humans.
As far as “fine Table Salt” is concerned, destined almost exclusively for human consumption, the average iodation levels of 57.3 ppm is above the limits of 20–40 ppm iodine recommended by ICCIDD/UNICEF/WHO in 1996. The same is true for the very high average values of 248.8 ppm of industrial extra fine salt for specific uses. The consumption of these fine grain varieties that are iodized with no conformity to any regulation will result in excess iodine intake. The fact that local industries producing common popular food commodities like NESTLE and CHOCOCAM used it amongst the ingredients for their final products which children of urban centres consume very much, is a great reason for iodine excess especially in the major cities like Yaounde as observed above in median UIC values. Here, the children of urbanizing African cities are beginning to follow the nutrition path of children in some industrialized Countries. Though the latter supply iodine to the masses through common and popular food commodities (biscuits, milk, sweets, chocolates, condiments etc), they also ensure that everything is meted with adequate control. This control that checks iodine excess is yet to fully happen in our context.
From the technical point of view, it is quite praise-worthy that the major salt dealers are working hard to respect the iodized salt norms although they still suffer from some mechanical and technological lapses which call for external vigilance through periodic external quality assurance and control by competent inspection teams. It is believed that these lapses are being objectively identified through this manuscript for correction.
In addition, iodine content tends to rise with the fine-ness of the salt. Since table (fine) salt tends to be over-iodized, city dwellers need to be counseled to stop over-consuming table (fine) salt so as to reduce iodine excess. However, restaurant keepers need to be drafted into the National Coalition and taught the special nutritional value of iodized salt and the brand of choice. They can do a lot to both promote Universal Iodized Salt Consumption and help in reducing iodine excess since regular eating in restaurants is much in fashion for urban workers, many of whom are not aware of USI and excess iodization.
Table 2 shows the imported varieties at the Douala port. Cerebos salt from France that was found only during the first visit of the inspection team contained iodine at an average of 45.5 ppm within a range of 44.9–46.6 ppm slightly above the limits of 20–40 ppm iodine recommended by ICCIDD/UNICEF/WHO in 1996. The SSS salt from Senegal contained iodine at an average of 182.2 ppm with a range of 42.3–878.1 ppm, far above the limits of 20–40 ppm iodine recommended.
Table 2.
Imported salt varieties and iodine content.
| Salt brand | Count | Iodine content Parts per million (ppm) |
|
|---|---|---|---|
| Average | Range | ||
| Cerebos | 04 | 45.4a | 44.9–46.6 |
| SSS | 26 | 182.2a | 42.3–878.1 |
| P value | 0.0994 | ||
| F ratio | 2.91 | ||
Values in the same column having the same superscripts are not significantly different from each other (p > 0.05).
From the baseline value of 0.0 ppm iodine in kitchen salt (Table 3) and median UIC of 62.5 μg/L (Fig. 1), it now seems reasonable to state that the current rapid increase in UIC median value is due to excessive consumption of iodine coming from table (fine) grain salt and increased consumption of industrial products using extra fine grain salt as ingredients.
Table 3.
Household Salt samples and iodine content.
| Year of sample collection | Count | Iodine content Parts per million (ppm) |
|
|---|---|---|---|
| Average | Range | ||
| 1991 | - | 0.0a | 0.0–0.0 |
| 2007 | 185 | 47.3b | 2.1–163.9 |
| 2009 | 150 | 110.9d | 6.3–215.8 |
| 2010 | 118 | 63.7c | 2.1–126.9 |
| 2014 | 182 | 72.0c | 0.0–201.0 |
| 2017 | 151 | 72.4c | 1.1–201.0 |
| P value | 0.0004 | ||
| F ratio | 25.67 | ||
Values in the same column having the same superscripts are not significantly different from each other (p > 0.05).
