Abstract
Introduction
Laypeople should be trained in basic life support and traditional and innovative methodologies may help to obtain this goal. However, there is a knowledge gap about the ideal basic life support training methods. Smart glasses could have a role facilitating laypeople learning of basic life support.
Aim
To analyze the potential impact on basic life support learning of a very brief training supported by smart glasses video communication.
Methods
Twelve laypeople were basic life support tele-trained by means of smart glasses by an instructor in this pilot study. During training (assisted trough smart glasses) and after the training (unassisted) participants’ performance and quality of basic life support and automated external defibrillation procedure were assessed on a standardized simulated scenario.
Results
After the training all participants were able to deliver good quality basic life support, with results comparable to those obtained when real time remotely guided by the instructor through the smart glasses. Mean chest compression rate was significantly higher when not guided (113 /min vs. 103 /min, p = 0.001). When not assisted, the participants spent less time delivering the sequential basic life support steps than when assisted while training.
Conclusions
A very brief remote training supported by instructor and smart glasses seems to be an effective educational method that could facilitate basic life support learning by laypeople. This technology could be considered in cases where instructors are not locally available or in general in remote areas, providing basic internet connection is available. Smart glasses could also be useful for laypeople rolling-refreshers.
Keywords: Learning, Laypeople, Smart Glasses, Cardiac arrest, Resuscitation, Remote area, Telemedicine
Introduction
According to EuReCa TWO study, the overall incidence of out-of-hospital cardiorespiratory arrest where cardiopulmonary resuscitation (CPR) was attempted is 56 per 100,000 population per year (range: 21–91).1 In this prospective study, in which data from 28 European cities are analyzed, CPR was started before the arrival of emergency medical services in 58% of the cases, and the rate of survival was twice as high when CPR was started by a bystander as when was started by emergency medical services.1
Teaching basic life support (BLS) to the general population is key to improve bystander immediate resuscitation attempts and survival rates in the event of out-of-hospital cardiorespiratory arrest.1, 2 Several traditional educational methodologies have proven to be effective for laypeople to be competent by applying the BLS protocol, using the automated external defibrillation (AED), and performing quality resuscitation.3 According to the systematic review by González-Salvado et al., there is great heterogeneity in the research designs on BLS training in laypeople.3 There is an apparent advantage of instructor-led methods with the practice of resuscitation skills, there seems to be a trend towards short training sessions, and practically all the designs evaluate the protocol of BLS and the quality of resuscitation. However, the ideal methodology to learn and retain the knowledge and skills to act in the event of a cardiorespiratory arrest remains unknown.4 In order to achieve the goal that most people be trained and be able to resuscitate with enough quality, it seems necessary to explore new methodologies and technologies.5
Thus, in the 2021 guidelines of the European Resuscitation Guidelines (ERC) it is advised to use technology to improve education by teaching resuscitation and engaging as many learners as possible.4 The use of technology in BLS training programs can, for example, promote better resuscitation learning with the real-time feedback system,6 make learning more attractive, or make it possible for teaching to reach more remote places with telematic training.7, 8, 9, 10
Among the new communication technologies used in skills training we can find smart glasses. This wearable has features similar to a smartphone, for example, one can make a video call to communicate by audio and video with another person by connecting with his/her computer, tablet, or smartphone. Communication between student and teacher by video call with smart glasses has been used in the hospital setting to video assist a surgeon or to show a surgical procedure in the medical classroom,11, 12 or in the extra-hospital setting to video assist an unplanned childbirth.13 However, it is unknown if this type of communication with this wearable would be effective and interesting for teaching the BLS in an out-of-hospital setting with laypeople.
Therefore, our objective of this pilot study was to analyze the potential impact on BLS learning of very brief training based on experiencing a performance in simulated cardiac arrest and with the support of smart glasses video communication in laypersons.
Methods
Participants
Twelve University students of the Degree in Physical Activity and Sports Sciences were invited to participate as a convenient sample for this pilot study. To be included, it was necessary for participants not to have received BLS training for the two years prior to the study, nor have physical impediments to perform chest compressions, nor have vision or hearing problems incompatible with video call communication from smart glasses.
Each individual signed an informed consent before his/her voluntary participation. This study has been approved by the Ethics Committee for Clinical Research of the Catalan Council (reference number 026/CEICGC/2022).
