Abstract
Introduction
Humeral shaft fractures can be treated non-operatively or operatively. The optimal management is subject to debate. The aim was to compare non-operative and operative treatment of a humeral shaft fracture in terms of fracture healing, complications, and functional outcome.
Methods
Databases of Embase, Medline ALL, Web-of-Science Core Collection, and the Cochrane Central Register of Controlled Trials (CENTRAL) were systematically searched for publications reporting clinical and functional outcomes of humeral shaft fractures after non-operative treatment with a functional brace or operative treatment by intramedullary nailing (IMN; antegrade or retrograde) or plate osteosynthesis (open plating or minimally invasive). A pooled analysis of the results was performed using MedCalc.
Results
A total of 173 studies, describing 11,868 patients, were included. The fracture healing rate for the non-operative group was 89% (95% confidence interval (CI) 84–92%), 94% (95% CI 92–95%) for the IMN group and 96% (95% CI 95–97%) for the plating group. The rate of secondary radial nerve palsies was 1% in patients treated non-operatively, 3% in the IMN, and 6% in the plating group. Intraoperative complications and implant failures occurred more frequently in the IMN group than in the plating group. The DASH score was the lowest (7/100; 95% CI 1–13) in the minimally invasive plate osteosynthesis group. The Constant–Murley and UCLA shoulder score were the highest [93/100 (95% CI 92–95) and 33/35 (95% CI 32–33), respectively] in the plating group.
Conclusion
This study suggests that even though all treatment modalities result in satisfactory outcomes, operative treatment is associated with the most favorable results. Disregarding secondary radial nerve palsy, specifically plate osteosynthesis seems to result in the highest fracture healing rates, least complications, and best functional outcomes compared with the other treatment modalities.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00402-023-04836-8.
Keywords: Complication, Fracture healing, Humeral shaft fracture, Non-operative treatment, Operative treatment, Review
Introduction
Treatment modalities for humeral shaft fractures have evolved over time. Non-operative treatment has been the preferred method for decades since the healing potential of the humerus was considered very good in terms of speed and fracture healing rates, restoration of anatomy is not a prerequisite for good functional outcome, and patients are not exposed to operative risks such as iatrogenic radial nerve palsy, postoperative infections, and implant failure. However, the very good results from functional bracing as published in landmark papers in the 70’s and 80’s by, e.g., Sarmiento, could not be reproduced by others [1]. Despite the possibility of early mobilization of the shoulder and elbow joints, impairment of range of motion (ROM) of especially the shoulder joint was often reported [2, 3]. The persisting clinical need led to the development of new and improved implants for surgical treatment.
Operative treatment for humeral shaft fractures is mostly performed using intramedullary nailing (IMN) or plate osteosynthesis. An IMN is placed in the medullary cavity of the humerus and is, thus, in line with its mechanical axis. If closed reduction can be achieved, periosteal blood supply and fracture biology can be preserved. Incisions are small and require less soft tissue stripping than open reduction and plate osteosynthesis [4]. However, shoulder-related complaints, such as pain and restriction of shoulder movement due to malrotation and impingement of the proximal nail tip or locking head screw, are frequently reported [5–8]. Open reduction and plate osteosynthesis (ORPO) offers the possibility of anatomic reduction and, depending on the fracture configuration, compression of fragments, as it requires extensive soft tissue exposure [9]. A potential disadvantage is a possible higher rate of (temporary) secondary radial nerve palsy [10]. Minimally invasive plate osteosynthesis (MIPO) has the advantage of limited soft tissue dissection and avoids the need to expose the radial nerve [10].
The development of anatomical and angular locked plate systems since approximately 2002 has led to a variety of reliable surgical techniques and a shift from non-operative management toward osteosynthesis, even when no absolute indication for surgery is present [11–15]. Some authors recommend to use IMN, whereas recently MIPO has been proposed as the preferred treatment [6, 8, 16–22]. The debate on the most optimal treatment strategy of humeral shaft fractures remained inconclusive after previous reviews, which only included 6–17 published randomized controlled trials and comparative prospective cohort studies in total [8, 16–26].
The primary aim of the current systematic review and pooled analysis was to compare fracture healing between non-operative and operative treatment of a humeral shaft fracture. The secondary aims were to compare complications and functional outcome.
Materials and methods
This systematic literature review and pooled analysis was conducted and reported according to the standards set out in Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [27]. Methods used for the analysis, search strategy, and inclusion criteria were specified in advance.
Search strategy
Databases of Embase, Medline ALL, Web-of-Science Core Collection, and the Cochrane Central Register of Controlled Trials (CENTRAL) were searched. Search strings were made by an experienced librarian and are shown in Table 1. The final search was done on July 30, 2021.
Table 1.
Search strategy
| Database searched | Via | Query | Records | Records after duplicates removed |
|---|---|---|---|---|
| Embase | Embase.com | ((('humerus fracture'/de OR 'humerus shaft fracture'/de OR 'forearm fracture'/de) NOT (proximal OR distal):ab,ti,kw) OR (((humeral-shaft* OR humerus-shaft* OR forearm-shaft* OR arm-shaft*) NEAR/3 (fracture*))):ab,ti,kw) AND (surgery/exp OR surgery:lnk OR 'orthopedic fixation device'/exp OR 'bone plate'/de OR 'conservative treatment'/exp OR brace/de OR 'plaster cast'/de OR splinting/de OR immobilization/exp OR (surg* OR operat* OR nailing OR nails OR pins OR plate* OR plating OR (extern* NEAR/3 fix*) OR screw* OR conservative* OR brace* OR bracing OR sling* OR plaster* OR cast OR casting OR nonoperat* OR nonsurg* OR Sarmiento OR splint* OR traction OR immobili*):ab,ti,kw) NOT ((animal/exp OR animal*:de OR nonhuman/de) NOT ('human'/exp)) NOT ([Conference Abstract]/lim) NOT ('child'/exp NOT ('adult'/exp OR 'adolescent'/de)) | 5809 | 5769 |
| Medline ALL | Ovid | ((("Humeral Fractures"/) NOT (proximal OR distal).ab,ti,kf.) OR (((humer* OR forearm OR arm) ADJ3 shaft* ADJ3 fracture*)).ab,ti,kf.) AND (surgery.xs. OR exp "Orthopedic Fixation Devices"/ OR braces/ OR immobilization/ OR (surg* OR operat* OR nailing OR nails OR pins OR plate* OR plating OR (extern* ADJ3 fix*) OR screw* OR conservative* OR brace* OR bracing OR sling* OR plaster* OR cast OR casting OR nonoperat* OR nonsurg* OR Sarmiento OR splint* OR traction OR immobili*).ab,ti,kf.) NOT (exp Animals/ NOT Humans/) NOT (news OR congres* OR abstract* OR book* OR chapter* OR dissertation abstract*).pt. NOT ((exp Child/ OR exp Infant/) NOT (exp Adult/ OR exp Adolescent/)) | 2975 | 861 |
| Web of Science Core Collection | Web of Knowledge | TS = ((((humer* OR forearm OR arm) NEAR/3 shaft* NEAR/3 fracture*)) AND ((surg* OR operat* OR nailing OR nails OR pins OR plate* OR plating OR (extern* NEAR/3 fix*) OR screw* OR conservative* OR brace* OR bracing OR sling* OR plaster* OR cast OR casting OR nonoperat* OR nonsurg* OR Sarmiento OR splint* OR traction OR immobili*)) NOT ((child* OR infan* OR pediatric*) NOT (adult* OR elderly* OR geriatric*)) NOT ((animal* OR rat OR rats OR mouse OR mice OR murine OR dog OR dogs OR canine OR cat OR cats OR feline OR rabbit OR cow OR cows OR bovine OR rodent* OR sheep OR ovine OR pig OR swine OR porcine OR veterinar* OR chick* OR zebrafish* OR baboon* OR nonhuman* OR primate* OR cattle* OR goose OR geese OR duck OR macaque* OR avian* OR bird* OR fish*) NOT (human* OR patient* OR women OR woman OR men OR man))) AND DT = (Article OR Review OR Letter OR Early Access) | 749 | 91 |
| Cochrane Central Register of Controlled Trials | Wiley | (((humer* OR forearm OR arm) NEAR/3 shaft* NEAR/3 fracture*)):ab,ti,kw AND ((surg* OR operat* OR nailing OR nails OR pins OR plate* OR plating OR (extern* NEAR/3 fix*) OR screw* OR conservative* OR brace* OR bracing OR sling* OR plaster* OR cast OR casting OR nonoperat* OR nonsurg* OR Sarmiento OR splint* OR traction OR immobili*):ab,ti,kw) NOT ((child* OR infan* OR pediatric*) NOT (adult* OR elderly* OR geriatric*)):ab,ti,kw | 92 | 33 |
| Total | 9625 | 6754 | ||
Search performed July 30, 2021
Eligibility criteria
Studies were included if they reported primary treatment of a humeral shaft fracture in patients aged 16 years or older with functional bracing, intramedullary nailing, or plate osteosynthesis. All study designs, except case reports, meta-analyses, and reviews, were included.
Studies were excluded if they met one or more of the following exclusion criteria: (1) recurrent, pathological, or periprosthetic fractures, (2) proximal or distal metaphyseal fracture extension, (3) grade III Gustilo Anderson open fractures, (4) treatment with external fixator, (5) experimental treatment, (6) outcome of less than five patients reported, (7) less than 6 months follow-up, (8) published before the year 2000 or (9) alternative operative methods for humeral shaft fractures (e.g., Ender nails, Marchetti nails, Rushs nails, Hackethal nailing, K wires, expandable, and flexible or elastic nails). Studies that reported on patients with concomitant injuries, such as vascular injury, compartment syndrome, or ipsilateral forearm fractures, were not excluded.
Study selection
First, four reviewers (KCM, SHVB, TVDT, and CAWN) independently screened the titles and abstracts of the studies to identify eligible studies. Inconsistencies were resolved by consensus. Second, the full-text articles of the remaining eligible publications were retrieved. The corresponding authors of studies with no available full-text version were contacted once by email. Third, the full-text articles were independently reviewed by the aforementioned reviewers. Any disagreement was resolved through consensus. Furthermore, the references of the included studies were reviewed for additional studies that may have been missed.
Data collection and data items
Data were extracted from the reports independently by three reviewers (KCM, SHVB, and PAJ) using a predefined data sheet. From each study, information was extracted on: study design, publication characteristics, demographics, treatment characteristics (including type of treatment, antegrade or retrograde IMN, ORPO, or MIPO), fracture classification according to the AO/OTA classification, complications, range of motion, and functional outcome scores, including patients-reported outcome measures (PROMs).
Fracture healing (time) was defined as (time to) radiologic or clinical fracture healing. Nonunion was defined as failure to heal at 6 months post-fracture with no progress toward healing seen on the most recent radiographs. Malunion was defined as fracture healing in an abnormal position. Primary radial nerve palsy was defined as radial nerve palsy as a result of initial trauma. Secondary radial nerve palsy was defined as radial nerve palsy as a result of reposition, during non-operative treatment or surgery. Implant failure was defined as the failure of the medical implant. Intraoperative complications included any deviation from the ideal intraoperative course occurring between skin incision and skin closure. Infection was defined as clinically diagnosed infection of (surgical) wounds as a consequence (of the treatment) of the humeral shaft fracture. Shoulder dysfunction was defined as experiencing pain or limited range of motion of the shoulder. Nail protrusion was defined as migration and subsequent protrusion of the intramedullary nail. Subacromial impingement was defined as irritation of the rotator cuff muscles in the subacromial space. (Sub)cutaneous problems included bursitis, cellulitis, granuloma’s, hypertrophic scarring of the wound, and skin irritation, macerations, or abrasions due to prolonged contact with the brace.
When measurements were done at different time points, the outcomes at the 12 months follow-up were used for calculation. The extracted data were compared, and disagreements were resolved by discussion between the three reviewers. Consensus was reached by discussion.
Risk of bias assessment
The Methodological Index for Non-Randomized Studies (MINORS) instrument was used to assess methodological quality of the included publications [28]. The MINORS scale yields a maximum score of 24 for comparative cohort studies and a maximum of 16 for non-comparative cohort studies, with a higher score indicating better quality. Studies were scored for the various items by three authors (KCM, SHVB, and PAJ) independently. Any disagreement was resolved by consensus. Funnel plots, for each outcome and per treatment type separately, were used to determine the risk of publication bias.
Statistical analysis
Data were analyzed using MedCalc Statistical Software (Version 18.2.1; MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org; 2018). Binary outcomes were transformed using a double arcsine transformation to ensure normal distribution [29]. The transformed rates and 95% confidence intervals were transformed back to prevalence estimates. Forest plots were constructed with 95% confidence intervals. Heterogeneity was quantified with Cochran’s Q test and I2 statistic. For the Cochran's Q test, a p value < 0.10 was considered statistically significant. A random effects model was used if the I2 statistic was > 40%. Otherwise, a fixed-effect model was used. Pooled percentages and means were calculated for binary and continuous variables, respectively, and are reported with their 95% confidence intervals (CI). Results are reported per treatment modality or per subgroup if differences between subgroups were deemed relevant.
