Summary
Infantile Epileptic Spasms Syndrome (IESS), commonly known as West syndrome, is the most common cause of infantile-onset epileptic encephalopathy. There is a peculiar epidemiological profile of IESS in South Asia. Specific features identified were a preponderance of acquired structural aetiology, male gender dominance, a long treatment lag, limited availability of adrenocorticotropic hormone (ACTH) and vigabatrin, and use of carboxymethyl cellulose derivative of ACTH. Because of the significant disease burden and limited resources, there are distinctive challenges to the optimal care of children with IESS in the South Asian region. Also, there are unique opportunities to bridge these challenges and improve outcomes. This review provides an overview of the landscape of IESS in South Asia and highlights its peculiarities, various challenges, and way forward.
Keywords: West syndrome, Infantile spasms, Salaam seizures, Epileptic spasms
Search strategy and selection criteria.
We searched the electronic database Embase in April 2022 for articles published in English without any restriction on publication date. We used the search terms ‘infantile spasms'/exp OR 'infantile spasms' OR (infantile AND spasms) OR 'epileptic spasms' OR (('epileptic'/exp OR epileptic) AND spasms) OR 'salaam seizures' OR (salaam AND ('seizures'/exp OR seizures)) AND 'South Asia'/exp OR 'South Asia' OR (south AND ('Asia'/exp OR Asia)) OR 'India'/exp OR India OR 'Pakistan'/exp OR Pakistan OR 'Afghanistan'/exp OR Afghanistan OR 'Sri Lanka'/exp OR 'Sri Lanka' OR 'Myanmar'/exp OR Myanmar OR 'Maldives'/exp OR Maldives OR 'Nepal'/exp OR Nepal OR 'Bhutan'/exp OR Bhutan OR 'Bangladesh'/exp OR Bangladesh. We identified additional references from the reference list of pertinent articles identified from the database and based on the existing knowledge of co-authors. We generated the final list of references based on originality and relevance to the broad scope of this review.
Introduction
Historical note
In 1841, William James West, a British surgeon, first classically described infantile spasms as peculiar bowing convulsions in his son. His historic letter to the editor of The Lancet reported that Drs. Clarke and Locock from London had recognized his son's symptoms. Clarke termed these seizures as “salaam convulsions”.1 Subsequently, various eponymous designations were used to describe this entity in literature, including nodding spasms, eclampsia nutans, tic de salaam, Blitz-Nick-und Salaam-krdmpfe, propulsiv petit mal, epilepsia generalizada en flexión, etc.2 In 1952, Gibbs and Gibbs coined the terms “infantile spasms” and “hypsarrhythmia” to describe the peculiar seizure and signature interictal electroencephalogram (EEG) pattern, respectively.3 In 1958, Sorel and Dusaucy-Bauloyethe demonstrated the effectiveness of adrenocorticotropic hormone (ACTH) therapy in infantile spasms.4 In 1960, the Marseilles colloquium led by Gastaut recognized the historical importance of West's eponym for the electroclinical syndrome.5 The term was subsequently famous as a classical triad of epileptic spasms, hypsarrhythmia, and developmental regression or stagnation. Furthermore, the term “infantile spasms” has been used interchangeably for decades in medical literature to refer both to a seizure type and an electroclinical syndrome. In a recently proposed syndrome classification, the International League Against Epilepsy (ILAE) renamed this disorder as Infantile epileptic spasms syndrome (IESS).6
Infantile Epileptic Spasms Syndrome (IESS)
IESS is characterised by the occurrence of a particular seizure, known as epileptic spasms (the preferred term for infantile spasms). The onset of epileptic spasms occurs typically between 3 and 12 months of age and sometimes from one to 24 months. Epileptic spasms consist of brief tonic contraction of axial muscles, lasting 0.5–2 s, which may be flexor, extensor, or mixed in appearance and classically occur in clusters. These are primarily associated with episodes of crying, screaming, or occasional laughter, either before or soon after a spasm. These commonly occur on awakening or just before sleep. Sometimes epileptic spasms are pretty subtle, and facial grimacing, smiling, chin movement, versive ocular movements, head nodding or trunk rotation are the only clinical clues.7 Many of these children have a pre-existing developmental delay due to underlying aetiology. Developmental arrest or regression is often evident with the occurrence of epileptic spasms. The syndrome is indeed an epileptic encephalopathy where the epileptic burden also contributes to developmental slowing or arrest beyond what is expected from pathology alone. Interictal EEG is characterized by hypsarrhythmia, which signifies chaotic background, continuous, random, high-amplitude slow waves intermixed with focal, multifocal or generalised epileptiform discharges with marked variability.
