Abstract
COVID-19, an acute respiratory viral infection conveyed by pneumonia caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has affected millions of individuals globally, and is a public health emergency of international concern. Till now, there are no highly effective therapies for this infection without vaccination. As they can evolve quickly and cross the strain level easily, these viruses are causing epidemics or pandemics that are allied with more severe clinical diseases. A new approach is needed to improve immunity to confirm the protection against emerging viral infections. Probiotics can modify gut microbial dysbiosis, improve the host immune system, and stimulate immune signaling, increasing systemic immunity. Several probiotic bacterial therapies have been proven to decrease the period of bacterial or viral infections. Superinduction of inflammation, termed cytokine storm, has been directly linked with pneumonia and severe complications of viral respiratory infections. In this case, probiotics as potential immunomodulatory agents can be an appropriate candidate to improve the host’s response to respiratory viral infections. During this COVID-19 pandemic, any approach that can induce mucosal and systemic immunity could be helpful. Here, we summarize contexts regarding the effectiveness of various probiotics for preventing virus-induced respiratory infectious diseases, especially those that could be employed for COVID-19 patients. In addition, the effects of probiotics, their mechanisms on different aspects of immune responses against respiratory viral infection, and their antiviral properties in clinical findings have been described in detail.
Keywords: SARS-CoV-2 viruses, Probiotics, Gut–lung axis, Clinical trial, Respiratory infection, COVID-19
Introduction
Probiotics are live organisms with immunological health benefits, which affect the host immune system as discovered by Elie Metchnikoff. When administered in precise doses (10^6 CFU/g), these probiotics improve gut microflora and the strains of lactic acid bacteria, especially Bifidobacterium and Lactobacillus strains, confer numerous health benefits mainly suppressing opportunistic bacteria (Nguyen et al. 2022). Beyond, the gastrointestinal system, probiotics or their metabolites have been proven to cure diarrhea and could regulate gut immunity and are resistant to antibiotics, xenobiotics, and pathogenicity or toxicity factors (Din et al. 2021). SARS-CoV-2, or novel coronavirus infections, are mainly located in the lung and can infect the gut, which causes diarrhea during infection (Wu et al. 2020). To fight against viral and bacterial infections, therapy with a modulatory immune system has attained more focus because of its safe use and proven altered host’s immune response (Malemud 2018). The use of immunomodulators like probiotics can alter the immune system and be beneficial for viral infection pathology (Malemud 2018).
Viral respiratory infections are among one of the most threatening diseases responsible for elevated morbidity and mortality worldwide. These infections are mainly caused by coronaviruses, rhinoviruses (RVs), adenoviruses, parainfluenza viruses (PIVs), respiratory syncytial virus (RSV) and influenza viruses (IVs) (Boncristiani et al. 2009; Pattemore and Jennings 2008). Since December 2019, the novel coronavirus has spread vigorously through person-to-person transmission (China Challenges for Global Health Governance 2020; Gorbalenya et al. 2020). As on 16th March 2023, over 760 million confirmed cases and more than six million deaths were recorded worldwide (www.who.int/covid-19).
Presently, conventional medicines are the only treatment option available for this pandemic infection. Chinese management strategies for treating COVID-19 recommend antiviral drugs like resochin, ritonavir/ lopinavir, alpha-interferon, arbidol, ribavirin and therapy with intestinal probiotics, immunopotentiators and corticosteroids, which are anti-inflammatory agents, are suggested to treat the COVID symptoms and to deal with novel coronavirus that causes COVID-19 as mentioned in the guidelines (Fan et al. 2020; Qiu et al. 2020).
Altered immune responses and respiratory tract homeostasis have been linked to changes in the gut microbiome's composition and function, leading to gut infections that result in respiratory tract infections via the gut–lung axis. The gut–lung axis plays a crucial role in shaping the gut microbiome's composition and function, which can impact inflammatory responses and worsen outcomes in respiratory infections caused by microorganisms. Certain microbiota strains, such as probiotics, have shown promising effects on host immunity and pathogen defence by effectively treating intestinal disorders (Yu et al. 2021). Probiotics may modulate the gut immune system by the activation of macrophages (Mfs) or dendritic cells (DCs), toll-like receptors (TLRs); DCs-directed signaling in the gut lumen; and directs cytokines induction through intestinal epithelial cells (IECs), altering the immune functions of immune cells (like B cells, T cells and DCs) in the gut-associated lymphoid tissue (GALT) (Both et al. 2011; Mahooti et al. 2020). The toll-like receptors are the PRRs, viz., pattern recognition receptors in the innate immunity that aids in associating both adaptive and innate immune systems. Toll-like receptors can particularly identify PAMPs, viz., pathogen-associated molecular patterns and send signals to immune cells via its transmembrane (TM) helix. This signal activates transcriptional pathways, like NF-κB, against foreign pathogens (Unterholzner and Bowie 2008; Mahooti et al. 2020). This signal transmission activates the innate and adaptive immune system against pathogens via a cascade (Davidson et al. 2011). Upon administration of probiotics, neomycin-treated mice showed increased TLR7 pathways besides restoring the gut microbiome (Wu et al. 2013). Other research findings have proven probiotics’ efficiency in regulating host immunity that leads to protection from viral infection (Hu et al. 2021).
Probiotics can also alternate interleukin-10 (IL-10) expression and reduce inflammatory cytokines such as TNF-α, IL-1, and IL-8 (Oliva et al. 2012). Probiotics can reduce the periods of respirational symptoms instigated by the coronavirus that causes the common cold followed by fever (Bozkurt and Quigley 2020). A medical report indicated a significant decrease in ventilator-linked pneumonia for those volunteers treated with probiotics comprised of Enterococcus faecalis, Bacillus subtilis and Lactobacillus rhamnosus GG when compared with volunteers treated without probiotics (Zeng et al. 2016).
The nutrients and their metabolites modulate gene expression, development and differentiation of immunogenic cells. (N. EFSA Panel on Dietetic Products 2016). Hence, immuno-nutrition with functional food constituents, probiotics, and prebiotics might be a possible treatment for COVID-19 patients via immunoregulation and microbial homeostasis (Gombart and Pierre 2020). Various clinical trials on COVID-19 are under research and limited studies are on the consequence of intestinal probiotics in treating and managing COVID-19. Therefore, this review summarizes the preventive and curative trial approaches based on immunobiotics against viral respiratory tract infections. We also discussed the immunobiotic effects of probiotics as a prophylactic approach against COVID-19.
Pathogenesis of novel coronavirus
The infection of COVID-19 occurs 5.2 days post incubation period, COVID-19 infection manifests with a median of 14 days, and the time from the onset of COVID-19 symptoms to mortality ranges from 6 to 41 days. The length of this time depends on the patient's age and immune system health. Fever, coughing, and exhaustion are the most typical initial signs of COVID-19 disease. Other symptoms include sputum production, headache, hemoptysis, diarrhea, dyspnea, and lymphopenia (Rothan and Byrareddy 2020). COVID-19 is not associated with the highest case fatality rate compared to other emerging viral diseases like SARS and Ebola. Still, the confluence of a high reproduction number, superspreading events, and a globally immunologically naive population has resulted in the highest global number of deaths in the past 20 years compared to any other pandemic. (Wilder-Smith 2020).
The virus targets the host cell receptor site, i.e., angiotensin-converting enzyme 2 (ACE2) cells present in the lungs. After attaching to the host’s receptor cells, the virus has a gestation period of 2–14 days. The primary infection caused by the virus is in the lungs, which triggers related symptoms to pneumonia with distinct variations in lung opacity on CT scanning. Additional COVID-19 symptoms related to pneumonia include sore throat, shortness of breath, cough and fever (Prompetchara et al. 2020). Other associated gastrointestinal symptoms like diarrhea, nausea, and vomiting also have been observed during COVID-19 infection due to the presence of the same ACE2 receptor cells in the intestinal epithelial cells. Also, coronaviral nucleic acid in a patient suffering from COVID-19 may explore a possible route for viral infection through feces (Jin et al. 2020).
During viral infection, when a virus invades a cell, antigen-presenting cells capture virus antigens by APCs, and send the signal toward antiviral immunity. The major histocompatibility complex (MHC) or human leukocyte antigen (HLA) offers the virus antigen viz., antigenic peptide to specific CTLS i.e., cytotoxic T lymphocytes. Antigen presentation introduces cellular and humoral responses through virus-specific T and B cells viz., adaptive immunity. As in acute viral infections, distinctive immunoglobulin IgG and IgM are activated in contradiction to SARS-CoV-1(Li et al. 2020). After 12 weeks, the IgM antibody disappears; however, the IgG antibody remains in the body for a more extended period to exert the protective role. Studies suggested that in SARS-CoV-1, S and N proteins are the primary targets for the induction of immunoglobulins (de Wit et al. 2016; Li et al. 2003, 2020). Studies reported that with humoral immunity, cellular immunity had been investigated against coronaviruses. The latest investigation of the peripheral blood of coronavirus-infected individuals has observed decreased numbers of CD8 + and CD4 + T cells, similar to the SARS-CoV-1 infection (Li et al. 2020). However, in some SARS patients, the immune cell CD8 + and CD4 + memory T lymphocytes can persist for a few more years with elevated IFN-γ generation, DTH reactions and T cell propagation (Fan et al. 2009; Tang et al. 2011). In the case of MERS-CoV, exact CD8 + T lymphocyte signaling is accountable for the clearance of these viruses in mice, which may be a suitable therapeutic method for dealing with SARS-CoV-2 infections (Mirzaei et al. 2021).
The probiotic effects on respiratory virus infection
The ability to trigger immunological responses at distant mucosal locations significantly influences the gut microbiota. An imbalance in the microbial population of the respiratory tract and gastrointestinal tract affects the lungs' mucosa resulting in respiratory viral infections. The patient may be more vulnerable to secondary bacterial infections due to this dysbiosis altering immune function. According to studies, treating respiratory viral infections with specific Bifidobacteria or Lactobacillus bacteria is advantageous (Darbandi et al. 2021).
Probiotics are living microbes that exert health benefits on the host (FAO/WHO 2001) through numerous latent systems via the local resistance maintained by gut wellbeing and gut wall integrity and systemic resistance via improving the specific and non-specific immune system (Sundararaman et al. 2020). They generally influence the adaptive and innate resistant reactions and might diminish the acuteness of disease in numerous disorders, with respiratory tract infections (Hill et al. 2014; Lehtoranta et al. 2014; Park et al. 2013). Probiotics enhance the activity of leucocytes (polymorphonuclear and monocytes), and the expression of the receptors (CR1, CR3, FccRI, and FcaR) are connected with phagocytosis activity, induce the microbicidal role of neutrophils, and increase the number as well as the activity of NK cells in the blood (Hao et al. 2011).