Procedures and training
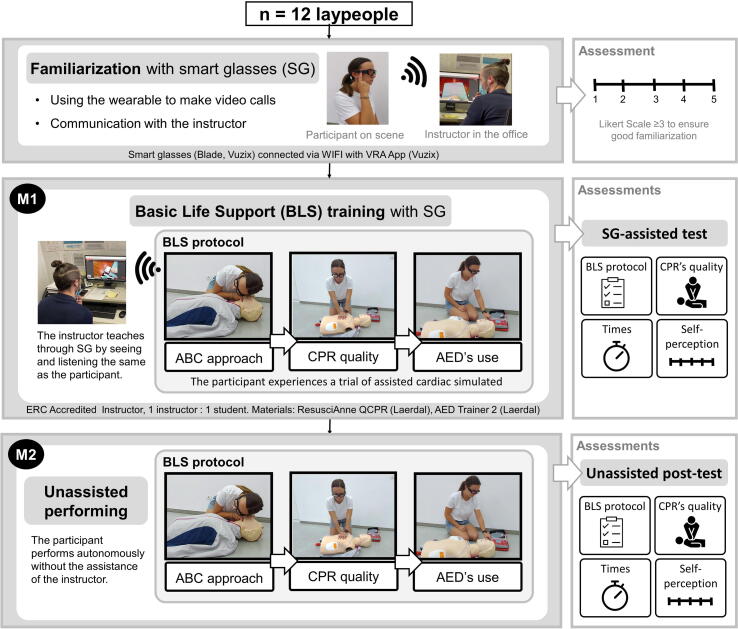
Each participant was familiarized with the smart glasses, then trained in a simulated cardiac arrest scenario with an instructor who taught them via video call using smart glasses, and then performed autonomously in a simulated cardiac arrest. The performance of each participant was evaluated twice: first test while training assisted with smart glasses (M1), and the second test once the training was finished as post-test without assistance of smart glasses (M2) (Fig. 1).
Fig. 1.
Participants' flowchart and study design scheme.
Familiarization with smart glasses and connectivity
Before the training, each participant became familiar with the basic functions of the smart glasses in their use of video calls (turn on glasses, enter the App, make calls, hang up/drop off video calls) in a short training < 5 minutes. A score of at least 3 points on a 5-point Likert scale was required after this training to ensure proper familiarization with the smart glasses.
The smart glasses (Vuzix Blade Upgraded, Vuzix, US) had the Vuzix Remote Assist App (VRA App) installed, which allows making video calls with another device, in this case with a laptop connected to the web page of the application (https://vra.vuzix.com). The smart glasses were connected via WIFI 4G as described in a previous study.13 The participant communicated with the instructor by video call with the smart glasses (voice and streaming the images captured by the front camera). The instructor could talk and view real-time video on his computer. The instructor was a member of the research team blinded to the study’s purpose.
BLS training
Each participant underwent BLS training in a simulation scenario. The training consisted of attending a simulated cardiac arrest with the remote assistance of an instructor in the role of an emergency medical services’ dispatcher. The instructor was tele-assisting based on the BLS protocol of the ERC.14 Being connected via video call with the smart glasses, the instructor could correct the student based on what he/she heard and saw through the smart glasses.
A member of the research team presented the following simulation training scenario: “This man has collapsed in front of you. He is this doll that's on the ground. You must act to the best of your ability and you have the help of an instructor from the emergency medical services who is seeing the same things you see. You can contact the instructor through the smart glasses you are wearing while making the video call as you already know”.
The training was carried out on a resuscitation manikin (Resusci Anne QCPR, Laerdal, Norway) connected to SimPad PLUS to record resuscitation quality (Laerdal, Norway). In the simulation, an investigator brought in the AED (AED trainer, Laerdal, Norway) when the participant completed two consecutive minutes of chest compressions.
