Abstract
Purpose
To determine the 50 most frequently cited studies on osteochondritis dissecans (OCD) and to conduct a bibliometric analysis of these studies.
Methods
We performed a search within the Clarivate Web of Science database, identifying articles published before December 2022 that encompass topics related to OCD. The search was conducted using the keywords “Osteochondritis Dissecans OR Osteochondritis OR Dissecans.”Search results were then filtered using predetermined guidelines and criteria, and the 50 most-cited articles were selected for analysis. Extracted data included title, journal, design, main topic, joint, citations, year, country of origin, and level of evidence.
Results
The search yielded 3,865 articles. The 50 most-cited articles were published between 1957 and 2018, with the greatest proportion published from 2000 to 2009 (60%). The most frequently studied topic was treatment (68%), followed by etiology (14%) and imaging (8%). The majority of articles had Level IV evidence (36%) and the largest proportion focused on the knee joint (36%), followed by the ankle (32%), and elbow (6%). The mean citation count per article was 287 (range: 157-1,050), with the most-cited articles primarily published from 2000 to 2003. The leading country of origin was the United States, accounting for 19 publications.
Conclusions
Most of the top 50 most-cited articles regarding OCD are about treatment, and the knee is the most-studied joint. The majority of the articles were Level IV evidence and were published in the United States between 2000 and 2009.
Clinical Relevance
The top 50 most-cited studies list will provide researchers, medical students, residents, and fellows with a foundational list of the most important and influential academic contributions regarding osteochondritis dissecans (OCD).
Osteochondritis dissecans (OCD) is a joint disorder that affects the bone and secondarily cartilage, causing pain, limiting range of motion, and hindering one’s quality of life.1 The most commonly affected joint is the knee, but the condition can also occur in other joints, such as the ankle and elbow.2, 3, 4 The disorder is characterized by the separation of a portion of bone and cartilage from the surrounding healthy tissue.5 This separation typically results from a lack of blood supply to the bone, causing it to weaken and eventually die, in some cases leading to cracking and separating of the cartilage that covers it, and the formation of loose fragments.6, 7, 8 Some risk factors that increase the likelihood of developing OCD include overuse of the joint, rapid growth during adolescence, and certain genetic conditions.9, 10, 11 The prevalence of OCD is considered low in the general population. However, in certain populations, such as young athletes, the prevalence may be greater, with studies estimating it to be approximately 2% to 4%.12 OCD is also more common in male than female patients and is typically diagnosed between 10 and 20 years of age. The diagnosis of OCD can be challenging, often requiring a combination of clinical findings and diagnostic imaging to confirm. Symptoms of the disorder can range from mild to severe, and in some cases, the condition may not cause any symptoms at all.13
Despite extensive research, the exact cause of OCD remains unknown, and there is still a lack of consensus on the best diagnostic and treatment methods.14,15 Nonetheless, The American Academy of Orthopaedic Surgeons (AAOS) publishes and updates a Clinical Practice Guideline to provide evidence-based recommendations to help clinicians make informed decisions when caring for patients with OCD.13 The management of OCD depends on various factors, including the location, size, and stability of the lesion, as well as the patient’s symptoms and level of activity.11 In some cases, conservative management with rest, limitation of weight-bearing, and physical therapy may be sufficient to alleviate symptoms and promote healing,16 whereas in other cases, surgery may be required to stimulate bony healing or remove the loose fragment and repair the joint.17,18
Bibliometric analysis is a powerful research method that allows for the identification and quantification of the most influential and significant articles in a field of study. This method is performed by analyzing citations and impact and has been applied in various subspecialties of orthopaedic surgery to assess research on topics such as hip and knee pathologies19, 20, 21 and arthroscopic surgeries.22, 23, 24, 25
The purpose of this study is to determine the 50 most frequently cited studies on OCD and to conduct a bibliometric analysis of these studies. We hypothesized that the most-influential articles would predominantly focus on the treatment and outcomes of OCD, would be Level IV evidence, and would be published predominantly in the United States.
Methods
In December 2022, the Clarivate Web of Science database was searched to find articles related to OCD. The search was conducted by a trained medical student researcher (N.T.) using the key words “Osteochondritis Dissecans OR Osteochondritis OR Dissecans.” To be included in the study, articles had to be original peer-reviewed studies, such as review articles, systematic reviews, meta-analyses, and guidelines. The articles were sorted by citation count and screened by title and abstract, and duplicates or articles that did not pertain to OCD injuries, pathology, healing, or management were excluded. The top 50-cited articles were selected after full text review and data extraction was conducted by 2 medical student independent investigators. The final decision for article inclusion was made by the board-certified orthopaedic surgeon and principal investigator (K.S.).
The following data were extracted from each article: title, source journal, study design, main topic, joint addressed, citations, year, country of origin, and level of evidence. The country of origin was identified by the address of the corresponding author's affiliated institution. The articles were ranked based on the number of citations per article. If multiple articles had the same number of citations, the most recently published one received priority ranking. The Level of Evidence (I-V) was assigned through a full-text review and confirmed using the guidelines of the Journal of Bone and Joint Surgery.26 The topics covered by the articles included anatomy, imaging, etiology, epidemiology, treatment, and outcomes. Only one topic was assigned to each article through reviewer determination, selecting the most appropriate for that article.
To verify the reproducibility of the search process, a second independent researcher (R.M.) with expertise in the field attempted to replicated the search. The initial search strategy and criteria were provided to the second researcher, who conducted the search independently and results were reviewed for any discrepancies. The search process followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines for systematic reviews.
