Abstract
Objective
To determine whether there are racial disparities associated with mortality, cost, and length of hospital stay after surgical repair of type A acute aortic dissection (TAAAD).
Methods
Patient data from 2015 to 2018 were collected using the National Inpatient Sample. In-hospital mortality was the primary outcome. Multivariable logistical modeling was used to identify factors independently associated with mortality.
Results
Among 3952 admissions, 2520 (63%) were White, 848 (21%) were Black/African American, 310 (8%) were Hispanic, 146 (4%) were Asian and Pacific Islander (API), and 128 (3%) were classified as Other. Black/African American and Hispanic admissions presented with TAAAD at a median age of 54 years and 55 years, respectively, whereas White and API admissions presented at a median age of 64 years and 63 years, respectively (P < .0001). Additionally, there were higher percentages of Black/African American (54%; n = 450) and Hispanic (32%; n = 94) admissions living in ZIP codes with the lowest median household income quartile. Despite these differences on presentation, when adjusting for age and comorbidity, there was no independent association between race and in-hospital mortality and no significant interactions between race and income on in-hospital mortality.
Conclusions
Black and Hispanic admissions present with TAAAD a decade earlier than White and API admissions. Additionally, Black and Hispanic TAAAD admissions are more likely to come from lower-income households. After adjusting for relevant cofactors, there was no independent association between race and in-hospital mortality after surgical treatment of TAAAD.
Key Words: aortic dissection, racial disparities, type A aortic dissection
Video Abstract
Graphical abstract

No independent association found between race and TAAAD mortality.
Central Message.
Black and Hispanic patients with type A acute aortic dissection (TAAAD) present a decade earlier than White patients with TAAAD. However, there was no independent association between race and hospital mortality after TAAAD surgical treatment.
Perspective.
Although mortality rate of type A acute aortic dissection (TAAAD) has been decreasing, few studies have investigated how mortality is distributed across race. Our findings suggest that Black and Hispanic patients with TAAAD are exposed to factors that predispose them to presenting a decade earlier than White patients with TAAAD. We found no independent association between race and mortality, but further investigation is needed to determine long-term outcomes.
Type A acute aortic dissection (TAAAD) is a rare, yet severe cardiovascular disease (CVD), with an in-hospital mortality rate of 10% to 49%.1, 2, 3 Given its high mortality and morbidity, several studies have been dedicated to the diagnosis and treatment of TAAAD, and mortality rates have decreased steadily over the past several decades.4
Despite these advances, few comprehensive studies to date have investigated how these improvements in management have been distributed across race and ethnicity. This dearth of data is surprising given the significant evidence demonstrating a higher CVD burden in Black and nonwhite Hispanic patients. Several other demographic factors, such as insurance status, are significantly associated with severity of presentation and mortality from aortic procedures.5 Hypertension, a primary risk factor for TAAAD, has a higher prevalence and more severe presentation in Black and nonwhite Hispanic populations.6, 7, 8 Similarly, Black and nonwhite Hispanic patients have a higher prevalence of diabetes and dyslipidemia, and are at greater risk of developing associated cardiovascular complications.9,10 Additionally, the prevalence, complication rate, and mortality associated with acute CVD are higher in Black and nonwhite Hispanic patients.11,12
Given the existing CVD disparities, the emergent nature of TAAAD provides a unique window into the processes of surgical care. Our hypothesis was that the greater acuity of these patients would highlight or aggravate previously observed disparities in care. Further investigation might identify patient populations with a higher incidence and mortality and potentially determine opportunities for improvement in the delivery of equitable care. Therefore, in this study, we aimed to identify whether there are racial disparities associated with mortality, cost, and hospital length of stay (LOS) after surgical repair of TAAAD (Video Abstract).
Methods
Identifying the Cohort
Patient data were collected using the National Inpatient Sample (NIS) from the fourth quarter of 2015 through 2018 (n = 21,401,460). The NIS is the largest in-patient all-payer database that contains deidentified data from 20% of the nation's total discharges, representing >96% of the US population. The NIS is a restricted-access public release database and is a limited data set as defined by HIPAA [45 CFR §164.514(c)(2)]. Access is governed by a HIPAA-compliant restrictive data use agreement. This study was exempt from Institutional Review Board approval because the NIS contains deidentified patient information. Patient data in the NIS during this period were codified using the International Classification of Diseases, 10th Revision (ICD-10) codes.
The NIS database receives racial demographic data from state-level partner organizations but does not record how each state collects demographic data. The database contains RACE as a combined racial/ethnic demographic variable with the following options: White, Black, Hispanic, Asian and Pacific Islander, Native American, and Other. If a data source provided both racial and ethnic data for an admission (ie, race, Black; ethnicity, Hispanic), the NIS ethnic data take precedence.
Identifying the TAAAD Patient Population
Patients were identified as having a TAAAD using the following criteria. Patients with aortic dissection were identified using the thoracic or thoracoabdominal aortic dissection ICD-10 codes (I71.01, I71.03; n = 18,431). Patients who underwent surgery for TAAAD were selected through any admission that included a surgical procedure code on the ascending aorta (n = 4943) (Table E1). It should be noted that coding of dissection does not permit distinction of ascending aortic dissection from any thoracic or thoracoabdominal dissection. Therefore, the only way to distinguish ascending aortic dissection was through the surgical codes, which make this distinction. Therefore, assessment of patients who may have presented with TAAAD but did not have surgery cannot be identified in this database. To distinguish patients with a TAAAD, nonelective admissions were selected (n = 4188) (Figure 1). We then stratified the patient population based on the RACE variable from the NIS and removed admissions with no associated RACE value (n = 236), which created a final cohort of 2520 White admissions, 848 Black/African American admissions, 310 Hispanic admissions, 146 API admissions, and 128 admissions identified as “Other.”
Figure 1.
Type A acute aortic dissection cohort selection was done using the National Inpatient Sample database for 2015 to 2018. Nonelective admissions were included if there was a thoracic or thoracoabdominal dissection diagnosis code and a surgical procedure code on the ascending aorta for a final cohort of 4204 admissions. This cohort was then stratified by the race variable. API, Asian and Pacific Islander.
Demographic data, including age, socioeconomic status, and insurance status, and hospital data, including teaching status, region, and bed size, are provided by the NIS for each admission. Comorbidity conditions, including hypertension, prior cardiac surgery, diabetes, and peripheral vascular disease 2, were defined by a combination of ICD-10 diagnosis and procedural codes and stratified by the NIS race category (Table E2).
Defining Outcomes
The primary outcome for the study was in-hospital mortality of TAAAD, measured by the DIED variable. Secondary outcomes included LOS and cost of stay (TOTCHG). All charges were adjusted using the cost-to-charge ratio data provided in supplemental NIS files. Postprocedural complications were identified as a secondary outcome by combining several ICD-10 diagnosis and procedural codes (Table E3). The metric “any complication” was defined as any admission containing any ICD-10 code that described a postprocedural complication. Because the NIS does not use “present on admission” modifiers, it was difficult to determine whether certain complications, such as stroke and renal failure, were antecedent or subsequent to the surgical procedure and therefore are not reported or included in the primary outcome analysis.
Statistical Analysis
To identify significant differences between racial groups in both the demographic and comorbid variables, we performed the chi-square or Fisher exact test, as appropriate, for frequency analysis of discrete variables. For continuous demographic variables, which were all non-normally distributed via Kolmogorov–Smirnov/Shapiro–Wilk tests, the Kruskal–Wallis test was used to determine significance. Factors that varied significantly among different racial groups were identified using a 2-sided P value < .05. These variables were included in a multivariable regression model to determine race’s independent impact on the primary and secondary outcomes. To minimize missing data (n = 322), the “missRanger” R package was used for imputation before regression modeling. Admissions with an ICD-10 code included in Ehlers–Danlos syndrome, Turner syndrome, or congenital aortic insufficiency were excluded from multivariable regression modeling owing to insufficient sample size, per NIS HIPAA restrictions. The “other” racial category also was excluded from multivariable regression modeling. Two comorbidity index scores (readmit_score, mortal_score) were calculated using the Elixhauser Comorbidity software. Cubic spline regression was done to determine the relationship between the Elixhauser Comorbidity Index and mortality (Figure E1), and 0 was chosen as an inflection point to redefine the Elixhauser score as a dichotomous variable.
Figure E1.
Cubic spline of the Elixhauser comorbidity index.
Results
Demographics
Using the NIS, from the fourth quarter of 2015 to 2018, we identified a final TAAAD cohort of 3952 patient admissions. Sixty-three percent of these admissions were White (n = 2520), 21% were Black/African American (n = 848), 8% were Hispanic (n = 310), 4% were API (n = 146), and 3% identified as Other (n = 128) (Figure 2).
Figure 2.
Type A acute aortic dissection (TAAAD) cohort by race. The final cohort of TAAAD admissions included 2520 White admissions, 848 Black admissions, 310 Hispanic admissions, 146 Asian and Pacific Islander (API) admissions, and 128 admissions classified as Other.
The majority of admissions in each racial group were from large urban teaching hospitals (Table 1). Most of Black/African American (52%) and Hispanic (42%) admissions were in hospitals located in the South, and the majority of API (71%) admissions were at hospitals in the West. Conversely, White admissions were distributed evenly throughout the various hospital regions (P < .0001) (Table 1).
Table 1.
Demographic and comorbid characteristics of patients with TAAAD
| Characteristic | White (N = 2520) | Black/African American (N = 848) | Hispanic (N = 310) | API (N = 146) | Other (N = 128) | P value |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Female sex, n (%) | 876 (35) | 290 (34) | 82 (26) | 58 (40) | 50 (39) | .02 |
| Age, yr, median (IQR) | 64 (54-73) | 54 (45-62) | 55 (45-65) | 63 (53-72) | 57 (49.5-68.5) | <.0001 |
| Insurance status, n (%) | <.0001 | |||||
| Medicare | 1208 (48) | 222 (26) | 82 (26) | 52 (36) | 42 (33) | |
| Medicaid | 282 (11) | 208 (25) | 70 (23) | 30 (21) | 32 (25) | |
| Private insurance | 860 (34) | 308 (37) | 108 (35) | 54 (37) | 40 (32) | |
| Self-pay | 96 (4) | 66 (8) | 34 (11) | 8 (5) | 10 (8) | |
| No charge | 6 (0.2) | 12 (1) | 2 (1) | 0 (0) | 0 (0) | |
| Other | 58 (2) | 26 (3) | 14 (5) | 2 (1) | 2 (2) | |
| Median household income, percentile, n (%) | <.0001 | |||||
| 0-25 | 522 (21) | 450 (54) | 94 (32) | 14 (10) | 34 (27) | |
| 26-50 | 582 (24) | 154 (19) | 64 (22) | 32 (23) | 28 (22) | |
| 51-75 | 684 (28) | 120 (15) | 82 (28) | 22 (15) | 20 (16) | |
| 75-100 | 676 (27) | 102 (12) | 56 (19) | 74 (52) | 44 (35) | |
| Patient location, n (%) | <.0001 | |||||
| “Central” metro counties ≥1 million people | 562 (23) | 390 (47) | 160 (54) | 72 (51) | 72 (57) | |
| “Fringe” metro counties ≤1 million people | 680 (27) | 158 (19) | 62 (21) | 28 (20) | 38 (30) | |
| Metro counties with 250,000-999,999 people | 560 (22) | 162 (19) | 58 (19) | 30 (21) | 8 (6) | |
| Metro counties with 50,000-249,999 people | 258 (10) | 54 (6) | 6 (2) | 6 (4) | 2 (2) | |
| Micropolitan counties | 262 (11) | 28 (3) | 4 (1) | 2 (1) | 4 (3) | |
| Non-metro/micropolitan counties | 172 (7) | 44 (5) | 8 (3) | 4 (3) | 2 (2) | |
| Hospital region, n (%) | <.0001 | |||||
| Northeast | 546 (22) | 102 (12) | 52 (17) | 10 (7) | 48 (38) | |
| Midwest | 602 (24) | 214 (25) | 12 (4) | 20 (14) | 14 (11) | |
| South | 762 (30) | 438 (52) | 130 (42) | 12 (8) | 32 (25) | |
| West | 610 (24) | 94 (11) | 116 (37) | 104 (71) | 34 (27) | |
| Hospital division, n (%) | <.0001 | |||||
| New England | 166 (7) | 20 (2) | 12 (4) | 2 (1) | 4 (3) | |
| Middle Atlantic | 380 (15) | 82 (10) | 40 (13) | 8 (5) | 44 (34) | |
| East North Central | 404 (16) | 182 (21) | 6 (2) | 10 (7) | 12 (9) | |
| West North Central | 198 (8) | 32 (4) | 6 (2) | 10 (7) | 2 (2) | |
| South Atlantic | 432 (17) | 268 (32) | 72 (23) | 8 (5) | 16 (13) | |
| East South Central | 154 (6) | 76 (9) | 6 (2) | 2 (1) | 0 (0) | |
| West South Central | 176 (7) | 94 (11) | 52 (17) | 2 (1) | 16 (13) | |
| Mountain | 188 (7) | 22 (3) | 16 (5) | 4 (3) | 2 (2) | |
| Pacific | 422 (17) | 72 (8) | 100 (32) | 100 (68) | 32 (25) | |
| Hospital size, n (%) | .42 | |||||
| Small | 142 (6) | 46 (5) | 16 (5) | 10 (7) | 8 (6) | |
| Medium | 452 (18) | 130 (15) | 56 (18) | 18 (12) | 16 (13) | |
| Large | 1926 (76) | 672 (79) | 238 (77) | 118 (81) | 104 (81) | |
| Hospital teaching status, n (%) | .0003 | |||||
| Rural | 26 (1) | 4 (1) | 2 (1) | 0 (0) | 0 (0) | |
| Urban nonteaching | 196 (9) | 28 (4) | 22 (8) | 14 (11) | 6 (5) | |
| Urban teaching | 2012 (90) | 722 (96) | 250 (91) | 118 (89) | 108 (95) | |
| Comorbidities, n (%) | ||||||
| Hypertension | 1982 (79) | 784 (92) | 274 (88) | 122 (84) | 110 (86) | <.0001 |
| Peripheral vascular disease | 48 (2) | 24 (3) | 2 (1) | 0 (0) | 0 (0) | .02 |
| Chronic ischemic heart disease | 610 (24) | 150 (18) | 52 (17) | 28 (19) | 26 (20) | .0002 |
| Cardiac inflammation | 14 (1) | 2 (0.2) | 0 (0) | 2 (1) | 0 (0) | .19 |
| History of transient ischemic attack/cerebral infarction | 110 (4) | 26 (3) | 22 (7) | 4 (3) | 10 (8) | .009 |
| History of circulatory disease | 80 (3) | 22 (3) | 2 (1) | 0 (0) | 0 (0) | .005 |
| Prior cardiac surgery | 232 (9) | 50 (6) | 24 (8) | 10 (7) | 12 (9) | .04 |
| Presence of cardiac pacemaker | 52 (2) | 8 (1) | 2 (1) | 2 (1) | 0 (0) | .05 |
| Preoperative shock | 576 (23) | 166 (20) | 78 (25) | 26 (18) | 24 (19) | .09 |
| Aortic aneurysm | 274 (11) | 68 (8) | 24 (8) | 16 (11) | 28 (22) | <.0001 |
| Chronic obstructive pulmonary disease | 336 (13) | 108 (13) | 16 (5) | 14 (10) | 18 (14) | .001 |
| Diabetes | 188 (7) | 106 (13) | 36 (12) | 10 (7) | 4 (3) | <.0001 |
| Chronic kidney disease | 346 (13.7) | 280 (33) | 70 (22.6) | 26 (17.8) | 18 (14.1) | <.0001 |
| Obesity | 278 (11) | 150 (18) | 50 (16) | 6 (4) | 12 (9) | <.0001 |
| Noncompliance | 4 (0.2) | 4 (0.5) | 0 (0) | 0 (0) | 0 (0) | .35 |
| Marfan disease | 48 (1.9) | 12 (1.4) | 8 (2.5) | 0 (0) | 2 (1.6) | .31 |
API, Asian and Pacific Islander; IQR, interquartile range; TAAAD, type A acute aortic dissection.