Results
Study selection
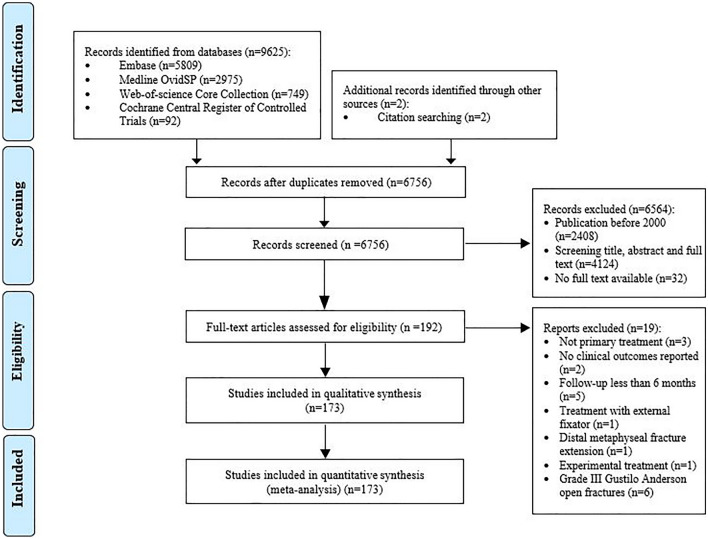
The search strings identified 9625 publications (Fig. 1). Duplicates were removed, resulting in 6754 unique publications. Two additional records were identified through other sources (citation searching). The remaining 6756 publications were reviewed for inclusion and exclusion criteria. A total of 192 eligible publications were identified. For 39, studies the full-text manuscripts were not available online. Of these, 13 publications had no contact details available. The remaining corresponding authors were contacted. This revealed seven full-text publications. After full-text assessment, 173 publications were included in this review and meta-analysis (Supplemental Table S1).
Fig. 1.
Flow diagram of study selection
Study characteristics
Supplemental Table S1 shows the study characteristics of all included studies. Of the 173 included studies, 23 were randomized controlled trials, 55 were prospective cohort studies, and 95 were retrospective cohort studies. A total of 79 studies were comparative studies and 94 studies were non-comparative. The included studies report on a total of 11,868 patients. Of these, 2204 were treated non-operatively with a functional brace, 3545 were treated with intramedullary nailing, and 6119 by plate osteosynthesis. The pooled mean age of the patients was 44 years in the non-operative group, 45 in the IMN group, and 41 in the plating group. The pooled mean percentage of males was 57% in the non-operative group, 62% in the IMN group, and 64% in the plate group. The pooled percentage of patients with AO type A fractures was 67% in the non-operative group, 53% in the IMN group, and 46% in the plating group. The pooled percentage of patients with AO type B fractures was 23% in the non-operative group, 34% in the IMN group, and 36% in the plating group. The pooled percentage of patients with AO type C fractures was 9% in the non-operative group, 12% in the IMN group, and 15% in the plating group.
Risk of bias assessment
The outcome of the methodological quality assessment, according to the MINORS score, is shown in Supplemental Table S2. The average score of the quality assessment for comparative studies was 20/24 (range 11–23) and 12/16 points (range 9–15) for non-comparative studies.
Fracture healing—time to union
Time to fracture healing (radiologic or clinical) was reported in 37 studies (Table 2). The pooled estimate time to fracture healing was 16 weeks (95% CI 14–18 weeks) for the non-operative group, 14 weeks (95% CI 13–15 weeks) for the IMN group, and 15 weeks (95% CI 14–16 weeks) for the plate group. An antegrade IMN approach resulted in a pooled estimate time to fracture healing of 14 weeks (95% CI 12–15 weeks) versus 12 weeks (95% CI 9–16 weeks) after a retrograde approach. Furthermore, considering plate osteosynthesis, ORPO resulted in a pooled estimate time to fracture healing of 16 weeks (95% CI 15–17 weeks) versus 14 weeks (95% CI 12–16 weeks) after MIPO. Much heterogeneity of effects was seen across studies in all treatment groups, varying from 91% in the MIPO group to 98% in the (antegrade) IMN group.
Table 2.
Fracture healing of a humeral shaft fracture per treatment group
| Treatment | Study arms | Population | Cases | Heterogeneity | Pooled value | ||
|---|---|---|---|---|---|---|---|
| N | N | N | Cochran’s Q (p value) | I2 (%) (95% CI) | (95% CI) | ||
| Fracture healing timea (weeks) [7, 10, 13, 57, 58, 60, 66, 70, 96, 106, 107, 112, 118, 119, 121, 126, 129, 131, 132, 134, 135, 144, 150, 151, 160, 162, 163, 166, 171, 176, 177, 181–184, 186, 192] | Non-operative | 5 | 286 | N.A | 60 (< 0.001) | 93 (87–97) | 16.4 (14.4–18.4) |
| IMN | 21 | 819 | N.A | 977 (< 0.001) | 98 (98–98) | 13.8 (12.5–15.1) | |
| Antegrade | 17 | 654 | N.A | 777 (< 0.001) | 98 (97–98) | 13.8 (12.4–15.2) | |
| Retrograde | 3 | 87 | N.A | 56 (< 0.001) | 96 (92–98) | 12.4 (9.1–15.8) | |
| Plate | 41 | 1392 | N.A | 1555 (< 0.001) | 97 (97–98) | 15.4 (14.4–16.4) | |
| ORPO | 31 | 1194 | N.A | 1416 (< 0.001) | 98 (98–98) | 15.8 (14.7–17.0) | |
| MIPO | 10 | 198 | N.A | 101 (< 0.001) | 91 (86–94) | 14.1 (12.2–15.9) | |
| Fracture healingb (%) [1, 3, 5, 7, 10, 11, 13, 22, 30–76, 79–85, 87–97, 99, 100, 102–107, 110–120, 122–139, 141–150, 152–186, 188–194] | Non-operative | 26 | 1979 | 1770 | 193 (< 0.001) | 87 (82–91) | 89 (84–92) |
| IMN | 73 | 2990 | 2811 | 156 (< 0.001) | 54 (40–65) | 94 (92–95) | |
| Antegrade | 55 | 2195 | 2060 | 88 (< 0.001) | 39 (15–56) | 94 (92–95) | |
| Retrograde | 8 | 265 | 255 | 9 (0.221) | 26 (0–67) | 94 (91–97) | |
| Plate | 136 | 5226 | 5030 | 227 (< 0.001) | 41 (27–52) | 96 (95–97) | |
| ORPO | 91 | 3896 | 3728 | 171 (< 0.001) | 47 (33–59) | 96 (95–96) | |
| MIPO | 45 | 1330 | 1302 | 46 (0.394) | 4 (0–31) | 98 (97–98) | |
| Nonunionc (%) [1, 5, 7, 10, 22, 30–33, 35–39, 41–50, 53–60, 62–76, 79–90, 92–95, 97, 99, 100, 102–106, 110–114, 116–120, 122–139, 141–150, 152–194] | Non-operative | 24 | 1959 | 182 | 175 (< 0.001) | 87 (82–91) | 11 (7–15) |
| IMN | 70 | 2787 | 156 | 106 (< 0.001) | 35 (12–51) | 6 (5–7) | |
| Antegrade | 55 | 2181 | 127 | 80 (0.013) | 32 (5–51) | 6 (5–8) | |
| Retrograde | 7 | 238 | 10 | 7 (0.278) | 20 (0–64) | 5 (2–8) | |
| Plate | 129 | 5098 | 163 | 205 (< 0.001) | 37 (22–50) | 3 (3–4) | |
| ORPO | 88 | 3865 | 139 | 167 (< 0.001) | 48 (33–60) | 4 (3–5) | |
| MIPO | 41 | 1233 | 24 | 33 (0.764) | 0 (0–23) | 2 (2–3) | |
| Maluniond (%) [5, 30, 31, 33, 43, 49, 50, 53, 57, 64, 69–71, 76, 79–81, 85–87, 91, 92, 94, 97, 99, 103–107, 110, 114, 115, 132, 138, 143, 144, 146, 148–151, 157, 160, 161, 163, 166, 168, 171, 176, 178, 180, 182, 183, 185, 188, 191–194] | Non-operative | 11 | 486 | 34 | 48 (< 0.001) | 79 (63–88) | 6 (2–12) |
| IMN | 22 | 798 | 23 | 53 (< 0.001) | 61 (37–75) | 3 (1–5) | |
| Antegrade | 17 | 555 | 20 | 50 (< 0.001) | 68 (47–81) | 3 (1–6) | |
| Retrograde | 1 | N.A | N.A | N.A | N.A | 0 (0–4) | |
| Plate | 59 | 1939 | 15 | 29 (1.000) | 0 (0–0) | 1 (1–2) | |
| ORPO | 37 | 1293 | 6 | 11 (1.000) | 0 (0–0) | 1 (1–2) | |
| MIPO | 22 | 646 | 9 | 15 (0.805) | 0 (0–26) | 2 (1–3) | |
95% CI 95% confidence interval, IMN intramedullary nailing, MIPO minimally invasive plate osteosynthesis, N.A. not applicable, ORPO open reduction plate osteosynthesis
aFracture healing time was defined as time to radiologic or clinical fracture healing
bFracture healing was defined as radiologic or clinical fracture healing
cNonunion was defined as failure to heal at 6 months post-fracture with no progress towards healing seen on the most recent radiographs
dMalunion was defined as fracture healing in an abnormal position
Fracture healing rate
In 160/173 (92%) studies consisting of 10,206 patients the fracture healing rate was reported (Table 2). The pooled fracture healing rate for the non-operative group was 89% (95% CI 84–92%), 94% (95% CI 92–95%) for the IMN group, and 96% (95% CI 95–97%) for the plating group. The pooled fracture healing rate was the highest in the MIPO group (98%; 95% CI 97–98%). In the non-operative group, high heterogeneity across studies was found (I2 = 87%) and seen in the funnel plot (Supplemental Fig. S1). In the IMN and plate group, the funnel plots showed comparable asymmetry and the heterogeneity was moderate (I2 = 54% and I2 = 41%, respectively; Supplemental Figure S1).
Fracture healing—nonunion
The pooled nonunion rate showed variation between the treatment groups (Table 2). In the non-operative group, 182 nonunions were reported in 1959 patients, resulting in a pooled estimate of 11% (95% CI 7–15%). In the IMN group, 156 nonunions were reported in 2787 patients, resulting in a pooled estimate of 6% (95% CI 5–7%) and in the plating group, 163 nonunions were reported in 5098 patients, resulting in a pooled estimate of 3% (95% CI 3–4%). In the plating group, an open approach resulted in more nonunions than a minimally invasive approach [4% (95% CI 3–5%) and 2% (95% CI 2–3%), respectively].
Fracture healing—malunion
Pooled malunion rates were 6% (95% CI 2–12%) in the non-operatively treated group, 3% (95% CI 1–5%) in the IMN group, and 1% (95% CI 1–2%) in the plating group (Table 2). However, malunion was often poorly defined and is expected to be reported differently across studies.
Complications—radial nerve palsy
The pooled primary radial nerve palsy rate showed no variation between the treatment groups (Table 3). Secondary radial palsy was reported in 146 studies (Table 3). The pooled secondary radial nerve palsy rate was 1% (95% CI 0–2%, 18 studies, N = 1377, 10 patients) in the non-operatively treated group, 3% (95% CI 2–3%, 58 studies, N = 2576, 66 patients) in the IMN group, 4% (95% CI 3–5%, 42 studies, N = 1292, 43 patients) in the MIPO group, and 7% (95% CI 6–9%, 82 studies, N = 4232, 275 patients) in the ORPO group.
Table 3.
