Abstract
This study aims to compare the clinical efficacy of arthroscopically assisted treatment versus traditional open reduction for Schatzker type III posterolateral tibial plateau collapse fractures. We retrospectively analyzed clinical data from 40 patients with Schatzker type III fractures (lateral plateau collapse) treated at our hospital between October 2020 and March 2024. Patients were divided into two groups: the arthroscopy group (n = 19) and the open incision group (n = 21). General patient information, hospitalization costs, length of stay, and wound length were collected. All patients were followed for one year postoperatively, with knee function assessed using the Lysholm score. Categorical data were analyzed using the chi-square test, and continuous variables using independent sample t-tests. A p-value < 0.05 was considered statistically significant. There were no significant differences in baseline characteristics between the two groups. The arthroscopy group had significantly shorter operation times and postoperative hospital stays compared to the open incision group (p < 0.05). Additionally, surgical costs were significantly lower in the arthroscopy group (p < 0.05). At 3 months postoperatively, the arthroscopy group demonstrated significantly higher Lysholm scores compared to the open incision group. However, there was no significant difference in Lysholm scores between the two groups at the 6 months and 1-year follow-up (p > 0.05). Compared to traditional open reduction and internal fixation, arthroscopic treatment of Schatzker type III posterolateral tibial plateau collapse fractures offers several advantages, including shorter operative time, lower cost, fewer incision-related complications, no need for secondary removal of internal fixation, faster postoperative functional recovery, and minimally invasive, cosmetically favorable incisions.
Keywords: Schatzker III type, Posterolateral collapse, Tibial plateau fracture, Knee arthroscopy
Subject terms: Medical research, Bone
Introduction
Tibial plateau fractures are a common type of intra-articular injury, accounting for approximately 1% of all fractures and 8% of fractures among the elderly1. These injuries can result from high-energy trauma—typically caused by motor vehicle accidents, falls, or sports injuries—as well as low-energy trauma, such as pathological fractures in elderly patients with osteoporosis2. The most widely used classification system for tibial plateau fractures in clinical practice is the Schatzker classification, originally proposed and later refined by Schatzker3.This study focuses on posterolateral plateau collapse fractures, a specific subtype of Schatzker type III fractures. Due to their unique anatomical location, these fractures are often easily overlooked. Failure to timely restore the height of the lateral plateau can alter the mechanical alignment of the knee joint, potentially leading to post-traumatic osteoarthritis, impaired knee function, and a decline in overall quality of life.
Lateral tibial plateau fractures present a significant challenge for orthopedic surgeons4. The annual incidence of Schatzker type III posterolateral plateau fractures is approximately 10.3 cases per 100,000 people5, and there remains ongoing debate regarding the optimal method of fixation. Surgical treatment options are highly varied and continue to evolve6–8. The most traditional approach is open reduction and internal fixation (ORIF), which typically involves the use of plates or screws in combination with bone grafting—either autologous cancellous bone or synthetic substitutes9–11. The primary goals of surgical intervention are to restore knee stability, re-establish the height of the lateral plateau12, and recover joint function. The conventional surgical technique utilizes classic anterior and posterior approaches13, which are often highly invasive and can cause substantial trauma to the surrounding soft tissue. These procedures require dissection and mobilization of the common peroneal nerve and may even necessitate fibular head osteotomy to achieve adequate visualization of the fracture site. However, despite these measures, it remains difficult to fully expose the posterolateral plateau, complicating the process of fracture reduction and stabilization.
Given the anatomical complexity of the posterolateral region—with its vulnerable nerves, blood vessels, and connective tissue structures14—fracture reduction and fixation in this area is especially demanding. Research has demonstrated that each millimeter of joint surface depression can result in a 2° increase in limb varus alignment. As mechanical loading increases, this varus deformity can worsen, ultimately elevating the risk of post-traumatic osteoarthritis15.
In recent years, advancements in science and technology have driven a growing preference for minimally invasive procedures and early functional rehabilitation. Arthroscopic minimally invasive techniques have become increasingly refined and widely adopted in joint surgery, gradually emerging as the standard of care. In particular, arthroscopy offers significant advantages in managing complex posterolateral tibial plateau depression fractures by avoiding many of the limitations and risks associated with open surgery. Arthroscopy allows for enhanced visualization of the articular surface and facilitates more precise reduction of the collapsed fracture site under direct vision16–18, thereby effectively restoring the height of the tibial plateau.
In this study, we retrospectively analyzed 40 cases of posterolateral tibial plateau collapse fractures treated at our hospital between October 2020 and March 2024. Patients were divided into two groups: an arthroscopically assisted treatment group and a traditional open incision group. The goal was to evaluate and compare the clinical effectiveness and economic value of arthroscopically assisted treatment for this specific fracture type.
Materials and methods
General information
A total of 40 patients with Schatzker type III fractures (lateral tibial plateau collapse) who were hospitalized at our institution between October 2020 and March 2024 were included in this study. All patients underwent preoperative imaging, including knee X-ray, computed tomography (CT), and magnetic resonance imaging (MRI), to confirm the diagnosis and evaluate fracture characteristics. Inclusion criteria: (1) Patients aged over 18 years with closed epiphyseal plates; (2) A confirmed diagnosis of Schatzker type III fracture (isolated lateral tibial plateau collapse); (3) No associated open injuries; (4) T Willingness to undergo surgical treatment and provide informed consent. Exclusion criteria: (1) Fractures involving other structures around the knee joint (e.g., femur, patella), or presence of vascular or nerve injury; (2) Patients lost to follow-up or with follow-up duration of less than 3 months; (3) Concomitant injury to the anterior or posterior cruciate ligament, or the medial collateral ligament; (4) Severe systemic disease, inability to perform activities of daily living, or pre-injury inability to walk independently.