Results
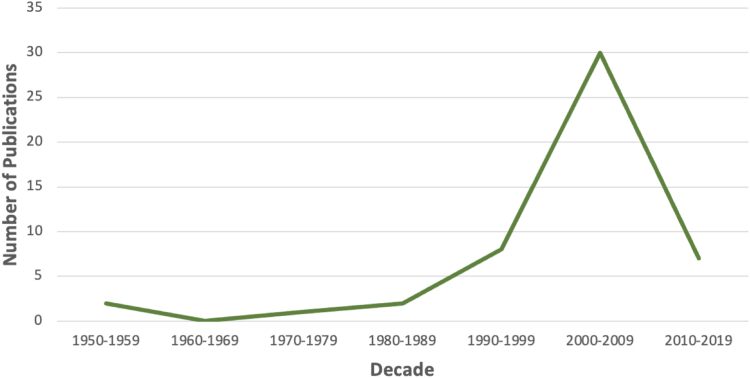
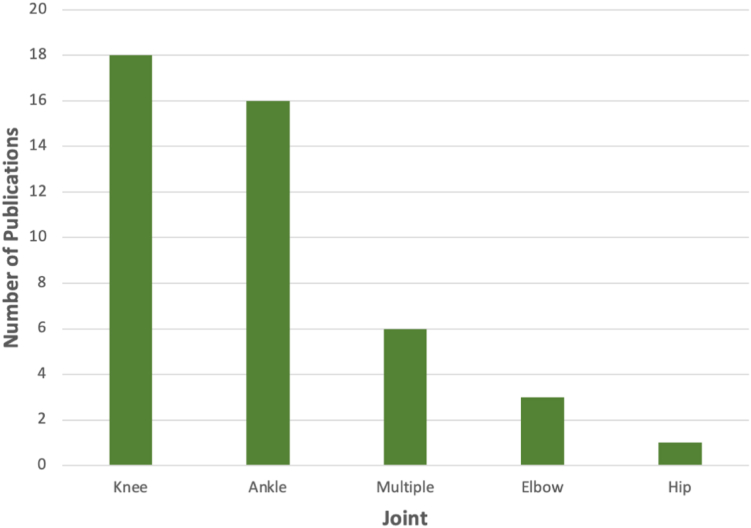
The search yielded 3,865 articles, which were ranked based on their citation count. After we screened the top 500 articles (Fig 1), 450 were excluded. This led to the final selection of 50 articles, listed in Table 1,27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53,54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73 which had a mean citation count of 287 (range: 157-1,090; median: 215). These articles were published between 1957 and 2018, with the greatest concentration of publications occurring between 2000 and 2009 (60%) and between 1990 and 1999 (32%). The remaining decades (1950s, 1980s, and 2010s) had fewer contributions, with 2, 2, and 7 publications, respectively (Fig 2). Original studies accounted for 29 of the top 50 articles (58%), with the majority being case series. 11 total articles were systematic reviews, 9 were guidelines based, and 1 clinical trial. The top 10 most-cited articles were primarily published from 2000 to 2003, accounting for 30% of those articles. The most common journal was the Journal of Bone and Joint Surgery–American Volume, contributing 24% of articles, followed by the American Journal of Sports Medicine with 20% and Clinical Orthopaedics and Related Research with 10% of all articles (Fig 3). Other journals contributed fewer than 5 articles each. The United States was the country of origin with the most publications, accounting for 19 of the 50 articles (38%) followed by Hungary and Sweden with 5 and 3 articles, respectively. The most researched topics were treatment (68%), etiology (14%), and imaging (8%) (Fig 4), with the knee being the most studied joint (36%), followed by the ankle (32%) and elbow (6%) (Fig 5). Average length of follow-up for studies pertaining to treatment was 5 years (range: 2-20). With the majority of papers discussing osteochondral autologous transplantation (OAT), bone marrow stimulation, i.e., microfracture, drilling, and autologous chondrocyte implantation (ACI).
Fig 1.
Modified Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram detailing the collection of the top 50 most cited articles pertaining to OCD. (OCD, Osteochondritis dissecans.)
Table 1.
List of Top 50 Most-Cited Articles in OCD Research
| Rank | Citation | Number of Citations |
|---|---|---|
| 1 | Peterson L, Minas T, Brittberg M, Nilsson A, Sjögren-Jansson E, Lindahl A. Two- to 9-year outcome after autologous chondrocyte transplantation of the knee. Clin Orthop Relat Res 2000;(374):212-234.27 | 1,090 |
| 2 | Brittberg M, Winalski CS. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 2003;85-A:58-69 (suppl 2).28 | 862 |
| 3 | Hangody L, Füles P. Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: Ten years of experimental and clinical experience. J Bone Joint Surg Am 2003;85-A:25-32 (suppl 2).29 | 717 |
| 4 | Berndt Al, Harty M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am 1959;41-A:988-1020.30 | 666 |
| 5 | Widuchowski W, Widuchowski J, Trzaska T. Articular cartilage defects: Study of 25,124 knee arthroscopies. Knee 2007;14:177-182.31 | 457 |
| 6 | Peterson L, Minas T, Brittberg M, Lindahl A. Treatment of osteochondritis dissecans of the knee with autologous chondrocyte transplantation: results at two to ten years. J Bone Joint Surg Am 2003;85-A 17-24 (suppl 2).32 | 457 |
| 7 | Gudas R, Kalesinskas RJ, Kimtys V, et al. A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy 2005;21:1066-1075.33 | 418 |
| 8 | Madry H, van Dijk CN, Mueller-Gerbl M. The basic science of the subchondral bone. Knee Surg Sports Traumatol Arthrosc 2010;18:419-433.5 | 369 |
| 9 | Hangody L, Kish G, Kárpáti Z, Udvarhelyi I, Szigeti I, Bély M. Mosaicplasty for the treatment of articular cartilage defects: Application in clinical practice. Orthopedics 1998;21:751-756.34 | 354 |
| 10 | Zengerink M, Struijs PA, Tol JL, van Dijk CN. Treatment of osteochondral lesions of the talus: A systematic review. Knee Surg Sports Traumatol Arthrosc 2010;18:238-246.35 | 346 |
| 11 | Bedi A, Feeley BT, Williams RJ 3rd. Management of articular cartilage defects of the knee. J Bone Joint Surg Am 2010;92:994-1009.36 | 320 |
| 12 | Marlovits S, Striessnig G, Resinger CT, et al. Definition of pertinent parameters for the evaluation of articular cartilage repair tissue with high-resolution magnetic resonance imaging. Eur J Radiol 2004;52:310-319.37 | 306 |
| 13 | Hangody L, Vásárhelyi G, Hangody LR, et al. Autologous osteochondral grafting—technique and long-term results. Injury 2008;39:S32-S39 (suppl 1).38 | 305 |
| 14 | Chuckpaiwong B, Berkson EM, Theodore GH. Microfracture for osteochondral lesions of the ankle: Outcome analysis and outcome predictors of 105 cases. Arthroscopy 2008;24:106-112.39 | 297 |
| 15 | Schenck RC Jr, Goodnight JM. Osteochondritis dissecans. J Bone Joint Surg Am 1996;78:439-456.8 | 283 |
| 16 | Cain EL Jr, Dugas JR, Wolf RS, Andrews JR. Elbow injuries in throwing athletes: A current concepts review. Am J Sports Med 2003;31:621-635.40 | 259 |
| 17 | Choi WJ, Park KK, Kim BS, Lee JW. Osteochondral lesion of the talus: is there a critical defect size for poor outcome? Am J Sports Med 2009;37:1974-1980.41 | 257 |
| 18 | Ferkel RD, Zanotti RM, Komenda GA, et al. Arthroscopic treatment of chronic osteochondral lesions of the talus: Long-term results. Am J Sports Med 2008;36:1750-1762.42 | 257 |
| 19 | Flick AB, Gould N. Osteochondritis dissecans of the talus (transchondral fractures of the talus): Review of the literature and new surgical approach for medial dome lesions. Foot Ankle 1985;5:165-185.43 | 252 |
| 20 | Kocher MS, Tucker R, Ganley TJ, Flynn JM. Management of osteochondritis dissecans of the knee: Current concepts review. Am J Sports Med 2006;34:1181-1191.11 | 246 |
