Abstract
Scrub typhus is caused by Orientia tsutsugamushi infection and occurs frequently in an area called the Tsutsugamushi Triangle. Currently, there is no vaccine for O. tsutsugamushi, and its infection is treated with antibiotics such as doxycycline. Scrub typhus responds to effective treatment, and early treatment shortens the course of the disease, reduces mortality, and accelerates recovery. Therefore, it is important to rapidly diagnose O. tsutsugamushi infection to ensure successful outcomes. Here, we developed a CRISPR-Cas12a-based diagnostic method targeting the bacterial 16S rRNA to detect O. tsutsugamushi infection of all known genotypes. To reduce the possibility of contamination and increase field applicability, we designed the one-pot assay system in addition to conventional two-pot assay system. Using this method, we successfully detected up to 100 copies of in vitro transcribed O. tsutsugamushi 16S rRNA within 1 hour under isothermal conditions. In blood samples from patients confirmed to be infected with O. tsutsugamushi by nested PCR, the developed method exhibited a clinical sensitivity of 98% and high specificity. These data demonstrate that the presented method is applicable for the rapid and universal diagnosis of scrub typhus to facilitate timely and appropriate treatment.
Author summary
Early treatment with antibiotics can shorten the course of scrub typhus, reduce mortality, and accelerate recovery, making the rapid diagnosis of O. tsutsugamushi infection critically important. In this study, we developed a CRISPR-Cas12a-based rapid diagnostic method targeting the bacterial 16S rRNA to detect O. tsutsugamushi infection across all known genotypes. Using this method, we successfully detected as few as 100 copies of in vitro-transcribed O. tsutsugamushi 16S rRNA within 1 hour under isothermal conditions. In blood samples from patients confirmed to be infected with O. tsutsugamushi by nested PCR, the developed method demonstrated a clinical sensitivity of 98% and high specificity.
Introduction
Scrub typhus, caused by Orientia tsutsugamushi (O. tsutsugamushi), is a clinically significant vector-borne disease prevalent in the Asia-Pacific region, particularly within the Tsutsugamushi Triangle, which encompasses the Russian Far East, northern Australia, Afghanistan, and surrounding areas. Transmission occurs via the bite of infected Trombiculidae larvae, with clinical symptoms including fever, rash, and eschar at the bite site [1]. Severe cases may lead to complications such as hemophagocytic syndrome, meningitis, and multi-organ failure, with a mortality rate of approximately 6% without treatment [1–4]. Appropriate antibiotic therapy, including doxycycline, tetracycline, chloramphenicol, and azithromycin, reduces the mortality rate to 1.4% [1,2,5,6]. Despite its clinical significance, there is no effective vaccine for scrub typhus, making early and accurate diagnosis essential to reducing mortality and improving patient outcomes [7].
Currently, culture tests, antibody-detection tests, and nucleic acid-based tests (NATs) are used to diagnose O. tsutsugamushi [8–12]. Culture tests take several weeks to perform, have a sensitivity < 50%, and must be performed in a BSL-3 laboratory; thus, this strategy is more often used for bacterial isolation than for diagnosis [13]. The antibody-detection tests include those based on an indirect immunofluorescent-antibody test (IFA), passive hemagglutination assay (PHA), and enzyme-linked immunosorbent assay (ELISA) [8,10,14]. IFA can be used to compare the antibody titer between the acute and convalescent phases, and is widely used for diagnostic purposes due to its high sensitivity and specificity [8]. However, it requires expensive equipment, such as a fluorescence microscope, and cannot be scaled up for high-throughput diagnosis. Given this, IFA is most commonly used as a confirmation test in current practice [15]. ELISA is also used to compare antibody titers for diagnostic purposes; it is less costly than IFA while yielding a similar sensitivity [14]. However, both of these techniques require comparison of antibody values in the acute and convalescent phases, and thus are not easily applicable for early diagnosis. PHA enables the user to visually detect the degree to which a patient’s serum aggregates with the antigen, but its sensitivity is low [10]. NATs using real-time or nested PCR represent the current standard for diagnosing O. tsutsugamushi infection; it and IFA are the most widely used methods for diagnosing scrub typhus [9,11]. However, real-time PCR may return false positives due to non-specific amplification and nested PCR, which avoids false positives, requires a secondary amplification step.
O. tsutsugamushi is an obligate, intracellular bacterium which belongs to family Rickettsiaceae and causes scrub typhus. Although the 16S rRNA sequence of O. tsutsugamushi matches those of Rickettsia species of the same family by about 90% [16–18], major differences are seen in their cell wall components. The cell walls of Rickettsia comprise lipopolysaccharides, outer membrane B, and a 17-kDa lipoprotein, whereas those of O. tsutsugamushi lack these components and instead have a 56 kDa type-specific antigen (TSA56) that serves as a criterion for the diversity of O. tsutsugamushi strains [19, 20]. O. tsutsugamushi was initially classified into three prototypes (Karp, Kato, and Gilliam) based on antigenic similarity detected by complement-fixation (CF) analysis [21, 22]. Subsequently, the TSA56, which exhibits high antigenic variability, was used as a major antigenic determinant. Based on sequence analysis of the TSA56, researchers proposed nine distinct genotypes of O. tsutsugamushi in 2009, namely Karp, Kuroki, TA763, Gilliam, Kawasaki, Japanese Gilliam, Kato, Saitama, and Shimokoshi [23].
Recently, a field-applicable rapid molecular method for diagnosing pathogenic infection was developed based on the clustered regularly interspaced short palindromic repeat (CRISPR) and CRISPR-associated proteins (Cas) immune system of bacteria [24–26]. The CRISPR-Cas system uses an RNA-guided endonuclease to provide sequence-specific immunity against an invaded nucleic acid sequence (e.g., from a plasmid or bacteriophage). The RNA used for the RNA-guided endonuclease is called guide RNA (gRNA) or CRISPR RNA (crRNA) and is derived from the invaded nucleic acid sequence. The previously reported diagnostic method utilized a Cas12a protein comprising a gRNA complementary to the target DNA sequence plus a T nucleotide-rich protospacer-adjacent motif (PAM). Binding of Cas12a to a target DNA activated its trans-cleavage activity to cleave nearby single-strand DNA. Using Cas12a and isothermal amplification, Jenifer Doudna and colleagues developed a molecular diagnostics technology called DNA Endonuclease-TargEted CRISPR Trans Reporter (DETECTR) [24]. Various pathogens, including human papilloma viruses (HPV), severe acute respiratory syndrome corona virus 2 (SARS-CoV-2), severe fever with thrombocytopenia syndrome virus (SFTSV), and human immunodeficiency virus (HIV) were detected using the DETECTR platform, and Cas12a-based pathogen diagnosis is currently utilized in the clinic [24,27,28].