Assessments and variables
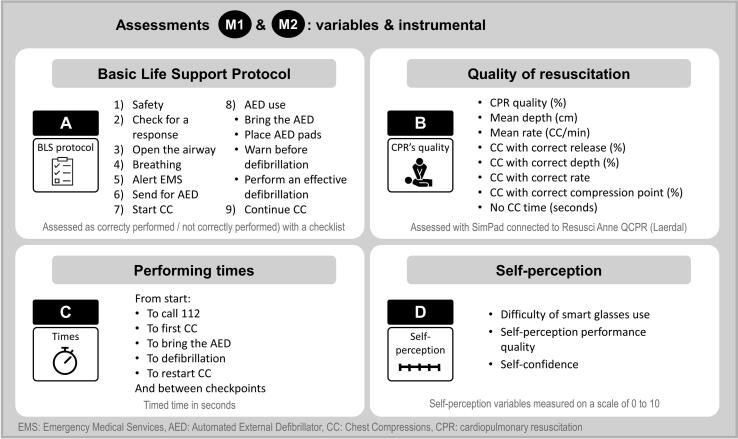
The evaluations of M1 (just while training with smart glasses) and M2 (unassisted alone post-test) recorded: A) the BLS performance protocol measured with a checklist and noting whether or not each step was carried out correctly (following the standards established by ERC in its guides published in 2021),14 B) quality of chest compressions for two consecutive minutes measured with the Simpad (Laerdal, Norway), C) performing times, and self-perception variables measured on a scale of 0 to 10 (Fig. 2).
Fig. 2.
Variables and measuring instruments of both assessments: M1 (just while training with smart glasses) and M2 (Unassisted post-test).
Data analysis
All analyses were performed with the IBM SPSS Statistics version 21 for Windows software (Armonk, NY, USA). Quantitative variables were described through measures of central tendency (median) and dispersion (interquartile range-IQR). The qualitative variables were described through absolute and relative frequencies. For the comparisons of the quantitative variables, the Wilcoxon’s signed ranked test or the Student’s t test were used, depending on the normality criteria (Shapiro-Wilk test). For the Effect Size, the Rosenthal's r test or the Cohen's d test were used respectively. To define the effect size, the following classification was used: < 0.2: Trivial / 0.2–0.5: Small / 0.5–0.8: Moderate / 0.8–1.3: Large / > 1.3: Very large.15, 16 For the comparisons of the qualitative variables, the McNemar test was used. The level of statistical significance was established when p < 0.05.
Results
Demographics
Participants had a median age of 23 years (IQR: 20–29), weight of 66 kg (IQR: 58–76), height of 170 cm (IQR: 166–177) and Body Mass Index of 22.5 kg/m2 (IQR: 21.9–24.6). 67% of the participants were men.
BLS protocol
The test carried out while the participants were trained thought the smart glasses (M1) showed how all or nearly all of them performed the steps of the BLS sequence following ERC guidelines (Table 1). That means that all participants did correctly ask for an AED, call 112, start chest compressions, bring the AED, bare victim’s chest, place AED pads correctly, perform an effective defibrillation, and restart chest compressions; all except one participant did correctly open victim’s airway, check victim’s breathing, and warn before defibrillation; and 9 out of 12 of them checked the victim’s response correctly. Otherwise, the test carried out after the training (M2 without assistance) showed that less participants than in M1 performed correctly the different steps of BLS sequence (Table 1). However, those differences were not statistically significant (p > 0.05). In M1 and M2, all the participants managed to make the call to 112, began the chest compressions and stripped the victim's chest before placing the AED when performing the Unassisted post-test. Only one of the participants did not use the AED or apply effective defibrillation in M2.
Table 1.
Performance of the BLS sequential steps by participants, while instructor-smart glasses assisted (M1) during training and when alone after the training (M2). (N = 12).
| M1: while training with smart glasses | M2: Unassisted post-test |
Significance | |
|---|---|---|---|
| N | N | ||
| Check victim’s response | 9 | 7 | p = 0.69 |
| Open victim’s airway | 11 | 8 | p = 0.25 |
| Check victim’s breathing | 11 | 10 | p = 1.00 |
| Ask for an AED | 12 | 9 | p = 0.25 |
| Call 112 | 12 | 12 | - |
| Start chest compressions | 12 | 12 | - |
| Bring the AED | 12 | 11 | p = 1.00 |
| Bare victim’s chest | 12 | 12 | - |
| Place AED pads | 12 | 11 | p = 1.00 |
| Warn before defibrillation | 11 | 7 | p = 0.13 |
| Perform an effective defibrillation | 12 | 11 | p = 1.00 |
| Restart chest compressions | 12 | 11 | p = 1.00 |
AED: Automated External Defibrillator. N: Absolute frequency.
