Abstract
PURPOSE
As frontline workers facing the COVID-19 pandemic, healthcare providers should be well-prepared to fight the disease and prevent harm to their patients and themselves. Our study aimed to evaluate the knowledge, attitude, and practice of oncologists in response to the COVID-19 pandemic and its impact on them.
METHODS
A cross-sectional study was conducted using a validated questionnaire disseminated to oncologists by SurveyMonkey. The tool had 42 questions that captured participants’ knowledge, attitude, and practice; their experiences; and the pandemic’s impact on various aspects of their lives. Participants from Middle East and North African countries, Brazil, and the Philippines completed the electronic survey between April 24 and May 15, 2020.
RESULTS
Of the 1,010 physicians who participated in the study, 54.75% were male and 64.95% were medical or clinical oncologists. The level of knowledge regarding the prevention and transmission of the virus was good in 52% of participants. The majority (92%) were worried about contracting the virus either extremely (30%) or mildly (62%), and 84.85% were worried about transmitting the virus to their families. Approximately 76.93% reported they would take the COVID 19 vaccine once available, with oncologists practicing in Brazil having the highest odds ratio of intention to receive the COVID-19 vaccine (odds ratio, 11.8, 95% CI, 5.96 to 23.38, P < .001). Participants reported a negative impact of the pandemic on relations with coworkers (15.84%), relations with family (27.84%), their emotional and mental well-being (48.51%), research productivity (34.26%), and financial income (52.28%).
CONCLUSION
The COVID-19 pandemic has adverse effects on various personal and professional aspects of oncologists’ lives. Interventions should be implemented to mitigate the negative impact and prepare oncologists to manage future crises with more efficiency and resilience.
BACKGROUND
Emerging at the end of 2019 with a rapid spread worldwide and a high death toll, COVID-19 was declared as a pandemic by the WHO on March 11, 2020.1,2 This pandemic overwhelmed healthcare systems in many countries, resulting in interruption of care and shortage of resources with a negative impact on care delivery for patients with COVID-19 and other patients. Cancer care was affected explicitly in a significant way at different levels, exposing patients with cancer to the risk of infection and harms from the interruption of their care.3-5
CONTEXT
Key Objective
To evaluate knowledge, attitude, and practice of oncologists in response to the COVID-19 pandemic and its impact on them.
Generated Knowledge
There is a regional variation in the level of knowledge about the disease; however, a majority of participants are worried about contracting the disease and transmitting to their family members. There is also variation in the willingness of receiving the COVID-19 vaccine once available, with highest odds ratio being among oncologists practicing in Brazil and those receiving flu vaccines routinely. There was a negative impact on participants’ relations with their coworkers, family members, their income, and research productivity.
Relevance
This study increases the awareness of various needs and challenges faced by oncologists and may help guide future efforts to mitigate these negative effects.
Healthcare staff are facing many challenges and risks too. These risks include, but are not limited to, infections, exhaustion, burnout, and emotional and well-being disorders.6-8 The crisis raised the awareness of the challenges encountered by healthcare staff and highlighted the importance of proper management of staff during and after the crisis.9,10
The amount of information related to COVID-19 is tremendous and increasing rapidly at an unprecedented pace. Many well-known entities including official bodies, such as WHO and Center for Disease Control; professional societies, such as ASCO and European Society of Medical Oncology; other organizations; and publishers launched their corona information centers to improve healthcare professionals’ access to information.11-13 Doctors face incredible tasks as they are expected to understand and use all the newly generated knowledge about this pandemic to provide better clinical care and to protect themselves and their patients from its harms.
Oncologists are facing the same aforementioned challenges in the pandemic including protecting their patients, their coworkers, themselves, and their families while continuing to provide timely care to their patients in suboptimal circumstances because of overwhelmed healthcare systems and lack of clear evidence on appropriate action, despite being exposed to a tsunami of information. Similar to other healthcare professionals, oncologists are at risk of acquiring the infection and experiencing all other pandemic adverse effects. Therefore, our study aimed to assess the response of oncologists to the pandemic in terms of knowledge, attitude, and practices and evaluate the pandemic’s impact on various aspects of their lives.
