Abstract
Background: The first wave of the COVID-19 pandemic initiated officially in October 2020. Since then several observations have been made regarding the disease and its symptoms. Patients and Methods: We included eighty seven in our observational study. Our main aim was to investigate their long term respiratory follow-up in correlation with their initial radiological and laboratory findings and values. The nose swab PCR test for COVID-19 was used for diagnosis. Patients were monitored at 3 and 6 months after their hospital reception whereas basic parameters of health condition (smoking, PO2, SPO2, WBC, CXR, CRP, intercurrent findings, days of nursing, colchicine administration) in joint with gender and age were recorded. Results: Males seem more susceptible to the viral disease than females in a ratio 1,8:1. The parameters FEV1 and FVC (as % relative changes) were not affected, apart from the DLCO to which CRP (in loge+1 transformation) and SPO2 showed a statistically significant effect. Conclusion: None of these patients were intubated, or admitted to the intensive care unit. The respiratory function is affected by the virus and the effect is reversed within the first three months. Males are more affected and the radiological and laboratory findings are associated with the respiratory functions.
Keywords: COVID-19, FEV1, FVC, DLCO, respiratory functions, respiratory infection
Background
The COVID-19 pandemic was initiated in October 2020 and since then several observations have been made regarding the symptoms of the disease. At the same time the medical community is trying to identify the best drug combination treatment in order to treat COVID-19 patients [1].
In 2009 we had the H1N1 pandemic and two minor virus transformations followed with H3N2 and H7N7 [2,3,4].
Clinical differences were observed between the two waves of H1N1, which is also observed with the COVID-19 in 2021 [5].
During the H1N1 pandemic oseltamivir and macrolides were used to block disease progression. The main symptoms were high fever ≥39 and fatigue while respiratory distress was observed a lower number of patients.
Moreover; the mean age of the patients was below 30 and a large number of patients did not have an underlying disease [6,7].
The health cost of these patients had been recorded to be higher than that of a respiratory bacterial infection [8].
It was also observed that the virus affected the respiratory functions of patients during a to six month observation [9].
On the contrary COVID-19 patients most of them have an underlying health condition and the mean age is ≥60 years old. At least these were the data presented for the first wave of COVID-19 [1].
During the second wave the mean age of the patients has been lower to ≤50 years of age. However; we have the experience of treatment during the first wave with macrolides, remdesivir and colchicine and therefore we can manage the disease symptoms in a more efficient way. One of the main characteristics of COVID-19 patients is the 14 day period where a patient remain contagious and many of these patients usually young adolescents have no symptoms. Moreover; severe thrombosis and respiratory distress has been observed to most of the patients. Fortunately nowadays we have vaccines and several novel immunomodulatory drugs are being investigated for treatment. Real-time polymerase chain reaction (PCR) from nasal swab is still the best method of COVID-19 diagnosis [10,11].
However; for asymptomatic patients saliva swab has been observed to have a higher diagnostic rate for asymptomatic patients [12].
We conducted a long-term evaluation of the respiratory values for COVID-19 patients that did not need intubation, we recorded their radiological and laboratory values.
Patients and Methods
Patients
Eighty seven patients were diagnosed upon admission with COVID-19 had a long term respiratory follow-up. All patients included in our study came at the emergency room of hospitals and after a positive RT-PCR result for COVID-19 were admitted in a ward. To all patients computed tomography scan was performed upon admission and laboratory values such white blood count, fever, age, c-reactive protein, partial oxygenation and saturation were recorded. Moreover; respiratory values were recorded with spirometry such as Forced Expiratory Value in 1sec (FEV1), Forced Vital Capacity (FVC) and Diffusing Capacity for Lung Monoxide (DLCO). Respiratory function tests were performed according to ERS guidelines [13].
Patients had their initial examination upon discharge and every 3 months and 6 months upon their follow up. All centers used the same equipment (Figure 1). We evaluated with PFTs the adverse effects of the virus on their respiratory capacity and observed the duration of these effects.
Figure 1.
Respironics system that can perform spirometry, DLCO measurement and FeNO measurement
DLCO measures the transfer for CO molecules from alveolar gas to the pulmonary circulation. It assists in the evaluation of possible parenchymal lung disease. Spirometry is an easy examination which evaluates how well your lungs work.
