Abstract
Purpose
to analyze the radiological and functional outcomes of patients after surgical treatment of coronal plane fractures of femoral condyle using headless compression screw and cannulated cancellous (CC) screws (headed screws).
Material and method
In this prospective study 30 cases were included, out of which 15 were treated with headed screws and other 15 were treated with headless screws. Active knee mobilization exercises were started from the third postoperative day. Initially, patients were kept non-weight bearing; partial weight bearing was started at 10 weeks and progressed to full weight bearing as tolerated. Follow-up visits conducted at 2, 4 and 12 weeks, thereafter at 6 and 12 months. The long term final results were rated using Neer's rating system.
Results
Results were graded as excellent (score > 85), Satisfactory (score 71–85), Unsatisfactory (score 56–70), and Failure (score < 55). In CC screw group the outcome was good in 10 cases (66.66%) and poor in 5 cases (33.33%) whereas in headless group outcome was good in 13 cases (86.66%) and poor in 2 (13.33%)
Conclusion
fixation of Hoffa fracture with headless compression screw in comparison to CC screw (Headed Screw) have no significant difference in terms of functional outcome like range of motion but complications and implant failure is significantly higher in cases fixed with CC screw than in headless screw. So we conclude that overall outcome is better in study group fixed with headless compression screw as compared to cases fixed with CC Screw.
1. Introduction
Fractures of femoral condyle in coronal plane are commonly known as Hoffa fractures. Coronal plane fractures of femoral condyles first described by Hoffa in 1904,1 representing only 0.65% of all femoral fractures.2 Approximately 40% of intercondylar femoral fractures have associated Hoffa fragment, and are common in open fractures Nork et al.3 It is classified as a 33b3 according to AO/OTA classification. Letenneuret al in 1978, classified these fracture into 3 types depending on the distance of the fracture line from the posterior femoral cortex and its direction.3
Some authors like Butler et al. have postulated that the mechanism of injury is axial compression to the knee with the transmission of the ground reaction force through the tibial plateau to the femoral condyles while others like Ostermann et al. have attributed the fracture to simultaneous vertical shear and twisting forces.4, 5, 6 The main zones of weakness in the distal femur are (1) the transition from diaphysis to metaphysis, (2) the sagittal plane through the intercondylar notch, where the patella can act as a wedge and (3) the junction between the trochlear groove and medial or lateral condyle. Coronal splits in the condyles may also occur.
The diagnosis may be difficult to detect with routine radiographs and need a high grade of suspicion. Oblique radiographs are likely to best demonstrate the Hoffa fracture and should be added to routine AP and lateral views whenever there are equivocal findings or there is a high index of clinical suspicion. At times it may require a CT scan for diagnosis.
Conservative treatment consists of a femoral malleolar cast or a functional cast with the knee in moderate flexion. But, non operative management of these fractures generally results in poor outcomes, including malunion, non union and avascular necrosis.3,7 Therefore, open reduction and internal fixation is strongly recommended in the literature for all kinds of Hoffa fractures. Previous studies have shown many fixation means for Hoffa fractures, such as cancellous screw, Herbert screw, headless compression screw and cancellous screw with lateral buttress plate, etc.8, 9, 10, 11
In this study we tried to analyze the radiological and functional outcomes of patients after surgical treatment of coronal plane fractures of femoral condyle using headless compression screw and CC screws (headed screws).
2. Material and method
This was a prospective study conducted during January 2015 to June 2016 after approval by institutional ethical committee.
Our study included 30 cases, between the age group of 18–65 years, of coronal fracture of distal femoral condyle from accident and emergency department and outdoor department of Orthopaedics. We excluded patients with open physis (<18 years of age), pathological fractures, pre-existing arthritis compromising knee function and associated neurovascular injuries.
All skeletally matured patients with coronal fracture of distal femur were managed initially with groin to toe slab with standard post – fracture care and were planned for surgery.
Headless Compression screw of 6.5 mm or Cannulated cancellous screw made of stainless steel or titanium alloy was chosen to fix the fracture using principles of fracture fixation.
2.1. Preoperative planning
All patients assessed for general fitness to undergo surgery. Associated medical co-morbidities were dealt with if present. Routine pre-operative blood investigation, digital X-ray, and NCCT with 3D reconstruction of affected knee joint was done in all patients, which aided in surgical planning.