All surgical procedures in this study were performed by the same surgical team, with each operation involving at least one senior, experienced orthopedic surgeon. Imaging evaluations were conducted by a team consisting of a radiologist and an orthopedic surgeon to ensure accuracy and consistency. The follow-up assessments were carried out by a multidisciplinary team that included an orthopedic surgeon, a rehabilitation physician, and a nurse. This study was approved by the Ethics Committee of Nanyang Hospital of Traditional Chinese Medicine (Nanyang Orthopedic Hospital; Approval No. KJGG123). As a retrospective study involving no additional interventions, the requirement for individual informed consent was waived. However, all patients had previously signed informed consent forms at the time of their initial treatment.A power analysis was conducted using a two-independent-sample t-test to estimate the required sample size. The Lysholm scores of a subset of patients at the 3-month follow-up were used as the primary outcome measure. With a significance level of α = 0.05 and power (1 − β) = 0.90, the results indicated that a minimum of 7 patients per group (14 total) would be sufficient to achieve statistical power greater than 0.90.
All methods used in this study were performed in accordance with the Declaration of Helsinki.
Pre-treatment evaluation
All patients underwent imaging evaluations prior to surgery and were diagnosed with Schatzker type III tibial plateau fractures (isolated lateral tibial plateau collapse). Preoperative management included administration of analgesics and anticoagulants, along with active surgical preparation. Patients were also instructed to perform daily ankle pump exercises and quadriceps isometric contractions to help prevent lower limb venous thrombosis and muscle disuse atrophy.
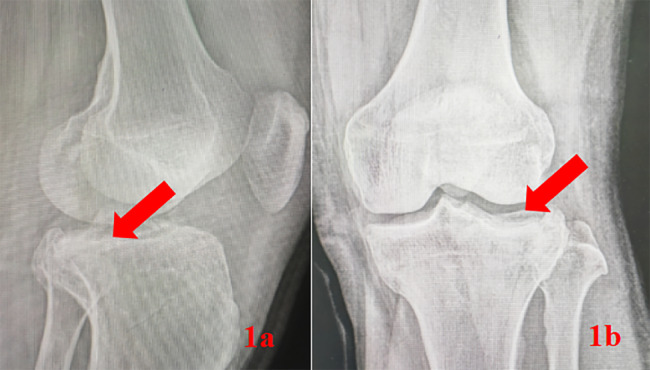
Following an intra-articular knee fracture, patients often experience joint swelling, hemarthrosis, and impaired mobility. The knee is typically held in a passive position, making it difficult to perform an accurate functional assessment using standardized scoring systems. Therefore, in this study, fracture displacement was evaluated using standard anteroposterior and lateral knee X-rays (Fig. 1a and b). In addition, a complete three-dimensional CT scan was performed for each patient to obtain a more detailed characterization of the fracture morphology (Fig. 2a and c), which was essential for guiding the surgical treatment plan.
Fig. 1.
(a) The lateral X-ray view, with the red arrow indicating the collapse of the tibial plateau. The arrow in (b) highlights the collapse of the lateral plateau fracture.
Fig. 2.
(a), (b) and (c) Present findings from CT three-dimensional reconstruction. The red arrow marks the collapse of the tibial plateau. Intra-articular fractures require further CT three-dimensional reconstruction to clarify the fracture type and guide treatment planning.
Surgical method
Arthroscopic bone bar fixation group
A conventional knee arthroscopy approach is established through an anterolateral and anteromedial entry. The arthroscopic power system is used to clear blood accumulation in the suprapatellar bursa, synovium, and infrapatellar fat pad, which obstructs the field of vision. A meniscus retractor is then employed to expose the collapsed joint surface under arthroscopic guidance.
A 2 cm incision is made on the lateral side of the proximal tibia, and the anterior cruciate ligament (ACL) positioning device is used to locate the depression on the lateral plateau. A 2.0 mm Kirschner wire is inserted, and a homemade hollow push rod is utilized to lift the collapsed part of the joint surface along the wire, all under arthroscopic visualization.
A conventional push rod is then used to further elevate the joint surface along the bone tunnel. Next, a bent bone graft push rod is employed to push the collapsed bone fragments back into place. Small blows are used gradually while constantly adjusting the direction to reposition the bone fragments, with the goal of achieving a flat joint surface.
An 8 mm hollow drill is then used to create a bone tunnel, through which bone grafting (artificial bone) is performed to support the collapsed joint surface (Figs. 3a and b and 4a, b and c). The artificial bone is implanted along the tunnel, using polylactic acid hydroxyapatite bone strips (Fig. 5a).
