Abstract
Aim
This study aimed to quantitatively summarise risk factors associated with surgical site infection (SSI) following surgically managed tibial fractures.
Method
We searched the Embase/Medline, Cochrane Library, and Scopus databases for relevant studies in October 2023. We included original studies investigating risk factors for SSI following surgically managed traumatic tibial fractures that included ≥10 adult patients with SSIs. Meta-analysis was performed when >5 studies investigated the same risk factor. The risk of bias was assessed using the critical appraisal checklist from Joanna Briggs Institute for cohort studies.
Results
This study included 42 studies comprising 24,610 patients with surgically managed tibial fractures and 2,418 SSI cases. The following were identified as significant risk factors for SSI (p < 0.05): compartment syndrome (odds ratio [OR] = 3.8, 95% confidence interval [CI]: 2.4–6.0), blood transfusion (OR = 3.8, 95% CI: 2.1–6.6), open fracture (OR = 3.6, 95% CI: 2.5–5.1), Gustilo–Anderson classification >2 (OR = 3.1, 95% CI: 2.1–4.6), external fixation (OR = 2.9, 95% CI: 2.3–3.8), American Society of Anesthesiologists classification >2 (OR = 2.5, 95% CI: 1.5–4.1), polytrauma (OR = 2.4, 95% CI: 1.5–4.0), dual incision approach (OR = 2.1, 95% CI: 1.5–3.0), smoking (OR = 1.8, 95% CI: 1.5–2.1), male sex (OR = 1.6, 95% CI: 1.3–1.8), high energy trauma (OR = 1.5, 95% CI: 1.1–2.1), and prolonged surgery time (OR = 0.62, 0.43–0.82). Other factors, including diabetes, hypertension, and time to surgery, were not identified as risk factors for SSI. However, the included studies were generally of poor quality and at risk of bias.
Conclusions
The review provides a basis for preoperatively assessing a patient's risk of developing an SSI, which could be used to initiate adjusted antibiotic regimes and more frequent postoperative controls. Furthermore, it indicates the risk factors future research should include when adjusting for confounding factors.
Keywords: Surgical site infection, Fractures, Meta-analysis, Osteosynthesis, Risk factors
Highlights
-
•
Patient related risk factors for infection are male sex, ASA classification>2 and smoking.
-
•
Fracture related risk factors are open fracture, Gustilo Anderson type, compartment syndrome, high energy- and polytrauma.
-
•
Surgery related risk factors are external fixation, blood transfusions, prolonged operative time, and dual incision.
-
•
This review provides basis for preoperative assessment of a patient’s risk for developing SSI.
-
•
This review indicates which risk factors future research should include when assessing for confounding factors.
1. Introduction
Tibial fractures are adults’ most common long bone fractures, often requiring surgery to stabilize the bone.1 One of the most challenging and devastating complications after surgery for tibial fractures is surgical site infection (SSI).2 SSI management often involves repeated operations, prolonged hospital stays, and rehabilitation. It comes with significant expenses for the patient, whose quality of life and ability to work can be significantly affected, and it is very costly for the healthcare system.3 Therefore, preventing SSIs is essential.
The risk factors for SSI in tibial fractures have been investigated in numerous studies with divergent results.4, 5, 6, 7 Numerous studies have confirmed compartment syndrome, open fractures, external fixation, and tobacco use as risk factors for SSI. However, male sex, operative time, and alcohol use have shown mixed results.4,5,8,9 Two systematic reviews have investigated risk factors for SSI after open reduction internal fixation (ORIF) of tibial plateau5 and ankle4 fractures comprising 2,214 and 8,103 patients, respectively. They both showed that open fracture was a risk factor for SSI but had opposing results for external fixation, operative time, and smoking. No published study has compiled current knowledge which would help assess patient susceptibility to SSI and initiate preventive measures when required.
Therefore, this study aimed to quantitatively estimate risk factors associated with SSI following surgically managed tibial fractures.
2. Methods
2.1. Protocol and registration
This systematic review and meta-analyses are reported to Systematic Reviews and Meta-Analyses (PRISMA) statement according to the Preferred Reporting Items.10 The study protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) database before data extraction (registration number: CRD42022324456).11
2.2. Eligibility criteria
The PECO model was used to create the research string:
Population: Patients with SSIs after osteosynthesis for traumatic tibia fractures.
Exposure: Risk factors associated with the development of SSIs.
Comparator: Patients who did not suffer from SSIs after osteosynthesis for traumatic tibia fractures.
Outcome: Patients with SSIs.
The inclusion criteria were peer-reviewed studies with patients aged >15 suffering from an open or closed traumatic tibial fracture treated with osteosynthesis.
The exclusion criteria were animal and cadaveric studies; studies with <10 patients developing an SSI after surgery12; studies where fractures were treated with prostheses or conservatively; studies on face, head, neck, thoracic, or spine fractures; studies involving cancer or tumor surgery; studies on periprosthetic fractures; studies on gunshot or explosive fractures; studies on arthrodesis; and studies published in languages other than English, Swedish, German, Norwegian, or Danish.
2.3. Definition of risk factors and infection
Infection was not defined before the screening process. All studies describing SSIs and investigating risk factors potentially affecting postoperative SSI risk for tibial fractures were included.
2.4. Information sources
We conducted a systematic literature search on 30 October 2023 in the Cochrane, Embase/Medline, Library, and Scopus electronic databases. Grey literature was sought on The European Bone and Joint Infection Society (https://ebjis.org; date: 30/10/2023) and European Wound Management Association (https://ewma.org; date: 30/10/2023) websites; no further studies were identified.
2.5. Search strategy
The search string comprised MeSH terms and free-text words in four blocks with the following synonyms; tibia, infection, fracture, and osteosynthesis. The Boolean operator “AND” combined the four blocks: “tibia AND infection AND fracture AND osteosynthesis”. In each block, the Boolean operator “OR” was used between synonyms. See Appendix A for the complete search string. No search limitations were included.
2.6. Study selection
All studies were imported into EndNote and searched for duplicates. Then, studies were imported into Covidence (Veritas Health Innovation, Australia; www.covidence.org) for screening. The included studies were screened against the inclusion and exclusion criteria independently and blindly by the two primary authors (DN and TM). The included studies were then full-text screened separately by the same two authors. Consultation with senior authors resolved any disagreements.
2.7. Data collection process
Relevant data were extracted independently by the two primary authors into a predesigned Excel sheet (Microsoft Excel for Mac, Office 365 version 16.44). We contacted 18 authors by email due to missing data (i.e., the number of patients in each exposure group). Five replied with a datasheet,6,13, 14, 15, 16 ten were excluded due to missing data, and three were included in the systematic review but excluded from meta-analysis due to missing raw data.7,8,17 Finally, the two primary authors double-checked all extracted data.