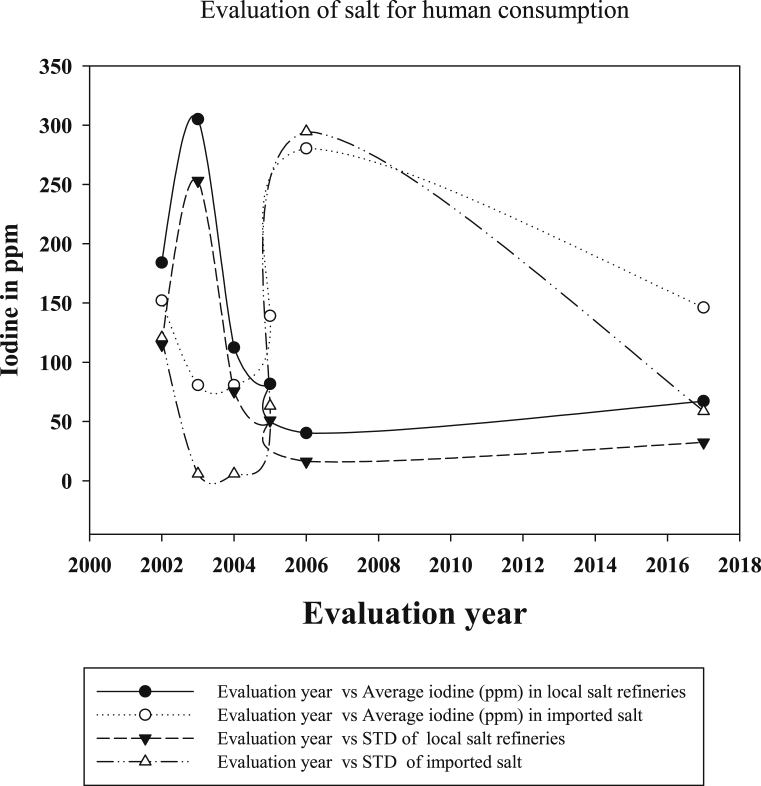
Fig. 2 shows average iodine in salt for human consumption in local refineries and imported varieties of salt. It is observed that during the years of consistent inspection, from 2002 – 2006, by the factory inspection team of the International Council for the Control of Iodine Deficiency Disorders (ICCIDD), impact was positive as average iodine in local refineries’ salt dropped, remaining virtually low up to 2017. The standard deviations (STDs) also behaved similarly, indicating that local refineries improved relatively in the iodization process. On the contrary, the average for imported salt remained high (though dropping slightly), far above the limits of 20–40 ppm iodine recommended by ICCIDD/UNICEF/WHO in 1996. However, the STDs of the imported salt are observed to drop drastically signifying a positive impact of the inspection team that provided IEC (information, Education and communication) booklets to the importers for knowledge transmission to foreign refineries in Senegal, the source of the imported SSS variety.
Fig. 2.
Evaluation year against average iodine in salt samples and their STDs.
Table 3 shows the averages of iodine in salt at household levels. It should be recalled that these samples were kitchen salt collected from children of ages 5–12 years with no information given as to the exact salt brand bought from the market by their mothers. Averages started from 0.0 ppm in 1991 to 47.3 ppm in 2007, peaked at 110.9 ppm in 2009, then dropped to 63.7 ppm in 2010 and increased slightly 72 ppm in 2014 and 2017 with statistical differences amongst the years (p = 0.0004). Though transportation or long storage induces deterioration or iodine loss as salt moves from the refineries to the hinterlands or cities far away from the refineries (Lantum, 1990–1995), the levels of iodine in household salt are still above acceptable levels. Apart from the baseline survey of 1991, where salt was not yet iodized, household salt samples averagely contained iodine above the limits of 20–40 ppm iodine recommended. High F-ratio (25.67) indicates great variation in iodine content of the salt samples.
It thus seems reasonable to state that UIC median iodine values are also skyrocketing due to increased consumption of imported salt that brings in more iodine to the household than is necessary. Importers do not have warehouse control units (laboratories) that can check the level of iodine in the tons of salt they import. There is need for collaboration with academia laboratories, the respect of legislation and ensuring continuous inspection at the port to salvage the situation. The current legislation at the ministry of public health that emphasizes 100 ppm for iodine in iodized salt is outdated and needs revision.
4. Conclusion
The study shows that there is adequate household coverage of iodized salt but there are lapses on iodization with consequence being high median urinary iodine concentration (UIC) value for the population.
The excessive iodine exposure cases are not clinically fatal but could be harmful. Hypothyroidism, hyperthyroidism and autoimmune thyroiditis occur in cases with more than adequate or excessive iodine level. The latter is unsafe especially for susceptible populations with recurring thyroid disease, the elderly, fetuses, and neonates and merits further investigation.
It appears quite recommendable that inspection teams should perpetuate their current periodic industrial visits to Iodized Salt Refineries and warehouses of salt importers ad infinitum besides pursuing the setting up of internal quality control laboratories by all refineries as a practical policy.
Declarations
Author contribution statement
Bonglaisin J.N., Ngondé E.M.C., Tsafack T.J.J., Lantum D.N.: Conceived and designed the experiments.
Ngo Nlend M.: Analyzed and interpreted the data; Wrote the paper. Mbakop C.D., Wirsiy E., Kimoun M.K., Ekambi M.A.: Performed the experiments.