Probiotic administration reduces the risk of respiratory tract infection in children (Araujo et al. 2015). Probiotic usage generally reduces the risk of the primary cold and diminishes the interval of infections appearing in the respiratory tract (Wang et al. 2016). Probiotics, generally regarded as safe, accessible therapy with immunobiotic effects via altering cytokines stimulation, have been pondered to be investigated against various coronavirus strains (Morais et al. 2020; Jiang et al. 2016). The intestinal dysbiosis, especially the reduced number of probiotics like Lactobacillus and Bifidobacterium among some COVID-19 individuals, may get in secondary infection in response to bacterial translocation (Xu et al. 2020). The recombinant Lactobacillus plantarum inhibits porcine epidemic diarrhea virus (PEDV), transmissible gastroenteritis virus (TGEV) infection IPEC-J2 cells, and alpha coronaviruses, which causes high morbidity and mortality in piglets resulting in the substantial economic loss (Liu et al. 2020a, b).
Depending on the various stains, probiotics can modulate the immune system in several ways (Maassen et al. 2003). Lin and colleagues suggested that Lactobacillus spp. affects antigen-specific IgG and cytokine reactions (Liu et al. 2009). The activation of myeloid dendritic cells with lactobacilli resulted in a clear shift towards T helper 1 and Tc1 polarization of CD4 + and CD8 + T cells, as indicated by the secretion of IFN-γ, but not IL-4 or IL-13. Due to lactobacilli's ability to activate myeloid dendritic cells, initiate T cell responses, and stimulate Th1 cytokines, specific strains and species of lactobacilli could be valuable in delivering biotherapeutics and vaccines (Mohamadzadeh et al. 2005). Probiotics-mediated immunomodulation also exerts through constituents like nucleic acid, lipoteichoic acid peptidoglycan which indorses Toll-like receptors, and muramyl dipeptide, which provokes Nod-like receptors (Pimentel-Nunes et al. 2010). Immune regulation arises along regulatory T cells, Th17 cells and type 3 innate lymphoid cells by identifying the strain of probiotic or its constituents and its influences on mucosal immunity (Goto et al. 2016; Kanauchi et al. 2018; Perez-Lopez et al. 2016). The probiotics could induce the number and activity of neutrophils, leukocytes, and natural killer cells during infection. Also, the expression of interleukin (IL)-10 is altered by probiotics. It also reduces the expression of inflammatory cytokines, such as tumor necrosis factor-a, IL1b, and IL-8 (Oliva et al. 2012), produces increased salivary immunoglobulin A and induces bacteriocins by eventual deliberation of the antimicrobic activity (Fooks and Gibson 2002).
Probiotics give out anti-inflammatory effects exerting bioactive compounds to restore intestinal permeability (Rosa et al. 2017). The lung’s anti-inflammatory activity can reduce inflammation by reducing pro-inflammatory cytokines and C-reactive protein (CRP) levels (Li et al. 2018). Probiotics reduce the production of IgE, interleukin-4 (IL-4), and IL-13 by suppressing the activation of Th2cells, thereby preventing asthma and allergic reactions (Rosa et al. 2017; Oeser et al. 2015). The probiotics may attach to viruses, thus hampering the attachment of viral to specific host receptors (Kanauchi et al. 2018).
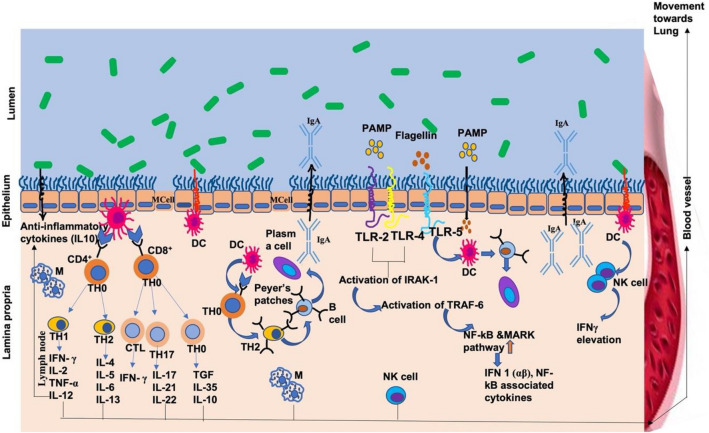
Essentially, some mechanisms have been offered for a better understanding of the modulatory probiotic effect on respiratory infections caused by viruses (Fig. 1) such as direct outcome by trapping approaches, stimulation of the immune responses by IgA, Th1, NK cells and interleukins assembly activation of mucosal defence mechanisms (mucins of gut may bind to viruses and restrict replication of virus), induction of antivirus elements such as hydrogen peroxide (H2O2), instigation by host cells and production of dehydrogenase, immunomodulation of resistance immune cells like macrophages and dendritic cells (DCs), stimulating CD8 + T cells differentiation into CTLs, that destroy cells that are infected, CD4 + T cells differentiation into Th1 and Th2 cells and ultimately B cells activation by Th2 cells (Kanauchi et al. 2018; Tapiovaara et al. 2016). Probiotics in the colonic epithelium produce short-chain fatty acids (SCFA) like acetate, propionate, and butyrate. The colonocytes use butyrate as energy, while the portal circulation absorbs acetate and propionate through the intestine (Natarajan and Pluznick 2014). The SCFA generally binds to the receptors such as free fatty acid receptor 2 (FFAR2/GPR43) / G-protein-coupled receptor 43, GPR41 / GPR109A and FFAR3 and macrophages are activated and induces differentiation of dendritic cell precursors which can transfer to the lungs and modify the regulator T cells with Th2 cells (Shukla and Budden 2017).
Fig. 1.
Mechanisms of probiotic immunomodulation effects in the intestine to defend against respiratory viral infections. Probiotics (highlighted in green color) can induce immunomodulation by directly and indirectly interacting with the cells lining the intestine. Dendritic cells (DC), which extend their dendrites between these intestinal epithelial cells, can sample and process probiotics, activating innate and adaptive immune responses. These dendritic cells (DCs) are located directly below specialized cells called M cells, which can also engulf probiotics and lead to the maturation of dendritic cells (DCs) and the production of plasma cells from B cells. Moreover, when macrophages and dendritic cells (DCs) in the lamina propria interact with probiotics, they become activated and stimulate natural killer (NK) cells to produce interferon-gamma (IFN-γ) to fight off viruses. Probiotics can also stimulate the expression of antiviral genes through toll-like receptors (TLRs) and the nuclear factor-kappa B (NF-κB) pathway. Ultimately, these activated immune cells can travel through the lymphatic and circulatory systems to reach sites of infection and defend against respiratory viruses
Probiotic mechanisms of gut–lung axis for respiratory viral clearance
Clinical information has revealed that specific probiotic strains enable to treat the bacterial and viral infections, such as sepsis, gastroenteric and respiratory tract disease syndrome (Lin et al. 2020; Reisinger and Stadlbauer 2019). Every organ like the lung has its commensal microbial association, and a gut–lung relationship is a state where host–microbe, microbe–microbe, and microbe-immune interactions pay attention to the progress of the respiratory illness (Enaud et al. 2020). The intestinal and lung connection is mediated through the lymphatic system via the TLR4 mechanism that stimulates immunoglobulin IgA related to gut-associated lymphoid tissue (GALT) (He et al. 2017). Probiotic bacteria increase T regulatory (Treg) cells and T helper 17 (Th17) cells and Th1 cell response (He et al. 2017). The lymphatic system's circulation permits the transmission of Th17 cells from intestinal mucosal cells to the bronchial epithelial mucosa in lymph nodes in the airways via the gut–lung axis. Probiotics direct the host's lung immunity defence, suppress respiratory pathogens' activity and hinder airway tissue impairment (He et al. 2017).
Respiratory tract infections like influenza are related to an improper microbe association of the gastrointestinal and respiratory tracts (Sencio et al. 2020; Hanada et al 2018). This dysbacteriosis may alter subsequent immune responses that influence the secondary bacterial infection. An acute disease COVID-19 might be allied with intestinal dysbacteriosis responsible for inflammation and a more flawed to pathogenic response (Gao et al. 2020a, b; Xu et al. 2020), for that probiotic can restore gut homeostasis (Di Pierro 2020). Probiotics also can influence the gut–lung axis, as some could transfer from the gut to outlying sites, like the breast, to treat mastitis (Arroyo et al. 2010). Probiotics upregulate the levels and activity of type I interferons, APCs, T cells, NK cells, and the state of mucosal and systemic specific immunoglobulins in lungs (de Vrese et al. 2005; Namba et al. 2010; Zelaya et al. 2016). The consumption of probiotics alters the balance between immunoregulatory cytokines and pro-inflammatory cytokines, which let clearance of viruses by minimizing immune response mediated impairment to the lungs (Fig. 1). This finding may be mostly appropriate to prevent the acute respiratory distress syndrome, a significant complication of COVID-19.
The middle-aged group who has given Lactobacillus DR7 revealed the destruction of plasma pro-inflammatory cytokines, like TNF- a and IFN-g. Additional trials of early adults displayed improvements in anti-inflammatory cytokines, such as IL-10 and IL-4, and reduced the plasma cell's peroxidation and levels of oxidative stress (Di Pierro 2020). Orally consumed probiotics can play an essential role in modulating the development of inevitable cytokine storms in volunteers suffering from COVID-19 infection. Orally consumed probiotics exert an immunogenic response derived from the intestine, which is a vital site of the host defences by improving tight junctions' integrity, and act as fuel for colonocytes by absorbing butyrate that theoretically reduces SARS-Cov-2 invasion (Sharma and Riva 2020).
The test analysis of SARS-CoV-2 RNA has been observed in the patient's gut and fecal samples and in the sewage pipelines. Being the carrier for COVID-19, SARS-CoV-2 can also contaminate intestinal cells (Wang et al. 2020a, b, c). Influenza viruses are linked to the variance of microbes in the respiratory and gastrointestinal tracts (Reisinger and Stadlbauer 2019). Consumption of particular bifidobacterial and lactobacilli strains can positively affect the clearance of the influenza virus from the respiratory tract. Probiotics have been proven via experimental and clinical studies to confer antiviral activity (Abt et al. 2012). However, these mechanisms and probiotic effects have not yet been verified on SARS-CoV-2. This prophylactic approach should not be rejected, mainly when probiotics have been positively tested against other respiratory coronavirus strains (Zafar et al. 2020). Furthermore, patients are also facing attack of secondary viral infections that must be treated soon.