2.8. Data items
For each study following variables were registered: author name, publication year, study design, country, number of participants, number of infected patients, minimum follow-up, patient mean age, open/closed fractures, and number of patient-related risk factors.
2.9. Risk of bias in individual studies
Studies included in the meta-analysis were assessed for risk of bias using the Joanna Briggs Institute critical appraisal checklist for cohort studies.18 The first two studies were evaluated as a pilot and then blindly assessed by a senior author (BV) to ensure agreement. Then, the remaining studies were all assessed by one author and subsequently discussed with another author (DN + TM and SS + NJ, respectively).
Three senior authors selected four critical confounding factors known to affect the risk of SSI: age, diabetes, tobacco use, and open fracture. The outcome was always SSI and was considered reliable in cases with purulent discharge, fistula or wound breakdown, or local and systemic infection symptoms with an affected blood test. The outcome was assessed as ‘unclear’ if a surgeon noted infection. A minimum of 6 months of follow-up was defined as sufficient for an outcome to have occurred. ‘Not applicable’ was used in question 10 when a follow-up was deemed ‘unclear’ in question 9.
2.10. Statistics and synthesis of results
SSI and risk factors were assessed as binary outcomes, and a 2 × 2 contingency table was created for each risk factor. The Stata 16 (version 2019; StataCorp LLC, College Station, USA) software was used for all statistical analyses. We assume that fracture localization does not influence the risk of infection and therefore compile data from the entire tibia for meta-analysis. Meta-analyses were performed when a potential risk factor was investigated in ≥5 studies. The evidence synthesis was performed using an odds ratio (OR) as the effect measure, with a p < 0.05 considered statistically significant. The meta-analyses were conducted using the built-in Meta function in Stata 16 and reported as forest and funnel plots. Data were assessed using a random-effects model and restricted maximum likelihood (REML) due to the heterogenicity in data.19
3. Results
3.1. Study selection
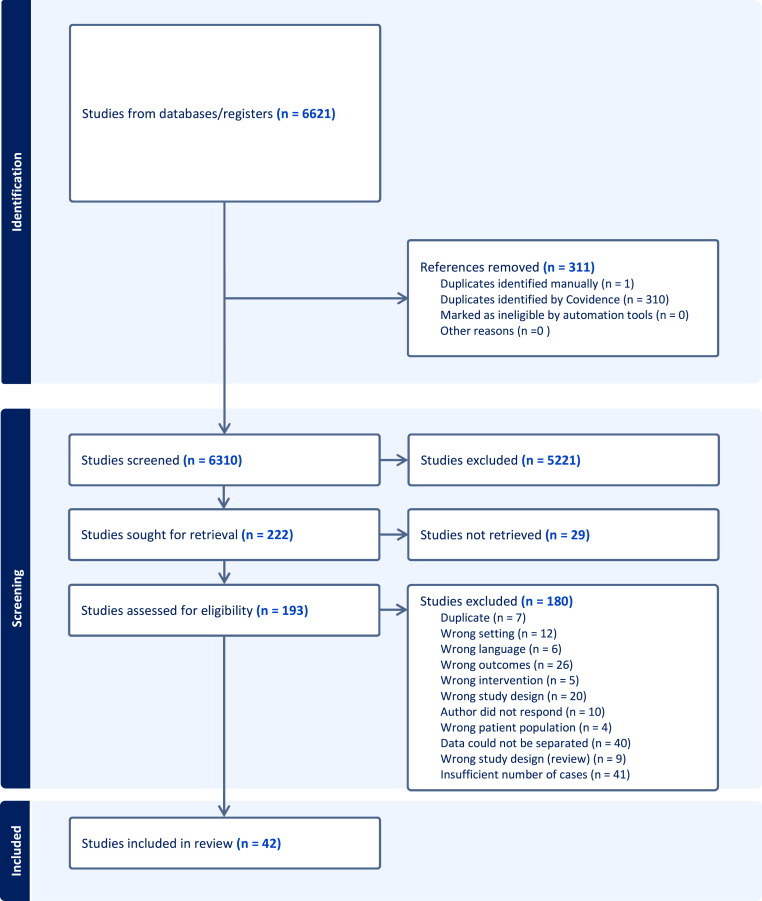
In total, 6,621 studies were identified by the systematic literature search, of which 193 articles were eligible for full-text screening (Fig. 1). Twenty-nine studies could not be retrieved, and the most common reason for exclusion was insufficient cases. Therefore, this study included 42 studies.
Fig. 1.
PRISMA flowchart.
3.2. Study characteristics
Six studies were prospective,8,9,20, 21, 22, 23 and the remaining 36 were retrospective6,7,13, 14, 15, 16, 17,24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52 (Table 1). The total number of included patients was 24,610, of which 2,418 had SSIs. The number of risk factors in each study varied from 1 to 26.
Table 1.
Overview of studies.