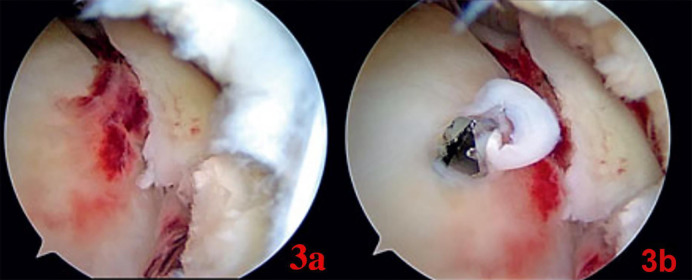
Fig. 3.
(a) Shows intraoperative arthroscopic findings, where the lateral platform has collapsed significantly, forming a step-off with the surrounding area. (b) Shows the Kirschner wire used to locate the collapsed fracture under the guidance of the locator.
Fig. 4.
(a) Presents an intraoperative arthroscopic view after the collapsed lateral platform has been lifted, showing the restored tibial plateau height. (b) and (c) Show the postoperative appearance, with the fracture lifted along the Kirschner wire. The Kirschner wires are inserted one by one, the skin is cut along the wires, and a push rod is used to elevate the collapsed tibial platform.
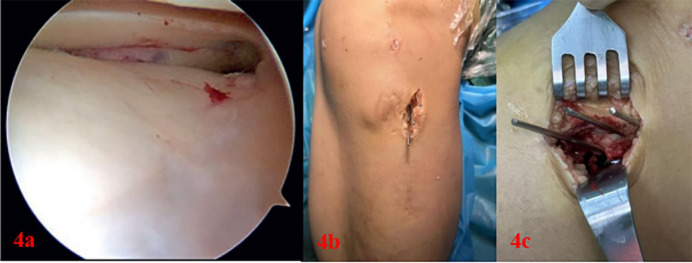
Fig. 5.
(a) and (b) show the completion of the procedure after artificial bone strips are inserted, and the wound is sutured. The technique is minimally invasive and aesthetically pleasing.
⑤During the procedure, reduction is reassessed under direct visualization, and the height of the lateral plateau is restored. The joint surface is flattened using a probe hook, ensuring that the fracture remains stable, with no need for fluoroscopy. The wound is closed with cosmetic sutures, requiring no stitches (Fig. 5b).
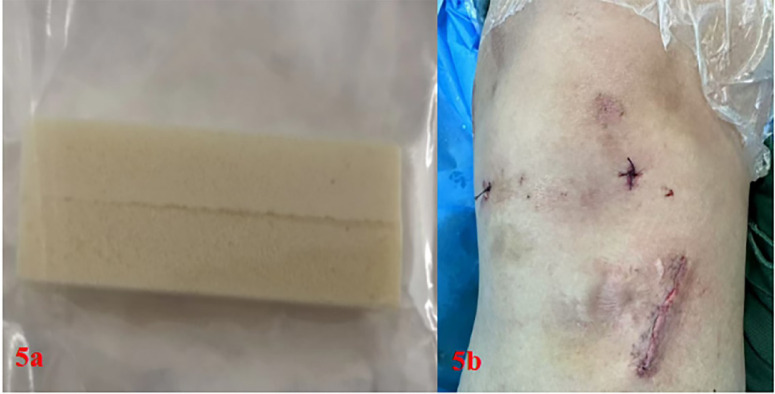
Postoperative CT and X-ray examinations confirm complete recovery of the collapsed fracture surface, demonstrating excellent results (Figs. 6a, b, c and d and 7).
Fig. 6.
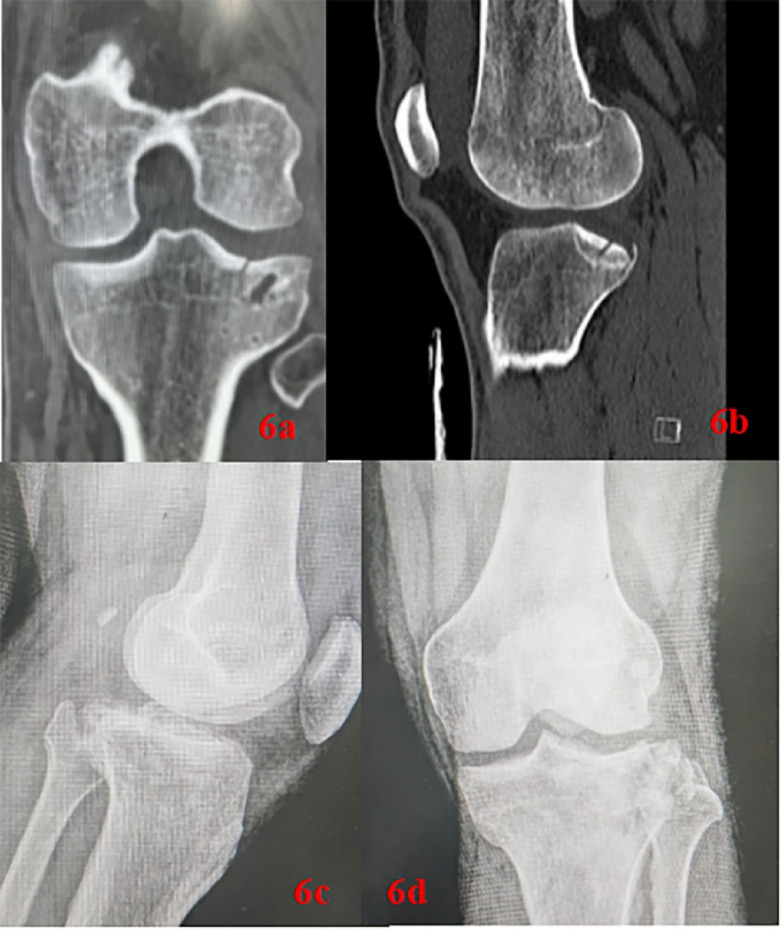
Postoperative CT and X-ray reexaminations (a–d) show that the collapsed fracture surface has fully healed with good results.