In the present study, we designed a primer-gRNA set for the targeted detection of the 16S rRNAs of O. tsutsugamushi. The 16S rRNA sequence is commonly used for bacterial classification. Unlike other mRNA molecules, this rRNA resembles DNA in having a stable structure with many secondary structures, and thus is not easily degraded during its isolation from cells or use in experiments. Furthermore, whereas O. tsutsugamushi contains a single copy of a given DNA target [29], it may have hundreds to thousands of copies of an RNA target. The O. tsutsugamushi 16S rRNA is transcribed consistently enough to be used as a housekeeping gene in the microarray analysis [30]. For these reasons, we hypothesized that using the 16S rRNA gene as a detection target would yield high-level sensitivity for O. tsutsugamushi. Both antibody-detection tests and NATs for scrub typhus diagnosis rely on the TSA56. However, the high antigenic variability of TSA56 complicates these methods, resulting in inconsistent detection and reduced sensitivity [31]. Molecular diagnostics targeting the conserved 16S rRNA sequence address these limitations, enabling consistent and reliable detection across diverse O. tsutsugamushi genotypes. We designed primer-gRNA sets to detect nine genotypes of O. tsutsugamushi, and used them to develop a CRISPR-Cas12a-based diagnostic method for detecting O. tsutsugamushi, which we named O. tsutsugamushi DETECTR or OT DETECTR.
Materials and methods
Ethics statement
This study was approved by the Institutional Review Board (IRB) of Jeju National University Hospital (IRB no.2022-05-002). Written informed consent was obtained from all the participants.
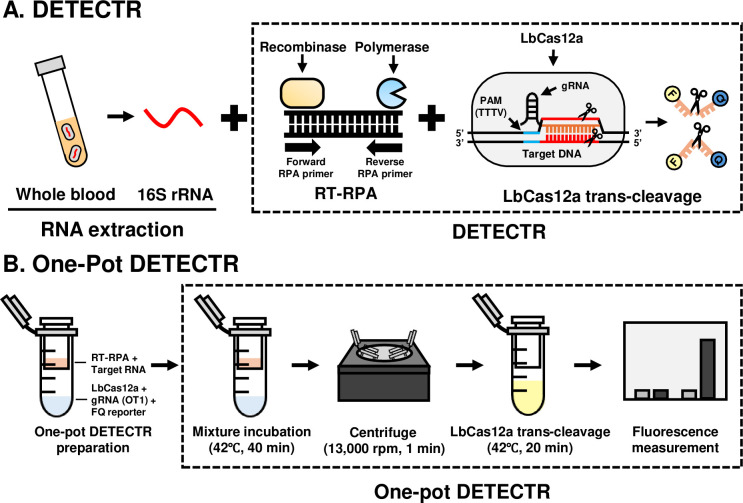
Two-pot OT DETECTR
In our two-pot Cas12a-based diagnostic method, the isothermal amplification and Cas12a trans-cleavage steps were performed in different Eppendorf tubes (two-pot) at two different temperatures (Fig 1A). The bacterial DNA and RNA were amplified by recombinase polymerase amplification (RPA) and reverse transcription recombinase polymerase amplification (RT-RPA), respectively, using a TwistAmp Basic kit (TwistDx, Cambridge, UK). The utilized primer sets, designed to detect the OT1 and OT2 sequences (Table 1), were designed according to the provided protocol, with reference to the aligned 16S rRNA sequence for nine genotypes of O. tsutsugamushi (S1 Fig): Karp, Kuroki, TA763, Gilliam, Kawasaki, Japanese Gilliam, Kato, and Shimokoshi (GenBank accession numbers: NR_025860.1, D38626.1, NZ_OUNA00000000.1, D38622.1, D38625.1, AP008981.1, NZ_LS398550.1, D38627.1, respectively; NCBI). The Saitama strain was excluded because it was not published in NCBI. As described in the provided protocol, the RPA reaction mixture comprised 29.5 μL rehydration buffer, 2.4 μL forward and reverse primers (10 μM each), and 2.5 μL of 280 mM magnesium acetate, with samples and nuclease-free water added obtain a final volume of 50 μL. Each RPA reaction mixture was incubated at 39°C for 40 min. The RT-RPA reaction mixture comprised 29.5 μL rehydration buffer, 2.4 μL forward and reverse primers (10 μM each), 1 μL SuperScript IV Reverse Transcriptase (Invitrogen, Waltham, Massachusetts, USA), 1 μL RNase inhibitor (Enzynomics, Daejeon, Korea), and 2.5 μL of 280 mM magnesium acetate, with samples and nuclease-free water added to obtain a final volume of 50 μL. Each RT-RPA reaction mixture was incubated at 42°C for 40 min.
Fig 1. Schematic diagrams of OT DETECTRs.
(A) Conventional two-pot OT DETECTR. (B) One-pot OT DETECTR.
Table 1. RT-RPA primer and gRNA sequences.
| Target gene | Sequence | PAM | ||
|---|---|---|---|---|
| RT-RPA primer | OT1-F | 16S rRNA | GGCTTAACCCTGGAACTGCTTCTAAAACTG | |
| OT1-R | 16S rRNA | CTTTCGCCACTGGTGTTCCTTCTAATATCT | ||
| OT2-F | 16S rRNA | GTGCTAGATATTGGGGGATTTTTCTTTCAG | ||
| OT2-R | 16S rRNA | TTGGTAAGGTTTTTCGCGGATCATCGAATT | ||
| gRNA | OT1 | 16S rRNA | TAGTGTAGAGGTAAAATTCT | TTTC |
| OT2 | 16S rRNA | GTAGCTAACGCATTAAGCAC | TTTC |
LbCas12a trans-cleavage assays were performed as previously described [24,27]. To design gRNA for detection the nine types of O. tsutsugamushi, the previously reported O. tsutsugamushi 16S rRNA sequences were obtained from NCBI and screened for shared subsequences. From this analysis, we designed and synthesized two gRNAs, OT1 and OT2 which corresponded to nucleotides 615–634 and 791–810, respectively (Bioneer, Daejeon, Korea) and were expected to specifically detect the O. tsutsugamushi 16S rRNA of all nine genotypes but not those of other bacterial genomes (Table 1). LbCas12a (New England Biolabs, Ipswich, Massachusetts, USA) and LbCas12a-specific gRNA were mixed with 1× NEBuffer 2.1 to final concentrations of 50 nM and 62.5 nM, respectively, and then mixed together and incubated at 37°C for 30 min to generate LbCas12a-gRNA complexes. For fluorescence assays, 2 μL of RT-RPA products, 80 μL of 1× NEBuffer 2.1, 18 μL of LbCas12a-gRNA complex and 2 μL of 10 μM FQ-labeled reporter (/56-FAM/TTATT/3IABkFQ/; Integrated DNA Technologies, Coralville, IA, USA) were dispensed directly to 96-well microplates, which were incubated at 37°C for 20 min. Fluorescence measurements were taken at the beginning and end of the incubation period using the Glomax Discover Microplate Reader (Promega, Madison, WI, USA) equipped with version 4.0.0 software (λex, 485 nm; λem, 535 nm). To simplify the visualization of results, we used a lateral flow assay (LFA). For the LFA, 2 μL of RT-RPA products, 40 μL of 1× NEBuffer 2.1, 36 μL of LbCas12a-gRNA complex and 2 μL of 10 μM lateral flow cleavage reporter (/56-FAM/TTATT/3Bio/; Integrated DNA Technologies) were combined in an Eppendorf tube and incubated at 37°C for 20 min. A Milenia HybriDetect 1 lateral flow strip (Milenia Biotec, Giesesen, Germany) was applied to the incubated sample according to the manufacturer’s instructions. The results were examined after 2 min and interpreted as previously described [27].