2.2. Surgical procedure
The surgical approach is typically dependent on the condylar involvement of the distal femur. For fixation of the coronal portions of the lateral condyle fracture, either a direct lateral or a lateral parapatellar approach is used; and visualization is aided by 20° of knee flexion. Similarly, for medial condyle coronal plane fractures, either a direct medial or medial parapatellar approach is used.
For fracture reduction, a pointed reduction clamp is placed in the antero-posterior plane to compress the fracture. The major fragments are temporarily fixed with Kirschner wires, followed by definitive fixation of the coronal plane fracture with 6.5 mm headless compression screws or cannulated cancellous screws. At least two screws were used to provide rotational stability. The screw insertion was performed in an anteroposterior or posteroanterior direction according to the surgeon's discretion. The cannulated cancellous screws were counter sunk below the articular cartilage surface. Screws were placed perpendicular to the fracture line with the maximal spread, as possible. A maximum possible screw length was used to optimize purchase. All the procedures were monitored by a C-arm to make sure no screw penetration into the articular cavity. The knee is manually ranged to assess overall knee stability and femorotibial gliding, and the overall construct and accuracy of the reduction are confirmed radiographically. Routine closure in layers over negative drains kept for 48 h was done. The tourniquet times ranged from 50 to 100 min Fig. 1, Fig. 2, Fig. 3.
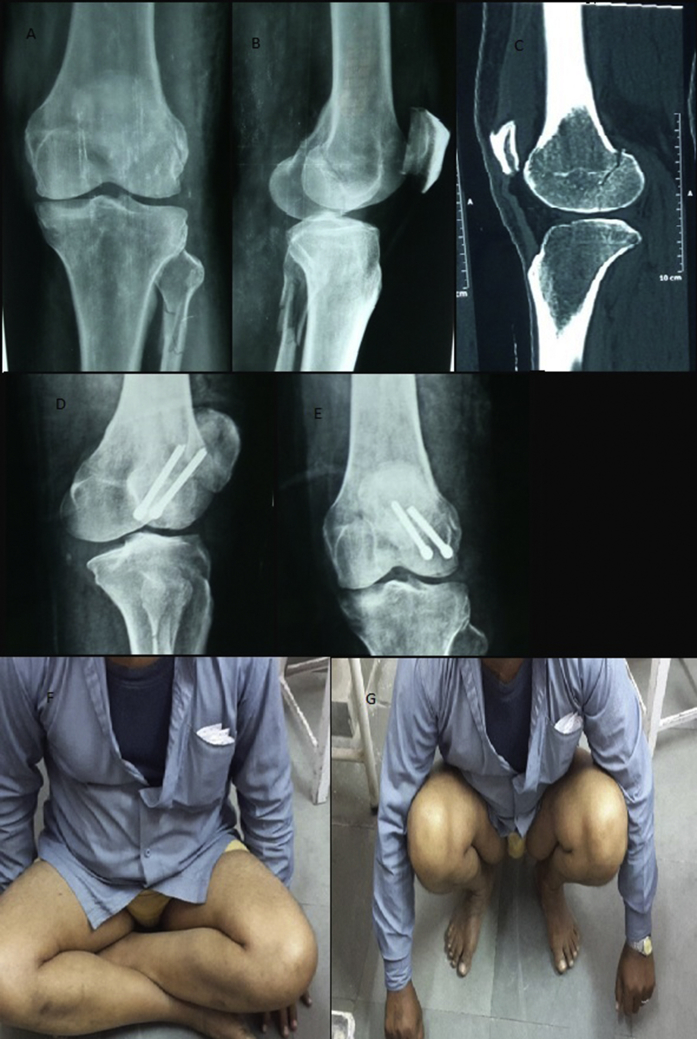
Fig. 1.
A 45 year Male present with complaints of pain, swelling, inability to bear weight on the right lower limb following slip & fall
A & B - Pre-operative X-ray AP and Lateral view
C - NCCT Right knee coronal section
D & E− Postoperative X-ray AP & Lateral View
F & G- Clinical photograph with crossed knee and flexed knee @ 6months.
Fig. 2.

A 34 year Male present with complaints of pain, swelling, inability to bear weight on the right lower limb following fall from height
A & B—Pre-Operative X-ray AP & Lateral View
C & D- Post-Operative X-ray Lateral & AP View
E- Clinical photograph with Flexed Knee @ 6months.