Fig. 7.

X-rays 6 months after surgery.
Open reduction and internal fixation group
An anterolateral submeniscal approach, approximately 12 cm in length, was used to expose the lateral tibial plateau fracture. The joint capsule was incised transversely below the lateral meniscus, which was then gently lifted upward, allowing direct visualization of the collapsed joint surface.
To access the bone cortex, an electric drill was used to open it 2 to 3 cm below the lateral plateau surface. The bone block was reduced using rod-assisted reduction forceps and secured in place with Kirschner wires. During the procedure, a C-arm X-ray machine was employed to assess the reduction of the joint surface, and if satisfactory, a locking plate was used for fixation.
Once the joint was stabilized, artificial bone was implanted into the bone tunnel, and the area was thoroughly irrigated. The meniscus and joint capsule were sutured, followed by closure of the incision.
Rehabilitation
All patients followed a standardized postoperative rehabilitation program. Passive knee motion was initiated on the 5th day after surgery, with flexion progressing up to 90° (performed every other day). Active knee motion began 2 weeks after surgery for both groups and was gradually increased over the first 8 weeks. Full weight-bearing was permitted starting 6 weeks post-surgery, depending on the radiographic healing of the fracture and the patient’s pain levels.
Postoperative follow-up observation and clinical evaluation
The patients were re-examined at 1, 2, 3, 6, and 12 months after surgery. Fracture healing was assessed using X-ray or CT three-dimensional reconstruction, and changes in knee joint angles were recorded at each visit. The Lysholm score was used to objectively evaluate the patients’ recovery at 3 months,6 months and 1 year post-surgery. Patients in the open group underwent a second surgery to remove the internal fixation plate 1 year after the final follow-up.
Statistical methods
The data collected in the study were analyzed using SPSS 26.0 software, and graphs were created using GraphPad Prism 8 software. Measurement data are presented as mean ± standard deviation and were analyzed using a t-test. Categorical data were analyzed using the chi-square test. Differences were considered statistically significant when P < 0.05.
Results
There was no significant difference in the general information of all patients (Table 1). The general data of the two patient groups showed no statistically significant differences. The arthroscopy group had significantly better results in terms of operation time [(83.05 ± 8.92) min vs. (102.19 ± 7.99) min], postoperative hospitalization time [(10.89 ± 0.98) days vs. (16.23 ± 2.04) days], and surgical cost [(1355.18 ± 28.19) $ vs. (1819.10 ± 72.28) $] compared to the incision group (P < 0.05).Follow-up results showed that, The Lysholm score of the arthroscopic group was significantly higher than that of the open group at 3 months post-surgery [(94.07 ± 2.71) vs. (90.37 ± 5.41)]. However, there was no statistically significant difference in the Lysholm score between the two groups at 6 months post-surgery [(96.16 ± 2.03) vs. (94.95 ± 2.64)] (P > 0.05). Similarly, at 1 year post-surgery, the Lysholm score showed no significant difference between the arthroscopic group and the open group [(97.31 ± 1.71) vs. (96.31 ± 2.44)] (P > 0.05). There were no instances of incision infections in either group. However, 5 cases of wound redness and swelling occurred in the incision group, which showed no statistically significant difference (P > 0.05) (Table 2).
Table 1.
Comparison of general data between the two groups of patients.
| Arthroscopy group | Open surgery group | P | |
|---|---|---|---|
| Age(year) | 46.21 ± 6.23 | 66.05 ± 7.44 | 0.944 |
| Weight(kg) | 46.05 ± 8.09 | 64.38 ± 11.36 | 0.59 |
| Gender (Male/Female) | 12/7 | 13/8 | 0.935 |
| Side (left/right) | 10/9 | 10/11 | 0.752 |
Table 2.
Comparison of intraoperative and postoperative conditions between the two groups.
| Arthroscopy group | Open surgery group | P | |
|---|---|---|---|
| Length of hospital stay(day) | 10.89 ± 0.98 | 16.23 ± 2.04 | < 0.001 |
| Operation time(min) | 83.05 ± 8.92 | 102.19 ± 7.99 | < 0.001 |
| Cost of surgery ($) | 1355.18 ± 28.19 | 1819.10 ± 72.28 | < 0.001 |
| Wound length(cm) | 10.11 ± 1.18 | 14.05 ± 1.63 | < 0.001 |
| Wound Infection(n) | 0 | 0 | 1 |
| Wound Redness and Swelling(n) | 0 | 5 | 0.023 |
| Lysholm 3 months after surgery | 94.07 ± 2.71 | 90.37 ± 5.41 | < 0.001 |
| Lysholm 6 months after surgery | 96.16 ± 2.03 | 94.95 ± 2.64 | 0.12 |
| Lysholm 1 year after surgery | 97.31 ± 1.71 | 96.31 ± 2.44 | 0.12 |
Discussion
The tibial plateau is a crucial weight-bearing surface of the human body. A Schatzker type III fracture19, which involves the collapse of the posterolateral plateau, affects the joint surface. If not reduced and fixed promptly, this fracture can lead to instability in knee flexion, altering the knee’s force distribution. This can progressively worsen knee varus, eventually resulting in severe osteoarthritis and functional impairment, which significantly impacts the patient’s quality of life.The primary goal of surgical treatment is to achieve anatomical reduction, restore the joint surface height, provide stable fixation, and appropriately address any associated intra-articular injuries20. Early functional rehabilitation is crucial to minimize the risk of knee stiffness, instability, and post-traumatic osteoarthritis. Therefore, active surgical intervention is of great importance.
