Abstract
Background
The ongoing global SARS-CoV-2 pandemic has caused over 4.7 million infections greatly challenging healthcare workers (HCW) and medical institutions worldwide. The SARS-CoV-2 pandemic has shown to significantly impact mental and physical health of HCW. Thus, implementation of testing facilities supporting HCW are urgently needed.
Methods
A low-threshold SARS-CoV-2 testing facility was introduced at the University Hospital Bonn, Germany, in March 2020. Irrespective of clinical symptoms employees were offered a voluntary and free SARS-CoV-2 test. Furthermore, employees returning from SARS-CoV-2 risk regions and employees after risk contact with SARS-CoV-2 infected patients or employees were tested for SARS-CoV-2 infection. Pharyngeal swabs were taken and reverse transcription polymerase chain reaction for detection of SARS-CoV-2 was performed, test results being available within 24 h. Profession, symptoms and reason for SARS-CoV-2 testing of employees were recorded.
Results
Between 9th March and April 30, 2020, a total of 1510 employees were tested for SARS-CoV-2 infection. 1185 employees took advantage of the low-threshold testing facility. One percent (n = 11) were tested positive for SARS-CoV-2 infection, 18% being asymptomatic, 36% showing mild and 36% moderate/severe symptoms (missing 10%). Furthermore, of 56 employees returning from SARS-CoV-2 risk regions, 18% (10/56) were tested SARS-CoV-2 positive. After risk contact tracking by the hospital hygiene 6 patient-to-employee transmissions were identified in 163 employees with contact to 55 SARS-CoV-2 positive patients.
Conclusion
In the absence of easily accessible public SARS-CoV-2 testing facilities low-threshold SARS-CoV-2 testing facilities in hospitals with rapid testing resources help to identify SARS-CoV-2 infected employees with absent or mild symptoms, thus stopping the spread of infection in vulnerable hospital environments. High levels of professional infection prevention training and implementation of specialized wards as well as a perfectly working hospital hygiene network identifying and tracking risk contacts are of great importance in a pandemic setting.
Keywords: SARS-CoV-2, COVID-19, Healthcare workers
Highlights
-
•
Incidence of SARS-CoV-2 infections are higher in employees of a hospital environment compared to the general population.
-
•
Low-threshold testing facility helps to identify SARS-CoV-2 positive employees with absent or mild clinical symptoms.
-
•
Tracking of risk contacts by the hospital hygiene prevent distribution of SARS-CoV-2 infection.
1. Introduction
In 2019 the World Health Organization (WHO) named high-threat pathogens as one of the world's top ten global health threats. The SARS-CoV-2 outbreak has caused a global pandemic with over 4.7 million cases around the world by the mid of May 2020, bringing great challenges to medical institutions and clinical staff worldwide (https://coronavirus.jhu.edu/map.html). This global major public health event is threatening people's physical and mental health as well as life safety. High levels of training and professional experience, resilience and social support has been shown to impact mental health during this pandemic (Cai et al., 2020).
During the ongoing outbreak of SARS-CoV-2 in Wuhan, China, hospitals were significant epicenters for human-to-human transmission of SARS-CoV-2 in healthcare workers (HCW), patients and visitors (Ye et al., 2020). Thus, adequate environmental cleaning, strengthening of professional infection prevention training and improvement of infection prevention among HCW are urgently needed.
The aim of this study was to evaluate, whether offering a free, voluntary low-threshold testing for all hospital staff may help to manage SARS-CoV-2 infections in medical institutions and prevent subsequent virus outbreaks.