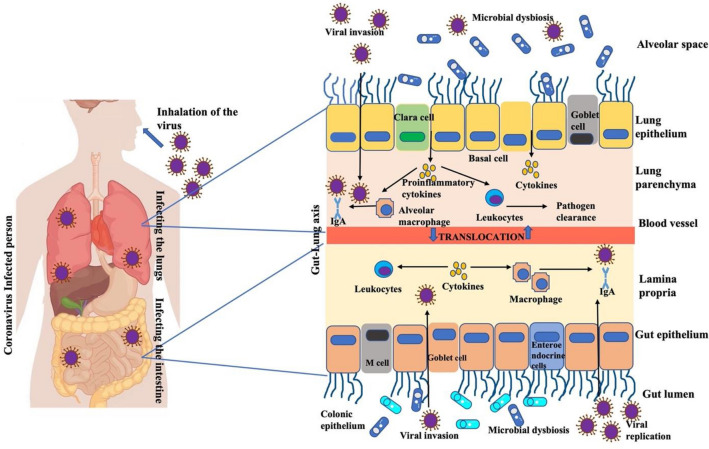
Gut microbial dysbiosis during COVID‑19 infection
The gut microbiome acts as a protective barrier and aids in altering intestinal immunity. Various environmental features manipulate the lower tract microbiota. Thus, the association between the microbiota and intestinal immunity is crucial to the reserve homeostasis of intestinal microbes. When there is the deliberation of this homeostasis by any way of contamination, the stable gut microbial population will alter, and the dysbiotic population leads to various intestinal and extraintestinal diseases (Fig. 2) (O’Toole and Jeffery 2015; Chang and Kao 2019; Belizario and Faintuch 2018; Mirzaei et al. 2021). This dysbiosis condition can initiate the host’s immune system, i.e., stimulate the immune cells, induce soluble cytokines, cell receptors activation, and the chief support of the immune defence system. The interaction between environmental factors and microbiota disturbs mucosal immunity (Neish 2014) present in both the lung and intestine. The connection between the pharyngeal microbes and COVID-19 infection was reported (Budding et al. 2020). With aging changes in the diversity of the pharyngeal microbial population or a decrease in their population in older individuals is possible (Antunes et al. 2020). The decreased microbial community might be responsible for the higher susceptibility of aged individuals to the coronavirus. When a person is infected with the COVID-19 virus, a dysbiotic microbial environment triggers inflammation in their body and an excessive release of cytokines, commonly referred to as a ‘cytokine storm’. (Antunes et al. 2020).
Fig. 2.
Probiotic effects associated with COVID-19 virus clearance from the host. (1) Entry of virus in the lungs and emphasis on the associated events: Following nasal inhalation of SARS-CoV-2 enters host cells and attaches to the respiratory tract's epithelium layer, leading to microbial dysbiosis. This triggers the activation of the innate immune system via dendritic cells and macrophages through the production of immune signals and pro-inflammatory cytokines. The release of these pro-inflammatory cytokines stimulates the involvement of macrophages and natural killer cells in engulfing and inhibiting virus particles and infected cells. (2) The interaction of the virus with the gut membrane and emphasis on the events associated with it: The initial spread of viruses through the circulatory system can cause changes in the microbiota of the gut epithelium and increase gut permeability, ultimately leading to an inflammatory immune response. Probiotics interact with the gut's epithelium layer and are detected by intestinal immune cells, which can influence the production of pro-inflammatory cytokines and regulate immune responses in the respiratory tract and gut. The pro-inflammatory cytokines secreted during this process disseminate in the blood circulation and reach the respiratory tract's epithelium layer, via the gut–lung axis, aiding alveolar macrophages and natural killer cells in eliminating the coronavirus. Several strains of probiotics produce these cytokines, enhancing the expression of genes related to the innate immune system, even in the lungs, and altering the lung's immune environment ultimately via producing virus-specific immunoglobulins and cytokines
Potential probiotic effects on COVID-19 virus
COVID-19 infection primarily infects the lung and initiates airway inflammations (Huang et al. 2020). Some patients with COVID-19 exhibit significantly increased levels of serum pro-inflammatory cytokines, including TNF-α, IFN-γ, IL-17, IL-15, IL-6, and IL-1B (Huang et al. 2020). Elevated cytokines can lead to the development of cytokine storms, which contribute to disease progression (Huang et al. 2020). The rise of cytokine storms leads to pulmonary fibrosis and impairment of respiratory organs and this inflammatory response may be activated by the activation of Th1 cells (Mortaz et al. 2013). Experimental and clinical studies have provided evidence that probiotics can induce antiviral activity through immunomodulation, even against common respiratory viruses such as rhinovirus, influenza, and the respiratory syncytial virus (Luoto et al. 2014; Waki et al. 2014; Turner et al. 2017; Lehtoranta et al. 2014; Tapiovaara et al. 2016; Mirzaei et al. 2021; Al Kassaa 2016). In mice, oral consumption of Lactobacillus acidophilus CMCC878 within 24 h of pulmonary inoculation of Staphylococcus aureus and Pseudomonas aeruginosa reduced the microbial count in the lungs, and mitigated lung impairment and systemic inflammation (Shoaib et al. 2019). Oral administration of probiotics like Bifidobacterium and lactobacilli has protective effects against RSV, RVs, IV, pneumovirus and adenovirus (Canani et al. 2011; Ma et al. 2019). In the context of COVID-19 infection, it has been suggested that the consumption of certain bacterial strains, including Bifidobacterium lactis DSM 32,247, Bifidobacterium lactis DSM 32,246, Lactobacillus brevis DSM 27,961, Lactobacillus plantarum DSM 32,244, Lactobacillus paracasei DSM 32,243, Lactobacillus helveticus DSM 32,242, Lactobacillus acidophilus DSM 32,241, Streptococcus thermophilus DSM 32,345 could mitigate the progression of COVID-19 infection (d’Ettorre et al. 2020). Patients treated with conventional medications with oral bacterial administration lowered the risk of rising respiratory collapse. Studied patients showed a higher survival rate and lower requirement of intensive recovery due to coronavirus infection than those treated with only conventional medications (d’Ettorre et al. 2020). Additionally, this bacterial therapy was observed to improve COVID-19-related symptoms, such as myalgia, diarrhea, dyspnea, pyrexia, asthenia, and cough, with significant improvements often seen within 24–48 h (d’Ettorre et al. 2020). It has been suggested that respiratory distress induced by the coronavirus may be related to dysbiosis in the gut and the consequent modulatory effects on immunity (Chiu et al. 2017) (see Fig. 2). These findings highlight the potential of probiotics to prevent or mitigate viral respiratory infections, including those caused by the various strains of coronavirus (Jiang et al. 2016; Morais et al. 2020). Studies have shown that COVID-19 patients with imbalanced intestinal flora, characterized by reduced levels of beneficial bacteria such as Lactobacillus and Bifidobacterium, are more susceptible to secondary microbial infections (Xu et al. 2020; Feng et al. 2020). A modified strain of Lactobacillus plantarum has been found to have antiviral properties against coronavirus infections in porcine intestinal epithelial cell lines (Liu et al. 2020a, b). Furthermore, Lactobacillus gasseri has been shown to inhibit the spread of coronavirus by hindering purine activity that thought to be a source for viral energy and viral mutation (Mirzaei et al. 2021).
Food supplemented with bacterial probiotics, like Lactobacillus and Bifidobacterium, have shown beneficial effects such as regulation of allergic reactions, and protection against microbial (bacterial and viral) infection in the host (Kanauchi et al. 2018; Zolnikova et al. 2018; Kawahara et al. 2015; Hajavi et al. 2019; Park et al. 2013). ACE2 is a known receptor for SARS-CoV, the virus responsible for COVID-19, and is expressed widely in various tissues including the lungs, heart, kidneys, and gut. ACE2 is a component of the renin–angiotensin system and plays important role in regulating inflammation, blood pressure, and fluid balance (Ziegler et al. 2020). In the gut, ACE2 expression is associated with suppressing inflammation, maintaining amino acid homeostasis, and promoting a healthy gut microbiome (Yu et al. 2021). Gut dysfunction has been linked to respiratory infections and worsened clinical outcomes. Peptides produced by lactic acid bacteria have been shown to have ACE inhibitory effects (Ettinger et al. 2014), suggesting that probiotics may improve respiratory tract infections in COVID-19 patients by modulating the ACE2 pathway. These immunobiotic benefits can support lung function and potentially treat and clear the virus from the host (Wu et al. 2018; Baud et al. 2020). Probiotics may also regulate the ratio of pro-inflammatory and anti-inflammatory cytokines (Li et al. 2021), which can help to mitigate cytokine storms in COVID-19 patients. Infected individuals have been found to have higher levels of interleukins IL-6 and TNF-α (Aziz et al. 2020).
A steady diet with probable probiotics and vitamin supplements can aid in upregulating the immune system against SARS-CoV-2. Probiotics and their metabolites, gamma-aminobutyric acid, acetic acid, lactic acid and plantaricin, might improve the immune systems response against infections caused by viruses (Albarracin et al. 2017). The infection and disease progression of the virus require its attachment to the host’s receptor. In the case of coronavirus, infections are initiated by attaching to the ACE2 receptor on the host by the viral surface via S glycoprotein homotrimers (Tortorici 2019). The microbial metabolites plantaricin prevents the coronaviral attachment with the host’s receptor, thus preventing the entry of SARS-CoV-2 that causes disease (Anwar et al. 2020). The computational bioinformatics was also used to understand the effect of metabolites on the viral RNA-dependent RNA polymerase (RdRp), which is essential for the replication of the virus. Also, multiple possibilities such as blocking residual binding domain (RBD) on spike (S) proteins or interface of S protein with ACE2 receptor proteins on the host or hindering RdRp from countering any COVID-19 effect by molecules of plantaricin, are suitable ways in the COVID-19 treatment. Metabolites of Lactobacillus plantarum inhibit viral invasion by interacting with ACE2, RBD and RdRp (Aanouz et al. 2020; Anwar et al. 2020). The S protein blockage, a foremost structural protein with an essential function of SARS-CoV-2 life cycle, might be one of the utmost promising approaches (Anwar et al. 2020). The finding was inveterated by a molecular model recognizing the sturdiness of the plantaricin networks and SARS-CoV-2 (ACE2, RBD and RdRp receptor) (Anwar et al. 2020). Molecular computational models can precisely recognize medicines that can be repurposed without requiring clinical trials. The medication with plantaricin can be measured as a temporary consideration till the discovery of definite antiviral medicines for COVID-19 (Mirzaei et al. 2021).
Interleukin-17 is a pro-inflammatory cytokine that aids in adaptive immunity and is an effective inducer of endoplasmic reticulum strain autophagy via inositol-demanding enzyme 1 (Bozkurt and Quigley 2019; Kim et al. 2015). Autophagy mediated stress and inflammation can be inhibited by hindering this interleukin (Kim et al. 2015; Hajeer et al. 2016). Evidence suggested that certain strains of Bifidobacterium have an inhibitory activity on interleukin-17 (Bozkurt and Quigley 2019). Therefore, usage of high doses of Bifidobacterium strains such as B. animalis subsp. lactis BB-12 and its lipopolysaccharides (Schiavi et al. 2016; Taipale et al. 2011) might be used as a potent preventive and therapeutic approach in patients suffering from COVID-19, especially in those suffering from gastrointestinal symptoms. The positive effect on symptoms and hospitalization period in COVID-19 patients who consumed probiotics with maltodextrin for 30 days was demonstrated. This benefits gut commensals and fewer severe clinical manifestations like illness (ClinicalTrials.gov 2020). Also, the preventive efficacy of Lactobacillus coryniformis K8 on the frequency and severity of COVID-19 in healthy workers dealing with the coronavirus when administered the probiotic (3 × 109 cfu/day) for 60 days was reported (Bioresearch 2020).