METHODS
Study Design and Participants
This cross-sectional study was conducted among oncologists from the Middle East (Gulf Council Countries and Levant), North Africa, Brazil, and the Philippines. Senior oncologists were enlisted as co-investigators from different countries to reach out to the participants.
Procedures
Demographic information, behavioral, knowledge, awareness, beliefs, and impact data were collected through an online anonymous survey using the SurveyMonkey platform. The research team chose SurveyMonkey for its advanced design capabilities. The target population was all physicians from various oncology subspecialties. An invitational message with an embedded link to the online survey was sent to potential study participants. The survey remained open for three consecutive weeks (from April 24 to May 15, 2020). The data collection instrument (online survey) consisted of 42 questions accumulated and validated by a panel of experts (oncologists and public health practitioners) to assess the knowledge and practices of COVID-19 control indicators across countries among oncologists. The online survey included sociodemographic information such as age, sex, specialty, years of experience, and practice region. All these characteristics were examined as categorical variables. The online survey also included knowledge questions about COVID-19 and the prevention practices, the pandemic’s impact on the participants’ personal and professional lives, level of anxiety about contracting the infection or transmitting to family members, and their intention to take the COVID-19 vaccine, if it becomes available.
Data Analysis
Responses were collected anonymously, and once the data collection process was completed, data were imported from SurveyMonkey into Stata (version 15.0, StataCorp LLC; College Station, TX) for analysis purposes. Study variables were summarized, in aggregate, using standard descriptive statistics such as mean, standard deviation, frequency, and proportion. Knowledge variables were scored (scores of 1 for correct answers and 0 for incorrect answers). Participants were classified as having a good versus poor level of knowledge based on the mean cutoff value of the knowledge score. The χ2 test of independence was conducted to assess the variation of study variables across the level of knowledge and level of worry about COVID-19. Odds ratios (ORs) and 95% CIs were calculated using logistic regression analysis to ascertain the effects of study variables on the likelihood of having poor knowledge and high level of worry regarding COVID-19 and intentions to take the COVID-19 vaccine if it becomes available. The significance level was set at P < .05 for all analyses.
This study was approved by Ethics Board of King Abdullah International Medical Research Center.
RESULTS
Of the 1,010 participants in the study, there was a slight male predominance and the majority were medical oncologists. About a quarter of them participated in official COVID-19 activities. Table 1 depicts the participants' characteristics.
TABLE 1.
Participants' Characteristics and Level of Knowledge, N = 1,010
Participants’ Knowledge
Bivariate analysis showed that knowledge among participants significantly varied by sex, specialty, and region. Regression analysis showed that level of knowledge is significantly higher among male (OR = 1.36; 95% CI, 1.06 to 1.75; P = .015), being from North Africa (OR = 2.54; 95% CI, 1.94 to 3.32; P < .001), being from East Asia (OR = 3.74; 95% CI, 1.62 to 8.64; P = .002), and being a medical or clinical oncologist (OR = 1.55; 95% CI, 1.21 to 1.99; P = .001). Less knowledge is associated with the female gender (OR = 0.73; 95% CI, 0.57 to 0.94; P = .015) and being from the Gulf Council Countries region (OR = 0.30; 95% CI, 0.20 to 0.43; P < .001) (Table 1).
Exposure to infections among patients and family members of coworkers did not affect knowledge, and participants who had infections did worse in the knowledge tests.
About 31% of participants believed that only the elderly, immunocompromised, and people with chronic illnesses are at risk of developing severe disease and complications if infected with COVID-19. Still, the overwhelming majority got the answers correct about the transmission of the virus by droplet and potentially transmitting the virus by asymptomatic patients. The correct answers about wearing the surgical masks and N95 masks were less (Table 2).
TABLE 2.
Participant’s Knowledge About COVID-19 and Their Behaviors

Participants’ Behavior
Adherence to precautionary measures such as social distancing, handshaking, and handwashing was variable among participants, with handwashing being the highest compliance practice (Table 3).
TABLE 3.
Participants’ Awareness, Perception, and Beliefs About COVID-19

Social distancing and handshaking varied by region. Those from Levant and North Africa were less likely to be compliant with distancing (OR = 0.55, 95% CI, 0.38 to 0.76; P < .001 and OR = 0.66, 95% CI, 0.44 to 0.98, P = .039), and those from North Africa less likely to be compliant with avoiding hand shaking (OR = 0.53, 95% CI, 0.41 to 0.69, P < .001).