2. Methods
In the absence of an easily accessible public SARS-CoV-2 testing facility a low-threshold testing facility was started at the University Hospital Bonn, Germany, on March 9, 2020. All persons employed by the University Hospital Bonn got the opportunity of voluntary and free SARS-CoV-2 testing using pharyngeal swabs irrespective of current clinical symptoms. Pharyngeal swabs were analyzed for SARS-CoV-2 using reverse transcription polymerase chain reaction (RT-PCR) (Corman et al., 2020) and test results were available within 24 hours. Mild symptoms were defined as sore throat, fatigue, and light cough, moderate/severe symptoms as fever, severe cough, loss of smell/taste and myalgia. Employees with clinical symptoms (mild and moderate/severe) received a doctor's note and could not return back to work before they were tested negative for SARS-CoV-2. SARS-CoV-2 testing was also provided for employees returning from regions declared as SARS-CoV-2 risk regions by the German federal government agency and research institute responsible for disease control and prevention in Germany (Robert Koch Institute (RKI), Berlin, Germany), either during their stay or shortly after their return (www.rki.de/covid-19-risikogebiete). The RKI continuously updated information on SARS-CoV-2 risk regions, which were regularly implemented on the University Hospital internal website. Furthermore, employees received SARS-CoV-2 testing after risk contacts with SARS-CoV-2 positive patients or colleagues identified by the hospital hygiene irrespective of clinical symptoms. Risk assessment after SARS-CoV-2 contact was conducted by the hospital hygiene applying equally for employee-to-employee and patient-to-employee risk contact. Employees were categorized according to type and time of exposure to COVID-19 contact depending on personal protective equipment and were informed personally by the hospital hygiene if there was any risk of SARS-CoV-2 infection when applying the current RKI risk contact definitions. Importantly, in close cooperation with the Institute of Virology of the University Bonn, test results were available within 24 h after sampling.
Employees after return from SARS-CoV-2 risk regions or with private or clinical SARS-CoV-2 risk contacts stayed in domestic quarantine for 14 days. Only when there was staffing shortage critical for the hospital infrastructure employees were allowed to return back to work after one negative test, being asymptomatic, wearing a mask, leading a 7-day temperature log and repeating the test after 7 days. Serial examinations were carried out in SARS-CoV-2 positive employees, who could return back to work after 2 negative SARS-CoV-2 tests in order to minimize the risk of false-negative results. A similar approach was chosen for COVID-19 patients, who stayed in isolation until 2 negative SARS-CoV-2 results were obtained.
Employees were categorized according to their profession as group I with direct contact to patients, e.g. nurses, doctors, allied health professionals, porters etc., group II with a non-patient facing profession but potentially at higher risk of nosocomial exposure, e.g. domestic and laboratory staff, group III working non-clinical, e.g. jobs in the hospital administration and information technology, secretarial jobs etc. (Hunter et al., 2020). Irrespective of their profession group IV was defined as employees returning from high risk regions according to the guidelines of the RKI.
This study was approved by the local ethics committee (No. 188/20).
3. Results
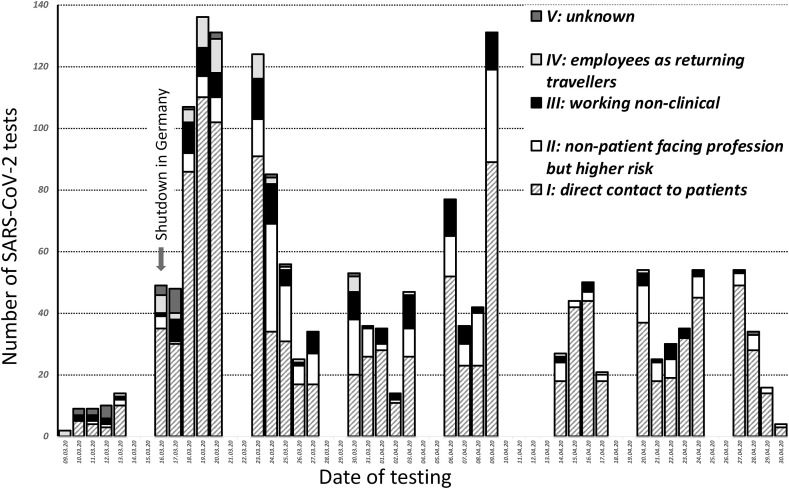
Between March 9, 2020 and April 30, 2020, 1726 pharyngeal swabs from 1510 employees of the University Hospital Bonn were tested for SARS-CoV-2 infection, thereof 1013 (67%) were women and 497 (33%) were men and the median age was 37 years (IQR 29; 51). Of a total of 7460 employees of the University Hospital Bonn 16% (n = 1185) took advantage of the low-threshold testing facility, 56 (0.8%) were tested after returning from SARS-CoV-2 high risk regions and 269 (3.6%) were tested after risk contacts with SARS-CoV-2 positive patients or infected employees. Fig. 1 shows the frequency of testing during the observation period according to profession. After the shutdown in Germany on March 16, 2020 the frequency of testing accelerated and slowed during the following week and peaked again before Easter.