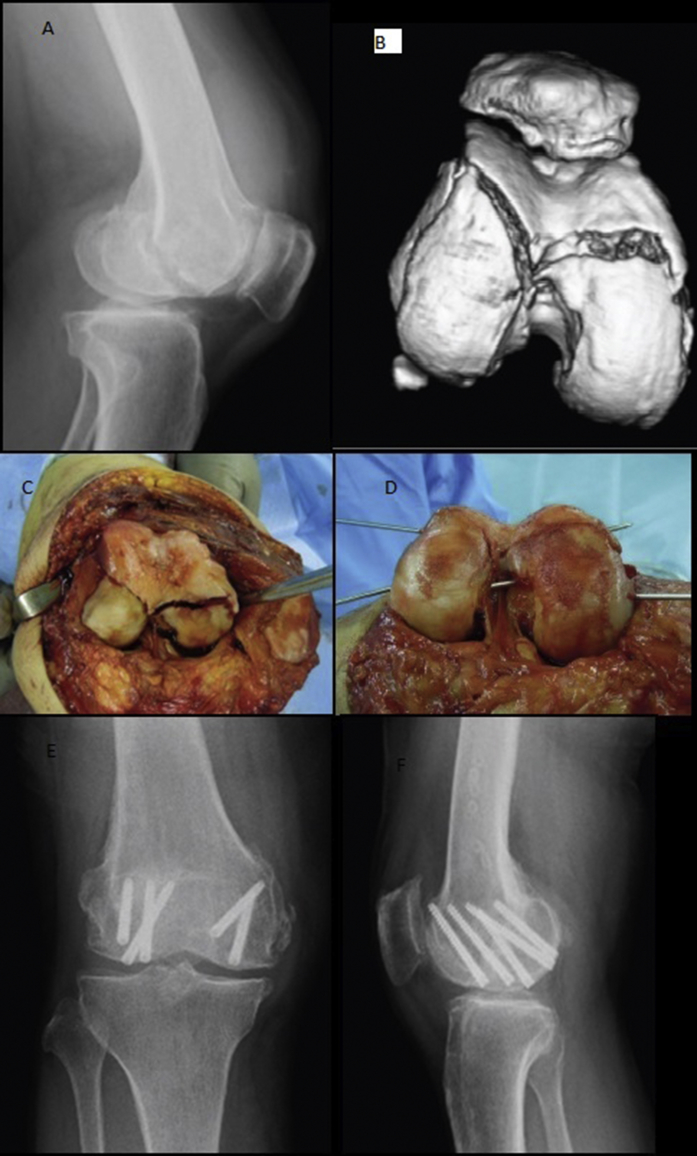
Fig. 3.
A 40 year Male present with complaints of pain, swelling, inability to bear weight on the left lower limb RTA
A- Initial posttraumatic lateral radiographs of the knee
B - A 3D reconstructed CT image of the femoral articular cartilage of the left knee, showing the bicondylar Hoffa fracture
C & D- Intraoperative photographs illustrating the exposure of the bicondylar Hoffa fracture through a lateral parapatellar arthrotomy and provision reduction with Kirschner wires
E & F— Anteroposterior (a) and lateral (b) radiographs obtained at the follow-up at 8 months after surgery.
2.3. Post-Operative
Post-operatively a posterior splint or articular split was applied for 2 days. For initial 48-h active toe movement and quadriceps strengthening exercises were done. Active knee mobilization exercises were started from the third postoperative day. Initially, patients were kept non-weight bearing; partial weight bearing was started at 10 weeks and progressed to full weight bearing as tolerated. Follow-up visits conducted at 2, 4 and 12 weeks, thereafter at 6 months. The long term final results were rated using Neer's rating system, which allots points for pain, function, working ability, joint movements, gross and radiological appearance.
3. Results
Out of 30 cases, 23 were male and 7 were female. (Male:Female: 3.29:1). Mean Age at time of surgery for CC Screw was 41.33 years and Headless Screw was 39.06 years. Most of the patients were between 21 and 40 years of age (60%). Right knee was involved in 11 cases (36.66%) & left knee was involved in 19 cases (63.33%). Lateral Condyle was involved in 25 cases (83.33%) while Medial Condyle involvement was in 4 cases (13.33%). One case had both the condyles involved.