One-pot OT DETECTR
To prevent contamination and increase the field-applicability of OT DETECTR, we designed a one-pot OT DETECTR that is performed in a single tube. For this method, the LbCas12a-gRNA complex was generated by combining 3 μL of 1μM LbCas12a, 1 μL of 10 μM gRNA, 2 μL of 10 μM FQ-labeled reporter, and 54 μL of 1× NEBuffer 2.1 in an Eppendorf tube, which was then fitted with a 0.22 μm filter tube (SPL Life Sciences, Pocheon, Korea). The above-described RT-RPA mixture was loaded to the 0.22 μm-filter tube, and the assemblage was incubated at 42°C for 40 min. The LbCas12a-gRNA complex and RT-RPA product were then mixed via centrifugation (13,000 rpm, 1 min) and further incubated at 42°C for 20 min (Fig 1B). Fluorescence results were obtained at the start and end of incubation (λex, 485 nm; λem, 535 nm).
Bacteria
Bacterial cultures of Staphylococcus aureus (SA), Klebsiella pneumoniae (KP), Salmonella enteritidis (SE), and E. coli were grown overnight at 37°C in 5 mL LB broth, and bacterial RNA was extracted using a bacterial RNA extraction kit (Bioneer, Daejeon, Korea). SA, KP and SE were kindly provided by Dr. Young-Seo Park (Gachon University, Korea).
O. tsutsugamushi (Ikeda strain; National Culture Collection for Pathogens, NCCP) was inoculated to a monolayer of L929 cells. At 4 days post-infection, the cells were collected and homogenized with sterile glass beads using a TissueLyser II (Qiagen, Hilden, Germany). The homogenate was centrifuged at 500×g for 5 min, the supernatant was collected, and cell-free bacteria were collected by high-speed centrifugation at 6000×g for 30 min and resuspended in DMEM. The infectivity titer of the inoculum was determined using an immunofluorescence assay, and the infected cell-counting unit (ICU) was calculated as follows: ICU = (total number of cells used for infection) × (ratio of infected cells to counted cells) × (dilution fold of O. tsutsugamushi Ikeda inoculum) [32]. The O. tsutsugamushi genomic DNA and RNA were extracted using Qiagen DNeasy Blood & Tissue Kit and Qiagen RNeasy Mini Kit (Qiagen, Hilden, Germany), respectively. The O. tsutsugamushi genomic DNA and RNA were used for comparative testing of O. tsutsugamushi DNA molecules and RNA molecules content rates.
In vitro transcription of O. tsutsugamushi and Rickettsia spp. 16S rRNAs
The 16S rRNA was synthesized by an in vitro transcription (IVT) reaction and used to test the limit of detection (LoD) and specificity for each version of OT DETECTR. The 16S rRNA sequences of 8 strains O. tsutsugamushi: Karp, Kuroki, TA763, Gilliam, Kawasaki, Japanese Gilliam, Kato, and Shimokoshi (GenBank accession numbers: NR_025860.1, D38626.1, NZ_OUNA00000000.1, D38622.1, D38625.1, AP008981.1, NZ_LS398550.1, D38627.1, respectively; NCBI), were synthesized in plasmid form (Macrogen, Seoul, Korea) and PCR amplified using primers with T7 promoter sequences (Table 2). The primers and gRNA designed for O. tsutsugamushi detection showed similarity to regions in the 16S rRNA of Rickettsia spp., including species from the spotted fever and typhus groups (S1 Table). This region was identical across all 18 Rickettsia species analyzed, and the sequence was synthesized as plasmid DNA for experimental use. The 16S rRNA sequence was then amplified using primers with T7 promoter sequences (Table 2). For the IVT reaction, the mMESSAGE mMACHINE T7 Transcription kit (Invitrogen, Waltham, MA, USA) was applied according to the manufacturer’s instructions, with the above-described PCR products used as the template. The synthesized 16S rRNA was purified with a GeneJET RNA Cleanup and Concentration Micro Kit (Thermo Scientific, Waltham, MA, USA).
Table 2. PCR primers used for in vitro transcription.
| Bacteria | Primer | Sequence |
|---|---|---|
| O. tsutsugamushi | T7 OT-F’ | TAATACGACTCACTATAGGGAGAAACGAACGCTGGCGG |
| T7 OT-R’ | GCAGGTTCCCCTACGGCTACCTTGTTACGACTTTAC | |
| Rickettsia spp. | T7 RS-F’ | TAATACGACTCACTATAGGGAGAGGCTTAACCTCGGAA |
| T7 RS-R’ | CCTTCGCCACCGGTGTTCCTCCTAATATCTAAGAATTT |
Preparation of O. tsutsugamushi clinical samples
All O. tsutsugamushi cases were confirmed using nested PCR, a method commonly employed for its diagnosis in Korea, at Jeju National University Hospital (Jeju, Korea). To confirm O. tsutsugamushi infection in clinical samples, bacterial DNA and RNA were extracted from whole blood using a QIAamp DNA Blood Mini kit (Qiagen, Hilden, Germany) and QIAamp RNA Blood Mini kit (Qiagen, Hilden, Germany), respectively. Nested PCR was performed as previously described [11] to detect the gene encoding the TSA56 of O. tsutsugamushi in extracted bacterial DNA, and OT DETECTR was performed to detect the 16S rRNA of O. tsutsugamushi in bacterial RNA.
Statistical analysis
Data are expressed as mean ± standard deviation (SD) of three independent experiments. The significance of differences between two means was determined with the Student’s t-test using GraphPad Prism 7 (GraphPad Software, Inc., Sandiego, CA. USA). P-values were determined by unpaired two-sided Student’s t-tests. P-values < 0.05 were considered statistically significant.
Results
Designing a CRISPR-Cas12a-based assay for O. tsutsugamushi
We herein designed a CRISPR-Cas12a-based diagnostic assay for rapid and accurate diagnosis of O. tsutsugamushi 16S rRNA and designated it OT DETECTR. The 16S rRNA of O. tsutsugamushi was selected as the target because it has a stable secondary structure and exists in more copies than a DNA target would. We screened previously reported sequences of O. tsutsugamushi to design RPA primer-gRNA sets that recognized the 16S rRNAs of all O. tsutsugamushi genotypes but not those of other organisms, and selected two sets, OT1 and OT2 (S1 Fig.). The O. tsutsugamushi 16S rRNA was extracted using a column-based extraction kit, amplified by isothermal amplification (RT-RPA), and detected by leveraging Cas12a trans-cleavage activity (Fig 1A), which was determined by either fluorescence assay or LFA. To prevent contamination and increase the field applicability of our method, we further developed a one-pot OT DETECTR in which all reactions are performed in a single tube at the same temperature (Fig 1B), as compared to the two-pot OT DETECTR.