| 21 | Elias I, Zoga AC, Morrison WB, Besser MP, Schweitzer ME, Raikin SM. Osteochondral lesions of the talus: Localization and morphologic data from 424 patients using a novel anatomical grid scheme. Foot Ankle Int 2007;28:154-161.44 | 246 |
| 22 | Kelly BT, Williams RJ 3rd, Philippon MJ. Hip arthroscopy: Current indications, treatment options, and management issues. Am J Sports Med 2003;31:1020-1037.45 | 243 |
| 23 | Hangody L, Kish G, Módis L, et al. Mosaicplasty for the treatment of osteochondritis dissecans of the talus: Two to seven year results in 36 patients. Foot Ankle Int 2001;22:552-558.46 | 220 |
| 24 | Imhof H, Sulzbacher I, Grampp S, Czerny C, Youssefzadeh S, Kainberger F. Subchondral bone and cartilage disease: A rediscovered functional unit. Invest Radiol 2000;35:581-588.47 | 219 |
| 25 | Gobbi A, Francisco RA, Lubowitz JH, Allegra F, Canata G. Osteochondral lesions of the talus: randomized controlled trial comparing chondroplasty, microfracture, and osteochondral autograft transplantation [published correction appears in Arthroscopy 2008;24:A16]. Arthroscopy 2006;22:1085-1092.48 | 216 |
| 26 | Linden B. Osteochondritis dissecans of the femoral condyles: A long-term follow-up study. J Bone Joint Surg Am 1977;59:769-776.49 | 215 |
| 27 | Hangody L, Feczkó P, Bartha L, Bodó G, Kish G. Mosaicplasty for the treatment of articular defects of the knee and ankle. Clin Orthop Relat Res 2001;(391 suppl):S328-S336.50 | 212 |
| 28 | Hefti F, Beguiristain J, Krauspe R, et al. Osteochondritis dissecans: A multicenter study of the European Pediatric Orthopedic Society. J Pediatr Orthop B 1999;8:231-245.51 | 210 |
| 29 | Tol JL, Struijs PA, Bossuyt PM, Verhagen RA, van Dijk CN. Treatment strategies in osteochondral defects of the talar dome: A systematic review. Foot Ankle Int 2000;21:119-126.52 | 210 |
| 30 | Emmerson BC, Görtz S, Jamali AA, Chung C, Amiel D, Bugbee WD. Fresh osteochondral allografting in the treatment of osteochondritis dissecans of the femoral condyle. Am J Sports Med 2007;35:907-914.53 | 207 |
| 31 | Jakob RP, Franz T, Gautier E, Mainil-Varlet P. Autologous osteochondral grafting in the knee: Indication, results, and reflections. Clin Orthop Relat Res 2002;(401):170-184.54 | 201 |
| 32 | Kumai T, Takakura Y, Higashiyama I, Tamai S. Arthroscopic drilling for the treatment of osteochondral lesions of the talus. J Bone Joint Surg Am 1999;81:1229-1235.55 | 201 |
| 33 | O'Loughlin PF, Heyworth BE, Kennedy JG. Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med 2010;38:392-404.56 | 199 |
| 34 | Outerbridge HK, Outerbridge AR, Outerbridge RE. The use of a lateral patellar autologous graft for the repair of a large osteochondral defect in the knee. J Bone Joint Surg Am. 1995;77:65-72.57 | 199 |
| 35 | Hepple S, Winson IG, Glew D. Osteochondral lesions of the talus: A revised classification. Foot Ankle Int 1999;20:789-793.58 | 195 |
| 36 | Giannini S, Buda R, Vannini F, Cavallo M, Grigolo B. One-step bone marrow-derived cell transplantation in talar osteochondral lesions. Clin Orthop Relat Res 2009;467:3307-3320.59 | 193 |
| 37 | Maffulli N, Longo UG, Gougoulias N, Loppini M, Denaro V. Long-term health outcomes of youth sports injuries. Br J Sports Med 2010;44:21-25.60 | 193 |
| 38 | Hughston JC, Hergenroeder PT, Courtenay BG. Osteochondritis dissecans of the femoral condyles. J Bone Joint Surg Am 1984;66:1340-1348.61 | 191 |
| 39 | Saxena A, Eakin C. Articular talar injuries in athletes: Results of microfracture and autogenous bone graft. Am J Sports Med 2007;35:1680-1687.62 | 191 |
| 40 | Selmi TA, Verdonk P, Chambat P, et al. Autologous chondrocyte implantation in a novel alginate-agarose hydrogel: Outcome at two years. J Bone Joint Surg Br 2008;90:597-604.63 | 190 |
| 41 | O'Driscoll SW, Morrey BF. Arthroscopy of the elbow. Diagnostic and therapeutic benefits and hazards. J Bone Joint Surg Am 1992;74:84-94.64 | 188 |
| 42 | Reddy S, Pedowitz DI, Parekh SG, Sennett BJ, Okereke E. The morbidity associated with osteochondral harvest from asymptomatic knees for the treatment of osteochondral lesions of the talus. Am J Sports Med 2007;35:80-85.65 | 182 |
| 43 | Takahara M, Mura N, Sasaki J, Harada M, Ogino T. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. J Bone Joint Surg Am 2007;89:1205-1214.66 | 176 |
| 44 | Roemer FW, Frobell R, Hunter DJ, et al. MRI-detected subchondral bone marrow signal alterations of the knee joint: Terminology, imaging appearance, relevance and radiological differential diagnosis. Osteoarthritis Cartilage 2009;17:1115-1131.67 | 176 |
| 45 | Kish G, Módis L, Hangody L. Osteochondral mosaicplasty for the treatment of focal chondral and osteochondral lesions of the knee and talus in the athlete. Rationale, indications, techniques, and results. Clin Sports Med 1999;18:45-66.68 | 164 |
| 46 | Gudas R, Stankevicius E, Monastyreckiene E, Pranys D, Kalesinskas RJ. Osteochondral autologous transplantation versus microfracture for the treatment of articular cartilage defects in the knee joint in athletes. Knee Surg Sports Traumatol Arthrosc 2006;14:834-842.69 | 162 |
| 47 | Alford JW, Cole BJ. Cartilage restoration, part 2: Techniques, outcomes, and future directions. Am J Sports Med 2005;33:443-460.70 | 161 |
| 48 | Krishnan Y, Grodzinsky AJ. Cartilage diseases. Matrix Biol 2018;71-72:51-69.71 | 158 |
| 49 | Levy YD, Görtz S, Pulido PA, McCauley JC, Bugbee WD. Do fresh osteochondral allografts successfully treat femoral condyle lesions? Clin Orthop Relat Res 2013;471:231-237.72 | 158 |
| 50 | Smillie Is. Treatment of osteochondritis dissecans. J Bone Joint Surg Br 1957;39-B:248-260.73 | 157 |
Fig 2.