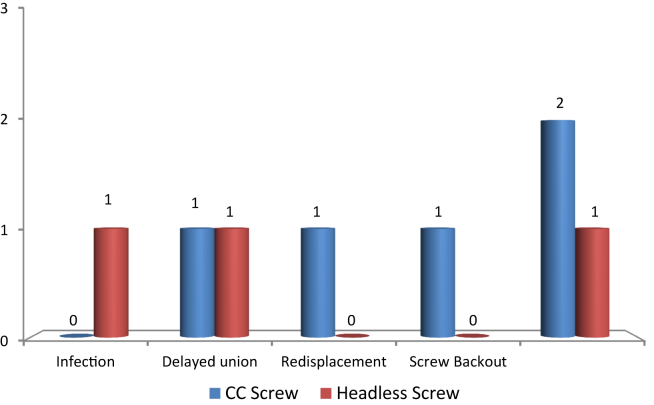
3 cases had superficial infection (2 cc screw and 1 headless screw) post op which were treated with higher antibiotics. Among headless screw group one patient had infection, one had delayed union and another one had stiff knee. Among CC screw group one patient had delayed union, one had redisplacement of fracture Fig. 4, another one had screw back out and two patients developed stiff knee Graph 1.
Fig. 4.
33 year Male present with complaints of pain, swelling, inability to bear weight on the left lower limb assault
A- Pre-Op X-ray Lateral View
B- Early Post-op X-ray Lateral View
C & d-Late Post-op X-ray AP & Lateral View showing redisplacement of fracture.
Graph 1.
Delayed Complications in headless and CC screw fixation.
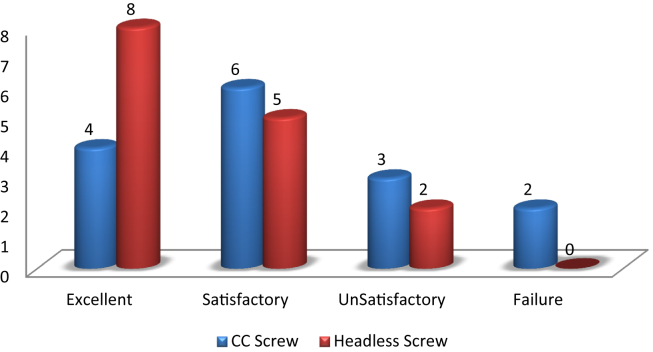
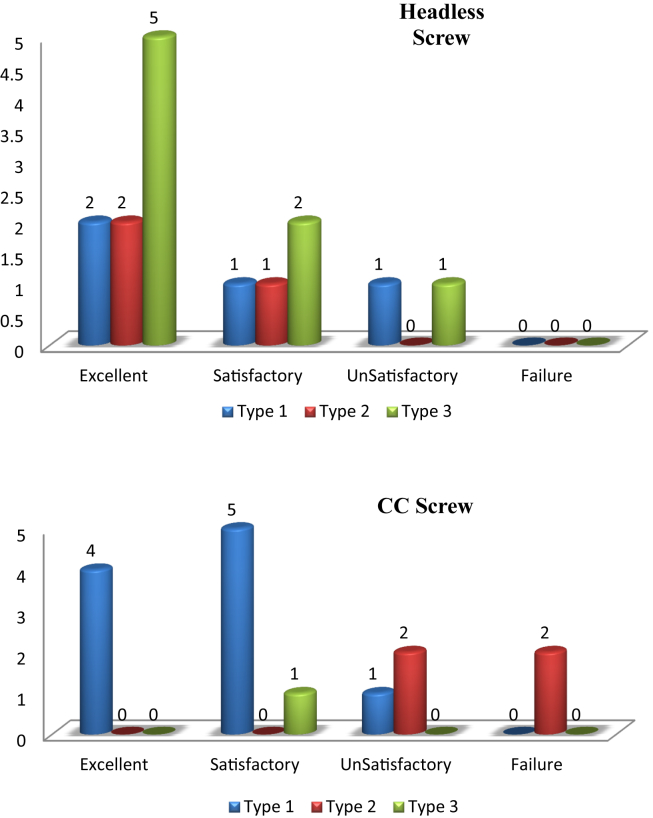
At the end of 6 months of follow up, the clinical outcome was rated as per the rating system of Neer et al. Results were graded as excellent (score > 85), Satisfactory (score 71–85), Unsatisfactory (score 56–70), and Failure (score < 55). In CC screw group the outcome was good in 10 cases (66.66%) and poor in 5 cases (33.33%) whereas in headless group outcome was good in 13 cases (86.66%) and poor in 2 (13.33%) Graph 2.