The COVID-19 patients were administered beta-gluten probiotic merged powder as a nutrition aid to investigate the practical clinical pathway and the results will be of great consequence for the prevention and therapy of SARS-CoV-2 infection (HwaMei Hospital UoCAoS 2020). The investigation on intestinal impairment during pneumonia caused by a coronavirus was conducted to explore the dynamic variations of intestinal flora and metabolomics pre- and post-intermediation with a microecological component with an effect on the clinical consequence, and to discover the use of precise strains and metabolites to support nutritious products for original influenza (Shanghai 10th People’s Hospital TU 2020). Scientists postulate that the administration of Omni-Biotic® 10 AAD can reduce the period of diarrhea, reduction of stool frequency, increase stool steadiness, reduces disease period and severity, decrease inflammation of the intestine and recover dysbiosis in COVID-19 volunteers (Hung et al. 2021). In Canada, a randomized clinical trial was conducted in a randomized way with single-blinded experiments in COVID-19 patients within 96 h of diagnosis. The trial aimed to investigate the effectiveness of BID nasal spraying for two weeks using either NeilMed Sinus rinse or Probiorinse probiotic nasal irrigation solution (Yamamoto et al. 2020). The clinical research aimed to investigate the efficacy of a probiotic mixture containing Pediococcus acidilactici and Lactobacillus plantarum as a co-adjuvant in adults with COVID-19 to reduce the risk of progression to moderate or severe COVID-19 and death. The trial also aimed to determine the effect of the probiotic mixture on fecal microbiota and its correlation with clinical outcomes (AB Biotics SA 2020). SARS-CoV-2 pneumonia allied with gut dysbiosis may progress subordinate bacterial infections and antibiotic-associated diarrhea (AAD). The research investigation engaged washed microbiota transplantation (WMT) to treat seriously ill individuals with AAD. This clinical experiment intends to assess the result of WMT associated with typical treatment for patients suffering from SARS-CoV-2 pneumonia, especially for those with dysbiosis-related situations (Zhang 2020).
Clinical outcomes of probiotics immunomodulation involved in respiratory viral infection
Probiotics exert several health-beneficial effects, including in the upper respiratory tract during infections. There are several pieces of evidence regarding the clinical use of probiotics to treat infections in individuals ranging from children to older age groups (Table. 1). It is observed that probiotic L. brevis KB290 has reduced the frequency of influenza infection among children with no adverse effects when administered with probiotic-drinks (Waki et al. 2014). Viral infection increases one of the potent marker proteins, i.e., C-reactive protein (CRP), in the liver and blood of the host cells. In patients with high CRP levels, bacteremia or pneumonia is treated with probiotics, which can reduce the CRP level. This treatment is safe and causes no inflammatory effects (Hu et al. 2016). Wang et al. 2018 have suggested that ingesting Lactobacillus rhamnosus GG decreases the hazards of influenza and other respiratory viral infections in elderly volunteers (Wang et al. 2018). Another investigation also indicated that probiotics positively prevent and treat common colds and upper respiratory infections (Olivares et al. 2007). Another research report recommended that the immunomodulatory effects of probiotics are involved in combating the progression of rhinovirus infection (Turner et al. 2017; Pang et al. 2012). Turner et al. 2017 observed that consumption of probiotic Bifidobacterium animalis ssp. lactis Bl-04 can decrease the level of CXCL8 response in nasal lavage, and downregulate rhinoviral replication and virus shedding in the nasal secretions. Probiotic-causing microbial alteration lowers the risk of viral respiratory tract infection and protects from virus-stimulated inflammation (Luoto et al. 2014; Rosenberg and Domachowske. 2012). The probiotics are linked to significant prevention or reduction in common upper respiratory tract infection duration (Kumpu et al. 2013), providing evidence from clinical studies. Regulation of immune responses by probiotic organisms has beneficial effects on respiratory infections in the studied individuals as listed in Table 1.
Table 1.
Clinical studies describing the immune responses of probiotic bacteria to treat viral respiratory infections
| Probiotics | Respiratory tract infections | Studied individuals | Findings | References |
|---|---|---|---|---|
| Lactobacillus rhamnosus GG | Viral respiratory infection, Upper respiratory tract infection, Respiratory tract infection | New-born, Children | Early modification of immune response and gut microbial change; Reduces the risk of respiratory tract infection; Potentially decreases the frequency of acute otitis media—the infections of upper respiratory system; | Luoto et al. (2014); Hojsak et al. (2010); Kumpu et al. 2013; Liu et al. (2013) |
| Lactiplantibacillus plantarum KABP022, KABP023, and KAPB033, Pediococcus acidilactici (KABP021) | Respiratory tract infection |
COVID-19 outpatients (Median age 18–60) |
Probiotics have been proposed has adjuvant for COVID-19 | Gutiérrez-Castrellón et al. (2021) |
|
Probiotics like Lactobacillus casei rhamnosus |
Respiratory infection | Children | Controls bacterial, viral and respiratory infections | Lin et al. (2009) |
| Lactobacillus casei DN-114 001 | URTI such as rhinopharyngitis | Elderly volunteers | Reduced duration of common infectious disease like URTI | Guillemard et al. (2010) |
|
Lactobacillus delbrueckii ssp. bulgaricus (L. bulgaricus) OLL1073R-1 |
Decreased the chances of common cold occurrence | Elderly individuals | Increased the activity of NK cells involved in antiviral defence | Makino et al. (2010) |
| Lactobacillus paracasei N1115 | Upper respiratory tract infections (URTI) | Middle-aged and older adults | The augmentation of T-cell-mediated immune protection may be one of the serious causal mechanisms by which probiotics aids in alleviation of infections | Pu et al. (2017) |
| Bifidobacterium, Lactobacillus, and Enterococcus | COVID-19 adult patients | Clinical improvement including fever, reduced stay in hospital, increased shedding for viral load of hospitalized COVID-19 patients | Zhang et al. (2021) | |
| Bifidobacterium lactis subsp. plactis Bl-04, Lactobacillus acidophilus NCFM, Bifidobacterium animalis subsp. Lactis Bi-07 | Respiratory tract infection | Volunteers (Men and Women) | Consumption of probiotics exerts valuable for diminishing the menace of URTI in healthy and physically energetic adults | West et al. (2014) |
|
Bacillus coagulans LBSC (DSM 17,654), Bacillus subtilis PLSSC (ATCC SD 7280), and Bacillus clausii 088 A E (MCC 0538) |
Respiratory tract infection | In adults with fatigue induced by post sequelae of previously confirmed COVID-19 | Improved mental and physical fatigue scores in the treatment group versus the control arm | Rati et al. (2021) |
|
Lactobacillus and Bifidobacterium strains |
Acute respiratory infection | Healthy children and adults | Probiotics decrease the duration of illness in healthy children and adults | King et al. (2014) |
A favorable probiotic-based oral approach, a vaccine against SARS‑CoV‑2
Various vaccines turned out to be industrialized against the coronavirus, and others are undergoing clinical trials (Gao et al. 2020a, b; Wang et al. 2020a, b, c; Zha et al. 2020). Injectable vaccines are more expensive and need proficient administration; however, oral vaccines are more reasonable, easy to preserve, simple to administer, and biofriendly (Shakoor et al. 2019). It has been reported that vaccines that are given orally can stimulate the vigorous construction of precise antibodies like IgA and IgG and Th17 and Th1 cells, thus preventing the replication of the virus in the intestinal mucosa and respiratory tract (Liu et al. 2020a, b; Wang et al. 2019). Therefore, an effective SARS-CoV-2 oral vaccine would benefit the society. Lactic acid bacteria are generally appropriate bacterial vectors for oral DNA and protein transportation (Wang et al. 2019). They usually present in the individual intestine and provide health benefits in gastrointestinal and inflammatory illnesses (Huang et al. 2020; Sun et al. 2018). A research investigated probiotic Lactobacillus plantarum can be employed in food, vaccines, and medication (Seddik et al. 2017; Park et al. 2019; Ren et al. 2015). A previous report stated that probiotics could be suitable to increase vaccine immunogenicity, enhancing the proportion of seroprotection and seroconversion in grown-ups immunized with flu vaccines (Lei et al. 2017). Wang et al. 2020a, b, c indicated that Lactobacillus plantarum as a system expresses the production of SARS-CoV-2 S protein. This protein exhibited significant awareness with a SARSCov-2-S-protein-specific monoclonal antibody and anti-HA-tagged rabbit polyclonal antibody (Wang et al. 2020a, b, c). The durability of the immunogenic protein is essential for oral vaccines. Accordingly, they considered the constancy of the S protein displayed on the surface of bacteria and its resistance to heat and low pH. The level of S protein expression was raised with the subsequent exposure to 0.2% bile salt, inferring that the recombinant Lactobacillus plantarum Lp18:S might be appealed as an oral vaccine for the treatment of COVID-19 (Wang et al. 2020a, b, c).
Conclusions
SARS-CoV-2 is a new emerging pathogen that is still under research on how the variants of the virus act and how mechanisms stimulate an immune response. In this present review, we discussed the recent advancements made in the consumption of probiotics to improve and treat viral infections of the respiratory tract. Also, we discussed the correlation between respiratory virus diseases with the dysbiotic intestinal microbiome and the imbalanced immunity as a consequence of virus and host connections. Introducing bacterial therapy with probiotics by moderating the inflammatory immune responses upon viral infection has exposed encouraging outcomes. Though most of the studies have been showing on respiratory viruses the revelation of probiotics and their mechanism of action is beneficial to conclude the efficiency of bacterial therapy in recent SARS-CoV-2 viral infections. Currently, we are frightened by the predominant pandemic era, COVID-19, with highly rapid spread and mortality. The COVID-19 agents, the newly developed SARS-CoV-2 variants, have been revealed to increase inflammatory responses that are directly correlated with the severity of symptoms and inpatient time. Though the benefits of drugs and vaccines for dealing with viral infections have been validated, their efficacy may be restricted by variations in viral inhabitants, making it more challenging to employ a practical method to inhibit viral infections. These observations and limited new information substantiate probiotics' effectiveness on SARS-CoV-2 disease. Previously established antiviral properties of probiotics against diverse respiratory viruses might be reflected in an alternative amelioration to prevent COVID-19 disease. The probiotic application is a safe and available corresponding medicine against COVID-19 disease.
Acknowledgements
The authors thank The Director, Dr Sridevi A Singh, CSIR- Central Food Technological Research Institute, Mysuru, India for the facilities and encouragement to write the article. Mousumi Ray would like to thank ICMR, New Delhi for providing the ICMR RA fellowship. Ashwini M would like to thank DST, New Delhi for the award of the WOS-B fellowship.
Author contributions
MR and PH produced the idea for the review article; MR and AM performed the literature survey, and critically revised and drafted the review article. MR and AM prepared Figs. 1–2. All authors reviewed the manuscript.
Funding
No external funding was used in the preparation of this review article.
Data availability
Not applicable.