Participant’s Awareness About Preparedness
About a quarter of the participants had concerns about hospital measures’ adequacy to control COVID-19 and the leadership communications about the crisis. About 27% do not have access to COVID-19 tests. More than half of them had coworkers with infections, followed by having patients infected. Only a small fraction had infections (Table 3).
Perception and Beliefs
More than 90% of participants were very worried or mildly worried about contracting the infection, and more than 84% worried about carrying the virus home to their families. More than three quarters of them will get the COVID-19 vaccine if approved, although only 40% of them regularly get the flu vaccine. About half of the participants feel that the job put them at increased risks, but they would continue with it; however, a few were considering changing jobs in the next 2 years (Table 3).
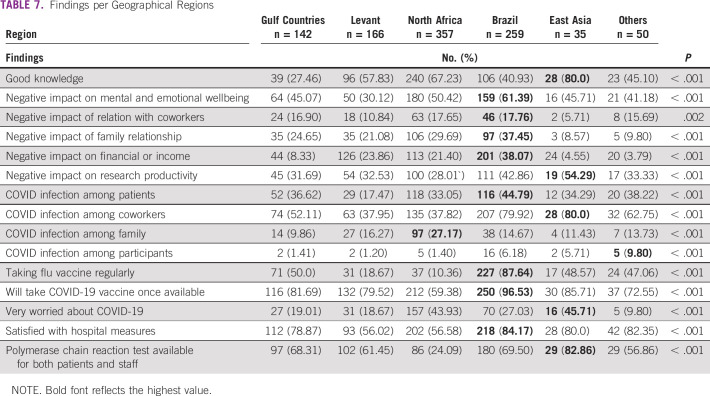
The analysis of the willingness to take the COVID-19 vaccine once available is depicted in Table 4. Males were 2.46 times more likely to take the COVID-19 vaccine, being a clinical oncologist 1.77 times and having infections among coworker more than twice the odds, three times more likely if they worked in a private hospital, 12 times more likely if they worked in Brazil, and about 50% less likely if they worked in the North Africa. Practicing in Brazil was the strongest predictor of taking the COVID-19 vaccine (OR 11.8, 95% CI, 5.96 to 23.38, P < .001) followed by taking the flu vaccine regularly (OR 8.78; 95% CI, 5.72 to 13.50; P < .001).
TABLE 4.
Factors Significantly and Positively Associated With Intention of Taking the COVID-19 Vaccine If It Becomes Available
The level of worry did not vary by holding an administrative position or being part of the team that participated in the COVID-19 efforts in bivariate analysis (Table 5). Logistic regression analysis showed that those practicing in North Africa were more likely to report being very worried about COVID-19 (OR = 2.66; 95% CI, 2.01 to 3.50; P < .001). Those practicing in governmental hospitals were more likely to express high level of worry (OR = 1.90; 95% CI, 1.44 to 2.49; P < .001); also, being a medical oncologist is associated with a higher level of anxiety (OR = 1.52; 95% CI, 1.01 to 2.29; P = .044), and being a female is associated with a higher level of anxiety (OR = 2.04; 95% CI, 1.55 to 2.64, P < .001). Those who suffered emotionally and mentally from COVID-19 significantly expressed being worried (OR = 2.39; 95% CI, 1.18 to 3.15; P < .001). Those who reported that COVID-19 affected relationships with coworkers were most likely to be worried (OR = 1.87, 95% CI, 1.33 to 2.65, P < .001), and few reported that it affected their relationship with their families (OR = 1.53, 95% CI, 1.14 to 2.05, P = .004) and their research conduct (OR = 1.43, 95% CI, 1.01 to 1.77, P = .041). Experiencing infection among patients, coworkers, family members, or the participants themselves did not affect the level of worrying.
TABLE 5.
Analysis of the Relation of the Severe Anxiety (Very Worried) With Various Characteristics and Behavior
Impact of Participants’ Well-Being and Social, Financial, and Professional Life
About a half of the participants reported a negative impact of the pandemic on their emotional and mental well-being and financial income. Nearly, a quarter of them reported a negative impact on family relationships and less than that on coworkers’ relationships. About a third of them reported a negative impact on their research productivity. It is noteworthy that many have also reported a positive impact on these domains (Table 6).