Graph 2.
Overall functional outcome according to fixation method.
As per Letenneuret classification, In type I out of 14 cases, 10 cases were fixed with CC screw and outcome was good in 9 cases and poor in 1 case. 4 cases were fixed with headless compression screw and outcome was good in 3 cases and poor in 1 case. In type II out of 7 cases, 4 cases were fixed with CC screw and all 4 cases had poor outcome. 3 cases fixed with headless compression screw and all 3 cases had good outcome. In type III out of 9 cases, 1 case was fixed with CC screw and had good outcome. 8 cases fixed with headless compression screw and outcome was good in 7 cases and poor in 1 case Graph 3.
Graph 3.
Overall functional outcome according to Letenneur classification & mode of fixation.
4. Discussion
‘Hoffa’ fractures are a rare entity and treatment methodologies are based on a few reports in the literature. These fractures are intra-articular and non-operative treatment can result in stiffness and poor joint function. Anatomical reduction is the goal and fixation is generally achieved using screws in varying configurations.
Hoffa fracture is usually overlooked or misdiagnosed. Firstly, it may be obscured by the intact part of the condyle on standard anteroposterior and lateral radiographs, particularly if the fracture is nondisplaced.12 So CT or MRI is recommended when patients have knee symptoms. Secondly, since the fracture usually results from high energy trauma, it is often associated with multiple injuries and may be easily overlooked or misdiagnosed at initial presentation.13 It has been reported that 25% Hoffa fractures associated with supracondylar femur fractures were not diagnosed in patients only with X-ray beam.14 And the consequence unfortunately are catastrophic: risk of displacement of the fracture fragments, nonunion and avascular necrosis.3
Coronal fractures of femoral condyle are unstable intraarticular fractures, and lateral Hoffa fractures are more common than medial ones (Ostermann et al., 1994; Nork et al., 2005; Biau and Schranz 2005).4,6,10 Bicondylar Hoffa fractures are rare (Papadopoulos et al., 2004).9 In our study, involvement of lateral condyle (83.33%) was more common than medial condyle (13.33%) with only one case of bicondylar involvement, which is comparable to the literature.
Hoffa fractures are seen in the setting of high velocity, high energy trauma. Four of five patients with isolated Hoffa fractures in one series were involved in motor vehicle accidents Holmes et al.8 In another series, five of seven fractures were sustained in motor vehicle accidents, while a sixth involved a pedestrian hit by a car Lewis Sl et al.15 In a large retrospective review of intra-articular distal femoral fractures performed at a large level 1 trauma center, a Hoffa fracture was an associated injury in 77 of 202 supracondylar-intercondylar distal femoral fractures. Of these 77 fractures, 62 were seen in the setting of motor vehicle trauma Nork SE et al.4 A fall from a height appears to be the next most common scenario. As in the literature, in our study also the majority of cases were reported with history of road traffic accident (73.33%) followed by fall from height (16.66%) then Slip & Fall (6.66%). The mechanism of injury of Hoffa fracture is still unknown. Some authors consider direct impact with the knee in a flexed position as the mechanism of injury, while others think that the fracture is caused by simultaneous vertical shear and twisting forces (Lewis et al., 1989; Papadopoulos et al., 2004).9,15
Although patients in past were managed conservatively with knee bracing and protected weight-bearing, loss of anatomic alignment of non-displaced Hoffa fractures treated with non-operative management exclusively is well-described. This was the case in 3 of 7 patients in one series Lewis et al.,15 and one of five patients in another Holmes et al.8 The remainder of the fractures in each of these two series were treated operatively. So they recommended internal fixation in all cases of coronal fracture of femoral condyle. Hoffa fractures are intraarticular fractures. Most of them need surgical open reduction and internal fixation to achieve good outcome (Lewis et al., 1989; McDonough and Bernstein 2000; Manfredini et al., 2001).2,12,15 But the operation approach and fixation method are still been improving. It is generally accepted that screw fixation is a good fixation method for treating Hoffa fractures.