To all patients azithromycin 500mg and remdesivir (five days) (Indicated for adults and pediatric patients aged ≥12 years who weigh ≥40kg for treatment of COVID-19 requiring hospitalization Day 1 loading dose: 200mg IV infused over 30-120 min, then Day 2 and thereafter: 100mg IV qDay) was administered.
Colchicine (1mg/12h) and corticosteroids (range 100mg-500mg per day for 5 days) were also used as per our protocol.
Moreover; anti-thrombotic agents were given as treatment after discharge with low-molecular weight heparin in every patient for 10 days.
Oxygen supplementation, and antibiotics was also administered to all those patients with c-reactive protein (C-RP) ≥5 and white blood count (WBC) ≥10000. The patients information upon admission can be found in Table 1.
Table 1.
Patients characteristics
|
Upon admission | |
|
Characteristic Convid-19 |
Range |
|
Age (years) |
14-90 |
|
Male/Female |
56/31 |
|
Smokers (male/female) |
15/7 |
|
Co-existing conditions |
74/87 |
|
Asthma |
15/74 |
|
COPD |
22/74 |
|
IPF |
4/74 |
|
Cancer |
5/74 |
|
Diabetes |
8/74 |
|
Coronary Heart Disease |
20/74 |
|
Outcomes-days | |
|
Duration of fever in hospital under treatment 1-8 days | |
Method of Covid-19 Diagnosis
All patients had samples for diagnostic tests for SARS-CoV-2. We had nurses educated to take nasal swab. Nasal swabs were taken upon admission in accordance with world health organization (WHO) and the results were ready within 2 hours [12].
Statistical Analysis
Patients were monitored at 3 and 6 months after their hospital reception whereas basic parameters of health condition (smoking, PO2, SPO2, WBC, CXR, CRP, intercurrent findings, days of nursing, colchicine administration) in joint with gender and age were recorded. In our statistical analysis CXR represents findings of ground glass opacities with computed tomography (Figure 2).
Figure 2.
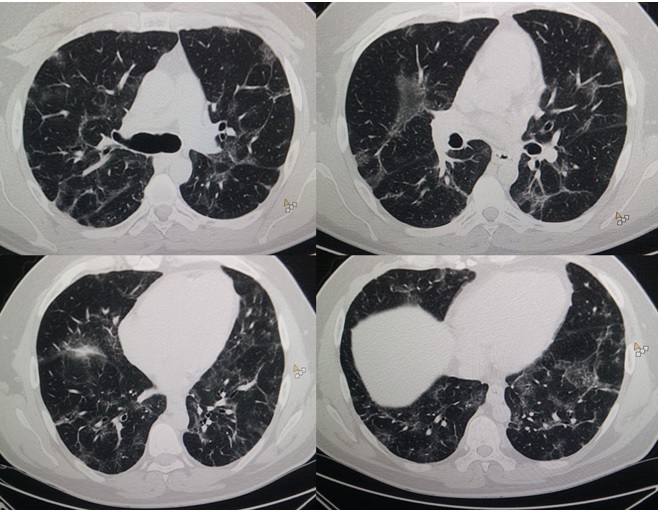
CT of the thorax of a patient diagnosed upon admission with Covid-19, ground glass opacities can be easily observed throughout the lung parenchyma. This patient did not have respiratory distress
The word background represents the underlying disease that the patients might have. The indices of lung function, FEV1, FVC and DLCO were measured in the two time follow up.
These parameters were transformed to % relative change of individual values, (final-initial)*100/initial, and particularly as a change from month 3 to month 0 and also from month 6 to month 3. The relative changes were regressed as responses against all the parameters (predictors) of the study applying a stepwise forward selection of significant variables at 0.05 entrance probability level (Figure 3).
Figure 3.
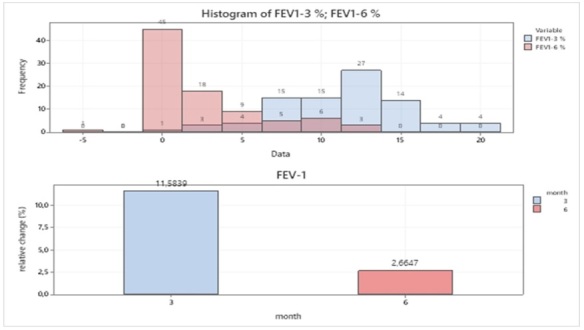
Size frequency distribution of % relative FEV1 changes and mean % relative change at two time intervals
A written consent was acquired for the figures included in our manuscript. The study was approved by the 3rd Surgery Department, AHEPA, University General Hospital, 12/2/20.