Quality of resuscitation (chest compressions only)
The median and interquartile range of the variables related to the quality of chest compressions in M1 and M2 can be seen in Table 2. The median of the mean depth variable for both tests were around 4 cm (no chest compressions with good depth), the median of the mean rate variable was 103 chest compressions/min in M1 and 113 chest compressions/min in M2, and always with de hands placed in correct compression point (in M1 and M2). No significant differences were observed between M2 and M1 in CPR quality (4%; IQR: 0–50 vs 7%; IQR: 1–68) or in the rest of the CPR variables studied, except for the mean rate of CC, which was significantly lower in M1 than in M2 (M1: 103 chest compressions/min, IQR: 98–107; M2: 113 chest compressions/min, IQR: 107–122; p = 0.001; effect size = 1.52).
Table 2.
Quality of cardiopulmonary resuscitation (CPR) during assisted training with smart glasses (smart glasses-assisted) and post-test without assistance (N = 12).
| M1: while training with smart glasses |
M2: Unassisted post-test |
Significance (Effect size) |
|||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| Mean depth (cm) | 4.0 | (2.8–5.0) | 4.2 | (3.2–5.1) | p = 0.45* |
| Mean rate (CC/min) | 103 | (98–107) | 113 | (107–122) |
p = 0.001* (1.52)‡ |
| CC with correct release (%) | 24 | (1–79) | 33 | (7–92) | p = 0.61† |
| CC with correct depth (%) | 0 | (0–54) | 0 | (0–45) | p = 0.50† |
| CC with correct rate (%) | 66 | (34–87) | 81 | (31–97) | p = 0.61† |
| CC with correct compression point (%) | 100 | (1–100) | 100 | (18–100) | p = 0.29† |
| No CC time (in seconds) | 0.5 | (0.0–1.8) | 1.5 | (0.0–2.8) | p = 0.17† |
AED: Automated External Defibrillator; CC: Chest compressions. IQR: Interquartile range; † Wilcoxon’s signed ranked test (p < 0.05). * Student’s t test (p < 0.05) and ‡ Cohen’s d for Effect Size (in brackets).
Performing times
The median and interquartile range of the variables related to the performance times in M1 and M2 can be seen in Table 3. In M1, the time from start to call 112 was 35 seconds (IQR: 21–44), time to the first chest compression 124 seconds (IQR: 106–153), and the time to defibrillation 332 seconds (IQR: 319–372). Otherwise, in M2, the time from start to call 112 was 25 seconds (IQR: 15–63), to the first chest compression was 61 seconds (IQR: 48–78), and to defibrillation was 240 seconds (IQR: 233–262). There were no differences between M1 and M2 in the performing time from the start of the scenario until the call to 112, nor from the discharge of the AED to the restart of the chest compressions (Table 3). However, a significantly shorter time was observed in M1 to start the chest compressions (both from the start of the scenario and from the 112 call to the start of the chest compressions), to bring the AED (both from the start of the scenario and from finishing the chest compressions), to the defibrillation, and in the total time of the scenario that ended when restarting the chest compressions after the shock (Table 3). This last difference was approximately one and a half minutes between M2 (249 s; IQR: 241–270) and M1 (340 s; IQR: 324–381; p = 0.062; effect size = 0.62).
Table 3.
Performance times during M1 (smart glasses-assisted test while training) and M2 (unassisted post-test) (N = 12): times and checkpoints (in seconds).