| Authors | Publication year | Country | Study design | Participants, n | Patients with infections | Minimum follow-up | Ageb | Open/closed fractures | Patient Related Risk factors |
|---|---|---|---|---|---|---|---|---|---|
| Ashworth et al.48 | 2022 | USA | Retrospective | 151 | 36 | 90 days | 44.8 ± 15.4 | Both | 9 |
| Burrus et al.24 | 2015 | USA | Retrospective | 10213 | 1118 | 90 days | Uncertain | Both | 1 |
| Colman et al.25 | 2012 | USA | Retrospective | 309 | 24 | 12 months | 47.8 | Both | 12 |
| Doshi et al.20 | 2017 | India | Prospective | 768 | 23 | 12 months | 40.1 ± 14 | Both | 6 |
| Dubina et al.26 | 2017 | USA | Retrospective | 675 | 69 | 8 weeks | 45.4 | Uncertain | 6 |
| Duckworth et al.13 | 2016 | UK | Retrospective | 99 | 18 | 3 months | 42 (16–86) | Both | 5 |
| Esposito et al.17 | 2019 | USA | Retrospective | 581 | 62 | Uncertain | 45 (35–55) | Both | 8 |
| Fonkoue et al.52 | 2023 | Cameroon | Retrospective | 105 | 33 | 12 months | 37.9 ± 13 | Both | 13 |
| Forni et al.51 | 2022 | Brazil | Retrospective | 44 | 11 | Uncertain | 48.5 ± 15.1 | Both | 12 |
| Gaunder et al.27 | 2018 | USA | Retrospective | 102 | 16 | 1 month | >60 | Both | 10 |
| Groznik et al.28 | 2019 | Slovenia | Retrospective | 86 | 20 | Uncertain | 69.3/66.8a | Both | 8 |
| Haase et al.29 | 2022 | USA | Retrospective | 244 | 34 | 3 months | 50 | Both | 8 |
| Henkelmann et al.30 | 2020 | Germany | Retrospective | 2106 | 94 | Uncertain | 50.2 ± 15.1 | Both | 12 |
| Jenny et al.33 | 1994 | France | Retrospective | 359 | 20 | Uncertain | Uncertain | Both | 2 |
| Kent et al.31 | 2015 | UK | Retrospective | 42 | 12 | 12 months | 57.5/49.6a | Both | 7 |
| Kline et al.32 | 2009 | USA | Retrospective | 83 | 12 | 6 months | 47 | Both | 1 |
| Kugelman et al.8 | 2017 | USA | Prospective | 275 | 10 | 12 months | 48.8 ± 14.63 | Both | 2 |
| Li et al. (2018)34 | 2018 | China | Retrospective | 370 | 21 | 2 months | 46.2 | Both | 16 |
| Li et al. (2020)21 | 2020 | China | Prospective | 1108 | 25 | 12 months | 45.6 | Both | 14 |
| Lin et al.35 | 2013 | USA | Retrospective | 251 | 20 | 6 months | 47.4/42.6a | Both | 12 |
| Ma et al.36 | 2018 | China | Retrospective | 676 | 17 | Uncertain | 44.4/46.9a | Both | 18 |
| Manon et al.6 | 2020 | Belgium | Retrospective | 168 | 13 | Uncertain | 45.6 | Both | 9 |
| Messori et al.49 | 2023 | Italy | Retrospective | 103 | 12 | 12 months | 49.9 | Open | 9 |
| Metsemakers et al.7 | 2014 | Belgium | Retrospective | 480 | 21 | 18 months | Uncertain | Both | 9 |
| Molina et al.37 | 2015 | USA | Retrospective | 355 | 57 | 6 months | 42.3 ± 14.2 | Both | 7 |
| Momaya et al.38 | 2016 | USA | Retrospectiv | 532 | 59 | 19.5 months (Average) | 47.76 ± 15.2 | Both | 13 |
| Morris et al.39 | 2013 | USA | Retrospective | 302 | 43 | 14.1 months (Average) | 45.7 ± 14.3 (19–76) | Both | 9 |
| Oladeji et al.40 | 2020 | USA | Retrospective | 276 | 46 | 12 months | 43.8 ± 15.2 | Both | 1 |
| Olesen et al.41 | 2015 | Denmark | Retrospective | 44 | 22 | 12 months | 42 (16–71) | Open | 4 |
| Olson et al.14 | 2021 | USA | Retrospective | 161 | 43 | 12 months | 46 ± 14 | Open | 4 |
| Parkkinen et al.42 | 2016 | Finland | Retrospective | 170 | 34 | 12 months | 55 (16–84) | Both | 12 |
| Ren et al.43 | 2015 | China | Retrospective | 519 | 12 | 12 months | >18 | Both | 10 |
| Ruffolo et al.16 | 2015 | USA | Retrospective | 138 | 33 | 3 months | 44.6 (16–78) | Both | 6 |
| Spitler et al.44 | 2020 | USA | Retrospective | 148 | 25 | Uncertain | 44 | Both | 10 |
| Viberg et al.15 | 2016 | Denmark | Retrospective | 70 | 17 | 36 months | 48 (15–85) | Both | 6 |
| Whiting et al.22 | 2019 | USA, Kenya | Prospective | 1061 | 113 | 4.9 months (Average) | 35.5 ± 14 | Both | 6 |
| Xie et al.23 | 2023 | China | Prospective | 417 | 30 | 12 months | 45.6 ± 15.2 | Both | 12 |
| Yeramosu et al.45 | 2022 | USA | Retrospective | 248 | 52 | 12 months | 45.5/42.5a | Both | 9 |
| Ying et al.22 | 2023 | China | Retrospective | 351 | 51 | 30 days | 44.0 (27.5–56.0) | Both | 26 |
| Yusof et al.46 | 2013 | Malaysia | Retrospective | 58 | 17 | 12 months | 34.2/27.8a | Open | 3 |
| Zhu et al.9 | 2017 | China | Prospective | 235 | 12 | 12 months | 45 (19–75) | Both | 13 |
| Zuelzer et al.47 | 2020 | USA | Retrospective | 127 | 11 | 6 weeks | 37/41a | Open | 7 |
Mean for infection/no-infection.
Presented as mean ± S.D. or range.
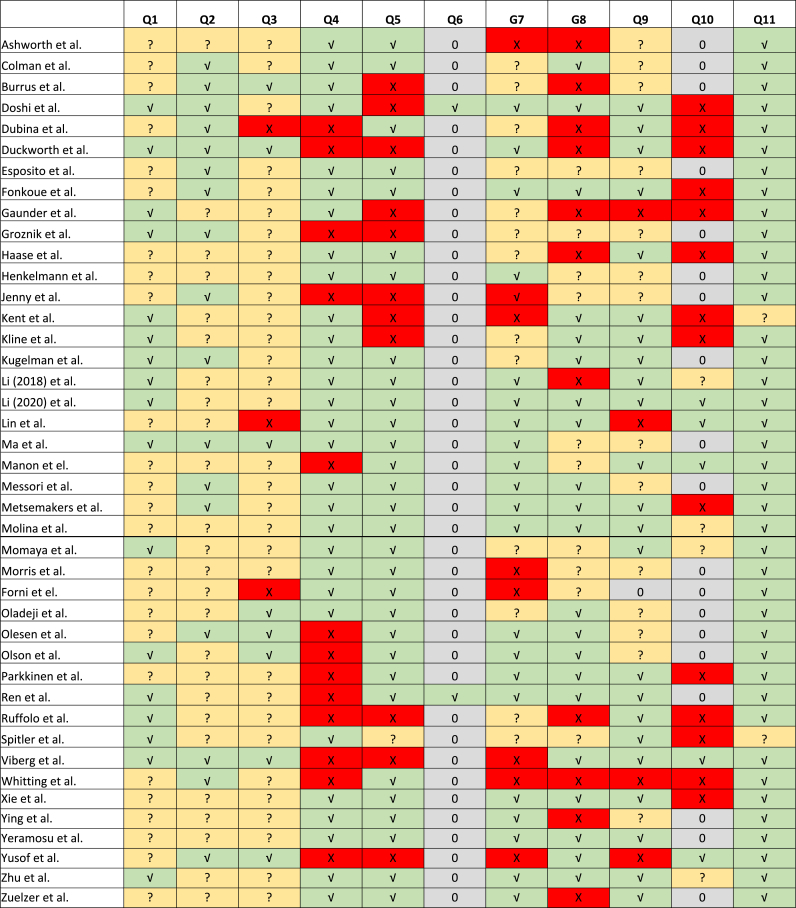
3.3. Risk of bias assessment
Study populations were generally similar and recruited from the same population (Fig. 2). Most studies identified confounding factors, and many performed multivariate regression analyses to adjust for confounders. Statistical analyses were performed accordingly, except for two studies.31,44
Fig. 2.