Distribution of highest cited articles by decade, 1950s through 2010s.
Fig 3.
Distribution of highest cited articles by journal.
Fig 4.
Distribution of highest cited articles by topic researched.
Fig 5.
Distribution of highest cited articles by joint addressed.
The largest group of articles were original studies that had a level of evidence of 4 (n = 18), mainly designed as case-series studies. Level III studies followed closely (n = 17), mostly retrospective cohort studies. All articles of Level I or II evidence with highest citations are listed in Table 2.
Table 2.
Articles With level I or II Evidence
| Title | Level of Evidence | Citations | Year | Journal |
|---|---|---|---|---|
| Articular cartilage defects: Study of 25,124 knee arthroscopies31 | II | 457 | 2007 | Knee |
| A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes33 | I | 418 | 2005 | Arthroscopy |
| The basic science of the subchondral bone5 | II | 369 | 2010 | Knee Surgery Sports Traumatology Arthroscopy |
| Definition of pertinent parameters for the evaluation of articular cartilage repair tissue with high-resolution magnetic resonance imaging37 | II | 306 | 2004 | European Journal of Radiology |
| Osteochondral lesions of the talus: Localization and morphologic data from 424 patients using a novel anatomical grid scheme44 | II | 246 | 2007 | Foot & Ankle International |
| Osteochondral lesions of the talus: Randomized controlled trial comparing chondroplasty, microfracture, and osteochondral autograft transplantation48 | I | 216 | 2006 | Arthroscopy |
| Osteochondritis dissecans of femoral condyles —long-term follow-up study49 | II | 215 | 1977 | JB&JS (American Volume) |
| Mosaicplasty for the treatment of articular defects of the knee and ankle50 | II | 212 | 2001 | Clinical Orthopaedics and Related Research |
| Osteochondritis dissecans: A multicenter study of the European Pediatric Orthopedic Society51 | II | 210 | 1999 | Journal of Pediatric Orthopaedics |
| Treatment strategies in osteochondral defects of the talar dome: a systematic review52 | II | 210 | 2000 | Foot & Ankle International |
| Autologous chondrocyte implantation in a novel alginate-agarose hydrogel - Outcome at two years63 | II | 190 | 2008 | JB&JS (British Volume) |
| Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum66 | II | 176 | 2007 | JB&JS (American Volume) |
| Osteochondral autologous transplantation versus microfracture for the treatment of articular cartilage defects in the knee joint in athletes69 | I | 162 | 2006 | Knee Surgery Sports Traumatology Arthroscopy |
Discussion
The top 50 articles based on citation count span a wide range of topics but focus mostly on treatment, and the knee was identified as the most extensively studied joint (36%). The majority of articles were published between 2000 and 2009, reflecting a significant concentration of research activity during this period. The United States emerged as the leading contributor to OCD research accounting for 38% of the top 50 articles.
Most-Cited Articles
The most-cited articles in this analysis provide foundational findings on OCD treatment methods and illustrate the gaps in research on cartilage defects. These articles were of II to IV Levels of Evidence. The top article was “Two- to 9-Year Outcome After Autologous Chondrocyte Plantation of the Knee,” published in 2000 by Peterson et al.27 The article provides results from the first 101 patients treated with autologous chondrocyte transplantation for large full-thickness chondral defects of the knee.27 Of the patients in the study, 18 of 101 individuals were treated for OCD lesions and the researchers found good to excellent clinical results in 89% of these patients.27 Similarly, in 2003 Hangody and Füles29 published “Autologous Osteochondral Mosaicplasty for the Treatment of Full-Thickness Defects of Weight Bearing Joints,” which assess clinical outcomes of 831 individuals who underwent an autologous chondrocyte mosaicplasty. The authors found good-to-excellent clinical results in 92% of the patients treated with femoral condylar implantations and concluded that mosaicplasty could be an alternative treatment of small and medium-sized focal chondral and osteochondral defects.
Several of the other top articles discuss the etiology and staging of cartilage injuries. In the “Evaluation of Cartilage Injuries and Repair,” Brittberg and Winalski28 describe the International Cartilage Repair Society classifications of cartilage injuries in arthroscopic and magnetic resonance imaging evaluations. The authors discuss evaluations of several different cartilage injuries, including OCD, and the need for a universal evaluation system for these injuries. Furthermore, in “Transchondral Fractures (Osteochondritis Dissecans) of the Talus,” Berndt and Harty30 provide a foundation of the etiology of osteochondral lesions and a 4-stage radiographic classification of OCD. This article was first published in 1959 and republished in the 2004 Journal of Bone and Joint Surgery due to the foundational knowledge on OCD provided. Lastly, the fifth most cited-article, “Articular Cartilage Defects: Study of 25,124 Knee Arthroscopies,”31 provides a retrospective analysis of 25,124 knee arthroscopies performed from 1989 to 2004. The researchers found chondral lesions in 60% of the patients and 58% of the lesions were traumatic noncontact onset such as daily living activities or non-contact sports.
AAOS Clinical Practice Guideline on OCD
In 2010, The AAOS Clinical Practice Guideline (CPG) provided a framework for the diagnosis and treatment of OCD.13 These guidelines have been supported and updated by appropriate use criteria documents based on the most current evidence.74,75 However, the quality of evidence of the CPG recommendations of OCD is defined by AAOS as limited.13 The guidelines suggest that initial management for OCD involves nonoperative measures, including activity modification, physical therapy, and pain management, which has been consistently supported by the guidelines based articles reviewed in this study.28,30,36,40,41,45,68 Surgical intervention is considered for lesions that fail to improve with conservative measures, and the guideline suggests several surgical options, including drilling, fixation, and cartilage repair procedures. This manuscript's analysis of the most cited articles on OCD research provides insight into the impact and influence of articles supporting these treatment modalities, including the effectiveness and outcomes of surgical interventions,27,56,72 which is a major area of current research. Understanding the current evidence base and knowledge gaps related to OCD is crucial in guiding clinical decision-making and future research directions.