Aristotle University of Thessaloniki, Thessaloniki, Greece.
Results
Males seem more susceptible to the viral disease than females in a ratio 1,8:1 (56/31), smokers were limited to 1:3 (65/22) in the sample, patients with CXR lesion totaled 30% and those with background (intercurrent) findings totaled 85,1% (Table 2).
Table 2.
Descriptive statistics of the categorical parameters of the study
|
SEX |
N |
Column % |
|
FEMALE |
31 |
35,63% |
|
MALE |
56 |
64,37% |
|
SMOKING |
|
|
|
0 |
65 |
74,71% |
|
1 |
22 |
25,29% |
|
CXR |
|
|
|
0 |
61 |
70,11% |
|
1 |
26 |
29,89% |
|
BACKGROUNG |
|
|
|
0 |
13 |
14,94% |
|
1 |
74 |
85,06% |
The individual percentage relative change of the forced expiratory volume (FEV1), jointly at months 3 and 6 is shown as size frequencies and mean changes in Figure 3.
An outstanding difference of mean % relative FEV1 change between month 3 and 6 is obvious reaching 11,6% and 2,7% correspondingly, also reflecting a clear shift of FEV1-3% size frequencies to the higher values.
It comes out, plausibly, the % change FEV1 in the first measurement should be given prominence as the reference index of FEV1 change.
A very similar pattern occurs in Figure 4 concerning the % relative changes, individual and means, of FVC. A high response of % mean change in the first-time interval (11.1%) and a low one in the time shift between month 3 to 6 (2,7%).
Figure 4.
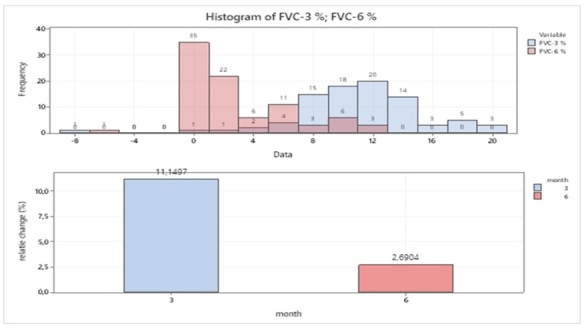
Size frequency distribution of % relative FVC changes and mean % relative change at two-time intervals
Again, the key variable should be thought as the first-time measurement of FEV1 (Figure 4).
On the contrary to the aforesaid findings, the diffusing capacity for carbon monoxide (DLCO) does not really change in % relative numbers in the two mid-time intervals, as the closed numbers of mean changes indicate (8,5% and 7,5%) and the great overlap of the two size frequencies (Figure 5).
Figure 5.
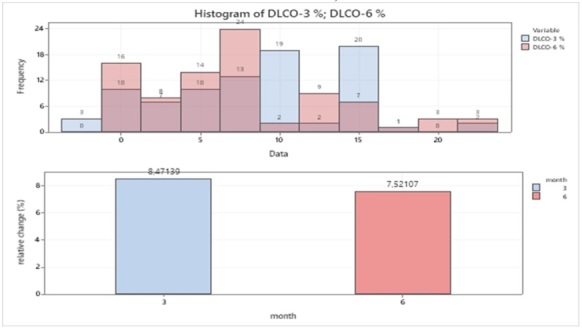
Size frequency distribution of % relative DLCO changes and mean % relative change at two time intervals
The DLCO% response is probably lower than the two previous indices at the first-time interval and much higher at the second one.
Considering the overall cumulative response at the final time for the three parameters, it appears that the total % mean relative changes do not differ substantially: 14,24%, 13,84% and 15,99%.
The lung function indices at month 3 were considered as dependent variables and their response due to the potential effect of all parameters of the study acting as predictors was examined via a multiple regression analysis.
The parameters FEV1 and FVC (as % relative changes) were not affected, apart from the DLCO to which CRP (in loge+1 transformation) and SPO2 showed a statistically significant effect (Figure 6).
Figure 6.