Risk of Bias Assessment
Green (✓) is ‘Yes’, yellow (?) is ‘Unclear’, red (✕) is ‘No’ and grey (0) is ‘Not applicable’.
However, the definition and measurement validity and reliability for exposures were unclear. Only 21 of the 42 studies defined SSI clearly according to our criteria, increasing the risk of information bias. While 21 studies had >6 months of follow-up, nine had <3 months of follow-up, which could lead to an underestimation. Only a few studies described strategies for addressing incomplete follow-up, creating a substantial risk of selection bias due to differential loss to follow-up since these were all cohort studies.
3.4. Outcomes
Information on 43 potentially influencing risk factors was included from 42 studies (Fig. 3). Ten risk factors were only examined in one study and are therefore not shown in Fig. 3. Twenty risk factors were eligible for meta-analysis since they were investigated in ≥5 studies. The meta-analysis is summarised in Table 2, and the funnel and forest plots can be found in Appendix B. The remaining risk factors were examined in 2–4 studies and are listed in Table 3, including risk factors examined in only one study. Three studies were consistently excluded from meta-analyses because of missing data7,8,17.
Fig. 3.
Risk Factor Occurrences
Blue bar depicts total number of risk factor occurrences and orange bar depicts number of significant results.
Table 2.
Overview of results from meta-analysis.
| Risk factor | Studies included | OR (95% CI) | P-value |
|---|---|---|---|
| Sex (male) | 29 | 1.6* (1.3–1.8) | <0.01 |
| Diabetes | 26 | 1.8 (0.95–3.3) | 0.07 |
| Smoking | 28 | 1.8* (1.5–2.1) | <0.01 |
| Open fracture | 25 | 3.6* (2.5–5.1) | <0.01 |
| Hypertension | 7 | 1.2 (0.7–2.1) | 0.49 |
| Gustillo G3 vs G1+2 | 15 | 3.1* (2.1–4.6) | <0.01 |
| ASA 3–4 vs 1-2 | 9 | 2.5* (1.5–4.1) | <0.01 |
| Compartment | 10 | 3.8* (2.4–6.0) | <0.01 |
| Polytrauma | 6 | 2.4* (1.5–4.0) | <0.01 |
| High energy | 11 | 1.5* (1.1–2.1) | 0.02 |
| External fixation | 14 | 2.9* (2.3–3.8) | <0.01 |
| Dual incision | 7 | 2.1* (1.5–3.0) | <0.01 |
| Duration of surgery | 7 | 0.62* (0.43–0.82) | <0.01 |
| Time to surgery | 9 | 0.42 (−0.68-1.52) | 0.45 |
| Blood transfusion | 6 | 3.8* (2.1–6.6) | <0.01 |
*Significant results with P-values <0.05.
Table 3.
Risk factors divided based on occurrence of significant association with infection.
| Significant result | Risk factors |
|---|---|
| All studies | Multiple comorbidities13,29 |
| IV drug use30 | |
| Comminution28 | |
| Pin-plate overlap29 | |
| Nighttime surgery30 | |
| 50% of studies | Intraoperative blood loss9,21,34,36 |
| Bone grafting21,23,38,43 | |
| Immunosuppressive drugs30,44 | |
| Fracture in shaft22,52 | |
| <50% of studies | Alcohol use21,23,36,42 |
| No studies | Drainage use9,34,36,43 |
| Surgery during summer9,34,36 | |
| Race38,39,45 | |
| Proximal fracture location22,41,52 | |
| Vascular injury38,44 | |
| Surgeon level (resident vs. visiting staff)9,34 | |
| Plate and screw vs. screw only21,36 | |
| Distal fracture location28,52 | |
| Tscherne classification20 | |
| Public vs private hospital20 | |
| Bone void filler27 |
A summary of fracture localization and risk factors can be seen in Appendix C. This table demonstrates that most data derive from tibia plateau fractures. We assumed that fracture localization did not influence the risk of infection. The table confirms this, as significant and not significant results are equally distributed across anatomical locations.
3.4.1. Patient-related risk factors
There were seven patient-related risk factors; age, male sex, diabetes, American Association of Anesthesiologists (ASA) classification, obesity, smoking, and hypertension. Meta-analyses were possible for sex, diabetes, ASA classification, smoking, and hypertension, showing significant associations with male sex, ASA classification >2, and active smoking (Table 2). No studies clearly defined smoking based on the amount consumed currently or previously. Furthermore, no studies defined blood pressure limits for hypertension or defined diabetes.
The remaining risk factors are listed in Table 4, showing the number of studies that included them and found a significant result.
Table 4.
Risk factors not eligible for meta-analysis.
Age data were ineligible for meta-analysis since most studies provided median or mean values. The same applies to obesity, where results were listed as mean values or divided into subgroups based on body mass index.
Table 5 shows the excluded studies’ data.
Table 5.
Data from studies not eligible for meta-analysis.
| Risk factor | Odds ratio estimates (95% CI) |
|---|---|
| Male sex | 2.1 (1.3–3.4)17,b |
| Diabetes | 1.4 (0.7–3.1)17,b |
| 5.87 (0.21–165.96)7,b | |
| ASA classification | 4.1 (1.4–12.3)42,a |
| 1.20 (0.23–6.19)b | |
| Smoking | 1.74 (0.87–3.49)7,b,* |
| Open fracture | 1.9 (1.2–3.0)17,b |
| 0.016 (0.001–0.269)8,b | |
| 5.84 (0.23–145.50)7,b | |
| Gustilo-Anderson classification I + II vs III | 1.34 (0.53–3.40)7,b |
| Compartment syndrome | 0.033 0.002–0.621)8,b |
| Polytrauma | 0.27 (0.02–3.29)7,b |
| Time to surgery | 1.1 (1.0–1.2)42 |
| External fixation | 2.0 (1.3–2.3)17 |
| 27.0 (1.74–419.36)7 | |
| Mean operative time | 1.3 (1.0–1.6)42,b |
| 1.78 (1.12–2.80)25 | |
| 2.72 (1.17–6.29)34,b |
*Non-significant result p-values >0.05.