| M1: while training with smart glasses |
M2: Unassisted post-test |
Significance (Effect Size) | |||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| From start to calling 112 | 35 | (21–44) | 25 | (15–63) | p = 0.78† |
| From calling 112 to CC | 91 | (74–116) | 25 | (9–35) |
p < 0.001* (3.38)‡ |
| From start to CC | 124 | (106–153) | 61 | (48–78) |
p < 0.001* (2.86)‡ |
| From start to bringing the AED | 244 | (229–273) | 182 | (169–198) | p = 0.004† (0.59)π |
| From bringing the AED to defibrillation | 95 | (80–103) | 62 | (53–71) | p < 0.001* (0.47)‡ |
| From start to defibrillation | 332 | (319–372) | 240 | (233–262) | p = 0.002† (0.62)π |
| From defibrillation to restarting CC | 8 | (6–9) | 8 | (7–9) | p = 0.78* |
| From start to restarting CC | 340 | (324–381) | 249 | (241–270) | p = 0.002† (0.62)π |
AED: Automated External Defibrillator; CC: Chest compressions; IQR: Interquartile range; † Wilcoxon’s signed ranked test (p < 0.05) and π Rosenthal’s r for Effect Size (in brackets); * Student’s t test (p < 0.05) and ‡ Cohen’s d test for Effect Size (in brackets).
Self-perceptive variables
Participants reported higher self-perception of performance quality in M2 (7.0; IQR: 6.0–7.8) than in M1 (5.5; IQR: 4.3–8.0; p = 0.020; effect size = 0.55) (Table 4). However, there were no differences in the difficulty of using the smart glasses or in their self-confidence during the performance.
Table 4.
Perceptual variables during M1 (smart glasses-assisted test while training) and M2 (unassisted post-test) (N = 12) (in a 0–10 scale).
| M1: while training with smart glasses |
M2: Unassisted post-test |
Significance (Effect Size) |
|||
|---|---|---|---|---|---|
| Median | IQR | Median | IQR | ||
| Difficulty of smart glasses use | 2.0 | (1.3–3.0) | 2.0 | (0.3–2.8) | p = 0.50† |
| Self-perception of performance quality * | 5.5 | (4.3–8.0) | 7.0 | (6.0–7.8) |
p = 0.020* (0.55)‡ |
| Self-confidence | 7.5 | (5.3–9.0) | 7.0 | (4.0–7.8) | p = 0.14* |
IQR: Interquartile range; † Wilcoxon’s signed ranked test (p < 0.05); * Student’s t test (p < 0.05) and ‡ Cohen’s test for Effect Size (in brackets).
Discussion
Teaching BLS to as many laypeople as possible is an aspiration to prevent the consequences of out-of-hospital cardiac arrest. In some cases, and environments, it can be difficult to access this type of education, which is why it may be interesting to explore training with new technologies. However, the new technological tools, such as augmented reality, should not be used without a previous rigorous evaluation of their feasibility, advantages, and disadvantages. For this reason, we consider essential to evaluate the smart glasses before proceeding to its routine use in training and that is why we set the objective of analyzing the learning process of the BLS after a very brief training in which the participants experienced a sequence of performing with the video assistance of an instructor through smart glasses.
Our main finding was that very brief training using a cardiac arrest simulation in which the participant is video-assisted through smart glasses is a valid alternative method for learning BLS. There was a good learning in the BLS protocol, the use of the AED, the performance times, and some parameters related to the quality of resuscitation.
This type of training, in which the participant experiences a simulated but quite realistic situation of cardiorespiratory arrest while being video-assisted through the smart glasses, was adequate for to learn the BLS protocol. After the training, practically all the participants performed most of the steps of the BLS protocol satisfactory (check breathing, use the AED, start chest compressions…). The steps that fewer participants performed correctly were assessing consciousness and alert that nobody touch the victim before shocking, which only 7 of 12 did correctly. However, this did not imply a deterioration in comparison to M1, so they performed as correctly as they were able to while learning with the smart glasses-assistance of the instructor.
In the event of a real cardiac arrest, a good performance following the BLS protocol would favor a good ABC approach, the call to emergency medical services, the initiation of resuscitation, and the use of the AED. All this is integrated into the so-called chain of survival in which the performance of the witness is key,17, 18 and if done properly, as the participants in this study learned, it can ensure more chances of survival.19 All except one participant in this study learned to use the AED without errors (one of them did not use it when asked to act autonomously). Also, when they acted without the help of the dispatcher, all AED defibrillations were completed within 5 minutes (mean: 4 minutes). Note that, in our simulation scenario, the AED arrived after 2 minutes of resuscitation and it took about 1 minute from the AED arrival until the shock was delivered. It is a quick action that in a real situation would be very important for survival.19, 20, 21 In our study, when participants performed autonomously, they started chest compressions quickly (mean: 62 seconds from the beginning, and after the ABC approach and the call to emergency medical services). In a real situation of out-of-hospital cardiorespiratory arrest, this immediate initiation of CPR would be positive because it could double or triple the survival rate from cardiac arrest.2, 22 It is remarkable that performing times even doubled in the smart glasses-assisted test (M1) compared to the unassisted post-test (M2). This was to be expected because in M1, the variables were assessed while they were training in communication with the instructor through the smart glasses. During the training, the participants took longer to perform because they were learning to act by listening to the trainer's instructions and corrections. Otherwise, in the unassisted post-test (M2), the participants limited themselves to performing autonomously.