About South Asia
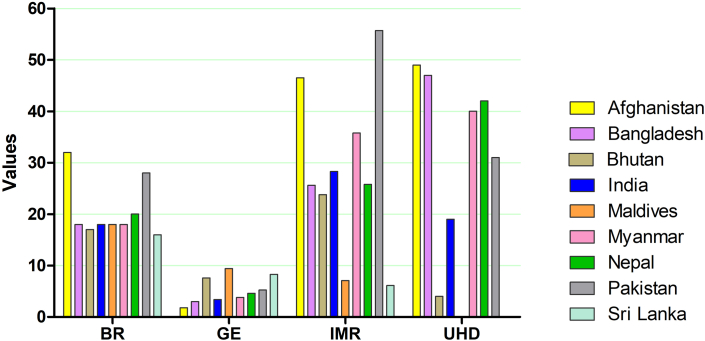
South Asia is peculiar for its geographical and ethnic-cultural diversity. It homes to nearly a quarter of the global population and is emerging as a vibrant, dynamic, and rapidly growing region. For our article, we included studies from nine countries: Afghanistan, Bangladesh, Bhutan, India, Maldives, Myanmar, Nepal, Pakistan, and Sri Lanka. All these countries, except Maldives (upper-middle-income), fall in or below the category of lower-middle-income countries, with nearly a quarter of the population falling below the international poverty line. This region has problems in the sphere of education, literacy, health, and nutrition. The significantly lower gross enrolment ratio in this region compared with the global average is concerning and leads to a vicious cycle of poor education, poor health and nutrition, and illness-related morbidity affecting economic growth and education. Although the prevailing conditions are improving in a few countries, the graveness of the situation persists. A high birth rate, infant mortality rate, unattended home delivery percentage, and a relatively low government expenditure on health are peculiar concerning health indices (Fig. 1).8
Fig. 1.
Health care related indices in South Asia. BR = Birth rate per 1000, GE = Government expenditure on health (percentage of government expenditure), IMR = Infant mortality (per 1000 live births), UHD = Unattended home delivery percentage.
Recognition of IESS in South Asia
During the initial six decades of the 19th century, there was a silence in the medical literature on IESS in South Asia. Various prevalent languages, a relative lack of paediatric journals in the region, political unrest and freedom struggles in many of these countries at that time, and relatively underdeveloped perinatal and neonatal services in the region might be the underlying reasons for the same. The precise initial description of IESS in English might be credited to Janaki and Chandy in 1964 and Warrier in 1965 and 1966 from India.9, 10, 11 In 1983, Anandam published a lucid description of the electroclinical profile of 50 children with IESS from South India.12 Later, much interest in this disorder ensued, and various publications including hospital-based experiences from multiple South Asian countries enhanced the literature (Supplementary Fig. S1, Supplementary Table S1). Over the last decade, few important intervention studies also emerged from this region (Supplementary Table S1).13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23 In 2020, Sahu and colleagues formed the South Asia West Syndrome Research group with members from Bangladesh, Bhutan, India, Myanmar, Nepal, Pakistan and Sri Lanka and later expanded to include members from Afghanistan and Maldives. The research group published articles on management practices, teleneurology, and etiological considerations related to IESS in South Asia.8,24, 25, 26
Epidemiology of IESS in South Asia
Burden
Globally, the pooled incidence estimate of IESS is 0.249 cases per 1000 live births, and pooled prevalence estimate is 0.015 cases per 1000 population.27 There is a lack of incidence estimates of IESS from South Asia.8 Two studies from the rural regions of India measured prevalence estimates of IESS. In 1988, Koul and colleagues published that the point prevalence of paediatric epilepsy and IESS was 31.8 and 1.5 per 10,000 children, respectively.28 In a recent study by Srivastava and colleagues (which screened 19,181 children aged 2 mos-18 yr), the prevalence of paediatric epilepsy and IESS was 34.4 and 2.0 per 10,000 children, respectively.29 The prevalence estimate in Indian studies is much higher than that reported globally. The two Indian studies probably demonstrate the tip of a hidden iceberg. A high prevalence of birth injuries, relatively poor health infrastructure, declining neonatal mortality with increasing morbidity, a high birth rate, and a high proportion of the young population might be the crucial determinants of the population burden of IESS in this region.8
Gender
IESS affects both sexes. Data based on incidence studies globally suggest a male proportion of 49% in the reference population.27 However, most studies from South Asia, either case series or hospital cohorts, observed a male gender preponderance. Besides, nearly 60% of surveyed child neurologists in South Asia observed a male preponderance. A meta-analysis of large South Asian cohorts also suggested a 68% (confidence interval [CI] 64%–73%) pooled estimate for male preponderance in IESS.24 However, the country estimates varied from 58% for Sri Lanka, 64% for Pakistan, and 72% for India. The plausible explanations for this finding might be male-predominant sex ratios at birth and child sex ratios in this region and preferential health-seeking behaviour of the community for boys.