Excluded due to different pooling of results.
Excluded due to missing results.
3.4.2. Fracture-related risk factors
There were seven fracture-related risk factors: open fracture, Gustilo–Anderson classification, compartment syndrome, polytrauma, high energy trauma, AO Foundation classification, and Schatzker classification. Meta-analyses were possible for open vs. closed fracture, Gustilo–Anderson classification type I + II vs. type III, compartment syndrome, polytrauma, and high-energy trauma, showing significant associations for all factors (Table 2).
While three studies stated that compartment syndrome was a clinical diagnosis and acutely treated with four-compartment fasciotomy,25,26,42 the remaining studies did not clarify the diagnosis further. Three studies defined polytrauma as having an Injury Severity Score >167,14,30. One study defined polytrauma as fractures in multiple sites in the tibia.28 The remaining three studies quantified polytrauma by adding points when patients sustained trauma to different body parts.9,34,35 Finally, two studies did not define low vs. high-energy trauma.44 The remaining studies had very similar definitions, with low energy defined as falls from standing height6,9,21,36 and high energy as traffic incidents and falls from height.
The remaining risk factors are listed in Table 4, showing the number of studies that included them and found a significant finding.
A meta-analysis of AO type 41 and 43 fractures could not be performed since the numbers of patients in several articles’ infected groups were <10 after AO classification. Neither was a meta-analysis of Schatzker classification possible due to different grouping and missing data.26
3.4.3. Surgery-related risk factors
There were five surgery-related risk factors: time to surgery, external fixation use, mean operative time, blood transfusions, and dual incision approach. Meta-analyses were possible for all factors, showing significant associations for external fixation use, blood transfusions, prolonged mean operative time, and dual incision approach (Table 2). The dual incision approach refers to operating through two separate incisions.
4. Discussion
In this systematic review, we conducted an extensive search to assess risk factors for postoperative tibial SSIs. To our knowledge, this is the first review to quantitively summarise existing data on risk factors for SSIs after ORIF for tibial fractures since our search found no existing reviews. We included 24,610 patients, of which 2,418 (9.8%) had SSIs, consistent with other similar studies.4,5,53,54
The systematic review included 42 studies, finding that SSIs were significantly associated with male sex, smoking, open fracture, Gustilo–Anderson score >2, blood transfusions, ASA score >2, compartment syndrome, high energy trauma, polytrauma, primary external fixation, dual incision approach, and prolonged surgery time.
Most included studies were retrospective cohort studies, often with significant selection and information bias risks. These studies have evident limitations since they depend directly on case documentation and lack traceability of further patient outcomes. Therefore, causality cannot be investigated and unambiguously established since any risk factors identified may be interactive and interrelated. For example, male patients could be more likely to sustain high-energy trauma or have higher alcohol consumption than female patients. Similarly, patients with polytrauma could be more likely to present with open fractures.
Despite these limitations, the current review has apparent advantages. We conducted a comprehensive literature search, including a larger sample size than similar reviews,4,5,55,56 enabling us to investigate numerous risk factors and collect data from up to 29 studies for a given risk factor. In case of missing data, authors were contacted in an attempt of collecting all existing data, this was however not possible to collect from all, contributing to risk of bias unpredictably.
Unlike other studies,4,55,57 diabetes was not a risk factor for SSIs in our analyses. While 26 studies examined diabetes mellitus as a risk factor for SSI, none defined diabetes or the presence of late complications or investigated the degree of glycemic control, increasing the risk of bias and possibly unpredictably affecting the results. If patients generally had well-controlled diabetes, this could explain the non-significant result to some extent. Furthermore, the mean age in population groups varied from 37 to 55 years in most studies and was 69 years in one study that only included patients aged >60 years.27 Therefore, the overall patient population was young and likely unaffected by late complications predisposing to SSIs.57,58 Finally, only 135 of 8.883 diabetic patients had SSIs. When events were divided into four groups for analysis, the number of diabetic patients with SSIs varied from zero to 16 across studies, with a mean of five. This low sample size reduced statistical power.
Compartment syndrome was the strongest predictor for SSIs (OR = 3.80), consistent with some studies5,35 and inconsistent with others.16,59,60 Ruffulo et al.16 found that a compartment syndrome diagnosis was not associated with increased SSI risk when pooling fasciotomy wounds closed primarily during or after definitive fixation. However, when examining only wounds closed secondarily, infection rates were significantly higher (OR = 7.5, p < 0.05). This finding may appear intuitively logical since open wounds are at greater risk of infection.5 As such, the presence of fasciotomy wounds may account for the increased risk of SSI. Zura et al.60 investigated how the timing of closing fasciotomy wounds affected SSI rates after ORIF for tibial plateau fractures, finding no significant association. Hak et al.59 showed that open fasciotomy wounds did not increase SSI risk after ORIF for tibial plateau fractures. However, both studies had low sample sizes and appreciable heterogeneity in study groups. Since little information exists on the optimal management of fasciotomy wounds concerning the subsequent definitive internal fixation,59 avoiding SSIs requires early compartment syndrome identification and implementing optimal wound care strategies.
Given the implications of SSIs, the importance of strategies for decreasing SSI risk is self-evident. While we cannot modify fracture-related risk factors, the high OR for SSIs with open fractures (OR = 3.6) and increasing Gustilo–Anderson score (OR = 3.1) emphasize the need for early intravenous antibiotic administration and adequate debridement. Further, a consequence of the current findings could be scheduled outpatient follow-ups including blood samples to detect SSIs sooner, especially when more risk factors are present. There is no evidence that patients benefit from postoperative continuation of prophylactic antibiotics61,62 but little data exist as to whether this also applies to patients with accumulating risk factors.
This leads to surgery-related risk factors; Blood transfusions were the second strongest predictor for SSIs (OR = 3.80). It is well established, that preoperative administration of prophylactic antibiotics prevents infection, but also that perioperative redosing is needed in case of excessive blood loss (i.e., >1,500 mL) to ensure adequate tissue and serum concentrations of the antimicrobial.61, 62, 63, 64 Included articles examining blood loss as a risk factor for SSI did not state, whether additional antibiotics were administered in case of excessive bleeding, one might speculate, that this was not the case.