Complication rates of (treatment of) a humeral shaft fracture per treatment group
| Treatment | Study arms | Population | Cases | Heterogeneity | Pooled value | ||||
|---|---|---|---|---|---|---|---|---|---|
| N | N | N | Cochran’s Q (p value) | I2 (%) (95% CI) | (%) (95% CI) | ||||
| Primary radial nerve palsya [1, 5, 7, 13, 22, 30, 33–36, 38–42, 44–49, 53–58, 60, 63, 65, 67, 69, 71, 73–75, 77, 80, 81, 83–85, 88, 89, 92–95, 98, 102–104, 106, 110, 112, 115, 116, 118, 119, 126, 131–136, 139–142, 145, 148, 149, 156, 157, 159, 160, 162, 166–170, 172–174, 176, 178–188, 190–194] | Non-operative | 23 | 1739 | 142 | 24 (0.364) | 7 (0–40) | 8 (7–10) | ||
| IMN | 44 | 1933 | 116 | 172 (< 0.001) | 75 (67–81) | 6 (4–8) | |||
| Antegrade | 31 | 1255 | 74 | 148 (< 0.001) | 80 (72–85) | 5 (3–8) | |||
| Retrograde | 6 | 213 | 11 | 8 (0.166) | 36 (0–75) | 5 (3–9) | |||
| Plate | 85 | 3371 | 291 | 494 (< 0.001) | 83 (79–86) | 6 (4–8) | |||
| ORPO | 62 | 2603 | 29 | 398 (< 0.001) | 85 (81–88) | 7 (4–9) | |||
| MIPO | 23 | 768 | 262 | 65 (< 0.001) | 66 (48–78) | 4 (2–7) | |||
| Secondary radial nerve palsyb [1, 5, 7, 10, 11, 13, 22, 30–43, 46–51, 53–56, 58–61, 63–71, 73, 75, 76, 78–85, 87–100, 102–108, 110–115, 117–123, 125–136, 139, 142–145, 147–152, 155–158, 160–162, 165–176, 178–188, 190–194] | Non-operative | 19 | 1377 | 10 | 36 (0.001) | 50 (15–71) | 1 (0–2) | ||
| IMN | 62 | 2576 | 66 | 81 (0.044) | 25 (0–45) | 3 (2–3) | |||
| Antegrade | 47 | 1872 | 39 | 57 (0.121) | 20 (0–45) | 2 (2–3) | |||
| Retrograde | 7 | 224 | 8 | 3 (0.751) | 0 (0–50) | 4 (2–8) | |||
| Plate | 136 | 5524 | 318 | 348 (< 0.001) | 61 (53–68) | 6 (5–7) | |||
| ORPO | 92 | 4232 | 275 | 287 (< 0.001) | 68 (61–74) | 7 (6–9) | |||
| MIPO | 44 | 1292 | 43 | 49 (0.250) | 12 (0–40) | 4 (3–5) | |||
| Intraoperative complicationsc [7, 22, 30, 31, 38, 39, 43, 58–60, 62, 63, 66, 67, 71, 73, 78, 80, 83–85, 90, 94, 97, 99, 104, 108, 112, 113, 119, 131, 135, 136, 139, 149, 150, 158, 162, 165, 167, 174, 176, 178–186, 188, 193, 194] | Non-operative | N.A | N.A | N.A | N.A | N.A | N.A | ||
| IMN | 40 | 1489 | 59 | 180 (< 0.001) | 78 (71–84) | 5 (3–8) | |||
| Antegrade | 27 | 872 | 33 | 62 (< 0.001) | 58 (35–73) | 4 (2–6) | |||
| Retrograde | 6 | 202 | 10 | 13 (< 0.001) | 63 (9–85) | 5 (1–11) | |||
| Plate | 43 | 1868 | 6 | 25 (0.980) | 0 (0–0) | 1 (0–1) | |||
| ORPO | 29 | 1409 | 4 | 18 (0.933) | 0 (0–7) | 1 (0–1) | |||
| MIPO | 14 | 459 | 2 | 7 (0.897) | 0 (0–18) | 1 (0–2) | |||
| Implant failured [5, 7, 10, 11, 31–33, 41, 42, 46, 48, 49, 54–56, 58–60, 62–64, 67, 68, 71, 73, 75, 76, 78, 83, 84, 86, 88, 90–92, 96, 97, 104, 105, 109, 113, 118, 119, 121, 122, 125, 132, 134, 135, 150, 152, 161, 162, 167–169, 176, 178–180, 182–186, 188, 193, 194] | Non-operative | N.A | N.A | N.A | N.A | N.A | N.A | ||
| IMN | 28 | 1034 | 51 | 48 (< 0.001) | 44 (12–64) | 4 (3–6) | |||
| Antegrade | 20 | 668 | 31 | 41 (< 0.001) | 54 (23–72) | 4 (2–6) | |||
| Retrograde | 3 | 128 | 8 | 3 (0.232) | 32 (0–98) | 7 (3–12) | |||
| Plate | 71 | 2839 | 40 | 88 (0.076) | 20 (0–41) | 2 (1–2) | |||
| ORPO | 50 | 2300 | 31 | 67 (0.043) | 27 (0–49) | 2 (1–3) | |||
| MIPO | 21 | 539 | 9 | 19 (0.515) | 0 (0–45) | 2 (1–4) | |||
|
Infectione [5, 7, 10, 22, 30–32, 37–39, 41, 43, 46, 48–50, 52, 54–56, 58, 60, 64, 67–73, 76–88, 90–93, 96, 97, 99, 100, 102–106, 108, 110–119, 121–123, 125–127, 129, 131, 133–135, 137, 139, 142–150, 152, 153, 155, 156, 158, 160–162, 165–176, 178–188, 190–194] |
Non-operative | 9 | 462 | 3 | 6 (0.685) | 0 (0–51) | 1 (0–2) | ||
| IMN | 60 | 2416 | 34 | 71 (0.143) | 16 (0–40) | 2 (1–2) | |||
| Antegrade | 48 | 1863 | 28 | 63 (0.059) | 25 (0–48) | 2 (1–2) | |||
| Retrograde | 6 | 235 | 2 | 5 (0.431) | 0 (0–75) | 1 (0–3) | |||
| Plate | 117 | 5108 | 124 | 193 (< 0.001) | 40 (25–52) | 3 (2–3) | |||
| ORPO | 83 | 3982 | 116 | 158 (< 0.001) | 48 (33–60) | 3 (3–4) | |||
| MIPO | 34 | 1126 | 8 | 22 (0.934) | 0 (0–7) | 1 (1–2) | |||
95% CI 95% confidence interval, IMN intramedullary nailing, MIPO minimally invasive plate osteosynthesis, N.A. not applicable, ORPO open reduction plate osteosynthesis
aPrimary radial nerve palsy was defined as radial nerve palsy as a result of initial trauma
bSecondary radial nerve palsy was defined as radial nerve palsy as a result of reposition, during non-operative treatment or surgery
cIntraoperative complications were defined as any deviation from the ideal intraoperative course occurring between skin incision and skin closure
dImplant failure was defined as the failure of the medical implant
eInfection was defined as clinically diagnosed infection of (surgical) wounds as a consequence (of the treatment) of the humeral shaft fracture
Complications—intraoperative complications
The pooled rate of intraoperative complications was 5% (95% CI 3–8%) in patients treated with an IMN and 1% (95% CI 0–1%) in patients treated with plate osteosynthesis (Table 3). Heterogeneity across studies was especially low in the plate group (I2 = 0%).
Complications—implant-related complications
Implant failures were reported more frequently in the IMN group (51/1034, pooled estimate of 4%; 95% CI 3–6%) than in patients in the plate group [pooled estimate of 2% (95% CI 1–2%), 40/2839 patients; Table 3]. An antegrade IMN approach resulted in less implant failures than a retrograde approach [4% (95% CI 3–6%) and 7% (95% CI 3–12%), respectively]. Implant failure did not differ between the surgical approaches in the plating group [ORPO 2% (95% CI 1–3%) and MIPO 2% (95% CI 1–4%)].
Complications—infection
The infection rate was reported in 124 studies consisting of 7986 patients, and was low in all treatment groups, especially in the non-operative [1% (95% CI 0–2%), 3/462 patients] and MIPO group [1% (95% CI 1–2%), 8/1126 patients; Table 3]. The infection rate in the IMN and ORPO group was 2% (95% CI 1–2%) and 3% (95% CI 3–4%), respectively.
Complications—shoulder dysfunction
The pooled rate of shoulder dysfunction was the highest in patients treated with an IMN (11%; 95% CI 8–15%) and the lowest in patients treated with plate osteosynthesis (6% (95% CI 4–8%); Supplemental Table S3). An antegrade IMN resulted in more shoulder dysfunction than a retrograde IMN [13% (95% CI 10–16%) and 5% (95% CI 1–15%), respectively].
Complications—nail protrusion
The pooled rate of nail protrusion was 10% (95% CI 6–14%) in patients treated with an IMN (17 studies, 61/666 patients; Supplemental Table S3).
Complications—subacromial impingement
Subacromial impingement was seen more in the antegrade IMN group than in the plate osteosynthesis group [pooled rate of 13% (95% CI 9–18%) and 2% (95% CI 1–3%), respectively; Supplemental Table S3].
Complications—(sub)cutaneous problems
The pooled rate of (sub)cutaneous problems in patients treated non-operatively was 6% (95% CI 4–9%, nine studies, 20/347 patients; Supplemental Table S3).
Range of motion
In the plating group, the pooled estimates of shoulder abduction and anteflexion were 151° (95% CI 116–186°) and 148° (95% CI 137–160°), respectively (Table 4). Anteflexion was better after MIPO than after ORPO [167° (95% CI 164–171°) and 141° (95% CI 124–158°), respectively]. In the IMN group, consisting of only 2 studies with a total of 34 patients, the pooled estimates of shoulder abduction and anteflexion were 132° (95% CI 76–189°) and 120° (95% CI 33–207°), respectively. All treatment groups showed high heterogeneity across studies, varying from 87% in the MIPO group to 100% in all other operative treatment groups.
Table 4.
Range of motion after treatment of a humeral shaft fracture per treatment group
| Study arms | Population | Heterogeneity | Pooled value | |||
|---|---|---|---|---|---|---|
| N | N | Cochran’s Q (p value) | I2 (%) (95% CI) | (degrees) (95% CI) | ||
| Shoulder abduction [76, 79, 115, 125, 153] | Non-operative | 0 | N.A | N.A | N.A | N.A |
| IMN | 2 | 34 | 309 (< 0.001) | 100 (99–100) | 132 (76–189) | |
| Antegrade | 2 | 34 | 309 (< 0.001) | 100 (99–100) | 132 (76–189) | |
| Retrograde | 0 | N.A | N.A | N.A | N.A | |
| Plate | 9 | 194 | 25,064 (< 0.001) | 100 (100–100) | 151 (116–186) | |
| ORPO | 8 | 146 | 19,692 (< 0.001) | 100 (100–100) | 148 (111–186) | |
| MIPO | 1 | N.A | N.A | N.A | N.A | |
| Shoulder anteflexion [10, 76, 79, 96, 107, 115, 153] | Non-operative | 0 | N.A | N.A | N.A | N.A |
| IMN | 2 | 34 | 181 (< 0.001) | 100 (99–100) | 120 (33–207) | |
| Antegrade | 2 | 34 | 181 (< 0.001) | 100 (99–100) | 120 (33–207) | |
| Retrograde | 0 | N.A | N.A | N.A | N.A | |
| Plate | 14 | 289 | 5444 (< 0.001) | 100 (100–100) | 148 (137–160) | |
| ORPO | 10 | 181 | 5202 (< 0.001) | 100 (100–100) | 141 (124–158) | |
| MIPO | 4 | 108 | 24 (< 0.001) | 87 (70–95) | 167 (164–171) | |
95% CI 95% confidence interval, IMN intramedullary nailing, MIPO minimally invasive plate osteosynthesis, N.A. not applicable, ORPO open reduction plate osteosynthesis
Functional outcome—DASH
The DASH score after on average 1 year (ranging from 6 to 24 months) showed variation in mean scores between the treatment groups (Table 5). For the non-operative group, the pooled estimate score was 17/100 (95% CI 3–31); for the IMN group, it was 23/100 (95% CI 17–29); and for the plating group, it was 13/100 (95% CI 8–19; Table 4). The DASH score was the highest in the antegrade IMN group (23/100; 95% CI 17–29) and the lowest in the MIPO group (7/100; 95% CI 1–13).
Table 5.
Functional outcome scores after treatment of a humeral shaft fracture per treatment group
| Instrument | Treatment | Study arms | Population | Heterogeneity | Pooled value | |
|---|---|---|---|---|---|---|
| N | N | Cochran’s Q (p value) | I2 (%) (95% CI) | (points) (95% CI) | ||
| DASH scorea [88, 115, 125, 134, 153, 161, 166, 168, 171, 173, 176, 182, 186, 188, 191] | Non-operative | 3 | 114 | 141 (< 0.001) | 99 (98–99) | 17 (3–31) |
| IMN | 5 | 192 | 181 (< 0.001) | 98 (97–99) | 23 (17–29) | |
| Antegrade | 5 | 192 | 181 (< 0.001) | 98 (97–99) | 23 (17–29) | |
| Retrograde | 0 | N.A | N.A | N.A | N.A | |
| Plate | 13 | 378 | 1292 (< 0.001) | 99 (99–99) | 13 (8–19) | |
| ORPO | 9 | 280 | 936 (< 0.001) | 99 (99–99) | 17 (9–24) | |
| MIPO | 4 | 98 | 97 (< 0.001) | 97 (94–98) | 7 (1–13) | |
| Constant–Murley scoreb [7, 11, 62, 66, 79, 110, 125, 128, 143, 153, 158, 161, 172, 176] | Non-operative | 1 | N.A | N.A | N.A | N.A |
| IMN | 9 | 499 | 2071 (< 0.001) | 100 (100–100) | 90 (85–95) | |
| Antegrade | 7 | 440 | 375 (< 0.001) | 98 (98–99) | 89 (85–93) | |
| Retrograde | 2 | 23 | N.A | N.A | N.A | |
| Plate | 13 | 569 | 199 (< 0.001) | 94 (91–96) | 93 (92–95) | |
| Open | 10 | 295 | 147 (< 0.001) | 94 (91–96) | 93 (91–95) | |
| MIPO | 3 | 274 | 48 (< 0.001) | 96 (91–98) | 93 (89–97) | |
| UCLA shoulder scorec [10, 107, 114, 115, 118, 127, 131, 160, 173] | Non-operative | 0 | N.A | N.A | N.A | N.A |
| IMN | 2 | 49 | 17 (< 0.001) | 94 (81–98) | 28 (22–34) | |
| Antegrade | 2 | 49 | 17 (< 0.001) | 94 (81–98) | 28 (22–34) | |
| Retrograde | 0 | N.A | N.A | N.A | N.A | |
| Plate | 15 | 501 | 385 (< 0.001) | 96 (95–97) | 33 (32–33) | |
| Open | 8 | 346 | 311 (< 0.001) | 98 (97–98) | 32 (32–33) | |
| MIPO | 7 | 155 | 69 (< 0.001) | 91 (85–95) | 33 (32–34) | |
95% CI 95% confidence interval, DASH Disabilities of the Arm, Ahoulder and Hand, IMN intramedullary nailing, MIPO minimally invasive plate osteosynthesis, N.A. not applicable, ORPO open reduction plate osteosynthesis, UCLA University of California at Los Angeles
aThe Disabilities of the Arm, Shoulder, and Hand (DASH) score ranges from 0 to100 points, with a lower score representing less disability [196, 197]
bThe Constant–Murley score ranges from 0 to 100 points, with a higher score representing better outcome [198]
cThe University of California at Los Angeles (UCLA) shoulder score ranges from 0 to 35 points, with a higher score representing better outcome [199]
Functional outcome—Constant–Murley
The pooled estimate of the Constant–Murley score was 90/100 (95% CI 85–95) in the IMN group and 93/100 (95% CI 92–95) in the plating group (Table 5). The Constant–Murley score did not differ between the surgical approaches in the treatment groups.