Treatment lag in South Asia
Treatment lag or lead time to treatment is recognized as a significant prognostic variable for therapeutic response in children with IESS. Untreated hypsarrhythmia for more than three weeks has been associated with poor neurodevelopmental outcomes.30 The risk ratio (as ascertained in a meta-analysis) for treatment lag <4 weeks relative to >4 weeks for good neurodevelopmental outcome was 1.52 (95% CI: 1.064–2.169).31 In a prospective study by Anbarasu and colleagues from North India, the median treatment lag duration was 90 days (95% CI: 110–198 days), and the significant determinants of treatment lag were: the pre-existing developmental delay of children, educational status of the parents and qualification of the first practitioner visited. Furthermore, the study showed shorter treatment lag (<1 month) was associated with a better spasms cessation rate (85% vs. 15%; p = 0.011).32 In a meta-analysis of seven studies–five from India, one from Sri Lanka and Pakistan, the pooled estimate of treatment lag was 2.4 months (CI: 2.1–2.6 months).24
The higher treatment lag in this region is bothersome because of the associated implications and a lack of significant efforts to reduce this figure. Capacity building of paediatricians through continuing medical education should help decrease the treatment lag. Although cumbersome, spreading awareness about this disorder among parents and caregivers is equally essential. Screening the at-risk population (infants with developmental delay, history of perinatal or postnatal insult) and educating the caregivers on epileptic spasms during vaccination visits and in between might be helpful. Although no vaccination visits are scheduled between 3.5 months and nine months (median age at onset of IESS being around five months), arranging a healthcare visit for at-risk children at 5–6 months of age might be a feasible solution. The utilization of mass media for awareness of the subject might be beneficial.
Aetiology of IESS
Traditionally, the aetiology of IESS was classified as symptomatic, idiopathic or cryptogenic. In 2010, the ILAE Commission on Classification and Terminology replaced these terms with specific aetiological categories—structural-metabolic, genetic, or unknown.33 In 2017, ILAE further updated the classification scheme into the following categories—structural, metabolic, infectious, immune, or unknown.34 Here, classifying as unknown aetiology is based on the assumption that clinicians should thoroughly investigate these children. However, a significant proportion of children with IESS remain incompletely investigated in resource-limited health care settings. Therefore, the South Asian West Syndrome Research Group proposed another classification scheme of etiological categories: known, incompletely investigated, or unknown.8
Database of 250 children with new-onset IESS from National Infantile Spasms Consortium in North America, identified aetiological distribution as follows: structural, 33.2% (congenital, 10.8%; acquired, 22.4%); genetic-structural, 10.0%; genetic alone, 14.4%; metabolic, 4.8%; infection, 2%; and unknown, 35.6%. Of those with known aetiologies, causes were further classified as prenatal (57.8%), perinatally structural acquired (24.2%), and postnatal (18%).35
However, the landscape of aetiologies is different in South Asian countries, with a predominance of acquired structural brain insults such as hypoxic and hypoglycaemic brain injuries in 61–76% of patients.24 The figures for structural brain insults as a cause of IESS are higher for India (71%) and Pakistan (64%), while estimates for countries like Nepal, Bhutan, Myanmar, and the Maldives are unavailable.24 IESS's association with nutritional deficiencies, specifically vitamin B12, is exclusive to this region, likely due to the high prevalence of malnutrition and vegetarianism here. Besides, other preventable causes of brain injury, such as vitamin K deficiency bleeding, are also eccentric to this region due to a relatively higher proportion of unattended births. Furthermore, due to consanguineous marriages, recessively inherited metabolic causes of IESS are not uncommon. With the advent, availability, and declining cost of next-generation sequencing, few Indian studies on the genetic landscape of IESS report pathogenic variants of CDKL5 and STXBP1 genes as common monogenetic causes of IESS.36,37 There is limited literature on the subject from the rest of South Asian countries.
Management practices
The management practices for IESS differ globally. The first-choice anti-seizure medications with high-quality evidence are intramuscular ACTH, oral steroids, and vigabatrin therapy. Furthermore, there is global variability in the use and availability of ACTH formulations. Natural ACTH is used in the USA, while synthetic preparations, e.g., tetracosactide and carboxymethylcellulose, are used in Europe and South Asia, respectively. Natural ACTH is costly, while tetracosactide and carboxymethylcellulose are relatively cheaper. There is a lack of head-to-head comparison studies on the relative efficacy of these preparations. Furthermore, studies comparing different doses and regimens of ACTH for different duration are also needed to identify the most effective and safe treatment option.