The use of external fixation (OR = 2.9) and dual incision approach (OR = 2.1) were also predictors for SSI. While the operating physician decides on the use of external fixation and the number of incisions, this could also reflect a more complex and possibly open fracture with extensive soft tissue injury. Given that prolonged surgery time was also a risk factor for SSI, choosing a more experienced surgeon for high-risk patients could be wise to limit their surgery time. However, prolonged surgery time could also reflect more complex fractures.
Finally, attention must be given to preoperatively addressing potentially modifiable patient-related risk factors such as smoking (OR = 1.8) and ASA score (OR = 2.5), depending on the cause of the higher ASA scores.
5. Conclusions
This systematic review provides a basis for preoperatively assessing patient risk for developing a SSI, which could be used to initiate adjusted antibiotic regimes and more frequently postoperative controls. Furthermore, it indicates the risk factors future research should include when assessing for confounding factors.
This systematic review found that male sex, smoking, open fracture, a Gustilo–Anderson classification >2, an ASA classification >2, high energy trauma, blood transfusions, compartment syndrome, polytrauma, primary external fixation, dual incision approach, and prolonged surgery time were risk factors for SSI. However, the included studies were generally of poor quality and at risk of bias.
Availability of data, code, and other material
If cited correctly, we can clarify whether the data are available upon reasonable request.
Credit author statement
Diana Niebuhr: Validation, Investigation, Writing - Original Draft, Visualization. Thomas Mattson: Investigation. Niels Martin Jensen: Conceptualization, Methodology, Writing – Review & Editing. Bjarke Viberg: Conceptualization, Methodology, Writing – Review & Editing. Signe Steenstrup Jensen: Conceptualization, Methodology, Formal analysis, Writing – Review & Editing.
Funding statement
This work did not receive any financial or non-financial support, and the authors made the decision to publish.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2024.102376.
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- 1.Thompson J.H. StatPearls Publishing; 2021. Tibia Fractures Overview. Published online August. [PubMed] [Google Scholar]
- 2.Trampuz A. Diagnosis and treatment of infections associated with fracture-fixation devices. 2006;37:59–66. doi: 10.1016/j.injury.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 3.Whitehouse J.D., Friedman N.D., Kirkland K.B., Richardson W.J., Sexton D.J. The impact of surgical-site infections following Orthopedic surgery at a community hospital and a university hospital adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol. 2002;23(4):183–189. doi: 10.1086/502033. [DOI] [PubMed] [Google Scholar]
- 4.Shao J., Zhang H., Yin B., Li J., Zhu Y., Zhang Y. Risk factors for surgical site infection following operative treatment of ankle fractures: a systematic review and meta-analysis. Int J Surg. 2018;56:124–132. doi: 10.1016/j.ijsu.2018.06.018. [DOI] [PubMed] [Google Scholar]
- 5.Shao J., Chang H., Zhu Y., et al. Incidence and risk factors for surgical site infection after open reduction and internal fixation of tibial plateau fracture: a systematic review and meta-analysis. Int J Surg. 2017;41:176–182. doi: 10.1016/j.ijsu.2017.03.085. [DOI] [PubMed] [Google Scholar]
- 6.Manon J., Detrembleur C., van de VeyVer S., et al. Can Infect Predict Int Nailing Tibial Shaft Fract? Orig Stud. 2020;86 [Google Scholar]
- 7.Metsemakers W.J., Handojo K., Reynders P., Sermon A., Vanderschot P., Nijs S. Individual risk factors for deep infection and compromised fracture healing after intramedullary nailing of tibial shaft fractures: a single centre experience of 480 patients. Injury. 2015;46(4):740–745. doi: 10.1016/j.injury.2014.12.018. [DOI] [PubMed] [Google Scholar]
- 8.Kugelman D., Qatu A., Haglin J., Leucht P., Konda S., Egol K. Complications and unplanned outcomes following operative treatment of tibial plateau fractures. Injury. 2017;48(10):2221–2229. doi: 10.1016/j.injury.2017.07.016. [DOI] [PubMed] [Google Scholar]
- 9.Zhu Y., Liu S., Zhang X., Chen W., Zhang Y. Incidence and risks for surgical site infection after adult tibial plateau fractures treated by ORIF: a prospective multicentre study. Int Wound J. 2017;14(6):982–988. doi: 10.1111/iwj.12743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liberati A., Altman D.G., Tetzlaff J., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339 doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.PROSPERO.
- 12.Peduzzi P., Concato J., Kemper E., Holford T.R., Feinstein A.R. A simulation study of the number of events per variable in logistic regression analysis. 1996;49 doi: 10.1016/s0895-4356(96)00236-3. [DOI] [PubMed] [Google Scholar]
- 13.Duckworth A.D., Jefferies J.G., Clement N.D., White T.O. Type C tibial pilon fractures. Bone Joint J Publ online. 2016:98–1106. doi: 10.1302/0301-620X.98B8. [DOI] [PubMed] [Google Scholar]
- 14.Olson J.J., Anand K., Esposito J.G., et al. Complications and soft-tissue coverage after complete articular, open tibial plafond fractures. J Orthop Trauma. 2021;35(10):e371–e376. doi: 10.1097/BOT.0000000000002074. [DOI] [PubMed] [Google Scholar]
- 15.Viberg B., Kleven S., Hamborg-Petersen E., Skov O. Complications and functional outcome after fixation of distal tibia fractures with locking plate - a multicentre study. Injury. 2016;47(7):1514–1518. doi: 10.1016/j.injury.2016.04.025. [DOI] [PubMed] [Google Scholar]
- 16.Ruffolo M.R., Gettys F.K., Montijo H.E., Seymour R.B., Karunakar M.A. 2014. Complications of High-Energy Bicondylar Tibial Plateau Fractures Treated with Dual Plating through 2 Incisions.www.jorthotrauma.com [DOI] [PubMed] [Google Scholar]
- 17.Esposito J.G., van der Vliet Q.M.J., Heng M., et al. vol. 34. Lippincott Williams and Wilkins; 2020. Does surgical approach influence the risk of postoperative infection after surgical treatment of tibial pilon fractures? pp. 126–130. (Journal of Orthopaedic Trauma). [DOI] [PubMed] [Google Scholar]
- 18.Moola S Mztcaesksrcmqrmplkmpf. Chapter 7: Systematic Reviews of Etiology and Risk. JBI Manual for Evidence Synthesis.