Although hospital size did not differ by racial group (P = .42), there was a discrepancy in the age at admission (P < .0001). Black/African American and Hispanic admissions presented with TAAAD at a median age of 54 years and 55 years, respectively, whereas White and API admissions presented at a median age of 64 years and 63 years, respectively. On average, these data demonstrate that Black/African American and Hispanic admissions present with TAAAD approximately a decade earlier than their White and API counterparts nationwide.
The majority of Black/African American (47%), Hispanic (54%), and API (51%) admissions were in urban, densely populated metro counties. In contrast, there was a more even distribution of White admissions between urban and metro counties (P < .0001). Furthermore, consistent with the literature,13 higher percentages of Black/African American (54%) and Hispanic admissions (32%) lived in ZIP codes belonging to the lowest median household income quartile ($0 to ∼$44,000). Comparatively, the highest percentage of White admissions (28%) lived in ZIP codes from the third-highest household income quartile (∼$55,000 to $74,000), and the highest percentage of API admissions (52%) lived in ZIP codes in the highest household median quartile ($74,000+) (P < .0001). Additionally, Black/African American (25%) patients had the highest percentage of admissions covered by Medicaid. Given that White and API admissions tended to be older than other racial groups, they correspondingly had higher percentages of their admissions covered by Medicare (White, 48%; API, 36%) (P < .0001).
Comorbidity Trends
The most widely reported comorbidities for TAAAD include cardiovascular conditions, such as hypertension, diabetes, and prior cardiac surgery, have previously been demonstrated to be present at higher rates in underserved patient populations.10, 11, 12 Similarly, in our TAAAD admissions cohort, 92% of Black/African American admissions, 88% of Hispanic admissions, and 84% of API admissions had a diagnosis of hypertension, compared to 79% of White admissions (P < .0001) (Table 1). Additionally, there were higher rates of diabetes and obesity in Black/African American and Hispanic admissions (P = .0001) (Table 1). Chronic ischemic heart disease was found at a higher proportion in White admissions (24%) compared to Black/African American admissions (18%), Hispanic admissions (17%), and API admissions (19%) (P = .0002). Rates of preoperative shock were largely comparable across the different racial groups (P = .09).
Primary and Secondary Outcomes
When studying our primary outcome of in-hospital mortality, White admissions had the highest raw mortality at 17%, and Black/African American admissions had the lowest rate of raw mortality at 11% (P < .0001) (Table 2). There were no significant differences among racial groups in several different types of postoperative complications, including pulmonary complications, hemorrhage, and stroke (all P > .05). API admissions had the highest rate of postprocedural shock/cardiac failure (22%), and Black/African American admissions had the lowest rate of postprocedural shock/cardiac failure (13%). Similarly, API admissions had the highest rates of adverse reactions following a procedure (23%), whereas Black/African American and Hispanic admissions had the lowest (12% and 14%, respectively). The overall complication rate also was not significantly different across the racial groups (P = .24) (Table 2).
Table 2.
Unadjusted mortality and complication rates of TAAAD
| Outcomes | White (N = 2520) | Black/African American (N = 848) | Hispanic (N = 310) | API (N = 146) | Other (N = 128) | P value |
|---|---|---|---|---|---|---|
| Discharge status, n (%) | ||||||
| Died | 438 (17) | 90 (11) | 38 (12) | 22 (15) | 14 (11) | <.0001 |
| Resource utilization | ||||||
| Length of stay, d, median (IQR) | 10 (6-16) | 11 (7-18) | 11 (7-17) | 11 (7-16) | 13.5 (7.5-23) | <.0001 |
| Total cost, USD, median (IQR) | 290,259 (195,413-459,875) | 291,043 (201,132-485,816) | 364,646 (252,824-634,016) | 291,469 (205,979-584,779) | 368,511 (231,915-620,019) | <.0001 |
| Complications | ||||||
| Any complication | 1142 (45) | 374 (44) | 138 (45) | 70 (48) | 70 (55) | .24 |
| Postprocedure shock/cardiac failure | 400 (16) | 110 (13) | 46 (15) | 32 (22) | 32 (25) | .002 |
| Pulmonary complications | 616 (24) | 240 (28) | 76 (25) | 28 (19) | 36 (28) | .07 |
| Hemorrhage/hematoma/seroma | 182 (7) | 72 (8) | 22 (7) | 8 (5) | 12 (9) | .55 |
| Stroke | 52 (2) | 12 (1) | 2 (1) | 4 (3) | 4 (3) | .22 |
| Adverse reaction | 430 (17) | 102 (12) | 42 (14) | 34 (23) | 34 (27) | <.0001 |
| Catheter-related complication | 14 (1) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | .09 |
| Postprocedure hypertension | 14 (1) | 8 (1) | 6 (2) | 2 (1) | 0 (0) | .06 |
| Other unspecified complications | 24 (1) | 4 (0.5) | 2 (1) | 0 (0) | 0 (0) | .36 |
API, Asian and Pacific Islander; IQR, interquartile range; TAAAD, type A acute aortic dissection.
Another secondary outcome that we investigated was resource utilization. Black/African American, Hispanic, and API admissions all had a median LOS of 11 days, and White admissions had a median LOS of 10 days (P < .0001) (Table 2). Additionally, Hispanic admissions had the highest total cost at $364,646, and White admissions had the lowest total cost at $290,259 (P < .0001).
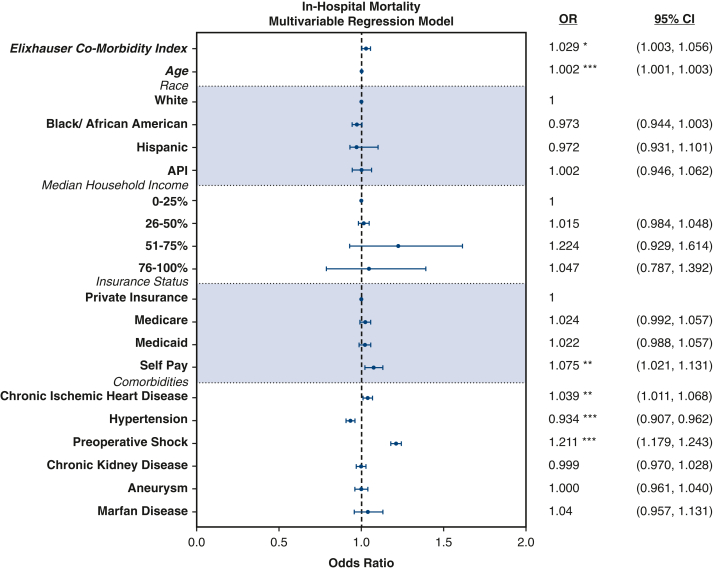
Multivariable Regression Model
After determining the demographic and comorbid factors that differed significantly among racial groups, we built multivariable logistic regression models using these variables to determine race’s independent association with mortality. The Elixhauser Comorbidity Index, a composite comorbidity score validated for use with administrative data, was significantly associated with mortality (odds ratio [OR], 1.029; 95% confidence interval [CI], 1.003-1.056). While the highest raw mortality was observed in White admissions, there was ultimately no association between race and hospital mortality in our multivariable model (Table 3, Figure 3). Additionally, median household income and hospital location also were not associated with mortality. We also ran analyses with several interaction variables to check for an interaction between race or median income in the setting of TAAAD mortality, but found none (Table 4). However, several comorbid variables, including increasing age (OR, 1.002; 95% CI, 1.001-1.003), chronic ischemic heart disease (OR, 1.039; 95% CI, 1.011-1.068), and preoperative shock (OR, 1.211; 95% CI, 1.011-1.068), were associated with higher mortality in TAAAD admissions. Private insurance status was more protective against TAAAD in-hospital mortality compared to the self-pay option (OR, 1.075; 95% CI, 1.021-1.131). Unexpectedly, hypertension was associated with a protective effect against mortality from TAAAD (OR, 0.934; 95% CI, 0.907-0.962). Chronic kidney disease (OR, 0.999; 95% CI, 0.970-1.028), aneurysm (OR, 1.000; 95% CI, 0.961-1.040), and Marfan syndrome (OR, 1.04; 95% CI, 0.957-1.131) showed no association with mortality.
Figure 3.
Multivariable regression model of in-hospital mortality. Forest plot representation of a multivariable regression model of in-hospital mortality, showing the Elixhauser Comorbidity Index, age, and race. Both the Elixhauser Comorbidity Index (odds ratio [OR], 1.046; 95% confidence interval [CI], 1.001-1.093) and age (OR, 1.029; 95% CI, 1.017-1.041) were independently associated with type A acute aortic dissection in-hospital mortality. However, race was not found to be independently associated with mortality. ∗P ≤ .05, ∗∗P ≤ .01, ∗∗∗P ≤ .001. API, Asian and Pacific Islander.
Table 3.
Independent variables associated with mortality, length of stay, and cost of stay for TAAAD
| Variable | OR/estimate∗ | 95% CI | P value |
|---|---|---|---|
| In-hospital mortality | |||
| Age | 1.002 | 1.001-1.003 | <.0001 |
| Elixhauser comorbidity index | 1.029 | 1.003-1.056 | .027 |
| Race | |||
| White (reference) | |||
| Black/African American | 0.973 | 0.944-1.003 | .072 |
| Hispanic | 0.972 | 0.931-1.1013 | .2 |
| API | 1.002 | 0.946-1.062 | .933 |
| Median household income percentile | |||
| 0-25 | 1 | ||
| 26-50 | 1.015 | 0.984-1.048 | .346 |
| 51-75 | 1.224 | 0.929-1.614 | .367 |
| 76-100 | 1.047 | 0.787-1.392 | .720 |
| Insurance | |||
| Private insurance | 1 | ||
| Medicare | 1.024 | 0.992-1.057 | .137 |
| Medicaid | 1.022 | 0.988-1.057 | .214 |
| Self-pay | 1.075 | 1.021-1.131 | .006 |
| Other | 0.995 | 0.930-1.065 | .322 |
| Hypertension | 0.934 | 0.907-0.962 | <.0001 |
| Chronic ischemic heart disease | 1.039 | 1.011-1.068 | .006 |
| Preoperative shock | 1.211 | 1.179-1.243 | <.0001 |
| Chronic kidney disease | 0.999 | 0.970-1.028 | .937 |
| Aneurysm | 1.000 | 0.961-1.040 | .993 |
| Marfan syndrome | 1.04 | 0.957-1.131 | .351 |
| Length of stay | |||
| Elixhauser comorbidity index | 1.256 | 0.358-2.156 | .006 |
| Race | |||
| White (reference) | 1 | ||
| Black/African American | 0.327 | −0.725 to 1.380 | .5 |
| Hispanic | 1.615 | 0.142-3.088 | .032 |
| API | 0.452 | −1.566 to 2.471 | .66 |
| Insurance status | |||
| Private insurance | 1 | ||
| Medicare | 0.672 | −0.425 to 1.768 | .229 |
| Medicaid | 1.900 | 0.705-3.086 | .001 |
| Self-pay | −1.844 | −3.639 to −0.049 | .044 |
| Other | −3.285 | −9.016 to 2.446 | .261 |
| Median household income percentile | |||
| 0-25 | 1 | ||
| 26-50 | −2.0633 | −3.516 to −1.311 | <.0001 |
| 51-75 | −2.1297 | −3.619 to −1.433 | <.0001 |
| 76-100 | −1.2002 | −3.041 to −0.803 | .0348 |
| Hypertension | −1.701 | −2.738 to −0.664 | .001 |
| Chronic ischemic heart disease | −0.290 | −1.243 to 0.669 | .556 |
| Preoperative shock | 1.675 | 0.745-2.605 | <.0001 |
| Chronic kidney disease | 3.800 | 2.781-4.812 | <.0001 |
| Aneurysm | −0.955 | −2.322 to 0.413 | .171 |
| Marfan syndrome | 6.558 | 3.651-9.465 | <.0001 |
| Associated cost, USD | |||
| Elixhauser comorbidity index | 85,140.79 | 53,726.66-116,554.92 | <.0001 |
| Race | |||
| White (reference) | 1 | ||
| Black/African American | −3046.50 | −39,814.08 to 33,721.08 | .871 |
| Hispanic | 156,616.55 | 105,193.82-208,039.28 | <.0001 |
| API | 249,059.36 | 177,622.48-320,496.23 | <.0001 |
| Insurance status | |||
| Private insurance | 1 | ||
| Medicare | 11,087.86 | −4883.800 to 71,790.56 | .087 |
| Medicaid | 6171.81 | −17,133.25 to 66,078.58 | .249 |
| Self-pay | −17,023.80 | −120,779.43 to 4602.75 | .069 |
| Other | 19,325.53 | −244,740.33 to 155,398.20 | .662 |
| Median household income percentile, n (%) | |||
| 0-25 | 1 | ||
| 26-50 | −5020.85 | (−43,587.93, 33,546.23) | .799 |
| 51-75 | −19,933.29 | (−58,132.83, 18,266.25) | .306 |
| 76-100 | 41,412.52 | (2211.11, 80,613.93) | .038 |
| Hypertension | −63,238.99 | (−99,445.26, −27,032.71) | .0006 |
| Chronic ischemic heart disease | −31,608.43 | (−65,011.43, 1794.56) | .064 |
| Preoperative shock | 123,883.67 | (91,403.90, 156,363.44) | <.0001 |
| Chronic kidney disease | 128,167.62 | (92,702.63, 163,632.61) | <.0001 |
| Aneurysm | −46,862.50 | (−94,720.90, 995.91) | .055 |
| Marfan syndrome | 66,230.72 | −35,270.98 to 167,732.42 | .201 |
Italics denote statistical significance with P value <.05.