Declarations
Conflict of interest
Mousumi Ray, Ashwini M and Prakash M Halami declare that there are no potential conflicts of interest that might be relevant to the contents of this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Aanouz I, Belhassan A, El-Khatabi K, Lakhlifi T, El-Ldrissi M, Bouachrine M (2020) Moroccan medicinal plants as inhibitors against SARS-CoV-2 main protease: computational investigations. J Biomol Struct Dyn. 39(8):2971–9. 10. 1080/07391.102.2020.17587.90 [DOI] [PMC free article] [PubMed]
- Abt MC, Osborne LC, Monticelli LA, Doering TA, Alenghat T, Sonnenberg GF, Paley MA, Antenus M, Williams KL, Erikson J, Wherry EJ. Commensal bacteria calibrate the activation threshold of innate antiviral immunity. Immunity. 2012;37(1):158–170. doi: 10.1016/j.immuni.2012.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AB Biotics SA (2020) Efficacy of L. plantarum and P. acidilactici in adults with SARS-CoV-2 and COVID19. ClinicalTrials.gov; 16/08/2020; TrialID: NCT04517422
- Al Kassaa I (2016) Antiviral probiotics: a new concept in medical sciences. In New Insights on Antiviral Probiotics. 1–46. Springer, Cham. 10.1007/978-3-319-49688-7_1
- Albarracin L, Kobayashi H, Iida H, Sato N, Nochi T, Aso H, Salva S, Alvarez S, Kitazawa H, Villena J. Transcriptomic analysis of the innate antiviral immune response in porcine intestinal epithelial cells: influence of immunobiotic lactobacilli. Front Immunol. 2017;8:57. doi: 10.3389/fimmu.2017.00057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antunes AE, Vinderola G, Xavier-Santos D, Sivieri K (2020) Potential contribution of beneficial microbes to face the COVID-19 pandemic. Food Res Int. 136:109577. 10.1016/j.foodres.2020.109577 [DOI] [PMC free article] [PubMed]
- Anwar F, Altayb HN, Al-Abbasi FA, Al-Malki AL, Kamal MA, Kumar V (2020) Antiviral effects of probiotic metabolites on COVID-19. J Biomol Struct Dyn. 39(11):4175–4184. 10.1080/07391.102.2020.17751.23 [DOI] [PMC free article] [PubMed]
- Araujo GV, Oliveira Junior MH, Peixoto DM, Sarinho ES. Probiotics for the treatment of upper and lower respiratory-tract infections in children: systematic review based on randomized clinical trials. J Pediatr. 2015;91(5):413–427. doi: 10.1016/j.jped.2015.03.002. [DOI] [PubMed] [Google Scholar]
- Arroyo R, Martin V, Maldonado A, Jimenez E, Fernandez L, Rodriguez JM. Treatment of infectious mastitis during lactation: antibiotics versus oral administration of lactobacilli isolated from breast milk. Clin Infect Dis. 2010;50(12):1551–1558. doi: 10.1086/652763. [DOI] [PubMed] [Google Scholar]
- Aziz M, Fatima R, Assaly R (2020) Elevated interleukin-6 and severe COVID-19: a meta-analysis, J Med Virol 10.1002/jmv.25948 [DOI] [PMC free article] [PubMed]
- Baud D, Dimopoulou Agri V, Gibson GR, Reid G, Giannoni E. Using probiotics to flatten the curve of coronavirus disease COVID-2019 pandemic. Front Public Health. 2020;8:186. doi: 10.3389/fpubh.2020.00186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belizario JE, Faintuch J (2018) Microbiome and gut dysbiosis metabolic interaction in infection. Springer, Berlin, pp 459–476. 10.1007/978-3-319-74932-7_13
- Biosearch SA (2020). Evaluation of the probiotic Lactobacillus coryniformis K8 on COVID-19 prevention in healthcare workers. ClinicalTrials.gov; 27/04/2020; TrialID: NCT04366180
- Boncristiani HF, Criado MF, Arruda E (2009) Respiratory viruses. Encyclopedia Microbiol. 10.1016/B978-01237.3944-5. 00314-X
- Both E, ´ Gy¨orgy E, Abrah´am B, L´anyi S (2011) Beneficial effects of probiotic microorganisms, a review. Acta Univ Sapientiae, Aliment. 4: 44–58
- Bozkurt HS, Quigley EM (2019) Bifidobacteria and mucosal associated invariant T (MAIT) cells: a new approach to colorectal cancer prevention? Gastrointestinal Dis 1(2):266–272. 10.3390/gidisord1020022
- Bozkurt HS, Quigley EM. The probiotic Bifidobacterium in the management of Coronavirus: a theoretical basis. Int J Immuno Pathol Pharmacol. 2020;34:2058738420961304. doi: 10.1177/2058738420961304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budding A, Sieswerda E, Wintermans B, Bos M (2020) An age dependent pharyngeal microbiota signature associated with SARS-CoV-2 infection. Available at SSRN 3582780
- Canani RB, Di Costanzo M, Leone L, Pedata M, Meli R, Calignano A (2011) Potential beneficial effects of butyrate in intestinal and extraintestinal diseases. World J Gastroenterol 17(12):1519. 10.3748/wjg.v17.i12.1519 [DOI] [PMC free article] [PubMed]
- Chang CS, Kao CY. Current understanding of the gut microbiota shaping mechanisms. J Biomed Sci. 2019;26(1):59. doi: 10.1186/s12929-019-0554-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- China Challenges for Global Health Governance JAMA-J. Am Med Assoc. 2020;323(8):709–710. doi: 10.1001/jama.2020.1097. [DOI] [PubMed] [Google Scholar]
- Chiu L, Bazin T, Truchetet M-E, Schaeverbeke T, Delhaes L, Pradeu T. Protective microbiota: from localized to long reaching co-immunity. Front Immunol. 2017;8:1678. doi: 10.3389/fimmu.2017.01678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ClinicalTrials.gov (2020) Efficacy of Intranasal Probiotic Treatment to Reduce Severity of Symptoms in COVID19 Infection. https://clinicaltrials.gov/ct2/show/results/NCT04458519
- d’Ettorre G, Ceccarelli G, Marazzato M, Campagna G, Pinacchio C, Alessandri F, Ruberto F, Rossi G, Celani L, Scagnolari C. Challenges in the management of SARS-CoV2 infection: the role of oral bacteriotherapy as complementary therapeutic strategy to avoid the progression of COVID-19. Front Med. 2020;7:389. doi: 10.3389/fmed.2020.00389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darbandi A, Asadi A, Ghanavati R, Afifirad R, Emamie AD, Talebi M (2021) The effect of probiotics on respiratory tract infection with special emphasis on COVID-19: Systemic review 2010–20. Int J Infect Dis 105:91–104. 10.1016%2Fj.ijid.2021.02.011 [DOI] [PMC free article] [PubMed]
- Davidson S, Kaiko G, Loh Z, Lalwani A, Zhang V, Spann K, Foo SY, Hansbro N, Uematsu S, Akira S, Matthaei KI. Plasmacytoid dendritic cells promote host defense against acute pneumovirus infection via the TLR7–MyD88-dependent signalling pathway. J Immunol. 2011;186(10):5938–5948. doi: 10.4049/jimmunol.1002635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Pierro F (2020) A possible probiotic (S. salivarius K12) approach to improve oral and lung microbiotas and raise defenses against SAR S-CoV-2. Minerva Med. 111(3):281–283. 10.23736/S0026-4806.20.06570-2. [DOI] [PubMed]
- de Vrese M, Winkler P, Rautenberg P, Harder T, Noah C, Laue C, Ott S, Hampe J, Schreiber S, Heller K, Schrezenmeir J (2005) Effect of Lactobacillus gasseri PA 16/8, Bifidobacterium longum SP 07/3, B. bifidum MF 20/5 on common cold episodes: a double blind, randomized, controlled trial. Clin Nutr. 24(4):481–91. 10.1016/j.clnu.2005.02.006 [DOI] [PubMed]
- de Wit E, van Doremalen N, Falzarano D, Munster VJ. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol. 2016;14(8):523–534. doi: 10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Din AU, Mazhar M, Waseem M, Ahmad W, Bibi A, Hassan A, Ali N, Gang W, Qian G, Ullah R, Shah T, Ullah M, Khan I, Nisar MF, Wu J (2021) SARS-CoV-2 microbiome dysbiosis linked disorders and possible probiotics role. Biomed. Pharmacother. 133. 10.1016/j.biopha.2020.110947 [DOI] [PMC free article] [PubMed]
- EFSA (2016) Panel on Dietetic Products, Nutrition and Allergies (NDA). Guidance on the scientific requirements for health claims related to the immune system, the gastrointestinal tract and defence against pathogenic microorganisms. 14(1):4369.10.2903/j.efsa.2016.4369
- Enaud R, Prevel R, Ciarlo E, Beaufils F, Wieërs G, Guery B, Delhaes L. The gut-lung axis in health and respiratory diseases: a place for inter-organ and inter-kingdom crosstalks. Front Cell Infect Microbiol. 2020;10:9. doi: 10.3389/fcimb.2020.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettinger G, MacDonald K, Reid G, Burton JP. The influence of the human microbiome and probiotics on cardiovascular health. Gut Microbes. 2014;5(6):719–728. doi: 10.4161/19490976.2014.983775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan Y-Y, Huang Z-T, Li L, Wu M-H, Yu T, Koup RA, Bailer RT, Wu C-Y. Characterization of SARS-CoV-specific memory T cells from recovered individuals 4 years after infection. Adv Virol. 2009;154(7):1093–1099. doi: 10.1007/s00705-009-0409-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan L, Jiang S, Yang X, Wang Z, Yang C (2020) COVID-19 drug treatment in China. Curr Pharmacol Rep 6(4):146–154. 10.1007%2Fs40495-020-00218-5 [DOI] [PMC free article] [PubMed]
- FAO/WHO (2001) Evaluation of health and nutritional properties of powder milk and live lactic acid bacteria. Report from FAO/WHO. 1–4
- Feng Z, Wang Y, Qi W (2020) The small intestine, an under estimated site of SARS-CoV-2 infection: from red queen effect to probiotics. Preprints. 10.20944/preprints202003.0161.v1
- Fooks LJ, Gibson GR. Probiotics as modulators of the gut flora. Br J Nutr. 2002;88:S39–S49. doi: 10.1079/BJN2002628. [DOI] [PubMed] [Google Scholar]
- Gao Q, Bao L, Mao H, Wang L, Xu K, Yang M, Li Y, Zhu L, Wang N, Lv Z (2020a) Development of an inactivated vaccine candidate for SARS-CoV-2. Science. 369(6499):77–81. 10.1126/science.abc1932 [DOI] [PMC free article] [PubMed]