Due to economic constraints and the search for less expensive therapies, evidence for high-dose oral prednisolone is also accumulating14,16 In a meta-analysis, oral prednisolone was relatively better than ACTH therapy in terms of day 14 and day 42 responses.24 But the meta-analysis was skewed by a study from Sri Lanka in which ACTH was prescribed every alternate day (half of the dose usually given in other South Asian countries).14 Indian clinical trials which used ACTH showed a trend of better efficacy for ACTH.16,18,20 Three intervention studies (two from India and one from Bangladesh) comparing methylprednisolone as a treatment option are also available.15,19,21 In Japan, child neurologists often prefer oral pyridoxine as an initial choice. However, two RCTs from India reported that the efficacy of pyridoxine in combination with hormonal therapy is not superior to hormonal therapy alone.17,20 Hence, the quest for the region's best therapeutic and cost-effective option continues.38
There are difficulties with licensing and availability of the first-line therapeutic options in many South Asian countries. Vigabatrin and ACTH are neither licensed nor available in Nepal and Myanmar, while ACTH is not licensed in Bhutan.24 In a recent development in India, vigabatrin has been approved and made available. Hence, many South Asian countries are not left with options and use oral prednisolone as a first-line drug. Furthermore, there is not much evidence for vigabatrin from the region due to these issues. Among the second-line options, topiramate and nitrazepam appear to be effective in nearly 23% and 50%, respectively, of hormonal therapy-resistant children.39,40
Outcome
IESS is a devastating condition, and the outcome is often poor. There is scarce data from prospective registries on short-term and long-term outcomes in South Asian countries, and most studies are single hospital-based experiences.41, 42, 43, 44, 45, 46, 47 A systematic review on the short-term effectiveness of hormonal therapy in South Asia identified that the short-term response rate was low (18–33%).24 Bhanudeep and colleagues from India studied >5-year age outcomes in a follow-up cohort of IESS. They demonstrated the following: ongoing epilepsy (261/402, 65%), moderate to profound intellectual disability (111/164, 68%), unfavourable motor status (130/402, 32%), and impaired quality of life (115/164, 70%).46 Authors highlighted that the early age of onset of epileptic spasms (<5 months) and the presence of structural aetiology were significant predictors of adverse outcomes.46 It is crucial because structural aetiologies constitute a substantial cause of IESS in South Asia. Wanigasinghe and colleagues from Sri Lanka also demonstrated a poor quality of life despite control of epilepsy in a follow-up cohort.46 IESS affects the child, but its impact extends to the whole family psychologically and financially.48
Challenges, opportunities, and feasible solutions
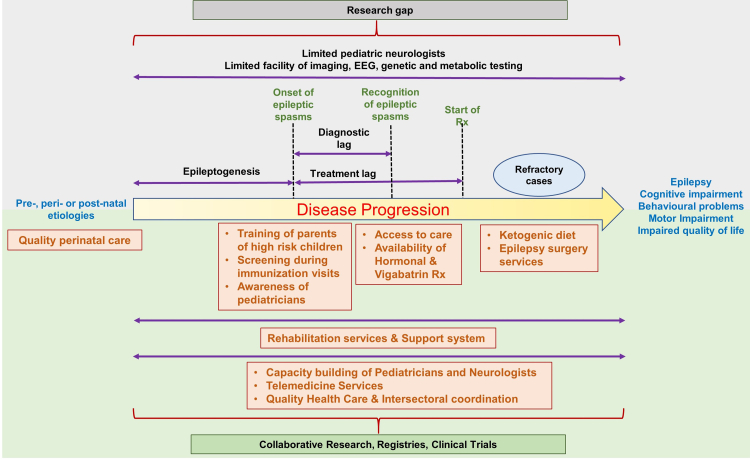
Considering the significant burden and limited resources, there are distinctive challenges to the optimal care of children with IESS in the South Asian region. Also, there are unique opportunities to bridge these challenges and improve outcomes (Fig. 2).
Fig. 2.
Challenges and opportunities for management of Infantile Epileptic Spasms Syndrome (IESS) in South Asia.
Prevention of perinatal injuries and other causes
Perinatal brain injuries, such as hypoxic brain injury, hypoglycaemic brain injury, infections, etc., is a significant public health concern and the predominant causes of IESS in South Asia.24 These indirectly reflect inadequate access to quality health care services. Therefore, reducing the burden of neonatal and early infantile brain injuries through appropriate obstetric and neonatal care should be fruitful. South Asian countries, e.g., Bangladesh, India, Nepal, and Pakistan have public health initiatives, including conditional cash transfers, voucher schemes, and cashless services aimed at promoting quality antenatal, natal, and postnatal care for pregnant women and neonatal care. Yet, these programs have had limited success and need to undergo significant expansion and outreach.
Furthermore, other preventable causes, such as nutritional deficiencies, need to be tackled with public health initiatives such as vitamin B12 and folic acid supplementation for pregnant and lactating females. Inbreeding and consanguinity are not uncommon in the region and indirectly enhance the possibility of IESS associated with autosomal recessive inherited inborn errors of metabolism and genetic disorders. Community awareness about the risks associated with consanguinity may be effective in this regard.