- 19.Tufanaru C., Munn Z., Stephenson M., Aromataris E. Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. Int J Evid Base Healthc. 2015;13(3):196–207. doi: 10.1097/XEB.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 20.Doshi P., Gopalan H., Sprague S., Pradhan C., Kulkarni S., Bhandari M. Incidence of infection following internal fixation of open and closed tibia fractures in India (INFINITI): a multi-centre observational cohort study. BMC Muscoskel Disord. 2017;18(1) doi: 10.1186/s12891-017-1506-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li J., Zhu Y., Zhao K., et al. Incidence and risks for surgical site infection after closed tibial plateau fractures in adults treated by open reduction and internal fixation: a prospective study. J Orthop Surg Res. 2020;15(1) doi: 10.1186/s13018-020-01885-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Whiting P.S., Galat D.D., Zirkle L.G., Shaw M.K., Galat J.D. Journal of Orthopaedic Trauma. vol. 33. Lippincott Williams and Wilkins; 2019. Risk factors for infection after intramedullary nailing of open tibial shaft fractures in low- A nd middle-income countries; pp. E234–E239. [DOI] [PubMed] [Google Scholar]
- 23.Xie L., Liu G., Wang X., et al. Development of a nomogram to predict surgical site infection after open reduction and internal fixation for closed pilon fracture: a prospective single-center study. J Orthop Surg Res. 2023;18(1) doi: 10.1186/s13018-023-03598-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burrus M.T., Werner B.C., Yarboro S.R. Obesity is associated with increased postoperative complications after operative management of tibial shaft fractures. Injury. 2016;47(2):465–470. doi: 10.1016/j.injury.2015.10.026. [DOI] [PubMed] [Google Scholar]
- 25.Colman M., Wright A., Gruen G., Siska P., Pape H.C., Tarkin I. Prolonged operative time increases infection rate in tibial plateau fractures. Injury. 2013;44(2):249–252. doi: 10.1016/j.injury.2012.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dubina A.G., Paryavi E., Manson T.T., Allmon C., O'Toole R v. Surgical site infection in tibial plateau fractures with ipsilateral compartment syndrome. Injury. 2017;48(2):495–500. doi: 10.1016/j.injury.2016.10.017. [DOI] [PubMed] [Google Scholar]
- 27.Gaunder C.L., Zhao Z., Henderson C., McKinney B.R., Stahel P.F., Zelle B.A. Wound complications after open reduction and internal fixation of tibial plateau fractures in the elderly: a multicentre study. Int Orthop. 2019;43(2):461–465. doi: 10.1007/s00264-018-3940-9. [DOI] [PubMed] [Google Scholar]
- 28.Groznik M., Cimerman M., Lusa L., Gorenjec N.R., Ihan A. Increased perioperative C-reactive protein and decreased postoperative albumin is associated with acute posttraumatic osteomyelitis in patients with high-energy tibial fractures. Injury. 2019;50(4):827–833. doi: 10.1016/j.injury.2019.02.019. [DOI] [PubMed] [Google Scholar]
- 29.Haase L.R., Haase D.R., Moon T.J., et al. Is pin-plate overlap in tibial plateau fractures associated with increased infection rates? Injury. 2022;53(4):1504–1509. doi: 10.1016/j.injury.2022.01.017. [DOI] [PubMed] [Google Scholar]
- 30.Henkelmann R., Frosch K.H., Mende M., et al. Risk factors for deep surgical site infection in patients with operatively treated tibial plateau fractures: a retrospective multicenter study. J Orthop Trauma. 2021;35(7):371–377. doi: 10.1097/BOT.0000000000002011. [DOI] [PubMed] [Google Scholar]
- 31.Kent M., Mumith A., McEwan J., Hancock N. The service impact of failed locking plate fixation of distal tibial fractures: a service and financial evaluation at a major trauma centre. Eur J Orthop Surg Traumatol. 2015;25(8):1333–1342. doi: 10.1007/s00590-015-1706-2. [DOI] [PubMed] [Google Scholar]
- 32.Kline A.J., Gruen G.S., Pape H.C., Tarkin I.S., Irrgang J.J., Wukich D.K. Early complications following the operative treatment of pilon fractures with and without diabetes. Foot Ankle Int. 2009;30(11):1042–1047. doi: 10.3113/FAI.2009.1042. [DOI] [PubMed] [Google Scholar]
- 33.Jenny J.Y., Jenny G., Kempf I. Infection after reamed intramedullary nailing of lower limb fractures: a review of 1,464 cases over 15 years. Acta Orthop. 1994;65(1):94–96. doi: 10.3109/17453679408993727. [DOI] [PubMed] [Google Scholar]
- 34.Li J., Zhu Y., Liu B., Dong T., Chen W., Zhang Y. Incidence and risk factors for surgical site infection following open reduction and internal fixation of adult tibial plateau fractures. Int Orthop. 2018;42(6):1397–1403. doi: 10.1007/s00264-017-3729-2. [DOI] [PubMed] [Google Scholar]
- 35.Lin S., Mauffrey C., Hammerberg E.M., Stahel P.F., Hak D.J. Surgical site infection after open reduction and internal fixation of tibial plateau fractures. Eur J Orthop Surg Traumatol. 2014;24(5):797–803. doi: 10.1007/s00590-013-1252-8. [DOI] [PubMed] [Google Scholar]
- 36.Ma Q., Aierxiding A., Wang G., Wang C., Yu L., Shen Z. Incidence and risk factors for deep surgical site infection after open reduction and internal fixation of closed tibial plateau fractures in adults. Int Wound J. 2018;15(2):237–242. doi: 10.1111/iwj.12856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Molina C.S., Stinner D.J., Fras A.R., Evans J.M. Risk factors of deep infection in operatively treated pilon fractures (AO/OTA: 43) J Orthop. 2015;12:S7–S13. doi: 10.1016/j.jor.2015.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Momaya A.M., Hlavacek J., Etier B., et al. Risk factors for infection after operative fixation of Tibial plateau fractures. Injury. 2016;47(7):1501–1505. doi: 10.1016/j.injury.2016.04.011. [DOI] [PubMed] [Google Scholar]
- 39.Morris B.J., Unger R.Z., Archer K.R., Mathis S.L., Perdue A.M., Obremskey W.T. Risk factors of infection after ORIF of bicondylar tibial plateau fractures. 2013. www.jorthotrauma.com [DOI] [PubMed]
- 40.Oladeji L.O., Platt B., Crist B.D. Diabetic pilon factures: are they as bad as we think? J Orthop Trauma. 2021;35(3):149–153. doi: 10.1097/BOT.0000000000001904. [DOI] [PubMed] [Google Scholar]