A midline incision with a medial/lateral parapatellar arthrotomy is the most common approach reported Holmes et al.8 Direct lateral approach with or without osteotomy of the Gerdy tubercle and posterior-based approaches have also been described Liebergall et al.16 We have done cases from direct lateral, direct medial & medial/lateral parapatellar approach and we feel that the midline parapatellar arthrotomy is reproducible, provides good access even on the posterolateral aspect and is familiar to all surgeons with the advent of total knee replacement.
Although some minimal access techniques have been reported recently, such as arthroscopy-assisted reduction and fixation Bansal et al., McCarthy et al.,17,18 open approaches are still preferable for Hoffa fractures for the following reasons: (1) chances of displacement after initial evaluation is possible and subtle displacements may not be appreciated intraoperatively, (2) assessment of fracture reduction with conventional fluoroscopy is difficult and (3) assessment of optimal screw length without intra-articular penetration is best done under vision.
The choice of fixation implants was determined by bone stock, bone quality, reduction stability, and implant capacity. However, there remains no consensus on the optimal form of internal fixation. Previous studies have shown many fixation means for Hoffa fracture, such as cancellous screw, Herbert screw, headless compression screw and cancellous screw with lateral buttress plate, etc.9−11Cancellous screw hardly get adequate compression. In addition, it will take more surgical time to countersink screw head. However, headless compression screw is self-compression and can be positioned beneath the outer cortex, which prevents irritation of soft tissue and does not need an additional procedure to countersink screw head. Herbert screws generate lower fragment compression than headless compression screws Baran et al.19.Our study was designed to compare the fixation of coronal fracture of femoral condyle with Headless compression screw & Headed screw.
For the direction of the screw, Jarit et al.20 showed that Hoffa fracture fixed with screws in a PA direction would be more stable than AP direction, but in our series, there was no significant difference between them. In our opinion, two screws perpendicular to the fracture line are beneficial not only for compression but also for rotational stability. And the direction of the screw should depend on the fracture type. There was no difference between PA and AP direction for type I and type III Hoffa fractures because of the big size of the distal fragment, but it is preferable to choose PA direction during fixation of type II Hoffa fracture.3
In our study there was no significant difference in the range of motion achieved by either CC screw (Headed Screw) or Headless screw but the results show slightly better results with Headless screw as compared to CC screw. Moreover complications like screw backout, fracture redisplacement were seen in cases fixed with CC screw, no such complication was seen with headless screw and the follow-up results showed that there were no obvious articular defects caused by headless screw. Fixation of Letennuer type 2 fracture with CC Screw gave unfavorable results whereas results with headless screw were good in Letennuer type 2 fracture. The difference of the risk of osteoarthritis between these two methods needs a long-term follow-up.
The limitation of this study is a small group of patients under evaluation and short duration of follow-up, so the findings need to be further validated with a study on large group of cases with long-term follow-up.
5. Conclusion
We found that fixation of Hoffa fracture with headless compression screw in comparison to CC screw (Headed Screw) have no significant difference in terms of functional outcome like range of motion but complications and implant failure is significantly higher in cases fixed with CC screw than in headless screw. So we conclude that overall outcome is better in study group fixed with headless compression screw as compared to cases fixed with CC Screw.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2018.10.011.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Hoffa A. fourth ed. Ferdinand Enke-Verlag; Stuttgart: 1904. Lehrbuch der Frakturen und Luxationen. [Google Scholar]