Fig. 1.
Number of SARS-CoV-2 swabs taken in the low-threshold screening facility between 9th March and 30th April (I: direct contact to patients, II: non-patient facing profession but potentially at higher risk of nosocomial exposure, III: working non-clinical, IV: employees as returning travellers, V: unknown).
The low-threshold facility was used by 1185 employees, the majority of whom belonged to group I with direct patient contact (66%). Only 21% belonged to group II with a non-patient facing profession and 12% to group III, who worked non-clinical (missing for n = 15). They received a SARS-CoV-2 test without having symptoms in 36% (n = 425), experiencing mild symptoms in 44% (n = 515), suffering of moderate/severe symptoms in 7% (n = 77) (missing in 14% (n = 168)).
Out of these 1185 employees 11 (1%) were tested positive for SARS-CoV-2. Sixty-four percent (n = 7) were women and the median age was 32 (IQR 31; 46). The majority of the 11 SARS-CoV-2 positive employees belonged to group I (n = 7) having direct contact to patients, only one was assigned to group II and 3 to group III. Importantly, 54% had no (n = 2) or mild (n = 4) symptoms, while 36% (n = 4) had moderate/severe symptoms (information missing in n = 1).
In 9 of these 11 SARS-CoV-2 positive tested individuals 133 risk contact persons were identified by the hospital hygiene. One employee-to-employee transmission was diagnosed by the contact tracing, however no further transmission was found in the subsequent 9 identified risk contacts. The remaining 2 (2/11) SARS-CoV-2 positive tested employees had no risk contacts in hospital as they were away on leave.
Fifty-six (0.8%) of all employees were tested as returning travelers from regions declared as SARS-CoV-2 risk regions by the RKI. As it was skiing season in Europe individuals mostly returned from Austria (n = 33). As many as 18% (10/56) of these individuals tested positive for SARS-CoV-2 returning from Austria (n = 8), Spain (n = 1) and Switzerland (n = 1), the majority (90%) of them belonging to group I with direct contact to patients. Two employees had already returned back to work, when the regions they had returned from were announced as SARS-CoV-2 risk region. The hospital hygiene identified 40 contact persons from the hospital staff, but no transmission was detected.
The hospital hygiene further informed employees after identifying risk contacts either with SARS-CoV-2 positive patients or with employees tested positive for SARS-CoV-2 in an external laboratory. For 55 SARS-CoV-2 positive patients 163 risk contact persons were identified with up to 9 risk contacts per individual. As much as 6 patient-to-employee transmissions were identified. Of note, 2 transmissions occurred in contact with a patient whose quarantine had been finished due to a false negative SARS-CoV-2 result. The other patient-to-employee transmissions occurred outside the COVID-19 specialized wards. Four of the 6 transmissions occurred in employees-in-training. Subsequently, 60 risk contact persons were identified by the hospital hygiene and one employee-to-employee transmission was detected. Here, no subsequent additional risk contact persons were identified.
Five employees tested SARS-CoV-2 positive outside the hospital SARS-CoV-2 testing facility lead to identification of 128 risk contacts of employees and thus one employee-to-employee transmission was detected. There was no further transmission in the subsequent 37 risk contacts identified by the hospital hygiene.
All 30 SARS-CoV-2 positive employees tested positive in the hospital testing facility were followed up and SARS-CoV-2 RT-PCR remained positive for a median time of 16.5 days (IQR 14; 22), the maximum time of SARS-CoV-2 RT-PCR being positive was 35 days. In 21/30 (70%) SARS-CoV-2 RT-PCR was still positive 14 days after first SARS-CoV-2 detection.
4. Discussion
In the beginning of the COVID-19 pandemic an easily accessible public SARS-CoV-2 testing was not available. Thus, the low-threshold testing facility was introduced to provide a free and voluntary SARS-CoV-2 testing opportunity for the employees of the University Hospital Bonn. Importantly, positive SARS-CoV-2 test results were not linked with mandatory leave. Thus, as much as 16% of employees of the University Hospital Bonn were tested for SARS-CoV-2 infection in the observation period of 53 days.