Minimizing diagnostic lag
A long diagnostic lag is a significant setback in achieving ideal outcomes in children with IESS. Paediatricians provide most of the healthcare to children with IESS, as child neurology is still a growing subspecialty in the region. A considerable awareness gap exists among caregivers and first point-of-contact healthcare providers. Survey studies from South Asia identified this gap and emphasized the importance of minimizing this gap.24,49 Awareness campaigns and targeted educational programs for paediatricians, healthcare providers, and caregivers of at-risk children might prove instrumental. It is an initial step to acquaint them with this epilepsy syndrome and its consequences. After that, apprising them of the characteristic epileptic spasms’ semiology and the importance of video recording any suspicious events may be helpful. Limited diagnostic facilities for EEG, neuroimaging, metabolic and genetic tests are also significant barriers. Furthermore, there is an inevitable need for a strategic National epilepsy control program for each of the South Asian countries with a special focus on paediatric epilepsies since most drug-resistant epilepsies originate in childhood.
The utility of a screening program for IESS is still ambiguous. However, using vaccination visits and telemedicine to screen high-risk populations can be rewarding. Since universalizing developmental screening has not yet been possible in the region, screening for IESS will be an arduous task. Cost-benefit analysis for the possibility of a regional screening program can further guide feasibility. Furthermore, neonatal screening for treatable neurometabolic disorders might be helpful in early diagnosis and treatment, restoring typical development and preventing epilepsy.
Minimizing treatment lag and improving access to holistic care
This is one of the significant challenges due to the burgeoning population in the region. Longer treatment lags and huge treatment gaps are associated with poor outcomes. Similarly, preferential healthcare-seeking behaviour for the male gender is also concerning. Although the improvement in health infrastructure has reduced the treatment gap, the unmet needs remain enormous. Access to care depends on many factors, including the availability of quality care, cost of care, expected out-of-pocket expenditure, the family's economic condition, and general health awareness. Hence, each of these needs to be targeted to improve access. Investing in health infrastructure for patients in difficult terrains, reducing the cost of care and out-of-pocket expenditure, health insurance schemes for the poor, working towards “economic progress for all”, and spreading health awareness are the need of the hour. Parents should also be educated to minimize gender bias in healthcare-seeking behavior. Importantly, these children commonly have neurodevelopmental comorbidities. Quality rehabilitation services are crucial to achieving the best possible outcome. Intersectoral coordination should be an essential part of the holistic care model.
Facilities for dietary therapies and epilepsy surgery program
A significant proportion of children with IESS is refractory to medical therapy. Some children may benefit from a ketogenic diet or epilepsy surgery. However, these services are limited to a few tertiary-level health care facilities. There is a dire need for equipped state-of-art paediatric epilepsy surgery centres in the region, considering their short-term and long-term effectiveness. Similarly, accessible facilities for initiation and monitoring of ketogenic diet therapy are much needed.
Deficiencies in research
Although IESS has been known to humankind for nearly two centuries, there are several unanswered questions concerning its epidemiology, pathophysiology, and management. Different regimes of synthetic ACTH (carboxymethylcellulose) have been used for over three decades in the region.24 However, there is no clear consensus on the best regime, with a sheer lack of pharmacokinetic studies on the subject. Also, there are no studies on biomarkers predicting therapeutic response, and there is a near-complete absence of basic science research from the region. In addition, there is a lack of uniform definitions and standards for research methodology in the context of IESS in South Asia. These inadequacies need to be countered with quality research and collaboration.
Collaboration between professionals in and across nations is a likely remedy to most maladies associated with IESS. Diagnosis and initiation of treatment for patients at the first point of contact can minimize treatment lag. Hence, promoting decentralization of care by a coalition among local healthcare providers and tertiary care centres is the need of the hour. Besides, multicentre collaboration for research can unravel IESS-related mysteries.
Setback due to COVID-19 pandemic
The COVID-19 pandemic has been unkind to humanity not only in terms of infection-related morbidity and mortality but also due to numerous indirect impacts such as pandemic restrictions, diversion of resources to COVID-related research and care, and interruption in routine care and research for other disorders. Although telemedicine gained importance and became a prolific solution in this difficult time, its utility in managing IESS craves further research and evidence.25,26 IESS is often challenging to diagnose, even during physical visits, based on history alone, due to poor awareness among caregivers. Therefore, novel telemedicine solutions are desirable for capturing epileptic spasms. These can be questionnaire-based tools for parents (who go through the questionnaire and a prototype video and answer it over a few days based on their observation of the child) and video analysis tools for analysis of suspicious movements. Future efforts in this direction might be helpful.
The COVID-19 pandemic should be viewed as an opportunity to grow telemedicine in the region. Telemedicine can be a feasible solution for improving access to care and reducing treatment lag. Novel telemedicine solutions for IESS, if developed, may be promising. Besides, this will likely reduce the cost of care by avoiding frequent face-to-face visits. Strengthening telemedicine infrastructure may help deal with the problem of attrition in clinical practice and research. Also, this might prove beneficial in adverse times such as pandemics, wars, etc.