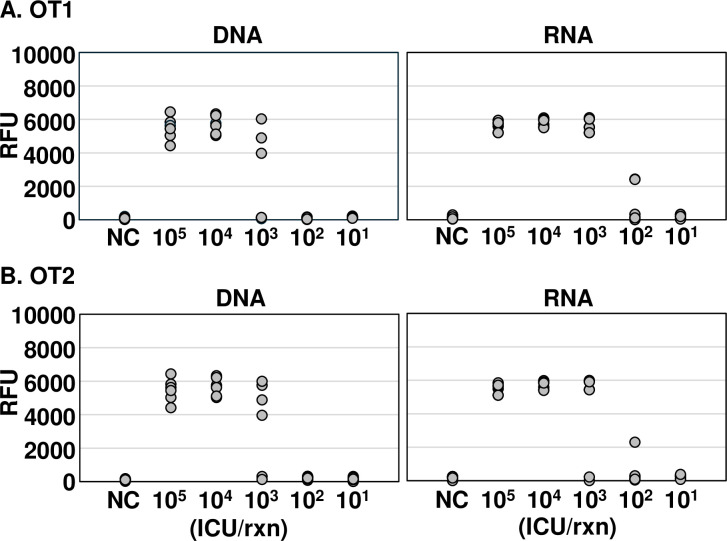
Using nucleic acids extracted from O. tsutsugamushi, we found that our 16S rRNA-based diagnostic method was more sensitive for RNA than DNA (Fig 2). DNA and RNA were extracted from various infected-cell counting units (ICUs) of O. tsutsugamushi, and the sensitivity of OT DETECTR was compared using a detection versus non-detection approach. The OT1 set could detect O. tsutsugamushi DNA at a titer of 104 ICU per reaction and RNA at a titer of 103 ICU per reaction, indicating that RNA target detection was 10 times more sensitive than DNA target detection (Fig 2A). The OT2 set detected both DNA and RNA of O. tsutsugamushi at a titer of 104 ICU per reaction and thus showed the same sensitivity (Fig 2B). Based on these results, we used the OT1 primer-gRNA set in subsequent experiments.
Fig 2. Comparative analysis of the sensitivity of the OT DETECTRs to O. tsutsugamushi DNA and RNA.
Various ICUs (105 to 101) of O. tsutsugamushi were lysed with a column-based extraction kit, and nucleic acids (DNA and RNA) were amplified via RT-RPA with primer sets specific for the 16S rRNA gene. RT-RPA products were detected using two-pot OT DETECTR combined with a fluorescence assay. Shown are results obtained using gRNAs (A) OT1 and (B) OT2 (n = 6 replicates). RFU, relative fluorescence unit; NC, no template control; ICU, infected cell-counting unit.
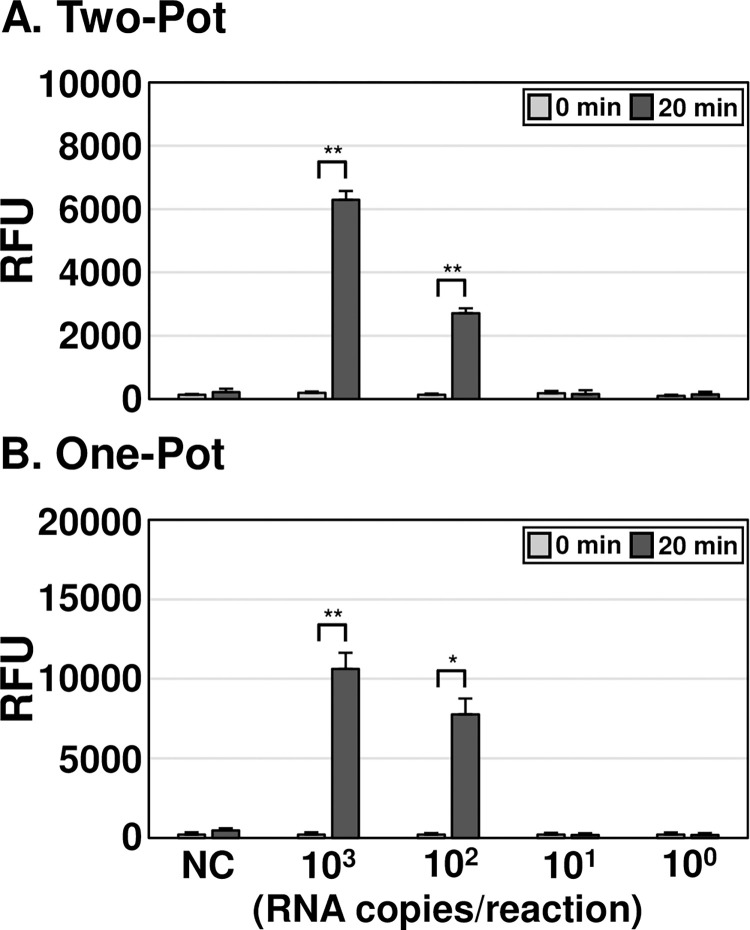
Measuring of the limit of detection (LoD) for OT DETECTR
To determine the LoD of the assay, two-pot and one-pot OT DETECTR methods combined with a fluorescence assay were performed using varying copy numbers of in vitro transcribed O. tsutsugamushi 16S rRNA from the Karp strain. Both OT DETECTRs could detect as little as 100 RNA copies per reaction (Fig 3A and 3B). The one-pot OT DETECTR showed higher fluorescence values compared to the two-pot DETECTR: The fluorescence values of the one-pot OT DETECTR were 70% and 187% higher than those of the two-pot DETECTR for 103 and 102 RNA copies per reaction, respectively.
Fig 3. LoD analyses of OT DETECTRs.
(A, B) To determine the LoD of each OT DETECTR, different copy numbers (103 to 100) of IVT O. tsutsugamushi 16S rRNA were used as templates for the (A) two-pot and (B) one-pot OT DETECTR combined with a fluorescence assay. Values are presented as means ± s.d. (error bars) (n = 3 replicates; ** P < 0.01, * P < 0.05 between samples, two-sample t-test). RFU, relative fluorescence unit; NC, no template control.