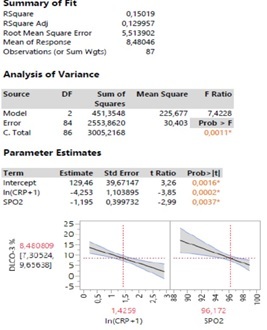
Statistical output of a multiple regression analysis of DLCO % relative response against the parameters under study. The results are based on the forward selection of predictors
The fit of the model is quite low (R2=15%), due presumably to the high individual variability of the sample, it does show, however, a decline of DLCO with loge CRP increase (b=-4,253) and with SPO2 increase (b=-1,195).
More specifically, at mean % relative change of DLCO of 8,48% a corresponding value of 3,2 CRP (antilogCRP-1) and a value 96,2% of SPO2 is expected. These values could be further thought as threshold levels for predicting potential occurrence of covid-19 infection.
Discussion
The pandemic COVID-19 influenza virus is an airborne transmitted virus that is highly contagious and can spread in the same way as seasonal influenza. The transmission occurs predominantly through droplets.
However; indirect transmission may occur after contact with surfaces or objects contaminated. The incubation period for pandemic COVID-19 virus is the main issue as it is understood to be approximately 14 days.
Consistent with seasonal influenza, transmission of the pandemic COVID-19 is most likely when a patient has severe disease symptoms such cough and sneezing.
However; as it has been observed another serious concern is that there are young adults or children that can transmit the disease and they do not have any symptoms [14].
The following isolation precautions were recommended by our ministry of health, people who were in close contact with patients with suspected or confirmed COVID-19 were isolated for 15 days. Close contact was defined as working within 2meters of a confirmed patient.
We precaution measures with all patients like: non-sterile gloves, hand hygiene immediately after glove removal and gowns along with eye.
As a protection from the air droplets a city population has to use according to our national CDC to be the use of a fit-tested disposable N95 respirator. A cocktail of drugs is definitely needed for the best treatment of this virus with anti-inflammatory agents, anti-thrombotic agents, anti-viral agents and antibiotics were necessary [15].
We have several vaccines which are definitely going to protect several groups of patients with underlying disease such diabetes, cancer, asthma and chronic obstructive pulmonary disease, however; we still have a long way until a large number of the population is vaccinated [16,17].
Our study has several limitations such as the small number of patients, secondly we did not have the baseline for the respiratory function for each patient.
Furthermore, we included only patients with a mild disease presentation since all the patients included were hospitalized, however; they were not intubated and we did not need to use non-invasive ventilation methods.
It is clear from the computed tomography scans that there were ground glass opacities which we know that are proteins produced from the virus within the alveoli and it takes several weeks for this material to be dissolved.
Indeed for our patients it was observed that most of them had their respiratory functions back normal within 3 months after their diagnosis.
Further improved from the 3 months to 6 months was observed only to those patients that had more extensive radiological findings.
An important observation is that even young patients ≤40 had although they had FEV1 values between 70-90 after the months of evaluation they reported shortness of breath with normal oxygen saturation. Probably there is an effect to the vessels which remains to be resolved with further studies. Males were more in our study and of course high values of WBC and CRP were associated with simultaneous respiratory infection.
These patients need to be handled in a special outpatient cabinet in order to follow-up the long term effect of this various. The body mass index (BMI) did have any statistical correlation with the days of hospitalization or respiratory functions. The number of patients with morbid obesity was not as high as expected from our previous experience with H1N1 viral infection. Moreover; there are differences between the two COVID-19 waves between 2020 and 2021 which remain to be recorded [18].
In some countries even three waves of the disease have been observed. Also, we have new treatment options and vaccines, therefore we expect the morbidity and the disease transmission to change.
Finally, we should not forget the mental health impact that this virus outbreak has and a multimodality treatment approach is necessary for these patients [19].
The virus outbreak had a severe effect to patients with chronic disease, since they could not easily enter hospitals and perform diagnostic or treatment procedures [20].
Certainly several measures should be taken for these patients.
Conclusions
Covid-19 is differentiated from the influenza airborne virus because a person can be asymptomatic and still able to transmit the virus with airborne droplets.
The transmission mainly occurs with airborne droplets.
The time length that a person is able to transmit the virus load is around 14 days more than the influenza virus strains.
Therefore a carrier that is asymptomatic is a serious issue.
The influenza virus strains cause symptoms such as high fever, fatigue, cough and rhinitis which makes the patient easily identifiable and this patient is usually admitted to the hospital and remains under isolation when necessary.