In addition to early resuscitation, CPR must be performed with quality. In our study, very brief training with smart glasses was useful for learning the proper compression point (100% of the chest compressions with hands positioned correctly), minimizing interruptions (they only stopped for an average of 1.5 seconds in the 2 minutes of chest compressions), and having a guideline conform compression rate within 100 and 120 chest compressions/min (which was 113 chest compressions/min). However, this training was not adequate to achieve a good chest compressions depth. Performing chest compressions too shallow is a recurring mistake in laypeople, and due to that some previous studies with self-learning BLS achieve good compression depth between 5 and 6 cm and others no,23, 24 the factors contributing to these differences need to be explored in the future. In our study, the visual information that the instructor had was through the smart glasses' front camera (subjective vertical vision of the participant). This angle of vision is not optimal to be able to correct just-in-time the depth of the chest compressions, so the instructor should have been encouraged to insist on the “push hard” correction. An improvement proposal for our educational methodology would be the incorporation of a double feedback system integrated into the smart glasses, in which both the instructor and student might see the real depth of each chest compression in real-time. It would be expected that this combination of technologies would favor the learning of a better quality of resuscitation with a better chest compressions depth.
This type of educational training has been adequate for learning BLS, with the exception of the recently named resuscitation quality parameters. The novelty of this type of CPR training lies in the use of the video call with smart glasses as a communication wearable. The instructor can carry out personalized training encouraging the learner to continue acting when he/she does it well or correcting him/her based on what he/she sees and hears through the smart glasses. This type of training through the use of wearable technology and augmented reality with smart glasses may engage many learners4 and it can be especially interesting to apply in remote places, such as rural areas, where it is more difficult to implement face-to-face BLS educational programs.9
A possible barrier to this type of tele-training could have been the use of the wearable itself. However, the participants stated that the smart glasses are very easy to use (ease of use: 2 out of 10, they had enough with less than 5 minutes to become familiar with them) and generated good self-confidence and self-perception of performance quality (7 over 10).
Based on the findings of this study, the option of teaching BLS with this new educational methodology which is characterized by being very brief (<7 minutes) and the use of telematics through augmented reality with smart glasses opens up. Experiencing a simulated cardiorespiratory arrest execution with the video assistance of the instructor with the smart glasses has made the laypeople participants quite competent to perform autonomously. It would be expected that, after this learning, if the participants witness a real cardiorespiratory arrest, they may have greater guarantees of helping the victim.
For the implementation of this type of training, it would be necessary to take into account the costs of the technology itself and the number of instructors. The 2021 cost of these smart glasses was around 1,200 euros and it is necessary to connect them to the Internet. Furthermore, there has to be an instructor for each student. The positive aspect is that the instructor can individualize the corrections of each student based on what he/she sees and hears in the video call through the smart glasses.
Apart from the future limitations in the implementation of this learning methodology, this study has had certain limitations in itself. It must be taken into account that this is a pilot study with a small sample size, a larger number of participants could favor a better statistical power and more significant differences. When interpreting the results, the profile of the participants must be considered. They were laypeople with no prior knowledge of BLS, so we value as very positive the fact that with such a short training, they learned substantially. In addition, they were all students from a university degree in sports, so one can assume that they had a certain ability for learning simple procedures such as BLS, and motor skills such as chest compressions.25
In the future, it could be interesting to explore whether short training programs and the use of new communication technologies, such as smart glasses, could be a good alternative method of learning BLS for laypeople in studies with a higher statistical power.