OR, Odds ratio; CI, confidence interval; API, Asian and Pacific Islander; TAAAD, type A acute aortic dissection.
OR for in-hospital mortality; estimates for length of stay and associated cost.
Table 4.
Median household income interaction analysis on independent association of race and mortality
| Race × income interactions | DF | OR | 95% CI |
|---|---|---|---|
| Black × quartile 2 | 1 | 1.037 | 0.962-1.116 |
| Black × quartile 3 | 1 | 1.038 | 0.959-1.123 |
| Black × quartile 4 | 1 | 0.986 | 0.907-1.072 |
| Hispanic × quartile 2 | 1 | 1.143 | 0.954-1.281 |
| Hispanic × quartile 3 | 1 | 1.047 | 0.939-1.168 |
| Hispanic × quartile 4 | 1 | 0.928 | 0.824-1.046 |
| API × quartile 2 | 1 | 0.859 | 0.699-1.056 |
| API × quartile 3 | 1 | 0.891 | 0.718-1.106 |
| API × quartile 4 | 1 | 0.832 | 0.692-1.000 |
DF, Degrees of freedom; OR, odds ratio; CI, confidence interval; API, Asian and Pacific Islander.
Although there was no association between race and mortality, we found that race was significantly associated with our secondary outcomes. Specifically, Hispanic admissions were associated with both increased LOS (day 1.615; 95% CI, 0.142-3.088) and increased cost of stay (cost $156,615.55; 95% CI, $105,193.82-$208,039.28) compared to White admissions. Interestingly, API admissions also showed an increased cost of stay (cost 249,059.36, 95% CI 177,622.48-320,496.23). Demographic characteristic such as median household income and insurance status, and comorbid variables, such as hypertension, ischemic heart disease, and preoperative shock, also were associated with both LOS and cost of stay (Table 3).
Discussion
TAAAD is an acute medical condition with a high mortality and severe postoperative complications. Given these risks, and the emergent nature of treatments, this syndrome provides a unique opportunity to investigate the impact of race and ethnicity on presentation and outcomes associated with emergent cardiac surgical care. Our results show that Black and Hispanic admissions present with TAAAD a decade earlier than White and API admissions. We also found that higher proportions of Black/African American and Hispanic admissions were from the lowest median household income quartile and had Medicaid insurance. Despite these differences on presentation, we found no significant association between race and surgical TAAAD in-hospital mortality. Hispanic admissions were associated with longer LOS and higher cost of stay, and API admissions had a higher associated cost of stay (Video 1).
These data suggest that Black and Hispanic patients may be exposed to healthcare disparities that precede and predispose patients to TAAAD. Black and Hispanic patients were shown to present with TAAAD a decade earlier than White and API patients, suggesting greater exposure to TAAAD risk factors earlier in life. Two factors that may contribute to this earlier age of onset are insurance status and socioeconomic status. In our TAAAD cohort, we found higher rates of Black/African American and Hispanic patients who either were from the lowest median income quartile or were covered by Medicaid. Patients of lower socioeconomic status have been shown to have poorer access to healthy diet, are at higher risk for developing substance abuse disorders, and have higher rates of hypertension, obesity, and diabetes, all of which are risk factors for TAAAD.14 Therefore, reducing early exposure through primary prevention may be an effective strategy to address the early presentation of minority patients.
Discrimination by healthcare providers in the primary care context also may contribute to these differences in presentation. Physicians have been shown to carry implicit bias against underserved patient populations, perceiving Black and Hispanic patients as “less cooperative, less compliant, and less responsible.”15 Treatment biases such as these understandably have led to a growing distrust of healthcare providers and the treatments that they prescribe in underrepresented patient populations.7 One observed effect is a lower rate of adherence to hypertensive medication regimens in Black patient populations, which is a reported risk factor for TAAAD.7 Strengthening these provider–patient relationships can improve earlier screening and improve treatment adherence, which may reduce the risk for TAAAD.
Despite disparities in presentation, it is encouraging that we found no racial disparities when looking at the association between race and TAAAD surgical mortality. This remained true even with the addition of several interaction factors, such as socioeconomic status. Interestingly, these findings run counter to other acute cardiovascular conditions. For example, Black patients have been reported to have worse surgical outcomes after abdominal aortic aneurysm repair, vascular trauma, and hemodialysis.16, 17, 18 Black race has been associated with increased mortality in coronary artery bypass surgery, even after accounting for socioeconomic and clinical factors.19 Results are not uniform for all cardiac operations, however. A recent analysis in Michigan revealed that, when adjusting for clinical factors, race was not associated with mitral surgical selection or with operative outcome.20
Although not the case for all surgical emergencies, it may be the case that an aspect of TAAAD surgical treatment is able to equitably address the immediate mortality risk in all patient populations. Similarly, Yammine and colleagues18 found that Black TAAAD patients presented earlier with greater comorbidities compared to White patients but had a lower in-hospital mortality rate. However, they also found significantly higher reintervention rates in Black patients, which also was noted in the Michigan mitral study, which similarly points to the fact that although surgical or endovascular treatment may benefit minority patient populations in the immediate context, care beyond the acute setting may need significant improvement.
Additionally, we found that Hispanic admissions were the only ethnic group demonstrating longer LOS. Interestingly, we found no significant difference in the total postoperative complication rate when stratified by race, a variable that drives longer hospital admissions (Table 2). This finding could be due to a limitation of the NIS database, as we were unable to study many of the complications commonly associated with TAAAD, such as acute myocardial infarction, acute kidney injury, and pulmonary embolism. However, several studies also demonstrated prolonged LOS in Hispanic patient populations despite a similar rate of complications.21, 22, 23, 24 It has been speculated that these race-specific differences could be due to disparities in housing security, which could affect safe hospital discharge. Another possibility is that this prolonged LOS is a reflection of provider bias, which has been shown to foster patient distrust, poor patient–provider communication, and greater patient stress, all of which could impact a patient’s postoperative course.
We also found that Hispanics and API admissions had higher costs of stay. This finding is less likely to be fully attributable to LOS, given that Hispanic admissions were longer by only 1 day, and API admissions were not found to be significantly longer. The higher cost of API admissions may be related to the finding that a higher proportion of API admissions belonged to the highest income quartile. These patients may access specialty care that may lead to higher costs without a corresponding increase in LOS. However, owing to the heterogeneity of these patient populations, and the lack of data surrounding previous access to healthcare and common complications, further study with a clinically driven descriptive database may be necessary to understand this difference in outcome.
Other studies using self-reporting methods have also pointed to likely racial disparities in aortic dissection. In a small retrospective study looking at a single institution, Black patients with aortic dissection were significantly younger, had poorer hypertension control, and required a greater number of reinterventions than their white counterparts.8 Owing to the rarity of acute aortic dissection, the study included a cohort of only 126 patients with type B aortic dissections. Another retrospective study investigating all acute hospitals in Maryland observed higher rates of hospitalization for all aortic dissections in non-White patients.9 Additionally, one nationwide study investigating the different types of aortic dissection in the early 2000s listed race as a significant determinant of mortality but failed to investigate this finding further.4 Although limited in scope, each of these studies pointed toward existing racial disparities in the development and presentation of aortic dissection, but further investigation is needed to gain a more comprehensive understanding of how this condition impacts underrepresented patient populations across the entire spectrum of disease.
Our study was subject to several limitations. First, the NIS does not distinguish whether a condition was present on admission or was a postoperative complication. Therefore, even though we did not observe differences in mortality, further investigation is needed to identify any significant differences in complications among racial groups. The NIS contains only deidentified admission data, which prevented longitudinal analysis of any individual patient’s care. For instance, we were unable to determine access to medical care prior to the patient’s TAAAD admission, nor were we able to study any follow-up care or longitudinal mortality. For instance, we were unable to determine differences in aneurysm burden between racial groups on admission, as the NIS does not provide clear indicators between diagnoses present on admission versus a postoperative complication. Additionally, because the NIS is an administrative database, it provides no diagnostic clinical details of a patient’s status that would have been included in a clinical registry. For example, we were not able to distinguish between patients who had well-controlled hypertension and those with poorly controlled hypertension, which would have a significant impact on the development of TAAAD. Finally, because we focused on patients who had undergone surgery, the data did not permit us to identify patients presenting with TAAAD who did not undergo surgery and thus may have masked potential selection bias.
Conclusions
Black/African American and Hispanic TAAAD admissions have higher rates of Medicaid coverage and hypertension, and lower socioeconomic status compared to their White and API counterparts. Additionally, Black and Hispanic patients present with TAAAD 10 years younger than their White and API counterparts. Despite these disparities, after adjusting for potential confounding variables, there was no association between race and TAAAD surgical mortality, but Hispanic TAAAD admissions were found to have longer LOS and higher costs of stay, and API admissions had higher costs of stay, compared to White admissions. Further investigation is needed to identify any racial disparities in associated postoperative complications in addition to other phases of care (Figure 4).
Figure 4.
Graphic abstract.
Conflict of Interest Statement
The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Footnotes
Funding for this work was provided by a National Heart, Lung and Blood InstituteT35 training grant.
The National Inpatient Sample (NIS) is a restricted access public release database under strict internal security and is a limited data set as defined by HIPAA (45 CFR §164.514(c)). Access is governed by a HIPAA-compliant restrictive data use agreement. This study was considered exempt from Institutional Review Board approval because the Healthcare Cost and Utilization Project-NIS contains deidentified patient information.
Supplementary Data
Summary of the article's purpose, main findings, and significance. Video available at: https://www.jtcvs.org/article/S2666-2736(23)00028-1/fulltext.
Racial disparities in surgical treatment of type A acute aortic dissection. Video available at: https://www.jtcvs.org/article/S2666-2736(23)00028-1/fulltext
Appendix 1
Table E1.
ICD-10 surgical procedure codes for the ascending aorta
| ICD-10 code | Description |
|---|---|
| 02QX0ZZ | Repair thoracic aorta, ascending/arch, open approach |
| 02UX07Z | Supplement thoracic aorta, ascending/arch with autologous tissue substitute, open approach |
| 02UX08Z | Supplement thoracic aorta, ascending/arch with zooplastic tissue, open approach |
| 02UX0JZ | Supplement thoracic aorta, ascending/arch with synthetic substitute, open Approach |
| 02UX0KZ | Supplement thoracic aorta, ascending/arch with nonautologous tissue substitute, open approach |
| 02VX0CZ | Restriction of thoracic aorta, ascending/arch with extraluminal device, open approach |
| 02VX0DZ | Restriction of thoracic aorta, ascending/arch with intraluminal device, open approach |
| 02VX0EZ | Restriction of thoracic aorta, ascending/arch with branched or fenestrated intraluminal device, one or two arteries, open approach |
| 02VX0FZ | Restriction of thoracic aorta, ascending/arch with branched or fenestrated intraluminal device, three or more arteries, open approach |
| 02VX0ZZ | Restriction of thoracic aorta, ascending/arch, open approach |
| 02BX0ZZ | Excision of thoracic aorta, ascending/arch, open approach |
| 02RX07Z | Replacement of thoracic aorta, ascending/arch with autologous tissue substitute, open approach |
| 02RX08Z | Replacement of thoracic aorta, ascending/arch with zooplastic tissue, open approach |
| 02RX0JZ | Replacement of thoracic aorta, ascending/arch with synthetic substitute, open approach |
| 02RX0KZ | Replacement of thoracic aorta, ascending/arch with nonautologous tissue substitute, open approach |
ICD-10, International Classification of Diseases, Tenth Revision.
Table E2.