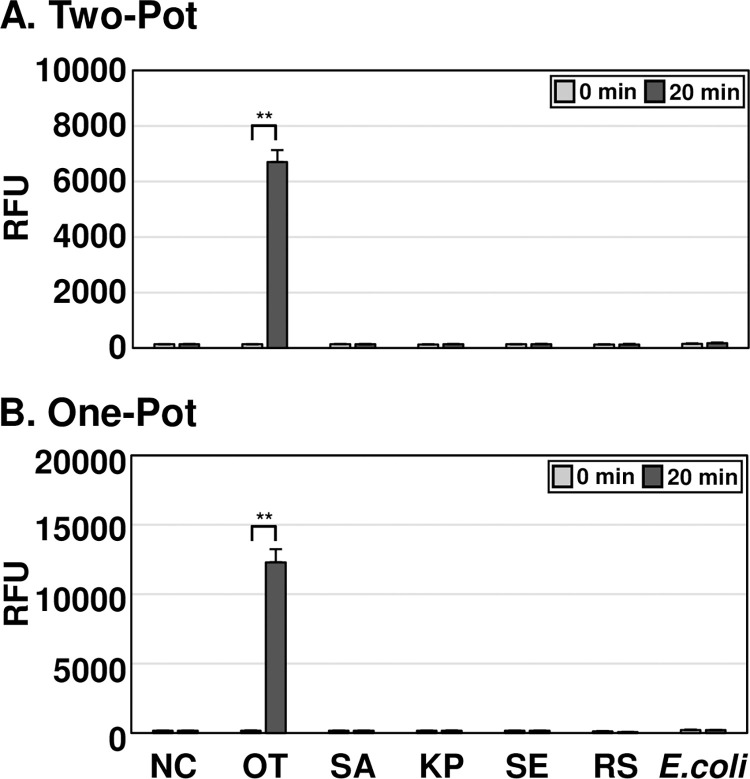
Specificity analysis of OT DETECTR
To determine the specificity of OT DETECTR, it was tested on genomic RNA from O. tsutsugamushi, S. aureus, K. pneumoniae, S. enteritidis, and E. coli, as well as on in vitro transcribed 16S rRNA from Rickettsia spp. (Fig 4). The two-pot and one-pot OT DETECTRs combined with a fluorescence assay both yielded positive results with RNA of O. tsutsugamushi, but not with that of S. aureus, K. pneumoniae, S. enteritidis, E. coli or Rickettsia spp.. Thus, OT DETECTR specifically detected O. tsutsugamushi without cross-reacting with S. aureus, K. pneumoniae, S. enteritidis, E. coli or Rickettsia spp.. The OT DETECTR’s ability to detect various O. tsutsugamushi strains was further evaluated. Both two-pot and one-pot OT DETECTR successfully detected major strains, including Karp, Kuroki, TA763, Gilliam, Kawasaki, Japanese Gilliam, Kato, and Shimokoshi (S2 Fig).
Fig 4. Specificity analyses of OT DETECTRs.
To determine the specificities of OT DETECTRs, 100 ng of RNA from each bacterial species and 105 copies of RNA from Rickettsia spp. were amplified using RT-RPA. The Cas12a trans-cleavage activity assay was subsequently performed, and the results were analyzed through fluorescence measurements. Values are presented as means ± s.d. (error bars) (n = 3 replicates; ** P < 0.01, between samples, two-sample t-test). RFU, relative fluorescence unit; NC, no template control; SA, Staphylococcus aureus; KP, Klebsiella pneumoniae; SE, Salmonella enteritidis; RS, Rickettsia spp.; OT, Orientia tsutsugamushi.
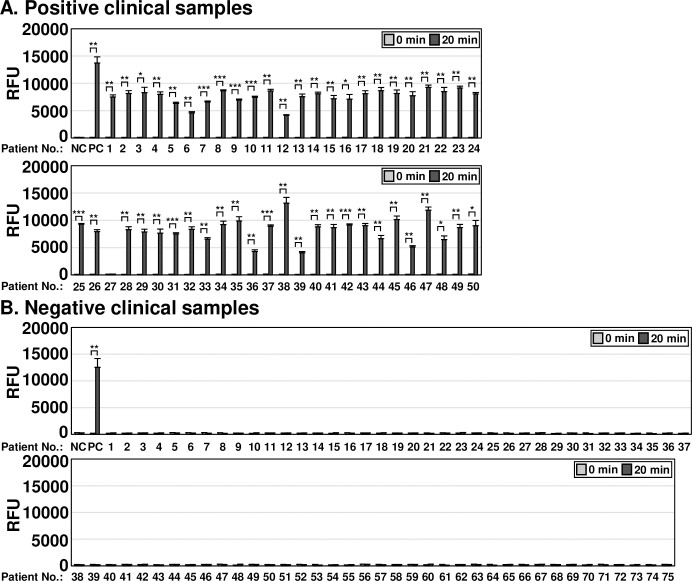
Applicability of OT DETECTR to clinical samples
To evaluate the clinical applicability of the one-pot and two-pot OT DETECTRs, we compared the results obtained from samples of patients confirmed to be infected with O. tsutsugamushi by nested PCR, a commonly used confirmatory method for diagnosing scrub typhus in Korea. A total of 125 clinical samples were evaluated for O. tsutsugamushi infection via nested PCR (S3 Fig). Among them, 50 clinical samples were confirmed to be positive for O. tsutsugamushi infection and 75 were confirmed to be negative (S3 Fig). The two-pot DETECTR combined with fluorescence assay or LFA detected 49 of 50 O. tsutsugamushi infection-positive samples (the long exception was patient #27) (Fig 5A). Similarly, the one-pot DETECTR combined with a fluorescence assay also confirmed infection in all clinical samples positive for O. tsutsugamushi infection except for patient #27 (Fig 6A). Among clinical samples negative for O. tsutsugamushi, the two-pot and one-pot DETECTRs yielded the same results as the nested PCR (Figs 5B and 6B). The application of OT DETECTR to clinical samples and its concordance analysis with nested PCR are summarized in Tables 3 and 4, respectively. Patient demographic and clinical characteristics, including age, gender, immunosuppression status, Charlson Comorbidity Index (CCI), and days since illness onset, are detailed in S2 Table.
Fig 5. Clinical applicability analysis of two-pot OT DETECTR.
Two-pot OT DETECTR was performed on clinical samples from (A) 50 patients confirmed positive or (B) 75 patients confirmed negative for O. tsutsugamushi infection by nested PCR. RNA was extracted from whole blood, RT-RPA was performed, the Cas12a trans-cleavage activity assay was performed, and the results were determined by a fluorescence assay or LFA. Genomic RNA of O. tsutsugamushi (100 ng) was used as a positive control. Values are presented as means ± s.d. (error bars) (n = 3 replicates; *** P < 0.001, ** P < 0.01, * P < 0.05 between samples, two-sample t-test). RFU, relative fluorescence unit; C-line, control line; T-line, test line; NC, no template control; PC, positive control.
Fig 6. Clinical applicability analysis of one-pot OT DETECTR.
One-pot OT DETECTR combined with a fluorescence assay was performed on clinical samples from (A) 50 patients confirmed positive or (B) 75 patients confirmed negative for O. tsutsugamushi infection by nested PCR. Genomic RNA of O. tsutsugamushi (100 ng) was used as a positive control. Values are presented as means ± s.d. (error bars) (n = 3 replicates; *** P < 0.001, ** P < 0.01, * P < 0.05 between samples, two-sample t-test). RFU, relative fluorescence unit; NC, no template control; PC, positive control.