Conclusions
Our pilot study suggest that smart glasses-assisted training can facilitate teaching basic life support to laypeople. Our very brief training experiencing a simulation of video-assisted cardiac arrest care with smart glasses has demonstrated promising results as an educational method for learning the basic life support protocol, the use of the automated external defibrillator, and some skills to perform basic life support. This technology can be easily used and seems useful for remotely learning how to respond to cardiorespiratory arrest, but additional studies are still needed to ascertain its impact at educational level. This method has potential for smart glasses assisted training to increase access to basic life support education, especially in remote or underserved areas. Future research should explore the potential synergies between smart glasses and cardiopulmonary resuscitation quality feedback systems.
Conflicts of Interest
None.
Acknowledgments
Acknowledgements
Thanks to Cristian Corpas for his help in the data collection.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Gräsner J.-T., Wnent J., Herlitz J., Perkins G.D., Lefering R., Tjelmeland I., et al. Survival after out-of-hospital cardiac arrest in Europe - Results of the EuReCa TWO study. Resuscitation. 2020;148:218–226. doi: 10.1016/j.resuscitation.2019.12.042. [DOI] [PubMed] [Google Scholar]
- 2.Yan S., Gan Y., Jiang N., Wang R., Chen Y., Luo Z., et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. 2020:24. doi: 10.1186/S13054-020-2773-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.González-Salvado V., Rodríguez-Ruiz E., Abelairas-Gómez C., Ruano-Raviña A., Peña-Gil C., González-Juanatey J.R., et al. Training adult laypeople in basic life support. A systematic review. Rev Esp Cardiol (Engl Ed) 2020;73:53–68. doi: 10.1016/J.REC.2018.11.013. [DOI] [PubMed] [Google Scholar]
- 4.Greif R., Lockey A., Breckwoldt J., Carmona F., Conaghan P., Kuzovlev A., et al. European Resuscitation Council Guidelines 2021: Education for resuscitation. Resuscitation. 2021;161:388–407. doi: 10.1016/j.resuscitation.2021.02.016. [DOI] [PubMed] [Google Scholar]
- 5.Lau Y., Nyoe R.S.S., Wong S.N., Ab Hamid Z., Bin L.-H., Lau S.T. Effectiveness of digital resuscitation training in improving knowledge and skills: A systematic review and meta-analysis of randomised controlled trials. Resuscitation. 2018;131:14–23. doi: 10.1016/j.resuscitation.2018.07.033. [DOI] [PubMed] [Google Scholar]
- 6.Yeung J., Meeks R., Edelson D., Gao F., Soar J., Perkins G.D. The use of CPR feedback/prompt devices during training and CPR performance: A systematic review. Resuscitation. 2009;80:743–751. doi: 10.1016/j.resuscitation.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 7.Nas J., Thannhauser J., Vart P., Van Geuns R.J., Muijsers H.E.C., Mol J.Q., et al. Effect of Face-to-Face vs Virtual Reality Training on Cardiopulmonary Resuscitation Quality: A Randomized Clinical Trial. JAMA Cardiol. 2020;5:328–335. doi: 10.1001/JAMACARDIO.2019.4992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuyt K., Park S.-H., Chang T.P., Jung T., MacKinnon R. 2021. The use of virtual reality and augmented reality to enhance cardio-pulmonary resuscitation: a scoping review; p. 6. (Adv Simul (London, England)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cross M., Harlow E., Morrison S.R., Place M., Sutherland M., Thomas J., et al. Bystander CPR training: is non-classroom based CPR training as effective as a classroom based approach? A systematic review of randomised controlled trials. Rural Remote Health. 2019;19 doi: 10.22605/RRH4772. [DOI] [PubMed] [Google Scholar]