ICD-10 codes for comorbidities
| ICD-10 code | Description |
|---|---|
| Hypertension | |
| I10 | Essential (primary) hypertension |
| I11 | Hypertensive heart disease |
| I12 | Hypertensive kidney disease |
| I13 | Hypertensive heart and chronic kidney disease |
| I15 | Secondary hypertension |
| I16 | Hypertensive crisis |
| I110 | Hypertensive heart disease with heart failure |
| I119 | Hypertensive heart disease without heart failure |
| I120 | Hypertensive chronic kidney disease with stage 5 chronic kidney disease or end stage renal disease |
| I129 | Hypertensive chronic kidney disease with stage 1 through stage 4 chronic kidney disease, or unspecified chronic kidney disease |
| I130 | Hypertensive heart and chronic kidney disease with heart failure and stage 1 through stage 4 chronic kidney disease or unspecified chronic kidney disease |
| I1310 | Hypertensive heart and chronic kidney disease without heart failure with stage 1 through stage 4 chronic kidney disease, or unspecified chronic kidney disease |
| I1311 | Hypertensive heart and chronic kidney disease without heart failure with stage 5 chronic kidney disease, or end stage renal disease |
| I132 | Hypertensive heart and chronic kidney disease with heart failure with stage 5 chronic kidney disease, or end stage renal disease |
| I150 | Renovascular hypertension |
| I151 | Hypertension secondary to other renal disorders |
| I152 | Hypertension secondary to endocrine disorders |
| I158 | Other secondary hypertension |
| I159 | Secondary hypertension, unspecified |
| I160 | Hypertensive urgency |
| I161 | Hypertensive emergency |
| I169 | Hypertensive crisis, unspecified |
| Peripheral vascular disease | |
| I70 | Atherosclerosis |
| I701 | Atherosclerosis of renal artery |
| I702 | Atherosclerosis of native arteries of the extremities |
| I7020 | Unspecified atherosclerosis of native arteries of extremities |
| I70201 | Unspecified atherosclerosis of native arteries of extremities right leg |
| I70202 | Unspecified atherosclerosis of native arteries of extremities left leg |
| I70203 | Unspecified atherosclerosis of native arteries of extremities bilateral legs |
| I70208 | Unspecified atherosclerosis of native arteries of extremities other extremity |
| I70209 | Unspecified atherosclerosis of native arteries of extremities unspecified extremity |
| I7021 | Atherosclerosis of native arteries of extremities with intermittent claudication |
| I70211 | Atherosclerosis of native arteries with intermittent claudication right leg |
| I70212 | Atherosclerosis of native arteries with intermittent claudication left leg |
| I70213 | Atherosclerosis of native arteries with intermittent claudication bilateral legs |
| I70218 | Atherosclerosis of native arteries with intermittent claudication other extremity |
| I70219 | Atherosclerosis of native arteries with intermittent claudication unspecified extremity |
| I7022 | Atherosclerosis of native arteries of extremities with rest pain |
| I70221 | Atherosclerosis of native arteries of extremities with rest pain right leg |
| I70222 | Atherosclerosis of native arteries of extremities with rest pain left leg |
| I70223 | Atherosclerosis of native arteries of extremities with rest pain bilateral legs |
| I70228 | Atherosclerosis of native arteries of extremities with rest pain other extremity |
| I70229 | Atherosclerosis of native arteries of extremities with rest pain unspecified extremity |
| I7023 | Atherosclerosis of native arteries of right leg with ulceration |
| I70231 | Atherosclerosis of native arteries of right leg with ulceration of thigh |
| I70232 | Atherosclerosis of native arteries of right leg with ulceration of calf |
| I70233 | Atherosclerosis of native arteries of right leg with ulceration of ankle |
| I70234 | Atherosclerosis of native arteries of right leg with ulceration of heel and midfoot |
| I70235 | Atherosclerosis of native arteries of right leg with ulceration of other part of foot |
| I70238 | Atherosclerosis of native arteries of right leg with ulceration of other part of lower leg |
| I70239 | Atherosclerosis of native arteries of right leg with ulceration of unspecified site |
| I7024 | Atherosclerosis of native arteries of left leg with ulceration |
| I70241 | Atherosclerosis of native arteries of left leg with ulceration of thigh |
| I70242 | Atherosclerosis of native arteries of left leg with ulceration of calf |
| I70243 | Atherosclerosis of native arteries of left leg with ulceration of ankle |
| I70244 | Atherosclerosis of native arteries of left leg with ulceration of heel and midfoot |
| I70245 | Atherosclerosis of native arteries of left leg with ulceration of other part of foot |
| I70248 | Atherosclerosis of native arteries of left leg with ulceration of other part of lower leg |
| I70249 | Atherosclerosis of native arteries of left leg with ulceration of unspecified site |
| I7025 | Atherosclerosis of native arteries of other extremities with ulceration |
| I7026 | Atherosclerosis of native arteries of extremities with gangrene |
| I70261 | Atherosclerosis of native arteries of extremities with gangrene right leg |
| I70262 | Atherosclerosis of native arteries of extremities with gangrene left leg |
| I70263 | Atherosclerosis of native arteries of extremities with gangrene bilateral legs |
| I70268 | Atherosclerosis of native arteries of extremities with gangrene other extremity |
| I70269 | Atherosclerosis of native arteries of extremities with gangrene unspecified extremity |
| I7029 | Other atherosclerosis of native arteries of extremities |
| I70291 | Other atherosclerosis of native arteries of extremities right leg |
| I70292 | Other atherosclerosis of native arteries of extremities left leg |
| I70293 | Other atherosclerosis of native arteries of extremities bilateral legs |
| I70298 | Other atherosclerosis of native arteries of extremities other extremity |
| I70299 | Other atherosclerosis of native arteries of extremities unspecified extremity |
| I703 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities |
| I7030 | Unspecified atherosclerosis of unspecified type of bypass graft(s) of the extremities |
| I70301 | Unspecified atherosclerosis of unspecified type of bypass graft(s) of the extremities right leg |
| I70302 | Unspecified atherosclerosis of unspecified type of bypass graft(s) of the extremities left leg |
| I70303 | Unspecified atherosclerosis of unspecified type of bypass graft(s) of the extremities bilateral legs |
| I70308 | Unspecified atherosclerosis of unspecified type of bypass graft(s) of the extremities other extremity |
| I70309 | Unspecified atherosclerosis of unspecified type of bypass graft(s) of the extremities unspecified extremity |
| I7031 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with intermittent claudication |
| I70311 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with intermittent claudication right leg |
| I70312 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with intermittent claudication left leg |
| I70313 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with intermittent claudication bilateral legs |
| I70318 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with intermittent claudication other extremity |
| I70319 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with intermittent claudication unspecified extremity |
| I7032 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with rest pain |
| I70321 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with rest pain right leg |
| I70322 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with rest pain left leg |
| I70323 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with rest pain bilateral legs |
| I70328 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with rest pain other extremity |
| I70329 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with rest pain unspecified extremity |
| I7033 | Atherosclerosis of unspecified type of bypass graft(s) of the right leg with ulceration |
| I70331 | Atherosclerosis of unspecified type of bypass graft(s) of the right leg with ulceration of thigh |
| I70332 | Atherosclerosis of unspecified type of bypass graft(s) of the right leg with ulceration of calf |
| I70333 | Atherosclerosis of unspecified type of bypass graft(s) of the right leg with ulceration of ankle |
| I70334 | Atherosclerosis of unspecified type of bypass graft(s) of the right leg with ulceration of heel and midfoot |
| I70335 | Atherosclerosis of unspecified type of bypass graft(s) of the right leg with ulceration of other part of foot |
| I70338 | Atherosclerosis of unspecified type of bypass graft(s) of the right leg with ulceration of other part of lower leg |
| I70339 | Atherosclerosis of unspecified type of bypass graft(s) of the right leg with ulceration of unspecified site |
| I7034 | Atherosclerosis of unspecified type of bypass graft(s) of the left leg with ulceration |
| I70341 | Atherosclerosis of unspecified type of bypass graft(s) of the left leg with ulceration of thigh |
| I70342 | Atherosclerosis of unspecified type of bypass graft(s) of the left leg with ulceration of calf |
| I70343 | Atherosclerosis of unspecified type of bypass graft(s) of the left leg with ulceration of ankle |
| I70344 | Atherosclerosis of unspecified type of bypass graft(s) of the left leg with ulceration of heel and midfoot |
| I70345 | Atherosclerosis of unspecified type of bypass graft(s) of the left leg with ulceration of other part of foot |
| I70348 | Atherosclerosis of unspecified type of bypass graft(s) of the left leg with ulceration of other part of lower leg |
| I70349 | Atherosclerosis of unspecified type of bypass graft(s) of the left leg with ulceration of unspecified site |
| I7035 | Atherosclerosis of unspecified type of bypass graft(s) of other extremity with ulceration |
| I7036 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with gangrene |
| I70361 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with gangrene right leg |
| I70362 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with gangrene left leg |
| I70363 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with gangrene bilateral legs |
| I70368 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with gangrene other extremity |
| I70369 | Atherosclerosis of unspecified type of bypass graft(s) of the extremities with gangrene unspecified extremity |
| I7039 | Other atherosclerosis of unspecified type of bypass graft(s) of the extremities |
| I70391 | Other atherosclerosis of unspecified type of bypass graft(s) of the extremities right leg |
| I70392 | Other atherosclerosis of unspecified type of bypass graft(s) of the extremities left leg |
| I70393 | Other atherosclerosis of unspecified type of bypass graft(s) of the extremities bilateral legs |
| I70398 | Other atherosclerosis of unspecified type of bypass graft(s) of the extremities other extremity |
| I70399 | Other atherosclerosis of unspecified type of bypass graft(s) of the extremities unspecified extremity |
| I704 | Atherosclerosis of autologous vein bypass graft(s) of the extremities |
| I7040 | Unspecified atherosclerosis of autologous vein bypass graft(s) of the extremities |
| I70401 | Unspecified atherosclerosis of autologous vein bypass graft(s) of the extremities right leg |
| I70402 | Unspecified atherosclerosis of autologous vein bypass graft(s) of the extremities left leg |
| I70403 | Unspecified atherosclerosis of autologous vein bypass graft(s) of the extremities bilateral legs |
| I70408 | Unspecified atherosclerosis of autologous vein bypass graft(s) of the extremities other extremity |
| I70409 | Unspecified atherosclerosis of autologous vein bypass graft(s) of the extremities unspecified extremity |
| I7041 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with intermittent claudication |
| I70411 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with intermittent claudication right leg |
| I70412 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with intermittent claudication left leg |
| I70413 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with intermittent claudication bilateral legs |
| I70418 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with intermittent claudication other extremity |
| I70419 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with intermittent claudication unspecified extremity |
| I7042 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with rest pain |
| I70421 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with rest pain right leg |
| I70422 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with rest pain left leg |
| I70423 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with rest pain bilateral legs |
| I70428 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with rest pain other extremity |
| I70429 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with rest pain unspecified extremity |
| I7043 | Atherosclerosis of autologous vein bypass graft(s) of the right leg with ulceration |
| I70431 | Atherosclerosis of autologous vein bypass graft(s) of the right leg with ulceration of thigh |
| I70432 | Atherosclerosis of autologous vein bypass graft(s) of the right leg with ulceration of calf |
| I70433 | Atherosclerosis of autologous vein bypass graft(s) of the right leg with ulceration of ankle |
| I70434 | Atherosclerosis of autologous vein bypass graft(s) of the right leg with ulceration of heel and midfoot |
| I70435 | Atherosclerosis of autologous vein bypass graft(s) of the right leg with ulceration of other part of foot |
| I70438 | Atherosclerosis of autologous vein bypass graft(s) of the right leg with ulceration of other part of lower leg |
| I70439 | Atherosclerosis of autologous vein bypass graft(s) of the right leg with ulceration of unspecified site |
| I7044 | Atherosclerosis of autologous vein bypass graft(s) of the left leg with ulceration |
| I70441 | Atherosclerosis of autologous vein bypass graft(s) of the left leg with ulceration of thigh |
| I70442 | Atherosclerosis of autologous vein bypass graft(s) of the left leg with ulceration of calf |
| I70443 | Atherosclerosis of autologous vein bypass graft(s) of the left leg with ulceration of ankle |
| I70444 | Atherosclerosis of autologous vein bypass graft(s) of the left leg with ulceration of heel and midfoot |
| I70445 | Atherosclerosis of autologous vein bypass graft(s) of the left leg with ulceration of other part of foot |
| I70448 | Atherosclerosis of autologous vein bypass graft(s) of the left leg with ulceration of other part of lower leg |
| I70449 | Atherosclerosis of autologous vein bypass graft(s) of the left leg with ulceration of unspecified site |
| I7045 | Atherosclerosis of autologous vein bypass graft(s) of other extremity with ulceration |
| I7046 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with gangrene |
| I70461 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with gangrene right leg |
| I70462 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with gangrene left leg |
| I70463 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with gangrene bilateral legs |
| I70468 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with gangrene other extremity |
| I70469 | Atherosclerosis of autologous vein bypass graft(s) of the extremities with gangrene unspecified extremity |
| I7049 | Other atherosclerosis of autologous vein bypass graft(s) of the extremities |
| I70491 | Other atherosclerosis of autologous vein bypass graft(s) of the extremities, right leg |
| I70492 | Other atherosclerosis of autologous vein bypass graft(s) of the extremities, left leg |
| I70493 | Other atherosclerosis of autologous vein bypass graft(s) of the extremities, bilateral legs |
| I70498 | Other atherosclerosis of autologous vein bypass graft(s) of the extremities, other extremity |
| I70499 | Other atherosclerosis of autologous vein bypass graft(s) of the extremities, unspecified extremity |
| I705A | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities |
| I7050 | Unspecified atherosclerosis of nonautologous biological bypass graft(s) of the extremities |
| I70501 | Unspecified atherosclerosis of nonautologous biological bypass graft(s) of the extremities, right leg |
| I70502 | Unspecified atherosclerosis of nonautologous biological bypass graft(s) of the extremities, left leg |
| I70503 | Unspecified atherosclerosis of nonautologous biological bypass graft(s) of the extremities, bilateral legs |
| I70508 | Unspecified atherosclerosis of nonautologous biological bypass graft(s) of the extremities, other extremity |
| I70509 | Unspecified atherosclerosis of nonautologous biological bypass graft(s) of the extremities, unspecified extremity |