Conclusions
IESS has a peculiar epidemiological profile and challenges in South Asia akin to other developing countries. A preponderance of acquired structural aetiology, male gender dominance, a long treatment lag, limited availability of ACTH and vigabatrin, poor therapeutic response, limited awareness among parents and healthcare providers, and limited resources are major challenges. Prevention of perinatal injuries by quality perinatal care, improvement in access to quality healthcare including rehabilitation services, surveillance of high-risk babies coupled with an awareness of the disease among parents, availability of hormonal and vigabatrin therapy, capacity building of paediatricians and neurologists, telemedicine facility, and quality research in the field are possible solutions.
Contributors
All authors JKS, PM, KP contributed equally and were involved in conceptualisation, literature search and writing the original draft.
Declaration of interests
None.
Acknowledgments
We acknowledge Ms. Nagita Devi for assisting in the systematic search and Mr. Sandeep Negi for assistance in formatting the paper. We also acknowledge the support provided by the Indian Council of Medical Research, New Delhi, vide No: 3/1/3/147/Neuro/2021-NCD-I.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lansea.2023.100170.
Appendix A. Supplementary data
References
- 1.West W.J. On a peculiar form of infantile convulsion. Lancet. 1841;1:724–725. doi: 10.1016/S0140-6736(00)40184-4. [DOI] [Google Scholar]
- 2.Eling P., Renier W.O., Pomper J., Baram T.Z. The mystery of the Doctor's son, or the riddle of West syndrome. Neurology. 2002;58:953–955. doi: 10.1212/wnl.58.6.953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gibbs E.L., Fleming M.M., Gibbs F.A. Diagnosis and prognosis of hypsarhythmia and infantile spasms. Pediatrics. 1954;13:66–73. doi: 10.1542/peds.13.1.66. [DOI] [PubMed] [Google Scholar]
- 4.Sorel L., Dusaucy-Bauloye A. Findings in 21 cases of Gibbs' hypsarrhythmia; spectacular effectiveness of ACTHActa Neurol Psychiatr Belg. 1958;58:130–141. [PubMed] [Google Scholar]
- 5.Lux A.L. West & son: the origins of West syndrome. Brain Dev. 2001;23:443–446. doi: 10.1016/s0387-7604(01)00266-2. [DOI] [PubMed] [Google Scholar]
- 6.Zuberi S.M., Wirrell E., Yozawitz E., et al. ILAE classification and definition of epilepsy syndromes with onset in neonates and infants: position statement by the ILAE task force on nosology and definitions. Epilepsia. 2022;63(6):1349–1397. doi: 10.1111/epi.17239. [DOI] [PubMed] [Google Scholar]
- 7.Pavone P., Polizzi A., Marino S.D., et al. West syndrome: a comprehensive review. Neurol Sci. 2020;41:3547–3562. doi: 10.1007/s10072-020-04600-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wanigasinghe J., Sahu J.K., Madaan P., et al. Classifying etiology of infantile spasms syndrome in resource-limited settings: a study from the South Asian region. Epilepsia Open. 2021;6:736–747. doi: 10.1002/epi4.12548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Janaki S., Chandy J. A study of 20 cases of infantile spasms treated with librium (chlordiazepoxide). a preliminary report. Neurol India. 1964;12:149–153. [Google Scholar]
- 10.Warrier C.B. Infantile spasms (salaam seizures): a case report. Indian Pediatr. 1965;2:460–463. [PubMed] [Google Scholar]
- 11.Warrier C. Infantile spasms (hypsarrhythmia)--a clinical study. J Assoc Physicians India. 1966;14(6):399–405. [PubMed] [Google Scholar]
- 12.Anandam R. Clinical and electroencephalographic study of infantile spasms. Indian J Pediatr. 1983;50:515–518. doi: 10.1007/BF02753291. [DOI] [PubMed] [Google Scholar]
- 13.Ahmed R. Comparative study of corticotrphin vs. vigabatrin therapy in infantile spasm. Pak J Med Sci. 2007;23:141–144. [Google Scholar]
- 14.Wanigasinghe J., Arambepola C., Sri Ranganathan S., Sumanasena S., Attanapola G. Randomized, single-blind, parallel clinical trial on efficacy of oral prednisolone versus intramuscular corticotropin on immediate and continued spasm control in West syndrome. Pediatr Neurol. 2015;53:193–199. doi: 10.1016/j.pediatrneurol.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 15.Fatema K., Rahman M., Hossain M.M., et al. Pulse methylprednisolone with oral prednisolone versus adrenocorticotropic hormone in children with West syndrome: a randomized controlled trial. J Epilepsy Res. 2021;11:136–141. doi: 10.14581/jer.21020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gowda V.K., Narayanaswamy V., Shivappa S.K., Benakappa N., Benakappa A. Corticotrophin-ACTH in comparison to prednisolone in West Syndrome - a randomized study. Indian J Pediatr. 2019;86:165–170. doi: 10.1007/s12098-018-2782-1. [DOI] [PubMed] [Google Scholar]