- 10.Alcázar Artero P.M., Pardo Rios M., Greif R., Ocampo Cervantes A.B., Gijón-Nogueron G., Barcala-Furelos R., et al. Efficiency of virtual reality for cardiopulmonary resuscitation training of adult laypersons: A systematic review. Medicine (Baltimore) 2023;102:e32736. doi: 10.1097/MD.0000000000032736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mitrasinovic S., Camacho E., Trivedi N., Logan J., Campbell C., Zilinyi R., et al. Clinical and surgical applications of smart glasses. Technol Health Care. 2015;23:381–401. doi: 10.3233/THC-150910. [DOI] [PubMed] [Google Scholar]
- 12.Kim D., Choi Y. Applications of Smart Glasses in Applied Sciences: A Systematic Review. Appl Sci. 2021;11:4956. doi: 10.3390/app11114956. [DOI] [Google Scholar]
- 13.Aranda-García S., Santos-Folgar M., Fernández-Méndez F., Barcala-Furelos R., Pardo Ríos M., Hernández Sánchez E., et al. “Dispatcher, Can You Help Me? A Woman Is Giving Birth”. A Pilot Study of Remote Video Assistance with Smart Glasses. Sensors (Basel) 2022:23. doi: 10.3390/S23010409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Olasveengen T.M., Semeraro F., Ristagno G., Castren M., Handley A., Kuzovlev A., et al. European Resuscitation Council Guidelines 2021: Basic Life Support. Resuscitation. 2021;161:98–114. doi: 10.1016/j.resuscitation.2021.02.009. [DOI] [PubMed] [Google Scholar]
- 15.Cohen J. 2nd ed. Lawrence Erlbaum; Hillsdale, NJ: 1988. Statistical power analysis for the behavioural sciences. [Google Scholar]
- 16.Rosenthal R. 2nd ed. Sage; Newbury Park, CA: 1991. Meta-analytic procedures for social research. [Google Scholar]
- 17.Perkins G.D., Graesner J., Semeraro F., Olasveengen T., Soar J., Lott C., et al. European Resuscitation Council Guidelines 2021: Executive summary. Resuscitation. 2021;161:1–60. doi: 10.1016/j.resuscitation.2021.02.003. [DOI] [PubMed] [Google Scholar]
- 18.Nolan J. European Resuscitation Council guidelines for resuscitation 2005. Section 1. Introduction. Resuscitation. 2005;67:1. doi: 10.1016/J.RESUSCITATION.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 19.Semeraro F., Greif R., Böttiger B.W., Burkart R., Cimpoesu D., Georgiou M., et al. European Resuscitation Council Guidelines 2021: Systems saving lives. Resuscitation. 2021;161:80–97. doi: 10.1016/j.resuscitation.2021.02.008. [DOI] [PubMed] [Google Scholar]
- 20.Gold L.S., Fahrenbruch C.E., Rea T.D., Eisenberg M.S. The relationship between time to arrival of emergency medical services (EMS) and survival from out-of-hospital ventricular fibrillation cardiac arrest. Resuscitation. 2010;81:622–625. doi: 10.1016/j.resuscitation.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 21.Berdowski J., Blom M.T., Bardai A., Tan H.L., Tijssen J.G.P., Koster R.W. Impact of onsite or dispatched automated external defibrillator use on survival after out-of-hospital cardiac arrest. Circulation. 2011;124:2225–2232. doi: 10.1161/CIRCULATIONAHA.110.015545. [DOI] [PubMed] [Google Scholar]
- 22.Hasselqvist-Ax I., Riva G., Herlitz J., Rosenqvist M., Hollenberg J., Nordberg P., et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2015;372:2307–2315. doi: 10.1056/NEJMoa1405796. [DOI] [PubMed] [Google Scholar]
- 23.Lim X.M.A., Liao W.A., Wang W., Seah B. The Effectiveness of Technology-Based Cardiopulmonary Resuscitation Training on the Skills and Knowledge of Adolescents: Systematic Review and Meta-analysis. J Med Internet Res. 2022;24:e36423. doi: 10.2196/36423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pedersen T.H., Kasper N., Roman H., Egloff M., Marx D., Abegglen S., et al. Self-learning basic life support: A randomised controlled trial on learning conditions. Resuscitation. 2018;126:147–153. doi: 10.1016/j.resuscitation.2018.02.031. [DOI] [PubMed] [Google Scholar]
- 25.Aranda-García S., Herrera-Pedroviejo E., Abelairas-Gómez C. Basic Life-Support Learning in Undergraduate Students of Sports Sciences: Efficacy of 150 Minutes of Training and Retention after Eight Months. Int J Environ Res Public Health. 2019;16:4771. doi: 10.3390/ijerph16234771. [DOI] [PMC free article] [PubMed] [Google Scholar]