Table 3. Performance of OT DETECTR on clinical samples.
| True positive | False negative | True negative | False positive | Sensitivity (95% CI) |
Specificity (95% CI) |
|
|---|---|---|---|---|---|---|
|
Two-pot
OT DETECTR |
49 | 1 | 75 | 0 |
98%
(89.35%~99.5%) |
100%
(95.2%~100%) |
|
One-pot
OT DETECTR |
49 | 1 | 75 | 0 |
98%
(89.35%~99.5%) |
100%
(95.2%~100%) |
Table 4. Concordance analysis between nested PCR and OT DETECTR for O. tsutsugamushi detection.
| Detection Outcome | Nested PCR positive | Nested PCR negative | Total | Percentage (%) |
|---|---|---|---|---|
| Two-pot OT DETECTR positive | 49 | 0 | 49 | * PPA: 98% |
| Two-pot OT DETECTR negative | 1 | 75 | 76 | ** NPA: 100% |
| Total | 50 | 75 | 125 | |
| One-pot OT DETECTR positive | 49 | 0 | 49 | * PPA: 98% |
| One-pot OT DETECTR negative | 1 | 75 | 76 | ** NPA: 100% |
| Total | 50 | 75 | 125 |
*PPA: positive percent agreement
**NPA: Negative percent agreement
Discussion
In this study, we developed a CRISPR-Cas12a-based diagnostic method for O. tsutsugamushi (OT DETECTR). We targeted the 16S rRNA, which is present in more copies than DNA, offers a stable secondary, and was found to yield a detection sensitivity more than 10 times greater than that for DNA when targeted by OT DETECTR. This enables reliable detection even in environments with low pathogen concentrations. Our method detected all O. tsutsugamushi genotypes with known sequences and exhibited high specificity (100%). The analytical sensitivity of this diagnostic method was 102 RNA copies per reaction, which is approximately 10-fold lower than that of the nested PCR used in conventional diagnostic methods [33]. Although nested PCR amplifies trace amounts of target DNA using two rounds of PCR, it has the disadvantages of requiring additional reaction time and posing a higher risk of contamination. Compared to the long reaction time of 3 hours 45 minutes for nested-PCR, OT DETECTR utilizes isothermal amplification and completes within 1 hour, making it a more suitable diagnostic technology for scrub typhus, where rapid diagnosis is critical.
Meanwhile, in an analysis conducted with blood samples from patients, the OT DETECTR exhibited a clinical sensitivity of 98% (49/50), which was highly consistent with the sensitivity of the nested PCR analysis (98%). The single false-negative sample (positive clinical sample no. 27) had a low purity ratio of absorbance at 260 nm and 280 nm (0.5), compared to other samples with ratios of 1.6 or higher. This suggests that the assay’s performance may be affected by sample quality. Moreover, while nested PCR requires a thermocycler and a reaction time of 3 h 45 min, OT DETECTR can provide results within 1 hour and uses an isothermal reaction. The ability of OT DETECTR to diagnose O. tsutsugamushi infection with high sensitivity and specificity in such a short time without the need for specialized equipment supports its applicability for the rapid diagnosis of scrub typhus to facilitate timely and appropriate treatment.
Beyond comparisons with nested PCR, evaluating OT DETECTR against quantitative methods like qPCR could further enhance its clinical applicability. While qPCR provides quantitative data, such as bacterial load in copies/ml, OT DETECTR focuses on rapid, qualitative detection, offering distinct advantages in resource-limited settings. A direct comparison with qPCR could provide deeper insights into OT DETECTR’s analytical performance and clinical applicability, especially in contexts requiring quantitative measurements. Future studies will include such comparisons to comprehensively assess OT DETECTR’s strengths and limitations.
In the conventional DETECTR protocol, the isothermal nucleic acid amplification and trans-cleavage reaction are conducted in separate tubes at different temperatures. This opens the possibility of sample contamination and/or error during the transfer of reaction materials. To address these issues, we devised a one-pot OT DETECTR. We placed the trans-cleavage reaction mixture at the bottom of an Eppendorf tube, inserted a filter into the tube, and loaded the nucleic acid amplification reaction mixture (i.e., RPA reaction mixture) into the filter. At a single temperature, the amplification step took place on the filter, a brief centrifugation was used to move the amplified product to the bottom of tube, and then the trans-cleavage reaction took place at the bottom of the tube. The devised one-pot DETECTR showed no difference in specificity and sensitivity compared to the conventional two-pot DETECTR, and actually exhibited higher fluorescence values in measuring trans-cleavage activity. This suggests that a one-pot system could perform at least as well as the corresponding two-pot system while potentially preventing contamination and/or errors during the diagnostic process and thereby resolving issues of false negatives. Currently, Inogenix Inc. is evaluating and developing an OT DETECTR-based O. tsutsugamushi diagnostic kit that offers these features. Further studies are warranted to use the diagnostic kit for additional clinical samples and to evaluate its performance in field-based testing.
For the OT DETECTR presented in this study to be used for point-of-care testing (POCT), several technological barriers need to be overcome. First, it must be easy to extract nucleic acids from the blood of suspected patients. To tackle the challenge of nucleic acid extraction in resource-limited settings, we plan to investigate simplified methods, such as heat-based extraction techniques. These approaches aim to streamline sample preparation and improve the test’s practicality in field conditions. Second, it should use a reaction temperature setting that can be achieved using a battery-based device or an air-activated hand warmer. Third, it should involve the sequential progression of isothermal nucleic acid amplification and trans-cleavage reaction using microfluidics or a nanoplatform. Finally, it should use LFA or a mobile device-based technique for measuring fluorescence. If these technologies are developed and integrated, it is expected that a CRISPR-Cas12a-based POCT can be developed for use in low- and middle-income countries (LMICs), as well as in rural and remote areas with fragile healthcare systems.
Recently, Bhardwaj et al. reported a conventional CRISPR-Cas12a-based detection method, combined with LFA, which could detect a single gene copy of the genomic DNA from O. tsutsugamushi Karp and Gilliam strains [34]. Since LFA has the drawback of displaying a positive band depending on reaction time [35], further studies are required to verify these findings using quantitative methods, such as fluorescence assays.
Several studies have reported that a CRISPR-Cas13a-based assay can detect RNA without nucleic acid amplification [36, 37]. Therefore, we also tested a CRISPR-Cas13a-based assay with OT1 gRNA on a subset of clinical samples confirmed positive for O. tsutsugamushi infection. However, we failed to obtain any results (S4 Fig). We further used the two gRNAs (OT1 and OT2) for a CRISPR-Cas13a-based assay because the sensitivity of the assay was reported to be enhanced by the use of multiple primers [37]. However, despite many attempts, we were unable to replicate the previously reported success with Cas13a (S4 Fig).
Supporting information
Sequence alignment of the (A) RPA primers and (B) gRNAs used in this study, relative to the different genotypes of O. tsutsugamushi. Sequences of OT1-R and OT2-R are shown in the reverse-complement orientation.
(TIF)
The in vitro transcribed RNA fragments from the 16S rRNA sequences of major O. tsutsugamushi strains (Karp, Kuroki, TA763, Gilliam, Kawasaki, Japanese Gilliam, Kato, and Shimokoshi) were used to evalulate (A) Two-pot DETECTR and (B) One-pot DETECTR. Values are presented as means ± s.d. (error bars) (n = 3 replicates; *** P < 0.001, ** P < 0.01, * P < 0.05 between samples, two-sample t-test). RFU, relative fluorescence unit; NC, no template control.