Functional outcome—UCLA
The pooled estimate of the UCLA shoulder score in the IMN group was 28/35 (95% CI 22–34) and 33/35 (95% CI 32–33) in the plating group (Table 5). The UCLA shoulder score did not differ between the surgical techniques in the treatment groups.
Functional outcome—other
Little to no differences were observed in the other functional outcome scores after IMN or plating osteosynthesis (Supplemental Table S4). Heterogeneity was high (I2 > 70%) in all subgroups for all functional outcomes, most likely due to the low number of studies with available data. For the non-operatively treated patients, little to no data of functional outcome scores were available for analyses.
The Broberg–Morrey, Gill, Hospital for Special Surgery, l’Insalata, Neer Shoulder, Oxford Shoulder Score, Quick-DASH, Rommens, Simple Shoulder Test, Short Musculoskeletal Functional Assessment, and Short Form-36, as well as the Hunter criteria did not have enough data reported for analyses. The nowadays seldom used Rodriguez–Merchan criteria were analyzed but not reported.
Discussion
This systematic review compared fracture healing, complications, and functional outcome of non-operative and operative treatment for humeral shaft fractures and results suggest that although all treatment modalities result in satisfactory outcomes, operative treatment, and specifically plate osteosynthesis, should be considered the preferred treatment as it results in the most favorable fracture healing rates, least complications, and best functional outcomes.
The current systematic review reveals that the risk to develop a nonunion after non-operative treatment is much higher (11%) than after any kind of surgical stabilization (6% and 3% in the IMN and plating group, respectively). This is in line with previous systematic reviews reporting higher absolute risks of nonunion after non-operative treatment (15% and 18%) and a risk ratio of 0.49 for nonunion in the operative group compared with in the non-operative group [8, 24, 25]. A first requirement for good functional recovery is fracture stability since it relieves pain in the upper limb. Stability can be achieved by fracture union, but also by relative or absolute surgical stabilization of a fresh fracture with IMN and plate osteosynthesis, respectively. A nonunion after non-operative treatment implicates that the patient has experienced pain and loss of function for months, whereas a patient who has been operated upon immediately after his injury has been able to recover functionally despite the development of the nonunion. In the balance of shared decision-making, such numbers call for a surgical and not a non-operative treatment.
The final goal of any type of treatment should be a good functional outcome. Overall, all treatment modalities result in satisfactory functional outcomes after 1 year, indicating that a good functional outcome can be achieved irrespective of treatment. However, a slight advantage of functional recovery can be found after operative treatment with plate osteosynthesis considering the Constant–Murley, DASH, and UCLA shoulder score. This is in line with a meta-analysis of RCTs describing better functional outcomes in patients treated with plate osteosynthesis than in patients treated with IMN [26]. Less complications and rotator cuff problems might enable these patients treated with plate osteosynthesis to regain function faster. These favorable results of functional recovery may tip the scale of the scientific debate toward plate osteosynthesis as the preferred treatment.
However, speed of functional recovery and a lower risk of nonunion after a humeral shaft fracture comes at a price. Both non-operative and operative treatment generate complications. The major complication is considered a radial nerve palsy. Primary nerve palsies are caused by the trauma itself, not by the therapy given to treat the injury. Secondary radial nerve palsy occurs from fracture reduction during non-operative treatment or manipulation during surgery. Not surprisingly, the rate of radial nerve palsy after non-operative treatment is much lower—albeit not absent—than after surgery in which the nerve is exposed. Within the operative group, the current systematic review showed a higher rate of secondary radial nerve palsy in the patients treated with (open) plating. However, the rate of persistent radial nerve palsy could not be defined due to the heterogeneity in reporting, and therefore questions about permanent disability after radial nerve palsy cannot be addressed. A meta-analysis of RCTs and observational studies, comparing non-operative and operative treatment, reported no difference in permanent (primary or secondary) radial nerve palsy rate between both groups suggesting that the risk of persistent radial nerve palsy should no longer be a deterrent for operative treatment [8]. Other complications inherent to operative treatment were more frequently reported in the IMN group than in the plating group. Results of other reviews are comparable, describing lower number of complications in the plating group than in the IMN group, suggesting plating is superior to IMN [18, 21, 26].
All previous meta-analyses only included randomized control trials and comparative prospective cohort studies of 6–17 published studies in total [8, 16–26]. A strength of the current study is that by including many study designs, it included all relevant recent comparative and non-comparative studies, resulting in 173 included studies reporting the results of 11,868 patients. In this way, this systematic review provides information on results of all relevant aspects of each treatment option, and therefore empowers both the patient and the doctor in their respective roles in the desired shared decision-making process.
However, some limitations of this study are the low methodological quality of the included studies as reflected by the MINORS scores. The studies meeting the inclusion criteria often had small sample sizes and lacked an adequate power calculation. Unfortunately, due to the lack of homogeneous reporting of, e.g., patient characteristics and treatment regimens of functional bracing, risk factor and subgroup analyses could not be performed. Furthermore, different outcome parameters and methods of reporting the results were used. Results were frequently reported without a standard deviation and thus could not be included in the pooled analysis. Therefore, the results of this study should be interpreted with care given the large statistical and clinical heterogeneity.
In the literature, a definitive answer on the optimal treatment strategy remains as high-quality data are lacking. This causes practice variation. Furthermore, uniform reporting of outcome of treatment is needed to compare the results of different studies. For instance, in the included studies, 18 different functional outcome scores were reported. The use of different instruments makes it hard to compare results. The DASH and Constant–Murley score have been validated and are recommended as preferred instruments for future studies [195].
Conclusion
This study suggests that even though all treatment modalities result in satisfactory outcomes, operative treatment is associated with the most favorable results. Disregarding secondary radial nerve palsy, specifically plate osteosynthesis seems to result in the highest fracture healing rates, least complications, and best functional outcomes compared with the other treatment modalities.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
SHVB, KCM, EMMVL, MHJV, and DDH have made contributions to the study design. SHVB, KCM, TVDT, CAWN, and PAJ performed data collection. EMMVL performed the statistical analysis. SHVB, KCM, EMMVL, MHJV, and DDH contributed to data interpretation. SHVB and KCM drafted the manuscript. All authors critically revised the manuscript, and read and approved the final manuscript.
Funding
No external funding was received for this study.
Data availability
No additional data are available. Data can be made available upon reasonable request to the principal investigator.
Declarations
Conflict of interest
The authors state that no conflicts of interest, financially or otherwise, exist.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sarmiento A, Zagorski JB, Zych GA, Latta LL, Capps CA. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Jt Surg Am. 2000;82:478–486. doi: 10.2106/00004623-200004000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Papasoulis E, Drosos GI, Ververidis AN, Verettas DA. Functional bracing of humeral shaft fractures. A review of clinical studies. Injury. 2010;41:e21–27. doi: 10.1016/j.injury.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 3.Rosenberg N, Soudry M. Shoulder impairment following treatment of diaphysial fractures of humerus by functional brace. Arch Orthop Trauma Surg. 2006;126:437–440. doi: 10.1007/s00402-006-0167-9. [DOI] [PubMed] [Google Scholar]
- 4.Walker M, Palumbo B, Badman B, Brooks J, Van Gelderen J, Mighell M. Humeral shaft fractures: a review. J Shoulder Elbow Surg. 2011;20:833–844. doi: 10.1016/j.jse.2010.11.030. [DOI] [PubMed] [Google Scholar]
- 5.Baltov A, Mihail R, Dian E. Complications after interlocking intramedullary nailing of humeral shaft fractures. Injury. 2014;45(Suppl 1):S9–S15. doi: 10.1016/j.injury.2013.10.044. [DOI] [PubMed] [Google Scholar]
- 6.Changulani M, Jain UK, Keswani T. Comparison of the use of the humerus intramedullary nail and dynamic compression plate for the management of diaphyseal fractures of the humerus. A randomised controlled study. Int Orthop. 2007;31:391–395. doi: 10.1007/s00264-006-0200-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Y, Wang C, Wang M, Huang L, Huang Q. Postoperative malrotation of humeral shaft fracture after plating compared with intramedullary nailing. J Shoulder Elbow Surg. 2011;20:947–954. doi: 10.12659/msm.924400. [DOI] [PubMed] [Google Scholar]
- 8.Van de Wall BJM, Ochen Y, Beeres FJP, et al. Conservative vs operative treatment for humeral shaft fractures: a meta-analysis and systematic review of randomized clinical trials and observation studies. J Shoulder Elbow Surg. 2020;29(7):1493–1504. doi: 10.1016/j.jse.2020.01.072. [DOI] [PubMed] [Google Scholar]
- 9.Zhao JG, Wang J, Meng XH, Zeng XT, Kan SL. Surgical interventions to treat humerus shaft fractures: a network meta-analysis of randomized controlled trials. PLoS ONE. 2017;12:e0173634. doi: 10.1371/journal.pone.0173634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.An Z, Zeng B, He X, Chen Q, Hu S. Plating osteosynthesis of mid-distal humeral shaft fractures: minimally invasive versus conventional open reduction technique. Int Orthop. 2010;34:131–135. doi: 10.1007/s00264-009-0753-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen Y, Qiang M, Zhang K, Li H, Dai H. Novel computer-assisted preoperative planning system for humeral shaft fractures: report of 43 cases. Int J Med Robot. 2015;11:109–119. doi: 10.1002/rcs.1604. [DOI] [PubMed] [Google Scholar]
- 12.Huttunen TT, Kannus P, Lepola V, Pihlajamaki H, Mattila VM. Surgical treatment of humeral-shaft fractures: a register-based study in Finland between 1987 and 2009. Injury. 2012;43:1704–1708. doi: 10.1016/j.injury.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 13.Mahabier KC, Vogels LMM, Punt BJ, Roukema GR, Patka P, Van Lieshout EMM. Humeral shaft fractures: retrospective results of non-operative and operative treatment of 186 patients. Injury. 2013;44:427–430. doi: 10.1016/j.injury.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 14.Schoch BS, Padegimas EM, Maltenfort M, Krieg J, Namdari S. Humeral shaft fractures: national trends in management. J Orthop Traumatol. 2017;18:259–263. doi: 10.1007/s10195-017-0459-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Steffner RJ, Lee MA. Emerging concepts in upper extremity trauma: humeral shaft fractures. Orthop Clin N Am. 2013;44:21–33. doi: 10.1016/j.ocl.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 16.Beeres FJP, van Veelen N, Houwert RM, et al. Open plate fixation versus nailing for humeral shaft fractures: a meta-analysis and systematic review of randomised clinical trials and observational studies. Eur J Trauma Emerg Surg. 2022;48(4):2667–2682. doi: 10.1007/s00068-021-01728-7. [DOI] [PubMed] [Google Scholar]