| I7051 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities, intermittent claudication |
| I70511 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with intermittent claudication, right leg |
| I70512 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with intermittent claudication, left leg |
| I70513 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with intermittent claudication, bilateral legs |
| I70518 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with intermittent claudication, other extremity |
| I70519 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with intermittent claudication, unspecified extremity |
| I7052 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with rest pain |
| I70521 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with rest pain, right leg |
| I70522 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with rest pain, left leg |
| I70523 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with rest pain, bilateral legs |
| I70528 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with rest pain, other extremity |
| I70529 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with rest pain, unspecified extremity |
| I7053 | Atherosclerosis of nonautologous biological bypass graft(s) of the right leg with ulceration |
| I70531 | Atherosclerosis of nonautologous biological bypass graft(s) of the right leg with ulceration of thigh |
| I70532 | Atherosclerosis of nonautologous biological bypass graft(s) of the right leg with ulceration of calf |
| I70533 | Atherosclerosis of nonautologous biological bypass graft(s) of the right leg with ulceration of ankle |
| I70534 | Atherosclerosis of nonautologous biological bypass graft(s) of the right leg with ulceration of heel and midfoot |
| I70535 | Atherosclerosis of nonautologous biological bypass graft(s) of the right leg with ulceration of other part of foot |
| I70538 | Atherosclerosis of nonautologous biological bypass graft(s) of the right leg with ulceration of other part of lower leg |
| I70539 | Atherosclerosis of nonautologous biological bypass graft(s) of the right leg with ulceration of unspecified site |
| I7054 | Atherosclerosis of nonautologous biological bypass graft(s) of the left leg with ulceration |
| I70541 | Atherosclerosis of nonautologous biological bypass graft(s) of the left leg with ulceration of thigh |
| I70542 | Atherosclerosis of nonautologous biological bypass graft(s) of the left leg with ulceration of calf |
| I70543 | Atherosclerosis of nonautologous biological bypass graft(s) of the left leg with ulceration of ankle |
| I70544 | Atherosclerosis of nonautologous biological bypass graft(s) of the left leg with ulceration of heel and midfoot |
| I70545 | Atherosclerosis of nonautologous biological bypass graft(s) of the left leg with ulceration of other part of foot |
| I70548 | Atherosclerosis of nonautologous biological bypass graft(s) of the left leg with ulceration of other part of lower leg |
| I70549 | Atherosclerosis of nonautologous biological bypass graft(s) of the left leg with ulceration of unspecified site |
| I7055 | Atherosclerosis of nonautologous biological bypass graft(s) of other extremity with ulceration |
| I7056 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with gangrene |
| I70561 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with gangrene, right leg |
| I70562 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with gangrene, left leg |
| I70563 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with gangrene, bilateral legs |
| I70568 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with gangrene, other extremity |
| I70569 | Atherosclerosis of nonautologous biological bypass graft(s) of the extremities with gangrene, unspecified extremity |
| I7059 | Other atherosclerosis of nonautologous biological bypass graft(s) of the extremities |
| I70591 | Other atherosclerosis of nonautologous biological bypass graft(s) of the extremities, right leg |
| I70592 | Other atherosclerosis of nonautologous biological bypass graft(s) of the extremities, left leg |
| I70593 | Other atherosclerosis of nonautologous biological bypass graft(s) of the extremities, bilateral legs |
| I70598 | Other atherosclerosis of nonautologous biological bypass graft(s) of the extremities, other extremity |
| I70599 | Other atherosclerosis of nonautologous biological bypass graft(s) of the extremities, unspecified extremity |
| I706 | Atherosclerosis of nonbiological bypass graft(s) of the extremities |
| I7060 | Unspecified atherosclerosis of nonbiological bypass graft(s) of the extremities |
| I70601 | Unspecified atherosclerosis of nonbiological bypass graft(s) of the extremities, right leg |
| I70602 | Unspecified atherosclerosis of nonbiological bypass graft(s) of the extremities, left leg |
| I70603 | Unspecified atherosclerosis of nonbiological bypass graft(s) of the extremities, bilateral legs |
| I70608 | Unspecified atherosclerosis of nonbiological bypass graft(s) of the extremities, other extremity |
| I70609 | Unspecified atherosclerosis of nonbiological bypass graft(s) of the extremities, unspecified extremity |
| I7061 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with intermittent claudication |
| I70611 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with intermittent claudication, right leg |
| I70612 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with intermittent claudication, left leg |
| I70613 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with intermittent claudication, bilateral legs |
| I70618 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with intermittent claudication, other extremity |
| I70619 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with intermittent claudication, unspecified extremity |
| I7062 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with rest pain |
| I70621 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with rest pain, right leg |
| I70622 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with rest pain, left leg |
| I70623 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with rest pain, bilateral legs |
| I70628 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with rest pain, other extremity |
| I70629 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with rest pain, unspecified extremity |
| I7063 | Atherosclerosis of nonbiological bypass graft(s) of the right leg with ulceration |
| I70631 | Atherosclerosis of nonbiological bypass graft(s) of the right leg with ulceration of thigh |
| I70632 | Atherosclerosis of nonbiological bypass graft(s) of the right leg with ulceration of calf |
| I70633 | Atherosclerosis of nonbiological bypass graft(s) of the right leg with ulceration of ankle |
| I70634 | Atherosclerosis of nonbiological bypass graft(s) of the right leg with ulceration of heel and midfoot |
| I70635 | Atherosclerosis of nonbiological bypass graft(s) of the right leg with ulceration of other part of foot |
| I70638 | Atherosclerosis of nonbiological bypass graft(s) of the right leg with ulceration of other part of lower leg |
| I70639 | Atherosclerosis of nonbiological bypass graft(s) of the right leg with ulceration of unspecified site |
| I7064 | Atherosclerosis of nonbiological bypass graft(s) of the left leg with ulceration |
| I70641 | Atherosclerosis of nonbiological bypass graft(s) of the left leg with ulceration of thigh |
| I70642 | Atherosclerosis of nonbiological bypass graft(s) of the left leg with ulceration of calf |
| I70643 | Atherosclerosis of nonbiological bypass graft(s) of the left leg with ulceration of ankle |
| I70644 | Atherosclerosis of nonbiological bypass graft(s) of the left leg with ulceration of heel and midfoot |
| I70645 | Atherosclerosis of nonbiological bypass graft(s) of the left leg with ulceration of other part of foot |
| I70648 | Atherosclerosis of nonbiological bypass graft(s) of the left leg with ulceration of other part of lower leg |
| I70649 | Atherosclerosis of nonbiological bypass graft(s) of the left leg with ulceration of unspecified site |
| I7065 | Atherosclerosis of nonbiological bypass graft(s) of other extremity with ulceration |
| I7066 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with gangrene |
| I70661 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with gangrene, right leg |
| I70662 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with gangrene, left leg |
| I70663 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with gangrene, bilateral legs |
| I70668 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with gangrene, other extremity |
| I70669 | Atherosclerosis of nonbiological bypass graft(s) of the extremities with gangrene, unspecified extremity |
| I7069 | Other atherosclerosis of nonbiological bypass graft(s) of the extremities |
| I70691 | Other atherosclerosis of nonbiological bypass graft(s) of the extremities, right leg |
| I70692 | Other atherosclerosis of nonbiological bypass graft(s) of the extremities, left leg |
| I70693 | Other atherosclerosis of nonbiological bypass graft(s) of the extremities, bilateral legs |
| I70698 | Other atherosclerosis of nonbiological bypass graft(s) of the extremities, other extremity |
| I70699 | Other atherosclerosis of nonbiological bypass graft(s) of the extremities, unspecified extremity |
| I707 | Atherosclerosis of other type of bypass graft(s) of the extremities |
| I7070 | Unspecified atherosclerosis of other type of bypass graft(s) of the extremities |
| I70701 | Unspecified atherosclerosis of other type of bypass graft(s) of the extremities, right leg |
| I70702 | Unspecified atherosclerosis of other type of bypass graft(s) of the extremities, left leg |
| I70703 | Unspecified atherosclerosis of other type of bypass graft(s) of the extremities, bilateral legs |
| I70708 | Unspecified atherosclerosis of other type of bypass graft(s) of the extremities, other extremity |
| I70709 | Unspecified atherosclerosis of other type of bypass graft(s) of the extremities, unspecified extremity |
| I7071 | Atherosclerosis of other type of bypass graft(s) of the extremities with intermittent claudication |
| I70711 | Atherosclerosis of other type of bypass graft(s) of the extremities with intermittent claudication, right leg |
| I70712 | Atherosclerosis of other type of bypass graft(s) of the extremities with intermittent claudication, left leg |
| I70713 | Atherosclerosis of other type of bypass graft(s) of the extremities with intermittent claudication, bilateral legs |
| I70718 | Atherosclerosis of other type of bypass graft(s) of the extremities with intermittent claudication, other extremity |
| I70719 | Atherosclerosis of other type of bypass graft(s) of the extremities with intermittent claudication, unspecified extremity |
| I7072 | Atherosclerosis of other type of bypass graft(s) of the extremities with rest pain |
| I70721 | Atherosclerosis of other type of bypass graft(s) of the extremities with rest pain, right leg |
| I70722 | Atherosclerosis of other type of bypass graft(s) of the extremities with rest pain, left leg |
| I70723 | Atherosclerosis of other type of bypass graft(s) of the extremities with rest pain, bilateral legs |
| I70728 | Atherosclerosis of other type of bypass graft(s) of the extremities with rest pain, other extremity |
| I70729 | Atherosclerosis of other type of bypass graft(s) of the extremities with rest pain, unspecified extremity |
| I7073 | Atherosclerosis of other type of bypass graft(s) of the right leg with ulceration |
| I70731 | Atherosclerosis of other type of bypass graft(s) of the right leg with ulceration of thigh |
| I70732 | Atherosclerosis of other type of bypass graft(s) of the right leg with ulceration of calf |
| I70733 | Atherosclerosis of other type of bypass graft(s) of the right leg with ulceration of ankle |
| I70734 | Atherosclerosis of other type of bypass graft(s) of the right leg with ulceration of heel and midfoot |
| I70735 | Atherosclerosis of other type of bypass graft(s) of the right leg with ulceration of other part of foot |
| I70738 | Atherosclerosis of other type of bypass graft(s) of the right leg with ulceration of other part of lower leg |
| I70739 | Atherosclerosis of other type of bypass graft(s) of the right leg with ulceration of unspecified site |
| I7074 | Atherosclerosis of other type of bypass graft(s) of the left leg with ulceration |
| I70741 | Atherosclerosis of other type of bypass graft(s) of the left leg with ulceration of thigh |
| I70742 | Atherosclerosis of other type of bypass graft(s) of the left leg with ulceration of calf |
| I70743 | Atherosclerosis of other type of bypass graft(s) of the left leg with ulceration of ankle |
| I70744 | Atherosclerosis of other type of bypass graft(s) of the left leg with ulceration of heel and midfoot |
| I70745 | Atherosclerosis of other type of bypass graft(s) of the left leg with ulceration of other part of foot |
| I70748 | Atherosclerosis of other type of bypass graft(s) of the left leg with ulceration of other part of lower leg |
| I70749 | Atherosclerosis of other type of bypass graft(s) of the left leg with ulceration of unspecified site |
| I7075 | Atherosclerosis of other type of bypass graft(s) of other extremity with ulceration |
| I7076 | Atherosclerosis of other type of bypass graft(s) of the extremities with gangrene |
| I70761 | Atherosclerosis of other type of bypass graft(s) of the extremities with gangrene, right leg |
| I70762 | Atherosclerosis of other type of bypass graft(s) of the extremities with gangrene, left leg |
| I70763 | Atherosclerosis of other type of bypass graft(s) of the extremities with gangrene, bilateral legs |
| I70768 | Atherosclerosis of other type of bypass graft(s) of the extremities with gangrene, other extremity |
| I70769 | Atherosclerosis of other type of bypass graft(s) of the extremities with gangrene, unspecified extremity |
| I7079 | Other atherosclerosis of other type of bypass graft(s) of the extremities |
| I70791 | Other atherosclerosis of other type of bypass graft(s) of the extremities, right leg |
| I70792 | Other atherosclerosis of other type of bypass graft(s) of the extremities, left leg |
| I70793 | Other atherosclerosis of other type of bypass graft(s) of the extremities, bilateral legs |
| I70798 | Other atherosclerosis of other type of bypass graft(s) of the extremities, other extremity |
| I70799 | Other atherosclerosis of other type of bypass graft(s) of the extremities, unspecified extremity |
| I708 | Atherosclerosis of other arteries |
| I709 | Other and unspecified atherosclerosis |
| I7090 | Unspecified atherosclerosis |
| I7091 | Generalized atherosclerosis |
| I7092 | Chronic total occlusion of artery of the extremities |
| Z8679 | Personal history of other diseases of the circulatory system |
| COPD | |
| J43 | Emphysema |
| J430 | Unilateral pulmonary emphysema |
| J431 | Panlobular emphysema |
| J432 | Centrilobular emphysema |
| J438 | Other emphysema |
| J439 | Emphysema, unspecified |
| J449 | Chronic obstructive pulmonary disease, unspecified |
| J44 | Other chronic obstructive pulmonary disease |
| J440 | Chronic obstructive pulmonary disease with (acute) lower respiratory infection |
| J441 | Chronic obstructive pulmonary disease with (acute) exacerbation |
| J442 | Chronic obstructive pulmonary disease, unspecified |
| Marfan syndrome | |
| Q8740 | Marfan syndrome unspecified |
| Q8741 | Marfan syndrome with cardiovascular manifestations |
| Q87410 | Marfan syndrome with aortic dilation |
| Q87418 | Marfan syndrome with other cardiovascular manifestations |
| Q8742 | Marfan syndrome with ocular manifestations |
| Q8743 | Marfan syndrome with skeletal manifestations |
| Q874 | Marfan syndrome |
| Ehlers-Danlos syndrome | |
| Q7960 | Ehlers-Danlos syndrome, unspecified |
| Q7961 | Classical Ehlers-Danlos syndrome |
| Q7962 | Hypermobile Ehlers-Danlos syndrome |
| Q7963 | Vascular Ehlers-Danlos syndrome |
| Q7969 | Other Ehlers-Danlos syndrome |
| Q796 | Ehlers-Danlos syndrome |
| Turner syndrome | |
| Q960 | Turner syndrome karyotype 45, X |
| Q961 | Turner syndrome karyotype 46, X iso (Xq) |
| Q962 | Turner syndrome karyotype 46, X with abnormal sex chromosome, except iso (Xq) |
| Q963 | Turner syndrome mosaicism, 45, X/46, XX or XY |
| Q964 | Turner syndrome mosaicism, 45, X/other cell line(s) with abnormal sex chromosome |
| Q968 | Turner syndrome, other variants of Turner syndrome |
| Q969 | Turner syndrome, unspecified |
| Q96 | Turner syndrome |
| Diabetes | |
| E101 | Type 1 diabetes mellitus with ketoacidosis |
| E1010 | Type 1 diabetes mellitus with ketoacidosis without coma |
| E1011 | Type 1 diabetes mellitus with ketoacidosis with coma |
| E102 | Type 1 diabetes mellitus with kidney complications |