Of these employees 1% were tested positive for SARS-CoV-2. This was 10 times higher compared to the cumulative incidence of SARS-CoV-2 infections during this time period in Bonn (199/100,000). Importantly, 64% of these employees had missing or mild symptoms, strengthening the significance of a low-threshold SARS-CoV-2 testing facility in a hospital setting. The high prevalence of SARS-CoV-2 positive individuals with missing or mild symptoms has also been shown in previous studies (Streeck et al., 2020).
Working in a medical institution during times of global pandemics threatening millions of lives worldwide is not only physical but also mental stress for HCW (Ives et al., 2009). It has been shown that besides professional experience also social support is desperately needed to handle a pandemic situation in a medical institution (Holmes et al., 2020). The majority (80%) of the 1185 employees taking advantage of the voluntary low-threshold testing facility had missing or mild symptoms. Providing a test opportunity, where test results are available within 24 h not only supports HCW in fear of SARS-CoV-2 infection psychologically, but also enables HCW to return back to work more rapidly in times of critical human resource planning (Chowell and Mizumoto, 2020).
The high percentage (18%) of employees with a positive SARS-CoV-2 test result returning from risk countries emphasizes the importance of tracking the current development of the SARS-CoV-2 infection rate not only countrywide but also region specific. Regarding the re-opening of boarders and increasing geographical mobility our data suggests that testing individuals returning from regions in- and outside of Germany with higher numbers of SARS-CoV-2 infections can prevent outbreaks in vulnerable surroundings such as medical institutions. As clinical symptoms are often mild or absent in SARS-CoV-2 positive individuals epidemiological data on spread of SARS-CoV-2 must lead decisions on screening politics.
The number of SARS-CoV-2 testing has decreased over time in the testing facility in parallel with the decline of the reproduction rate of SARS-CoV-2 in Germany, which had reached R = 3 beginning of March and stabilizing around R = 1 since the 22nd of March (Seedat, 2020).
In total 3 clusters of patient-to-employee transmission appeared over the observation period leading to 6 infected HCW. Identifying and screening the risk contacts of these HCW led to identification of one employee-to-employee SARS-CoV-2 infection thereby preventing the further spread of this SARS-CoV-2 cluster. Importantly, 2 of 3 clusters occurred on non-COVID-19 specialized wards emphasizing the importance of high levels of training and professional experience in pandemic settings. The third cluster occurred after false termination of quarantine most probably due to a poor specimen collection and thus false negative SARS-CoV-2 swab results further underlining the need for specialized training of all HCW involved. Four of these 6 patient-to-employee transmissions occurred in HCW in training, further stressing the necessity of professional training (Pung et al., 2020).
One cluster occurred after an employee was tested positive for SARS-CoV-2 outside our testing facility. Tracking of risk contacts and his place of employment by the hospital hygiene in the University Hospital, lead to identification of one employee-to-employee transmission, followed by intervention measures interrupting successfully further spread of infection. All cases of clusters of patient-to-employee and employee-to-employee transmission highlight the great importance of a perfectly working hospital hygiene network identifying risk contacts fast and receiving SARS-CoV-2 test results rapidly in order to interrupt further spread of infection (Rivett et al., 2020; Wee et al., 2020).
Our study has limitations. Clusters of employee-to-employee and patient-to-employee transmission were defined after risk contact assessment by the hospital hygiene. Further genomic analysis of SARS-CoV-2, however, was not performed to directly confirm these transmission clusters.
5. Conclusions
Incidence of SARS-CoV-2 infections in employees of a hospital are shown to be higher compared to the general population. Thus, offering a low-threshold SARS-CoV-2 testing facility in the absence of an easily accessible public testing facility identifies SARS-CoV-2 positive employees with absent or mild clinical symptoms of infection, thereby stopping further spread of infection in a vulnerable hospital environment. A perfectly working hospital hygiene network tracking risk contacts and high levels of professional infection prevention training are important factors to prevent continuous distribution of SARS-CoV-2 infection.
Funding
None.
Declaration of competing interest
None to declare.