Treatment
The analyzed articles focused primarily on the treatment of OCD. As new techniques and interventions are developed, they provide promising ways to restore joint function. Effective management and treatment are crucial in preventing progression and improving the chances of full recovery. Mild cases may respond well to conservative options like physical therapy, bracing, and pain management with medications, while severe cases may require surgery to repair or replace the affected joint. Arthroscopic treatment was generally effective, requiring less invasive and postoperative immobilization.
Although the AAOS CPG does not definitively recommend a specific cartilage repair technique when treating OCD,13 a highly discussed treatment option in the articles analyzed in this study was ACI. This procedure has gained popularity as a means of treating OCD, especially due to its potential to restore joint function and improve outcomes. A recent study assessing the long-term follow-up after ACI showed favorable outcomes after this operation with only about a 3% conversion rate to total knee arthroplasty.76 Long-term follow-up is important in understanding the progression of the condition and evaluating the effectiveness of management and treatment, as the long-term outcome of OCD management is not well understood. Further long-term follow-up studies are necessary to increase understanding of the benefits and limitations the multitude of treatment options for OCD.
Etiology
Articles discussing the etiology of OCD were also popular among researchers as the exact cause of the condition not yet fully understood. The articles in the current study suggest that OCD results from a combination of genetic and environmental factors, such as variations in genes involved in bone metabolism and blood vessel formation, overuse of the joint, rapid growth during adolescence, and certain sports activities.6,10,28 One idea is the recognition of the subchondral bone's crucial role, both in its anatomy and pathophysiology. The subchondral bone is highlighted as an area often overlooked, despite its significance in the development of targeted therapies for osteochondral defects.28,47 The challenges associated with these conditions, including diagnostic delays due to cartilage's aneural nature and difficulties in drug delivery due to its avascular nature, were also addressed.62 These findings collectively underscore the complexity of cartilage-related disorders and the importance of continued research and therapeutic development in this field.10
Joint Addressed
Most articles in the analysis focused on OCD of the knee, with the ankle being a close second. The complexity of the ankle joint, made up of 3 bones, makes it more susceptible to injury and is increasingly studied, particularly among young athletes participating in high-stress sports (i.e., basketball, soccer, and gymnastics).35 Advances in imaging technology have made it easier to diagnose OCD of the ankle, leading to an increase in research on the condition. With more studies being conducted on OCD in other joints, such as the elbow, researchers have gained a deeper understanding of the condition and its underlying causes, which can be applied to the study of OCD in the most commonly affected joints.
-
•
Knee: The findings related to knee osteochondritis highlight the effectiveness of ACI, with good-to-excellent clinical results reported.27 Epidemiologic studies have assessed the prevalence and etiology of knee articular cartilage lesions, indicating common occurrences on the patellar articular surface and medial femoral condyle.53,56 Another study compared mosaic-type OAT and microfracture favored the former, showing better clinical scores and higher rates of athletes returning to sports.33 Long-term outcomes of fresh OAT revealed sustained improvements in pain and function, with graft survivorship at 20 years, albeit with some reoperations.65
-
•
Ankle: Studies explored various treatment strategies, including non-operative and operative management. Notably, OATs, bone marrow stimulation, and ACI demonstrated success rates ranging from 76% to 87%.35 Lesion size was identified as a crucial prognostic factor.39,41 Surgical approaches varied by lesion size and location, with autogenous osteochondral transplantation recommended for larger or unstable lesions.41
-
•
Elbow: Studies discussed injury mechanism associated with repetitive overhead throwing, leading to acute or chronic injuries.64,66 It stresses the importance of understanding elbow anatomy and biomechanics for accurate diagnosis and treatment. A risk–benefit analysis showed positive results for elbow arthroscopy in a majority of patients, particularly in cases of loose bodies.64 The classification of OCD of the capitellum influenced the choice of treatment, emphasizing stability as a key factor.66
Limitations
The primary limitation of this bibliometric analysis is that it only includes the most highly cited works on OCD research. High-impact studies from the past 5 years may have been excluded, as well as articles not available in the public domain like those published in textbooks, nonindexed journals, or privately cited articles. The number of absolute citations may also be inflated by subpublications, which are difficult to control for with this study design. In addition, historical articles that have been available for a longer period may be cited more frequently. However, this observation was not appreciated in our study, considering the top 10 articles with the highest citations were all published within the past 2 decades.
In addition, to maintain consistency in our data collection process, our study used data exclusively from the Clarivate Web of Science database for the identification and analysis of the top-cited articles. Although this source is recognized for its extensive coverage of academic literature, we acknowledge that the decision to use a single database has certain limitations. One primary limitation is the potential for database-specific biases. Different databases may index articles differently, which could result in variations in the selection of highly cited articles. Therefore, it is important to recognize that this may have resulted in the omission of relevant articles that are indexed exclusively in other databases.
Conclusions
Most of the top 50 most-cited articles regarding OCD are about treatment and the knee is the most-studied joint. The majority of the articles were Level IV evidence and were published in the United States between 2000 and 2009.