| E1021 | Type 1 diabetes mellitus with diabetic nephropathy |
| E1022 | Type 1 diabetes mellitus with diabetic chronic kidney disease |
| E1029 | Type 1 diabetes mellitus with other diabetic kidney complication |
| E103 | Type 1 diabetes mellitus with ophthalmic complications |
| E1031 | Type 1 diabetes mellitus with unspecified diabetic retinopathy |
| E10311 | Type 1 diabetes mellitus with unspecified diabetic retinopathy with macular edema |
| E10319 | Type 1 diabetes mellitus with unspecified diabetic retinopathy without macular edema |
| E1032 | Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy |
| E10321 | Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema |
| E103211 | Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema right eye |
| E103212 | Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema left eye |
| E103213 | Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema bilateral |
| E103219 | Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema unspecified eye |
| E10329 | Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy without macular edema |
| E103291 | Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy without macular edema right eye |
| E103292 | Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy without macular edema left eye |
| E103293 | Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy without macular edema bilateral |
| E103299 | Type 1 diabetes mellitus with mild nonproliferative diabetic retinopathy without macular edema unspecified eye |
| E1033 | Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy |
| E10331 | Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema |
| E103311 | Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema right eye |
| E103312 | Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema left eye |
| E103313 | Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema bilateral |
| E103319 | Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema unspecified eye |
| E10339 | Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy without macular edema |
| E103391 | Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy without macular edema right eye |
| E103392 | Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy without macular edema left eye |
| E103393 | Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy without macular edema bilateral |
| E103399 | Type 1 diabetes mellitus with moderate nonproliferative diabetic retinopathy without macular edema unspecified eye |
| E1034 | Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy |
| E10341 | Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy with macular edema |
| E103411 | Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy with macular edema right eye |
| E103412 | Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy with macular edema left eye |
| E103413 | Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy with macular edema bilateral |
| E103419 | Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy with macular edema unspecified eye |
| E10349 | Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy without macular edema |
| E103491 | Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy without macular edema right eye |
| E103492 | Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy without macular edema left eye |
| E103493 | Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy without macular edema bilateral |
| E103499 | Type 1 diabetes mellitus with severe nonproliferative diabetic retinopathy without macular edema unspecified eye |
| E1035 | Type 1 diabetes mellitus with proliferative diabetic retinopathy |
| E10351 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with macular edema |
| E103511 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with macular edema right eye |
| E103512 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with macular edema left eye |
| E103513 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with macular edema bilateral |
| E103519 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with macular edema unspecified eye |
| E10352 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment involving the macula |
| E103521 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment involving the macula right eye |
| E103522 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment involving the macula left eye |
| E103523 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment involving the macula bilateral |
| E103529 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment involving the macula unspecified eye |
| E10353 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment not involving the macula |
| E103531 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment not involving the macula |
| E103532 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment not involving the macula left eye |
| E103533 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment not involving macula bilateral |
| E103539 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment not involving macula unspecified eye |
| E10354 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with combined traction retinal detachment and rhegmatogenous retinal detachment |
| E103541 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with combined traction retinal detachment and rhegmatogenous retinal detachment right eye |
| E103542 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with combined traction retinal detachment and rhegmatogenous retinal detachment left eye |
| E103543 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with combined traction retinal detachment and rhegmatogenous retinal detachment bilateral |
| E103549 | Type 1 diabetes mellitus with proliferative diabetic retinopathy with combined traction retinal detachment and rhegmatogenous retinal detachment unspecified eye |
| E10355 | Type 1 diabetes mellitus with stable proliferative diabetic retinopathy |
| E103551 | Type 1 diabetes mellitus with stable proliferative diabetic retinopathy right eye |
| E103552 | Type 1 diabetes mellitus with stable proliferative diabetic retinopathy left eye |
| E103553 | Type 1 diabetes mellitus with stable proliferative diabetic retinopathy bilateral |
| E103559 | Type 1 diabetes mellitus with stable proliferative diabetic retinopathy unspecified eye |
| E10359 | Type 1 diabetes mellitus with proliferative diabetic retinopathy without macular edema |
| E103591 | Type 1 diabetes mellitus with proliferative diabetic retinopathy without macular edema right eye |
| E103592 | Type 1 diabetes mellitus with proliferative diabetic retinopathy without macular edema left eye |
| E103593 | Type 1 diabetes mellitus with proliferative diabetic retinopathy without macular edema bilateral |
| E103599 | Type 1 diabetes mellitus with proliferative diabetic retinopathy without macular edema unspecified eye |
| E1036 | Type 1 diabetes mellitus with diabetic cataract |
| E1037 | Type 1 diabetes mellitus with diabetic macular edema, resolved following treatment |
| E1037X1 | Type 1 diabetes mellitus with diabetic macular edema, resolved following treatment right eye |
| E1037X2 | Type 1 diabetes mellitus with diabetic macular edema, resolved following treatment left eye |
| E1037X3 | Type 1 diabetes mellitus with diabetic macular edema, resolved following treatment bilateral |
| E1037X9 | Type 1 diabetes mellitus with diabetic macular edema, resolved following treatment unspecified eye |
| E1039 | Type 1 diabetes mellitus with other diabetic ophthalmic complication |
| E104 | Type 1 diabetes mellitus with neurological complications |
| E1040 | Type 1 diabetes mellitus with diabetic neuropathy, unspecified |
| E1041 | Type 1 diabetes mellitus with diabetic mononeuropathy |
| E1042 | Type 1 diabetes mellitus with diabetic polyneuropathy |
| E1043 | Type 1 diabetes mellitus with diabetic autonomic (poly)neuropathy |
| E1044 | Type 1 diabetes mellitus with diabetic amyotrophy |
| E1049 | Type 1 diabetes mellitus with other diabetic neurologic complication |
| E105 | Type 1 diabetes mellitus with circulatory complications |
| E1051 | Type 1 diabetes mellitus with diabetic peripheral angiopathy without gangrene |
| E1052 | Type 1 diabetes mellitus with diabetic peripheral angiopathy with gangrene |
| E1059 | Type 1 diabetes mellitus with other circulatory complications |
| E106 | Type 1 diabetes mellitus with other specified complications |
| E1061 | Type 1 diabetes mellitus with diabetic arthropathy |
| E10610 | Type 1 diabetes mellitus with diabetic neuropathic arthropathy |
| E10618 | Type 1 diabetes mellitus with other diabetic arthropathy |
| E1062 | Type 1 diabetes mellitus with skin complications |
| E10620 | Type 1 diabetes mellitus with diabetic dermatitis |
| E10621 | Type 1 diabetes mellitus with foot ulcer |
| E10622 | Type 1 diabetes mellitus with other skin ulcer |
| E10628 | Type 1 diabetes mellitus with other skin complications |
| E1063 | Type 1 diabetes mellitus with oral complications |
| E10630 | Type 1 diabetes mellitus with periodontal disease |
| E10638 | Type 1 diabetes mellitus with other oral complications |
| E1064 | Type 1 diabetes mellitus with hypoglycemia |
| E10641 | Type 1 diabetes mellitus with hypoglycemia with coma |
| E10649 | Type 1 diabetes mellitus with hypoglycemia without coma |
| E1065 | Type 1 diabetes mellitus with hyperglycemia |
| E1069 | Type 1 diabetes mellitus with other specified complication |
| E108 | Type 1 diabetes mellitus with unspecified complications |
| E109 | Type 1 diabetes mellitus without complications |
| E110 | Type 2 diabetes mellitus with hyperosmolarity |
| E1100 | Type 2 diabetes mellitus with hyperosmolarity without nonketotic hyperglycemic-hyperosmolar coma (NKHHC) |
| E1101 | Type 2 diabetes mellitus with hyperosmolarity with coma |
| E111 | Type 2 diabetes mellitus with ketoacidosis |
| E1110 | Type 2 diabetes mellitus with ketoacidosis without coma |
| E1111 | Type 2 diabetes mellitus with ketoacidosis with coma |
| E112 | Type 2 diabetes mellitus with kidney complications |
| E1121 | Type 2 diabetes mellitus with diabetic nephropathy |
| E1122 | Type 2 diabetes mellitus with diabetic chronic kidney disease |
| E1129 | Type 2 diabetes mellitus with other diabetic kidney complication |
| E113 | Type 2 diabetes mellitus with ophthalmic complications |
| E1131 | Type 2 diabetes mellitus with unspecified diabetic retinopathy |
| E11311 | Type 2 diabetes mellitus with unspecified diabetic retinopathy with macular edema |
| E11319 | Type 2 diabetes mellitus with unspecified diabetic retinopathy without macular edema |
| E1132 | Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy |
| E11321 | Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema |
| E113211 | Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema right eye |
| E113212 | Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema left eye |
| E113213 | Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema bilateral |
| E113219 | Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema unspecified eye |
| E11329 | Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy without macular edema |
| E113291 | Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy without macular edema right eye |
| E113292 | Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy without macular edema left eye |
| E113293 | Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy without macular edema bilateral |
| E113299 | Type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy without macular edema unspecified eye |
| E1133 | Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy |
| E11331 | Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema |
| E113311 | Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema right eye |
| E113312 | Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema left eye |
| E113313 | Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema bilateral |
| E113319 | Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy with macular edema unspecified eye |
| E11339 | Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy without macular edema |
| E113391 | Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy without macular edema right eye |
| E113392 | Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy without macular edema left eye |
| E113393 | Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy without macular edema bilateral |
| E113399 | Type 2 diabetes mellitus with moderate nonproliferative diabetic retinopathy without macular edema unspecified eye |
| E1134 | Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy |
| E11341 | Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy with macular edema |
| E113411 | Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy with macular edema right eye |
| E113412 | Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy with macular edema left eye |
| E113413 | Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy with macular edema bilateral |
| E113419 | Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy with macular edema unspecified eye |
| E11349 | Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy without macular edema |
| E113491 | Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy without macular edema right eye |
| E113492 | Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy without macular edema left eye |
| E113493 | Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy without macular edema bilateral |
| E113499 | Type 2 diabetes mellitus with severe nonproliferative diabetic retinopathy without macular edema unspecified eye |
| E1135 | Type 2 diabetes mellitus with proliferative diabetic retinopathy |
| E11351 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with macular edema |
| E113511 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with macular edema right eye |
| E113512 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with macular edema left eye |
| E113513 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with macular edema bilateral |
| E113519 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with macular edema unspecified eye |
| E11352 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment involving the macula |
| E113521 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment involving the macula right eye |
| E113522 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment involving the macula left eye |
| E113523 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment involving the macula bilateral |
| E113529 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment involving the macula unspecified eye |
| E11353 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment not involving macula |
| E113531 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment not involving macula right eye |
| E113532 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment not involving macula left eye |
| E113533 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment not involving macula bilateral |
| E113539 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with traction retinal detachment not involving macula unspecified eye |
| E11354 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with combined traction retinal detachment and rhegmatogenous retinal detachment |
| E113541 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with combined traction retinal detachment and rhegmatogenous retinal detachment right eye |
| E113542 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with combined traction retinal detachment and rhegmatogenous retinal detachment left eye |
| E113543 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with combined traction retinal detachment and rhegmatogenous retinal detachment bilateral |
| E113549 | Type 2 diabetes mellitus with proliferative diabetic retinopathy with combined traction retinal detachment and rhegmatogenous retinal detachment unspecified eye |
| E11355 | Type 2 diabetes mellitus with stable proliferative diabetic retinopathy |
| E113551 | Type 2 diabetes mellitus with stable proliferative diabetic retinopathy right eye |
| E113552 | Type 2 diabetes mellitus with stable proliferative diabetic retinopathy left eye |
| E113553 | Type 2 diabetes mellitus with stable proliferative diabetic retinopathy bilateral |
| E113559 | Type 2 diabetes mellitus with stable proliferative diabetic retinopathy unspecified eye |
| E11359 | Type 2 diabetes mellitus with proliferative diabetic retinopathy without macular edema |
| E113591 | Type 2 diabetes mellitus with proliferative diabetic retinopathy without macular edema right eye |
| E113592 | Type 2 diabetes mellitus with proliferative diabetic retinopathy without macular edema left eye |