Traditionally, internal fixation has been performed via the classic anterolateral approach. However, this method has limitations, primarily due to poor exposure of the surgical field. The distribution of blood vessels and nerves in the posterolateral approach is particularly complex, as the popliteal artery, vein, and common peroneal nerve all run through this area21. Moreover, the posterolateral plateau fracture is often located deeply, making it difficult to visualize the fracture. Even when exposure is possible, effective fixation is hindered by obstruction from the fibular head and the common peroneal nerve. In some cases, fibular osteotomy is required. Any damage to the common peroneal nerve or the posterolateral complex can lead to severe complications, impairing knee joint function and affecting the patient’s quality of life.Therefore, it is essential to explore surgical methods that are minimally invasive yet offer effective reduction and fixation.
In recent years, with the continuous advancement of arthroscopic surgery, it has become widely used in the treatment of intra-articular fractures. Arthroscopic-assisted treatment of intra-articular fractures dates back to the 1980s. This approach offers several benefits, including better visualization, endoscopic reduction, stable internal fixation, less damage to bones and soft tissues, fewer complications, and faster recovery of knee function for patients.Andrew et al.22. used arthroscopic-assisted treatment for posterolateral tibial plateau collapse fractures and achieved more satisfactory results compared to traditional open surgery23–25. They also demonstrated that arthroscopic assistance aids in fracture reduction, provides clear observation of the reduction process, avoids excessive support, and leads to a shorter recovery time with fewer complications26–30. These findings are consistent with our study.
We compared the postoperative outcomes of patients with Schatzker III posterolateral tibial plateau collapse fractures treated with arthroscopic-assisted artificial bone grafting and internal fixation to those treated with traditional open reduction and internal fixation techniques31,32,17,33,34. Functional outcomes were evaluated between 3 months and 1 year post-surgery. The results showed that, at the 3-month follow-up, the Lysholm score for the arthroscopy group was significantly higher than that of the traditional open reduction and internal fixation group. This preliminary evidence suggests that arthroscopically assisted tibial arthroplasty may offer better functional results for type III fractures in the short term. However, there was no significant difference in knee joint scores between the two groups 6-month and 1-year after surgery (P > 0.05). In terms of long-term outcomes, both reduction techniques appear to yield satisfactory results.
In recent years, with the continuous advancement of internal fixation materials35–37, the use of bioartificial bone for support and fixation in the reduction of fracture fragments has become more common for this type of fracture. This approach helps avoid the damage to articular cartilage typically caused by titanium or steel implants, which are commonly used for tibial plateau fracture fixation, and eliminates the risk of implant-related skin irritation. In this article, we employ arthroscopic fracture reduction and artificial bone grafting for internal fixation38,39. The artificial bone provides support, and importantly, no fluoroscopy is required during the procedure, nor does it necessitate secondary removal of the implant post-surgery. Additionally, non-metallic materials do not interfere with security checks or imaging examinations, such as MRIs, in routine life.Similarly, Lubowit40 et al. described a similar technique using absorbable screw fixation, which yielded good results. Krzysztof Hermanowicz41 et al. used additional intervention screws to support and stabilize the posterolateral platform. Furthermore, Hakukawa42 et al. introduced a tibial balloon plasty technique combined with arthroscopy to treat this type of fracture, offering a novel approach.
In general, this surgical method has many advantages, including: (1) Enhanced intra-articular visualization: The arthroscope provides a clear view of the joint, allowing the surgeon to assess the damage to various structures of the joint and prevent complications that may arise from the limitations of direct visual inspection; (2) Ensured joint surface flatness: During the procedure, the arthroscope allows direct visualization of the joint surface, ensuring its proper alignment. Surgical instruments, such as probes, can assist in reducing bone fragments effectively. (3) Thorough removal of blood clots and bone fragments: Endoscopic irrigation allows for the complete removal of blood clots and bone fragments, preventing bone tissue from being exposed to air during open surgery and reducing the risk of postoperative infections. (4)Minimized damage to intra-articular tissue: The minimally invasive nature of the endoscopic technique results in less damage to the joint’s soft tissues, minimizes disruption to blood circulation, and promotes faster postoperative recovery. (5) No need for traditional fixation devices: The use of bioartificial bone grafting eliminates the need for traditional metal plates or screws, reducing the need for intraoperative fluoroscopy and eliminating the need for secondary removal of the internal fixation device, thus avoiding additional surgeries, minimizing trauma, and reducing surgical costs. In terms of surgical complications, arthroscopic surgery is more minimally invasive, avoiding prolonged exposure of joint tissues to the air as seen in open surgery. This leads to less bleeding and a reduced incidence of postoperative redness, swelling, or infection. Furthermore, arthroscopic surgery enables early knee flexion exercises, which helps prevent joint adhesions and venous thrombosis, leading to a lower rate of complications.In conclusion, compared to traditional open reduction and internal fixation, this method is more effective in helping patients regain knee joint function post-surgery and reducing the occurrence of complications.