(TIF)
Nested PCR was performed to assess O. tsutsugamushi infection in 125 clinical samples from patients believed to be positive or negative for infection, and the product (483 bp) was visualized via gel electrophoresis. Of the total 125 samples, (A) 50 samples were confirmed positive for O. tsutsugamushi infection, and (B) 75 samples were confirmed negative for O. tsutsugamushi infection.
(TIF)
Clinical samples from 10 patients with confirmed O. tsutsugamushi infection were analyzed using OT DETECTR with (A) Cas13a-OT1 gRNA or (B) multiple gRNAs (Cas13a-OT1 and Cas13a-OT2). Values are presented as means ± s.d. (error bars) (n = 3 replicates; * p < 0.05 between samples, two-sample t-test). RFU, relative fluorescence unit; NC, no template control; PC, Positive control (in vitro transcribed O. tsutsugamushi 16S rRNA)
(TIF)
(DOCX)
(DOCX)
(DOCX)
Data Availability
The manuscript provides patient demographics and clinical characteristics, such as age, gender, immunosuppression status, Charlson Comorbidity Index (CCI), and days since illness onset. Beyond this information, the disclosure of raw clinical data (including personal details) to third parties without prior consent from the data subjects is prohibited by law. For inquiries regarding the raw clinical data, please contact Jeju National University Hospital Institutional Review Board (irb1503@jejunuh.co.kr). The utilized primer sets, designed to detect the OT1 and OT2 sequences (Table 1), were designed according to the provided protocol, with reference to the aligned 16S rRNA sequence for nine genotypes of O. tsutsugamushi (S1 Fig): Karp, Kuroki, TA763, Gilliam, Kawasaki, Japanese Gilliam, Kato, and Shimokoshi (GenBank accession numbers: NR_025860.1, D38626.1, NZ_OUNA00000000.1, D38622.1, D38625.1, AP008981.1, NZ_LS398550.1, D38627.1, respectively; NCBI). The Saitama strain was excluded because it was not published in NCBI.
Funding Statement
This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HI22C0286). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Taylor AJ, Paris DH, Newton PN. A systematic review of mortality from untreated scrub typhus (Orientia tsutsugamushi). PLoS neglected tropical diseases. 2015;9(8):e0003971. doi: 10.1371/journal.pntd.0003971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li W, Huang L, Zhang W. Scrub typhus with multi-organ dysfunction syndrome and immune thrombocytopenia: a case report and review of the literature. Journal of Medical Case Reports. 2019;13(1):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ono Y, Ikegami Y, Tasaki K, Abe M, Tase C. Case of scrub typhus complicated by severe disseminated intravascular coagulation and death. Emergency Medicine Australasia. 2012;24(5):577–80. doi: 10.1111/j.1742-6723.2012.01600.x [DOI] [PubMed] [Google Scholar]
- 4.Sankhyan N, Saptharishi L, Sasidaran K, Kanga A, Singhi SC. Clinical profile of scrub typhus in children and its association with hemophagocytic lymphohistiocytosis. Indian pediatrics. 2014;51:651–3. doi: 10.1007/s13312-014-0470-4 [DOI] [PubMed] [Google Scholar]
- 5.Kim Y-S, Lee HJ, Chang M, Son SK, Rhee YE, Shim SK. Scrub typhus during pregnancy and its treatment: a case series and review of the literature. The American journal of tropical medicine and hygiene. 2006;75(5):955–9. [PubMed] [Google Scholar]
- 6.Phimda K, Hoontrakul S, Suttinont C, Chareonwat S, Losuwanaluk K, Chueasuwanchai S, et al. Doxycycline versus azithromycin for treatment of leptospirosis and scrub typhus. Antimicrobial agents and chemotherapy. 2007;51(9):3259–63. doi: 10.1128/AAC.00508-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walker DH, Mendell NL. A scrub typhus vaccine presents a challenging unmet need. npj Vaccines. 2023;8(1):11. doi: 10.1038/s41541-023-00605-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blacksell SD, Bryant NJ, Paris DH, Doust JA, Sakoda Y, Day NP. Scrub typhus serologic testing with the indirect immunofluorescence method as a diagnostic gold standard: a lack of consensus leads to a lot of confusion. Clinical infectious diseases. 2007;44(3):391–401. doi: 10.1086/510585 [DOI] [PubMed] [Google Scholar]
- 9.Jiang J, Chan T-C, Temenak JJ, Dasch GA, Ching W-M, Richards AL. Development of a quantitative real-time polymerase chain reaction assay specific for Orientia tsutsugamushi. American Journal of Tropical Medicine and Hygiene. 2004;70(4):351. [PubMed] [Google Scholar]
- 10.Kim D, Lee Y-M, Back J-H, Yang T, Lee J, Song H-J, et al. A serosurvey of Orientia tsutsugamushi from patients with scrub typhus. Clinical Microbiology and Infection. 2010;16(5):447–51. doi: 10.1111/j.1469-0691.2009.02865.x [DOI] [PubMed] [Google Scholar]
- 11.Lee Y-M, Kim D-M, Lee S-H, Jang M-S, Neupane GP. Phylogenetic analysis of the 56 kDa protein genes of Orientia tsutsugamushi in southwest area of Korea. The American journal of tropical medicine and hygiene. 2011;84(2):250. doi: 10.4269/ajtmh.2011.09-0601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Urakami H, Tsuruhara T, Tamura A. Penetration of Rickettsia tsutsugamushi into cultured mouse fibroblasts (L cells): an electron microscopic observation. Microbiology and immunology. 1983;27(3):251–63. doi: 10.1111/j.1348-0421.1983.tb03587.x [DOI] [PubMed] [Google Scholar]
- 13.Fdr Gouriet, Fenollar F, Patrice J-Y, Drancourt M, Raoult D. Use of shell-vial cell culture assay for isolation of bacteria from clinical specimens: 13 years of experience. Journal of clinical microbiology. 2005;43(10):4993–5002. doi: 10.1128/JCM.43.10.4993-5002.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ha N-Y, Kim Y, Choi J-H, Choi M-S, Kim I-S, Kim Y-S, et al. Detection of antibodies against Orientia tsutsugamushi Sca proteins in scrub typhus patients and genetic variation of sca genes of different strains. Clinical and Vaccine Immunology. 2012;19(9):1442–51. doi: 10.1128/CVI.00285-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Luce-Fedrow A, Lehman ML, Kelly DJ, Mullins K, Maina AN, Stewart RL, et al. A review of scrub typhus (Orientia tsutsugamushi and related organisms): then, now, and tomorrow. Tropical medicine and infectious disease. 2018;3(1):8. doi: 10.3390/tropicalmed3010008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moron CG, Popov VL, Feng H-M, Wear D, Walker DH. Identification of the target cells of Orientia tsutsugamushi in human cases of scrub typhus. Modern Pathology. 2001;14(8):752–9. doi: 10.1038/modpathol.3880385 [DOI] [PubMed] [Google Scholar]