TABLE 6.
Reported Impact of COVID-19 on Participants
Mental and emotional well-being impact varied by gender, with females being more likely to be affected (OR = 1.57, 95% CI, 1.23 to 2.02, P < .001) and being in practice for more than 20 years less likely to be mentally and emotionally affected (OR = 0.61, 95% CI, 0.42 to 0.87, P = .007).
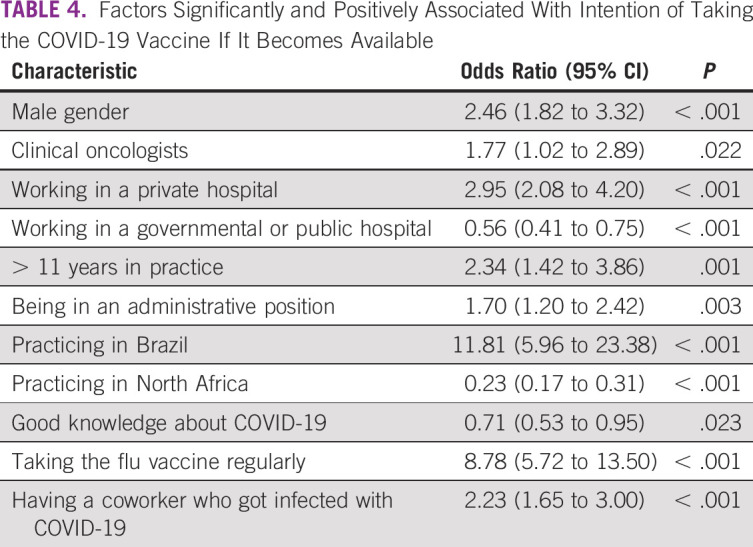
Regional Differences
Comparison of findings among regions revealed a significant regional difference in these findings (Table 7). Oncologists in Brazil had the highest negative impact of the pandemic on their emotional well-being, relationships with their coworkers, their relationships with family members, and their financial income. However, they were more likely to take the flu vaccine regularly, willing to take the COVID-19 vaccines once available, and most satisfied with their hospital measures against COVID-19. Oncologists in East Asia scored better in knowledge questions. Still, they reported a more negative impact on research productivity, infection among their coworkers, worrying more about contracting infection, and better access to COVID-19 tests for their patients and staff.
TABLE 7.
Findings per Geographical Regions
DISCUSSION
Our study included oncology physicians from different regions and different specialties at different stages of their careers and experience. The study revealed interesting results about the knowledge behaviors and impact of the pandemic on participants.
The level of knowledge was poor in a large fraction of participants, which may reflect the nature of the pandemic with many uncertainties, relying heavily on social media and other nonprofessional sources of information and a different COVID-19 impact in specific countries. This necessitates assuring credible and accessible sources of reliable information that people could follow rather than counting on social media and other sources of noncredible information.15 This is particularly important for healthcare professionals as knowledge does affect attitude, health behaviors, and practices.14,16-18
It is expected that physicians will experience different kinds of negative emotions and psychological reactions during the pandemic.9,19 Our study showed that significant numbers of our participants worry about acquiring infections themselves or transmitting the infection to their family members. These feelings may evolve with time and maybe mixed. In an Italian study of 956 oncologists during the early phase of the pandemic, analyses of the conversations over WhatsApp messenger over 4 weeks showed an increase of the negative emotion of fear, anger, and sadness over time. However, positive emotions, such as trust, also increased with time.20 In our group, female, younger physicians with less experience duration were more likely to worry about the disease and report a negative impact of the pandemic on their well-being. The concerns about healthcare providers’ emotional well-being were raised by many authors highlighting the need for a systemic approach to prevent and recognize problems early and intervene appropriately.21-24 The worries about transmitting the infection to family members were very high in our population. Similar concerns were identified in other studies.25,26
In addition to the anxiety and negative impact on emotional well-being, our study revealed the pandemic’s multidimensional impact on participants, such as their relationships with their family and coworkers, financial income, and research productivity.