Funding statement
This work was supported by Global Iodine Forum (formerly; International Council for the Control of Iodine Deficiency Disorders, ICCIDD) for field studies and the purchase of reagents used in the analyses, and UNICEF.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- Aburto J.N., Abudou M., Candeias V., Wu T. World Health Organization (WHO); 2014. Effect and Safety of Salt Iodization to Prevent Iodine Deficiency Disorders; S Systematic Review with Meta-Analyses. 2014. [Google Scholar]
- Angela M.L., Lewis E.B. Consequences of excess iodine. Nat. Rev. Endocrinol. 2014;10(3):136–142. doi: 10.1038/nrendo.2013.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coindet J.F. Nouvelles recherches sur les effets d'iode, et sur les précautions à suivre dans le traitement du goitre par ce nouveau remède. Ann. Chem. Phys. 1821;16:252–266. [Google Scholar]
- DeGroot J.D. 2016. Diagnosis and Treatment of Graves’Disease.https://www.ncbi.nlm.nih.gov/books/NBK285548/ access November 2018 at. [Google Scholar]
- Duncan B. Vol. 11. 1955. pp. 1–42. (New multiple range test biometrics). [Google Scholar]
- Ertek S., Cicero A.F. Hyperthyroidism and cardiovascular complications: a narrative review on the basis of pathophysiology. Arch Med. Sci. 2013;9(5):944–952. doi: 10.5114/aoms.2013.38685. 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fereia M., Gebremedhin S., Gebreegziabher T., Girma M., Stoecker B.J. Prevalence of iodine deficiency and associated factors among pregnant women in Ada district, Oromia region, Ethiopia: a cross- sectional study. BMC Pregnancy Childbirth. 2018;18:257. doi: 10.1186/s12884-018-1905-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hetzel B.S. second ed. Oxford Medical Publications; Great Britain: 1991. The Story of Iodine Deficiency; p. 3. [Google Scholar]
- ICCIDD/UNICEF/WHO . 1996. Taux Recommandés D’Iodation du Sel et Directives Pour la Surveillance de Leur Adéquation et de leur Efficacité. WHO/NUT/96.1.3. [Google Scholar]
- Karmarkar M.G., Pandav C.S., Krishnamachari K.A.V.R. Indian Council of Medical Research; New Delhi: 1986. Principle and Procedure for Iodine Estimation; A Laboratory Manual. [Google Scholar]
- Kirstie L., Symonds C. Severe Thyrotoxicosis Secondary to Povidone-Iodine from Peritoneal Dialysis. Case Rep. Endocrinol. 2017;2017 doi: 10.1155/2017/2683120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lantum D.N. 1991. Baseline survey of iodine deficiency disorders in Cameroon, National IDD Control: Series N 3. [Google Scholar]
- Lantum D.N. Action for eliminating iodine deficiency in central Africa. Public Health Triumph. 2011:31–58. [Google Scholar]
- Lantum D.N. 1999. «The conquest of iodine deficiency in Cameroon » in Biodiagnostics and Therapy, N 006, September 1999; pp. 20–24. [Google Scholar]
- Lantum D.N. 1990 -1995. Action towards Elimination of Iodine Deficiency Disorders (Cameroon) [Google Scholar]
- Martin A.W., Matthias B., Mirjam C.C., Steen J.B., John C., David S.C., Heiner C.B., Jan M.B., Beat M. Effects of antithyroid drugs on radioiodine treatment: systematic review and meta-analysis of randomised controlled trials. BMJ. 2007;334(7592):514. doi: 10.1136/bmj.39114.670150.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministère de Santé Publique . 2002. Evaluation de l’Impact de la Consommation du Sel Iodé sur la population Camerounaise. [Google Scholar]
- Rasmussen L.B., Ovesen L., Christiansen E. Day-to-day and within-day variation in urinary iodine excretion. Eur. J. Clin. Nutr. 1999;53:401–407. doi: 10.1038/sj.ejcn.1600762. [PubMed] [DOI] [PubMed] [Google Scholar]
- Steel R.G.D., Torrie H.H. McGraw-Hill Co. Inc.; New York: 1980. Principles and Procedures of Statistics. [Google Scholar]
- Stokes L., Tom B. American Statistical Association; 2004. What is a margin of error? What is a survey? Survey Research Methods Section; pp. 63–67.http://www.amstat.org/sections/srms/pamphlet.pdf [Google Scholar]
- Thaker V.V., Galler M.F., Marshall A.C., Almodovar M.C., Ho-Wen H., Addis C.J., Feldman A.H., Brown S.R., Levine B. Hypothyroidism in infants with congenital heart disease exposed to excess iodine. J Endocr Soc. 2017;1(8):1067–1078. doi: 10.1210/js.2017-00174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO/NHD/01.1 . second ed. 2001. Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination: A Guide for Programme Managers. [Google Scholar]
- WHO/UNICEF/ICCIDD . 2007. Assessment of the Iodine Deficiency Disorders and Monitoring Their Elimination. WHO/NHD/01.1.http://whqlibdoc.who.int/publications/2007/9789241595827eng.pdf [online] [Google Scholar]
- World Health Organization . third ed. 2007. Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination: A Guide for Programme Managers. [Google Scholar]
- World Health Organization . second ed. 2001. (WHO)/NHD/01.1 (2001) Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination A Guide for Programme Managers; pp. 69–70. [Google Scholar]