- 17.Kunnanayaka V., Jain P., Sharma S., Seth A., Aneja S. Addition of pyridoxine to prednisolone in the treatment of infantile spasms: a pilot, randomized controlled trial. Neurol India. 2018;66:385–390. doi: 10.4103/0028-3886.227281. [DOI] [PubMed] [Google Scholar]
- 18.Angappan D., Sahu J.K., Malhi P., Singhi P. Safety, tolerability, and effectiveness of oral zonisamide therapy in comparison with intramuscular adrenocorticotropic hormone therapy in infants with West syndrome. Eur J Paediatr Neurol. 2019;23:136–142. doi: 10.1016/j.ejpn.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 19.Rajpurohit M., Gupta A., Madaan P., Sahu J.K., Singhi P. Safety, feasibility and effectiveness of pulse methylprednisolone therapy in comparison with intramuscular adrenocorticotropic Hormone in children with West Syndrome. Indian J Pediatr. 2021;88:663–667. doi: 10.1007/s12098-020-03521-7. [DOI] [PubMed] [Google Scholar]
- 20.Banerjee A., Sahu J.K., Sankhyan N., et al. Randomized trial of high-dose pyridoxine in combination with standard hormonal therapy in West syndrome. Seizure. 2021;91:75–80. doi: 10.1016/j.seizure.2021.05.012. [DOI] [PubMed] [Google Scholar]
- 21.Kapoor D., Sharma S., Garg D., et al. Intravenous methylprednisolone versus oral prednisolone for West Syndrome: a randomized open-label trial. Indian J Pediatr. 2021;88:778–784. doi: 10.1007/s12098-020-03630-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chellamuthu P., Sharma S., Jain P., Kaushik J.S., Seth A., Aneja S. High dose (4 mg/kg/day) versus usual dose (2 mg/kg/day) oral prednisolone for treatment of infantile spasms: an open-label, randomized controlled trial. Epilepsy Res. 2014;108:1378–1384. doi: 10.1016/j.eplepsyres.2014.06.019. [DOI] [PubMed] [Google Scholar]
- 23.Sharma S., Goel S., Kapoor D., et al. Evaluation of the modified atkins diet for the treatment of epileptic spasms refractory to hormonal therapy: a randomized controlled trial. J Child Neurol. 2021;36:686–691. doi: 10.1177/08830738211004747. [DOI] [PubMed] [Google Scholar]
- 24.Madaan P., Chand P., Linn K., et al. Management practices for West syndrome in South Asia: a survey study and meta-analysis. Epilepsia Open. 2020;5:461–474. doi: 10.1002/epi4.12419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sahu J.K., Madaan P., Chand P., et al. Management of West syndrome during COVID-19 pandemic: a viewpoint from South Asian West syndrome research group. Epilepsy Res. 2020;167 doi: 10.1016/j.eplepsyres.2020.106453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Madaan P., Sahu J.K., Wanigasinghe J., et al. Teleneurology based management of infantile spasms during COVID-19 pandemic: a consensus report by the South Asia Allied West syndrome research group. Epilepsy Behav Rep. 2021;15 doi: 10.1016/j.ebr.2020.100423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jia J.L., Chen S., Sivarajah V., Stephens D., Cortez M.A. Latitudinal differences on the global epidemiology of infantile spasms: systematic review and meta-analysis. Orphanet J Rare Dis. 2018;13:216. doi: 10.1186/s13023-018-0952-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koul R., Razdan S., Motta A. Prevalence and pattern of epilepsy (Lath/Mirgi/Laran) in rural Kashmir, India. Epilepsia. 1988;29:116–122. doi: 10.1111/j.1528-1157.1988.tb04406.x. [DOI] [PubMed] [Google Scholar]
- 29.Srivastava K., Agarwal E., Rajadhyaksha S., et al. Significant treatment gap and co-morbidities identified in an epidemiological survey of pediatric epilepsy in rural suburbs of India. Seizure. 2021;91:417–424. doi: 10.1016/j.seizure.2021.07.018. [DOI] [PubMed] [Google Scholar]
- 30.Primec Z.R., Stare J., Neubauer D. The risk of lower mental outcome in infantile spasms increases after three weeks of hypsarrhythmia duration. Epilepsia. 2006;47:2202–2205. doi: 10.1111/j.1528-1167.2006.00888.x. [DOI] [PubMed] [Google Scholar]
- 31.Widjaja E., Go C., McCoy B., Snead O.C. Neurodevelopmental outcome of infantile spasms: a systematic review and meta-analysis. Epilepsy Res. 2015;109:155–162. doi: 10.1016/j.eplepsyres.2014.11.012. [DOI] [PubMed] [Google Scholar]
- 32.Anbarasu A., Sahu J.K., Sankhyan N., Singhi P. Evaluation of the magnitude, determinants and impact of treatment lag in West syndrome. Arch Dis Child. 2017;102:A153. doi: 10.1136/archdischild-2017-313087.383. [DOI] [Google Scholar]