- 17.Heineman DJ, Bhandari M, Poolman RW. Plate fixation or intramedullary fixation of humeral shaft fractures—an update. Acta Orthop. 2012;83:317–318. doi: 10.3109/17453674.2012.695677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hohmann E, Glatt V, Tetsworth K. Minimally invasive plating versus either open reduction and plate fixation or intramedullary nailing of humeral shaft fractures: a systematic review and meta-analysis of randomized controlled trials. J Shoulder Elbow Surg. 2016;25:1634–1642. doi: 10.1016/j.jse.2016.05.014. [DOI] [PubMed] [Google Scholar]
- 19.Keshav K, Baghel A, Kumar V, Neradi D, Kaustubh K, Mishra P. Is minimally invasive plating osteosynthesis better than conventional open plating for humeral shaft fractures? A systematic review and meta-analysis of comparative studies. Indian J Orthop. 2021;55(Suppl 2):283–303. doi: 10.1007/s43465-021-00413-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ouyang H, Xiong J, Xiang P, Cui Z, Chen L, Yu B. Plate versus intramedullary nail fixation in the treatment of humeral shaft fractures: an updated meta-analysis. J Shoulder Elbow Surg. 2013;22:387–395. doi: 10.1016/j.jse.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 21.Qiu H, Wei Z, Liu Y, Dong J, Zhou X, Yin L, et al. A Bayesian network meta-analysis of three different surgical procedures for the treatment of humeral shaft fractures. Medicine (Baltimore) 2016;95:e5464. doi: 10.1097/MD.0000000000005464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rommens PM, Kuechle R, Bord T, Lewens T, Engelmann R, Blum J. Humeral nailing revisited. Injury. 2008;39:1319–1328. doi: 10.1016/j.injury.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 23.Clement ND. Management of humeral shaft fractures; non-operative versus operative. Arch Trauma Res. 2015;4:e28013. doi: 10.5812/atr.28013v2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lode I, Nordviste V, Erichsen JL, Schmal H, Viberg B. Operative versus nonoperative treatment of humeral shaft fractures: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2020;29(12):2495–2504. doi: 10.1016/j.jse.2020.05.030. [DOI] [PubMed] [Google Scholar]
- 25.Sargeant HW, Farrow L, Barker S, Kumar K. Operative versus non-operative treatment of humeral shaft fractures: a systematic review. Shoulder Elbow. 2020;12(4):229–242. doi: 10.1177/1758573218825477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang X, Chen Z, Shao Y, Ma Y, Fu D, Xia Q. A meta-analysis of plate fixation versus intramedullary nailing for humeral shaft fractures. J Orthop Sci. 2013;18:388–397. doi: 10.1007/s00776-013-0355-8. [DOI] [PubMed] [Google Scholar]
- 27.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 29.Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health. 2013;67:974–978. doi: 10.1136/jech-2013-203104. [DOI] [PubMed] [Google Scholar]
- 30.Chapman JR, Henley MB, Agel J, Benca PJ. Randomized prospective study of humeral shaft fracture fixation: intramedullary nails versus plates. J Orthop Trauma. 2000;14:162–166. doi: 10.1097/00005131-200003000-00002. [DOI] [PubMed] [Google Scholar]
- 31.McCormack RG, Brien D, Buckley RE, McKee MD, Powell J, Schemitsch EH. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail. A prospective, randomised trial. J Bone Jt Surg Br. 2000;82:336–339. doi: 10.1302/0301-620X.82B3.0820336. [DOI] [PubMed] [Google Scholar]
- 32.Paris H, Tropiano P, Clouet D'orval B, Chaudet H, Poitout DG. [Fractures of the shaft of the humerus: systematic plate fixation. Anatomic and functional results in 156 cases and a review of the literature] Fractures diaphysaires de l'humerus : osteosynthese systematique par plaque. Resultats anatomiques et fonctionnels d'une serie de 156 cas et revue de la litterature] Rev Chir Orthop Reparatrice Appar Mot. 2000;86:346–359. [PubMed] [Google Scholar]
- 33.Tingstad EM, Wolinsky PR, Shyr Y, Johnson KD. Effect of immediate weightbearing on plated fractures of the humeral shaft. J Trauma. 2000;49:278–280. doi: 10.1097/00005373-200008000-00014. [DOI] [PubMed] [Google Scholar]
- 34.Blum J, Janzing H, Gahr R, Langendorff HS, Rommens PM. Clinical performance of a new medullary humeral nail: antegrade versus retrograde insertion. J Orthop Trauma. 2001;15:342–349. doi: 10.1097/00005131-200106000-0007. [DOI] [PubMed] [Google Scholar]
- 35.Koch PP, Gross DF, Gerber C. The results of functional (Sarmiento) bracing of humeral shaft fractures. J Shoulder Elbow Surg. 2002;11:143–150. doi: 10.1067/mse.2002.121634. [DOI] [PubMed] [Google Scholar]
- 36.Chaker A, Filipinsky J. [Sport-related spiral fractures of the humeral diaphysis are not simple injuries] Sportovni spiralni zlomeniny diafyzy humeru nejsou jednoduchym poranenim. Rozhl Chir. 2003;82(235–238):44. [PubMed] [Google Scholar]
- 37.Kesemenli CC, Subasi M, Arslan H, Necmioglu S, Kapukaya A. [Comparison between the results of intramedullary nailing and compression plate fixation in the treatment of humerus fractures] Humerus kirikli olgularda kilitli intrameduller civi ve plak ile tedavi sonuclarinin karsilastirilmasi. Acta Orthop Traumatol Turc. 2003;37:120–125. [PubMed] [Google Scholar]
- 38.Ni JD, Tan J. Dong ZG [Treatment of humeral shaft fractures with Russell–Taylor interlocking intramedullar nail] Hunan Yi Ke Da Xue Xue Bao. 2003;28:159–161. [PubMed] [Google Scholar]
- 39.Fernandez FF, Matschke S, Hulsenbeck A, Egenolf M, Wentzensen A. Five years' clinical experience with the unreamed humeral nail in the treatment of humeral shaft fractures. Injury. 2004;35:264–271. doi: 10.1016/s0020-1383(03)00220-1. [DOI] [PubMed] [Google Scholar]
- 40.Flinkkila T, Hyvonen P, Siira P, Hamalainen M. Recovery of shoulder joint function after humeral shaft fracture: a comparative study between antegrade intramedullary nailing and plate fixation. Arch Orthop Trauma Surg. 2004;124:537–541. doi: 10.1007/s00402-004-0727-9. [DOI] [PubMed] [Google Scholar]
- 41.Livani B, Belangero WD. Bridging plate osteosynthesis of humeral shaft fractures. Injury. 2004;35:587–595. doi: 10.1016/j.injury.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 42.Niall DM, O'Mahony J, McElwain JP. Plating of humeral shaft fractures–has the pendulum swung back? Injury. 2004;35:580–586. doi: 10.1016/j.injury.2003.10.021. [DOI] [PubMed] [Google Scholar]
- 43.Chao TC, Chou WY, Chung JC, Hsu CJ. Humeral shaft fractures treated by dynamic compression plates, Ender nails and interlocking nails. Int Orthop. 2005;29:88–91. doi: 10.1007/s00264-004-0620-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kirdemir V, Sehirlioglu A, Baykal B, Bek D, Demiralp B. The results for the treatment of humeral shaft fractures using functional bracing. Gulhane Med J. 2005;47:40–43. [Google Scholar]
- 45.Toivanen JA, Nieminen J, Laine HJ, Honkonen SE, Jarvinen MJ. Functional treatment of closed humeral shaft fractures. Int Orthop. 2005;29:10–13. doi: 10.1007/s00264-004-0612-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Apard T, Lahogue JF, Prove S, Hubert L, Talha A, Cronier P, et al. [Retrograde locked nailing of humeral shaft fractures: a prospective study of 58 cases] Traitement des fractures recentes de la diaphyse humerale par enclouage centromedullaire verrouille retrograde: une etude prospective de 58 cas. Rev Chir Orthop Reparatrice Appar Mot. 2006;92:19–26. doi: 10.1016/S0035-1040(06)75670-7. [DOI] [PubMed] [Google Scholar]
- 47.Ekholm R, Tidermark J, Tornkvist H, Adami J, Ponzer S. Outcome after closed functional treatment of humeral shaft fractures. J Orthop Trauma. 2006;20:591–596. doi: 10.1097/01.bot.0000246466.01287.04. [DOI] [PubMed] [Google Scholar]
- 48.Hernandez C, Villanueva M, Juarez J, Torres M, Esparragoza L, Benito F. Technical complications of Seidel's nailing of the humerus. Rev Ortop Traumatol. 2006;50:342–353. [Google Scholar]
- 49.Jawa A, McCarty P, Doornberg J, Harris M, Ring D. Extra-articular distal-third diaphyseal fractures of the humerus. A comparison of functional bracing and plate fixation. J Bone Jt Surg Am. 2006;88:2343–2347. doi: 10.2106/JBJS.F.00334. [DOI] [PubMed] [Google Scholar]
- 50.Martinez-Diaz S, Ramirez M, Marques F, Gines A, Monllau JC, Martinez-Gomez X, et al. Fracturas diafisarias de húmero en mayores de 60 años: enclavado intramedular rigido [Rigid intramedullary nailing of humeral shaft fractures in patients older than 60] Rev Ortop Traumatol. 2006;50:8–13. doi: 10.1016/S0482-5985(06)74927-6. [DOI] [Google Scholar]
- 51.Pospula W, Abu NT. Percutaneous fixation of comminuted fractures of the humerus: initial experience at Al Razi hospital Kuwait. Med Princ Pract. 2006;15:423–426. doi: 10.1159/000095487. [DOI] [PubMed] [Google Scholar]
- 52.Rochet S, Obert L, Sarlieve P, Clappaz P, Lepage D, Garbuio P, et al. [Functional and sonographic shoulder assessment after Seidel nailing: a retrospective of 29 cases] Evaluation fonctionnelle et echographique de l'epaule apres enclouage de Seidel. Rev Chir Orthop Reparatrice Appar Mot. 2006;92:549–555. doi: 10.1016/S0035-1040(06)75912-8. [DOI] [PubMed] [Google Scholar]
- 53.Rutgers M, Ring D. Treatment of diaphyseal fractures of the humerus using a functional brace. J Orthop Trauma. 2006;20:597–601. doi: 10.1097/01.bot.0000249423.48074.82. [DOI] [PubMed] [Google Scholar]
- 54.Cuny C, Irrazi M, Ionescu N, Locquet V, Chaumont PL, Berrichi A, et al. [The long Telegraph nail for humeral fractures] Le clou Telegraph long dans les fractures de l'humerus. Rev Chir Orthop Reparatrice Appar Mot. 2007;93:564–570. doi: 10.1016/S0035-1040(07)92678-1. [DOI] [PubMed] [Google Scholar]
- 55.Jiang R, Luo CF, Zeng BF, Mei GH. Minimally invasive plating for complex humeral shaft fractures. Arch Orthop Trauma Surg. 2007;127:531–535. doi: 10.1007/s00402-007-0313-z. [DOI] [PubMed] [Google Scholar]
- 56.Numbela BX, Aceves LH, Gonzalez AB, Castro CT. [Minimally invasive surgery in diaphyseal humeral fractures with helicoidal plate. One year result in seven patients] Placa helicoidal aplicada en fracturas diafisarias de humero por cirugia de minima invasion (MIS). Resultados de un ano de seguimiento en 7 casos. Acta Ortop Mex. 2007;21:239–246. [PubMed] [Google Scholar]
- 57.Ozkurt B, Altay M, Aktekin CN, Toprak A, Tabak Y. [The role of functional bracing in the treatment of humeral shaft fractures] Humerus cisim kiriklarinda fonksiyonel breys tedavisinin yeri. Acta Orthop Traumatol Turc. 2007;41:15–20. [PubMed] [Google Scholar]
- 58.Raghavendra S, Bhalodiya HP. Internal fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail: a prospective study. Indian J Orthop. 2007;41:214–218. doi: 10.4103/0019-5413.33685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhiquan A, Bingfang Z, Yeming W, Chi Z, Peiyan H. Minimally invasive plating osteosynthesis (MIPO) of middle and distal third humeral shaft fractures. J Orthop Trauma. 2007;21:628–633. doi: 10.1097/BOT.0b013e31815928c2. [DOI] [PubMed] [Google Scholar]
- 60.Cheng HR, Lin J. Prospective randomized comparative study of antegrade and retrograde locked nailing for middle humeral shaft fracture. J Trauma. 2008;65:94–102. doi: 10.1097/TA.0b013e31812eed7f. [DOI] [PubMed] [Google Scholar]
- 61.Ekholm R, Ponzer S, Tornkvist H, Adami J, Tidermark J. The Holstein–Lewis humeral shaft fracture: aspects of radial nerve injury, primary treatment, and outcome. J Orthop Trauma. 2008;22:693–697. doi: 10.1097/BOT.0b013e31818915bf. [DOI] [PubMed] [Google Scholar]
- 62.Muckley T, Diefenbeck M, Sorkin AT, Beimel C, Goebel M, Buhren V. Results of the T2 humeral nailing system with special focus on compression interlocking. Injury. 2008;39:299–305. doi: 10.1016/j.injury.2007.08.031. [DOI] [PubMed] [Google Scholar]
- 63.An Z, He X, Zeng B. A comparative study on open reduction and plating osteosynthesis and minimal invasive plating osteosynthesis in treating mid-distal humeral shaft fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2009;23:41–44. [PubMed] [Google Scholar]