The impact of the pandemic on physician income has been reported previously in different settings and specialties. For example, in a Brazilian study of 744 urologists, 54% of them reported a 50% reduction in their income.27 Another study predicted a 50%-70% reduction in imaging studies for 3-4 months.28
The impact of COVID-19 on scientific activities was also reported in previous studies. In an Italian survey of 165 breast oncologists, more than 80% reported a decrease in their scientific and research activities.29
However, some of the participants reported a positive impact of the pandemic on different aspects that were evaluated, including a positive impact on relations with family, coworkers, and research productivity. Oncologists reported a high level of collegiality and cooperation across borders, which resulted in large-scale international studies published in a record time.30,31
Our study revealed interesting regional differences that are worth discussion and further evaluation. For example, oncologists in Brazil had the highest negative impact on their emotional well-being and their relations with their family and coworkers, in addition to a negative impact on their financial status and income. However, they were more likely to express willingness to take the COVID-19 vaccine once available. The reasons for regional differences in the knowledge and some of the participants’ behaviors require further investigation, but this can be attributed to the whole country’s experience with the pandemic, available sources of information, or cultural variation.32-34
The experience with COVID-19 infection in patients, coworkers, family members, and participants did not change the worry level and did not affect the participants’ knowledge. Interestingly, the participants’ infection correlated negatively with the knowledge, which may reflect personal perception and the experience of the participants with the infection rather than the common scientific knowledge. However, having infection among coworkers was a significant factor in expressing willingness to take the COVID-19 vaccine, which may reflect vulnerability from being at risk of infection because of the profession.
One of the critical concerns about our findings is that many oncologists feel that their job puts them at an increased risk for exposure to harm, and a small fraction of them was considering career changing in the next couple of years. Oncologists are worried about contracting the infection or transmitting it to their families, having concerns about their social and work relations, being exposed to a financial decline in addition to the workload, and exhaustion like most healthcare professionals during the pandemic. Understanding the multiple factors that lead to physician dissatisfaction and burnout is very important to plan interventions to mitigate the negative impact on physicians.10,26 These interventions should aim to help physicians cope better with the challenges of work and prevent their attrition from the practice, especially an existing oncology physicians shortage.35,36
The question about the intention to receive the COVID-19 vaccine once available revealed variable results with certain groups being likely to receive it (male, working in private hospitals, being in practice for a long time, and working in Brazil) and others not to receive it (working in governmental hospitals, practicing in North Africa, and having good knowledge about COVID-19).
Those who get the flu vaccines routinely were 8 times more likely to declare their intention to receive the COVID-19 vaccine, reflecting their health behavior toward preventive measures for infectious diseases. Since there are multiple barriers to receiving the flu vaccines, those who do receive them are likely to make extra efforts to do so as shown in previous studies about the influenza vaccination.37
Our study’s limitation is related to the cross-sectional design that captures information at a specific point of time, which may be subject to change with time, especially in the pandemic era that was rapidly evolving and introducing new knowledge and facts that may affect behaviors and feelings of physicians.
In summary, our study highlighted the complex multilevel impact of the COVID-19 pandemic on various aspects of oncologists’ personal and professional lives. These findings require the need to implement interventions that assure the oncologists’ well-being and their productivity.
There should be better educational intervention to enhance the oncologists’ knowledge about the pandemic, not just the medical aspects of it but also the pandemic’s impact on various aspects of their lives. Healthcare leaders should ensure the availability of employee support programs for their well-being and mental health. Oncologists should acquire the knowledge of self-care and self-preservation and enhance their coping skills for such a major crisis.