| E113593 | Type 2 diabetes mellitus with proliferative diabetic retinopathy without macular edema bilateral |
| E113599 | Type 2 diabetes mellitus with proliferative diabetic retinopathy without macular edema unspecified eye |
| E1136 | Type 2 diabetes mellitus with diabetic cataract |
| E1137 | Type 2 diabetes mellitus with diabetic macular edema, resolved following treatment |
| E1137X1 | Type 2 diabetes mellitus with diabetic macular edema, resolved following treatment right eye |
| E1137X2 | Type 2 diabetes mellitus with diabetic macular edema, resolved following treatment left eye |
| E1137X3 | Type 2 diabetes mellitus with diabetic macular edema, resolved following treatment bilateral |
| E1137X9 | Type 2 diabetes mellitus with diabetic macular edema, resolved following treatment unspecified eye |
| E1139 | Type 2 diabetes mellitus with other diabetic ophthalmic complication |
| E114 | Type 2 diabetes mellitus with neurological complications |
| E1140 | Type 2 diabetes mellitus with diabetic neuropathy, unspecified |
| E1141 | Type 2 diabetes mellitus with diabetic mononeuropathy |
| E1142 | Type 2 diabetes mellitus with diabetic polyneuropathy |
| E1143 | Type 2 diabetes mellitus with diabetic autonomic (poly)neuropathy |
| E1144 | Type 2 diabetes mellitus with diabetic amyotrophy |
| E1149 | Type 2 diabetes mellitus with other diabetic neurological complication |
| E115 | Type 2 diabetes mellitus with circulatory complications |
| E1151 | Type 2 diabetes mellitus with diabetic peripheral angiopathy without gangrene |
| E1152 | Type 2 diabetes mellitus with diabetic peripheral angiopathy with gangrene |
| E1159 | Type 2 diabetes mellitus with other circulatory complications |
| E116 | Type 2 diabetes mellitus with other specified complications |
| E1161 | Type 2 diabetes mellitus with diabetic arthropathy |
| E11610 | Type 2 diabetes mellitus with diabetic neuropathic arthropathy |
| E11618 | Type 2 diabetes mellitus with other diabetic arthropathy |
| E1162 | Type 2 diabetes mellitus with skin complications |
| E11620 | Type 2 diabetes mellitus with diabetic dermatitis |
| E11621 | Type 2 diabetes mellitus with foot ulcer |
| E11622 | Type 2 diabetes mellitus with other skin ulcer |
| E11628 | Type 2 diabetes mellitus with other skin complications |
| E1163 | Type 2 diabetes mellitus with oral complications |
| E11630 | Type 2 diabetes mellitus with periodontal disease |
| E11638 | Type 2 diabetes mellitus with other oral complications |
| E1164 | Type 2 diabetes mellitus with hypoglycemia |
| E11641 | Type 2 diabetes mellitus with hypoglycemia with coma |
| E11649 | Type 2 diabetes mellitus with hypoglycemia without coma |
| E1165 | Type 2 diabetes mellitus with hyperglycemia |
| E10 | Type I diabetes |
| E11 | Type II diabetes |
| Prior cardiac surgery | |
| Z951 | Presence of aortocoronary bypass graft |
| Z952 | Presence of prosthetic heart valve |
| Z953 | Presence of xenogenic heart valve |
| Z954 | Presence of other heart valve replacement |
| Z955 | Presence of coronary angioplasty implant and graft |
| Z958 | Presence of other cardiac and vascular implants and grafts |
| Z95810 | Presence of automatic (implantable) cardiac defibrillator |
| Z95811 | Presence of heart assist device |
| Z95812 | Presence of fully implantable artificial heart |
| Z95818 | Presence of other cardiac implants and grafts |
| Z9582 | Presence of other vascular implants and grafts |
| Z95820 | Peripheral vascular angioplasty status with implants and grafts |
| Z95828 | Presence of other vascular implants and grafts |
| Z959 | Presence of cardiac and vascular implant and graft, unspecified |
| Z95 | Presence of vascular implants and grafts on presentation |
| Chronic heart disease | |
| I25 | Chronic ischemic heart disease |
| I251 | Atherosclerotic heart disease of native coronary artery |
| I2510 | Atherosclerotic heart disease of native coronary artery without angina pectoris |
| I2511 | Atherosclerotic heart disease of native coronary artery with angina pectoris |
| I25110 | Atherosclerotic heart disease of native coronary artery with unstable angina pectoris |
| I25111 | Atherosclerotic heart disease of native coronary artery with unstable angina pectoris with documented spasm |
| I25118 | Atherosclerotic heart disease of native coronary artery with other forms of angina pectoris |
| I25119 | Atherosclerotic heart disease of native coronary artery with unspecified angina pectoris |
| I252 | Old myocardial infarction |
| I253 | Aneurysm of heart |
| I254 | Coronary artery aneurysm and dissection |
| I2541 | Coronary artery aneurysm |
| I2542 | Coronary artery dissection |
| I255 | Ischemic cardiomyopathy |
| I256 | Silent myocardial ischemia |
| I257 | Atherosclerosis of coronary artery bypass graft(s) and coronary artery of transplanted heart with angina pectoris |
| I2570 | Atherosclerosis of coronary artery bypass graft(s), unspecified, with angina pectoris |
| I25700 | Atherosclerosis of coronary artery bypass graft(s), unspecified, with unstable angina pectoris |
| I25701 | Atherosclerosis of coronary artery bypass graft(s), unspecified, with unstable angina pectoris with documented spasm |
| I25708 | Atherosclerosis of coronary artery bypass graft(s), unspecified, with other forms of angina pectoris |
| I25709 | Atherosclerosis of coronary artery bypass graft(s), unspecified, with unspecified angina pectoris |
| I2571 | Atherosclerosis of autologous vein coronary artery bypass graft(s) with angina pectoris |
| I25710 | Atherosclerosis of autologous vein coronary artery bypass graft(s) with unstable angina pectoris |
| I25711 | Atherosclerosis of autologous vein coronary artery bypass graft(s) with unstable angina pectoris with documented spasm |
| I25718 | Atherosclerosis of autologous vein coronary artery bypass graft(s) with other forms of angina pectoris |
| I25719 | Atherosclerosis of autologous vein coronary artery bypass graft(s) with unspecified angina pectoris |
| I2572 | Atherosclerosis of autologous artery coronary artery bypass graft(s) with angina pectoris |
| I25720 | Atherosclerosis of autologous artery coronary artery bypass graft(s) with unstable angina pectoris |
| I25721 | Atherosclerosis of autologous artery coronary artery bypass graft(s) with unstable angina pectoris with documented spasm |
| I25728 | Atherosclerosis of autologous artery coronary artery bypass graft(s) with other forms of angina pectoris |
| I25729 | Atherosclerosis of autologous artery coronary artery bypass graft(s) with unspecified angina pectoris |
| I2573 | Atherosclerosis of nonautologous biological coronary artery bypass graft(s) with angina pectoris |
| I25730 | Atherosclerosis of nonautologous biological coronary artery bypass graft(s) with unstable angina pectoris |
| I25731 | Atherosclerosis of nonautologous biological coronary artery bypass graft(s) with unstable angina pectoris with documented spasm |
| I25738 | Atherosclerosis of nonautologous biological coronary artery bypass graft(s) with other forms of angina pectoris |
| I25739 | Atherosclerosis of nonautologous biological coronary artery bypass graft(s) with unspecified angina pectoris |
| I2575 | Atherosclerosis of native coronary artery of transplanted heart with angina pectoris |
| I25750 | Atherosclerosis of native coronary artery of transplanted heart with unstable angina |
| I25751 | Atherosclerosis of native coronary artery of transplanted heart with unstable angina with documented spasm |
| I25758 | Atherosclerosis of native coronary artery of transplanted heart with other forms of angina pectoris |
| I25759 | Atherosclerosis of native coronary artery of transplanted heart with unspecified angina pectoris |
| I2576 | Atherosclerosis of bypass graft of coronary artery of transplanted heart with angina pectoris |
| I25760 | Atherosclerosis of bypass graft of coronary artery of transplanted heart with unstable angina |
| I25761 | Atherosclerosis of bypass graft of coronary artery of transplanted heart with unstable angina with documented spasm |
| I25768 | Atherosclerosis of bypass graft of coronary artery of transplanted heart with other forms of angina pectoris |
| I25769 | Atherosclerosis of bypass graft of coronary artery of transplanted heart with unspecified angina pectoris |
| I2579 | Atherosclerosis of other coronary artery bypass graft(s) with angina pectoris |
| I25790 | Atherosclerosis of other coronary artery bypass graft(s) with unstable angina pectoris |
| I25791 | Atherosclerosis of other coronary artery bypass graft(s) with unstable angina pectoris with documented spasm |
| I25798 | Atherosclerosis of other coronary artery bypass graft(s) with other forms of angina pectoris |
| I25799 | Atherosclerosis of other coronary artery bypass graft(s) with unspecified angina pectoris |
| I258 | Other forms of chronic ischemic heart disease |
| I2581 | Atherosclerosis of other coronary vessels without angina pectoris |
| I25810 | Atherosclerosis of coronary artery bypass graft(s) without angina pectoris |
| I25811 | Atherosclerosis of native coronary artery of transplanted heart without angina pectoris |
| I25812 | Atherosclerosis of bypass graft of coronary artery of transplanted heart without angina pectoris |
| I2582 | Chronic total occlusion of coronary artery |
| I2583 | Coronary atherosclerosis due to lipid rich plaque |
| I2584 | Coronary atherosclerosis due to calcified coronary lesion |
| I2589 | Other forms of chronic ischemic heart disease |
| I259 | Chronic ischemic heart disease, unspecified |
| Chronic kidney disease | |
| N18 | Chronic kidney disease (CKD) |
| N18.1 | Chronic kidney disease, stage 1 |
| N18.2 | Chronic kidney disease, stage 2 (mild) |
| N18.3 | Chronic kidney disease, stage 3 (moderate) |
| N18.30 | Chronic kidney disease, stage 3 unspecified |
| N18.31 | Chronic kidney disease, stage 3a |
| N18.32 | Chronic kidney disease, stage 3b |
| N18.4 | Chronic kidney disease, stage 4 (severe) |
| N18.5 | Chronic kidney disease, stage 5 |
| N18.6 | End-stage renal disease |
| N18.9 | Chronic kidney disease, unspecified |
| Aortic aneurysm | |
| I71.1 | Thoracic aortic aneurysm, ruptured |
| I71.2 | Thoracic aortic aneurysm, without rupture |
| I71.3 | Abdominal aortic aneurysm, ruptured |
| I71.4 | Abdominal aortic aneurysm, without rupture |
| I71.5 | Thoracoabdominal aortic aneurysm, ruptured |
| I71.6 | Thoracoabdominal aortic aneurysm, without rupture |
| I71.8 | Aortic aneurysm of unspecified site, ruptured |
| I71.9 | Aortic aneurysm of unspecified site, without rupture |
| Obesity | |
| Z6843 | Body mass index 50-59.9 |
| E669 | Obesity |
| Cardiac inflammation | |
| M314 | Takayasu (aortic arch syndrome) |
| M315 | Giant cell arteritis with polymyalgia rheumatica |
| M316 | Other giant cell arteritis |
| A5200 | Cardiovascular syphilis, unspecified |
| A5201 | Syphilitic aneurysm of aorta |
| A5202 | Syphilitic aortitis |
| A5203 | Syphilitic endocarditis |
| A5206 | Other syphilitic heart involvement |
| A5209 | Other cardiovascular syphilis |
| A1884 | Tuberculosis of heart |
| Z950 | Presence of cardiac pacemaker |
| Q231 | Congenital insufficiency of aortic valve |
| Z8673 | Personal history of transient ischemic attack (TIA), and cerebral infarction without residual deficits |
| Preoperative shock | |
| R57.0 | Cardiogenic shock |
| R57.1 | Hypovolemic shock |
| R57.8 | Other shock |
| R57.9 | Shock, unspecified |
ICD-10, International Classification of Diseases, Tenth Revision.
Table E3.
ICD-10 codes for complications
| ICD-10 code | Description |
|---|---|
| Postprocedural shock/cardiac failure | |
| T8110XA | Postprocedural shock unspecified, initial encounter |
| T8111XA | Postprocedural cardiogenic shock, initial encounter |
| T8112XA | Postprocedural septic shock, initial encounter |
| T8119XA | Other postprocedural shock |
| T882 | Shock due to anesthesia |
| T882XXA | Shock due to anesthesia initial encounter |
| I970 | Postcardiotomy syndrome |
| I97110 | Postprocedural cardiac insufficiency following cardiac surgery |
| I97120 | Postprocedural cardiac arrest following cardiac surgery |
| I97130 | Postprocedural heart failure following cardiac surgery |
| I97190 | Other postprocedural cardiac functional disturbances following cardiac surgery |
| I97710 | Intraoperative cardiac arrest during cardiac surgery |
| I97790 | Other intraoperative cardiac functional disturbances during cardiac surgery |
| I977 | Intraoperative cardiac functional disturbances |
| I97711 | Intraoperative cardiac arrest during other surgery |
| I97791 | Other intraoperative cardiac functional disturbances during other surgery |
| I971 | Other postprocedural cardiac functional disturbances |
| I97121 | Postprocedural cardiac arrest following other surgery |
| I97131 | Postprocedural heart failure following other surgery |
| I97191 | Other postprocedural cardiac functional disturbances following other surgery |
| I9788 | Other intraoperative complications of the circulatory system, not elsewhere classified |
| I9789 | Other procedural complications and disorders of the circulatory system, not elsewhere classified |
| Pulmonary complications | |
| Z9911 | Dependence on a ventilator |
| Z930 | Tracheostomy status |
| 0B110D6 | Bypass trachea to esophagus with intraluminal device, open approach |
| 0B110F4 | Bypass trachea to cutaneous with tracheostomy device, open approach |
| 0B110Z4 | Bypass trachea to cutaneous, open approach |
| 0B113F4 | Bypass trachea to cutaneous with tracheostomy device, percutaneous approach |
| 0B113Z4 | Bypass trachea to cutaneous, percutaneous approach |
| 0B114F4 | Bypass trachea to cutaneous with tracheostomy device, percutaneous endoscopic approach |
| 0B114Z4 | Bypass trachea to cutaneous, percutaneous endoscopic approach |
| J952 | Acute pulmonary insufficiency following nonthoracic surgery |
| J95821 | Acute postprocedural respiratory failure |
| J951 | Acute pulmonary insufficiency following thoracic surgery |
| J95822 | Acute and chronic postprocedural respiratory failure |
| J95851 | Ventilator-associated pneumonia |
| J95859 | Other complication of respirator |
| J9588 | Chronic pulmonary insufficiency following surgery |
| T8282XA | Emphysema (subcutaneous) resulting from a procedure, initial encounter |
| J950 | Tracheostomy complications |
| J9500 | Unspecified tracheostomy complication |
| J9501 | Hemorrhage from tracheostomy stoma |
| J9502 | Infection of tracheostomy stoma |
| J9503 | Malfunction of tracheostomy stoma |
| J9504 | Tracheoesophageal fistula following tracheostomy |
| J9509 | Other tracheostomy complication |
| J951 | Acute pulmonary insufficiency following thoracic surgery |
| J952 | Acute pulmonary insufficiency following nonthoracic surgery |
| J953 | Chronic pulmonary insufficiency following surgery |
| J954 | Chemical pneumonitis due to anesthesia |
| J955 | Postprocedural subglottic stenosis |
| J956 | Intraoperative hemorrhage and hematoma of a respiratory system organ or structure complicating a procedure |
| J9561 | Intraoperative hemorrhage and hematoma of a respiratory system organ or structure complicating a respiratory system procedure |
| J9562 | Intraoperative hemorrhage and hematoma of a respiratory system organ or structure complicating other procedure |
| J957 | Accidental puncture and laceration of a respiratory system organ or structure during a procedure |
| J9571 | Accidental puncture and laceration of a respiratory system organ or structure during a respiratory system procedure |
| J9572 | Accidental puncture and laceration of a respiratory system organ or structure during other procedure |
| J958 | Other intraoperative and postprocedural complications and disorders of respiratory system, not elsewhere classified |
| J9581 | Postprocedural pneumothorax and air leak |
| J95811 | Postprocedural pneumothorax |
| J95812 | Postprocedural air leak |
| J9582 | Postprocedural respiratory failure |
| J95821 | Acute postprocedural respiratory failure |
| J95822 | Acute and chronic postprocedural respiratory failure |
| J9583 | Postprocedural hemorrhage of a respiratory system organ or structure following a procedure |
| J95830 | Postprocedural hemorrhage of a respiratory system organ or structure following a respiratory system procedure |
| J95831 | Postprocedural hemorrhage of a respiratory system organ or structure following other procedure |
| J9584 | Transfusion-related acute lung injury (TRALI) |
| J9585 | Complication of respirator [ventilator] |
| J95850 | Mechanical complication of respirator |
| J95851 | Ventilator-associated pneumonia |
| J95859 | Other complication of respirator [ventilator] |
| J9586 | Postprocedural hematoma and seroma of a respiratory system organ or structure following a procedure |