This surgical technique also has some limitations. It requires a good knowledge of anatomy and some experience with arthroscopic posterior approaches, especially for the establishment of a posterior approach. During the procedure, there is a risk of injury to the popliteal neurovascular bundle. To reduce this risk, the arthroscopic lens needs to be placed in a safe area (with the medial head of the gastrocnemius as an anatomical landmark) and the arthroscopic power system needs to be away from the popliteal structures. In addition, there is a risk of overcorrection of the lateral tibial plateau concavity during the use of the push rod elevation; to avoid this risk, the articular surface of the posterolateral plateau should be observed through the anterior approach during the posterolateral bone block elevation. Additionally, the limitations of this study include a small sample size. To ensure the stability of the knee joint, when artificial bone fixation is used alone, external brace fixation is required for 3 months. This precaution may be avoidable in the future. A biomechanical analysis could be conducted to assess the possibility of forgoing brace fixation after surgery. Looking ahead, with the ongoing development of biological internal fixation materials and advancements in arthroscopic technology, arthroscopic treatment of tibial plateau fractures will continue to improve.
Conclusion
Arthroscopic treatment of Schatzker type III posterolateral plateau collapse fractures offers several advantages compared to conventional open reduction and internal fixation. These benefits include shorter operation time43,44, lower costs, fewer incision-related complications, no need for secondary removal of internal fixation, faster recovery of joint function, and minimally invasive, aesthetically pleasing incisions.
Author contributions
R.F.-Z. and Y.Q.-W. designed this study. Data were acquired by Y.Q.-W., Y.X.-Q. and X.-Z., R.F.-Z. and Y.Q.-W. analyzed the data. All authors participated in the interpretation of the data. All reviewed and revised the manuscript, and approved the final manuscript as submitted.
Funding
This study was supported by the Research and Development Fund Project of Affiliated Hospital (Teaching Hospital) of Shandong Second Medical University in 2024 (2024FYQ029) and the 2023 Weifang Science and Technology Development Plan (Medical) Project (NO.2023YX115).
Data availability
All data generated or analysed during this study are included in this published article.
Declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The studies approved by the Ethics Committee of Nanyang Hospital of Traditional Chinese Medicine (Nanyang Orthopedic Hospital; KJGG123). Meanwhile, informed consent from patients was waived (this was a retrospective study and no other intervention was required on the patients), and all patients signed an informed consent form when they initially received treatment.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rongfang Zhang and Yuqi Wang contributed equally to this work.
6 References
- 1.Rozell, J. C., Vemulapalli, K. C., Gary, J. L. & Donegan, D. J. Tibial plateau fractures in elderly patients. Geriatr. Orthop. Surg. Rehabil.7, 126–134. 10.1177/2151458516651310 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prat-Fabregat, S. & Camacho-Carrasco, P. Treatment strategy for tibial plateau fractures: An update. EFORT Open. Rev.1, 225–232. 10.1302/2058-5241.1.000031 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kfuri, M. & Schatzker, J. Revisiting the Schatzker classification of tibial plateau fractures. Injury49, 2252–2263. 10.1016/j.injury.2018.11.010 (2018). [DOI] [PubMed] [Google Scholar]
- 4.Elsoe, R. et al. Population-Based epidemiology of tibial plateau fractures. Orthopedics38(9), e780–e786. 10.3928/01477447-20150902-55 (2015). [DOI] [PubMed] [Google Scholar]
- 5.Prat-Fabregat, S. & Camacho-Carrasco, P. Treatment strategy for tibial plateau fractures: An update. 1(5), 225–232. 10.1302/2058-5241.1.000031 (2017). [DOI] [PMC free article] [PubMed]
- 6.Ziogas, K., Tourvas, E., Galanakis, I. & Kouvidis, G. Arthroscopy assisted balloon osteoplasty of a tibia plateau depression fracture: A case report. N Am. J. Med. Sci.7(9), 411–414. 10.4103/1947-2714.166223 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andonov, Y. Lateral tibial plateau fractures with posterior comminution. Can a rim plate offer sufficient support? Acta Orthop. Belg.89(2), 275–279. 10.52628/89.2.10533 (2023). [DOI] [PubMed] [Google Scholar]