- 33.Berg A.T., Berkovic S.F., Brodie M.J., et al. Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005–2009. Epilepsia. 2010;51:676–685. doi: 10.1111/j.1528-1167.2010.02522.x. [DOI] [PubMed] [Google Scholar]
- 34.Scheffer I.E., Berkovic S., Capovilla G., et al. ILAE classification of the epilepsies: position paper of the ILAE commission for classification and terminology. Epilepsia. 2017;58:512–521. doi: 10.1111/epi.13709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wirrell E.C., Shellhaas R.A., Joshi C., et al. How should children with West syndrome be efficiently and accurately investigated? Results from the National Infantile Spasms Consortium. Epilepsia. 2015;56:617–625. doi: 10.1111/epi.12951. [DOI] [PubMed] [Google Scholar]
- 36.Mitta N., Menon R.N., McTague A., et al. Genotype-phenotype correlates of infantile-onset developmental & epileptic encephalopathy syndromes in South India: a single centre experience. Epilepsy Res. 2020;166 doi: 10.1016/j.eplepsyres.2020.106398. [DOI] [PubMed] [Google Scholar]
- 37.Surana P., Symonds J.D., Srivastava P., et al. Infantile spasms: etiology, lead time and treatment response in a resource limited setting. Epilepsy Behav Rep. 2020;14 doi: 10.1016/j.ebr.2020.100397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sahu J.K., Madaan P. What matters the most for hormonal therapy in West syndrome: drug, dosage, or duration? Indian J Pediatr. 2021;88:751–752. doi: 10.1007/s12098-021-03747-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nadig P.L., Sahu J.K., Suthar R., Saini A., Sankhyan N. Topiramate as an adjunct in the management of West syndrome. Indian J Pediatr. 2020;87:6–11. doi: 10.1007/s12098-019-03105-0. [DOI] [PubMed] [Google Scholar]
- 40.Zahan S., Sahu J.K., Madaan P., et al. Effectiveness and safety of nitrazepam in children with resistant West syndrome. Indian J Pediatr. 2022;89:37–44. doi: 10.1007/s12098-021-03823-4. [DOI] [PubMed] [Google Scholar]
- 41.Banu S.H., Khan N.Z., Hossain M., et al. Prediction of seizure outcome in childhood epilepsies in countries with limited resources: a prospective study. Dev Med Child Neurol. 2012;54:918–924. doi: 10.1111/j.1469-8749.2012.04325.x. [DOI] [PubMed] [Google Scholar]
- 42.Aramanadka R., Sahu J.K., Madaan P., Sankhyan N., Malhi P., Singhi P. Epilepsy and neurodevelopmental outcomes in a cohort of West syndrome beyond two years of age. Indian J Pediatr. 2022;89:765–770. doi: 10.1007/s12098-021-03918-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bhanudeep S., Madaan P., Sankhyan N., et al. Long-term epilepsy control, motor function, cognition, sleep and quality of life in children with West syndrome. Epilepsy Res. 2021;173 doi: 10.1016/j.eplepsyres.2021.106629. [DOI] [PubMed] [Google Scholar]
- 44.Sehgal R., Gulati S., Sapra S., Tripathi M., Kabra M., Pandey R.M. Neurodevelopmental and epilepsy outcome in children aged one to five years with infantile spasms--a North Indian cohort. Epilepsy Res. 2014;108:526–534. doi: 10.1016/j.eplepsyres.2013.12.009. [DOI] [PubMed] [Google Scholar]
- 45.Kulsoom S., Ibrahim S.H., Jafri S.K., Moorani K.N., Anjum M. Infantile spasms: clinical profile and treatment outcomes. Pak J Med Sci. 2018;34:1424–1428. doi: 10.12669/pjms.346.15869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wanigasinghe J., Arambepola C., Murugupillai R., Kapurubandara R., Jayawickrama A. Quality of life at 6 years in children treated for West syndrome with hormonal therapy. Epilepsy Behav. 2021;119 doi: 10.1016/j.yebeh.2021.107974. [DOI] [PubMed] [Google Scholar]
- 47.Wanigasinghe J., Arambepola C., Ranganathan S.S., Jayasundara K., Weerasinghe A., Wickramarachchi P. Epilepsy outcome at four years in a randomized clinical trial comparing oral prednisolone and intramuscular ACTH in West syndrome. Pediatr Neurol. 2021;119:22–26. doi: 10.1016/j.pediatrneurol.2021.01.008. [DOI] [PubMed] [Google Scholar]
- 48.Raithatha D., Sahu J.K., Bhanudeep S., et al. Financial burden in families of children with West syndrome. Indian J Pediatr. 2022;89:118–124. doi: 10.1007/s12098-021-03761-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vaddi V.K., Sahu J.K., Dhawan S.R., Suthar R., Sankhyan N. Knowledge, Attitude and Practice (KAP) study of pediatricians on infantile spasms. Indian J Pediatr. 2018;85:836–840. doi: 10.1007/s12098-018-2630-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.