| J95860 | Postprocedural hematoma of a respiratory system organ or structure following a respiratory system procedure |
| J95861 | Postprocedural hematoma of a respiratory system organ or structure following other procedure |
| J95862 | Postprocedural seroma of a respiratory system organ or structure following a respiratory system procedure |
| J95863 | Postprocedural seroma of a respiratory system organ or structure following other procedure |
| J9588 | Other intraoperative complications of respiratory system, not elsewhere classified |
| J9589 | Other postprocedural complications and disorders of respiratory system, not elsewhere classified |
| Z990 | Dependence on aspirator |
| Z991 | Dependence on respirator |
| Z9912 | Encounter for respirator [ventilator] dependence during power failure |
| Z9981 | Dependence on supplemental oxygen |
| 0B110D6 | Bypass trachea to esophagus with intraluminal device, open approach |
| 0B110F4 | Bypass trachea to cutaneous with tracheostomy device, open approach |
| 0B110Z4 | Bypass trachea to cutaneous, open approach |
| 0B113F4 | Bypass trachea to cutaneous with tracheostomy device, percutaneous approach |
| 0B113Z4 | Bypass trachea to cutaneous, percutaneous approach |
| 0B114F4 | Bypass trachea to cutaneous with tracheostomy device, percutaneous endoscopic approach |
| 0B114Z4 | Bypass trachea to cutaneous, percutaneous endoscopic approach |
| Hemorrhage/hematoma/seroma | |
| I97410 | Intraoperative hemorrhage and hematoma of a circulatory system organ or structure complicating a cardiac catheterization |
| I97411 | Intraoperative hemorrhage and hematoma of a circulatory system organ or structure complicating a cardiac bypass |
| I97418 | Intraoperative hemorrhage and hematoma of a circulatory system organ or structure complicating other circulatory system procedure |
| I9742 | Intraoperative hemorrhage and hematoma of a circulatory system organ or structure complicating other procedure |
| I97610 | Postprocedural hemorrhage of a circulatory system organ or structure following cardiac catheterization |
| I97611 | Postprocedural hemorrhage of a circulatory system organ or structure following cardiac bypass |
| I97618 | Postprocedural hemorrhage of a circulatory system organ or structure following other circulatory system procedure |
| I97620 | Postprocedural hemorrhage of a circulatory system organ or structure following other procedure |
| I97621 | Postprocedural hematoma of a circulatory system organ or structure following other procedure |
| I97630 | Postprocedural hematoma of a circulatory system organ or structure following cardiac catheterization |
| I97631 | Postprocedural hematoma of a circulatory system organ or structure following cardiac bypass |
| I97638 | Postprocedural hematoma of a circulatory system organ or structure following other circulatory system procedure |
| I97622 | Postprocedural seroma of a circulatory system organ or structure following other procedure |
| I97640 | Postprocedural seroma of a circulatory system organ or structure following a cardiac catheterization |
| I97641 | Postprocedural seroma of a circulatory system organ or structure following cardiac bypass |
| I97648 | Postprocedural seroma of a circulatory system organ or structure following other circulatory system procedure |
| I9761 | Postprocedural hemorrhage of a circulatory system organ or structure following a circulatory system procedure |
| I9762 | Postprocedural hemorrhage, hematoma, and seroma of a circulatory system organ or structure following other procedure |
| I9763 | Postprocedural hematoma of a circulatory system organ or structure following a circulatory system procedure |
| I9764 | Postprocedural seroma of a circulatory system organ or structure following a circulatory system procedure |
| Stroke | |
| I97810 | Intraoperative cerebrovascular infarction during cardiac surgery |
| I97820 | Postprocedural cerebrovascular infarction following cardiac surgery |
| Adverse reaction | |
| T886 | Anaphylactic reaction due to adverse effect of correct drug or medicament properly administered |
| T886XXA | Anaphylactic reaction due to adverse effect of correct drug or medicament properly administered, initial encounter |
| T887 | Unspecified adverse effect of drug or medicament |
| T887XXA | Unspecified adverse effect of drug or medicament, initial encounter |
| Y83 | Surgical operation and other surgical procedures as the cause of abnormal reaction of the patient, or of later complication, without mention of misadventure at the time of the procedure |
| Y830 | Surgical operation with transplant of whole organ as the cause of abnormal reaction of the patient, or of later complication, without mention of misadventure at the time of the procedure |
| Y831 | Surgical operation with implant of artificial internal device as the cause of abnormal reaction of the patient, or of later complication, without mention of misadventure at the time of the procedure |
| Y832 | Surgical operation with anastomosis, bypass or graft as the cause of abnormal reaction of the patient, or of later complication, without mention of misadventure at the time of the procedure |
| Y833 | Surgical operation with formation of external stoma as the cause of abnormal reaction of the patient, or of later complication, without mention of misadventure at the time of the procedure |
| Y834 | Other reconstructive surgery as the cause of abnormal reaction of the patient, or of later complication, without mention of misadventure at the time of the procedure |
| Y835 | Amputation of limb(s) as the cause of abnormal reaction of the patient, or of later complication, without mention of misadventure at the time of the procedure |
| Y836 | Removal of other organ (partial) (total) as the cause of abnormal reaction of the patient, or of later complication, without mention of misadventure at the time of the procedure |
| Y838 | Other surgical procedures as the cause of abnormal reaction of the patient, or of later complication, without mention of misadventure at the time of the procedure |
| Y839 | Surgical procedure, unspecified as the cause of abnormal reaction of the patient, or of later complication, without mention of misadventure at the time of the procedure |
| T886 | Anaphylactic reaction due to adverse effect of correct drug or medicament properly administered |
| T886XXA | Anaphylactic reaction due to adverse effect of correct drug or medicament properly administered, initial encounter |
| T887 | Unspecified adverse effect of drug or medicament |
| T887XXA | Unspecified adverse effect of drug or medicament, initial encounter |
| Y832 | Surgical operation with anastomosis, bypass, or graft as the cause of abnormal reaction |
| Y839 | Surgical procedure, unspecified as the cause of abnormal reaction of the patient, or of later complication, without mention of misadventure at the time of the procedure |
| Catheter-related complication | |
| T801XXA | Vascular complications following infusion, transfusion and therapeutic injection, initial encounter |
| T80219A | Unspecified infection due to central venous catheter, initial encounter |
| T80211A | Bloodstream infection due to central venous catheter, initial encounter |
| T80212A | Local infection due to central venous catheter, initial encounter |
| T8022XA | Acute infection following transfusion, infusion, or injection of blood or blood products, initial encounter |
| T8029XA | Infection following other infusion, transfusion, and therapeutic injection, initial encounter |
| T800 | Air embolism following infusion, transfusion, and therapeutic injection |
| T801 | Vascular complications following infusion, transfusion and therapeutic injection |
| T801XXA | Vascular complications following infusion, transfusion and therapeutic injection, initial encounter |
| T802 | Infections following infusion, transfusion and therapeutic injection |
| T8021 | Infection due to central venous catheter |
| T80211 | Bloodstream infection due to central venous catheter |
| T80211A | Bloodstream infection due to central venous catheter, initial encounter |
| T80212 | Local infection due to central venous catheter |
| T80212A | Local infection due to central venous catheter, initial encounter |
| T80218 | Other infection due to central venous catheter |
| T80 218A | Other infection due to central venous catheter, initial encounter |
| T80219 | Unspecified infection due to central venous catheter |
| T80219A | Unspecified infection due to central venous catheter, initial encounter |
| T8022 | Acute infection following transfusion, infusion, or injection of blood and blood products |
| T8022XA | Acute infection following transfusion, infusion, or injection of blood and blood products, initial encounter |
| T8029 | Acute infection following other transfusion, infusion, or injection of blood and blood products, initial encounter |
| T8029XA | Acute infection following transfusion, infusion, or injection of blood and blood products, initial encounter, initial encounter |
| Postprocedural hypertension | |
| I973 | Postprocedural hypertension |
| Other unspecified complications | |
| T888 | Other specified complications of surgical and medical care, not elsewhere classified |
| T889 | Complication of surgical and medical care, unspecified |
| T889XXA | Complication of surgical and medical care, unspecified initial encounter |
| Z99 | Dependence on enabling machines and devices, not elsewhere classified |
| Z998 | Dependence on other enabling machines and devices |
| Z9989 | Dependence on other enabling machines and devices |
| T888XXA | Other specified complications of surgical and medical care, not elsewhere classified, initial encounter |
| T8132XA | Disruption of internal operation (surgical) wound, not elsewhere classified, initial encounter |
| K6811 | Postprocedural retroperitoneal abscess |
ICD-10, International Classification of Diseases, Tenth Revision.
References
- 1.Melvinsdottir I.H., Lund S.H., Agnarsson B.A., Sigvaldason K., Gudbjartsson T., Geirsson A. The incidence and mortality of acute thoracic aortic dissection: results from a whole nation study. Eur J Cardio Thorac Surg. 2016;50:1111–1117. doi: 10.1093/ejcts/ezw235. [DOI] [PubMed] [Google Scholar]
- 2.Olsson C., Thelin S., Ståhle E., Ekbom A., Granath F. Thoracic aortic aneurysm and dissection: increasing prevalence and improved outcomes reported in a nationwide population-based study of more than 14 000 cases from 1987 to 2002. Circulation. 2006;114:2611–2618. doi: 10.1161/CIRCULATIONAHA.106.630400. [DOI] [PubMed] [Google Scholar]
- 3.Rylski B., Hoffmann I., Beyersdorf F., Suedkamp M., Siepe M., Nitsch B., et al. Acute aortic dissection type A: age-related management and outcomes reported in the German Registry for Acute Aortic Dissection Type A (GERAADA) of over 2000 patients. Ann Surg. 2014;259:598–604. doi: 10.1097/SLA.0b013e3182902cca. [DOI] [PubMed] [Google Scholar]
- 4.Zimmerman K.P., Oderich G., Pochettino A., Hanson K.T., Habermann E.B., Bower T.C., et al. Improving mortality trends for hospitalization of aortic dissection in the National Inpatient Sample. J Vasc Surg. 2016;64:606–615.e1. doi: 10.1016/j.jvs.2016.03.427. [DOI] [PubMed] [Google Scholar]
- 5.Andersen N.D., Brennan J.M., Zhao Y., Williams J.B., Williams M.L., Smith P.K., et al. Insurance status is associated with acuity of presentation and outcomes for thoracic aortic operations. Circ Cardiovasc Qual Outcomes. 2014;7:398–406. doi: 10.1161/CIRCOUTCOMES.113.000593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Muntner P., He J., Cutler J.A., Wildman R.P., Whelton P.K. Trends in blood pressure among children and adolescents. JAMA. 2004;291:2107–2113. doi: 10.1001/jama.291.17.2107. [DOI] [PubMed] [Google Scholar]
- 7.Kressin N.R., Orner M.B., Manze M., Glickman M.E., Berlowitz D. Understanding contributors to racial disparities in blood pressure control. Circ Cardiovasc Qual Outcomes. 2010;3:173–180. doi: 10.1161/CIRCOUTCOMES.109.860841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lackland D.T. Racial differences in hypertension: implications for high blood pressure management. Am J Med Sci. 2014;348:135–138. doi: 10.1097/MAJ.0000000000000308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Howard G., Safford M.M., Moy C.S., Howard V.J., Kleindorfer D.O., Unverzagt F.W., et al. Racial differences in the incidence of cardiovascular risk factors in older black and white adults. J Am Geriatr Soc. 2017;65:83–90. doi: 10.1111/jgs.14472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mansour O., Golden S.H., Yeh H.-C. Disparities in mortality among adults with and without diabetes by sex and race. J Diabetes Complicat. 2020;34:107496. doi: 10.1016/j.jdiacomp.2019.107496. [DOI] [PubMed] [Google Scholar]
- 11.Tsao C.W., Aday A.W., Almarzooq Z.I., Alonso A., Beaton A.Z., Bittencourt M.S., et al. Heart disease and stroke statistics—2022 update: a report from the American Heart Association. Circulation. 2022;145:e153–e639. doi: 10.1161/CIR.0000000000001052. [DOI] [PubMed] [Google Scholar]
- 12.Levine D.A., Duncan P.W., Nguyen-Huynh M.N., Ogedegbe O.G. Interventions targeting racial/ethnic disparities in stroke prevention and treatment. Stroke. 2020;51:3425–3432. doi: 10.1161/STROKEAHA.120.030427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams D.R., Priest N., Anderson N.B. Understanding associations among race, socioeconomic status, and health: patterns and prospects. Health Psychol. 2016;35:407–411. doi: 10.1037/hea0000242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kabbani L.S., Wasilenko S., Nypaver T.J., Weaver M.R., Taylor A.R., Abdul-Nour K., et al. Socioeconomic disparities affect survival after aortic dissection. J Vasc Surg. 2016;64:1239–1245. doi: 10.1016/j.jvs.2016.03.469. [DOI] [PubMed] [Google Scholar]
- 15.Hall W.J., Chapman M.V., Lee K.M., Merino Y.M., Thomas T.W., Payne B.K., et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic Review. Am J Public Health. 2015;105:e60–e76. doi: 10.2105/AJPH.2015.302903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Osborne N.H., Upchurch G.R., Jr., Mathur A.K., Dimick J.B. Explaining racial disparities in mortality after abdominal aortic aneurysm repair. J Vasc Surg. 2009;50:709–713. doi: 10.1016/j.jvs.2009.05.020. [DOI] [PubMed] [Google Scholar]
- 17.Zarkowsky D.S., Arhuidese I.J., Hicks C.W., Canner J.K., Qazi U., Obeid T., et al. Racial/ethnic disparities associated with initial hemodialysis access. JAMA surgery. 2015;150:529–536. doi: 10.1001/jamasurg.2015.0287. [DOI] [PubMed] [Google Scholar]
- 18.Hicks C.W., Canner J.K., Zarkowsky D.S., Arhuidese I., Obeid T., Malas M.B. Racial disparities after vascular trauma are age-dependent. J Vasc Surg. 2016;64:418–424. doi: 10.1016/j.jvs.2016.01.049. [DOI] [PubMed] [Google Scholar]
- 19.Rangrass G., Ghaferi A.A., Dimick J.B. Explaining racial disparities in outcomes after cardiac surgery: the role of hospital quality. JAMA Surg. 2014;149:223–227. doi: 10.1001/jamasurg.2013.4041. [DOI] [PubMed] [Google Scholar]
- 20.Pienta M.J., Theurer P.F., He C., Zehr K., Drake D., Murphy E., et al. Racial disparities in mitral valve surgery: a statewide analysis. J Thorac Cardiovasc Surg. 2022 doi: 10.1016/j.jtcvs.2021.11.096. [DOI] [PubMed] [Google Scholar]
- 21.Ravi P., Sood A., Schmid M., Abdollah F., Sammon J.D., Sun M., et al. Racial/ethnic disparities in perioperative outcomes of major procedures. Annals of surgery. 2015;262:955–964. doi: 10.1097/SLA.0000000000001078. [DOI] [PubMed] [Google Scholar]
- 22.Ghosh A.K., Geisler B.P., Ibrahim S. Racial/ethnic and socioeconomic variations in hospital length of stay: a state-based analysis. Medicine. 2021;100 doi: 10.1097/MD.0000000000025976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Giglia M.D., DeRussy A., Morris M.S., Richman J.S., Hawn M.T., Vickers S.M., et al. Racial disparities in length-of-stay persist even with no postoperative complications. J Surg Res. 2017;214:14–22. doi: 10.1016/j.jss.2017.02.063. [DOI] [PubMed] [Google Scholar]
- 24.Elsamadicy A.A., Koo A.B., David W.B., Sarkozy M., Freedman I.G., Reeves B.C., et al. Portending influence of racial disparities on extended length of stay after elective anterior cervical discectomy and interbody fusion for cervical spondylotic myelopathy. World Neurosurg. 2020;142:e173–e182. doi: 10.1016/j.wneu.2020.06.155. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Summary of the article's purpose, main findings, and significance. Video available at: https://www.jtcvs.org/article/S2666-2736(23)00028-1/fulltext.
Racial disparities in surgical treatment of type A acute aortic dissection. Video available at: https://www.jtcvs.org/article/S2666-2736(23)00028-1/fulltext