References
- Cai W., Lian B., Song X., Hou T., Deng G., Li H. A cross-sectional study on mental health among health care workers during the outbreak of Corona Virus Disease 2019. Asian J Psychiatr. 2020;51:102111. doi: 10.1016/j.ajp.2020.102111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowell G., Mizumoto K. The COVID-19 pandemic in the USA: what might we expect? Lancet. 2020;395:1093–1094. doi: 10.1016/S0140-6736(20)30743-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corman V.M., Landt O., Kaiser M., Molenkamp R., Meijer A., Chu D.K., Bleicker T., Brünink S., Schneider J., Schmidt M.L., Mulders D.G., Haagmans B.L., van der Veer B., van den Brink S., Wijsman L., Goderski G., Romette J.-L., Ellis J., Zambon M., Peiris M., Goossens H., Reusken C., Koopmans M.P., Drosten C. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25:2431. doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatr. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter E., Price D.A., Murphy E., van der Loeff I.S., Baker K.F., Lendrem D., Lendrem C., Schmid M.L., Pareja-Cebrian L., Welch A., Payne B.A.I., Duncan C.J.A. First experience of COVID-19 screening of health-care workers in England. Lancet. 2020;395:e77–e78. doi: 10.1016/S0140-6736(20)30970-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ives J., Greenfield S., Parry J.M., Draper H., Gratus C., Petts J.I., Sorell T., Wilson S. Healthcare workers' attitudes to working during pandemic influenza: a qualitative study. BMC Publ. Health. 2009;9 doi: 10.1186/1471-2458-9-56. 56–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pung R., Chiew C.J., Young B.E., Chin S., Chen M.I.-C., Clapham H.E., Cook A.R., Maurer-Stroh S., Toh M.P.H.S., Poh C., Low M., Lum J., Koh V.T.J., Mak T.M., Cui L., Lin R.V.T.P., Heng D., Leo Y.-S., Lye D.C., Lee V.J.M., Singapore 2019 Novel Coronavirus Outbreak Research Team Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet. 2020;395:1039–1046. doi: 10.1016/S0140-6736(20)30528-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivett L., Sridhar S., Sparkes D., Routledge M., Jones N.K., Forrest S., Young J., Pereira-Dias J., Hamilton W.L., Ferris M., Torok M.E., Meredith L., Citiid-Nihr Covid-19 BioResource Collaboration, Curran M.D., Fuller S., Chaudhry A., Shaw A., Samworth R.J., Bradley J.R., Dougan G., Smith K.G.C., Lehner P.J., Matheson N.J., Wright G., Goodfellow I.G., Baker S., Weekes M.P. Screening of healthcare workers for SARS-CoV-2 highlights the role of asymptomatic carriage in COVID-19 transmission. Elife. 2020;9 doi: 10.7554/eLife.58728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seedat J. Epidemiologisches bulletin 17/2020. Epidemiol. Bull. 2020;17:17. doi: 10.25646/6811. 2020. [DOI] [Google Scholar]
- Streeck H., Schulte B., Kümmerer B., Richter E., Höller T., Fuhrmann C., Bartok E., Dolscheid R., Berger M., Wessendorf L., Eschbach-Bludau M., Kellings A., Schwaiger A., Coenen M., Hoffmann P., Stoffel-Wagner B., Nöthen M., Eis-Hübinger A.-M., Exner M., Schmithausen R., Schmid M., Hartmann G. Infection fatality rate of SARS-CoV-2 infection in a German community with a super-spreading event. 2020. [DOI] [PMC free article] [PubMed]
- Wee L.E., Sim J.X.Y., Conceicao E.P., Aung M.K., Goh J.Q., Yeo D.W.T., Gan W.H., Chua Y.Y., Wijaya L., Tan T.T., Tan B.H., Ling M.L., Venkatachalam I. Containment of COVID-19 cases amongst healthcare workers: the role of surveillance, early detection and outbreak management. Infect. Control Hosp. Epidemiol. 2020:1–21. doi: 10.1017/ice.2020.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye G., Lin H., Chen S., Wang S., Zeng Z., Wang W., Zhang S., Rebmann T., Li Y., Pan Z., Yang Z., Wang Y., Wang F., Qian Z., Wang X. Environmental contamination of SARS-CoV-2 in healthcare premises. J. Infect. 2020 doi: 10.1016/j.jinf.2020.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]