- Gao QY, Chen YX, Fang JY. (2020b) 2019 Novel coronavirus infection and gastrointestinal tract. J Dig Dis. 12:3. 10.1111/1751-2980.12851. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- Gombart AF, Pierre A, Maggini S. A review of micronutrients and the immune system-working in harmony to reduce the risk of infection. Nutrients. 2020;12(1):236. doi: 10.3390/nu12010236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorbalenya AE, Baker SC, Baric RS, de Groot RJ, Drosten C, Gulyaeva AA, Haagmans BL, Lauber C, Leontovich AM, Neuman BW, Penzar D, Perlman S, Poon LLM, Samborskiy DV, Sidorov IA, Sola I, J. Ziebuhr, (2020) Coronaviridae Study Group of the International Committee on Taxonomy of viruses. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol 5 (4): 536–544. 10.1038/s41564-020-0695-z [DOI] [PMC free article] [PubMed]
- Goto Y, Uematsu S, Kiyono H. Epithelial glycosylation in gut homeostasis and inflammation. Nat Immunol. 2016;17(11):1244–1251. doi: 10.1038/ni.3587. [DOI] [PubMed] [Google Scholar]
- Guillemard E, Tondu F, Lacoin F, Schrezenmeir J. Consumption of a fermented dairy product containing the probiotic Lactobacillus casei DN-114001 reduces the duration of respiratory infections in the elderly in a randomised controlled trial. Br J Nutr. 2010;103(1):58–68. doi: 10.1017/S0007114509991395. [DOI] [PubMed] [Google Scholar]
- Gutiérrez-Castrellón P, Gandara-Martí T, Abreu AT, Nieto-Rufino CD, López-Orduña E, Jiménez-Escobar I, Espadaler-Mazo J (2021) Efficacy and safety of novel probiotic formulation in adult Covid19 outpatients: a randomized, placebo-controlled clinical trial. medRxiv, 2021–05. 10.1101/2021.05.20.21256954
- Hajavi J, Esmaeili SA, Varasteh AR, Vazini H, Atabati H, Mardani F, Momtazi-Borojeni AA, Hashemi M, Sankian M, Sahebkar A. The immunomodulatory role of probiotics in allergy therapy. J Cell Physiol. 2019;234(3):2386–2398. doi: 10.1002/jcp.27263. [DOI] [PubMed] [Google Scholar]
- Hajeer AH, Balkhy H, Johani S, Yousef MZ, Arabi Y (2016) Association of human leukocyte antigen class II alleles with severe Middle East respiratory syndrome-coronavirus infection. Ann. Thorac. Med. 11(3):211. 10.4103/1817-1737.185756 [DOI] [PMC free article] [PubMed]
- Hanada S, Pirzadeh M, Carver KY, Deng JC (2018) Respiratory viral infection-induced microbiome alterations and secondary bacterial pneumonia. Front Immunol. 9:2640. 10.3389/fimmu.2018.02640 [DOI] [PMC free article] [PubMed]
- Hao Q, Dong BR, Wu T (2015) Probiotics for preventing acute upper respiratory tract infections. Cochrane database of systematic reviews. 9. Art. No.: CD006895 10.1002/14651858.CD006895.pub3 [DOI] [PubMed]
- He Y, Wen Q, Yao F, Xu D, Huang Y, Wang J. Gut–lung axis: The microbial contributions and clinical implications. Crit Rev Microbiol. 2017;43(1):81–95. doi: 10.1080/1040841X.2016.1176988. [DOI] [PubMed] [Google Scholar]
- Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, Morelli L, Canani RB, Flint HJ, Salminen S (2014) Expert consensus document: the international scientific association for probiotics and prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol 11:506–514. http://www.nature.com/doifinder/10.1038/nrgastro.2014.66 [DOI] [PubMed]
- Hojsak I, Snovak N, Abdović S, Szajewska H, Misak Z, Kolacek S (2010) Lactobacillus GG in the prevention of gastrointestinal and respiratory tract infections in children who attend day care centers: a randomized, double-blind, placebo-controlled trial. Clin Nutr 29(3):312–316. 10.1016/j.clnu.2009.09.008 [DOI] [PubMed]
- Hu J, Zhang L, Lin W, Tang W, Chan FKL, Ng SC. Review article: probiotics, prebiotics and dietary approaches during COVID-19 pandemic. Trends Food Sci Technol. 2021;108:187–196. doi: 10.1016/j.tifs.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu X, Zhang H, Lu H, Qian G, Lv L, Zhang C, Guo J, Jiang H, Zheng B, Yang F, Gu S (2016) The effect of probiotic treatment on patients infected with the H7N9 influenza virus. PloS One. 11(3):e0151976. 10.1371/journal.pone.0151976 [DOI] [PMC free article] [PubMed]
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China the Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung YP, Lee CC, Lee JC, Tsai PJ, Ko WC (2021). Gut dysbiosis during COVID-19 and potential effect of probiotics. Microorganisms 9(8):1605. 10.3390%2Fmicroorganisms9081605 [DOI] [PMC free article] [PubMed]
- HwaMei Hospital UoCAoS (2020) Evaluation of the effect of taking Newgen beta-gluten probiotic composite powder to nutrition intervention of patients with novel coronavirus pneumonia (COVID-19). University of Chinese Academy of Sciences. ChiCTR; TrialID: ChiCTR2000030897
- Jiang X, Hou X, Tang L, Jiang Y, Ma G, Li Y. A phase trial of the oral Lactobacillus casei vaccine polarizes Th2 cell immunity against transmissible gastroenteritis coronavirus infection. Appl Microbiol Biotechnol. 2016;100(17):7457–7469. doi: 10.1007/s00253-016-7424-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin X, Lian JS, Hu JH, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69(6):1002–1009. doi: 10.1136/gutjnl-2020-320926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanauchi O, Andoh A, AbuBakar S, Yamamoto N. Probiotics and paraprobiotics in viral infection: clinical application and effects on the innate and acquired immune systems. Curr Pharm Des. 2018;24(6):710–717. doi: 10.2174/1381612824666180116163411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawahara T, Takahashi T, Oishi K, Tanaka H, Masuda M, Takahashi S, Takano M, Kawakami T, Fukushima K, Kanazawa H, Suzuki T. Consecutive oral administration of Bifidobacterium longum MM-2 improves the defense system against influenza virus infection by enhancing natural killer cell activity in amurine model. Microbiol Immunol. 2015;59(1):1–12. doi: 10.1111/1348-0421.12210. [DOI] [PubMed] [Google Scholar]
- Kim SR, Kim HJ, Im Kim D, Lee KB, Park HJ, Jeong JS, Cho SH, Lee YC (2015) Blockade of interplay between IL-17A and endoplasmic reticulum stress attenuates LPS-induced lung injury. Theranostics 5(12):1343. 10.7150%2Fthno.11685 [DOI] [PMC free article] [PubMed]
- King S, Glanville J, Sanders ME, Fitzgerald A, Varley D. Effectiveness of probiotics on the duration of illness in healthy children and adults who develop common acute respiratory infectious conditions: a systematic review and meta-analysis. Br J Nutr. 2014;112(1):41–54. doi: 10.1017/S0007114514000075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korea Biomedical Review (2020) Korean researchers found substance inhibiting COVID-19. https://www.koreabiomed.com/news/articleView.html?idxno=7744
- Kumpu M, Lehtoranta L, Roivainen M, Rönkkö E, Ziegler T, Söderlund-Venermo M, Kautiainen H, Järvenpää S, Kekkonen R, Hatakka K. The use of the probiotic Lactobacillus rhamnosus GG and viral findings in the nasopharynx of children attending day care. J Med Virol. 2013;85(9):1632–1638. doi: 10.1002/jmv.23623. [DOI] [PubMed] [Google Scholar]
- Lehtoranta L, Pitkaranta A, Korpela R. Probiotics in respiratory virus infections. Euro J Clin Microbiol Infect Dis. 2014;33(8):1289–1302. doi: 10.1007/s10096-014-2086-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei W-T, Shih P-C, Liu S-J, Lin C-Y, Yeh T-L. Effect of probiotics and prebiotics on immune response to influenza vaccination in adults: a systematic review and meta-analysis of randomized controlled trials. Nutrients. 2017;9(11):1175. doi: 10.3390/nu9111175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li B, Zheng J, Zhang X, Hong S. Probiotic Lactobacillus casei Shirota improves efficacy of amoxicillin-sulbactam against childhood fast breathing pneumonia in a randomized placebo-controlled double blind clinical study. J Clin Biochem Nutr. 2018;63(3):233–237. doi: 10.3164/jcbn.17-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Geng M, Peng Y, Meng L, Lu S. Molecular immune pathogenesis and diagnosis of COVID-19. J Pharmaceutical Anal. 2020;10(2):102–108. doi: 10.1016/j.jpha.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li G, Chen X, Xu A (2003) Profile of specific antibodies to the SARS-associated coronavirus. N Engl J Med 349:508–509. 10.1056/NEJM200307313490520 [DOI] [PubMed]
- Li Q, Cheng F, Xu A, Su Y, Cai X, Zeng F, Zhang Y (2021) The role of probiotics in coronavirus disease-19 infection in Wuhan: A retrospective study of 311 severe patients. Int. Immunopharmacol 95:107531. 10.1016/j.intimp.2021.107531 [DOI] [PMC free article] [PubMed]
- Lin J-S, Chiu Y-H, Lin N-T, Chu C-H, Huang K-C, Liao K-W, Peng K-C. Different effects of probiotic species/strains on infections in preschool children: a double-blind, randomized, controlled study. Vaccine. 2009;27(7):1073–1079. doi: 10.1016/j.vaccine.2008.11.114. [DOI] [PubMed] [Google Scholar]
- Lin L, Jiang X, Zhang Z, Huang S, Zhang Z, Fang Z, et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 2020;69(6):997–1001. doi: 10.1136/gutjnl-2020-321013. [DOI] [PubMed] [Google Scholar]
- Liu W, Ouyang X, Yang J, Liu J, LiQ GuY, Fukata M, Lin T, He JC, Abreu M. AP-1 activated by toll-like receptors regulates expression of IL-23 p19. J Biol Chem. 2009;284(36):24006–24016. doi: 10.1074/jbc.M109.025528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu M, Zhong Y, Chen J, Liu Y, Tang C, Wang X, Zhang Y, Wang P, Logan SM, Chen W. Oral immunization of mice with a multivalent therapeutic subunit vaccine protects against Helicobacter pylori infection. Vaccine. 2020;38(14):303–341. doi: 10.1016/j.vaccine.2020.02.036. [DOI] [PubMed] [Google Scholar]
- Liu Y-S, Liu Q, Jiang Y-L, Yang W-T, Huang H-B, Shi C-W, Yang G-L, Wang C-F. Surface-displayed porcine IFN-λ3 in Lactobacillus plantarum inhibits porcine enteric coronavirus infection of porcine intestinal epithelial cells. J Microbiol Biotechnol. 2020;30(4):515–525. doi: 10.4014/jmb.1909.09041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S, Hu P, Du X, Zhou T, Pei X. Lactobacillus rhamnosus GG supplementation for preventing respiratory infections in children: a meta-analysis of randomized, placebo-controlled trials. Indian pediatrics 50(4):377–81. 10.1007/s13312-013-0123-z [DOI] [PubMed]