During the H1N1 pandemic we observed ground glass opacities in several patients, however; patients with Covid-19 almost all of those admitted had ground glass opacities.
The extent of the lesions within the lung parenchyma has an impact to the respiration of the patients and therefore patients with extended lesions have severe respiratory distress.
However; in many hospital computed tomography of Covid-19 patients is not within their protocol during admission.
The results of the respiratory functions are also associated with the extent of the lesions within the lung parenchyma.
These lesions take more time to dissolve as it has been observed during our observational study.
The H1N1 patients certainly had less respiratory distress and less ground glass opacities when compared with previously published data.
Moreover; influenza patients have usually morbid obesity and the mean age recorded during the first wave was ≥15.
The percentage of Covid-19 patients with morbid obesity is much lower and mean age is ≥30.
These characteristics of course defer from one country to another and from the first wave in a country to the third wave when this was observed.
However; certainly there are differences from the influenza A patients.
The methods also to identify patients with Covid-19 have to be validated and revalidated during the first months.
Each center for controlled disease in every country issued differed guidelines for the testing of a patient for different diagnostic and therapeutic procedures.
In the case of a bronchoscopy the patients had to do a RT-PCR no more than 1 day before the examination, while for a gastroscopy an antigen test was enough.
In the case of cancer patients, a rapid test was enough before every chemotherapy session.
According to the guidelines of WHO a person with the suspicion of Covid-19 had to call the health authorities to a specific number that was provided in every country and report its symptoms and according to the symptoms a guidance was provided either the patient to go to the hospital or remain at home in quarantine.
However; it was recorded in many countries that the people provided health information were not trained medical stuff and therefore in many cases the health situation of a patient was not properly diagnosed.
Mental illness with depression being the first was observed in many people not only to patients that were isolated alone positive with Covid-19 in an isolation room, but also in many people staying at home isolated due the quarantine restrictions of a city virus load.
Several matters will certainly arise after this health crises either with mental illness or chronic respiratory patients.
In the next two years evaluation of the vaccines will continue and new measures will be taken for the protection for the case of a new pandemic.
Conflict of interests
None to declare.
Glossary
ABBREVIATIONS
- PCR
Real-time polymerase chain reaction Forced Expiratory Value in 1sec (FEV1)
- FVC
Forced Vital Capacity
- DLCO
Diffusing Capacity for Lung Monoxide
- CO
Carbon monoxide
- WBC
White blood count
- WHO
World health organization
- PO2
Partial pressure of oxygen
- SPO2
Saturation of partial pressure of oxygen
- CXR
Chest x-ray
- C-RP
C-reactive protein
- BMI
Body mass index
References
- 1.Radovanovic D, Pini S, Franceschi E, Pecis M, Airoldi A, Rizzi M, Santus P. Characteristics and outcomes in hospitalized COVID-19 patients during the first 28 days of the spring and autumn pandemic waves in Milan: An observational prospective study. Respir Med. 2021;178:106323–106323. doi: 10.1016/j.rmed.2021.106323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Venkatesan S, Myles PR, Bolton KJ, Muthuri SG, Al Khuwaitir T, Anovadiya AP, Azziz-Baumgartner E, Bajjou T, Bassetti M, Beovic B, Bertisch B, Bonmarin I, Booy R, Borja-Aburto VH, Burgmann H, Cao B, Carratala J, Chinbayar T, Cilloniz C, Denholm JT, Dominguez SR, Duarte PAD, Dubnov-Raz