Supplementary Data
References
- 1.Nepple J.J., Milewski M.D., Shea K.G. Research in osteochondritis dissecans of the knee: 2016 update. J Knee Surg. 2016;29:533–538. doi: 10.1055/s-0036-1586723. [DOI] [PubMed] [Google Scholar]
- 2.Kessler J.I., Weiss J.M., Nikizad H., et al. Osteochondritis dissecans of the ankle in children and adolescents: demographics and epidemiology. Am J Sports Med. 2014;42:2165–2171. doi: 10.1177/0363546514538406. [DOI] [PubMed] [Google Scholar]
- 3.Zanon G., Di Vivo G., Marullo M. Osteochondritis dissecans of the talus. Joints. 2014;2:115–123. doi: 10.11138/jts/2014.2.3.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malik S.S., Rasodivic D., Saeed A., Jordan R.W., Maclean S., I Bain G. Management of osteochondritis dissecans (OCD) of the elbow trochlea in the adolescent population: A systematic review. Shoulder Elbow. 2022;14:415–425. doi: 10.1177/17585732221079585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Madry H., van Dijk C.N., Mueller-Gerbl M. The basic science of the subchondral bone. Knee Surg Sports Traumatol Arthrosc. 2010;18:419–433. doi: 10.1007/s00167-010-1054-z. [DOI] [PubMed] [Google Scholar]
- 6.Barrie H.J. Hypothesis—a diagram of the form and origin of loose bodies in osteochondritis dissecans. J Rheumatol. 1984;11:512–513. [PubMed] [Google Scholar]
- 7.Olstad K., Shea K.G., Cannamela P.C., et al. Juvenile osteochondritis dissecans of the knee is a result of failure of the blood supply to growth cartilage and osteochondrosis. Osteoarthritis Cartilage. 2018;26:1691–1698. doi: 10.1016/j.joca.2018.06.019. [DOI] [PubMed] [Google Scholar]
- 8.Schenck R.C.J., Goodnight J.M. Current concept review—osteochondritis dissecans∗. J Bone Joint Surg Am. 1996;78:439–456. [PubMed] [Google Scholar]
- 9.Yellin J.L., Trocle A., Grant S.F.A., Hakonarson H., Shea K.G., Ganley T.J. Candidate loci are revealed by an initial genome-wide association study of juvenile osteochondritis dissecans. J Pediatr Orthop. 2017;37:e32–e36. doi: 10.1097/BPO.0000000000000660. [DOI] [PubMed] [Google Scholar]
- 10.Chau M.M., Klimstra M.A., Wise K.L., et al. Osteochondritis dissecans. J Bone Joint Surg Am. 2021;103:1132–1151. doi: 10.2106/JBJS.20.01399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kocher M.S., Tucker R., Ganley T.J., Flynn J.M. Management of osteochondritis dissecans of the knee: current concepts review. Am J Sports Med. 2006;34:1181–1191. doi: 10.1177/0363546506290127. [DOI] [PubMed] [Google Scholar]
- 12.Kessler J.I., Nikizad H., Shea K.G., Jacobs J.C., Bebchuk J.D., Weiss J.M. The demographics and epidemiology of osteochondritis dissecans of the knee in children and adolescents. Am J Sports Med. 2014;42:320–326. doi: 10.1177/0363546513510390. [DOI] [PubMed] [Google Scholar]
- 13.Chambers H.G., Shea K.G., Carey J.L. AAOS Clinical Practice Guideline: Diagnosis and treatment of osteochondritis dissecans. J Am Acad Orthop Surg. 2011;19:307–309. doi: 10.5435/00124635-201105000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Heyworth B.E., Edmonds E.W., Kocher M.S., et al. Variation in surgical treatment of knee osteochondritis dissecans (OCD) among high-volume OCD surgeons. Orthop J Sports Med. 2015;3 (7_suppl 2) [Google Scholar]
- 15.Carey J.L., Grimm N.L. Treatment algorithm for osteochondritis dissecans of the knee. Clin Sports Med. 2014;33:375–382. doi: 10.1016/j.csm.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 16.Andriolo L., Candrian C., Papio T., Cavicchioli A., Perdisa F., Filardo G. Osteochondritis dissecans of the knee—conservative treatment strategies: A systematic review. Cartilage. 2019;10:267–277. doi: 10.1177/1947603518758435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ewing J.W., Voto S.J. Arthroscopic surgical management of osteochondritis dissecans of the knee. Arthrosc J Arthrosc Relat Surg. 1988;4:37–40. doi: 10.1016/s0749-8063(88)80010-0. [DOI] [PubMed] [Google Scholar]
- 18.Kramer D.E., Yen Y.M., Simoni M.K., et al. Surgical management of osteochondritis dissecans lesions of the patella and trochlea in the pediatric and adolescent population. Am J Sports Med. 2015;43:654–662. doi: 10.1177/0363546514562174. [DOI] [PubMed] [Google Scholar]
- 19.Arshi A., Siesener N.J., McAllister D.R., Williams R.J., Sherman S.L., Jones K.J. The 50 most cited articles in orthopedic cartilage surgery. Cartilage. 2016;7:238–247. doi: 10.1177/1947603515621997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luxenburg D., Destine H., Rizzo M.G., et al. The 50 most cited articles in knee medial collateral ligament injury research. Orthop J Sports Med. 2022;10 doi: 10.1177/23259671221124575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang W., Tang N., Li X., George D.M., He G., Huang T. The top 100 most cited articles on total hip arthroplasty: a bibliometric analysis. J Orthop Surg. 2019;14:412. doi: 10.1186/s13018-019-1476-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moore M.L., Pollock J.R., McQuivey K.S., Bingham J.S. The top 50 most-cited shoulder arthroscopy studies. Arthrosc Sports Med Rehabil. 2021;3:e277–e287. doi: 10.1016/j.asmr.2020.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murphy S.N., Moore M.L., Pollock J.R., McQuivey K.S., Bingham J.S. The top 50 most-cited knee arthroscopy studies. Arthrosc Sports Med Rehabil. 2021;3:e1243–e1253. doi: 10.1016/j.asmr.2021.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee S., Shin J., Haro M., et al. Fifty most cited articles for femoroacetabular impingement and hip arthroscopy. Front Surg. 2015;2 doi: 10.3389/fsurg.2015.00041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barbera J., Selverian S., Courington R., Mikhail C., Colvin A. The top 50 most influential articles in hip arthroscopy. Arthroscopy. 2020;36:716–722. doi: 10.1016/j.arthro.2019.09.031. [DOI] [PubMed] [Google Scholar]
- 26.Wright J.G., Swiontkowski M.F., Heckman J.D. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85:1. [PubMed] [Google Scholar]