- 41.Olesen U.K., Juul R., Bonde C.T., et al. A review of forty five open tibial fractures covered with free flaps. Analysis of complications, microbiology and prognostic factors. Int Orthop. 2015;39(6):1159–1166. doi: 10.1007/s00264-015-2712-z. [DOI] [PubMed] [Google Scholar]
- 42.Parkkinen M., Madanat R., Lindahl J., Mäkinen T.J. Risk factors for deep infection following plate fixation of proximal tibial fractures. J Bone Joint Surg- American. 2016;98(15):1292–1297. doi: 10.2106/JBJS.15.00894. [DOI] [PubMed] [Google Scholar]
- 43.Ren T., Ding L., Xue F., He Z., Xiao H. Risk factors for surgical site infection of pilon fractures. Clinics. 2015;70(6):419–422. doi: 10.6061/clinics/2015(06)06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Spitler C.A., Hulick R.M., Weldy J., Howell K., Bergin P.F., Graves M.L. What are the risk factors for deep infection in OTA/AO 43C pilon fractures? J Orthop Trauma. 2020;34(6):E189–E194. doi: 10.1097/BOT.0000000000001726. [DOI] [PubMed] [Google Scholar]
- 45.Yeramosu T., Satpathy J., Perdue P.W., et al. Risk factors for infection and subsequent adverse clinical results in the setting of operatively treated pilon fractures. J Orthop Trauma. 2022;36(8):406–412. doi: 10.1097/BOT.0000000000002339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yusof NM, Khalid KA, Hafiz Zulkifly A, Zakaria Z, Azril M, Amin M, et al. Factors Associated with the Outcome of Open Tibial Fractures. www.mjms.usm.my. [PMC free article] [PubMed]
- 47.Zuelzer D.A., Hayes C.B., Hautala G.S., et al. Early antibiotic administration is associated with a reduced infection risk when combined with primary wound closure in patients with open tibia fractures. Clin Orthop Relat Res. 2021;479(3):613–619. doi: 10.1097/CORR.0000000000001507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ashworth T.J., Alvarez P.M., Laux J.P., Ganga S., Ostrum R.F. 2022. A Multicenter Retrospective Analysis of Risk Factors for Poor Outcomes after Tibial Pilon Fractures.www.c-orthopaedicpractice.com [Google Scholar]
- 49.Messori M., Touloupakis G., Gilli A., et al. The risk of infection in open distal tibial fracture: the DANGER score. Eur J Orthop Surg Traumatol. 2023;33(7):2965–2970. doi: 10.1007/s00590-023-03517-x. [DOI] [PubMed] [Google Scholar]
- 50.Ying H., Guo B.W., Wu H.J., Zhu R.P., Liu W.C., Zhong H.F. Using multiple indicators to predict the risk of surgical site infection after ORIF of tibia fractures: a machine learning based study. Front Cell Infect Microbiol. 2023;13 doi: 10.3389/fcimb.2023.1206393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nogueira Forni J.E., Tardivo Fraga S.E., Jalikj W. Risk factors for infection in patients undergoing osteosynthesis for tibial plateau fracture in a university hospital. Cureus. Publ online April. 2022;29 doi: 10.7759/cureus.24587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fonkoue L., Tissingh E.K., Muluem O.K., et al. Predictive factors for fracture-related infection in open tibial fractures in a Sub-Saharan African setting. Injury. 2023;(7):54. doi: 10.1016/j.injury.2023.05.047. [DOI] [PubMed] [Google Scholar]
- 53.de Carvalho R.L.R., Campos C.C., Franco LM. de C., Rocha A. de M., Ercole F.F. Incidence and risk factors for surgical site infection in general surgeries. Rev Lat Am Enfermagem. 2017;25 doi: 10.1590/1518-8345.1502.2848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mu Y., Edwards J.R., Horan T.C., Berrios-Torres S.I., Fridkin S.K. Improving risk-adjusted measures of surgical site infection for the national healthcare safely network. Infect Control Hosp Epidemiol. 2011;32(10):970–986. doi: 10.1086/662016. [DOI] [PubMed] [Google Scholar]
- 55.Gortler H., Rusyn J., Godbout C., Chahal J., Schemitsch E.H., Nauth A. Diabetes and healing outcomes in lower extremity fractures: a systematic review. Injury. 2018;49(2):177–183. doi: 10.1016/j.injury.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 56.Wang TaoGJunfeiLYubin. Predictors of acute compartment syndrome in patients with tibial fractures: a meta-analysis. Int Orthop. 2023;47(1):51–56. doi: 10.1007/s00264-022-05643-3. [DOI] [PubMed] [Google Scholar]
- 57.Dane K. Wukich MAJDMRDCRBJJIPPA. Outcomes of ankle fractures in patients with uncomplicated VersusComplicated diabetes. Foot Ankle Int. 2011;32(2):113–224. doi: 10.3113/FAI.2011.0120. [DOI] [PubMed] [Google Scholar]
- 58.Jones K.B., Maiers-Yelden K.A., Marsh J.L., et al. Ankle fractures in patients with diabetes mellitus. 2005;87(4) doi: 10.1302/0301-620X.87B4. [DOI] [PubMed] [Google Scholar]
- 59.Hak Djmmlmmgdr Do. Influence of prior fasciotomy on infection after open reduction and internal fixation of tibial plateau fractures. Injury. 2010;69(4):886–888. doi: 10.1097/TA.0b013e3181b83fe9. [DOI] [PubMed] [Google Scholar]
- 60.Zura R. Adams S. Jeray K. Obremskey W. Stinett S. Olson S. Timing of definitive fixation of severe tibial plateau fractures with compartment syndrome does not have an effect on the rate of infection. J Trauma Inj Infect Crit Care. 2010;69(6):1523–1526. [DOI] [PubMed]
- 61.Noble D.W.G.I. Antibiotics for surgical patients: the faster the better? Lancet Infect Dis. 2012:741–742. doi: 10.1016/S1473-3099(12)70208-6. [DOI] [PubMed] [Google Scholar]
- 62.Bratzler D.W., Dellinger E.P., Olsen K.M., et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect. 2013;14(1):73–156. doi: 10.1089/sur.2013.9999. [DOI] [PubMed] [Google Scholar]
- 63.Zelenitsky S.A., Ariano R.E., Harding G.K.M., Silverman R.E. Antibiotic pharmacodynamics in surgical prophylaxis: an association between intraoperative antibiotic concentrations and efficacy. Antimicrob Agents Chemother. 2002;46(9):3026–3030. doi: 10.1128/AAC.46.9.3026-3030.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Swoboda SM, Merz C, Kostuik J, Trentler B, Lipsett PA. Does Intraoperative Blood Loss Affect Antibiotic Serum and Tissue Concentrations?. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.