- Luoto R, Ruuskanen O, Waris M, Kalliomäki M, Salminen S, Isolauri E. Prebiotic and probiotic supplementation prevents rhinovirus infections in preterm infants: a randomized, placebo-controlled trial. J Allergy Clin Immunol. 2014;133(2):405–413. doi: 10.1016/j.jaci.2013.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma WT, Pang M, Fan Q-L, Chen D-K. The commensal microbiota and viral infection: a comprehensive review. Front Immunol. 2019;10:1551. doi: 10.3389/fimmu.2019.01551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maassen CB, Boersma WJ, van Holten-Neelen C, Claassen E, Laman JD. Growth phase of orally administered Lactobacillus strains differentially affects IgG1/IgG2a ratio for soluble antigens: implications for vaccine development. Vaccine. 2003;21(21–22):2751–2757. doi: 10.1016/S0264-410X(03)00220-2. [DOI] [PubMed] [Google Scholar]
- Mahooti M, Mohammad Miri S, Abdolalipour E, Ghaemi A (2020) The immunomodulatory effects of probiotics on respiratory viral infections: A hint for COVID-19 treatment? Microb. Pathog 148:104452. 10.1016/j.micpath.2020.104452 [DOI] [PMC free article] [PubMed]
- Makino S, Ikegami S, Kume A, Horiuchi H, Sasaki H, Orii N (2010) Reducing the risk of infection in the elderly by dietary intake of yoghurt fermented with Lactobacillus delbrueckii ssp. bulgaricus OLL1073R-1. Br J Nutr 104(7):998–1006. [DOI] [PubMed]
- Malemud CJ (2018) Immunomodulators in Autoimmunity and Viral Infections. J Clin Cell Immunol 9(1). 10.4172/2155-9899.1000537
- Mirzaei R, Attar A, Papizadeh S, et al. The emerging role of probiotics as a mitigation strategy against coronavirus disease 2019 (COVID-19) Arch. Virol. 2021;166:1819–1840. doi: 10.1007/s00705-021-05036-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohamadzadeh M, Olson S, Kalina WV, Ruthel G, Demmin GL, Warfield KL, Bavari S, Klaenhammer TR. Lactobacilli activate human dendritic cells that skew T cells toward T helper 1 polarization. Proc Natl Acad Sci. 2005;102(8):2880–2885. doi: 10.1073/pnas.0500098102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morais AH, Passos TS, Maciel BL, da Silva-Maia JK. Can probiotics and diet promote beneficial immune modulation and purine control in coronavirus infection? Nutrients. 2020;12(6):1737. doi: 10.3390/nu12061737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortaz E, Adcock IM, Folkerts G, Barnes PJ, Paul Vos A, Garssen J (2013) Probiotics in the management of lung diseases. Mediat Inflamm. 2013. 10.1155/2013/751068 [DOI] [PMC free article] [PubMed]
- Namba K, Hatano M, Yaeshima T, Takase M, Suzuki K. Effects of Bifidobacterium longum BB536 administration on influenza infection, influenza vaccine antibody titer, and cell-mediated immunity in the elderly. Biosci Biotechnol Biochem. 2010;74(5):939–945. doi: 10.1271/bbb.90749. [DOI] [PubMed] [Google Scholar]
- Natarajan N, Pluznick JL. From microbe to man: The role of microbial short chain fatty acid metabolites in host cell biology. Am J Physiol—Cell Physiol. 2014;307(11):C979–C985. doi: 10.1152/ajpcell.00228.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neish AS. Mucosal immunity and the microbiome. Ann Am Thorac Soc. 2014;11(1):S28–S32. doi: 10.1513/AnnalsATS.201306-161MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen QV, Chong LC, Hor YY, Lew LC, Rather IA, Choi SB (2022) Role of probiotics in the management of COVID-19: A computational perspective. Nutrients. 14(2):274. 10.3390%2Fnu14020274 [DOI] [PMC free article] [PubMed]
- O’Toole PW, Jeffery IB (2015) Gut microbiota and aging. Science. 350(6265):1214–1215. 10.1126/science.aac8469 [DOI] [PubMed]
- Oeser K, Maxeiner J, Symowski C, Stassen M, Voehringer D. T cells are the critical source of IL-4/IL-13 in a mouse model of allergic asthma. Allergy Eur J Allergy Clin Immunol. 2015;70(11):1440–1449. doi: 10.1111/all.12705. [DOI] [PubMed] [Google Scholar]
- Oliva S, Nardo DG, Ferrari F, Mallardo S, Rossi P, Patrizi G, Cucchiara S, Stronati L. Randomised clinical trial: the effectiveness of Lactobacillus reuteri ATCC 55730 rectal enema in children with active distal ulcerative colitis. Aliment Pharmacol Ther. 2012;35(3):327–334. doi: 10.1111/j.1365-2036.2011.04939.x. [DOI] [PubMed] [Google Scholar]
- Olivares M, Díaz-Ropero MP, Sierra S, Lara-Villoslada F, Fonolla ´ J, Navas M, et al., (2007) Oral intake of Lactobacillus fermentum CECT5716 enhances the effects of influenza vaccination. Nutrition 23(3):254–260. 10.1016/j.nut.2007.01.004 [DOI] [PubMed]
- Pang IK, Iwasaki A. Control of antiviral immunity by pattern recognition and the microbiome. Immunol Rev. 2012;245(1):209–226. doi: 10.1111/j.1600-065X.2011.01073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park DM, Bae JH, Kim MS, Kim H, Dal Kang S, Shim S, Lee D, Seo JH, Kang H, Han NS. Suitability of Lactobacillus plantarum SPC-SNU 72–2 as a probiotic starter for sourdough fermentation. J Microbiol Biotechnol. 2019;29(11):1729–1738. doi: 10.4014/jmb.1907.07039. [DOI] [PubMed] [Google Scholar]
- Park M-K, Vu N, Kwon Y-M, Lee Y-T, Yoo S, Cho Y-H, Hong S-M, Hwang HS, Ko E-J, Jung Y-J (2013) Lactobacillus plantarum DK119 as a probiotic confers protection against influenza virus by modulating innate immunity. PloS one 8(10):e75368. 10.1371/journal.pone.0075368 [DOI] [PMC free article] [PubMed]
- Pattemore PK, Jennings LC (2008) Epidemiology of respiratory infections. Pediatr Respir Med 15(3):184–194. 10. 1016/B978-03230 4048–8.50035–9
- Perez-Lopez A, Behnsen J, Nuccio S-P, Raffatellu M. Mucosal immunity to pathogenic intestinal bacteria. Nat Rev Immunol. 2016;16(3):135–148. doi: 10.1038/nri.2015.17. [DOI] [PubMed] [Google Scholar]
- Pimentel-Nunes P, Soares JB, Roncon-Albuquerque R, Jr, Dinis-Ribeiro M, Leite-Moreira AF. Toll-like receptors as therapeutic targets in gastrointestinal diseases. Expert Opin Ther Targets. 2010;14(4):347–368. doi: 10.1517/14728221003642027. [DOI] [PubMed] [Google Scholar]
- Prompetchara E, Ketloy C, Palaga T (2020) Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic. Asian Pacific J allergy Immunol. 38(1):1–9. 10.12932/AP-200220-0772 [DOI] [PubMed]
- Pu F, Guo Y, Li M, Zhu H, Wang S, Shen X, He M, Huang C, He F (2017) Yogurt supplemented with probiotics can protect the healthy elderly from respiratory infections: a randomized controlled open-label trial. Clin Interv Aging 12:1223–1231. 10.2147/CIA.S141518 [DOI] [PMC free article] [PubMed]
- Qiu T, Liang S, Dabbous M, Wang Y, Han R, Toumi M (2020) Chinese guidelines related to novel coronavirus pneumonia. j mark access health policy 8(1):1818446. 10.1080%2F20016689.2020.1818446 [DOI] [PMC free article] [PubMed]
- Rathi A, Jadhav SB, Shah N. A randomized controlled trial of the efficacy of systemic enzymes and probiotics in the resolution of post-COVID fatigue. Medicines. 2021;8(9):47. doi: 10.3390/medicines8090047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisinger A, Stadlbauer V. Letter on synbiotics modulate gut microbiota and reduce enteritis and ventilator-associated pneumonia in patients with sepsis: a randomized controlled trial. Crit Care. 2019;23(1):56. doi: 10.1186/s13054-019-2319-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren D, Li C, Qin Y, Yin R, Du S, Liu H, Zhang Y, Wang C, Rong F, Jin N (2015) Evaluation of immunomodulatory activity of two potential probiotic Lactobacillus strains by in vivo tests. Anaerobe 35(B):22–27. 10.1016/j.anaerobe.2015.06.008 [DOI] [PubMed]
- Rosa DD, Dias MMS, Grześkowiak ŁM, Reis SA, Conceição LL, Peluzio MDCG. Milk kefir: nutritional, microbiological and health benefits. Nutr Res Rev. 2017;30(1):82–96. doi: 10.1017/S0954422416000275. [DOI] [PubMed] [Google Scholar]
- Rosenberg HF, Domachowske JB. Inflammatory responses to respiratory syncytial virus (RSV) infection and the development of immunomodulatory pharmacotherapeutics. Curr Med Chem. 2012;19(10):1424–1431. doi: 10.2174/092986712799828346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothan HA, Byrareddy SN (2020) The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 109:102433. 10.1016/j.jaut.2020.102433 [DOI] [PMC free article] [PubMed]
- Schiavi E, Gleinser M, Molloy E, Groeger D, Frei R, Ferstl R, Rodriguez-Perez N, Ziegler M, Grant R, Moriarty TF. The surface-associated exopolysaccharide of Bifidobacterium longum 35624 plays an essential role in dampening host pro-inflammatory responses and repressing local TH17 responses. Appl Environ Microbiol. 2016;82(24):7185–7196. doi: 10.1128/AEM.02238-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seddik HA, Bendali F, Gancel F, Fliss I, Spano G, Drider D. Lactobacillus plantarum and its probiotic and food potentialities. Probiotics Antimicrobial Proteins. 2017;9(2):111–122. doi: 10.1007/s12602-017-9264-z. [DOI] [PubMed] [Google Scholar]
- Sencio V, Barthelemy A, Tavares LP, Machado MG, Soulard D, Cuinat C, et al. (2020) Gut dysbiosis during influenza contributes to pulmonary pneumococcal superinfection through altered short-chain fatty acid production. Cell Rep. 30(9):2934–47 e6. 10.1016/j.celrep.2020.02.013 [DOI] [PubMed]
- Shakoor S, Rao A, Shahid N, Yaqoob A, Samiullah T, Latif A, Tabassum B, Khan M, Shahid A, Husnain T (2019) Role of oral vaccines as an edible tool to prevent infectious diseases. Acta Virol 63(3):245–252. 10.4149/av_2019_301 [DOI] [PubMed]
- Shanghai 10th People’s Hospital TU (2020) A clinical study for probiotics in the regulation of intestinal function and microflora structure of novel coronavirus pneumonia (COVID-19)
- Sharma L, Riva A (2020) Intestinal Barrier Function in Health and Disease—Any Role of SARS-CoV-2? Microorganisms 8(11):1744. 10.3390/microorganisms8111744 [DOI] [PMC free article] [PubMed]