- 64.Apivatthakakul T, Phornphutkul C, Laohapoonrungsee A, Sirirungruangsarn Y. Less invasive plate osteosynthesis in humeral shaft fractures. Oper Orthop Traumatol. 2009;21:602–613. doi: 10.1007/s00064-009-2008-9. [DOI] [PubMed] [Google Scholar]
- 65.Ji F, Tong D, Tang H, Cai X, Zhang Q, Li J, et al. Minimally invasive percutaneous plate osteosynthesis (MIPPO) technique applied in the treatment of humeral shaft distal fractures through a lateral approach. Int Orthop. 2009;33:543–547. doi: 10.1007/s00264-008-0522-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li WY, Zhang BS, Zhang L, Zheng SH, Wang S. Comparative study of antegrade and retrograde intramedullary nailing for the treatment of humeral shaft fractures. Zhongguo Gu Shang. 2009;22:199–201. [PubMed] [Google Scholar]
- 67.Putti AB, Uppin RB, Putti BB. Locked intramedullary nailing versus dynamic compression plating for humeral shaft fractures. J Orthop Surg (Hong Kong) 2009;17:139–141. doi: 10.1177/230949900901700202. [DOI] [PubMed] [Google Scholar]
- 68.Wang ZH, Xiang M, Xie J, Tang HC, Chen H, Liu X. Treatment of humerus shaft fractures using minimally invasive percutaneous plate osteosynthesis through anterior approach. Zhongguo Gu Shang. 2009;22:681–683. [PubMed] [Google Scholar]
- 69.Concha JM, Sandoval A, Streubel PN. Minimally invasive plate osteosynthesis for humeral shaft fractures: are results reproducible? Int Orthop. 2010;34:1297–1305. doi: 10.1007/s00264-009-0893-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Denard A, Jr, Richards JE, Obremskey WT, Tucker MC, Floyd M, Herzog GA. Outcome of nonoperative vs operative treatment of humeral shaft fractures: a retrospective of 213 patients. Orthopedics. 2010 doi: 10.3928/01477447-20100625-16. [DOI] [PubMed] [Google Scholar]
- 71.Denies E, Nijs S, Sermon A, Broos P. Operative treatment of humeral shaft fractures. Comparison of plating and intramedullary nailing. Acta Orthop Belg. 2010;76:735–742. [PubMed] [Google Scholar]
- 72.Kobayashi M, Watanabe Y, Matsushita T. Early full range of shoulder and elbow motion is possible after minimally invasive plate osteosynthesis for humeral shaft fractures. J Orthop Trauma. 2010;24:212–216. doi: 10.1097/BOT.0b013e3181c2fe49. [DOI] [PubMed] [Google Scholar]
- 73.Singisetti K, Ambedkar M. Nailing versus plating in humerus shaft fractures: a prospective comparative study. Int Orthop. 2010;34:571–576. doi: 10.1007/s00264-009-0813-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yin B, Yang B, Li J, Zhang Z, Zhang L, Song L, et al. Antegrade intramedullary nailing versus retrograde intramedullary nailing for humeral shaft fracture in 18 cases. J Clin Rehab Tissue Eng Res. 2010;14:4899–4902. doi: 10.3969/j.issn.1673-8225.2010.26.037. [DOI] [Google Scholar]
- 75.Ziran BH, Kinney RC, Smith WR, Peacher G. Sub-muscular plating of the humerus: an emerging technique. Injury. 2010;41:1047–1052. doi: 10.1016/j.injury.2010.04.021. [DOI] [PubMed] [Google Scholar]
- 76.Algarin-Reyes JA, Bello-Gonzalez A, Perez-Calzadilla M, Flores-Giron J. [Treatment of distal humeral shaft fractures at Polanco Mexican Red Cross] Tratamiento de las fracturas diafisarias del tercio distal de humero en la Cruz Roja Mexicana Polanco. Acta Ortop Mex. 2011;25:264–272. [PubMed] [Google Scholar]
- 77.Grass G, Kabir K, Ohse J, Rangger C, Besch L, Mathiak G. Primary exploration of radial nerve is not required for radial nerve palsy while treating humerus shaft fractures with Unreamed Humerus Nails (UHN) Open Orthop J. 2011;5:319–323. doi: 10.2174/1874325001105010319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kirin I, Jurisic D, Grebic D, Nadalin S. The advantages of humeral anteromedial plate osteosynthesis in the middle third shaft fractures. Wien Klin Wochenschr. 2011;123:83–87. doi: 10.1007/s00508-010-1523-x. [DOI] [PubMed] [Google Scholar]
- 79.Li Y, Tian Q, Leng K, Guo M. Comparison of the posterior and anterolateral surgical approaches in the treatment of humeral mid-shaft fractures: a retrospective study. Med Sci Monit. 2020 doi: 10.12659/MSM.924400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lopez-Arevalo R, de Llano-Temboury AQ, Serrano-Montilla J, de Llano-Gimenez EQ, Fernandez-Medina JM. Treatment of diaphyseal humeral fractures with the minimally invasive percutaneous plate (MIPPO) technique: a cadaveric study and clinical results. J Orthop Trauma. 2011;25:294–299. doi: 10.1097/BOT.0b013e3181f98421. [DOI] [PubMed] [Google Scholar]
- 81.Prasarn ML, Ahn J, Paul O, Morris EM, Kalandiak SP, Helfet DL, et al. Dual plating for fractures of the distal third of the humeral shaft. J Orthop Trauma. 2011;25:57–63. doi: 10.1097/BOT.0b013e3181df96a7. [DOI] [PubMed] [Google Scholar]
- 82.Shetty MS, Kumar MA, Sujay K, Kini AR, Kanthi KG. Minimally invasive plate osteosynthesis for humerus diaphyseal fractures. Indian J Orthop. 2011;45:520–526. doi: 10.4103/0019-5413.87123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tsourvakas S, Alexandropoulos C, Papachristos I, Tsakoumis G, Ameridis N. Treatment of humeral shaft fractures with antegrade intramedullary locking nail. Musculoskelet Surg. 2011;95:193–198. doi: 10.1007/s12306-011-0126-7. [DOI] [PubMed] [Google Scholar]
- 84.Van Middendorp JJ, Kazacsay F, Lichtenhahn P, Renner N, Babst R, Melcher G. Outcomes following operative and non-operative management of humeral midshaft fractures: a prospective, observational cohort study of 47 patients. Eur J Trauma Emerg Surg. 2011;37:287–296. doi: 10.1007/s00068-011-0099-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Brunner A, Thormann S, Babst R. Minimally invasive percutaneous plating of proximal humeral shaft fractures with the Proximal Humerus Internal Locking System (PHILOS) J Shoulder Elbow Surg. 2012;21:1056–1063. doi: 10.1016/j.jse.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 86.Firat A, Deveci A, Guler F, Ocguder A, Oguz T, Bozkurt M. Evaluation of shoulder and elbow functions after treatment of humeral shaft fractures: a 20–132-month follow-up study. Acta Orthop Traumatol Turc. 2012;46:229–236. doi: 10.3944/aott.2012.2486. [DOI] [PubMed] [Google Scholar]
- 87.Iacobellis C, Agro T, Aldegheri R. Locked antegrade intramedullary nailing of humeral shaft fractures. Musculoskelet Surg. 2012;96:67–73. doi: 10.1007/s12306-011-0166-z. [DOI] [PubMed] [Google Scholar]
- 88.Idoine JD, 3rd, French BG, Opalek JM, DeMott L. Plating of acute humeral diaphyseal fractures through an anterior approach in multiple trauma patients. J Orthop Trauma. 2012;26:9–18. doi: 10.1097/BOT.0b013e318214ebd5. [DOI] [PubMed] [Google Scholar]
- 89.Kulkarni SG, Varshneya A, Jain M, Kulkarni VS, Kulkarni GS, Kulkarni MG, et al. Antegrade interlocking nailing versus dynamic compression plating for humeral shaft fractures. J Orthop Surg (Hong Kong) 2012;20:288–291. doi: 10.1177/230949901202000304. [DOI] [PubMed] [Google Scholar]
- 90.Kumar R, Singh P, Chaudhary LJ, Singh S. Humeral shaft fracture management, a prospective study; nailing or plating. J Clin Orthop Traum. 2012;3:37–42. doi: 10.1016/j.jcot.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Malhan S, Thomas S, Srivastav S, Agarwal S, Mittal V, Nadkarni B, et al. Minimally invasive plate osteosynthesis using a locking compression plate for diaphyseal humeral fractures. J Orthop Surg (Hong Kong) 2012;20:292–296. doi: 10.1177/230949901202000305. [DOI] [PubMed] [Google Scholar]
- 92.Oh CW, Byun YS, Oh JK, Kim JJ, Jeon IH, Lee JH, et al. Plating of humeral shaft fractures: comparison of standard conventional plating versus minimally invasive plating. Orthop Traumatol Surg Res. 2012;98:54–60. doi: 10.1016/j.otsr.2011.09.016. [DOI] [PubMed] [Google Scholar]
- 93.Pagonis T, Ditsios K, Christodoulou A, Petsatodis G. Outcome of surgical treatment for complicated humeral shaft fractures in elderly adults with osteoporosis. J Am Geriatr Soc. 2012;60:795–796. doi: 10.1111/j.1532-5415.2011.03876.x. [DOI] [PubMed] [Google Scholar]
- 94.Shin SJ, Sohn HS, Do NH. Minimally invasive plate osteosynthesis of humeral shaft fractures: a technique to aid fracture reduction and minimize complications. J Orthop Trauma. 2012;26:585–589. doi: 10.1097/BOT.0b013e318254895f. [DOI] [PubMed] [Google Scholar]
- 95.Tan JC, Kagda FH, Murphy D, Thambiah JS, Khong KS. Minimally invasive helical plating for shaft of humerus fractures: technique and outcome. Open Orthop J. 2012;6:184–188. doi: 10.2174/1874325001206010184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yang Q, Wang F, Wang Q, Gao W, Huang J, Wu X, et al. Surgical treatment of adult extra-articular distal humeral diaphyseal fractures using an oblique metaphyseal locking compression plate via a posterior approach. Med Princ Pract. 2012;21:40–45. doi: 10.11817/j.issn.1672-7347.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 97.Zhou ZB, Gao YS, Tang MJ, Sun YQ, Zhang CQ. Minimally invasive percutaneous osteosynthesis for proximal humeral shaft fractures with the PHILOS through the deltopectoral approach. Int Orthop. 2012;36:2341–2345. doi: 10.1007/s00264-012-1649-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Aydin BK, Akmese R, Agar M. Humeral shaft fractures secondary to hand grenade throwing. ISRN Orthop. 2013;2013:962609. doi: 10.1155/2013/962609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Biber R, Zirngibl B, Bail HJ, Stedtfeld HW. An innovative technique of rear entry creation for retrograde humeral nailing: how to avoid iatrogenic comminution. Injury. 2013;44:514–517. doi: 10.1016/j.injury.2012.12.019. [DOI] [PubMed] [Google Scholar]
- 100.Boschi V, Pogorelic Z, Gulan G, Vilovic K, Stalekar H, Bilan K, et al. Subbrachial approach to humeral shaft fractures: new surgical technique and retrospective case series study. Can J Surg. 2013;56:27–34. doi: 10.1503/cjs.011911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Chen F, Wang Z, Bhattacharyya T. Outcomes of nails versus plates for humeral shaft fractures: a Medicare cohort study. J Orthop Trauma. 2013;27:68–72. doi: 10.1007/s00264-004-0620-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kapil Mani KC, Gopal Sagar DC, Rijal L, Govinda KC, Shrestha BL. Study on outcome of fracture shaft of the humerus treated non-operatively with a functional brace. Eur J Orthop Surg Traumatol. 2013;23:323–328. doi: 10.1007/s00590-012-0982-3. [DOI] [PubMed] [Google Scholar]
- 103.Lee TJ, Kwon DG, Na SI, Cha SD. Modified combined approach for distal humerus shaft fracture: anterolateral and lateral bimodal approach. Clin Orthop Surg. 2013;5:209–215. doi: 10.4055/cios.2013.5.3.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Lee HJ, Oh CW, Oh JK, Apivatthakakul T, Kim JW, Yoon JP, et al. Minimally invasive plate osteosynthesis for humeral shaft fracture: a reproducible technique with the assistance of an external fixator. Arch Orthop Trauma Surg. 2013;133:649–657. doi: 10.1007/s00402-013-1708-7. [DOI] [PubMed] [Google Scholar]
- 105.Lian K, Wang L, Lin D, Chen Z. Minimally invasive plating osteosynthesis for mid-distal third humeral shaft fractures. Orthopedics. 2013;36:e1025–1032. doi: 10.3928/01477447-20130724-18. [DOI] [PubMed] [Google Scholar]
- 106.Sharaby M, Elhawary A. A simple technique for double plating of extraarticular distal humeral shaft fractures. Acta Orthop Belg. 2012;78:708–713. [PubMed] [Google Scholar]
- 107.Shen L, Qin H, An Z, Zeng B, Yang F. Internal fixation of humeral shaft fractures using minimally invasive plating: comparative study of two implants. Eur J Orthop Surg Traumatol. 2013;23:527–534. doi: 10.1007/s00590-012-1039-3. [DOI] [PubMed] [Google Scholar]
- 108.Tyllianakis M, Tsoumpos P, Anagnostou K, Konstantopoulou A, Panagopoulos A. Intramedullary nailing of humeral diaphyseal fractures. Is distal locking really necessary? Int J Shoulder Surg. 2013;7:65–69. doi: 10.4103/0973-6042.114233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Verdano MA, Pellegrini A, Schiavi P, Somenzi L, Concari G, Ceccarelli F. Humeral shaft fractures treated with antegrade intramedullary nailing: what are the consequences for the rotator cuff? Int Orthop. 2013;37:2001–2007. doi: 10.1007/s00264-013-2007-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Wang C, Dai G, Wang S, Liu Q, Liu W. The function and muscle strength recovery of shoulder after humeral diaphysis fracture following plating and intramedullary nailing. Arch Orthop Trauma Surg. 2013;133:1089–1094. doi: 10.1007/s00402-013-1768-8. [DOI] [PubMed] [Google Scholar]