G, Fanella S, Gao Z, Gerardin P, Giannella M, Gubbels S, Herberg J, Higuera Iglesias AL, Hoeger PH, Hu XY, Islam QT, Jimenez MF, Keijzers G, Khalili H, Kusznierz G, Kuzman I, Langenegger E, Lankarani KB, Leo YS, Libster RP, Linko R, Madanat F, Maltezos E, Mamun A, Manabe T, Metan G, Mickiene A, Mikic D, Mohn KGI, Oliva ME, Ozkan M, Parekh D, Paul M, Rath BA, Refaey S, Rodriguez AH, Sertogullarindan B, Skret-Magierlo J, Somer A, Talarek E, Tang JW, To K, Tran D, Uyeki TM, Vaudry W, Vidmar T, Zarogoulidis P, Investigators PC, Nguyen-Van-Tam JS. Neuraminidase Inhibitors and Hospital Length of Stay: A Meta-analysis of Individual Participant Data to Determine Treatment Effectiveness AmongAmong Patients Hospitalized With Nonfatal 2009 Pandemic Influenza A(H1N1) Virus Infection. J Infect Dis. 2020;221(3):356–366. doi: 10.1093/infdis/jiz152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petridis D, Zarogoulidis P, Kallianos A, Kioumis I, Trakada G, Spyratos D, Papaiwannou A, Porpodis K, Huang H, Rapti A, Hohenforst-Schmidt W, Zarogoulidis K. Clinical differences between H3N2 and H1N1 influenza 2012 and lower respiratory tract infection found using a statistical classification approach. Ther Clin Risk Manag. 2014;10:77–86. doi: 10.2147/TCRM.S57429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang W, Li X, Tang L, Wang T, He G. Characterization of the low-pathogenic H7N7 avian influenza virus in Shanghai, China. Poultry science. 2021;100(2):565–574. doi: 10.1016/j.psj.2020.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zarogoulidis P, Glaros D, Kioumis I, Terzi E, Porpodis K, Tsiotsios A, Kallianos A, Trakada G, Machairiotis N, Stylianaki A, Sakas A, Rapti A, Courcoutsakis N, Constantinidis TC, Maltezos E, Zarogoulidis K. Clinical differences between influenza A (H1N1) virus and respiratory infection between the two waves in 2009 and 2010. Int J Gen Med. 2012;5:675–682. doi: 10.2147/IJGM.S34940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muthuri SG, Venkatesan S, Myles PR, Leonardi-Bee J, Lim WS, Al Mamun A, Anovadiya AP, Araujo WN, Azziz-Baumgartner E, Baez C, Bantar C, Barhoush MM, Bassetti M, Beovic B, Bingisser R, Bonmarin I, Borja-Aburto VH, Cao B, Carratala J, Cuezzo MR, Denholm JT, Dominguez SR, Duarte PA, Dubnov-Raz G, Echavarria M, Fanella S, Fraser J, Gao Z, Gerardin P, Giannella M, Gubbels S, Herberg J, Higuera Iglesias AL, Hoeger PH, Hoffmann M, Hu X, Islam QT, Jimenez MF, Kandeel A, Keijzers G, Khalili H, Khandaker G, Knight M, Kusznierz G, Kuzman I, Kwan AM, Lahlou Amine I, Langenegger E, Lankarani KB, Leo YS, Linko R, Liu P, Madanat F, Manabe T, Mayo-Montero E, McGeer A, Memish ZA, Metan G, Mikic D, Mohn KG, Moradi A, Nymadawa P, Ozbay B, Ozkan M, Parekh D, Paul M, Poeppl W, Polack FP, Rath BA, Rodriguez AH, Siqueira MM, Skret-Magierlo J, Talarek E, Tang JW, Torres A, Torun SH, Tran D, Uyeki TM, van Zwol A, Vaudry W, Velyvyte D, Vidmar T, Zarogoulidis P, Investigators PC, Nguyen-Van-Tam JS. Impact of neuraminidase inhibitors on influenza A(H1N1)pdm09-related pneumonia: an individual participant data meta-analysis. Influenza Other Respir Viruses. 2016;10(3):192–204. doi: 10.1111/irv.12363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zarogoulidis P, Constantinidis T, Steiropoulos P, Papanas N, Zarogoulidis K, Maltezos E. Are there any differences in clinical and laboratory findings on admission between H1N1 positive and negative patients with flu-like symptoms. BMC research notes. 