- 2.Manfredini M., Gildone A., Ferrante R., Bernasconi S., Massari L. Unicondylar femoral fractures : therapeutic strategy and long term results. A review of 23 patients. Acta Orthop Belg. 2001;67(2):132–138. [PubMed] [Google Scholar]
- 3.Letenneur J., Labour P.R., Rogez J.M., Lignon J., Bainvel J.V. Fractures de Hoffa: a propos de observations. Ann Chir. 1978;32 213—9 (Eng. Absr.) [PubMed] [Google Scholar]
- 4.Nork S.E., Segina D.N., Aflatoon K. The association between supracondylar- intercondylar distal femoral fractures and coronal plane fractures. J Bone Joint Surg Am. 2005;87(3):564–569. doi: 10.2106/JBJS.D.01751. [DOI] [PubMed] [Google Scholar]
- 5.Butler M.S., Brumback R.J., Ellison T.S., Poka A., Bathon G.H., Burgess A.R. Interlocking intramedullary nailing for ipsilateral fractures of the femoral shaft and distal part of the femur. J Bone Joint Surg Am. 1991;73:1492–1502. [PubMed] [Google Scholar]
- 6.Ostermann P.A., Neumann K., Ekkernkamp A., Muhr G. Long term results ofunicondylar fractures of the femur. J Orthop Trauma. 1994;8:142–146. doi: 10.1097/00005131-199404000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Hak D.J., Nguyen J., Curtiss S., Hazelwood S. Coronal fractures of the distal femoral condyle: a biomechanical evaluation of four internal fixation constructs. Injury. 2005;36(9):1103–1106. doi: 10.1016/j.injury.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 8.Holmes S.M., Bomback D., Baumgaertner M.R. Coronalfractures of the femoral condyle: a brief report of five cases. J Orthop Trauma. 2004;18(5):316–319. doi: 10.1097/00005131-200405000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Papadopoulos A.X., Panagopoulos A., Karageorgos A., Tyllianakis M. Operative treatment of unilateral bicondylar Hoffa fractures. J Orthop Trauma. 2004;18(2):119–122. doi: 10.1097/00005131-200402000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Biau D.J., Schranz P.J. Transverse Hoffa's or deep osteochondralfracture? An unusual fracture of the lateral femoralcondyle in a child. Injury. 2005;36(7):862–865. doi: 10.1016/j.injury.2004.11.028. [DOI] [PubMed] [Google Scholar]
- 11.Chang J.J., Fan J.C., Lam H.Y., Cheung K.Y., Chu V.W., Fung K.Y. Treatment of an osteoporotic Hoffa fracture. Knee Surg Sports Traumatol Arthrosc. 2010;18(6):784–786. doi: 10.1007/s00167-009-0960-4. [DOI] [PubMed] [Google Scholar]
- 12.McDonough P.W., Bernstein R.M. Nonunion of a hoffafracture in a child. JOrthop Trauma. 2000;14(7):519–521. doi: 10.1097/00005131-200009000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Thakar C. The Hoffa fracture—a fracture not to miss. Emerg Med J. 2010;27(5):391–392. doi: 10.1136/emj.2009.087213. [DOI] [PubMed] [Google Scholar]
- 14.Baker B.J., Escobedo E.M., Nork S.E., Henley M.B. Hoffa fracture:a common association with high-energy supracondylar fracturesof the distal femur. AJR Am J Roentgenol. 2002;178(4):994. doi: 10.2214/ajr.178.4.1780994. [DOI] [PubMed] [Google Scholar]
- 15.Lewis S.L., Pozo J.L., Muirhead-Allwood W.F.G. Coronal fractures of the lateral femoral condyle. J Bone Joint Surg Br. 1989;71 doi: 10.1302/0301-620X.71B1.2914979. 118—20. [DOI] [PubMed] [Google Scholar]
- 16.Liebergall M., Wilber J.H., Mosheiff R., Segal D. Gerdy’stubercle osteotomy forthetreatment of coronal fractures of the lateral femoral condyle. J Orthop Trauma. 2000;14:214–215. doi: 10.1097/00005131-200003000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Lal H., Bansal P., Khare R., Mittal D. Conjoint bicondylar Hoffa fracture in a child: a rare variant treated by minimally invasive approach. J Orthop Trauma. 2011;12(2):111–114. doi: 10.1007/s10195-011-0133-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCarthy J.J., Parker R.D. Arthroscopic reduction and internal fixation of a displaced intraarticular lateral femoral condyle fracture of the knee. Arthroscopy. 1996;12(2):224–227. doi: 10.1016/s0749-8063(96)90016-x. [DOI] [PubMed] [Google Scholar]
- 19.Baran O., Sagol E., Oxaz H., Sarikanat M., Havitcioglu H. A biomechanical study on preloaded compression effect on headless screws. Arch Orthop Trauma Surg. 2009;129(12):1601–1605. doi: 10.1007/s00402-009-0971-0. [DOI] [PubMed] [Google Scholar]
- 20.Jarit G.J., Kummer F.J., Gibber M.J., Egol K.A. A mechanical evaluation of two fixation methods using cancellous screws for coronal fractures of the lateral condyle of the distal femur (OTA type 33B) J Orthop Trauma. 2006;20(4):273–276. doi: 10.1097/00005131-200604000-00007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.