- 111.Yi JW, Oh JK, Han SB, Shin SJ, Oh CW, Yoon YC. Healing process after rigid plate fixation of humeral shaft fractures revisited. Arch Orthop Trauma Surg. 2013;133:811–817. doi: 10.1007/s00402-013-1727-4. [DOI] [PubMed] [Google Scholar]
- 112.Yin P, Mao Z, Zhang L, Tao S, Zhang Q, Liang X, et al. Effectiveness comparison between locking compression plate fixation and locked intramedullary nail fixation for humeral shaft fracture of types B and C. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2013;27:1457–1461. [PubMed] [Google Scholar]
- 113.Balam KM, Zahrany AS. Posterior percutaneous plating of the humerus. Eur J Orthop Surg Traumatol. 2014;24:763–768. doi: 10.1007/s00590-013-1355-2. [DOI] [PubMed] [Google Scholar]
- 114.Benegas E, Ferreira Neto AA, Gracitelli ME, Malavolta EA, Assuncao JH, Prada FD, et al. Shoulder function after surgical treatment of displaced fractures of the humeral shaft: a randomized trial comparing antegrade intramedullary nailing with minimally invasive plate osteosynthesis. J Shoulder Elbow Surg. 2014 doi: 10.1016/j.jse.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 115.Huri G, Bicer OS, Ozturk H, Deveci MA, Tan I. Functional outcomes of minimal invasive percutaneous plate osteosynthesis (MIPPO) in humerus shaft fractures: a clinical study. Acta Orthop Traumatol Turc. 2014;48:406–412. doi: 10.3944/AOTT.2014.13.0009. [DOI] [PubMed] [Google Scholar]
- 116.Neuhaus V, Menendez M, Kurylo JC, Dyer GS, Jawa A, Ring D. Risk factors for fracture mobility six weeks after initiation of brace treatment of mid-diaphyseal humeral fractures. J Bone Jt Surg Am. 2014;96:403–407. doi: 10.2106/JBJS.M.00089. [DOI] [PubMed] [Google Scholar]
- 117.Radulescu R, Badila A, Nutiu O, Japie I, Terinte S, Radulescu D, et al. Osteosynthesis in fractures of the distal third of humeral diaphysis. Maedica (Buchar) 2014;9:44–48. [PMC free article] [PubMed] [Google Scholar]
- 118.Singh AK, Narsaria N, Seth RR, Garg S. Plate osteosynthesis of fractures of the shaft of the humerus: comparison of limited contact dynamic compression plates and locking compression plates. J Orthop Traumatol. 2014 doi: 10.1007/s10195-014-0290-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wali MG, Baba AN, Latoo IA, Bhat NA, Baba OK, Sharma S. Internal fixation of shaft humerus fractures by dynamic compression plate or interlocking intramedullary nail: a prospective, randomised study. Strategies Trauma Limb Reconstr. 2014;9:133–140. doi: 10.1007/s11751-014-0204-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wang X, Yin D, Liang B, Qiu D. Anterolateral minimally invasive plate osteosynthesis technique for distal humeral shaft fracture. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2014;39:1157–1162. doi: 10.11817/j.issn.1672-7347.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 121.Yin P, Zhang L, Mao Z, Zhao Y, Zhang Q, Tao S, et al. Comparison of lateral and posterior surgical approach in management of extra-articular distal humeral shaft fractures. Injury. 2014 doi: 10.1016/j.injury.2014.02.034. [DOI] [PubMed] [Google Scholar]
- 122.Zogaib RK, Morgan S, Belangero PS, Fernandes HJ, Belangero WD, Livani B. Minimal invasive ostheosintesis for treatment of diaphiseal transverse humeral shaft fractures. Acta Ortop Bras. 2014;22:94–98. doi: 10.1590/1413-78522014220200698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zogbi DR, Terrivel AM, Mouraria GG, Mongon ML, Kikuta FK, Filho AZ. Fracture of distal humerus: MIPO technique with visualization of the radial nerve. Acta Ortop Bras. 2014;22:300–303. doi: 10.1590/1413-78522014220601003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ali E, Griffiths D, Obi N, Tytherleigh-Strong G, Van Rensburg L. Nonoperative treatment of humeral shaft fractures revisited. J Shoulder Elbow Surg. 2015;24:210–214. doi: 10.1016/j.jse.2014.05.009. [DOI] [PubMed] [Google Scholar]
- 125.Campochiaro G, Baudi P, Loschi R, Serafin F, Catani F. Complex fractures of the humeral shaft treated with antegrade locked intramedullary nail: clinical experience and long-term results. Acta Biomed. 2015;86:69–76. [PubMed] [Google Scholar]
- 126.Ebrahimpour A, Najafi A, Manafi RA. Outcome assessment of operative treatment of humeral shaft fractures by antegrade Unreamed Humeral Nailing (UHN) Indian J Surg. 2015;77:186–190. doi: 10.1007/s12262-012-0756-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Esmailiejah AA, Abbasian MR, Safdari F, Ashoori K. Treatment of humeral shaft fractures: Minimally invasive plate osteosynthesis versus open reduction and internal fixation. Trauma Mon. 2015;20:e26271. doi: 10.5812/traumamon.26271v2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Fan Y, Li YW, Zhang HB, Liu JF, Han XM, Chang X, et al. Management of humeral shaft fractures with intramedullary interlocking nail versus locking compression plate. Orthopedics. 2015;38:e825–829. doi: 10.3928/01477447-20150902-62. [DOI] [PubMed] [Google Scholar]
- 129.Feng T. Fixation with intramedullary nail and plate in the treatment of adult humeral shaft fracture: Comparison of radial nerve injury and non-union rate. Chin J Tissue Eng Res. 2015;19:2086–2090. doi: 10.3969/j.issn.2095-4344.2015.13.022. [DOI] [Google Scholar]
- 130.Gallucci GL, Boretto JG, Alfie VA, Donndorff A, De Carli P. Posterior minimally invasive plate osteosynthesis (MIPO) of distal third humeral shaft fractures with segmental isolation of the radial nerve. Chir Main. 2015;34:221–226. doi: 10.1016/j.main.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 131.Hadhoud DA, Mesriga MM. Minimally invasive plate osteosynthesis versus open reduction and plate fixation of humeral shaft fractures. Menoufia Med J. 2015;28:154–161. doi: 10.4103/1110-2098.155974. [DOI] [Google Scholar]
- 132.Kim SJ, Lee SH, Son H, Lee BG. Surgical result of plate osteosynthesis using a locking plate system through an anterior humeral approach for distal shaft fracture of the humerus that occurred during a throwing motion. Int Orthop. 2015 doi: 10.1007/s00264-015-2895-2893. [DOI] [PubMed] [Google Scholar]
- 133.Koca K, Ege T, Kurklu M, Ekinci S, Bilgic S. Spiral-medial butterfly fractures (AO-12-B1) in distal diaphysis of humerus with rotational forces: preliminary results of open reduction and plate-screw fixation. Eur Rev Med Pharmacol Sci. 2015;19:4494–4497. [PubMed] [Google Scholar]
- 134.Kumar MN, Ravishankar MR, Manur R. Single locking compression plate fixation of extra-articular distal humeral fractures. J Orthop Traumatol. 2015;16:99–104. doi: 10.1007/s10195-014-0325-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Modi N, Pundkar GN. Comparative study of functional outcome of dynamic compression plating with Intramedullary Interlocking nailing in close fracture shaft of humerus in adults. J Med Dent Sci. 2015;3:298–302. doi: 10.5455/jrmds.20153412. [DOI] [Google Scholar]
- 136.Patino JM, Ramella JC, Michelini AE, Abdon IM, Rodriguez EF, Corna AFR. Plates vs nails in humeral shaft fractures: do plates lead to a better shoulder function? JSES Int. 2021;5:765–768. doi: 10.1016/j.jseint.2021.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Reddy BJ, Athmaram M, Swaroop VS. A clinical study of fixation of fracture of shaft of humerus with interlocking nail. JEMDS. 2015;4:2172–2179. doi: 10.14260/JEMDS/2015/312. [DOI] [Google Scholar]
- 138.Sahu RL, Ranjan R, Lal A. Fracture union in closed interlocking nail in humeral shaft fractures. Chin Med J (Engl) 2015;128:1428–1432. doi: 10.4103/0366-6999.157630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Sanjeevaiah RP. Minimally invasive plate osteosynthesis (Mipo) in humeral shaft fractures—biomechanics—design—clinical results. JEMDS. 2015;4:9449–9456. doi: 10.14260/jemds/2015/1368. [DOI] [Google Scholar]
- 140.Shields E, Sundem L, Childs S, Maceroli M, Humphrey C, Ketz JP, et al. The impact of residual angulation on patient reported functional outcome scores after non-operative treatment for humeral shaft fractures. Injury. 2015 doi: 10.1016/j.injury.2015.12.014. [DOI] [PubMed] [Google Scholar]
- 141.Singhal R, Stewart P, Panayiotou CC. A pre-fabricated bracing system for the management of humeral shaft fractures: experience of a centre in the United Kingdom. Ortop Traumatol Rehabil. 2015;17:463–470. doi: 10.5604/15093492.1186816. [DOI] [PubMed] [Google Scholar]
- 142.Srinivas K, Rajaiah D, Ramana Y, Omkaram S, Reddy SV. A study of surgical management of diaphyseal fractures of humerus by dynamic compression plate osteosynthesis. JEMDS. 2015;4:1290–1296. doi: 10.14260/jemds/2015/181. [DOI] [Google Scholar]
- 143.Wang C, Li J, Li Y, Dai G, Wang M. Is minimally invasive plating osteosynthesis for humeral shaft fracture advantageous compared with the conventional open technique? J Shoulder Elbow Surg. 2015;24:1741–1748. doi: 10.1016/j.jse.2015.07.032. [DOI] [PubMed] [Google Scholar]
- 144.Abril Gaona C, Arroyo CA, David AE, Plata GV. Treatment of distal diaphyseal humeral fractures with minimally invasive posterior approach and anatomical extraarticular plate. Rev Colomb Ortop Traumatol. 2018;32:178–183. doi: 10.1016/j.rccot.2017.11.005. [DOI] [Google Scholar]
- 145.Anand Kumar BS, Soraganvi P, Satyarup D. Treatment of middle third humeral shaft fractures with anteromedial plate osteosynthesis through an anterolateral approach. Malays Orthop J. 2016;10:38–43. doi: 10.5704/moj.1603.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Gang Z, Haonan L, Ning L, Liang H, Xinbao W. Comparison of mid-term surgical results between plate and intramedullary nail for humeral shaft fracture. Nat Med J China. 2016;96:2988–2992. doi: 10.3760/cma.j.issn.0376-2491.2016.37.07. [DOI] [PubMed] [Google Scholar]
- 147.Guzmán-Guevara J, López-Cázares G, Barragán-Hervella RG, Villegas-Rosas JS, Alvarado-Ortega I, Montiel-Jarquín Á. Evaluation of patients with humeral midshaft fractures treated with DCP plate vs intramedullary nail UHN. Rev Med Inst Mex Seguro Soc. 2016;54:S270–S274. [PubMed] [Google Scholar]
- 148.Karunanithi S, Anbu S, Palaniappan M, Kolundan K, Kannan K, Ganesan RP. A study of functional, clinical and radiological outcome of fracture shaft of humerus mid and distal third managed by Mippo technique. JEMDS. 2016;5:5285–5291. doi: 10.14260/jemds/2016/1198. [DOI] [Google Scholar]
- 149.Kumar S, Ul Haq SN, Iqbal SM. The complications of diaphyseal fractures of humerus treated by dynamic compression plate. Gomal J Med Sci. 2016;14:167–170. [Google Scholar]
- 150.Lee SK, Yang DS, Chang SH, Choy WS. LCP metaphyseal plate fixation for fractures of the distal third humeral shaft using brachialis splitting approach. Acta Orthop Belg. 2016;82:85–93. [PubMed] [Google Scholar]
- 151.Lee T, Yoon J. Newly designed minimally invasive plating of a humerus shaft fracture; a different introduction of the plate. Int Orthop. 2016 doi: 10.1007/s00264-015-3097-8. [DOI] [PubMed] [Google Scholar]
- 152.Lu S, Wu J, Xu S, Fu B, Dong J, Yang Y, et al. Medial approach to treat humeral mid-shaft fractures: a retrospective. J Orthop Surg Res. 2016;11:32. doi: 10.1186/s13018-016-0366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Mahajan AS, Kim YG, Kim JH, D’sa P, Lakhani A, Ok HS. Is anterior bridge plating for mid-shaft humeral fractures a suitable option for patients predominantly involved in overhead activities? A functional outcome study in athletes and manual laborers. CIOS Clin Orthop Surg. 2016;8:358–366. doi: 10.4055/cios.2016.8.4.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Mehmood M, Abdul-Rehman-Yaseen M, Farooq S. Compare the functional outcome of dynamic compression platting and locked intramedullary nailing for primary surgical fixation of non-pathological fractures of humeral shaft in adults. Pak J Med Health Sci. 2016;10:250–252. [Google Scholar]
- 155.Wahed MA, Prasad PN, Reddy N. Prospective study of management of fracture shaft of humerus with locking compression plating. JEMDS. 2016;5:1950–1953. doi: 10.14260/jemds/2016/460. [DOI] [Google Scholar]