2011;4:4–4. doi: 10.1186/1756-0500-4-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zarogoulidis P, Glaros D, Kontakiotis T, Froudarakis M, Kioumis I, Kouroumichakis I, Tsiotsios A, Kallianos A, Steiropoulos P, Porpodis K, Nena E, Papakosta D, Rapti A, Constantinidis TC, Kerenidi T, Panopoulou M, Trakada G, Courcoutsakis N, Fouka E, Zarogoulidis K, Maltezos E. Health costs from hospitalization with H1N1 infection during the 2009-2010 influenza pandemic compared with non-H1N1 respiratory infections. Int J Gen Med. 2012;5:175–182. doi: 10.2147/IJGM.S28454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zarogoulidis P, Kouliatsis G, Papanas N, Spyratos D, Constantinidis TC, Kouroumichakis I, Steiropoulos P, Mabroudi M, Matthaios D, Kerenidi T, Courcoutsakis N, Zarogoulidis K, Maltezos E. Long-term respiratory follow-up of H1N1 infection. Virol J. 2011;8:319–319. doi: 10.1186/1743-422X-8-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Onwuamah CK, Okwuraiwe AP, Salu OB, Shaibu JO, Ndodo N, Amoo SO, Okoli LC, Ige FA, Ahmed RA, Bankole MA, Sokei JO, Mutiu BP, Ayorinde J, Saka BA, Obiekea C, Mba N, Adegbola RA, Omilabu S, Ihekweazu C, Salako BL, Audu R. Comparative performance of SARS-CoV-2 real-time PCR diagnostic assays on samples from Lagos, Nigeria. PloS one. 2021;16(2):e0246637–e0246637. doi: 10.1371/journal.pone.0246637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bostan M, Ataman M, Bostan IS, Bleotu C. Targets and assay types for COVID-19 diagnosis. J Immunoassay Immunochem. 2020;41(6):946–959. doi: 10.1080/15321819.2020.1862866. [DOI] [PubMed] [Google Scholar]
- 12.Teo AKJ, Choudhury Y, Tan IB, Cher CY, Chew SH, Wan ZY, Cheng LTE, Oon LLE, Tan MH, Chan KS, Hsu LY. Saliva is more sensitive than nasopharyngeal or nasal swabs for diagnosis of asymptomatic and mild COVID-19 infection. Scientific reports. 2021;11(1):3134–3134. doi: 10.1038/s41598-021-82787-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J, Force AET. Standardisation of spirometry. The Eur Respir J. 2005;26(2):319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 14.MacIntyre CR, Cauchemez S, Dwyer DE, Seale H, Cheung P, Browne G, Fasher M, Wood J, Gao Z, Booy R, Ferguson N. Face mask use and control of respiratory virus transmission in households. Emerg Infect Dis. 2009;15(2):233–241. doi: 10.3201/eid1502.081167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zarogoulidis P, Papanas N, Kioumis I, Chatzaki E, Maltezos E, Zarogoulidis K. Macrolides: from in vitro anti-inflammatory and immunomodulatory properties to clinical practice in respiratory diseases. European journal of clinical pharmacology. 2012;68(5):479–503. doi: 10.1007/s00228-011-1161-x. [DOI] [PubMed] [Google Scholar]
- 16.von Meijenfeldt FA, Havervall S, Adelmeijer J, Lundstrom A, Rudberg AS, Magnusson M, Mackman N, Thalin C, Lisman T. Prothrombotic changes in patients with COVID-19 are associated with disease severity and mortality. Res Pract Thromb Haemost. 2021;5(1):132–141. doi: 10.1002/rth2.12462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li LL, Wang HR, Zhou ZY, Luo J, Xiao XQ, Wang XL, Li JT, Zhou YB, Zeng Y. One-prime multi-boost strategy immunization with recombinant DNA, adenovirus, and MVA vector vaccines expressing HPV16 L1 induces potent, sustained, and specific immune response in mice. Antiviral Res. 2016;128:20–27. doi: 10.1016/j.antiviral.2016.01.014. [DOI] [PubMed] [Google Scholar]
- 18.Scoppetta C, Casciato S, Di Gennaro G. Lethality rate of the two waves of the COVID-19 pandemic in Italy. Eur Rev Med Pharmacol Sci. 2021;25(1):9–10. doi: 10.26355/eurrev_202101_24318. [DOI] [PubMed] [Google Scholar]
- 19.Muller AE, Hafstad EV, Himmels JPW, Smedslund G, Flottorp S, Stensland SO, Stroobants S, Van de Velde S, Vist GE. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Res. 2020;293:113441–113441. doi: 10.1016/j.psychres.2020.113441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tsamakis K, Gavriatopoulou M, Schizas D, Stravodimou A, Mougkou A, Tsiptsios D, Sioulas V, Spartalis E, Sioulas AD, Tsamakis C, Charalampakis N, Mueller C, Arya D, Zarogoulidis P, Spandidos DA, Dimopoulos MA, Papageorgiou C, Rizos E. Oncology during the COVID-19 pandemic: challenges, dilemmas and the psychosocial impact on cancer patients. Oncol Lett. 2020;20(1):441–447. doi: 10.3892/ol.2020.11599. [DOI] [PMC free article] [PubMed] [Google Scholar]