AUTHOR CONTRIBUTIONS
Conception and design: Abdul Rahman Jazieh, Assia A. Bensalem, Abdullah A. Alsharm, Hassan Errihani, Layth Mula-Hussain, Ola M. R. Khorshid, Mohammad O. Alkaiyat, Hoda A. Jradi
Administrative support: All authors
Provision of study materials or patients: All authors
Collection and assembly of data: Abdul Rahman Jazieh, Anelisa K. Coutinho, Assia A. Bensalem, Abdullah A. Alsharm, Hassan Errihani, Layth Mula-Hussain, Sana Al-Sukhun, Carlos A. Sampaio-Filho, Ola M. R. Khorshid, Roselle B. De Guzman, Mohammad O. Alkaiyat, Hoda A. Jradi
Data analysis and interpretation: Abdul Rahman Jazieh, Assia A. Bensalem, Abdullah A. Alsharm, Hassan Errihani, Layth Mula-Hussain, Sana Al-Sukhun, Ola M. R. Khorshid, Mohammad O. Alkaiyat, Hoda A. Jradi
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Abdul Rahman Jazieh
Research Funding: MSD Oncology, AstraZeneca, Pfizer
Travel, Accommodations, Expenses: AstraZeneca, Bristol-Myers Squibb
Anelisa K. Coutinho
Consulting or Advisory Role: Amgen, Bayer, Roche/Genentech, Merck Serono, MSD Oncology, Sanofi/Aventis, SERVIER, United Medical
Speakers' Bureau: Amegn, Bayer, Lilly, Roche/Genentech, Merck Serono, MSD Oncology, Roche Molecular Diagnostics, Sanofi/Aventis, Novartis, SERVIER, United Medical, Johnson & Johnson/Janssen, AstraZeneca
Research Funding: Bristol-Myers Squibb, SERVIER
Hassan Errihani
Consulting or Advisory Role: Pfizer, Roche, MSD, Merck, Janssen Oncology, AstraZeneca
Speakers' Bureau: Novartis, Amgen
Research Funding: Roche
Travel, Accommodations, Expenses: Pierre Fabre, Merck
Sana Al-Sukhun
Honoraria: MSD Oncology
Consulting or Advisory Role: MSD Oncology
Speakers' Bureau: Aventis Pharma, Janssen-Cilag
Travel, Accommodations, Expenses: Merck Serono, Roche, Bristol-Myers Squibb
Carlos A. Sampaio-Filho
Employment: Clinica AMO
Leadership: Clinica AMO, Salvador, Brazil
Stock and Other Ownership Interests: Clinica AMO
Consulting or Advisory Role: Pneuma Respiratory
Roselle B. De Guzman
Honoraria: Roche, AstraZeneca, Novartis, Merck Serono, MSD Oncology, Boehringer Ingelheim
Consulting or Advisory Role: Roche, Novartis, Boehringer Ingelheim, AstraZeneca
Research Funding: Centus Biotherapeutics
Travel, Accommodations, Expenses: Hospira, Roche, Merck Sharp & Dohme, Eisai, Boehringer Ingelheim, AstraZeneca, Lilly, Novartis
No other potential conflicts of interest were reported.
REFERENCES
- 1.WHO : Pneumonia of Unknown Cause—China. WHO, 2020. http://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/ [Google Scholar]
- 2.WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [Google Scholar]
- 3.van de Haar J, Hoes LR, Coles CE, et al. : Caring for patients with cancer in the COVID-19 era. Nat Med 26:665-671, 2020 [DOI] [PubMed] [Google Scholar]
- 4.Fabiana G, Caliandro M, Surgo A, et al. : Cancer patients in COVID-19 era: Swimming against the tide. Radiother Oncol 149:109-110, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Richards M, Anderson M, Carter P, et al. : The impact of the COVID-19 pandemic on cancer care. Nat Cancer 1:565-567, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mayor S: COVID-19: Impact on cancer workforce and delivery of care. Lancet Oncol 21:633, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rahman Jazieh A: Managing healthcare workers during the COVID-19 pandemic and beyond. J Qual Safety Healthcare 3:33-35, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tan BYQ, Chew NWS, Lee GKH, et al. : Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med 173:317-320, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greenberg N, Docherty M, Gnanapragasam S, et al. : Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ 368:m1211, 2020 [DOI] [PubMed] [Google Scholar]
- 10.Shanafelt T, Ripp J, Trockel M: Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA 323:2133-2134, 2020 [DOI] [PubMed] [Google Scholar]
- 11.Archived News. https://www.nccn.org/about/news/newsinfo.aspx?NewsID=1949
- 12.ASCO Coronavirus Resources. ASCO. https://www.asco.org/asco-coronavirus-information [Google Scholar]
- 13.Coronavirus Disease 2019 (COVID-19). CDC. https://www.cdc.gov/coronavirus/2019-ncov/index.html [Google Scholar]