- 27.Peterson L., Minas T., Brittberg M., Nilsson A., Sjögren-Jansson E., Lindahl A. Two- to 9-year outcome after autologous chondrocyte transplantation of the knee. Clin Orthop. 2000;374:212–234. doi: 10.1097/00003086-200005000-00020. [DOI] [PubMed] [Google Scholar]
- 28.Brittberg M., Winalski C.S. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85-A(suppl 2):58–69. doi: 10.2106/00004623-200300002-00008. [DOI] [PubMed] [Google Scholar]
- 29.Hangody L., Füles P. Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: Ten years of experimental and clinical experience. J Bone Joint Surg Am. 2003;85-A(suppl 2):25–32. doi: 10.2106/00004623-200300002-00004. [DOI] [PubMed] [Google Scholar]
- 30.Berndt A.L., Harty M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 1959;41-A:988–1020. [PubMed] [Google Scholar]
- 31.Widuchowski W., Widuchowski J., Trzaska T. Articular cartilage defects: Study of 25,124 knee arthroscopies. Knee. 2007;14:177–182. doi: 10.1016/j.knee.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 32.Peterson L., Minas T., Brittberg M., Lindahl A. Treatment of osteochondritis dissecans of the knee with autologous chondrocyte transplantation: Results at two to ten years. J Bone Joint Surg Am. 2003;85-A(suppl 2):17–24. doi: 10.2106/00004623-200300002-00003. [DOI] [PubMed] [Google Scholar]
- 33.Gudas R., Kalesinskas R.J., Kimtys V., et al. A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy. 2005;21:1066–1075. doi: 10.1016/j.arthro.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 34.Hangody L., Kish G., Kárpáti Z., Udvarhelyi I., Szigeti I., Bély M. Mosaicplasty for the treatment of articular cartilage defects: Application in clinical practice. Orthopedics. 1998;21:751–756. doi: 10.3928/0147-7447-19980701-04. [DOI] [PubMed] [Google Scholar]
- 35.Zengerink M., Struijs P.A.A., Tol J.L., van Dijk C.N. Treatment of osteochondral lesions of the talus: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2010;18:238–246. doi: 10.1007/s00167-009-0942-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bedi A., Feeley B.T., Williams R.J.I. Management of articular cartilage defects of the knee. J Bone Joint Surg Am. 2010;92:994–1009. doi: 10.2106/JBJS.I.00895. [DOI] [PubMed] [Google Scholar]
- 37.Marlovits S., Striessnig G., Resinger C.T., et al. Definition of pertinent parameters for the evaluation of articular cartilage repair tissue with high-resolution magnetic resonance imaging. Eur J Radiol. 2004;52:310–319. doi: 10.1016/j.ejrad.2004.03.014. [DOI] [PubMed] [Google Scholar]
- 38.Hangody L., Vásárhelyi G., Hangody L.R., et al. Autologous osteochondral grafting—technique and long-term results. Injury. 2008;39(suppl 1):S32–S39. doi: 10.1016/j.injury.2008.01.041. [DOI] [PubMed] [Google Scholar]
- 39.Chuckpaiwong B., Berkson E.M., Theodore G.H. Microfracture for osteochondral lesions of the ankle: Outcome analysis and outcome predictors of 105 cases. Arthroscopy. 2008;24:106–112. doi: 10.1016/j.arthro.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 40.Cain E.L., Dugas J.R., Wolf R.S., Andrews J.R. Elbow injuries in throwing athletes: A current concepts review. Am J Sports Med. 2003;31:621–635. doi: 10.1177/03635465030310042601. [DOI] [PubMed] [Google Scholar]
- 41.Choi W.J., Park K.K., Kim B.S., Lee J.W. Osteochondral lesion of the talus: Is there a critical defect size for poor outcome? Am J Sports Med. 2009;37:1974–1980. doi: 10.1177/0363546509335765. [DOI] [PubMed] [Google Scholar]
- 42.Ferkel R.D., Zanotti R.M., Komenda G.A., et al. Arthroscopic treatment of chronic osteochondral lesions of the talus: Long-term results. Am J Sports Med. 2008;36:1750–1762. doi: 10.1177/0363546508316773. [DOI] [PubMed] [Google Scholar]
- 43.Flick A.B., Gould N. Osteochondritis dissecans of the talus (transchondral fractures of the talus): Review of the literature and new surgical approach for medial dome lesions. Foot Ankle. 1985;5:165–185. doi: 10.1177/107110078500500403. [DOI] [PubMed] [Google Scholar]
- 44.Elias I., Zoga A.C., Morrison W.B., Besser M.P., Schweitzer M.E., Raikin S.M. Osteochondral lesions of the talus: Localization and morphologic data from 424 patients using a novel anatomical grid scheme. Foot Ankle Int. 2007;28:154–161. doi: 10.3113/FAI.2007.0154. [DOI] [PubMed] [Google Scholar]
- 45.Kelly B.T., Williams R.J., Philippon M.J. Hip arthroscopy: Current indications, treatment options, and management issues. Am J Sports Med. 2003;31:1020–1037. doi: 10.1177/03635465030310060701. [DOI] [PubMed] [Google Scholar]
- 46.Hangody L., Kish G., Módis L., et al. Mosaicplasty for the treatment of osteochondritis dissecans of the talus: Two to seven year results in 36 patients. Foot Ankle Int. 2001;22:552–558. doi: 10.1177/107110070102200704. [DOI] [PubMed] [Google Scholar]
- 47.Imhof H., Sulzbacher I., Grampp S., Czerny C., Youssefzadeh S., Kainberger F. Subchondral bone and cartilage disease: A rediscovered functional unit. Invest Radiol. 2000;35:581–588. doi: 10.1097/00004424-200010000-00004. [DOI] [PubMed] [Google Scholar]
- 48.Gobbi A., Francisco R.A., Lubowitz J.H., Allegra F., Canata G. Osteochondral lesions of the talus: Randomized controlled trial comparing chondroplasty, microfracture, and osteochondral autograft transplantation [published correction appears in Arthroscopy 2008;24:A16] Arthroscopy. 2006;22:1085–1092. doi: 10.1016/j.arthro.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 49.Linden B. Osteochondritis dissecans of the femoral condyles: A long-term follow-up study. J Bone Joint Surg Am. 1977;59:769–776. [PubMed] [Google Scholar]
- 50.Hangody L., Feczkó P., Bartha L., Bodó G., Kish G. Mosaicplasty for the treatment of articular defects of the knee and ankle. Clin Orthop Relat Res. 2001;(391 suppl):S328–S336. doi: 10.1097/00003086-200110001-00030. [DOI] [PubMed] [Google Scholar]
- 51.Hefti F., Beguiristain J., Krauspe R., et al. Osteochondritis dissecans: A multicenter study of the European Pediatric Orthopedic Society. J Pediatr Orthop B. 1999;8:231–245. [PubMed] [Google Scholar]