- 17.Ohashi N, Fukuhara M, Shimada M, Tamura A. Phylogenetic position of Rickettsia tsutsugamushi and the relationship among its antigenic variants by analyses of 16S rRNA gene sequences. FEMS microbiology letters. 1995;125(2–3):299–304. doi: 10.1111/j.1574-6968.1995.tb07372.x [DOI] [PubMed] [Google Scholar]
- 18.Tamura A, Ohashi N, Urakami H, Miyamura S. Classification of Rickettsia tsutsugamushi in a new genus, Orientia gen. nov., as Orientia tsutsugamushi comb. nov. International Journal of Systematic and Evolutionary Microbiology. 1995;45(3):589–91. [DOI] [PubMed] [Google Scholar]
- 19.Tamura A, Ohashi N, Urakami H, Takahashi K, Oyanagi M. Analysis of polypeptide composition and antigenic components of Rickettsia tsutsugamushi by polyacrylamide gel electrophoresis and immunoblotting. Infection and immunity. 1985;48(3):671–5. doi: 10.1128/iai.48.3.671-675.1985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stover C, Marana D, Carter J, Roe B, Mardis E, Oaks E. The 56-kilodalton major protein antigen of Rickettsia tsutsugamushi: molecular cloning and sequence analysis of the sta56 gene and precise identification of a strain-specific epitope. Infection and immunity. 1990;58(7):2076–84. doi: 10.1128/iai.58.7.2076-2084.1990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.SHISHIDO A. Strain variation of Rickettsia orientalis in the complement fixation test. Japanese Journal of Medical Science and Biology. 1964;17(2–3):59–72. doi: 10.7883/yoken1952.17.59 [DOI] [PubMed] [Google Scholar]
- 22.Shishido A. Identification and serological classification of the causative agent of scrub typhus in Japan. Jpn J Sci Biol. 1962;15:308–21. [Google Scholar]
- 23.Kelly DJ, Fuerst PA, Ching W-M, Richards AL. Scrub typhus: the geographic distribution of phenotypic and genotypic variants of Orientia tsutsugamushi. Clinical infectious diseases. 2009;48(Supplement_3):S203–S30. doi: 10.1086/596576 [DOI] [PubMed] [Google Scholar]
- 24.Chen JS, Ma E, Harrington LB, Da Costa M, Tian X, Palefsky JM, et al. CRISPR-Cas12a target binding unleashes indiscriminate single-stranded DNase activity. Science. 2018;360(6387):436–9. Epub 20180215. doi: 10.1126/science.aar6245 ; PubMed Central PMCID: PMC6628903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gootenberg JS, Abudayyeh OO, Kellner MJ, Joung J, Collins JJ, Zhang F. Multiplexed and portable nucleic acid detection platform with Cas13, Cas12a, and Csm6. Science. 2018;360(6387):439–44. Epub 20180215. doi: 10.1126/science.aaq0179 ; PubMed Central PMCID: PMC5961727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Myhrvold C, Freije CA, Gootenberg JS, Abudayyeh OO, Metsky HC, Durbin AF, et al. Field-deployable viral diagnostics using CRISPR-Cas13. Science. 2018;360(6387):444–8. doi: 10.1126/science.aas8836 ; PubMed Central PMCID: PMC6197056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Broughton JP, Deng X, Yu G, Fasching CL, Servellita V, Singh J, et al. CRISPR-Cas12-based detection of SARS-CoV-2. Nat Biotechnol. 2020;38(7):870–4. Epub 20200416. doi: 10.1038/s41587-020-0513-4 ; PubMed Central PMCID: PMC9107629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Park BJ, Yoo JR, Heo ST, Kim M, Lee KH, Song YJ. A CRISPR-Cas12a-based diagnostic method for multiple genotypes of severe fever with thrombocytopenia syndrome virus. PLoS Negl Trop Dis. 2022;16(8):e0010666. Epub 20220802. doi: 10.1371/journal.pntd.0010666 ; PubMed Central PMCID: PMC9345333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stoddard SF, Smith BJ, Hein R, Roller BR, Schmidt TM. rrn DB: improved tools for interpreting rRNA gene abundance in bacteria and archaea and a new foundation for future development. Nucleic acids research. 2015;43(D1):D593–D8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cho BA, Cho NH, Min CK, Kim SY, Yang JS, Lee JR, et al. Global gene expression profile of Orientia tsutsugamushi. Proteomics. 2010;10(8):1699–715. doi: 10.1002/pmic.200900633 [DOI] [PubMed] [Google Scholar]
- 31.Kim G, Ha N-Y, Min C-K, Kim H-I, Yen NTH, Lee K-H, et al. Diversification of Orientia tsutsugamushi genotypes by intragenic recombination and their potential expansion in endemic areas. PLoS neglected tropical diseases. 2017;11(3):e0005408. doi: 10.1371/journal.pntd.0005408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kim CG, Kim WK, Kim N, Pyung YJ, Park D-J, Lee J-C, et al. Intranasal immunization with nanoparticles containing an Orientia tsutsugamushi protein vaccine candidate and a polysorbitol transporter adjuvant enhances both humoral and cellular immune responses. Immune Network. 2023;23(6). doi: 10.4110/in.2023.23.e47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim D-M, Park G, Kim HS, Lee JY, Neupane GP, Graves S, et al. Comparison of conventional, nested, and real-time quantitative PCR for diagnosis of scrub typhus. Journal of clinical microbiology. 2011;49(2):607–12. doi: 10.1128/JCM.01216-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bhardwaj P, Nanaware NS, Behera SP, Kulkarni S, Deval H, Kumar R, et al. CRISPR/Cas12a-Based Detection Platform for Early and Rapid Diagnosis of Scrub Typhus. Biosensors (Basel). 2023;13(12). Epub 20231208. doi: 10.3390/bios13121021 ; PubMed Central PMCID: PMC10742217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Park BJ, Park MS, Lee JM, Song YJ. Specific Detection of Influenza A and B Viruses by CRISPR-Cas12a-Based Assay. Biosensors (Basel). 2021;11(3). Epub 20210319. doi: 10.3390/bios11030088 ; PubMed Central PMCID: PMC8003587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fozouni P, Son S, Diaz de Leon Derby M, Knott GJ, Gray CN, D’Ambrosio MV, et al. Amplification-free detection of SARS-CoV-2 with CRISPR-Cas13a and mobile phone microscopy. Cell. 2021;184(2):323–33 e9. Epub 20201204. doi: 10.1016/j.cell.2020.12.001 ; PubMed Central PMCID: PMC7834310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shinoda H, Taguchi Y, Nakagawa R, Makino A, Okazaki S, Nakano M, et al. Amplification-free RNA detection with CRISPR–Cas13. Communications biology. 2021;4(1):476. doi: 10.1038/s42003-021-02001-8 [DOI] [PMC free article] [PubMed] [Google Scholar]