- 156.Bisaccia M, Meccariello L, Rinonapoli G, Rollo G, Pellegrino M, Schiavone A, et al. Comparison of plate, nail and external fixation in the management of diaphyseal fractures of the humerus. Med Arch. 2017;71:97–102. doi: 10.5455/medarh.2017.71.97-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Dielwart C, Harmer L, Thompson J, Seymour RB, Karunakar MA. Management of closed diaphyseal humerus fractures in patients with injury severity score ≥17. J Orthop Trauma. 2017;31:220–224. doi: 10.1097/bot.0000000000000768. [DOI] [PubMed] [Google Scholar]
- 158.Duygun F, Aldemir C. Is locked compressive intramedullary nailing for adult humerus shaft fractures advantageous? Eklem Hastalik Cerrahisi. 2017;28:80–86. doi: 10.5606/ehc.2017.55687. [DOI] [PubMed] [Google Scholar]
- 159.Harkin FE, Large RJ. Humeral shaft fractures: union outcomes in a large cohort. J Shoulder Elbow Surg. 2017;26:1881–1188. doi: 10.1016/j.jse.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 160.Ko SH, Cha JR, Lee CC, Joo YT, Eom KS. Minimally invasive plate osteosynthesis using a screw compression method for treatment of humeral shaft fractures. CIOS Clin Orthop Surg. 2017;9:506–513. doi: 10.4055/cios.2017.9.4.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Matsunaga FT, Tamaoki MJS, Matsumoto MH, Netto NA, Faloppa F, Belloti JC. Minimally invasive osteosynthesis with a bridge plate versus a functional brace for humeral shaft fractures: A randomized controlled trial. J Bone Jt Surg Am. 2017;99:583–592. doi: 10.2106/jbjs.16.00628. [DOI] [PubMed] [Google Scholar]
- 162.Wei SH, Qinruixian BL, Guangyu D, Chuanxiu S, Xuegang S, et al. Comparison study of the clinical effect and biomechanics between locking compression plate and interlocking intramedullary nail for humerus shaft fracture. Biomed Res. 2017;28:6251–6255. [Google Scholar]
- 163.Crespo AM, Konda SR, Egol KA. Set it and forget it: diaphyseal fractures of the humerus undergo minimal change in angulation after functional brace application. Iowa Orthop J. 2018;38:73–77. [PMC free article] [PubMed] [Google Scholar]
- 164.Goncalves FF, Dau L, Grassi CA, Palauro FR, Martins Neto AA, Pereira PCG. Evaluation of the surgical treatment of humeral shaft fractures and comparison between surgical fixation methods. Rev Bras Ortop. 2018;53:136–141. doi: 10.1016/j.rboe.2017.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Ferrara F, Biancardi E, Touloupakis G, Bibiano L, Ghirardelli S, Antonini G, et al. Residual interfragmentary gap after intramedullary nailing of fragility fractures of the humeral diaphysis: short and midterm term results. Acta Biomed. 2019;90:432–438. doi: 10.23750/abm.v90i4.7315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Hosseini Khameneh SM, Abbasian M, Abrishamkarzadeh H, Bagheri S, Abdollahimajd F, Safdari F, et al. Humeral shaft fracture: a randomized controlled trial of nonoperative versus operative management (plate fixation) Orthop Res Rev. 2019;11:141–147. doi: 10.2147/orr.S212998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Mehraj M, Shah I, Mohd J, Rasool S. Early results of bridge plating of humerus diaphyseal fractures by MIPO technique. Ortop Traumatol Rehabil. 2019;21:117–121. doi: 10.5604/01.3001.0013.1915. [DOI] [PubMed] [Google Scholar]
- 168.Pooja Sri S, Subash Y. Comparison of outcome in mipo versus orif with plate osteosynthesis in the management of fractures of the shaft of humerus. Res J Pharm Technol. 2019;12:3933–3937. doi: 10.5958/0974-360x.2019.00677.2. [DOI] [Google Scholar]
- 169.Seo JB, Heo K, Yang JH, Yoo JS. Clinical outcomes of dual 3.5-mm locking compression plate fixation for humeral shaft fractures: comparison with single 4.5-mm locking compression plate fixation. J Orthop Surg. 2019 doi: 10.1177/2309499019839608. [DOI] [PubMed] [Google Scholar]
- 170.Vidović D, Benčić I, Ćuti T, Gajski D, Čengić T, Bekić M, et al. Treatment of humeral shaft fractures: antegrade interlocking intramedullary nailing with additional interlocking neutralization screws through fracture site. Acta Clin Croat. 2019;58:632–638. doi: 10.20471/acc.2019.58.04.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Wang Z, Song S, Guo Q, Yang D, Chen X, Ling J, et al. Therapeutic effect of anterior approach mipo combined with LCP in the treatment of humeral shaft fracture. Acta Med Mediterr. 2019;35:2765–2768. doi: 10.19193/0393-6384_2019_5_434. [DOI] [Google Scholar]
- 172.Yuan H, Wang R, Zheng J, Yang Y. Comparison between intramedullary nailing and minimally invasive percutaneous plate osteosynthesis in treatment of humeral shaft fractures. J Coll Phys Surg Pak. 2019;29:942–945. doi: 10.29271/jcpsp.2019.10.942. [DOI] [PubMed] [Google Scholar]
- 173.Akalin Y, Şahin İG, Çevik N, Güler BO, Avci Ö, Öztürk A. Locking compression plate fixation versus intramedullary nailing of humeral shaft fractures: which one is better? A single-centre prospective randomized study. Int Orthop. 2020;44:2113–2121. doi: 10.1007/s00264-020-04696-6. [DOI] [PubMed] [Google Scholar]
- 174.Desai NR, Patil S, Gunaki R. A comparative study of functional outcomes of fracture shaft humerus in adults treated with dynamic compression plating and interlocking nailing. Int J Res Pharm Sci. 2020;11:4944–4948. doi: 10.26452/ijrps.v11i3.2798. [DOI] [Google Scholar]
- 175.Hendy BA, Zmistowski B, Wells Z, Abboud JA, Namdari S. Humeral shaft fractures: surgical versus nonsurgical management in workers' compensation. Arch Bone Jt Surg. 2020;8:668–674. doi: 10.22038/abjs.2020.44301.2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Huichao F, Xiaoming W. Reduced surgical time and higher accuracy of distal locking with the electromagnetic targeting system in humeral shaft intramedullary nailing. Orthop Surg. 2020;12:1413–1420. doi: 10.1111/os.12785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Hussain B, Ullah Z, Hussain G, Napar AR, Latif M, Arif M. Compare the functional outcome of dynamic compression plating versus interlocking nail procedure for fracture shaft of humerus. Pak J Med Health Sci. 2020;14:1314–1316. [Google Scholar]
- 178.Omrani FA, Rezayian M, Ejlali M, Sayadi S, Baroutkoub M, Omidian MM, et al. Intramedullary nailing Vs Plate fixation for the treatment of humeral shaft fractures; which one is better? Syst Rev Pharm. 2020;11:770–774. doi: 10.31838/srp.2020.8.111. [DOI] [Google Scholar]
- 179.Rai SK, Sud AD, Kashid M, Gogoi B. Anteromedial surface plating for midshaft fracture humerus through an anterolateral approach—a better option than anterolateral plating. Malays Orthop J. 2020;14:66–72. doi: 10.5704/moj.2011.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Rämö L, Sumrein BO, Lepola V, Lähdeoja T, Ranstam J, Paavola M, et al. Effect of surgery vs functional bracing on functional outcome among patients with closed displaced humeral shaft fractures: the FISH randomized clinical trial. JAMA. 2020;323:1792–1801. doi: 10.1001/jama.2020.3182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Sharma GM, Bhardwaj AR, Shah S. Antegrade versus retrograde nailing in humeral shaft fractures: a prospective study. J Clin Orthop Traum. 2020;11:S37–S41. doi: 10.1016/j.jcot.2019.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Varghese VD, Bhowmick K, Prithishkumar IJ, Nithyananth M. Anteromedial surgical approach for minimally invasive fixation of humerus shaft fractures: a cadaveric and clinical study. Techn Shoulder Elbow Surg. 2020;21:42–49. doi: 10.1097/bte.0000000000000188. [DOI] [Google Scholar]
- 183.Wang Y, Chen H, Wang L, Chen X, Zhi X, Cui J, et al. Comparison between osteosynthesis with interlocking nail and minimally invasive plating for proximal- and middle-thirds of humeral shaft fractures. Int Orthop. 2020 doi: 10.1007/s00264-020-04869-3. [DOI] [PubMed] [Google Scholar]
- 184.Wang Y, Kayastha Y, Cao Y, Guo Z, Yuan Y, Bi Y. Outcome of humeral shaft fracture treated with intramedullary nail and plate fixation. J Coll Phys Surg Pak. 2020;30:73–78. doi: 10.29271/jcpsp.2020.01.73. [DOI] [PubMed] [Google Scholar]
- 185.Yiğit Ş. What should be the timing of surgical treatment of humeral shaft fractures? Medicine (Baltimore) 2020;99:e19858. doi: 10.1097/md.0000000000019858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Zhang R, Yin Y, Li S, Hou Z, Jin L, Zhang Y. Intramedullary nailing versus a locking compression plate for humeral shaft fracture (AO/OTA 12-A and B): a retrospective study. Orthop Traumatol: Surg Res. 2020;106:1391–1397. doi: 10.1016/j.otsr.2019.12.016. [DOI] [PubMed] [Google Scholar]
- 187.Cannada LK, Nelson L, Tornetta P, Hymes R, Jones CB, Obremskey W, et al. Operative vs nonoperative treatment of isolated humeral shaft fractures: a prospective cohort study. J Surg Orthop Adv. 2021;30:67–72. [PubMed] [Google Scholar]
- 188.Capitani P, Chiodini F, Di Mento L, Cavanna M, Bove F, Capitani D, et al. Locking compression plate fixation in humeral shaft fractures: a comparative study to literature conservative treatment. Injury. 2021 doi: 10.1016/j.injury.2021.03.027. [DOI] [PubMed] [Google Scholar]
- 189.Furuhata R, Kamata Y, Kono A, Kiyota Y, Morioka H. Influence of timing on surgical outcomes for acute humeral shaft fractures. Adv Orthop. 2021 doi: 10.1155/2021/8977630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Huang Q, Lu Y, Wang ZM, Sun L, Ma T, Wang Q, et al. Anterolateral approach with two incisions versus posterior median approach in the treatment of middle- and distal-third humeral shaft fractures. J Orthop Surg Res. 2021;16:197. doi: 10.1186/s13018-021-02355-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Kumar B, Kumar A, Mheshwari LD, Tunio ZH, Jhatiyal RA, Umrani KB. Diaphyseal humeral fractures treated by bracing versus dynamic compression plate. Pak J Med Health Sci. 2021;15:1466–1468. doi: 10.53350/pjmhs211561466. [DOI] [Google Scholar]
- 192.Mohammed MO, Mahmmod HF, Imam AHF, Almantasir FAF. Intramedullary nailing versus plating for treatment of humeral shaft fractures in adults. Eur J Mol Clin Med. 2021;8:2879–2889. [Google Scholar]
- 193.Patino JM. Treatment of humeral shaft fractures using antegrade nailing: functional outcome in the shoulder. J Shoulder Elbow Surg. 2015;24:1302–1306. doi: 10.1016/j.jse.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 194.Rellán I, Gallucci GL, Donndorff AG, De Carli P, Zaidenberg EE, Richard MJ, et al. Time until union in absolute vs relative stability MIPO plating in simple humeral shaft fractures. Eur J Orthop Surg Traumatol. 2021 doi: 10.1007/s00590-021-02920-6. [DOI] [PubMed] [Google Scholar]
- 195.Mahabier KC, Den Hartog D, Theyskens N, Verhofstad MHJ, Van Lieshout EMM, HUMMER Investigators Reliability, validity, responsiveness, and minimal important change of the disabilities of the arm, shoulder and hand and Constant–Murley scores in patients with a humeral shaft fracture. J Shoulder Elbow Surg. 2017;26:e1–e12. doi: 10.1016/j.jse.2016.07.072. [DOI] [PubMed] [Google Scholar]
- 196.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29:602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 197.Smith MV, Calfee RP, Baumgarten KM, Brophy RH, Wright RW. Upper extremity-specific measures of disability and outcomes in orthopaedic surgery. J Bone Jt Surg Am. 2012;94(3):277–285. doi: 10.2106/JBJS.J.01744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. doi: 10.1097/00003086-198701000-00023. [DOI] [PubMed] [Google Scholar]
- 199.Amstutz HC, Sew Hoy AL, Clarke IC. UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res. 1981;155:7–20. doi: 10.1097/00003086-198103000-00002. [DOI] [PubMed] [Google Scholar]
- 200.Richards RR, An KN, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347–352. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 201.Morrey BF, Adams RA. Semiconstrained arthroplasty for the treatment of rheumatoid arthritis of the elbow. J Bone Jt Surg Am. 1992;74:479–490. doi: 10.2106/00004623-199274040-00003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No additional data are available. Data can be made available upon reasonable request to the principal investigator.