- 14.Bhagavathula A, Aldhaleei WA, Rahmani JR, et al. : Novel coronavirus (COVID-19) knowledge and perceptions: A survey of healthcare workers. JMIR Public Heal Surveill 6:e19160, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karasneh R, Al-Azzam S, Muflih S, et al. : Media’s effect on shaping knowledge, awareness risk perceptions and communication practices of pandemic COVID-19 among pharmacists. Res Soc Adm Pharm 17:1897-1902, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giao H, Le An P, Thi Ngoc Han N, et al. : Knowledge and attitude toward COVID-19 among healthcare workers at District 2 Hospital, Ho Chi Minh City. Asian Pac J Trop Med 13:6-11, 2020 [Google Scholar]
- 17.Zhong BL, Luo W, Li HM, et al. : Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: A quick online cross-sectional survey. Int J Biol Sci 16:1745-1752, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang M, Zhou M, Tang F, et al. : Knowledge, attitude, and practice regarding COVID-19 among healthcare workers in Henan, China. J Hosp Infect 105:183-187, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Preti E, Di Mattei V, Perego G, et al. : The psychological impact of epidemic and pandemic outbreaks on healthcare workers: Rapid review of the evidence. Curr Psychiatry Rep 22:43, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blasi L, Bordonaro R, Borsellino N, et al. : Reactions and countermeasures of medical oncologists towards the incoming COVID-19 pandemic: A WhatsApp messenger-based report from the Italian College of Chief Medical Oncologists. Ecancermedicalscience 14:1046, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jazieh A-R, Al Hadab A, Al Olayan A, et al. : Managing oncology services during a major coronavirus outbreak: Lessons from the Saudi Arabia experience. JCO Glob Oncol 6:518-524, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kang L, Li Y, Hu S, et al. : The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 7:e14, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu Y, Wang J, Luo C, et al. : A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manage 60:e60-e65, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xiang YT, Yang Y, Li W, et al. : Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7:228-229, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Louie PK, Harada GK, McCarthy MH, et al. : The impact of COVID-19 pandemic on spine surgeons worldwide. Glob Spine J 10:534-552, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matsuo T, Kobayashi D, Taki F, et al. : Prevalence of health care worker burnout during the coronavirus disease 2019 (COVID-19) pandemic in Japan. JAMA Netw Open 3:e2017271, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gomes CM, Favorito L, Victor J, et al. : Impact of COVID-19 on clinical practice, income, health and lifestyle behavior of Brazilian urologists. Int Braz J Urol 46:1042-1071, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cavallo JJ, Forman HP: The economic impact of the COVID-19 pandemic on radiology practices. Radiology 296:E141-E144, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Poggio F, Tagliamento M, Di Maio M, et al. : Assessing the impact of the COVID-19 outbreak on the attitudes and practice of Italian oncologists toward breast cancer care and related research activities. JCO Oncol Pract 16:e1304-e1314, 2020 [DOI] [PubMed] [Google Scholar]
- 30.Schrag D, Hershman DL, Basch E: Oncology practice during the COVID-19 pandemic. JAMA 323:2005-2006, 2020 [DOI] [PubMed] [Google Scholar]
- 31.From a Tweet to The Lancet in 10 weeks: COVID-Cancer Consortium. https://www.medscape.com/viewarticle/932478
- 32.Bavel JJV, Baicker K, Boggio PS, et al. : Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav 4:460-471, 2020 [DOI] [PubMed] [Google Scholar]
- 33.Cialdini RB, Goldstein NJ: Social influence: Compliance and conformity. Annu Rev Psychol 55:591-621, 2004 [DOI] [PubMed] [Google Scholar]
- 34.Hawthorn A, Kleidon T, Larsen E, et al. : Peripheral intravenous catheter protection. Br J Nurs 30:28, 2018 [Google Scholar]
- 35.Yang W, Williams JH, Hogan PF, et al. : Projected supply of and demand for oncologists and radiation oncologists through 2025: An aging, better-insured population will result in shortage. J Oncol Pract 10:39-45, 2014 [DOI] [PubMed] [Google Scholar]
- 36.Mathew A: Global survey of clinical oncology workforce. J Glob Oncol 2018:1-12, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bellia C, Setbon M, Zylberman P, et al. : Healthcare worker compliance with seasonal and pandemic influenza vaccination. Influenza Other Respi Viruses 7(suppl 2):97-104, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]