- Shoaib A, Xin L, Xin Y. Oral administration of Lactobacillus acidophilus alleviates exacerbations in Pseudomonas aeruginosa and Staphylococcus aureus pulmonary infections. Pak J Pharm Sci. 2019;32(4):1621–1630. [PubMed] [Google Scholar]
- Shukla SD, Budden KF, Neal R, Hansbro PM. Microbiome effects on immunity, health and disease in the lung. Clin Transl Immunol. 2017;6(3):e133–e212. doi: 10.1038/cti.2017.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Y, Qian J, Xu X, Tang Y, Xu W, Yang W, Jiang Y, Yang G, Ding Z, Cong Y. Dendritic cell-targeted recombinant-lactobacilli induce DC activation and elicit specific immune responses against G57 genotype of avian H9N2 influenza virus infection. Vet Microbiol. 2018;223:9–20. doi: 10.1016/j.vetmic.2018.07.009. [DOI] [PubMed] [Google Scholar]
- Sundararaman A, Ray M, Ravindra PV, Halami PM. Role of probiotics to combat viral infections with emphasis on COVID-19. Appl Microbiol Biotechnol. 2020;104:8089–8104. doi: 10.1007/s00253-020-10832-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taipale T, Pienih.kkinen K, Isolauri E, Larsen C, Brockmann E, Alanen P, Jokela J, S.derling E (2011) Bifidobacterium animalis subsp. lactis BB-12 in reducing the risk of infections in infancy. Br J Nutr 105(3):409–416. 10.1017/S0007114510003685 [DOI] [PubMed]
- Tang F, Quan Y, Xin Z-T, Wrammert J, Ma M-J, Lv H, Wang T-B, Yang H, Richardus JH, Liu W. Lack of peripheral memory B cell responses in recovered patients with severe acute respiratory syndrome: a 6-year follow-up study. J Immunol. 2011;186(12):7264–7268. doi: 10.4049/jimmunol.0903490. [DOI] [PubMed] [Google Scholar]
- Tapiovaara L, Pitkaranta A, Korpela R (2016) Probiotics and the upper respiratory tract-a review. Pediatric Infect Dis 1(3):100019. 10.4172/PIDO.100019
- Tortorici MA, Veesler D. Structural insights into coronavirus entry. Adv Virus Res Elsevier. 2019;105:93–116. doi: 10.1016/bs.aivir.2019.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner RB, Woodfolk JA, Borish L, Steinke JW, Patrie JT, Muehling LM, Lahtinen S, Lehtinen MJ. Effect of probiotic on innate inflammatory response and viral shedding in experimental rhinovirus infection–a randomised controlled trial. Benef Microbes. 2017;8(2):207–215. doi: 10.3920/BM2016.0160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unterholzner L, Bowie AG. The interplay between viruses and innate immune signalling: recent insights and therapeutic opportunities. Biochem Pharmacol. 2008;75(3):589–602. doi: 10.1016/j.bcp.2007.07.043. [DOI] [PubMed] [Google Scholar]
- Waki N, Matsumoto M, Fukui Y, Suganuma H. Effects of probiotic Lactobacillus brevis KB 290 on incidence of influenza infection among schoolchildren: an open- label pilot study. Lett Appl Microbiol. 2014;59(6):565–571. doi: 10.1111/lam.12340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B, Hylwka T, Smieja M, Surrette M, Bowdish DM, Loeb M. Probiotics to prevent respiratory infections in nursing homes: a pilot randomized controlled trial. J Am Geriatr Soc. 2018;66(7):1346–1352. doi: 10.1111/jgs.15396. [DOI] [PubMed] [Google Scholar]
- Wang S, Geng N, Zhou D, Qu Y, Shi M, Xu Y, Liu K, Liu Y, Liu J. Oral immunization of chickens with recombinant Lactobacillus plantarum vaccine against early ALV-J infection. Front Immunol. 2019;10:2299. doi: 10.3389/fimmu.2019.02299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M, Fu T, Hao J, Li L, Tian M, Jin N, Ren L, Li C. A recombinant Lactobacillus plantarum strain expressing the spike protein of SARS-CoV-2. Int J Biol Macromolecules. 2020;160(1):736–740. doi: 10.1016/j.ijbiomac.2020.05.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W, Tang J, Wei F. Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan. China J Med Virol. 2020;92(4):441–447. doi: 10.1002/jmv.25689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Li X, Ge T, Xiao Y, Liao Y, Cui Y, Zhang Y, Ho W, Yu G, Zhang T (2016) Probiotics for prevention and treatment of respiratory tract infections in children A systematic review and meta analysis of randomized controlled trials. Medicine 95(31):e4509. 10.1097/MD.0000000000004509 [DOI] [PMC free article] [PubMed]
- Wang F, Kream RM, Stefano GB (2020a) An evidence-based perspective on mRNA-SARS-CoV-2 vaccine development. Med Sci Monitor 26: e924700–924701. 10.12659%2FMSM.924700 [DOI] [PMC free article] [PubMed]
- West NP, Horn PL, Pyne DB, Gebski VJ, Lahtinen SJ, Fricker PA, Cripps AW. Probiotic supplementation for respiratory and gastrointestinal illness symptoms in healthy physically active individuals. Clin Nutr. 2014;33(4):581–587. doi: 10.1016/j.clnu.2013.10.002. [DOI] [PubMed] [Google Scholar]
- Wilder-Smith A. COVID-19 in comparison with other emerging viral diseases: risk of geographic spread via travel. Trop Dis Travel Med Vaccines. 2021;7:1–11. doi: 10.1186/s40794-020-00129-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S, Jiang ZY, Sun YF, Yu B, Chen J, Dai CQ, Wu XL, Tang XL, Chen XY. Microbiota regulates the TLR7 signaling pathway against respiratory tract influenza A virus infection. Curr Microbiol. 2013;67:414–422. doi: 10.1007/s00284-013-0380-z. [DOI] [PubMed] [Google Scholar]
- Wu D, Lewis ED, Pae M, Meydani SN. Nutritional Modulation of Immune Function: Analysis of Evidence, Mechanisms, and Clinical Relevance. Front Immunol. 2018;9:3160. doi: 10.3389/fimmu.2018.03160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu F, Xiao A, Zhang J, Gu X, Lee WL, Kauffman K, Hanage W, Matus M, Ghaeli N, Endo N, Duvallet C, Moniz K, Erickson T, Chai P, Thompson J, Alm E (2020) SARS-CoV-2 titers in wastewater are higher than expected from clinically confirmed cases.5(4):e00614–20. 10.1128/mSystems.00614-20 [DOI] [PMC free article] [PubMed]
- Xu K, Cai H, Shen Y, Ni Q, Chen Y, Hu S, Li J, Wang H, Yu L, Huang H. Management of corona virus disease-19 (COVID-19): the Zhejiang experience. J Zhejiang Univ (medical Science) 2020;49:1–12. doi: 10.3785/j.issn.1008-9292.2020.02.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto V, Bolanos JF, Fiallos J, Strand SE, Morris K, Shahrokhinia S, Cushing TR, Hopp L, Tiwari A, Hariri R, Sokolov R, Wheeler C, Kaushik A, Elsayegh A, Eliashiv D, Hedrick R, Jafari B, Johnson JP, Khorsandi M, Gonzalez N, Balakhani G, Lahiri S, Ghavidel K, Amaya M, Kloor H, Hussain N, Huang E, Cormier J, Wesson A, Wang JC, Yaghobian S, Khorrami P, Shamloo B, Moon C, Shadi P, Kateb B. COVID-19: review of a 21st century pandemic from etiology to neuro-psychiatric implications. J Alzheimers Dis. 2020;77(2):459–504. doi: 10.3233/JAD-200831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Z, Yang Z, Wang Y, Zhou F, Li S, Li C, Li L, Zhang W, Li X (2021) Recent advance of ACE2 and microbiota dysfunction in COVID-19 pathogenesis. Heliyon. 7(7):e07548. doi: 10.1016/j.heliyon.2021.e07548. PMID: 34296023; PMCID: PMC8270732 [DOI] [PMC free article] [PubMed]
- Zafar N, Aslam M A, Ali A, Khatoon A, Nazir A, Tanveer Q, Bilal M, Kanwar R, Qadeer A, Sikandar M, Zafar A (2020) Probiotics: Helpful for the prevention of COVID-19? Biomed. Res. Ther. 7(11):4086–4099. 10.15419/bmrat.v7i11.646
- Zelaya H, Alvarez S, Kitazawa H, Villena J. Respiratory antiviral immunity and immunobiotics: beneficial effects on inflammation-coagulation interaction during influenza virus infection. Front Immunol. 2016;7:633. doi: 10.3389/fimmu.2016.00633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng J, Wang CT, Zhang FS, Qi F, Wang SF, Ma S, Wu TJ, Tian H, Tian ZT, Zhang SL, Qu Y, Liu LY, Li YZ, Cui S, Zhao HL, Du QS, Ma Z, Li CH, Li Y, Si M, Chu YF, Meng M, Ren HS, Zhang JC, Jiang JJ, Ding M, Wang YP (2016) Effect of probiotics on the incidence of ventilator-associated pneumonia in critically ill patients: a randomized controlled multicenter tria. Intensive Care Med. 42 (6):1018–1028. 10.1007/s00134-016-4303-x [DOI] [PubMed]
- Zha L, Zhao H, Mohsen MO, Hong L, Zhou Y, Li Z, Yao C, Chen H, Liu X, Chang X (2020) Development of a COVID-19 vaccine based on the receptor binding domain displayed on virus-like particles. bioRxiv. 1:2020–05. 10.1101/2020.05.06.079830 [DOI] [PMC free article] [PubMed]
- Zhang L, Han H, Li X, Chen C, Xie X, Su G, Lai T (2021) Probiotics use is associated with improved clinical outcomes among hospitalized patients with COVID-19. Therap Adv Gastroenterol. 14:17562848211035670. 10.1177%2F17562848211035670 [DOI] [PMC free article] [PubMed]
- Zhang F (2020). Washed microbiota transplantation for patients with 2019-nCoV infection: a randomized, double-blind, placebo-controlled study. clinicaltrials. gov
- Ziegler CGK, Allon SJ, Nyquist SK, Mbano IM, Miao VN, Tzouanas CN, Cao Y, Yousif AS, Bals J, Hauser BM, Feldman J, Muus C, Wadsworth MH, Kazer SW, Hughes TK, Doran B, Gatter GJ, Vukovic M, Taliaferro F, Mead BE, Guo Z, Wang JP, Gras D, Plaisant M, Ansari M, Angelidis I, Adler H, Sucre JMS, Taylor CJ, Lin B, Waghray A, Mitsialis V, Dwyer DF, Buchheit KM, Boyce JA, Barrett NA, Laidlaw TM, Carroll SL, Colonna L, Tkachev V, Peterson CW, Yu A, Zheng HB, Gideon HP, Winchell CG, Lin PL, Bingle CD, Snapper SB, Kropski JA, Theis FJ, Schiller HB, Zaragosi LE, Barbry P, Leslie A, Kiem HP, Flynn JL, Fortune SM, Berger B, Finberg RW, Kean LS, Garber M, Schmidt AG, Lingwood D, Shalek AK, Ordovas-Montanes J. SARS-CoV-2 receptor ACE2 is an interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell. 2020;181(5):1016–1035.e19. doi: 10.1016/j.cell.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zolnikova O, Komkova I, Potskherashvili N, Trukhmanov A, Ivashkin V. Application of probiotics for acute respiratory tract infections. Italian J Med. 2018;12(1):32–38. doi: 10.4081/itjm.2018.931. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.