- 8.Hartwich, M. et al. Joint depression in tibial plateau fractures: to bone graft or not to bone graft? Injury210.1016/j.injury.2023.02.050 (2023). [DOI] [PubMed]
- 9.Chase, R., Usmani, K., Shahi, A., Graf, K. & Mashru, R. Arthroscopic-assisted reduction of tibial plateau fractures. 50(3), 305–314. 10.1016/j.ocl.2019.03.011 (2019). [DOI] [PubMed]
- 10.Mitev, K., Zafiroski, G., Mladenovski, S. & Nikolov, L. A. Arthroscopic reduction and percutaneous osteosynthesis of tibial plateau fractures. Open Access Maced. J. Med.Sci.7(5), 779–781. 10.3889/oamjms.2019.197 (2019). [DOI] [PMC free article] [PubMed]
- 11.Gálvez-Sirvent, E., Ibarzábal-Gil, A. & Rodríguez-Merchán E. C. Complications of the surgical treatment of fractures of the tibial plateau: Prevalence, causes, and management. 7(8), 554–568. 10.1530/EOR-22-0004 (2022) [DOI] [PMC free article] [PubMed]
- 12.Rudran, B., Little, C., Wiik, A. & Logishetty, K. T. Tibial plateau fracture: Anatomy, diagnosis and management. Br. J. Hospital Med.81(10), 1–9. 10.12968/hmed.2020.0339 (2020). [DOI] [PubMed]
- 13.Garner, M. R., Warner, S. J. & Lorich, D. G. Surgical approaches to posterolateral tibial plateau fractures. J. Knee Surg.29, 12–20. 10.1055/s-0035-1564731 (2016). [DOI] [PubMed] [Google Scholar]
- 14.Heidari, N., Lidder, S., Grechenig, W., Tesch, N. P. & Weinberg, A. M. The risk of injury to the anterior tibial artery in the posterolateral approach to the tibia plateau: A cadaver study. J. Orthop. Trauma.27, 221–225. 10.1097/BOT.0b013e318271f8f0 (2013). [DOI] [PubMed] [Google Scholar]
- 15.Jagdev, S. S., Pathak, S., Kanani, H. & Salunke, A. Functional outcome and incidence of osteoarthritis in operated tibial plateau fractures. Arch. Bone Jt. Surg.6, 508–516 (2018). [PMC free article] [PubMed] [Google Scholar]
- 16.Ackermann, C., Frings, J., Alm, L. & Frosch, K. H. Arthroscopic controlled closed reduction and percutaneous fixation of posterolateral tibia plateau impression fractures. Arthrosc. Tech.8(8), e867–e874. 10.1016/j.eats.2019.04.001 (2019). [DOI] [PMC free article] [PubMed]
- 17.Shamrock, A. G. et al. Trends and complications of arthroscopic-assisted tibial plateau fracture fixation: a matched cohort analysis. Arthrosc. Sports Med. Rehabil.2, e569–e574. 10.1016/j.asmr.2020.06.016 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zawam, S. H. M. & Gad, A. M. Arthroscopic assisted reduction and internal fixation of tibial plateau fractures. Open. Access. Maced J. Med. Sci.7, 1133–1137. 10.3889/oamjms.2019.248 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Christodoulidis, A., Giardini, P., Menna, C. R., Pagliari, M. & Molinari, M. Treatment of Schatzker type III tibial plateau fractures: report of an alternative, percutaneous technique and brief review of the literature. J. Long. Term Eff. Med. Implants. 34(3), 23–26. 10.1615/JLongTermEffMedImplants.2023048152 (2024). [DOI] [PubMed] [Google Scholar]
- 20.Vendeuvre, T. & Gayet, L. É. Percutaneous treatment of tibial plateau fractures. Orthop. Traumatol. Surg. Res.107(1S), 102753. 10.1016/j.otsr.2020.102753 (2021). [DOI] [PubMed] [Google Scholar]
- 21.Deemer, A. R., Jejurikar, N., Konda, S., Leucht, P. & Egol, K. A. Approach variation affects outcomes after operative repair of lateral tibial plateau fractures. Eur. J. Orthop. Surg. Traumatol.33(5), 1705–1711. 10.1007/s00590-022-03343-7 (2023). [DOI] [PubMed] [Google Scholar]
- 22.Blankenship, A., Singleton, A., Hiatt, L., Evanson, K. W., Phillips, S. & Miller, R. Outcomes following balloon tibioplasty versus conventional osteosynthesis techniques for Schatzker type III tibial plateau fractures: A systematic review. J. Orthop. Surg. Res.17(1), 210. 10.1186/s13018-022-02973-1 (2022). [DOI] [PMC free article] [PubMed]
- 23.Malla, B., Patra, P. & Dash, S. A prospective study of clinical outcomes of management of arthroscopic assisted tibial plateau fractures fixation. Indian J. Res.9, 97–99 (2020). [Google Scholar]
- 24.Elabjer, E. et al. Tibial plateau fracture management: arthroscopically-assisted versus ORIF procedure—clinical and radiological comparison. Injury48(Suppl 5), S61–s64. 10.1016/s0020-1383(17)30742-8 (2017). [DOI] [PubMed] [Google Scholar]
- 25.Doria, C. et al. Tibioplasty, a new technique in the management of tibial plateau fracture: A multicentric experience review. J. Orthop.14, 176–181. 10.1016/j.jor.2016.12.002 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jyothiprasanth, M., JeyaVenkatesh, P., Khan, P. S. & Gopakumar, T. S. Arthroscopy-assisted tibial plateau fracture surgery - minimum 2 years follow up results. J. Arthrosc. Joint Surg.7, 74–77 (2020). [Google Scholar]