- 52.Tol J.L., Struijs P.A., Bossuyt P.M., Verhagen R.A., van Dijk C.N. Treatment strategies in osteochondral defects of the talar dome: A systematic review. Foot Ankle Int. 2000;21:119–126. doi: 10.1177/107110070002100205. [DOI] [PubMed] [Google Scholar]
- 53.Emmerson B.C., Görtz S., Jamali A.A., Chung C., Amiel D., Bugbee W.D. Fresh osteochondral allografting in the treatment of osteochondritis dissecans of the femoral condyle. Am J Sports Med. 2007;35:907–914. doi: 10.1177/0363546507299932. [DOI] [PubMed] [Google Scholar]
- 54.Jakob R.P., Franz T., Gautier E., Mainil-Varlet P. Autologous osteochondral grafting in the knee: Indication, results, and reflections. Clin Orthop Relat Res. 2002;401:170–184. doi: 10.1097/00003086-200208000-00020. [DOI] [PubMed] [Google Scholar]
- 55.Kumai T., Takakura Y., Higashiyama I., Tamai S. Arthroscopic drilling for the treatment of osteochondral lesions of the talus. J Bone Joint Surg Am. 1999;81:1229–1235. doi: 10.2106/00004623-199909000-00004. [DOI] [PubMed] [Google Scholar]
- 56.O’Loughlin P.F., Heyworth B.E., Kennedy J.G. Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med. 2010;38:392–404. doi: 10.1177/0363546509336336. [DOI] [PubMed] [Google Scholar]
- 57.Outerbridge H.K., Outerbridge A.R., Outerbridge R.E. The use of a lateral patellar autologous graft for the repair of a large osteochondral defect in the knee. J Bone Joint Surg Am. 1995;77:65–72. doi: 10.2106/00004623-199501000-00009. [DOI] [PubMed] [Google Scholar]
- 58.Hepple S., Winson I.G., Glew D. Osteochondral lesions of the talus: A revised classification. Foot Ankle Int. 1999;20:789–793. doi: 10.1177/107110079902001206. [DOI] [PubMed] [Google Scholar]
- 59.Giannini S., Buda R., Vannini F., Cavallo M., Grigolo B. One-step bone marrow-derived cell transplantation in talar osteochondral lesions. Clin Orthop Relat Res. 2009;467:3307–3320. doi: 10.1007/s11999-009-0885-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Maffulli N., Longo U.G., Gougoulias N., Loppini M., Denaro V. Long-term health outcomes of youth sports injuries. Br J Sports Med. 2010;44:21–25. doi: 10.1136/bjsm.2009.069526. [DOI] [PubMed] [Google Scholar]
- 61.Hughston J.C., Hergenroeder P.T., Courtenay B.G. Osteochondritis dissecans of the femoral condyles. J Bone Joint Surg Am. 1984;66:1340–1348. [PubMed] [Google Scholar]
- 62.Saxena A., Eakin C. Articular talar injuries in athletes: Results of microfracture and autogenous bone graft. Am J Sports Med. 2007;35:1680–1687. doi: 10.1177/0363546507303561. [DOI] [PubMed] [Google Scholar]
- 63.Selmi T.A., Verdonk P., Chambat P., et al. Autologous chondrocyte implantation in a novel alginate-agarose hydrogel: Outcome at two years. J Bone Joint Surg Br. 2008;90:597–604. doi: 10.1302/0301-620X.90B5.20360. [DOI] [PubMed] [Google Scholar]
- 64.O’Driscoll S.W., Morrey B.F. Arthroscopy of the elbow. Diagnostic and therapeutic benefits and hazards. J Bone Joint Surg Am. 1992;74:84–94. [PubMed] [Google Scholar]
- 65.Reddy S., Pedowitz D.I., Parekh S.G., Sennett B.J., Okereke E. The morbidity associated with osteochondral harvest from asymptomatic knees for the treatment of osteochondral lesions of the talus. Am J Sports Med. 2007;35:80–85. doi: 10.1177/0363546506290986. [DOI] [PubMed] [Google Scholar]
- 66.Takahara M., Mura N., Sasaki J., Harada M., Ogino T. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. J Bone Joint Surg Am. 2007;89:1205–1214. doi: 10.2106/JBJS.F.00622. [DOI] [PubMed] [Google Scholar]
- 67.Roemer F.W., Frobell R., Hunter D.J., et al. MRI-detected subchondral bone marrow signal alterations of the knee joint: Terminology, imaging appearance, relevance and radiological differential diagnosis. Osteoarthritis Cartilage. 2009;17:1115–1131. doi: 10.1016/j.joca.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 68.Kish G., Módis L., Hangody L. Osteochondral mosaicplasty for the treatment of focal chondral and osteochondral lesions of the knee and talus in the athlete: Rationale, indications, techniques, and results. Clin Sports Med. 1999;18:45–66. doi: 10.1016/s0278-5919(05)70129-0. [DOI] [PubMed] [Google Scholar]
- 69.Gudas R., Stankevicius E., Monastyreckiene E., Pranys D., Kalesinskas R.J. Osteochondral autologous transplantation versus microfracture for the treatment of articular cartilage defects in the knee joint in athletes. Knee Surg Sports Traumatol Arthrosc. 2006;14:834–842. doi: 10.1007/s00167-006-0067-0. [DOI] [PubMed] [Google Scholar]
- 70.Alford J.W., Cole B.J. Cartilage restoration, part 2: Techniques, outcomes, and future directions. Am J Sports Med. 2005;33:443–460. doi: 10.1177/0363546505274578. [DOI] [PubMed] [Google Scholar]
- 71.Krishnan Y., Grodzinsky A.J. Cartilage diseases. Matrix Biol. 2018;71-72:51–69. doi: 10.1016/j.matbio.2018.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Levy Y.D., Görtz S., Pulido P.A., McCauley J.C., Bugbee W.D. Do fresh osteochondral allografts successfully treat femoral condyle lesions? Clin Orthop. 2013;471:231–237. doi: 10.1007/s11999-012-2556-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Smillie Is. Treatment of osteochondritis dissecans. J Bone Joint Surg Br. 1957;39-B:248–260. doi: 10.1302/0301-620X.39B2.248. [DOI] [PubMed] [Google Scholar]
- 74.Carey J.L., Shea K.G. AAOS Appropriate Use Criteria: Management of osteochondritis dissecans of the femoral condyle. J Am Acad Orthop Surg. 2016;24:e105. doi: 10.5435/JAAOS-D-16-00227. [DOI] [PubMed] [Google Scholar]
- 75.Shea K.G., Carey J.L., Brown G.A., Murray J.N., Pezold R., Sevarino K.S. Management of osteochondritis dissecans of the femoral condyle. J Am Acad Orthop Surg. 2016;24:e102. doi: 10.5435/JAAOS-D-16-00226. [DOI] [PubMed] [Google Scholar]
- 76.Carey J.L., Shea K.G., Lindahl A., Vasiliadis H.S., Lindahl C., Peterson L. Autologous chondrocyte implantation as treatment for unsalvageable osteochondritis dissecans: 10- to 25-year follow-up. Am J Sports Med. 2020;48:1134–1140. doi: 10.1177/0363546520908588. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.