- 27.Haq, S. N., Adil, S. S. & Askari, R. To evaluate results of operative management of tibial plateau fractures. J. Liaquat Uni Med. Health Sci.16, 135–138. 10.22442/jlumhs.171630521 (2017). [Google Scholar]
- 28.Rudran, B., Little, C., Wiik, A. & Logishetty, K. Tibial plateau fracture: Anatomy, diagnosis and management. Br. J. Hosp. Med.81(10), 1–9. 10.12968/hmed.2020.0339 (2020). [DOI] [PubMed] [Google Scholar]
- 29.Adams, J. D. Jr. & Della Rocca, G. J. Management of posterior articular depression in tibial plateau fractures. J. Knee Surg.29, 28–33. 10.1055/s-0035-1566737 (2016). [DOI] [PubMed] [Google Scholar]
- 30.Ozkut, A. T., Poyanli, O. S., Ercin, E., Akan, K. & Esenkaya, I. Arthroscopic technique for treatment of Schatzker type III tibia plateau fractures without fluoroscopy. Arthrosc. Tech.6, e195–e199. 10.1016/j.eats.2016.09.023 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cho, J. W., Kim, J. & Cho, W. T. Approaches and fixation of the posterolateral fracture fragment in tibial plateau fractures: A review with an emphasis on rim plating via modified anterolateral approach. 41, 1887–1897. 10.1007/s00264-017-3563-6 (2017). [DOI] [PubMed]
- 32.Yoon, R. S., Liporace, F. A. & Egol, K. A. Definitive fixation of tibial plateau fractures. Orthop. Clin. North. Am.46, 363–375 (2015). [DOI] [PubMed] [Google Scholar]
- 33.Van den Berg, J. D., Quintens, L., Zhan, Y. & Hoekstra, H. Why address posterior tibial plateau fractures? Injury51(12), 2779–2785. 10.1016/j.injury.2020.09.011 (2020). [DOI] [PubMed] [Google Scholar]
- 34.Frosch, K. H., Korthaus, A., Thiesen, D., Frings, J. & Krause, M. The concept of direct approach to lateral tibial plateau fractures and stepwise extension as needed. Eur. J. Trauma. Emerg. Surg.46(6), 1211–1219. 10.1007/s00068-020-01422-0 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ali, A. M., Saleh, M., Bolongaro, S. & Yang, L. The strength of different fixation techniques for bicondylar tibial plateau fractures–a biomechanical study. Clin. Biomech. (Bristol) . 18(9), 864–870. 10.1016/s0268-0033(03)00149-9 (2003). [DOI] [PubMed] [Google Scholar]
- 36.Rohra, N., Suri, H. S. & Gangrade, K. Functional and radiological outcome of Schatzker type V and VI tibial plateau fracture treatment with dual plates with minimum 3 years follow-up: A prospective study. J. Clin. Diagn. Res.10 (5), RC05–RC10. 10.7860/JCDR/2016/18732.7855 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Scolaro, J. A. et al. Fixation of Extra-articular proximal tibia fractures: Biomechanical comparison of single and dual implant constructs. J. Am. Acad. Orthop. Surg.30(13), 629–635. 10.5435/JAAOS-D-21-01089 (2022). [DOI] [PubMed] [Google Scholar]
- 38.Adams, D., Patel, J. N., Tyagi, V., Yoon, R. S. & Liporace, F. A simple method for bone graft insertion during Schatzker II and III plateau fixation. Knee Surg. Sports Traumatol. Arthrosc.27(3), 850–853. 10.1007/s00167-018-5134-9 (2019). [DOI] [PubMed] [Google Scholar]
- 39.Quattrini, F., Ciatti, C., Strigini, G. & Maniscalco, P. Preliminary experience in the arthroscopically assisted treatment of tibial plateau fractures. Acta Biomed.90(1-S), 136–140. 10.23750/abm.v90i1-S.8023 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lubowitz, J. H., Vance, K. J., Ayala, M., Guttmann, D. & Reid, J. B. III interference screw technique for arthroscopic reduction and internal fixation of compression fractures of the tibial plateau. Arthroscopy22, 1359e1–1359e3. 10.1016/j.arthro.2006.04.110 (2006). [DOI] [PubMed] [Google Scholar]
- 41.Hermanowicz, K., Mrozek, T., Góralczyk, A., & Malinowski, K. Arthroscopy-assisted management of Schatzker type III lateral tibial plateau fracture with interference screw fixation. Arthrosc. Tech.10.1016/j.eats.2021.01.014 (2021). [DOI] [PMC free article] [PubMed]
- 42.Hakukawa, S., Kashiwagura, K., Kishimoto, H., Saito, A. & Fukae, K. Impact of quadriceps and hip abductor strengthening on knee joint biomechanics during gait after Schatzker type III tibial plateau fracture: A case study. Cureus17(1), e78092. 10.7759/cureus.78092 (2025). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Giordano, V. et al. Posterolateral fractures of the tibial plateau revisited: A simplified treatment algorithm. J. Knee Surg.35(9), 959–970. 10.1055/s-0040-1721026 (2022). [DOI] [PubMed] [Google Scholar]
- 44.Liu, C. D. et al. Treatment of posterolateral tibial plateau fractures: A narrative review and therapeutic strategy. Int. J. Surg.111(1), 1071–1082. 10.1097/JS9.0000000000001955 (2025). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.